Professional Documents
Culture Documents
Lecture - Blood & Homeostasis - Part 2
Uploaded by
Keila RosalesOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lecture - Blood & Homeostasis - Part 2
Uploaded by
Keila RosalesCopyright:
Available Formats
1 TERM
BIOCHEMISTRY NU
LECTURE \ MR. GALVEZ 03 01
TRANS UNIT 7.2: REGULATORY PROTEINS
OUTLINE
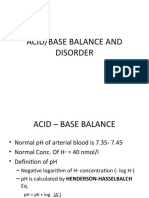
ACID-BASE BALANCE
I) Acid-Base Balance • Acid – a substance that can donate hydrogen ions
A) Types of Acid o Lower pH = below 7
B) How the Body Proceeds to Acidic Condition • Base – substance that can accept hydrogen ions
i) CO2 Excretion and Production • Higher pH
ii) Kidneys Excretory Function
C) Fixed Acids
D) Clinical pH Range TYPES OF ACID
II) Plasma Bicarbonate Concentration • Mostly dictate the pH level in our body
A) Bicarbonate Buffer System • Carbonic Acid
B) Determining pH o Volatile Acid - readily change composition
i) pH vs. [H+] o Carbon Dioxide - released to make body less acidic
ii) Normal Values
III) Metabolic Disorders
o Note: Carbonic acids has 15000 mmol/d and is
IV) Respiratory Disorders eliminated by the lungs
V) Buffering • Non-carbonic acids
A) Effects of Buffers on pH o Nonvolatile acids such as phosphoric and sulfuric
VI) Purpose of Acid-Base Balance acids, 50-100 meq/d).
A) Compensatory Mechanisms o Present to the body but in minimal accounts only
B) Summary o Byproducts of processes in the body
C) Simple Acid-Base Disorders
VII) Disorders
• Combine with buffers and subsequently excreted by the
A) Metabolic Acidosis kidneys
i) Causes o Buffers – prevent drastic changes in pH
B) Respiratory Acidosis o Cushion changes in pH
C) Respiratory Alkalosis
D) Metabolic Alkalosis HOW THE BODY PROCEEDS TO ACIDIC CONDITION
i) Causes
E) Expected Changes for Respiratory Disorders
• CO2 production
VIII) Renal Acid Excretion o 13,000-20,000 Millimoles/day
IX) Titratable Acidity o If not released from the body, can cause acidosis
X) Ammonium Excretion (acidic blood = ph 6.5)
XI) Sodium-Chloride Relationship
XII) Mixed Acid-Base Disorder
XIII) Mineral Balance
A) Fluid and Electrolyte Balance
B) Regulation of Fluid and Electrolyte Balance
C) Regulation of Blood Pressure
XIV) Electrolytes
A) Sodium
B) Chloride
C) Potassium
D) Calcium
i) Blood Calcium Regulation
ii) Effects of Chronically Low Calcium Intake
iii) Factors That Enhance Calcium Absorption
E) Phosphorus • Kidneys Excretory Function
F) Magnesium o If not excreted by the lungs or liver, it will be excreted
G) Sulfur
XV) Trace Minerals
by the kidneys
A) Iron o Other acids will be excreted in kidneys
i) Iron Toxicity
B) Zinc
C) Iodine
D) Selenium
E) Copper
F) Manganese
G) Chromium
H) Molybdenum
BENIG | BERNARDINO | COLLAMAR | CALOMOT | DANCEL | GO | GONZALVO | LACAO | MANGOBA | ROALES |
ROSALES | SORIANO | PARULI | PORLAS | VILLEGAS | VILLAFLOR | VILLAMAYOR
TRANS UNIT 7.2: REGULATORY PROTEINS
FIXED ACIDS pH vs. [H+]
• H2SO4 [H+] = 80-decimal digit of pH
o Helps with degradation of proteins
• H3PO4
o Helps with degradation of phospholipids
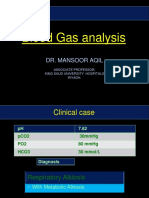
CLINICAL PH RANGE
• pH between 7.80 and 6.80 (H+ concentrations between 16
-160 meq/l) are the extremes of pH compatible with life
• Clinical laboratories measured pH, carbon dioxide, and
oxygen in arterial samples.
• Bicarbonate concentration can be calculated from the
Henderson equation.
• Laboratories measure total CO2 concentration (dissolved
CO2 plus bicarbonate concentration, ~25-26 meq/l) in
venous samples
• Note: remember the equation namely Henderson–
Hasselbalch equation (no need to memorize)
PLASMA BICARBONATE CONCENTRATION
• Measured by the amount of carbon dioxide present, partial
pressure of CO2
• Laboratories measure total CO2 concentration (dissolved
carbon dioxide plus bicarbonate concentration, ~25-26
meq/l)
• As a result, total CO2 concentration exceeds plasma NORMAL VALUES
bicarbonate concentration by 1.0 to 1.5 meq/l Normal pH – 7.35-7.45 (7.40)
• Normal plasma bicarbonate concentration is approximately – pH = -log[H+]
24 mEq/l – [H+] = 24 x pCO2/[HCO3-]
Normal pCO2 36-44 mm Hg (40 mmHg)
CONDITIONS/PROCESS Normal HCO3- 22-26 meq/L (24 meq/L)
Acidemia Reduced pH (elevated hydrogen ion
concentration) METABOLIC DISORDERS
• Processes that modify bicarbonate concentration directly
Alkalemia Increased pH (reduced hydrogen ions o Bicarbonate deficiency is a symptom of metabolic
concentration) acidosis.
