Professional Documents
Culture Documents
Demo Ahmm
Demo Ahmm
Uploaded by
DELOS SANTOS JESSIECAHOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Demo Ahmm
Demo Ahmm
Uploaded by
DELOS SANTOS JESSIECAHCopyright:
Available Formats
GTPAL stands for Gravidity (number of pregnancies including current), Term (number of pregnancies
carried to 37+ weeks), Preterm (number of pregnancies carried between 20 and 36.6 weeks ),
Abortion (number of losses prior to 20 weeks), and Living (number of living children)
Tell me about your patient.
- So the patient name is Pamela Barth, a 17 year old G1 P1, she is transferred in post-partal
service following the birth of a 9lb(pound) 4oz(ounce) infant boy. She is in vaginal bleeding is so
heavy saturating perineal pad every 20 minutes.
What is the medical diagnosis of the patient?
- Mild uterine Antony
What is uterine Atony?
- A complication after the delivery of the mother which is a failure of the uterus contract after
delivery which is a life threatening, cause by post-partum hemorrhage.
What are the cause of uterine atony?
- Prolonged labor
- Rapid labor
- The use of oxytocin or other drugs or general anesthesia during labor
- Enlargement of the uterus
How to prevent uterine atony?
- Taking prenatal vitamins like iron supplements to help prevent anemia and other complications
after delivery.
- Folic acid to help the infant the growth and the development.
What is oxytocin?
- Use to activate the oxytocin receptors so that it can give pressure, it can strengthen the uterine
contraction for the delivery.
What is your nursing care plan.
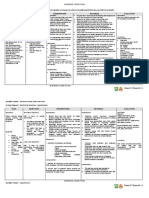
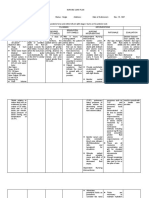
CLUSTERED NURSING RATIONALE OUTCOME NURSING RATIONALE EVALUATION
CUES DIAGNOSIS CRITERIA INTERVENTION
S
The The patient The After 8 First is to assess
The blood After 8 hours the
Subjective: diagnosed from postpartum hours the and document loss and the patient is able to:
“Should I be the uterine hemorrhage patient is the amount of existence of
bleeding this agotty one of can cause of able to: bleeding count the blood Manifest the improved
much? as the decreasing and weigh the clots will fluid balance by the
what the pathophysiolog fluid She need to perineal pads help to lochial flow in the
patient said. y of postpartum volume, and have a and save blood determine perineal pad per hour
hemorrhage. it can lead normal clots to be the and obtain a
The to result of evaluated by appropriate hemoglobin level of
Objective: dehydration. her the physician. displacement 12g/dl
Blood loss is hemoglobin for the
750 ml level of Need to monitor patient’s
12g/dl, the the vital signs need.
Temperature: vital signs specifically the
98.6F must be blood pressure, Increasing of
Blood stable and pulse and heart the heart
she needs rate. rate can be
Blood to have a result of
Pressure: lochial flow Administer decrease of
100/60 less than uterotonic fluid volume
one agents and that will
Heart Rate: saturated medications as change the
100bpm perineal prescribed by blood
pad per the physician. pressure.
Respiratory hour.
Rate: The agent
22bpm (uterotonic
agent) to
Hemoglobin: control the
8.9g/dl postpartum
hemorrhage.
Uterus:
Boggy Uterus Oxytocin
used to
prevent and
one of the
treatments
for PPH, to
decrease the
blood flow
through the
uterus after
delivery.
