Professional Documents
Culture Documents
Mod 1 CONCEPT OF HOSPICE-PALLIATIVE CARE, DEATH and DYING
Uploaded by
Jorese Hannah Victorino0 ratings0% found this document useful (0 votes)
21 views3 pagesCopyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
21 views3 pagesMod 1 CONCEPT OF HOSPICE-PALLIATIVE CARE, DEATH and DYING
Uploaded by
Jorese Hannah VictorinoCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 3
Nursing Care of Clients with Problems in Oxygenation, Fluid and Electrolyte, Infectious,
Inflammatory and Immunologic Response, Cellular Aberration, Acute and Chronic
Module 1: Nursing Care Management of Clients with Cellular Aberration (Cancer)
Clinical Instructor: Racquel C. Cruz RN, MSN
1st Semester | S.Y. 2022-2023
HOSPICE PALLIATIVE CARE Use other ways to control pain, including
massage, music, and comfortable positioning
A. Principles of Palliative Care: of the patient. Sometimes a hot pad or hot
water bottle is helpful with pain.
1. Affirms life and regards dying as a normal process Addiction to medication is never important for
2. Neither hastens nor postpones death dying patients
3. Provides relief from pain and other distressing
symptoms 2. Keep the patient comfortable
4. Integrates the psychological, ethical, legal, and If the patient is constipated, a laxative may be
spiritual aspects of care helpful. Also encourage the patient to drink fruit
5. Offers a support system to help patients live as juices.
actively as possible until death As much as possible, give the patient a high-
6. Offers a support system to help patient’s families calorie, high-vitamin diet. Do not force the
cope during the patient’s illness and in their own patient to eat. The patient should eat only what
bereavement foods he or she wishes to eat.
Keep the patient clean; give frequent baths,
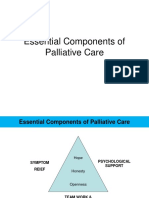
B. Essential Components of Palliative Care give mouth care if the mouth is dry, and clean
1. Symptom control the eyelids if secretions collect
2. Effective communication Help the patient to get out of bed and sit in a
3. Rehabilitation chair if he or she is able. If not, change the
4. Continuity of care position every two hours and try to keep the
5. Terminal care patient in whatever positions are most
6. Support in bereavement comfortable.
7. Education If the patient has trouble breathing, help him or
8. Research her to sit up a little
If the airway is obstructed, you may need to
Nurses Role suction the patient’s throat.
a. Providing direct care If the patient feels short of breath or gasps for
b. Advocate air, give oxygen.
c. Counselor Even when patients are close to death, they
d. Collaborative Role can hear, so do not speak in a whisper. Speak
clearly. The patient will also still feel your touch
END-OF-LIFE (EOL) CARE
CONCEPT OF HOSPICE-PALLIATIVE CARE, LOSS, GRIEVING, DYING, AND DEATH
LOSS, GRIEVING, DYING, AND DEATH
“To everything there is a season and a time to every Terminal illness
purpose under the heaven, a time to be born and a time
to die.” – Ecclesiastes 3:1-2 Progressive, irreversible illness that despite-
cure focused medical treatment will result in
HOSPICE – PALLIATIVE CARE patient’s death.
Hospice Needs of a terminally ill → (1) Spiritual, (2)
A coordinated program of interdisciplinary care Emotional, (3) Physical
and services provided primarily in the home to
terminally ill patients and their families. Advance Directives
Palliative Care
Comprehensive care for patients whose Written documents that allow the individual of
disease is not responsive to cure sound mind to document preferences
Common S/Sx: Pain, Dyspnea, Anorexia, regarding end-of-life care that SHOULD BE
Cachexia, Delirium, and depression FOLLOWED when the SIGNER (patient
himself) is terminally ill and unable to verbally
1. Relieve the dying person's pain communicate his/her wishes.
Always trust what patients say about their pain. The documents are generally completed in
Never just make your own decision about how advance of serious illness but may be
much pain they are suffering. completed after a diagnosis of serious illness if
Many patients fear that they will die in agony. the signer is still of sound mind.
Be kind when people express or show fear.