Acidosis The process that lowers pH o Metabolic alkalosis: increased bicarbonate
Alkalosis The process that increases pH
RESPIRATORY DISORDERS
BICARBONATE BUFFER SYSTEM • Processes that directly alter CO2
CO2 + H20 H2CO3 → H+ + HCO3 - • Respiratory acidosis – increased CO2
• If a closed system, pKa = 6.1 (normal pH= 7.40) o Asthma, COPD, Fibrosis, muscle disorders, medicines
• We are an open system, with CO2 being excreted through that suppressed breathing
the lungs, making this a highly efficient buffer. o Bronchodilator – vasoconstrictor
o Narcotics and alcohol
DETERMINING PH o Severe obesity
• The concentration of the hydronium ion in moles per liter is • Respiratory alkalosis – decreased CO2
required to calculate the pH of an aqueous solution o Asthma, hyperventilation (respiratory rate is high),
(molarity). COPD
o After that, using the expression, the pH is computed. • Buffer Effect – slightly increased HCO3 with respiratory
alkalosis
o Prevent from going into alkalosis or acidosis
BUFFERING
• Prevent wide changes in pH in response to the addition of
base or acid
• Bicarbonate is the major extracellular buffer (can be easily
measured)
• There are also intracellular buffers (electrolytes)
BENIG | BERNARDINO | COLLAMAR | CALOMOT | DANCEL | GO | GONZALVO | LACAO | MANGOBA | ROALES |
ROSALES | SORIANO | PARULI | PORLAS | VILLEGAS | VILLAFLOR | VILLAMAYOR
TRANS UNIT 7.2: REGULATORY PROTEINS
EFFECTS OF BUFFERS ON PH SUMMARY
• The presence of buffers attenuates changes in pH in Disorder pH HCO3 - pCO2 Comment
response to acid-base disorders. Metabolic ↓ ↓ primary ↓ All 3
acidosis Compensatory markers
• Immediate onset
• Isohydric principle (all buffers change in the same direction) go in
same
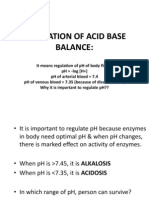
PURPOSE OF ACID-BASE BALANCE direction
• Because enzyme action is pH dependent, maintaining an Metabolic ↑ primary ↑ All 3
alkalosis ↑ Compensatory markers
acid–base balance is critical for the regular functioning of
biological systems. go in
• This page discusses acid–base balance definitions as well same
as the normal physiology of acid–base metabolism in the direction
extracellular fluid and blood. Resp. ↓ ↑ ↑ primary pH goes
acidosis Compensatory opp. Other
2 markers
BUFFER PAIR BUFFER PAIR H+ DONOR Resp. ↓ ↓ primary pH goes
alkalosis ↑ Compensatory opp. Other
Bicarbonate HCO₃- H₂CO₃ 2 markers
(ECFV)
GOLDEN RULES: SIMPLE-ACID BASE DISORDERS
Phosphate (Urine) H₂PO₄²- H₂PO₄ 1 • PCO2 and HCO3 always change in the same
direction.
Ammonia (Urine) NH₃ NH₄+ o They are related to one another
2 • The secondary physiologic compensatory
Protein Protein Protein mechanisms must be present.
o When you say secondary physiologic
COMPENSATORY MECHANISMS compensatory mechanism this is the other
homeostatic balance or checkpoints within
• In addition to buffering mechanisms, additional secondary
your body for example the blood, food, and
(compensatory) physiologic responses occur in response to
nutrients.
changes in pH.
3 • The compensatory mechanisms never fully
• Invariably present in simple acid-base disorders (if not
present, it is a mixed disorder) correct pH.
o It's always your body which will be correcting it
• The respiratory system compensates for metabolic
naturally.
disorders by altering CO2 (via the lungs, rapid onset,
o Your compensatory mechanism will only be for
minutes)
us for initial responses, it is more like a first aid
o The respiratory system compensates for metabolic
but it is not a total cure.
disorders by altering the carbon dioxide or its either by
o Your body will always go in its natural state
hyperventilation.
because that is homeostasis that will make
o So if you need a lot of carbs you need an exchange of
your body balanced.
the gases within your body it will be signaling your body
so that it could increase the amount of the exchange of
carbon dioxide or if ever hyperventilation is not possible DISORDERS
what happens is that you could deep breaths
• Compensation for respiratory disorders occurs by METABOLIC ACIDOSIS
alterations in bicarbonate concentration (via the kidney, • Process the reduces plasma bicarbonate concentration
slower onset 1-2days) • Etiology:
Buffer systems Extracellular Immediate
o Decreased renal acid excretion
(primarily fluid (HCO - + H+ ↔ H₂CO
3
o Direct bicarbonate losses (GI tract or urine)
bicarbonate) ↔CO + H₂O )
2
o Increased acid generation (exogenous or endogenous)
Increased rate Lungs Minutes to hours
and depth of CAUSES OF METABOLIC ACIDOSIS
breathing to 1 • Increased Acid Generation
decrease CO o Lactic acidosis
Buffer systems Intracellular 2-4 hours o Ketoacidosis
(phosphate, fluid o Ingestion of acids (aspirin, ethylene glycol,
bicarbonate, methanol)
protein) o Dietary protein intake (animal source)
Hydrogen ion Kidneys Hours to days 2 • Loss of Bicarbonate
excretion, bicarb o Gastrointestinal (diarrhea, intestinal fistulas)
reabsorption, & o Renal: type 2 proximal renal tubular acidosis
bicarb 3 • Decreased acid excretion (impaired NH4+
generation excretion)
BENIG | BERNARDINO | COLLAMAR | CALOMOT | DANCEL | GO | GONZALVO | LACAO | MANGOBA | ROALES |
ROSALES | SORIANO | PARULI | PORLAS | VILLEGAS | VILLAFLOR | VILLAMAYOR
TRANS UNIT 7.2: REGULATORY PROTEINS
o Renal failure (reduced GFR) EXPECTED PH CHANGES IN RESPIRATORY
o Decreased ammonium excretion DISORDERS
o Type I (distal) renal tubular acidosis
o Type 4 renal tubular acidosis Acute • A condition in which carbon dioxide
(hypoaldosteronism) respiratory builds up very quickly, before the kidneys
acidosis can return the body to a state of balance.