You might also like
- Post Partum Hemorrhage Nursing Care PlanDocument2 pagesPost Partum Hemorrhage Nursing Care PlanCyrus De Asis82% (33)
- Chapter 22 Nursing Management of The Postpartum Woman at RiskDocument18 pagesChapter 22 Nursing Management of The Postpartum Woman at RiskSusanna ConigliaroNo ratings yet
- NURSING CARE PLAN - Spontaneous AbortionDocument2 pagesNURSING CARE PLAN - Spontaneous Abortionderic97% (36)
- Nursing Care Plan AbortionDocument4 pagesNursing Care Plan AbortionJane Casiquin100% (1)
- Waiters PATIENT CARE PLAN 2020 For PPHDocument3 pagesWaiters PATIENT CARE PLAN 2020 For PPHmp1757No ratings yet
- BOX 17.4 NCP Postpartum HemorrhageDocument4 pagesBOX 17.4 NCP Postpartum HemorrhageJam AliNo ratings yet
- Post Partum Hemorrhage Nursing Care Plan PDFDocument2 pagesPost Partum Hemorrhage Nursing Care Plan PDFA sison100% (1)
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument5 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationBiway RegalaNo ratings yet
- Final Drug Study and Nursing Care For Cs Final Na GidDocument7 pagesFinal Drug Study and Nursing Care For Cs Final Na GidMor Shi DA BalutintikNo ratings yet
- NCP GI EditedDocument4 pagesNCP GI EditednicoleNo ratings yet
- Final NCP For PostpartumDocument8 pagesFinal NCP For PostpartumJam Ali100% (1)
- NCP PlanningDecreased in Cardiac Output Related To Low Hemoglobin and Hematocrit CountDocument6 pagesNCP PlanningDecreased in Cardiac Output Related To Low Hemoglobin and Hematocrit CountMabelle SorianoNo ratings yet
- Mod 3C Nursing Care Plan - Macanas, Evangeline Anne A. BSN 2BDocument4 pagesMod 3C Nursing Care Plan - Macanas, Evangeline Anne A. BSN 2BEvangeline Anne MacanasNo ratings yet
- Acute Kidney Injury W/ Hyperkalemia NCPDocument5 pagesAcute Kidney Injury W/ Hyperkalemia NCPMyrvic Ortiz La OrdenNo ratings yet
- Agn - NCPDocument3 pagesAgn - NCPRap De la CruzNo ratings yet
- Acute Renal Failure Nursing Care PlanDocument4 pagesAcute Renal Failure Nursing Care PlanKrisianne Mae Lorenzo Francisco80% (5)
- Ineffective Tissue PerfusionDocument3 pagesIneffective Tissue PerfusionAngel Hernandez100% (1)
- ICU 2 - Management For DICDocument20 pagesICU 2 - Management For DICNur Aziemah Mohd ZamriNo ratings yet
- NCP Risk For Decreased CO 1 PDFDocument2 pagesNCP Risk For Decreased CO 1 PDFdubsNo ratings yet
- Tams NCP and DrugDocument5 pagesTams NCP and DrugNicholas Xavier VenturaNo ratings yet
- Nursing Care Plan Rep FinalDocument7 pagesNursing Care Plan Rep Finalhanna castueraNo ratings yet
- Risk For Decreased Cardiac Output NCPDocument2 pagesRisk For Decreased Cardiac Output NCPMae Denn LabordoNo ratings yet
- Assessment Diagnosis Scientific Background Planning Intervention Rationale Evaluation Subjective: Short-Term Goals: Independent: Short-Term GoalsDocument2 pagesAssessment Diagnosis Scientific Background Planning Intervention Rationale Evaluation Subjective: Short-Term Goals: Independent: Short-Term GoalsMelvin D. RamosNo ratings yet
- NCP For Delivery RoomDocument4 pagesNCP For Delivery RoomGiselle EstoquiaNo ratings yet
- Cva NCPDocument2 pagesCva NCPSharewin PulidoNo ratings yet
- Nursing Care Plan For Client With Risk of Excess Fluid VolumeDocument2 pagesNursing Care Plan For Client With Risk of Excess Fluid VolumeThe Right WayNo ratings yet
- Nursing Care Plan: SubjectiveDocument6 pagesNursing Care Plan: SubjectiveAlimansor M. DarpingNo ratings yet
- NCP Example Pre EclampsiaDocument6 pagesNCP Example Pre EclampsiaChristian Joseph OpianaNo ratings yet
- Ectopic and Abortion NCPDocument6 pagesEctopic and Abortion NCPElizabeth Quiñones100% (1)
- DONE - NCM 116 RLE Week 9.docx ROXASDocument19 pagesDONE - NCM 116 RLE Week 9.docx ROXASBatiao Camille ClaireNo ratings yet
