Professional Documents
Culture Documents
Acupuncture (Reseach Ion
Uploaded by
Ralph NicolasOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acupuncture (Reseach Ion
Uploaded by
Ralph NicolasCopyright:
Available Formats
CENTRO ESCOLAR UNIVERSITY COLLEGE OF NURSING MENDOLA, MANILA
CLINICAL RESEARCH (FINALS)
Using Acupuncture for Acute Pain in Hospitalized Children
Submitted by: BSN4E0 Brotonel, Karren Cassandra Nicolas, Keith BSN4E1 Almacen, Hannah Grace Cuenco, Jhannel Lyn Ejanda, Yasmeen Hall, Arianne Caress Llanes, Florence Mae Loberiano, Aivyn Portuguez, Emily Gapatan, Dan Wayne Juan, Jay Ryan Pelayo, Christopher
Submitted to: Ms. Grace Pascua Aruta, RN February 12, 2011
CHAPTER 1 The Problem and Its Background
Introduction There has been a nationwide increase in attention to the assessment and management of pediatric pain. Despite the increased knowledge and advances in pediatric pain, acute pain in hospitalized children remains a significant problemthat is difficult to manage in everyday clinical practice. Children admitted to the pediatric intensive care unit are especially at risk for painand its associated adverse physiologic responses, including increased oxygen consumption, atelectasis, increased work of breathing, hypertension, and tachyarrhythmia. Management of acute pain is best accomplished using a multifaceted approach involving both pharmacologic and nonpharmacologic therapies. Using
nonpharmacologic treatments may be beneficial by reducing the need for opioids or other analgesics and subsequent drug-induced side effects, such as nausea and vomiting, respiratory depression, and ileus. Recently, complementary and alternative medical therapies, such as acupuncture, have become widely accepted. In fact, as of 2005, about a one-third of pediatric pain management services affiliated with major universities offer acupuncture, primarily for chronic pain management. Acupuncture was developed >2500 years ago in China according to the theory that energy, or qi, flows although pathways, or meridians, within the body. In the Chinese medical model, blockages along the meridians of energy result in pain and disease. Acupuncture needles placed at identifiable acupuncture points close to the skin may restore the flow of energy. The biomedical explanation is that placing acupuncture needles at specific pain points releases endogenous opioid peptides, such as betaendorphin, and perhaps other neurotransmitters and neurohormones in the brain. Clinically, acupuncture can help with adult postoperative and chemotherapy nausea and vomiting as well as postoperative dental pain. Although most studies of acupuncture for pain control are in adults, there are some studies in pediatric chronic pain, such as in migraine headachesand cystic fibrosis. However, there are limited data on the use of acupuncture for acute pain in hospitalized children. Therefore, the objectives of the study were to primarily determine the feasibility and acceptability of acupuncture as an adjunctive treatment for acute pain in critically ill, postoperative children in the hospital setting and secondarily collect important preliminary data required to design future randomized controlled trials.
Statement of the Problem This study aims to determine the effectiveness of Acupuncture for acute pain in hospitalized children.
1. Is acupuncture and acupressure still applicable even there are high technological medicines? 2. What are the effect of acupuncture and acupressure to the patient experiencing pain? 3. Is it beneficial or is it going to worsen the patients condition? Significance of the Study This study regarding the effects of acupuncture and acupressure in treating pain would give importance to: Patients This study will help the patients especially to those who are experiencing so much pain and to know some alternative pain managements for them. Nursing Profession This study will help our profession to assist the nurses in recognizing his/her accountability in effectively managing patients pain through assessment, right intervention and advocacy.
CHAPTER 2 Review of Related Literature Local Literature
Acupuncture for asthma may sound like an odd combination. One is a common disease that affects approximately 20 million Americans; the other is a mysterious, esoteric, alternative medicine technique. Lots of people have asthma, but not many people have tried acupuncture. But if you are an asthma sufferer, it can seem at times that anything even something as mysterious as acupuncture is worth trying. does acupuncture for asthma work of doctors and scientists who have been trained in traditional, Western medicine and scientific methodology, and the answer will be quite different. Acupuncture, they say, is as interesting phenomenon, but the question of how it works is less important than the question does it work, and their answer to that is no. There is no conclusive evidence that acupuncture for asthma works, and a review of the scientific studies that have attempted to answer this question have not proven acupuncture to be a viable technique for treating asthma. If there are reports that it works, these can be explained by the placebo effect (The placebo effect states that medications or medical techniques/ procedures may be perceived by the patient as effective because they believe they are effective, but there is no measurable effect). So can acupuncture truly help someone who suffers from asthma? That seems to depend on your point of view. If you feel that illness is caused by disruption in energy flow and you are convinced by anecdotal reports, the only reasonable answer is: try it and find out. Acupuncture for asthma is very safe; serious adverse effects are very rare. But if you are the type of person who needs proof in the traditional sense, it may make more sense to stick with the medications/therapies you are taking and wait for solid evidence that acupuncture can help treat your asthma.