RESPIRATORY ACIDOSIS o HCO3- increases 1 meq for each 10
• Induced by hypercapnia (decreased alveolar ventilation). mm increase in pCO2
o Buildup of CO2 in the bloodstream Chronic • The PaCO2 is elevated above the upper
• Buffering mechanisms raise plasma bicarbonate Respiratory limit of the reference range, with a normal
concentration. Acidosis or near-normal pH secondary to renal
• Kidney minimizes the change in extracellular pH by compensation and an elevated serum
increasing acid excretion generating new bicarbonate bicarbonate levels (i.e., >30 mEq/L).
ions. o HCO3 increases 4 mEq for each 10
mm increases in PCO2
RESPIRATORY ALKALOSIS Acute • The PaCO2 is below the lower limit of
• Reduced carbon dioxide due to increased alveolar Respiratory normal and the serum pH is alkemic.
ventilation. Alkalosis o HCO3 decreases 2 mEq for each 10
• Buffering processes lower plasma bicarbonate mm decrease in PCO2
concentration. Chronic • A common acid base disturbance
• Kidney response is to reduce net acid excretion (eliminate Respiratory characterized by a primary and sustained
bicarbonate into the urine or decrease ammonium Alkalosis decrease in arterial carbon dioxide
excretion). tension (PaCO2).
• The PaCO2 is below the lower limit of
NOTE: RESPIRATORY DISORDERS normal, but the pH level is relatively
• Acute respiratory acid-base disorders always have a normal or near normal due to
greater change in pH than chronic disorders compensatory mechanisms.
• Plasma Cl changes equally and inversely with plasma o HCO3 decreases 5 mEq for each 10
HCO3. mm decrease in PCO2
• The plasma anion gap does not change with respiratory •
disorders.
• Plasma sodium is not directly altered by acid-base RENAL ACID EXCRETION
disorders. • All of the filter of bicarbonate must be reabsorbed (primarily
in the proximal tubule and loop of Henle)
METABOLIC ALKALOSIS • Final excretion of the daily acid load occurs primarily in the
• Raise plasma bicarbonate concentration. collecting duct (approximately 50-100 meq/d)
• ORIGIN/CAUSES: Vomiting and Diuretic Therapy
• Excessive urinary net acid excretion (primary TITRABLE ACIDITY
hyperaldosteronism). • Phosphate homeostasis is maintained by urinary excretion
of dietary phosphate
CAUSES OF METABOLIC ALKALOSIS • Monobasic phosphate is an effective urinary buffer,
HYDROGEN LOSS especially at lower urinary pH
1 • Gastrointestinal loss • Accounts for excretion of 10 to 40 mEq of hydrogen ion daily
o Removal of gastric secretions • Cannot be increased beyond this due to the fixed amount
o Due to vomiting or nasogastric suction of phosphate in urine
2 • Urinary loss
o Loop or thiazide-type diuretics AMMONIUM EXCRETION
o Hyperaldosteronism • Contributes the major adaptive response to an acid load
o Posthypercapnic alkalosis • Can be increased in response to physiologic needs
3 • Movement into the cells • Normally 30-40 mEq/d and maximal excretion is
o Hypokalemia approximately 300 mEq/d
• Administration of bicarbonate or an organic ion that can • NH4+ is lipid soluble and therefore trapped in the urinary
be metabolized to bicarbonate, such as citrate in blood lumen
transfusions. • An indirect estimate of Urinary NH4+ excretion
CONTRACTION ALKALOSIS • Urine Na+ K+ minus urine Cl
1 • Loop or thiazide-type diuretics in edematous • Normally ~ 10 meq/ and becomes less positive and even
patients. become negative with increase urinary NH4 excretion (Cl-
must accompany NH4+)
• URINE CHLORIDE CONCENTRATION:
o Cl responsive: urine Cl <20 meq/l (usually <10 meq/l)
o Cl resistant: urine Cl > 20 meq/l (usually >50 meq/l)
BENIG | BERNARDINO | COLLAMAR | CALOMOT | DANCEL | GO | GONZALVO | LACAO | MANGOBA | ROALES |
ROSALES | SORIANO | PARULI | PORLAS | VILLEGAS | VILLAFLOR | VILLAMAYOR
TRANS UNIT 7.2: REGULATORY PROTEINS
SODIUM CHLORIDE RELATIONSHIP TRACE MINERALS
• Law of Electroneutrality: • Iron, zinc, iodine, selenium, copper, chromium,
o Sodium concentration is not directly altered by acid manganese, fluoride, chromium, and molybdenum.
base disorders FLUID AND ELECTROLYTE BALANCE
o Plasma Cl is altered in all acid base disorders (except • Dissociation of salt in water results to the electrolyte
increased plasma anion gap metabolic acidosis) solution.
• Conclusion: If sodium concentration stays constant but o This is because as salt dissolves, the dissociated ions
chloride concentration changes, an acid base disorder is in the solution are free to move around, allowing a
present charge to flow freely.
o The resulting solution will conduct electricity since it
MIXED-ACID DISORDER contains ions.
• Defined as the presence of just one of the foregoing • Ions – any atom or group of atoms that has one or more
derangements. positive or negative electrical charges
• More than one disorder may be present at the same time in o Cations – ions with positive charge
a mixed disorder. o Anions – ions with negative charge
• A mixed disorder may include an acidosis and alkalosis that • Positive & negative charges balance inside and outside
partly counterbalance each other, or two separate of the cell
conditions impacting the pH in the same direction. o A neuron is negatively charged while it is at rest: the
inside of the cell is about 70 millivolts more negative
Respiratory • Occurs when the lungs are unable to than the outside
acidosis eliminate all of the carbon dioxide o It has a positive charge because it is missing one
produced by the body. electron.
• the bodily fluids, particularly the blood, • Count charges in milliequivalents
become overly acidic as a result of this. o The expression mEq represents the amount of solute
Metabolic • Is a condition in which the body's fluids in mg equal to 1/1000 the gram of the equivalent weight
acidosis contain too much acid. of the substance.
Respiratory • Characterized by a primary reduction in o Equivalent weight = 147/2 = 73.5 grams and 73.5
alkalosis carbon dioxide partial pressure (PCO2), grams/1000 = 0.0735 grams or 73.5 mgs.
which may or may not be accompanied
by a compensatory decrease in
bicarbonate (HCO3)
o pH may be high or near normal.
• An increase in respiratory rate or volume
(hyperventilation) or both may be the • Dissociation of water
cause. o At 25 °C, water molecules break into equal amounts of
• Acute or chronic respiratory alkalosis H3O+ and OH, resulting in concentrations of 1.00107
may occur. mol dm3.