- To Facilitate The Maintenance of Fluid and Electrolytes ImbalanceDocument2 pagesTo Facilitate The Maintenance of Fluid and Electrolytes ImbalanceRainier IbarretaNo ratings yet
- KKKDocument4 pagesKKKAngelo LacsaNo ratings yet
- Postpartum HemorrhageDocument3 pagesPostpartum HemorrhageClaire Canapi BattadNo ratings yet
- Pih-Ncp - BSN2D ZacalDocument3 pagesPih-Ncp - BSN2D ZacalIllaizah EdictoNo ratings yet
- CASE-SCENARIO 5 QuestionareDocument16 pagesCASE-SCENARIO 5 QuestionareEduard GarchitorenaNo ratings yet
- 3amali TR 2Document7 pages3amali TR 2Arsh KaiwanNo ratings yet
- GI Bleeding Case 2Document4 pagesGI Bleeding Case 2Imah ArmildezNo ratings yet
- Nursing Care Plan AbortionDocument3 pagesNursing Care Plan Abortionnengsk84% (19)
- Assessment Diagnosis Planning Implementation Rationale EvaluationDocument2 pagesAssessment Diagnosis Planning Implementation Rationale EvaluationMargareth DandanNo ratings yet
- Hernandez NCP Drug StudyDocument7 pagesHernandez NCP Drug StudyEliza Joyce HernandezNo ratings yet
- Abruptio PlacentaeDocument8 pagesAbruptio Placentaealma santos100% (2)
- Nursing Care PlanDocument4 pagesNursing Care PlanMariel GamaloNo ratings yet
- Drug Study and NCP OutlineDocument3 pagesDrug Study and NCP Outlinerobertvaliente471No ratings yet
- Nursing Care PlanDocument11 pagesNursing Care PlanKirstin del CarmenNo ratings yet
- Impaired Electrolytes NCPDocument2 pagesImpaired Electrolytes NCPNora BacolNo ratings yet
- Ct7 Fluid, Electrolyte ImbalanceDocument9 pagesCt7 Fluid, Electrolyte ImbalanceAlondra VelascoNo ratings yet
- CT 11 - HPNDocument12 pagesCT 11 - HPNLycah RotoneNo ratings yet
- NCP Post PartumDocument2 pagesNCP Post PartumsteffiNo ratings yet
- Uterine Atony: Group 3Document23 pagesUterine Atony: Group 3Trisha Mae MarquezNo ratings yet
- Vehicular Accident (VA) Manifesting Hypovolemic Shock NCPDocument6 pagesVehicular Accident (VA) Manifesting Hypovolemic Shock NCPCHRISTIE MONTANONo ratings yet
- Nursing Care Plan - Spontaneous AbortionDocument2 pagesNursing Care Plan - Spontaneous Abortionderic100% (2)
- Nursing Care Plan Spontaneous AbortionDocument2 pagesNursing Care Plan Spontaneous AbortionAbigael Rubio de LeonNo ratings yet
- Nursing Care Plan: Lorma Colleges Con Template Related Learning ExperienceDocument4 pagesNursing Care Plan: Lorma Colleges Con Template Related Learning ExperienceMelinda Cariño BallonNo ratings yet
- Ob NCP PDFDocument5 pagesOb NCP PDFShakira Yvonne C. BORREROSNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Rationale Planning Intervention Rationale EvaluationDocument1 pageNursing Care Plan: Assessment Diagnosis Rationale Planning Intervention Rationale EvaluationMelody B. MiguelNo ratings yet
- PPH Transfusion Strategies NPEC 2017 PDFDocument90 pagesPPH Transfusion Strategies NPEC 2017 PDFRahmayanti YuliaNo ratings yet
- Nursing Care Plan On Platelet DisordersDocument8 pagesNursing Care Plan On Platelet DisordersbhavanaNo ratings yet
- Retained PlacentaDocument22 pagesRetained PlacentaLeander Isabelle NoolNo ratings yet
- Conceptual Framework PDFDocument1 pageConceptual Framework PDFDELOS SANTOS JESSIECAHNo ratings yet
- Group 1 ResearchDocument4 pagesGroup 1 ResearchDELOS SANTOS JESSIECAHNo ratings yet
- GRADE 1 - 2ND QUARTER - Xlsx.odsDocument99 pagesGRADE 1 - 2ND QUARTER - Xlsx.odsDELOS SANTOS JESSIECAHNo ratings yet
- NresDocument1 pageNresDELOS SANTOS JESSIECAHNo ratings yet
- Conceptual Framework PDFDocument1 pageConceptual Framework PDFDELOS SANTOS JESSIECAHNo ratings yet
- ACERDocument24 pagesACERDELOS SANTOS JESSIECAHNo ratings yet
