Professional Documents
Culture Documents
118 - WK 5 - ER Assessment Part 1
Uploaded by
JUDE MARIANO JR. ALBANCES CARLOS0 ratings0% found this document useful (0 votes)
5 views2 pagesOriginal Title
118_Wk-5_ER-Assessment-Part-1
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views2 pages118 - WK 5 - ER Assessment Part 1
Uploaded by
JUDE MARIANO JR. ALBANCES CARLOSCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
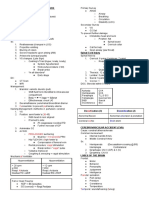
Emergency Room (ER) Assessment ■ Circulation
■ priority→peripheral pulses of upper &
lower torso
● Primary Survey/Assessment↔organized ■ check if normal rat esp sa distal body
approach to identify threat and apply parts (peripheral)
interventions ■ intiate BP taking + apical pulse
○ Resuscitation interventions needs securing (discrepancy)
the {{envt}} ■ evaluate skin color
■ includes→PPE ■ skin temperature (check if diaphoretic)
■ uncover obvious bleeding
ABCDE ■ need {{4092812833573358::two large
bore}} IV lines
■ Airway/cervical spine↓
■ start
■ cervical spine injury is always
{{5085015058761044::isotonic}}
suspected when the person falls, how
fluids
high?→taller than their height
■ blood loss→fluids and blood is required
■ priority→estb patient airway
■ what if no pulses?→CPR
■ AIRWAY
■ CAB→compression, airway, breathing
■ always immobilize cervical spine
■ life threatening→bleeding, hemorrhage,
■ implement short conversation w/
cardiac tamponade
pt (if pt can speak then they have
■ Disability
a patent airway)
■ DISABLE
■ reposition pt w/ neck in midline
■ do neurologic assessment (GCS)
(head tilt-chin lift method)
■ immobilization is maintained
■ ways of opening airway is
■ size of pupil and reactivity
implemented
■ reactivity (PERLA)→pupil equally
■ allot time in checking for
round reactive to light
obstructions
accomodation
■ common causes→tongue,
■ AVPU = rapid screening tool for LOC
blood, loose teeth or vomit
■ A→alert
■ you should clear obstructions
■ V→respond to voice?
■ how to get rid of
■ P→responsive to pain
obstructions→jaw thrust
■ U→unresponsive
method, suctioning,
■ be mindful of LOC impairment causes
intubation (if wlala na estb
■ Alcohol = CNS depressant
ang airway)
■ Epilepsy = problem w/ electrolytes
■ Breathing
■ Insulin = hypo/hyperglycemia
■ assess→respi rate, breath sounds
■ Opiates = dec LOC
and respiratory effort
■ Uremia = problems with kidney
■ pulse oxi and use of accessory muscles
■ Trauma = esp if naay bleeding
■ evaluate chest wall movement
■ Infection
(asymmetrical or nah)
■ Poisoning
■ tracheal deviation
■ Psychosis
■ administer O2 via BVM (Ambubag)
■ Syncope
(100%)
■ leave C-collar unless SCI is not
■ airway adjuncts
confirmed (aka wait for xray)
■ oral/nasopharyngeal airway
■ enhance secondary assessment if it
■ ET tube
isnt alert
■ suctioning PRN
■ Exposure/envt
■ remove obstructive foreign bodies
■ remove clothing of pt to perform
■ life-threatening
thorough assessment (cover w/ drape
condition→pneumothorax, hydrothorax,
lang dayun)
hemothorax
■ prevent hypothermia
■ observe evidence preservation as ■ cover neurologic status assessment
policy ■ uncover pain via frequent assessment
■ warm fluids/blanket if needed ■ secure follow-up measures
■ determine extent of injury
● Secondary Survey/Assessment↔identify other
injuries or other issues that need to be
assessed; head-to-toe assessment for ALL
injuries
○ FGHI
■ Full set of vital signs
■ vs= TPR, BP, O2
■ biometrics = H&W
■ vs evaluated serially
■ Give comfort measures (Pain assessment)
■ Assess pain (5th vs)
■ PQRST→provoking factors, quality of
pain, radiation, severity, timing
■ wong-baker faces pain scale
■ chief complaints
■ non-pharma measures first
■ History taking→while doing head to toe
assessment
■ health hx
■ focus on chief complaints (not a dx
tho!)