Comfort them and tell them that you can take Two types:
care of the pain and that they do not need to 1. Durable power of attorney for Health Care
fear.
Give doses of pain medication that give the • aka: health care power of attorney or
most pain control with the least side-effects. Proxy directive
Give pain medication all through the day and • A legal document through which the
night to make sure that the patient has enough signer appoints and authorizes another
pain relief. individual to make medical decisions on
Use the simplest route to give medicine. Give it his/her behalf when he/she is no longer
by mouth, if the person can swallow. able to speak for him/herself.
• Notarized, read twice before signing.
Nursing Care of Clients with Problems in Oxygenation, Fluid and Electrolyte, Infectious, Inflammatory and Immunologic Response,
Cellular Aberration, Acute and Chronic
Module 1: Nursing Care Management of Clients with Cellular Aberration (Cancer)
Clinical Instructor: Racquel C. Cruz RN, MSN
1st Semester | S.Y. 2022-2023
CHANGES IN THE BODY AFTER DEATH
2. Living will 1. Rigor Mortis
Is the stiffening of the body that occurs
▪ aka: medical directive or treatment about 2 – 4 hours after death
directive Most noticeable 48 – 96 hours after
▪ Provides specific instructions for care death
should the signer becomes terminally ill Rapid (Physically active); gradual
and not able to communicate his/her (bedridden)
wishes directly and often is accompanied Starts on the muscles of the Head and
by durable power of attorney for health Neck → Trunk → Lower extremities
care. it is therefore advisable to perform Last
▪ Accept / refuse medical care Offices (aka: post-mortem care) prior to
this occurring, as movement and
Factors Affecting Response to Loss positioning will otherwise be impossible
FACTORS EXAMPLES Position the body properly, place
1. Emotional Family or acquaintance dentures in the mouth and close the
Involvement eyes and mouth before rigor mortis
2. Nature of Acute or chronic sets in.
Death 2. Algor Mortis
3. Characteristic Adult VS. Children Is the gradual decrease of body’s
of survivor temperature after death.
4. Social and Rural VS. Urban When the blood circulation terminates
Cultural milieu and the hypothalamus ceases
5. Nature of Relatives and Friends functions, body temperature falls about
support 1°C per hour until reaches room
network temperature.
3. Livor Mortis
SIGNS OF IMPENDING / IMMINENT DEATH Discoloration of the skin after death
A. Loss of Muscle Tone after circulation has ceased.
a. Relaxation of the facial muscles (jaw The RBC breakdown, releasing
may sag) hemoglobin which discolor the
b. Difficulty in speaking surrounding tissues.
c. Dysphagia with gradual loss of gag 4. Skin indentation
reflex Due to loss of turgor and elasticity
d. Decreased in the activity of the GIT 5. Autolysis
e. Possible urinary and bowel Digestion of tissues from enzymes and
incontinence lysosomes.
f. Diminished body movement Organs swell and are spongy
6. Putrefaction
B. Slowing of Circulation Invasion of the body by
a. Diminished sensation microorganisms
b. Mottling and cyanosis of the Produces greenish discoloration of the
extremities skin, production of gases, and causes
c. Cold skin, first on the feet and later in foamy and spongy organs.
the hands, ears, and nose.
POST-MORTEM CARE
C. Changes in Vital Signs -care of the body after death
a. Decelerated and weaker pulse Purposes:
b. Decreased in blood pressure a. To keep the body clean and odor free.
c. Rapid, shallow, irregular or abnormally b. To prepare the body for discharge from the
slow respirations (Cheyne-Stoke’s health facility.