At 70, Dr. Maria Miguela Santiago remains active in her brand of community health work in this town. This eye, ear, nose and throat specialist has been helping people restore or retain good health by combining the use of western medical approaches and acupuncture for cure. She has also been applying the two alternative methods to ease disorders like rheumatism, she gout, has migraine, trained hypertension people, and mostly body pains. to
A licensed acupuncturist,
1,442
mothers,
do acupressure on sick relatives and neighbors. Santiago has done these in the last 36 years, during much of the 44 years since she moved into this town from San Pablo City in Laguna in 1966. She has not lost love for this former Pampanga business capital, especially the old Betis district, because this was her husband Manuels beloved place, where they built their family and worked as a team in bringing services to common people. To people here, she is Doctora Leleng and her late husband, Attorney Manoling. Manuel gave free legal services to the poor, taught new planting techniques to Aetas and lowland farmers and introduced baseball to poor boys and girls. He died in 2005, after serving as Guagua mayor and bringing reforms to the town. Santiago began practicing acupuncture in 1974, 11 years after she finished medicine at the University of Santo Tomas. She trained under Dr. Helen Paulino-Abundo, director of the Philippine Acupuncture Center and among the first Filipinos who trained in China. Then she turned to acupuncture in treating patients with tinnitus (Menieres syndrome or ringing in the ears), later vertigo and sudden blindness. Santiago says she does not advise patients to stop seeing doctors.
Foreign Literature Postoperative pain management remains a significant challenge for healthcare providers. Many patients experience pain after surgery, with about 86% reporting moderate, severe, or extreme pain. Opioids remain the mainstay for postoperative pain control. However, opioid analgesics are associated with undesirable side-effects, including nausea, vomiting, pruritus, sedation, dizziness, and decreased gut motility which can lead to delayed postoperative recovery.The use of adjunct analgesics that provide opioid-sparing effects and decrease the incidence of opioid-related side-effects is therefore useful. Acupuncture, a component of traditional Chinese medicine, is a wellknown and widely used treatment for pain and other conditions that has been employed in China for more than 3000 yr. There have been increasing numbers of clinical trials evaluating the efficacy of acupuncture and related techniques as an adjuvant method for postoperative analgesia. Therefore, we performed this systematic review to quantitatively evaluate the available evidence for the efficacy of acupuncture and related techniques in postoperative pain management. we found that acupuncture and related techniques are effective adjuncts for postoperative pain management as demonstrated by a significant reduction of postoperative pain scores and opioid consumption. While the reduction in pain scores achieved with acupuncture was statistically significant at 8 and 72 h, the reduction in pain intensity was moderate and it could be argued that it may not be clinically relevant. The same applies to the small absolute reductions in opioid consumption. he side-effects attributable to acupuncture were minimal and resolved spontaneously. In conclusion, this systematic review suggests that the perioperative administration of acupuncture may be a useful adjunct for postoperative analgesia. Further large, well-designed studies are required to confirm those findings and to answer questions regarding the most efficacious type of acupuncture and optimal timing of administration. In a the study conducted by J. Yuan about the effectiveness of acupuncture for low back pain,there is moderate evidence that acupuncture is more effective than no treatment, and strong evidence of no significant difference between acupuncture and
sham acupuncture, for short-term pain relief. There is strong evidence that acupuncture can be a useful supplement to other forms of conventional therapy for nonspecific low back pain , but the effectiveness of acupuncture compared with other forms of conventional therapies still requires further investigation. According to the study of Kerr D. in his research entitled Treatment regimens of acupuncture for low back pain--a systematic review, low back pain or non-specific low back pain , treatment regimens of acupuncture differ by the types of reference sources, in terms of treatment frequency, the points chosen, number of points needled per session, duration and sessions, and co-interventions. Another study entitled Assessment of a traditional acupuncture therapy for chronic neck pain: a pilot randomised controlled study, revealed that traditional acupuncture can relieve pain intensity and improve the quality of daily life with a relative long-term clinical efficacy in patients with chronic neck pain. The analgesic effect of magnetic acupressure in cancer patients undergoing bone marrow aspiration and biopsy had been studied by Bao T. The study shows that magnetic acupressure at the LI4 acupoint requires minimal training and expense and is well tolerated. Although its use did not significantly reduce median pain scores in patients undergoing BMAB, it does appear to reduce the proportion of patients with severe pain associated with this invasive procedure. In a study accomplished by Hopton A. about acupuncture and pain, findings show that For short-term outcomes, acupuncture showed significant superiority over sham for back pain, knee pain, and headache. For longer-term outcomes (6 to12 months), acupuncture was significantly more effective for knee pain and tension-type headache but inconsistent for back pain (one positive and one inconclusive). Current data regarding the clinical efficacy of acupuncture and related techniques suggest that the benefits are short-lasting. There is substantial evidence to support the use of acupuncture in the treatment of low back pain. The main predictors of chronic low back pain are non-medical and psychosocial. The understanding of how acupuncture can modulate the pain experience has recently been enhanced by the elucidation of the role of C fibre afferents on the limbic system. C fibre deactivation of the limbic system can only occur in the presence of intact corticosubcortical neuronal pathways. The normal development of these pathways is determined by social factors in the early years of life. The effect of acupuncture treatment for low back pain may be determined by successful relationships between the mother and child in the first 18 months of life.