■ contact reliable source of information
■ organize adequate history with
SAMPLE (types of info
needed)→subjective; allergies;
medications; past medical hx; last meal
eaten, tetatnus shot, period; events
leading to injury
■ open-ended but direct questioning
■ family and social history
■ Institute head to toe assessment
■ elaborate causes of altered LOC
■ head, face, neck
■ chest and abdomen
■ pelvis and perineum
■ both extremities
■ posterior surfaces
● Ongoing Assessment/Focus
Assessment↔integrated throughout the nsg
process; identify problems that is overlooked
earlier; q15 min follow-up
○ indications→identify response to
interventions and to determine
improvement or deterioration in patient
status; need for RE-assessment
○ example→I&O hourly monitoring
○ FOCUS
■ facilitate trauma score calculation
■ often repeat for vs taking
You might also like
- S T A R T: Imple Riage ND Apid ReatmentDocument17 pagesS T A R T: Imple Riage ND Apid ReatmentNavine NavNo ratings yet
- M4 - Didactic - NCM 118Document4 pagesM4 - Didactic - NCM 118KARL FESARITNo ratings yet
- Mrcem C AtlsDocument4 pagesMrcem C AtlsMohammad Irfan khanNo ratings yet
- Bec Quick CardsDocument14 pagesBec Quick CardsUmidagha BaghirzadaNo ratings yet
- Exit Osce BedahDocument52 pagesExit Osce BedahLovely PoppyNo ratings yet
- Screenshot 2024-03-29 at 20.24.01Document12 pagesScreenshot 2024-03-29 at 20.24.01hennywahyuni363No ratings yet
- IVTherapyDocument24 pagesIVTherapydiaNaNo ratings yet
- ReviewDocument25 pagesReviewsamuelNo ratings yet
- (OSCE) 3.0 Cardiovascular ExaminationDocument5 pages(OSCE) 3.0 Cardiovascular ExaminationJara RogacionNo ratings yet
- Operative Print3 Medad-NotesDocument46 pagesOperative Print3 Medad-NotesOliverYousryNo ratings yet
- 1.2 Intro To Oxy Diagnostic Procedures For Problems in OxygentionDocument3 pages1.2 Intro To Oxy Diagnostic Procedures For Problems in OxygentionCamille Joy BaliliNo ratings yet
- DRR ReviewerDocument4 pagesDRR ReviewerBong KalotNo ratings yet
- NZ Crisis Handbook - DiagnosingDocument16 pagesNZ Crisis Handbook - DiagnosingSean SmythNo ratings yet
- CA - Emergency and Disaster Nursing PDFDocument5 pagesCA - Emergency and Disaster Nursing PDFMarvin Heramis RyanNo ratings yet
- Step 3 Surgery Uworld NotesDocument11 pagesStep 3 Surgery Uworld Notesaleks patralskaNo ratings yet
- Perioperative NursingDocument5 pagesPerioperative NursingMikhaela Andree MarianoNo ratings yet
- Transes Tra - Peri-OpDocument11 pagesTranses Tra - Peri-OpJoshua DelantarNo ratings yet
- General Assessment: Additional Notes: BlueDocument4 pagesGeneral Assessment: Additional Notes: BlueKaiken DukeNo ratings yet
- Approach To TraumaDocument43 pagesApproach To TraumaAlmonz AndoriasNo ratings yet
- Resumen AudioDocument31 pagesResumen AudioYoselyn Acuña TorresNo ratings yet
- NCM 118 Midterms ReviewerDocument7 pagesNCM 118 Midterms ReviewerKai SamaNo ratings yet