Respiration); noisy breathing (Death c. To make the dead presentable for viewing by
Rattle), labored breathing the SO.
d. Fixed dilated pupils Steps:
1. Ensure that death has been verified by a doctor
D. Sensory Impairment
a. Blurred vision 2. Familiarize yourself with the client’s/ relatives’
b. Impaired sense of taste and smell wishes and cultural and religious needs before
c. Note: Hearing → the last sense lost touching the deceased, as procedures vary
depending on religious beliefs
POSITIVE SIGNS OF DEATH
3. Wear disposable gloves and other personal
1. Total lack of response to external stimuli protective equipment (PPE) as necessary
2. No muscular movement
3. No reflexes 4. Make the environment as clean and as pleasant
4. Absence of brain activity as evidenced by Flat as possible.
electroencephalogram (EEG). → the most
accurate indicator of death. 5. Make the body appear natural and comfortable
Nursing Care of Clients with Problems in Oxygenation, Fluid and Electrolyte, Infectious, Inflammatory and Immunologic Response,
Cellular Aberration, Acute and Chronic
Module 1: Nursing Care Management of Clients with Cellular Aberration (Cancer)
Clinical Instructor: Racquel C. Cruz RN, MSN
1st Semester | S.Y. 2022-2023
6. Remove all equipment and supplies from the
bedside.
7. Remove soiled linen, so the room is free from
odors.
8. Place the body in supine position, arms on the
side and palms down.
9. Place one pillow under the head and shoulders
to prevent blood from discoloring the skin.
10. Close the eyelids, insert dentures, and close
the mouth.
11. Wash soiled areas of the body.
12. Place absorbent pads under the buttocks to
take up any feces and urine released because
of relaxation of the sphincter muscles.
13. Provide clean gown, brush / comb the hair.
14. Remove all jewelries. All the client’s valuables
are listed and placed in a safe storage area for
the family to take away.
15. Provide an environment conducive to viewing
by:
ensuring privacy and dignity
covering the deceased with clean,
fresh linen
controlling room temperature
ensuring good ventilation
speaking quietly and avoiding
unnecessary/inappropriate
conversation in the vicinity of the
bereaved
offering to stay with the relatives if
required
reducing environmental noise such as
telephones, alarms, machinery,
banging doors, and movement of
equipment
making sure there is adequate seating
for the bereaved
16. Allow the family to view the patient’s body.
17. Apply identification tags, one on the ankle and
one on the wrist.
If the body will be brought to the morgue:
a. Wrap the body in shroud; apply another
identification tag to the outside of the
shroud.
b. Bring the body to the morgue for
cooling.
18. Ensure that the bereaved have some form of
transport home (To demonstrate compassion
and ensure safety)
19. Clean the bed following hospital policy and
remake it before drawing back the curtains
around the deceased’s bed area
20. Inform other clients and provide an opportunity
to express their thoughts and feelings, as they
are often very distressed by such an event
You might also like
- Care of The DyingDocument4 pagesCare of The Dyingprokuno89% (9)
- Mod 1 Holistic Care of Client With CancerDocument3 pagesMod 1 Holistic Care of Client With CancerJorese Hannah VictorinoNo ratings yet
- 3 Death and DyingDocument34 pages3 Death and Dyingikram ullah khanNo ratings yet
- NS Compounding Set 4 PDFDocument24 pagesNS Compounding Set 4 PDFJulia BottiniNo ratings yet
- Module 19 Post Mortem 2Document8 pagesModule 19 Post Mortem 2Alvin Josh CalingayanNo ratings yet