Based from the previous studies, acupuncture is potentially useful adjunctive treatment for acute pediatric pain management. It is significantly effective for knee pain and tension-type headache. Acupuncture, an ancient form of medicine that originated in China several thousand years ago, has been used by Canadian physicians since the 1970s. Research on the neurophysiology of acupuncture analgesia supports the theory that it is mediated primarily via the selective release in the central nervous system of neuropeptides. Evidence of its anti-inflammatory effects is emerging. Meta-analyses of randomized controlled trials provide evidence for acupuncture's effectiveness in treating back pain, neck pain, and osteoarthritis. Applications of electroacupuncture using transcutaneous electrical nerve stimulation can provide good pain relief via home treatment and make management of cancer pain using acupuncture knowledge realistic.
END NOTES Y. Sun, T. J. Gan, J. W. Dubose, A. S. Habib (2007). Department of
Anesthesiology, Duke University Medical Center, Durham, NC.Retrieved from http://www.medscape.com/viewarticle/581266_5
Acupressure and Chinese Medicine(2008). Retrieved from http://www.articlegems.com
. Linda M. Rapson, MD and Robert Banner, MD (2008). Acupuncture for Pain Management. Retrieve from http://www.medscape.com/viewarticle/573858_7
Edzard Ernst and Myeong Soo Lee(2010). Acupuncture for Rheumatic Conditions: An Overview of Systematic Reviews. Retrieved from
http://www.medscape.com/viewarticle/729644
1. Kate Kelland (2008). Iraqi Anesthetist Uses Acupuncture During Drug Shortage. Retrieved from http://www.medscape.com/viewarticle/721109
Rebecca Prescott (2009) . Acupuncture For Asthma Fact Or Fiction. Retrieved from http://www.filipinoherbshealingwonders.filipinovegetarianrecipe.com/acupuncturefor-asthma-fact-or-fiction.htm Wu, Shelley MD, MPH and Sapru, Anil MD (2009). Using Acupuncture for Acute Pain in Hospitalized Children. Retrieved from http://www.medscape.com/viewarticle/708318 Tonette Orejas (2010). Doctor brings acupuncture to ordinary Kapampangan. Retrieved from http://newsinfo.inquirer.net/inquirerheadlines/regions/view/20100818287410/Doctor-brings-acupuncture-to-ordinary-Kapampangan
CHAPTER 3 Methodology
Research Design This study made use of the Nonrandomized clinical trial or quantitative quasi-experimental, the research methodology used by the researcher to maintain control over all factors that may affect the result of an experiment. In doing this, the researcher attempts to determine or predict what may occur. Two patient cohorts were enrolled in the study. The inclusion criteria for the first cohort (group 1) were patients aged 7 to 18 years who were postoperative from spinal fusion surgery, spontaneously breathing, and developmentally able to use patientcontrolled analgesia (PCA). The inclusion criteria for the second cohort (group 2) were patients aged 6 months to 18 years admitted to the pediatric intensive care unit who required intravenous pain medication. Exclusion criteria were age <6 months, prior acupuncture treatment, hemodynamic instability, immunodeficiency, increased
intracranial pressure, inability to react to painful stimuli, moderate or severe developmental delay, severe dermatologic conditions, extensive burns, use of cardiopulmonary bypass within last 24 hours, therapeutic anticoagulant medication (excluding aspirin, nonsteroidal anti-inflammatory drugs, and/or prophylactic heparin), chronic steroid use, neutropenia (absolute neutrophil count <1000), thrombocytopenia (platelets <100,000), excessive pain/sedation medication inducing deep sedation, or muscle relaxant medication. Patients younger than 3 years of age were not treated with acupuncture needles (see below) so were still eligible if they were on therapeutic anticoagulant therapy. As a part of patient screening, we contacted eligible patients who were scheduled for posterior spinal fusion or other surgeries. Whenever possible, we obtained consent preoperatively to allow more time for anticipatory guidance regarding acupuncture. We reassured parents and patients it was common to have anxiety or fear about the idea of having needles inserted. We explained that acupuncture needles, unlike thick and hollow needles used for injection or phlebotomy, are extremely thin, fine, and solid. We also offered to show a sterile acupuncture needle to the children and families so they could look at it and touch them if they so desired. We stated that although some children did not feel the needle insertion, others feel a little pinch or prick that might last a second. It was also explained that most children do not feel the needles after placement but if any needle should cause pain for longer than a couple of seconds, then the acupuncturist would either adjust or remove the needle so there would be no further pain.