Metabolic • A condition in which the blood becomes o A neutral solution is defined as one in which the
alkalosis too alkaline. concentrations of H3O+ and OH are equal.
o The pH of the neutral point is usually calculated to be
• The polar opposite of alkaline is acidic.
12pKw.
• When the acid-alkaline balance in our
• Electrolytes attract water
blood is slightly tilted toward the alkaline,
o Your body maintains its fluid balance through the action
our bodies function optimally.
of substances called electrolytes, which are mineral
compounds that, when dissolved in water, become
MINERAL BALANCE electrically charged particles called ions.
• Water follows electrolytes
DISSOCIATION OF SALT IN WATER o In this case, electrolytes come into play. The cell (or,
• Positively or negatively charged ions that help your body more precisely, the numerous sodium-potassium
regulate fluid balance. pumps in its membrane) continually pumps sodium
• Three important electrolytes that carry out this function ions out to form a chemical gradient.
are: o The sodium-potassium pump restores equilibrium by
o Sodium reintroducing sodium into the extracellular fluid,
o Potassium followed by water.
o Chloride • Osmosis is when water moves across a membrane
BONE GROWTH AND MAINTENANCE toward more concentrated solutes (proteins regulate
• Normal bone development requires vitamins D, C, and flow)
A, as well as minerals like calcium, phosphorus, and o When a semipermeable membrane divides two fluid
magnesium. spaces, water will flow from one with a lower solute
• Hormones such as parathyroid hormone, growth concentration to the other with a greater solute
hormone, and calcitonin are also important for bone concentration to reach equilibrium and balance the
growth and maintenance. osmotic pressures.
BENIG | BERNARDINO | COLLAMAR | CALOMOT | DANCEL | GO | GONZALVO | LACAO | MANGOBA | ROALES |
ROSALES | SORIANO | PARULI | PORLAS | VILLEGAS | VILLAFLOR | VILLAMAYOR
TRANS UNIT 7.2: REGULATORY PROTEINS
REGULATION OF FLUID AND ELECTROLYTE o Creates much of the osmotic pressure of ECF; the
BALANCE most abundant cation in ECF
• Mineral concentrations and variations in the body must be o Essential for electrical activity of neurons and muscle
consistent cells.
• Regulation occurs in the GI tract and kidneys • Salt in diet
• Liver recycles 8 liters of fluids/minerals per day o 2400 mg per day
• The adrenal glands are responsible for regulating the o High sodium intake lead to high blood pressure
kidneys, potassium, and sodium o Will adapt to a low-sodium diet
REGULATION OF BLOOD PRESSURE CHLORIDE
• 750mg/day
MECHANISMS • Functions
1 Blood pressure drops = renin is excreted o Major anion of extracellular
• The renin-angiotensin-aldosterone system is a o Part of HCI in gastric juice
fundamental regulator of arterial blood pressure, with o Most abundant anion in ECF, diffuses easily into and
activation of the cascade boosting blood pressure out of cells, helps regulate osmotic pressure.
and suppression reducing it. • Toxicity
2 Blood pressure drops = kidney reabsorbs sodium o Vomiting – acts on goblet cells
• Aldosterone helps the kidney to reabsorb more salt
and water into the bloodstream, increasing blood POTASSIUM (K+)
volume and restoring salt levels and blood pressure. • 2000mg/day
3 Angiotensin excreted = vasoconstrictor • Functions
• Angiotensin also promotes salt retention by the o Intracellular cation
kidneys by stimulating the production of aldosterone o Creates much of the osmotic pressure in ICF; the most
from the adrenal cortex. abundant cations in ICF
• It's a part of the blood pressure-controlling renin- o Essential for electrical activity of neurons and muscle
angiotensin system. cells
4 Aldosterone and sodium retention = retain more • Deficiency
sodium and water o Paralysis, muscular weakness
• Aldosterone helps the kidney to reabsorb more salt • Toxicity
and water into the bloodstream, increasing blood o Vomiting, heart, muscular weakness
volume and restoring salt levels and blood pressure.
5 High sodium diets aggravate hypertension through CALCIUM (Ca2+)
water retention (interstitial space) • 1000-1200 mg /day
• When you consume too much sodium-containing • Functions
salt, your body stores more water to "flush" the salt o Most (98%) is found in bones and teeth
out of your system. This may cause blood pressure o Maintains normal excitability of neurons and muscle
to rise in certain persons. The extra water puts your cells
heart and blood arteries under strain. o Essential for blood clotting
o Nerve function
ELECTROLYTES • Food source
• Cations (positively charged ions) o Fish w/ bones, dark green vegetables, fortified foods
o Calcium (Ca2+)
o Extracellular BLOOD CALCIUM REGULATION
§ Sodium (Na+) • Calcitonin
o Intracellular • Lower Blood Calcium
§ Potassium (K+) and Magnesium (Mg2+) o Decrease calcitriol and parathyroid hormone
• Anions (negatively charged ions) • Parathyroid Hormone
o Extracellular o Increase calcium absorption via increased calcitriol
§ Chloride (Cl− ) o Increase calcium release from bone
o Intracellular o Increase blood calcium
§ Phosphate (HPO42−) o Retain calcium from excretion
o Bicarbonate (HCO3−) EFFECTS OF CHRONICALLY LOW CALCIUM INTAKE
o Sulfate (SO42−) • Deficiency
o Stunted growth, osteoporosis