- Oto.s1.l04.nasal Discharge (Rhinitides) (CD)Document9 pagesOto.s1.l04.nasal Discharge (Rhinitides) (CD)VICTOR AMORESNo ratings yet
- Physical Diagnosis of The ThoraxDocument3 pagesPhysical Diagnosis of The ThoraxSeff Causapin100% (1)
- Surgery Cases: CASE 1: Blunt Abdominal TraumaDocument3 pagesSurgery Cases: CASE 1: Blunt Abdominal TraumaGio Tamaño BalisiNo ratings yet
- H.A. Lec (L7 B) - Assessing Head and Neck, Eyes and Visual Acuity, Ears and BalanceDocument4 pagesH.A. Lec (L7 B) - Assessing Head and Neck, Eyes and Visual Acuity, Ears and BalanceCastallia LascuñaNo ratings yet
- Management of TraumaDocument21 pagesManagement of Traumablazingdk sriNo ratings yet
- Complete PE Check ListDocument4 pagesComplete PE Check ListgurneeNo ratings yet
- Cardiology - CVS OSCE ChecklistDocument5 pagesCardiology - CVS OSCE ChecklistPraveenaNo ratings yet
- NCM 118 A Review Random FinalDocument3 pagesNCM 118 A Review Random FinalRosel Vivien EstoqueNo ratings yet
- Respi Hema NotesDocument16 pagesRespi Hema NotesLucky GomezNo ratings yet
- Scope of Practice Paramedic BSCDocument9 pagesScope of Practice Paramedic BSCdeejrogers96No ratings yet
- Neurology: o o o o oDocument18 pagesNeurology: o o o o oTrixia Joy R NachorNo ratings yet
- CVS, Respi Heent ExamDocument8 pagesCVS, Respi Heent ExamDranreb Berylle MasangkayNo ratings yet
- Defibrillation & Cardioversion: Ns. Retno Setyawati, M.Kep., SP - KMBDocument34 pagesDefibrillation & Cardioversion: Ns. Retno Setyawati, M.Kep., SP - KMBSokhifatun NajahNo ratings yet
- Schwartz's Hour Notes On TraumaDocument19 pagesSchwartz's Hour Notes On TraumaEver Seneca EscaLera100% (2)
- Week 10 - Neural DisturbancesDocument5 pagesWeek 10 - Neural Disturbanceszh4hft6pnzNo ratings yet
- 7.3 Injured ChildDocument4 pages7.3 Injured ChildΜατθαίος ΠαππάςNo ratings yet
- Primary SurveyDocument30 pagesPrimary SurveyLeo SihombingNo ratings yet
- Osce AbcdeDocument5 pagesOsce AbcdeJoseph JoseNo ratings yet
- Anesthesia Pocket Guide 2020 PDFDocument2 pagesAnesthesia Pocket Guide 2020 PDFMaksym DemianchukNo ratings yet
- ? - Pedia MidtermsDocument18 pages? - Pedia Midtermsysabel.mendozaNo ratings yet
- Atenolol 1Document4 pagesAtenolol 1Nicko Pazon AranasNo ratings yet
- Freemedicalbooks 4 DownloadDocument98 pagesFreemedicalbooks 4 Downloadموسى التميميNo ratings yet
- Integumentary Physical Therapy: Int1 Lab FinalsDocument10 pagesIntegumentary Physical Therapy: Int1 Lab FinalsVenice Marie CordetaNo ratings yet
- 10 Medical Surgical Nursing Intensive Review PDFDocument68 pages10 Medical Surgical Nursing Intensive Review PDFShanine Alexia CordovezNo ratings yet
- Aortic Aneurysm-: NUR2744 Test 3 OutlineDocument10 pagesAortic Aneurysm-: NUR2744 Test 3 Outlinemara5140No ratings yet
- Emergency NursingDocument3 pagesEmergency NursingJennie KimNo ratings yet
- RVT ATLS Review & General Principles in TraumaDocument91 pagesRVT ATLS Review & General Principles in TraumaJamaluddin Ahmad A.MNo ratings yet