Eligible patients meeting study criteria underwent two 10- to 15-minute acupuncture sessions. For postoperative patients, the first session was performed on the first postoperative day to minimize the impact of the clinical effects of anesthesia and intraoperative medication as a confounding factor. The second acupuncture session was performed approximately 2448 hours after the first session, when there was likely minimal residual effect of the first acupuncture treatment. A licensed acupuncturist (MAS) performed acupuncture on all the patients using the Japanese method of acupuncture. The patients received 36 needles and individually tailored acupuncture treatment depending on their diagnosis. All points were needled using Seirin number 3 (0.20) 30-mm needles. The needles were inserted and manipulated by hand at insertion and then again after 10 minutes. Needles were removed after 15 minutes. Acupuncture was done at the following points for patients after posterior spinal fusion surgery: a) Large Intestine 4 (Hegu). Located on the dorsum of the hand between the first and second metacarpal bones, at the midpoint of the second metacarpal bone and close to its radial border. b) Liver 3 (Taichong). Located on the dorsum of the foot in the hollow distal to the junction of the first and second metatarsal bones. c) Urinary Bladder 60 (Kunlun). Located between the prominence of the lateral malleolus and the Achilles tendon. d) Kidney 3 (Taixi). Located in the depression between the medial malleolus and the Achilles tendon, level with the prominence of the medial malleolus. All four points are located on the extremities. They were chosen for their effectiveness primarily and ease of access secondarily. The combination of liver 3 and large intestine 4 is known for its ability to vigorously activate the qi and blood and ensure their smooth passage throughout the body. Trauma, such as surgery, directly disrupts the free flow of qi and blood. When qi and blood are not moving freely, pain is felt. This combination of points has a general effect on all the qi and blood of the body. It is often used to treat pain anywhere in the body. Urinary bladder 60 was chosen because it activates the entire bladder channel and clears obstructionsi.e., qi and blood flow disrupted by surgeryall down the back. It is vital in the treatment of disorders of the back and spine from the neck right down to the coccyx. It is often referred to as the aspirin point for back pain. Kidney 3 was chosen for its effect of nourishing the kidneys, which control the low back, including the lumbar area, and support the bones. For the patients with spinal surgery, the fact that their spines had formed improperly and required surgery implied a
kidney disharmony. The kidney channel also connects with the bladder channel and can be used to treat the back. For each patient who had posterior spinal fusion surgery, all four points were used. There were a total of six needles used. Large intestine 4 and liver 3 were needled bilaterally. Urinary bladder 60 and kidney 3 were each needled only on one side, contralateral to each other. Patients were always able to move around easily and accessibility to the needling site determined the side on which these latter two points were needled.
All other surgical patients seen were treated according to the particular surgery/pain they experienced. Most received treatment at the points liver 3 and large intestine 4 described above. Children younger than 2 years of age were treated with Shonishin, a Japanese needling technique that stimulates the meridian system with small tools made for that purpose. Young children's meridian system is not developed fully, and therefore, it is more effective to treat the whole area or affected meridian. A spring-loaded noninsertion probe was gently bounced on particular point areas and a smooth scraper was lightly rubbed along the meridian(s). We measured the following clinical parameters at different intervals before and after each acupuncture session: heart rate, blood pressure, pain score, amount of pain and sedation medication, and number of PCA attempts if applicable. Patient selfreported pain scores using a standard numeric scale ranging from 0 to 10 whenever possible. Otherwise, other validated pain scales, such as the Face, Legs, Activity, Cry, Consolability scale, were used.[31] In assessing narcotic usage, we focused on morphine PCA in group 1 because this was the most common form of intravenous analgesic administered. The data were collected at 2 hours before and immediately pretreatment, and at 2, 4, 8, and 24 hours posttreatment. We asked the parent and child (if older than 7 years) to answer four questions after both sessions of acupuncture. First, we asked if they thought the acupuncture helped the child's pain and if they would consider acupuncture for the child in the future. Then, we asked parents who would consider future acupuncture for their child if they were willing to pay out of pocket for acupuncture (if not covered by insurance) and if so, the amount they would pay per treatment. Finally, we also collected general comments about the acupuncture treatment.
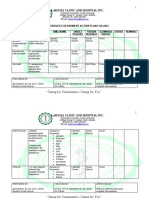
CHAPTER 4 Research Findings Table 1. Patient characteristics
Characteristic Group 1 Number of patients Male Median age (range, in yrs) Mean age (SD, in yrs) Use of morphine patient controlled analgesia Days in the intensive care unit (median, range) Days in the hospital (median, range) Group 2 Number of patients Male Median age (range, in mos/yrs) Mean age (SD, in yrs) Days in the intensive care unit (median, range, in days) Days in the hospital (median, range, in days) 9 6 (67%) .7 yr (7 mo 16 yr) 7.6 yr 6.9 3 d (1 21) 5 d (2 24) 11 4 (36%) 13 yr (818) 13.2 yr 3.1 11 (100%) 2 d (1 6) 7 d (6 63) Number (Percent/Range)
There are 11 respondents in group 1 where 36% are males. All of the 11 respondents had used morphine patient controlled analgesia.The median age is 13. The median number of days in the intensive care unit is two days and the median number of days in the hospital is 7 days. In group 2, there are 9 respondents where 67% are males.The median age is 7 years old.The median number of days in the intensive care unit is 3 days while the median number of days in the hospital is 5 days.