SODIUM (Na+) • Increase in Blood Parathyroid Hormone
• Minimum requirement: 500mg/day Concentration
• Rare deficiency o Persistent
o Muscle cramps, mental apathy o Increase in Bone Resorption, hence bone turnover
• Toxicity • Reduction in Bone Mineral Content (BMC) and
o Acute hypertension, edema Density (BMD)
• Chief functions = extracellular cations
BENIG | BERNARDINO | COLLAMAR | CALOMOT | DANCEL | GO | GONZALVO | LACAO | MANGOBA | ROALES |
ROSALES | SORIANO | PARULI | PORLAS | VILLEGAS | VILLAFLOR | VILLAMAYOR
TRANS UNIT 7.2: REGULATORY PROTEINS
• Increased Risk of Fracture of Trabecular and Cortical • Carrier proteins
Bone Tissue in Bones o Mucosal transferrin
• Increased Risk of Osteoporotic Fractures o Blood transferrin
FACTORS THAT ENHANCE CALCIUM ABSORPTION § Delivers iron to bone marrow & cells
• Stomach acid • Storage – protects from free radical action
• Vitamin D o GI mucosal ferritin
• Lactose § Receives iron & stores it in intestinal cells
• Growth hormone o Ferritin
o High levels store as hemosiderin
PHOSPHORUS
IRON TOXICITY
• Recommended Daily Allowance = 700mg/day
• Iron Overload = tissue damage (tissue damage = iron
• Function
overload)
o Mineralization of bones & teeth, part of every cell, part
o Hemochromatosis
of phospholipids, used in energy transfer & in buffering
system o Hemosiderosis
o Worsened by ETOH, Vitamin C
• Deficiency
• Iron & Heart Disease - inconclusive
o Weakness & bone pain
• Toxicity • Iron & Cancer
o Low blood calcium levels • Iron Poisoning - 200 mg Fe has led to death of young
children (5 tablets)
o This is why iron supplements needs to be
MAGNESIUM maintained
• RDA = 310 - 400 mg/day • Constipation with supplements
• Function
o Bone mineralization, building of protein, enzyme
action, muscle contraction ZINC
o Protects against hypertension and heart disease • Functions
• Deficiency o Cofactor for over 100 enzymes - this is why you can
o Weakness, confusion, convulsions, growth failure see zinc in multivitamins even vitamin C
• Toxicity - not known o Helps make DNA/RNA
o Helps manufacture heme
o Helps release Vitamin A for storage
SULFUR
o Helps metabolize CHO (carbohydrates)
• Function o Synthesize proteins
o Part of proteins, biotin, thiamin and insulin
o Metabolize ETOH (Ethanol)
• Deficiency – none known • Absorption & Metabolism
• Toxicity o Cell storage binding protein = metallothionein (also
o Depresses growth binds copper)
• Sources – all protein foods o Transport protein = albumin
o Transferrin also binds zinc
TRACE MINERALS • Excretion via feces
IRON IODINE
• Reduced iron (Fe2+) = ferrous iron • Function
• Oxidized Iron (Fe3+) = Ferric Iron o Part of the hormone thyroxine (T3 & T4 - thyroid gland
• Allows Fe to participate in oxidation reduction reactions in hormones)
every cell, such as o Regulates body temperature, metabolic rate,
o ETC protein reproduction, growth, blood cell production, nerve and
• Accepts carries & releases oxygen muscle functions
o Myoglobin – muscle • Example:
o Hemoglobin – red blood cells o Females have thyroid diseases = usually they have a
• Iron Sources to meet RDA 10 – 15 mg/day hard time conceiving a child
o Heme iron (meat sources) o Affects muscle functions and calcium concentration
§ Absorption >20% within the body
§ Meat fish protein factor (MFP)
• Nonheme iron (veg & meat sources) NOTE:
o Absorption 2-20% • Females are more sensitive to deficiencies and
o Enhance absorption: vitamin C (keeps non-heme concentration of minerals in the body.
iron reduced), as does citric acid, lactic acid, HCl from • This is why they should be vigilant in taking vitamins
the stomach, sugars and always eat a balanced amount of food because
o Iron deficiency they are prone to a lot of disorders, especially mineral
o Inhibit absorption: phytates & fiber, calcium & disorders.
phosphorus, EDTA, tannic acid - bind iron
BENIG | BERNARDINO | COLLAMAR | CALOMOT | DANCEL | GO | GONZALVO | LACAO | MANGOBA | ROALES |
ROSALES | SORIANO | PARULI | PORLAS | VILLEGAS | VILLAFLOR | VILLAMAYOR
TRANS UNIT 7.2: REGULATORY PROTEINS
• RDA = 150 micrograms/day MOLYBDENUM
o Iodized salt, seafood, plant & animals from soil • Function
• Deficiency o Facilitator of many enzymes
o Goiter leading to sluggishness & weight gain • Al = 75 = 260 microgram/day
o During pregnancy leads to cretinism (MR) - a disorder • Deficiency = rare
for the unborn child • Toxicity rare
o Iodized salt is developed to fight off deficiency in iodine. o Gout like symptoms with exposure
• Toxicity > 2000 micrograms o “With exposure” – meaning one have other conditions
o Goiter that could lead to the increase of the viability of having
toxicity with molybdenum
SELENIUM
• Function NOTE:
o Antioxidant working with vitamin E • Most of the traced elements mentioned, they are
• RDA = 55 to 70 micrograms/day usually related to being cofactors and coenzymes.
o Seafood, meat, grains (where you can get selenium) • That is why even in small amounts they are important
• Deficiency because it triggers a lot of cellular functions and
o Heart disease from viruses and cancer like symptoms metabolic functions.
o Cancer – lacking evidence, needs more research • If not for these, there are metabolic functions that will
• Toxicity (rare & minimal) not continue or ensue.