- Care of Dying and DeadDocument10 pagesCare of Dying and Deadd1choosenNo ratings yet
- Grief, Loss, Death and Coping: Stages of Grief and Nursing ResponsibilitiesDocument35 pagesGrief, Loss, Death and Coping: Stages of Grief and Nursing ResponsibilitiesGummie Akalal Sugala0% (1)
- Group 5 BioethicsDocument12 pagesGroup 5 BioethicsSexbomb Adela KirstenNo ratings yet
- End-of-Life Care For The Newly Licensed Practical Nurse: State of Nebraska Transition GrantDocument8 pagesEnd-of-Life Care For The Newly Licensed Practical Nurse: State of Nebraska Transition GrantGee YorkNo ratings yet
- Principles of Palliative CareDocument4 pagesPrinciples of Palliative CareSHERMINA HASANNo ratings yet
- Death and Dying HandoutsDocument3 pagesDeath and Dying HandoutsGlads D. Ferrer-JimlanoNo ratings yet
- Nikka Shanna Lingolingo Gerontology Assignment Exercise 2 1Document2 pagesNikka Shanna Lingolingo Gerontology Assignment Exercise 2 1ARISNo ratings yet
- DNR or End of Life Care DecisionsDocument20 pagesDNR or End of Life Care DecisionsAllessandria Daphne Sac BagacinaNo ratings yet
- Nursing Case Study of Pulmonary Congestion and MRSA PatientDocument12 pagesNursing Case Study of Pulmonary Congestion and MRSA PatientJude Remso LabajoNo ratings yet
- BSN 1 H Case Application Nursing Care PlanDocument3 pagesBSN 1 H Case Application Nursing Care PlanAntonio EscotoNo ratings yet
- EuthanesiaDocument58 pagesEuthanesiatarshaNo ratings yet
- End of Life CommunicationDocument27 pagesEnd of Life CommunicationjintuNo ratings yet
- L14 Reading Reflections Study GuideDocument5 pagesL14 Reading Reflections Study GuideMaria Camila Vangh-egas JNo ratings yet
- Compiled Notes of Bernie C. ButacDocument12 pagesCompiled Notes of Bernie C. ButacVeigner Whyng CabugayanNo ratings yet
- Module 1 Am Activity On Prioritization v2Document5 pagesModule 1 Am Activity On Prioritization v2KeanuNo ratings yet
- PSYCH CP DepressionDocument8 pagesPSYCH CP DepressionKendricNo ratings yet
- Care of The Dying PatientDocument6 pagesCare of The Dying PatientAnastasia Bouy-upNo ratings yet
- Managing Abdominal Pain from DiverticulitisDocument11 pagesManaging Abdominal Pain from DiverticulitisMa. Sofia Andrei AlcabazaNo ratings yet
- 1 - Lenguaje Del CPPDocument4 pages1 - Lenguaje Del CPPAlejandra ChaconNo ratings yet
- Essential Components of Palliative CareDocument20 pagesEssential Components of Palliative CareJonah R. Merano50% (4)
- Geron 3FDocument5 pagesGeron 3FJeann sumbillaNo ratings yet
- Osteoporosis Prognosis and Nursing CareDocument4 pagesOsteoporosis Prognosis and Nursing CareJanine Mae MacaraigNo ratings yet
- Managing Generalized Anxiety Disorder: CBT Intervention for Worrying MotherDocument20 pagesManaging Generalized Anxiety Disorder: CBT Intervention for Worrying MotherErleNo ratings yet
- Chapter 37: The Experience of Loss, Death, and Grief: Fundamentals of Nursing, 9th Edition Multiple ChoiceDocument12 pagesChapter 37: The Experience of Loss, Death, and Grief: Fundamentals of Nursing, 9th Edition Multiple ChoicehenryNo ratings yet
- Week 1nur 212Document12 pagesWeek 1nur 212Oliver NamyaloNo ratings yet
- Concept MapDocument7 pagesConcept Mapapi-507879066No ratings yet
- Nori Enjelika Banunaek - PO5303201211401 I - Week 10 - Tugas BINGDocument10 pagesNori Enjelika Banunaek - PO5303201211401 I - Week 10 - Tugas BINGAngelina BanunaekNo ratings yet
- Comfort Care for Terminally Ill Patient with Multiple ComorbiditiesDocument14 pagesComfort Care for Terminally Ill Patient with Multiple ComorbiditiesNestley TiongsonNo ratings yet