Table 2. Vital signs and pain scores before and after the first treatment
Baseline Group 1 (n =11) Heart rate Systolic BP Diastolic BP Pain score 125 114 62 3.7 10 13 8 3.2
2 Hours After Treatment
4 Hours After Treatment
8 Hours After Treatment
24 Hours After Treatment
122 107 56 3.4
16 12 9 3.1
113 107 59 1.7
19 12 5 2.1
118 111 62 2.9
18 10 12 2.2
116 107 58 3.1
25 8 13 2.8
Group 2 (n = 7) Heart rate Systolic BP Diastolic BP Pain score 120 117 63 2.5 39 24 20 1.9 115 109 55 0.3 38 12 8 0.8 115 115 58 0.3 42 16 10 0.5 112 110 54 0.9 35 11 18 1.5 118 118 59 1.6 26 25 14 2.6
BP, blood pressure. a Data presented as mean
sd.
Four hours after the first treatment in group 1, seven patients (64%) had decreases in pain scores, three had no change (27%), and one had an increase in pain score (9%). In group 2, five patients (71%) had a decrease in pain scores and two had no change (29%). Four hours after the first treatment, group 1 had a decrease in pain scores (p < 0.05) and a decrease in heart rates (p < 0.05). Group 2 had a decrease in pain scores (p < 0.05) 4 hours after the first treatment and a decrease in systolic blood pressures (p < 0.05) 4 hours after the second treatment.
In a study by Stewart and colleagues about using acupuncture for acute pain in hospitalized children, the treatment was highly accepted (27 patients were approached and 4 patients refused; of the 23 patients enrolled, 20 patients completed the study). Acupuncture was well tolerated by patients without adverse events related to treatment. In follow-up interviews, 70% of both parents and patients believed acupuncture helped the child's pain.The pain scores, vital signs, and narcotic usage were recorded before and several times after acupuncture.
Table 3. Vital signs and pain scores before and after the second treatment
Baseline Group 1 (n =11) Heart rate Systolic BP Diastolic BP Pain score 120 115 69 3.6 16 9 13 2.7
2 Hours After Treatment
4 Hours After Treatment
8 Hours After Treatment
24 Hours After Treatment
119 107 59 2.0
14 11 14 1.9
115 107 65 2.2
16 11 12 2.0
113 113 65 2.1
18 9 13 1.7
109 113 69 3.2
17 10 11 2.5
Group 2 (n = 7) Heart rate Systolic BP Diastolic BP Pain score 118 114 59 0.2 29 18 13 0.4 118 105 65 0.68 38 7 10 1.1 119 104 57 0.8 44 17 13 1.8 125 97 60 0.4 36 12 12 0.9 123 111 71 1.8 38 16 7 2.5
BP, blood pressure.
Table 4. Morphine use (mg/kg/hr) before and after acupuncture the first session in group 1 a
2 Hours Before Treatment (Baseline) 04 Hours After Treatment 48 Hours After Treatment 812 Hours After Treatment 1224 Hours After Treatment
Mean Difference from baseline
a
0.04
0.02
0.03
0.02
0.02
0.02
0.03
0.02
0.03
0.01 0.01
0.01 0.01
sd.
0.01 0.01 0.02
0.01 0.00
Data presented as mean
We used the data from group 1, session 1 for the following estimates because group 1 was comprised of similar surgical patients and because pain was more likely to be greater before session 1 than before session 2. Here, the descriptive data (mean SD) were 2.0 3.29 for the 0 4 hours change in pain score and 0.011 0.017 for the
baseline to 4 8 hours change in morphine use (mg/kg/hr). Using these data and assuming a 5% type I error rate, a randomized controlled trial with 43 subjects per group would have 80% power to detect a two-point decrease in pain score 4 hours after
acupuncture and a 0.01 mg/kg/hr decrease in morphine usage 48 hours after acupuncture.
In the New Jersey study, twelve patients were monitored using functional magnetic resonance imaging (fMRI), a technology that reveals what parts of the brain are receiving increased blood flow. Increased blood flow to different areas of the brain indicates that those areas of the brain are being stimulated. During 30 minutes of treatment, the patients rated their pain level on a scale of one to 10 every five minutes, with the fMRI continually monitoring their brains. In four of the seven subjects who received traditional acupuncture (57%), the fMRI showed considerably decreased levels of brain activity associated with the pain. This shows that there is a decrease in the level of pain with the use of acupuncture.
CHAPTER 5 Conclusion
Summary The treatment was highly accepted (27 patients were approached and 4 patients refused; of the 23 patients enrolled, 20 patients completed the study). Acupuncture was well tolerated by patients without adverse events related to treatment. In follow-up interviews, 70% of both parents and patients believed acupuncture helped the child's pain. Eighty-five percent of the parents said they would pay out of pocket for acupuncture if not covered by insurance. The pain scores, vital signs, and narcotic usage were recorded before and several times after acupuncture. In posterior spinal fusion patients, the mean pain scores (010) immediately before and 4 and 24 hours after acupuncture were: 3.7, 1.7, and 3.1, respectively, after the first acupuncture session and 3.7, 2.2, and 3.1, respectively, after the second session. In the other surgical cohort, the mean pain scores immediately before and 4 and 24 hours after the first session of acupuncture were 2.5, 0.3, and 1.6, respectively.