o Vomiting, diarrhea, loss of hair & nails, skin lesions, •
and NS problems
COPPER
• Function
o Many reactions - like iron in metabolic reactions related
to release of energy
o Related to enzymatic functions and cofactors
• RDA = 1.5 - 3.0 mg/day
• Deficiency rare
o Genetic disorder
o Only happens in Menkes disorder
o Menkes disorder – releases copper into the
bloodstream and it could be life threatening because it
could poison the blood
• Toxicity
o Genetic disorder = Wilson’s disease copper
accumulates in liver and brain (give chelating agents
such as zinc)
o Usually doesn’t happen unless we have Wilson’s
disease
MANGANESE
• Function
o Cofactor of many enzymes
• RDA = 2-5 mg/day in most foods
• Deficiency rare
o Phytates, iron & calcium inhibit absorption
• Toxicity
o Brain disease
CHROMIUM
• Function
o Facilitates CHO (carbohydrate) & Lipid metabolism
• AI = 50 - 200 microgram/day
• Deficiency
o Diabetes like syndrome
• Toxicity
o Damage skin & kidneys
o Supplements for chromium picolinate
• Others
o Nickel, Silicon, Vanadium, Cobalt
BENIG | BERNARDINO | COLLAMAR | CALOMOT | DANCEL | GO | GONZALVO | LACAO | MANGOBA | ROALES |
ROSALES | SORIANO | PARULI | PORLAS | VILLEGAS | VILLAFLOR | VILLAMAYOR
You might also like
- Water: PH and BuffersDocument63 pagesWater: PH and BuffersSoffa ShmuelNo ratings yet
- Acid Base Imbalance (Rubina)Document98 pagesAcid Base Imbalance (Rubina)Parvathy R Nair100% (1)
- Gep Crash Course - FoundationsDocument50 pagesGep Crash Course - Foundationsyecib80467No ratings yet
- Acid-Base BalanceDocument47 pagesAcid-Base BalanceEmmanuel RocksonNo ratings yet
- Blood Gas Analysis4231 PDFDocument84 pagesBlood Gas Analysis4231 PDFEng-Mugahed AlmansorNo ratings yet
- Acid Base DisordersDocument66 pagesAcid Base DisordersIvan HensonNo ratings yet
- Clinical Chemistry II ELECTROLYTESDocument2 pagesClinical Chemistry II ELECTROLYTESEden MaeNo ratings yet
- Understand Acid-Base DisordersDocument89 pagesUnderstand Acid-Base DisordersEdouinaNo ratings yet
- Acid Base Regulation - ppt@BVSCAH-6th SemDocument95 pagesAcid Base Regulation - ppt@BVSCAH-6th SemDr. Prakash PanthiNo ratings yet
- Acid-Base Balance: Editor: Dr. Husnil Kadri, MkesDocument66 pagesAcid-Base Balance: Editor: Dr. Husnil Kadri, MkesDwi SiregarNo ratings yet
- BIO 024 Session 1 7Document67 pagesBIO 024 Session 1 7Tracy DavidNo ratings yet
- Acid Base2005Document64 pagesAcid Base2005AgusNo ratings yet
- Acid-Base Imbalances: Dr. Emmanuel Sandy Department of Chemical Pathology Comahs-UslDocument49 pagesAcid-Base Imbalances: Dr. Emmanuel Sandy Department of Chemical Pathology Comahs-UslVivian KamaraNo ratings yet
- 9 - (D) Acid Base Balance Dec 4.17Document61 pages9 - (D) Acid Base Balance Dec 4.17khaledNo ratings yet
- Chapter-7 Acid Base Regulation I) Blood Hydrogen Ion Concentration Is Normally Maintained Around Normal Value ofDocument33 pagesChapter-7 Acid Base Regulation I) Blood Hydrogen Ion Concentration Is Normally Maintained Around Normal Value ofPukhtoon ZalmyNo ratings yet
- Hydrogen Hydroxide: Acid-Base Balance Overview of Acids and Bases DescriptionDocument15 pagesHydrogen Hydroxide: Acid-Base Balance Overview of Acids and Bases DescriptionElisha WorworNo ratings yet
- ACID BASE BALANCE and disordersDocument47 pagesACID BASE BALANCE and disordersShivanand MaliNo ratings yet
- Functions of Cells and Human Bod1Document24 pagesFunctions of Cells and Human Bod1Dawlat SlamaNo ratings yet
- Maintaining Normal PH Through BuffersDocument40 pagesMaintaining Normal PH Through BuffersRJ Noor JanNo ratings yet
- Acid-Base Balance ABGs InterpretationDocument30 pagesAcid-Base Balance ABGs InterpretationQusai IbraheemNo ratings yet
- Acid Based Disorders Med07Document28 pagesAcid Based Disorders Med07Salem Ali BawazeerNo ratings yet
- Acid-Base Balance and Its DisordersDocument37 pagesAcid-Base Balance and Its Disordersmaria angela SaldajenoNo ratings yet
- Autonomous State Medical College Shahjahanpur, Uttar Pradesh AnantDocument17 pagesAutonomous State Medical College Shahjahanpur, Uttar Pradesh Anantrahul dev varunNo ratings yet
- Acid - Base Balance: Basic Facts - Repetition Regulation of A-B Balance Pathophysiology of Clinically Important DisordersDocument25 pagesAcid - Base Balance: Basic Facts - Repetition Regulation of A-B Balance Pathophysiology of Clinically Important DisordersRrNo ratings yet
- Acidosis & AlkalosisDocument29 pagesAcidosis & Alkalosiszaeem1993No ratings yet
- Acid/Base Balance and DisorderDocument39 pagesAcid/Base Balance and DisorderKuzhandai VeluNo ratings yet
- BicarbonateDocument5 pagesBicarbonateRace MendezNo ratings yet
- ACID BASE PHYSIOLOGY: A GUIDE TO CHEMICAL BUFFER SYSTEMS AND H+ REGULATIONDocument28 pagesACID BASE PHYSIOLOGY: A GUIDE TO CHEMICAL BUFFER SYSTEMS AND H+ REGULATIONParvathy R NairNo ratings yet
- Acid Base BalanceDocument76 pagesAcid Base BalanceSobha MatthewNo ratings yet
- Acid Base Balance OR OR Regulation of Blood PHDocument175 pagesAcid Base Balance OR OR Regulation of Blood PHhirendra patel100% (1)