- Initial Assessment in ShortDocument2 pagesInitial Assessment in Shorta.e.noushiNo ratings yet
- Prelims Disaster Skills 1st NotesDocument6 pagesPrelims Disaster Skills 1st NotesbercoaprilgraceNo ratings yet
- 9 5神經系統Document59 pages9 5神經系統陳姿螢No ratings yet
- Blood Transfusion Blood Transfusion Equipment: Packed RBCDocument2 pagesBlood Transfusion Blood Transfusion Equipment: Packed RBCAdiel CalsaNo ratings yet
- Lumbar Puncture-2Document24 pagesLumbar Puncture-2Aditya rajNo ratings yet
- CPRDocument41 pagesCPRPreethi BNo ratings yet
- 8 10 21 Neuro - OrthoDocument7 pages8 10 21 Neuro - OrthoReymart AcalaNo ratings yet
- 07 TraumScenario Short New May2023Document4 pages07 TraumScenario Short New May2023AmruthNo ratings yet
- Complete Guide To Physical ExamDocument19 pagesComplete Guide To Physical ExamSeff Causapin100% (2)
- Algorithm For The Management of A High Regional Block in ObstetricsDocument5 pagesAlgorithm For The Management of A High Regional Block in ObstetricsRaditya DidotNo ratings yet
- NCM 112 - Med SurgDocument7 pagesNCM 112 - Med SurgKierzteen Brianna TaromaNo ratings yet
- Terrorism, Mass Casualty, and Disaster NursingDocument3 pagesTerrorism, Mass Casualty, and Disaster NursingJUDE MARIANO JR. ALBANCES CARLOSNo ratings yet
- Psychiatric EmergenciesDocument1 pagePsychiatric EmergenciesJUDE MARIANO JR. ALBANCES CARLOSNo ratings yet
- Emergency NursingDocument2 pagesEmergency NursingJUDE MARIANO JR. ALBANCES CARLOSNo ratings yet
- Emergency NursingDocument2 pagesEmergency NursingJUDE MARIANO JR. ALBANCES CARLOSNo ratings yet
- Environmental EmergencyDocument4 pagesEnvironmental EmergencyJUDE MARIANO JR. ALBANCES CARLOSNo ratings yet
- Psychiatric EmergenciesDocument1 pagePsychiatric EmergenciesJUDE MARIANO JR. ALBANCES CARLOSNo ratings yet
- Terrorism Mass Casualty Disaster NursingDocument3 pagesTerrorism Mass Casualty Disaster NursingJUDE MARIANO JR. ALBANCES CARLOSNo ratings yet
- Perioperative Nursing Reviewer Part 3Document13 pagesPerioperative Nursing Reviewer Part 3JUDE MARIANO JR. ALBANCES CARLOSNo ratings yet
- ER Diagonostics Reviewer Part 2Document9 pagesER Diagonostics Reviewer Part 2JUDE MARIANO JR. ALBANCES CARLOSNo ratings yet
- +chapter 6 Binomial CoefficientsDocument34 pages+chapter 6 Binomial CoefficientsArash RastiNo ratings yet
- Rubber Lined Piping - A Solution To Corrosion ResistanceDocument5 pagesRubber Lined Piping - A Solution To Corrosion ResistanceMohamed AghilaNo ratings yet
- FORD Falcon XA Repair ManualDocument770 pagesFORD Falcon XA Repair ManualMark Kenzie100% (10)
- Tamil NaduDocument64 pagesTamil Nadushanpaga priyaNo ratings yet
- Assignment On Cholera: Submitted ToDocument17 pagesAssignment On Cholera: Submitted ToEhesanulHaqueSaifNo ratings yet
- Non-Pen MountDocument17 pagesNon-Pen MountT BagNo ratings yet