Conclusions Acupuncture may be a potentially useful adjunctive treatment for acute pediatric pain management. Our study showed that acupuncture is both feasible and highly accepted by parents and children for the treatment of acute pain, particularly postoperative pain, in hospitalized pediatric patients. There is a probable therapeutic effect at approximately 28 hours after acupuncture that wanes by 24 hours after the intervention, and it may be reproducible with subsequent acupuncture sessions. Adequately powered randomized controlled studies are necessary to evaluate the role of repeated and prolonged acupuncture sessions as a complementary therapy for acute pain control in hospitalized children.
Recommendation In the light of these conclusions, the following recommendations are offered: 1) Acupuncture is primarily used to ease symptoms of pain and discomfort: help to treat, including post-operative pain in pediatric patient. 2) Future nurses could further more recognize his/her accountability in effectively managing patients pain through assessment, right intervention and advocacy. 3) The hospital should quantitatively evaluate the available evidence for the efficacy of acupuncture and related techniques in postoperative pain management.
You might also like
- PLDT Area CodesDocument53 pagesPLDT Area Codesmcdale44% (81)
- 2006 2009.honda - Civic.service - ManualDocument4,763 pages2006 2009.honda - Civic.service - ManualTodd Julien89% (65)
- Management of Postoperative Pain With AcupunctureDocument384 pagesManagement of Postoperative Pain With AcupunctureCica Jovic100% (1)
- Food PoisoningDocument24 pagesFood PoisoningSena AjahNo ratings yet
- Hashimoto ThyroiditisDocument6 pagesHashimoto Thyroiditismananginsiang100% (1)
- Exams NAC Guideline Rating Scale PDFDocument2 pagesExams NAC Guideline Rating Scale PDFprakash13lNo ratings yet
- Surgical Nursing Brunner 2016Document74 pagesSurgical Nursing Brunner 2016Faisol Kabir100% (1)
- Children: Acupuncture For Pediatric PainDocument15 pagesChildren: Acupuncture For Pediatric PainRachel GreeneNo ratings yet
- Acupuncture - 11 10 2015Document6 pagesAcupuncture - 11 10 2015Rafael EscalanteNo ratings yet
- ACUPUNCTUREDocument9 pagesACUPUNCTUREyuviebNo ratings yet
- Acupuncture in Pain Management 2015Document203 pagesAcupuncture in Pain Management 2015PedroSuzana100% (1)
- Accupressure, Pain 4Document5 pagesAccupressure, Pain 4Akmal ThariqNo ratings yet
- Acupuncture: Ancient Treatment For Modern IllnessesDocument31 pagesAcupuncture: Ancient Treatment For Modern IllnessesJessica PaulNo ratings yet
- Preliminary Clinical Evaluation of Acupuncture Therapy in Patients With Postpartum SciaticaDocument7 pagesPreliminary Clinical Evaluation of Acupuncture Therapy in Patients With Postpartum SciaticasemnasNo ratings yet
- 0443103615Document361 pages0443103615Cristina Dríade100% (1)
- The Effectiveness of Hypnotherapy in Reducing PainDocument7 pagesThe Effectiveness of Hypnotherapy in Reducing PainArie DwianggaNo ratings yet
- Alternative Therapies in LabourDocument65 pagesAlternative Therapies in Labourhiral mistryNo ratings yet
- Auriculo ResearchDocument12 pagesAuriculo Researchtvmedicine100% (1)
- MediUnite Journal Pamphlets 2024 January EDITIONDocument8 pagesMediUnite Journal Pamphlets 2024 January EDITIONMediUnite JournalNo ratings yet
- Research Paper - FinalDocument14 pagesResearch Paper - Finalapi-660321588No ratings yet
- Dissertation Chronic PainDocument4 pagesDissertation Chronic PainWriteMyCollegePaperForMeSingapore100% (1)
- Research PaperDocument14 pagesResearch Paperapi-654024779No ratings yet
- Acupuncture Is My WorkDocument13 pagesAcupuncture Is My WorkDe BaronNo ratings yet
- Integrando Terapia Manual e Neurociencia Da DorDocument274 pagesIntegrando Terapia Manual e Neurociencia Da DorÁtila HanemannNo ratings yet
- Hypnosis and Pain ManagemententDocument6 pagesHypnosis and Pain ManagemententWanchankeinNo ratings yet
- Acup Utk TonsiltektomiDocument7 pagesAcup Utk Tonsiltektominewanda1112No ratings yet
- Acupuncture in Los AngelesDocument1 pageAcupuncture in Los Angelesjohngregz11No ratings yet
- Shiatsu Relieves Back PainDocument33 pagesShiatsu Relieves Back PainlaukuneNo ratings yet
- Acupuncture Trial Northern HospitalDocument8 pagesAcupuncture Trial Northern HospitalvicarofskepticNo ratings yet
- Thesis On Pain ManagementDocument5 pagesThesis On Pain ManagementWhatShouldIWriteMyPaperOnCincinnati100% (1)