- Blood Gases, PH, and Buffer SystemDocument22 pagesBlood Gases, PH, and Buffer SystemAhmed GaberNo ratings yet
- Acid-Base ImbalancesDocument18 pagesAcid-Base ImbalancesChrisnel CaoileNo ratings yet
- Arterial Blood Gas Analysis: DR - Rakesh Chandra Chaurasia PGT 3 Ims, Bhu Moderator: DR - Manjaree Mishra Asset - ProfDocument64 pagesArterial Blood Gas Analysis: DR - Rakesh Chandra Chaurasia PGT 3 Ims, Bhu Moderator: DR - Manjaree Mishra Asset - ProfArmaanjeet SinghNo ratings yet
- Acid - Base BalancesDocument68 pagesAcid - Base Balancesjames makulaNo ratings yet
- 4.20 4.21+Buffers+in+Blood+++Acid+Rain+ (ONLINE)Document24 pages4.20 4.21+Buffers+in+Blood+++Acid+Rain+ (ONLINE)aliNo ratings yet
- Acid-Base Regulation SummaryDocument59 pagesAcid-Base Regulation SummaryInzamamul Haque ShihabNo ratings yet
- Physiology Acid Base EditedDocument46 pagesPhysiology Acid Base EditedSarah BirechNo ratings yet
- Acid base disorders simplified/TITLEDocument48 pagesAcid base disorders simplified/TITLEAGUNG SETIADI NUGROHONo ratings yet
- Unit 5 ACID BASE MAINTENANCEDocument21 pagesUnit 5 ACID BASE MAINTENANCEanulalparayil2003No ratings yet
- DECIPHER THE NUMBERS ABGsDocument8 pagesDECIPHER THE NUMBERS ABGsBeatrice Joy TombocNo ratings yet
- Acid-Base BalanceDocument38 pagesAcid-Base BalanceNym Angga SantosaNo ratings yet
- Fluid-Electrolytes and Acid-Base Disturbance in Surgery: Haidi Hu, MD, PHDDocument68 pagesFluid-Electrolytes and Acid-Base Disturbance in Surgery: Haidi Hu, MD, PHDHUNEL KimNo ratings yet
- Final MCW .ABDpptxDocument124 pagesFinal MCW .ABDpptxFazlul KarimNo ratings yet
- 7 Acidbase-ImbalanceDocument5 pages7 Acidbase-ImbalanceMarie Louise Nicole TuvillaNo ratings yet
- Physiology of Acid Base Balance by Dr. ROOMIDocument70 pagesPhysiology of Acid Base Balance by Dr. ROOMIMudassar Roomi100% (1)
- Acid - Base BalanceDocument13 pagesAcid - Base Balanceadam yassineNo ratings yet
- BCH 201 ModuleDocument15 pagesBCH 201 ModuleJoyNo ratings yet
- 295 - Renal Pathology) Acid Base Disorders and ABG Interpretation - IntroductionDocument6 pages295 - Renal Pathology) Acid Base Disorders and ABG Interpretation - IntroductionMuhammadR1No ratings yet
- Regulating The Internal Environment: AP BiologyDocument45 pagesRegulating The Internal Environment: AP Biologyjulie rainesNo ratings yet
- Arterial Blood Gas AnalysisDocument32 pagesArterial Blood Gas AnalysisPradip ChougaleNo ratings yet
- BASIC CONCEPT OF ACID-BASEDocument30 pagesBASIC CONCEPT OF ACID-BASEYaniNo ratings yet
- Acid-Base Balance and Anion GapDocument37 pagesAcid-Base Balance and Anion GapMsa AhhfaaNo ratings yet
- "If One Advances Confidently in The Direction of His Dreams, He Will Meet With A Success Unexpected in Common HoursDocument44 pages"If One Advances Confidently in The Direction of His Dreams, He Will Meet With A Success Unexpected in Common Hourssantana2007No ratings yet
- Acid Base TutorialDocument47 pagesAcid Base TutorialDiah Puspita Rini100% (2)
- Abg PPT NewDocument69 pagesAbg PPT NewMalaka Atapattu100% (2)
- Unit 1: Renal System: Acid-Base BalanceDocument48 pagesUnit 1: Renal System: Acid-Base BalancePPP MOHD SUKRINo ratings yet
- Thursday 15 1-30 Jonathan TaliercioDocument74 pagesThursday 15 1-30 Jonathan TaliercioCroitoru CosminNo ratings yet
- Renal Physiology The Collecting DuctDocument3 pagesRenal Physiology The Collecting DuctSahnusha SryenNo ratings yet
- 14 Metabolic AlkalosisDocument32 pages14 Metabolic AlkalosisJoel Topf100% (2)
- Journal On Gender, Socio Economic, Cultural Attributes of The LearnerDocument1 pageJournal On Gender, Socio Economic, Cultural Attributes of The LearnerKeila RosalesNo ratings yet
- ROSALES, Keila C.Document2 pagesROSALES, Keila C.Keila RosalesNo ratings yet
- November 23Document2 pagesNovember 23Keila RosalesNo ratings yet
- Medication PreparationDocument3 pagesMedication PreparationKeila RosalesNo ratings yet
- Providing Health Education to Special PopulationsDocument2 pagesProviding Health Education to Special PopulationsKeila RosalesNo ratings yet
- Changing Infusion TubingDocument2 pagesChanging Infusion TubingKeila RosalesNo ratings yet
- Pathophysiology Impetigo-AgnDocument1 pagePathophysiology Impetigo-AgnKeila RosalesNo ratings yet
- 2nu08 - Rosales, Keila C - Journal#1Document1 page2nu08 - Rosales, Keila C - Journal#1Keila RosalesNo ratings yet
- CATHETERIZATIONDocument3 pagesCATHETERIZATIONKeila RosalesNo ratings yet
- 1nu09 - Rosales, Keila C.Document6 pages1nu09 - Rosales, Keila C.Keila RosalesNo ratings yet
- Changing Iv SolutionsDocument2 pagesChanging Iv SolutionsKeila RosalesNo ratings yet
- Acute GlomerulonephritisDocument1 pageAcute GlomerulonephritisKeila RosalesNo ratings yet
- Bedmaking Occupied Bed 22Document2 pagesBedmaking Occupied Bed 22Keila RosalesNo ratings yet
- DrugDocument19 pagesDrugKeila RosalesNo ratings yet
- Parenteral Administration - ChecklistDocument4 pagesParenteral Administration - ChecklistKeila RosalesNo ratings yet