- Notice: Environmental Statements Notice of Intent: Eldorado National Forest, CADocument2 pagesNotice: Environmental Statements Notice of Intent: Eldorado National Forest, CAJustia.comNo ratings yet
- 1 Name of Work:-Improvement of Epum Road (Northern Side) Connecting With Imphal-Saikul Road I/c Pucca DrainDocument1 page1 Name of Work:-Improvement of Epum Road (Northern Side) Connecting With Imphal-Saikul Road I/c Pucca DrainHemam PrasantaNo ratings yet
- HardikDocument21 pagesHardikGohil HardikNo ratings yet
- Israel StandardDocument15 pagesIsrael StandardDũng Bùi Đức100% (1)
- Phineas Gage: From The Passage of An Iron Rod Through The Head"Document1 pagePhineas Gage: From The Passage of An Iron Rod Through The Head"GlupiaSprawaNo ratings yet
- TR189 Kathuria PDFDocument168 pagesTR189 Kathuria PDFuqiNo ratings yet
- Eoi QAMDocument6 pagesEoi QAMPeeyush SachanNo ratings yet
- High Performance Dialysis GuideDocument28 pagesHigh Performance Dialysis GuideRoxana ElenaNo ratings yet
- Resource Access ControlDocument19 pagesResource Access Controlusamadar707No ratings yet
- 100 Years of Hydrodynamic PDFDocument28 pages100 Years of Hydrodynamic PDFnikodjoleNo ratings yet
- Cateora2ce IM Ch012Document9 pagesCateora2ce IM Ch012Priya ShiniNo ratings yet
- Iloilo City Regulation Ordinance 2006-010Document4 pagesIloilo City Regulation Ordinance 2006-010Iloilo City CouncilNo ratings yet
- Progress Report Week#9 UlubeluDocument6 pagesProgress Report Week#9 UlubelutiantaufikNo ratings yet
- Deld12070 CC18 GT 371 C CDocument1 pageDeld12070 CC18 GT 371 C CDEBASIS BARMANNo ratings yet
- Good Stuff Courage, Resilience, Gratitude, Generosity, Forgiveness, and Sacrifice (Akhtar, Salman)Document221 pagesGood Stuff Courage, Resilience, Gratitude, Generosity, Forgiveness, and Sacrifice (Akhtar, Salman)madhugaggar999No ratings yet
- BHLP Year Long Plan Required English Medium 2023 24 Batch Final 991676721629413Document3 pagesBHLP Year Long Plan Required English Medium 2023 24 Batch Final 991676721629413A V GamingNo ratings yet
- Panasonic Refrigeraor NR-B472TZ - B412TZ v1.1Document24 pagesPanasonic Refrigeraor NR-B472TZ - B412TZ v1.1Anonymous 2iQ1B59No ratings yet
- Brock Planetary Declination SDocument6 pagesBrock Planetary Declination SDositheus Seth100% (2)
- Icpc11 - Thermodynamics and Fluid MechanicsDocument22 pagesIcpc11 - Thermodynamics and Fluid MechanicsAPARNANo ratings yet
- Chapter 2Document82 pagesChapter 2Kavitha Selvaraj50% (2)
- EB-300 310 Service ManualDocument32 pagesEB-300 310 Service ManualVictor ArizagaNo ratings yet
- Output Process Input: Conceptual FrameworkDocument4 pagesOutput Process Input: Conceptual FrameworkCHRISTINE DIZON SALVADORNo ratings yet
- EASA - Design OrganisationsDocument30 pagesEASA - Design Organisationsyingqi.yangNo ratings yet
- Orifice Assembly With D-D2 Taps PDFDocument1 pageOrifice Assembly With D-D2 Taps PDFArup MondalNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)