- Nursing and Reflexology ResearchDocument39 pagesNursing and Reflexology ResearchJacqueline FerdinandNo ratings yet
- Ojsadmin, 58Document6 pagesOjsadmin, 58Gayathri K MNo ratings yet
- Acupuncture: A Therapeutic Modality, But Not A Placebo: Martin WangDocument74 pagesAcupuncture: A Therapeutic Modality, But Not A Placebo: Martin WangirmaNo ratings yet
- Effects of Auricular Point Sticking On Labor Pain and AnxietyDocument10 pagesEffects of Auricular Point Sticking On Labor Pain and AnxietyGlotta IdiomasNo ratings yet
- FullTextKopf+Patel v2Document390 pagesFullTextKopf+Patel v2Lidwina ElisabethNo ratings yet
- Acupuncture - MeniereDocument4 pagesAcupuncture - MeniereTinnitus Man IndonesiaNo ratings yet
- Research Paper On PainDocument8 pagesResearch Paper On Painyjtpbivhf100% (1)
- ENERGY PSYCH THERAPY EVIDENCEDocument19 pagesENERGY PSYCH THERAPY EVIDENCElandburender100% (1)
- Doctor, What 'S This Acupuncture All About?Document7 pagesDoctor, What 'S This Acupuncture All About?Lev KalikaNo ratings yet
- Acupunct Med 2014 p242Document9 pagesAcupunct Med 2014 p242Anonymous PFNzHoNo ratings yet
- Acupuncture Relieves Asthma AttacksDocument4 pagesAcupuncture Relieves Asthma AttacksriezzzadityaNo ratings yet
- Acupuncture Is Underutilized in Hospice and Palliative MedicineDocument11 pagesAcupuncture Is Underutilized in Hospice and Palliative MedicinetvmedicineNo ratings yet
- 1281-Article Text-4723-1-10-20221214 PDFDocument5 pages1281-Article Text-4723-1-10-20221214 PDFTan AwiNo ratings yet
- Acupuncture Produces Amazing Results in Reversing InfertilityDocument9 pagesAcupuncture Produces Amazing Results in Reversing InfertilityIffah AfifahNo ratings yet
- University of People PSYC 1111 - AY2021-T2 Written Assignment Unit 4Document5 pagesUniversity of People PSYC 1111 - AY2021-T2 Written Assignment Unit 4Divya BharthiNo ratings yet
- Aspirin in Episodic Tension-Type Headache: Placebo-Controlled Dose-Ranging Comparison With ParacetamolDocument9 pagesAspirin in Episodic Tension-Type Headache: Placebo-Controlled Dose-Ranging Comparison With ParacetamolErwin Aritama IsmailNo ratings yet
- 05 N111 7399Document16 pages05 N111 7399rudolfpeterssonNo ratings yet
- Acupuncture BasicsDocument2 pagesAcupuncture BasicsandreasNo ratings yet
- Assessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsFrom EverandAssessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsNo ratings yet
- Psychological And Behavioral Treatment Of Insomnia UpdateDocument17 pagesPsychological And Behavioral Treatment Of Insomnia UpdateIta Punya ShintaNo ratings yet
- Acupuncture Against Depression Acupuncture Against Depression Acupuncture Against Depression Acupuncture Against DepressionDocument20 pagesAcupuncture Against Depression Acupuncture Against Depression Acupuncture Against Depression Acupuncture Against DepressionFrancois du RizNo ratings yet
- Acupuncture Has Been Used For Thousands of YearsDocument13 pagesAcupuncture Has Been Used For Thousands of Yearsoluwasegun DavidNo ratings yet
- Fibromyalgia A Clinical ReviewDocument9 pagesFibromyalgia A Clinical ReviewastrogliaNo ratings yet
- Some Common A: Acupuncture For Evaluative ResearchDocument5 pagesSome Common A: Acupuncture For Evaluative ResearchocoxodoNo ratings yet
- Clinical Applications of Acupuncture: An Overview of The EvidenceDocument8 pagesClinical Applications of Acupuncture: An Overview of The EvidenceAntonio ANo ratings yet
- Journal of Anesthesiology MP State Vol 1Document37 pagesJournal of Anesthesiology MP State Vol 1cardiacanesthesiaNo ratings yet
- Acute Service Pain Handbook 2011Document116 pagesAcute Service Pain Handbook 2011Iskandar414No ratings yet
- Nur340 Problem-Based Research Paper FinalDocument7 pagesNur340 Problem-Based Research Paper Finalapi-569642906No ratings yet
- Pain ManagementDocument9 pagesPain Managementapi-655053476No ratings yet
- Auriculo Research PDFDocument18 pagesAuriculo Research PDFOdin Tachón100% (1)
- Patil 2016Document8 pagesPatil 2016Ichwan MalikNo ratings yet
- Chronic Pain Thesis PDFDocument5 pagesChronic Pain Thesis PDFtehuhevet1l2100% (2)
- Migraine: Emerging Innovations and Treatment OptionsFrom EverandMigraine: Emerging Innovations and Treatment OptionsShalini ShahNo ratings yet
- Acupuncture: A Patient's Guide to Acupuncture, Herbal Medicine, Nutrition & More (The Ultimate Step-by-step Guide for Building and Growing a Profitable Acupuncture Practice)From EverandAcupuncture: A Patient's Guide to Acupuncture, Herbal Medicine, Nutrition & More (The Ultimate Step-by-step Guide for Building and Growing a Profitable Acupuncture Practice)No ratings yet