- Regulating IV Performance ChecklistDocument2 pagesRegulating IV Performance ChecklistKeila RosalesNo ratings yet
- Bathing of The Newborn ChecklistDocument5 pagesBathing of The Newborn ChecklistKeila RosalesNo ratings yet
- Pathophysiology Impetigo-AgnDocument1 pagePathophysiology Impetigo-AgnKeila RosalesNo ratings yet
- ROSALES, KeilaDocument8 pagesROSALES, KeilaKeila RosalesNo ratings yet
- Vital SignsDocument3 pagesVital SignsKeila RosalesNo ratings yet
- Biochemistry in HomeostasisDocument2 pagesBiochemistry in HomeostasisKeila RosalesNo ratings yet
- Gastroenteritis PathophysiologyDocument1 pageGastroenteritis PathophysiologyKeila RosalesNo ratings yet
- Drug Study School Nsg.Document12 pagesDrug Study School Nsg.Keila RosalesNo ratings yet
- Tracheostomy Suctioning ChildDocument3 pagesTracheostomy Suctioning ChildKeila RosalesNo ratings yet
- Dengue Fever Case ScenarioDocument1 pageDengue Fever Case ScenarioKeila RosalesNo ratings yet
- Lecture - Blood & Homeostasis - Part 1Document6 pagesLecture - Blood & Homeostasis - Part 1Keila RosalesNo ratings yet
- Rosales, Keila - 2nu08 - Journal#3Document2 pagesRosales, Keila - 2nu08 - Journal#3Keila RosalesNo ratings yet
- First and Second RecitationDocument2 pagesFirst and Second RecitationKeila RosalesNo ratings yet
- Laboratory - ImmunityDocument7 pagesLaboratory - ImmunityKeila RosalesNo ratings yet
- Biochemistry of Aging Lab OutlineDocument1 pageBiochemistry of Aging Lab OutlineKeila RosalesNo ratings yet
- STC Bec Wir Plu D 0209 01 PDFDocument10 pagesSTC Bec Wir Plu D 0209 01 PDFAdel MorsyNo ratings yet
- A 1116Document15 pagesA 1116Rama S. SinghNo ratings yet
- M&SDocument39 pagesM&Sgo.pushp70910% (1)
- GORUCK Heavy - 6-week training program overviewDocument4 pagesGORUCK Heavy - 6-week training program overviewJohn Rohrer100% (2)
- Biomechinics PDFDocument8 pagesBiomechinics PDFImran KhanNo ratings yet
- Trisyl Silica Gel: For Oils/Fats and Biofuel RefiningDocument4 pagesTrisyl Silica Gel: For Oils/Fats and Biofuel RefiningJosé Mauricio Bonilla TobónNo ratings yet
- Proper Application of Duff Phelps ERP Adjustment PDFDocument4 pagesProper Application of Duff Phelps ERP Adjustment PDFramsiva354No ratings yet
- Roof Construction Dr. Fixit Newcoat PDFDocument1 pageRoof Construction Dr. Fixit Newcoat PDFRishabh VijayNo ratings yet
- Presley v. Lockwood: Respondent's Trial BriefDocument37 pagesPresley v. Lockwood: Respondent's Trial BriefTony Ortega100% (2)
- Waleed Alomari CVDocument2 pagesWaleed Alomari CValomari_waleedNo ratings yet
- CH 2Document20 pagesCH 2Vivek SinghNo ratings yet
- Pengaruh Ukuran Potongan Kopra Dalam Proses Pengeringan: Effect of The Copra Cut Size in The Drying ProcessDocument5 pagesPengaruh Ukuran Potongan Kopra Dalam Proses Pengeringan: Effect of The Copra Cut Size in The Drying ProcessAlexia Desi Ratnasari Loi 1841100210No ratings yet
- General Biology 1 - Power Point Presentation (Group 8)Document14 pagesGeneral Biology 1 - Power Point Presentation (Group 8)Archan Dom ReyesNo ratings yet
- 4 WP 2013Document8 pages4 WP 2013TUTORKIMNo ratings yet
- MFT28 - Greg Plitt's 4-Week Military Fitness Trainer by MET-RxDocument7 pagesMFT28 - Greg Plitt's 4-Week Military Fitness Trainer by MET-RxRayNo ratings yet
- LV CB Catalogue PDFDocument260 pagesLV CB Catalogue PDFBoobesh Kumar SekarNo ratings yet
- Della Core DutiesDocument12 pagesDella Core DutiesSt SNo ratings yet
- REBA Employee Assessment Worksheet: A. Neck, Trunk and Leg AnalysisDocument1 pageREBA Employee Assessment Worksheet: A. Neck, Trunk and Leg AnalysisAgni JayantiNo ratings yet
- Chemistry in Everyday LifeDocument33 pagesChemistry in Everyday LifeArya StarkNo ratings yet
- Lubricants: Chapter - 5 Lubricants and LubricationDocument5 pagesLubricants: Chapter - 5 Lubricants and LubricationMalaika AzeemNo ratings yet
- Nihms 223615 PDFDocument15 pagesNihms 223615 PDFElay PedrosoNo ratings yet
- SonoAce R7 v3.01.00 EDocument544 pagesSonoAce R7 v3.01.00 EEcomedical PlussNo ratings yet
- Paper 1Document8 pagesPaper 1Santhoshi Sadhanaa SankarNo ratings yet
- BW Mc2 XWHM y Na ManualDocument23 pagesBW Mc2 XWHM y Na ManualSatyasrinivas PulavarthiNo ratings yet
- Salary Exchange... A Tax Efficient Way To Boost Your Plans For The FutureDocument4 pagesSalary Exchange... A Tax Efficient Way To Boost Your Plans For The FutureStandard Life UKNo ratings yet
- Administrative Case ResolutionDocument2 pagesAdministrative Case ResolutionEunice Osam RamirezNo ratings yet
- Cat Helimax 2016 Esp 1Document74 pagesCat Helimax 2016 Esp 1HKM IngenierosNo ratings yet
- LC Used in ProteimicsDocument15 pagesLC Used in ProteimicsMandu ManNo ratings yet
- Holy Childhood High School Chemistry 601 Topic: Electronic StructureDocument6 pagesHoly Childhood High School Chemistry 601 Topic: Electronic StructureBriana BartonNo ratings yet
- Impact of Excessive Mobile Phone Usage On Human JCSB 1000235Document5 pagesImpact of Excessive Mobile Phone Usage On Human JCSB 1000235nidNo ratings yet