- Emergency Nursing: Compiled Notes of Bernie C. ButacDocument14 pagesEmergency Nursing: Compiled Notes of Bernie C. ButacLouie ParillaNo ratings yet
- Case StudyDocument23 pagesCase StudyIzel Monica Osorio BollonNo ratings yet
- Nursing Care PlanDocument7 pagesNursing Care PlanJane LiNo ratings yet
- Quarter 3 Health Week 3 4Document19 pagesQuarter 3 Health Week 3 4Art Lance TolentinoNo ratings yet
- Myths UpdatedDocument3 pagesMyths UpdatedMashael SulimanNo ratings yet
- Utilizing The Concepts of Holistic HealthDocument5 pagesUtilizing The Concepts of Holistic HealthMegainaNo ratings yet
- Health Care Ethics-Wks.78Document50 pagesHealth Care Ethics-Wks.78Majestic RavenNo ratings yet
- Mulyani 2Document7 pagesMulyani 2arjuridallah883No ratings yet
- Hypnosis in Terminal CareDocument4 pagesHypnosis in Terminal Careapolloe215No ratings yet
- Rationalization Activity 18Document3 pagesRationalization Activity 18rica sebabillonesNo ratings yet
- Cancer Burden: Global Picture. Number of New Cancer Cases (In Millions)Document5 pagesCancer Burden: Global Picture. Number of New Cancer Cases (In Millions)Samantha BolanteNo ratings yet
- Casepres TUBERCULOSISDocument35 pagesCasepres TUBERCULOSISjhaninahNo ratings yet
- Management of The Critically Ill PatientDocument36 pagesManagement of The Critically Ill PatientZhi Hao OoiNo ratings yet
- Introduction To Palliative Care: by Yonas T. (BSC, MSC)Document64 pagesIntroduction To Palliative Care: by Yonas T. (BSC, MSC)Abdi Mohammed100% (1)
- NCPDocument7 pagesNCPJo Chiko FlorendoNo ratings yet
- Patient's Anxiety Managed Through Coping StrategiesDocument4 pagesPatient's Anxiety Managed Through Coping StrategiesAaLona Robinson86% (7)
- DocumentDocument1 pageDocumentAtasha Margaret PedrazaNo ratings yet
- IPIndianJNeurosci 9 4 186 190Document5 pagesIPIndianJNeurosci 9 4 186 190keerthi.sakthi0794No ratings yet
- Nursing Care of Clients with Anxiety DisordersDocument6 pagesNursing Care of Clients with Anxiety DisordersJaylord VerazonNo ratings yet
- YIN QIANHE ON LONGEVITY - Brennan Translation PDFDocument182 pagesYIN QIANHE ON LONGEVITY - Brennan Translation PDFfofofofo100% (4)
- Absayk MidtermDocument27 pagesAbsayk MidtermAndrew NavarraNo ratings yet
- Palliative Care Advance Directives GuideDocument19 pagesPalliative Care Advance Directives GuideSophia Gayle RaagasNo ratings yet
- IAPHD Hand Book On Palliative Care PDFDocument37 pagesIAPHD Hand Book On Palliative Care PDFMohammed ArshadNo ratings yet
- Abnormal-Uterine-Bleeding Case StudyDocument57 pagesAbnormal-Uterine-Bleeding Case StudyOneForAll :100% (1)
- Hospice and Palliative Nursing: Rainier C. Moreno-Lacalle NLAC-SON Clinical InstructorDocument67 pagesHospice and Palliative Nursing: Rainier C. Moreno-Lacalle NLAC-SON Clinical InstructorRainier Moreno-LacalleNo ratings yet
- Theoretical Foundation of Nursing - Martha RogersDocument1 pageTheoretical Foundation of Nursing - Martha RogersAshley Nicole BeltranNo ratings yet
- K220 Accessories BrochureDocument6 pagesK220 Accessories Brochurehh8g9y6ggcNo ratings yet
- Synopsis MphilDocument10 pagesSynopsis MphilAyesha AhmadNo ratings yet
- Squidpy: A Scalable Framework For Spatial Omics Analysis: ArticlesDocument14 pagesSquidpy: A Scalable Framework For Spatial Omics Analysis: ArticlesXin XuNo ratings yet
- Cycle1 Parta GettingtoknowyourstudentsDocument7 pagesCycle1 Parta Gettingtoknowyourstudentsapi-295073409No ratings yet
- Maths Homework Project Year 4Document8 pagesMaths Homework Project Year 4afeuwbdev100% (1)