- Small Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationFrom EverandSmall Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationSung-Tsang HsiehNo ratings yet
- Chapter 1Document8 pagesChapter 1Ralph NicolasNo ratings yet
- International Flight Schedule from ManilaDocument4 pagesInternational Flight Schedule from ManilaRalph NicolasNo ratings yet
- RA 544 Civil Engineering LawDocument5 pagesRA 544 Civil Engineering LawThomas John Doblas AgrabioNo ratings yet
- Week No. Start END Date Target SavingsDocument4 pagesWeek No. Start END Date Target SavingsRalph NicolasNo ratings yet
- The Comprehensive Adulth Health History GuideDocument4 pagesThe Comprehensive Adulth Health History GuideRalph NicolasNo ratings yet
- Front Row ProductsDocument11 pagesFront Row ProductsRalph NicolasNo ratings yet
- Detailed Patientob Health History GuideDocument5 pagesDetailed Patientob Health History GuideRalph NicolasNo ratings yet
- Gun Control PowerpointDocument11 pagesGun Control Powerpointapi-319208107No ratings yet
- Wilfredo Mallari Resume Safety Supervisor UpdatedDocument1 pageWilfredo Mallari Resume Safety Supervisor Updatedwilly mallariNo ratings yet
- Database Clerk Vacancy in MawlamyineDocument3 pagesDatabase Clerk Vacancy in MawlamyineHein Min NaingNo ratings yet
- SOCIAL SERVICES aCTION PLAN FOR 2022Document6 pagesSOCIAL SERVICES aCTION PLAN FOR 2022Rocel Cañete Ordoyo-GabrielNo ratings yet
- University of Caloocan City: Bachelor of Arts Major in Political Science The Problem and Its BackgroundDocument7 pagesUniversity of Caloocan City: Bachelor of Arts Major in Political Science The Problem and Its BackgroundJericko Perez AvilaNo ratings yet
- Basic Tools in NutritionDocument23 pagesBasic Tools in NutritionSeanmarie Cabrales0% (1)
- Mindfulness-Based Cognitive Therapy For DepressionDocument10 pagesMindfulness-Based Cognitive Therapy For DepressionCMValmaNo ratings yet
- How To Use The FYI FlagsDocument5 pagesHow To Use The FYI FlagsFuji guruNo ratings yet
- Ovr New MohDocument2 pagesOvr New MohhyNo ratings yet
- Method of Statement and Risk Assessment FormDocument4 pagesMethod of Statement and Risk Assessment FormBala KrishnanNo ratings yet
- Viva XT Brochure - 201203539IEp3Document6 pagesViva XT Brochure - 201203539IEp3Lubna LuaiNo ratings yet
- IBM India Benefits - Emergency Transport Assistance GuidelinesDocument6 pagesIBM India Benefits - Emergency Transport Assistance GuidelinesSushovan NandiNo ratings yet
- Case Study Report (Peptic Ulcer) Group 1Document9 pagesCase Study Report (Peptic Ulcer) Group 1Khrizlynne SoberanoNo ratings yet
- 100 Papers in Clinical Psychiatry Psychosomatic Medicine Malingering in The Medical Setting.Document18 pages100 Papers in Clinical Psychiatry Psychosomatic Medicine Malingering in The Medical Setting.J. M. SolisNo ratings yet
- Jme by Country May2023Document347 pagesJme by Country May2023kaysbookishNo ratings yet
- Health and Safety Policy Manual Issue 14Document34 pagesHealth and Safety Policy Manual Issue 14caskevNo ratings yet
- Legacy of Tuskegee Syphilis StudyDocument2 pagesLegacy of Tuskegee Syphilis StudyLcgessamanNo ratings yet
- HIV Testing and Management in IndonesiaDocument31 pagesHIV Testing and Management in IndonesiayurdiansyahNo ratings yet
- Effects of Virtual Reality Training On Limb Movement in Children With Spastic Diplegia Cerebral PalsyDocument5 pagesEffects of Virtual Reality Training On Limb Movement in Children With Spastic Diplegia Cerebral PalsyZharif MuzaniNo ratings yet
- Dme Information Form Cms-10125 - External Infusion PumpsDocument2 pagesDme Information Form Cms-10125 - External Infusion PumpsSonof GoddNo ratings yet
- HEALTH INSURANCE NON-EU CITIZENSDocument2 pagesHEALTH INSURANCE NON-EU CITIZENSSufian AbusninaNo ratings yet
- Natural Pregnancy and ParentingDocument70 pagesNatural Pregnancy and ParentingAmela SabicNo ratings yet
- Asthma Management in 40 CharactersDocument10 pagesAsthma Management in 40 CharactersAmalNo ratings yet
- Lab Activity #8Document3 pagesLab Activity #8Kristelito Grace MarinoNo ratings yet
- ICU patient transfer guidelineDocument8 pagesICU patient transfer guidelineInnas DoankNo ratings yet
- Block M2 EYE Distribution by MMCDocument3 pagesBlock M2 EYE Distribution by MMCF ParikhNo ratings yet