- E - Program Files (x86) - Schneider - sft2841 - sft2841 Serie 80 - Notice - en - Manual - Sepam - Series80 - Operation - ENDocument180 pagesE - Program Files (x86) - Schneider - sft2841 - sft2841 Serie 80 - Notice - en - Manual - Sepam - Series80 - Operation - ENJuan Cristóbal Rivera PuellesNo ratings yet
- Power Transformer Fundamentals: CourseDocument5 pagesPower Transformer Fundamentals: CoursemhNo ratings yet
- EPFO Declaration FormDocument4 pagesEPFO Declaration FormSiddharth PednekarNo ratings yet
- Telstra Strategic Issues and CEO Leadership Briefing PaperDocument16 pagesTelstra Strategic Issues and CEO Leadership Briefing PaperIsabel Woods100% (1)
- Achmad Nurdianto, S.PD: About MeDocument2 pagesAchmad Nurdianto, S.PD: About Medidon knowrezNo ratings yet
- The World in Which We Believe in Is The Only World We Live inDocument26 pagesThe World in Which We Believe in Is The Only World We Live inYusufMiddeyNo ratings yet
- Envision Math 8.1 - Use Models To Multiply A Whole Number by A Fraction PracticeDocument2 pagesEnvision Math 8.1 - Use Models To Multiply A Whole Number by A Fraction PracticeMerlin D SilvaNo ratings yet
- 4.2 Force and Motion 1Document19 pages4.2 Force and Motion 1ammarsyahmiNo ratings yet
- A Is Called The Base and N Is Called The Exponent: Grade 7 Math Lesson 21: Laws of Exponents Learning GuideDocument4 pagesA Is Called The Base and N Is Called The Exponent: Grade 7 Math Lesson 21: Laws of Exponents Learning GuideKez MaxNo ratings yet
- Xpand!2 - User Guide - V1.1Document18 pagesXpand!2 - User Guide - V1.1JamesNo ratings yet
- Hanix h15b 2 h15b Plus 2 Service Manual Sept 09Document10 pagesHanix h15b 2 h15b Plus 2 Service Manual Sept 09vickie100% (41)
- MR Explorer: Magnetic Resonance Logging ServiceDocument7 pagesMR Explorer: Magnetic Resonance Logging ServiceRoberto DominguezNo ratings yet
- June 28th Altran Capital Market Day Presentation DeckDocument52 pagesJune 28th Altran Capital Market Day Presentation Deckvenkata.krishnan100% (1)
- Experiences in The OperationDocument7 pagesExperiences in The OperationUsama Bin SabirNo ratings yet
- Welder Training in SMAW, GTAW & GMAW Welding Engineering & NDT Consultancy Welding Engineering Related TrainingDocument4 pagesWelder Training in SMAW, GTAW & GMAW Welding Engineering & NDT Consultancy Welding Engineering Related TrainingKavin PrakashNo ratings yet
- IEU - BBA - Final Project - Business Plan - Guidelines and Requirements - v02.07Document11 pagesIEU - BBA - Final Project - Business Plan - Guidelines and Requirements - v02.07Jorge Eduardo Ortega PalaciosNo ratings yet
- Advanced Long Range Proximity Reader PDFDocument1 pageAdvanced Long Range Proximity Reader PDFPhangkie RecolizadoNo ratings yet
- 11.1 Exam Practice 30 U11Document6 pages11.1 Exam Practice 30 U11Đỗ LoanNo ratings yet
- TOS - MathDocument4 pagesTOS - MathGeorge Ezar N. QuiriadoNo ratings yet
- E-Ship Assignment 2 Utkarsh Surjey MBA-FT-EDocument3 pagesE-Ship Assignment 2 Utkarsh Surjey MBA-FT-Eutkarsh surjeyNo ratings yet
- Four Process StrategyDocument10 pagesFour Process StrategyChandria FordNo ratings yet
- Develop, Implement and Maintain WHS Management System Task 2Document4 pagesDevelop, Implement and Maintain WHS Management System Task 2Harry Poon100% (1)
- Circuit Diagram Eng 5582-2-01Document95 pagesCircuit Diagram Eng 5582-2-01edolzaNo ratings yet
- Automobiles Seat ComfortDocument10 pagesAutomobiles Seat ComfortAnushree DeshingeNo ratings yet
- Professional Industrial Engineering Program: Technical EnglishDocument15 pagesProfessional Industrial Engineering Program: Technical EnglishFabio fernandezNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (41)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)