- GRADE 4 6 SUMMARY - FINAL GRADES - Xlsx.odsDocument10 pagesGRADE 4 6 SUMMARY - FINAL GRADES - Xlsx.odsDELOS SANTOS JESSIECAHNo ratings yet
- Background of The StudyDocument1 pageBackground of The StudyDELOS SANTOS JESSIECAHNo ratings yet
- GRADE-4-6-EDUKASYONG PANTAHANAN AT PANGKABUHAYAN - Xlsx.odsDocument54 pagesGRADE-4-6-EDUKASYONG PANTAHANAN AT PANGKABUHAYAN - Xlsx.odsDELOS SANTOS JESSIECAHNo ratings yet
- GRADE 4 6 MATHEMATICS - Xlsx.odsDocument54 pagesGRADE 4 6 MATHEMATICS - Xlsx.odsDELOS SANTOS JESSIECAHNo ratings yet
- AcerDocument24 pagesAcerDELOS SANTOS JESSIECAHNo ratings yet
- GRADE-4-6-EDUKASYON SA PAGPAPAKATAO - Xlsx.odsDocument54 pagesGRADE-4-6-EDUKASYON SA PAGPAPAKATAO - Xlsx.odsDELOS SANTOS JESSIECAHNo ratings yet
- Worksheet 3-Subject and Content of ArtDocument2 pagesWorksheet 3-Subject and Content of ArtDELOS SANTOS JESSIECAHNo ratings yet
- Week 7 Study Guide Assumption and ApprehensionDocument1 pageWeek 7 Study Guide Assumption and ApprehensionDELOS SANTOS JESSIECAHNo ratings yet
- Application Letter TINAY T3Document1 pageApplication Letter TINAY T3DELOS SANTOS JESSIECAHNo ratings yet
- Group 1 ResearchDocument7 pagesGroup 1 ResearchDELOS SANTOS JESSIECAHNo ratings yet
- EngLISH 1 Q3 Mod4c Inferring The Character Feelings and Traits After Listening To A PoemongStory V2 1Document17 pagesEngLISH 1 Q3 Mod4c Inferring The Character Feelings and Traits After Listening To A PoemongStory V2 1DELOS SANTOS JESSIECAH100% (4)
- Certification Manang JoyDocument1 pageCertification Manang JoyDELOS SANTOS JESSIECAHNo ratings yet
- AP1 Q3 Modyul 4 Semana 6 Ang Importansiya Kang Eskuwelahan Sa Kabuhi Kag Sa Komunidad - V2 PDFDocument17 pagesAP1 Q3 Modyul 4 Semana 6 Ang Importansiya Kang Eskuwelahan Sa Kabuhi Kag Sa Komunidad - V2 PDFDELOS SANTOS JESSIECAHNo ratings yet
- Local Media8482552116122636235Document1 pageLocal Media8482552116122636235DELOS SANTOS JESSIECAHNo ratings yet
- PPIEL Art 39697-10Document8 pagesPPIEL Art 39697-10DELOS SANTOS JESSIECAHNo ratings yet
- Final Research ProposalDocument18 pagesFinal Research ProposalDELOS SANTOS JESSIECAHNo ratings yet
- English1 Q3 MOD 4 MELC4d Identifying Cause and Effect of Events Through Listening To Short StoriesPoem V2 1Document18 pagesEnglish1 Q3 MOD 4 MELC4d Identifying Cause and Effect of Events Through Listening To Short StoriesPoem V2 1DELOS SANTOS JESSIECAH100% (1)
- Contents of The CHN RLE Written RequirementsDocument4 pagesContents of The CHN RLE Written RequirementsRoshie Kaye AbalorioNo ratings yet
- CELLE DismenorreaDocument7 pagesCELLE DismenorreaJose Vergara GNo ratings yet
- Case Blighted Ovum - Jenni Mutiara Saragih (202006010015)Document28 pagesCase Blighted Ovum - Jenni Mutiara Saragih (202006010015)Jenni SaragihNo ratings yet
- 01a Growth and DevelopmentDocument3 pages01a Growth and DevelopmentAmaetenNo ratings yet
- MCP Guide BookDocument80 pagesMCP Guide BookJeyakumar SNo ratings yet
- Uterine AdenomyosisDocument21 pagesUterine AdenomyosisBatch V Med 2 SY 21-22No ratings yet
- Circulation During Fetal LifeDocument1 pageCirculation During Fetal LifeHannah Philene D. CalubNo ratings yet
- Fetal DistressDocument3 pagesFetal DistressMaria Donabella OngueNo ratings yet
- Downsyndrome 150808111351 Lva1 App6892Document20 pagesDownsyndrome 150808111351 Lva1 App6892Mohammad Saadullah Khan KakarNo ratings yet
- Breathing Techniques During Labor (Lamaze Method) : Procedure Rationale Rating RemarksDocument4 pagesBreathing Techniques During Labor (Lamaze Method) : Procedure Rationale Rating Remarksadrian lozanoNo ratings yet
- Routine Prenatal CareDocument2 pagesRoutine Prenatal CareRINETTINo ratings yet
- Obstetrics and GynacologyDocument14 pagesObstetrics and GynacologykalkidanNo ratings yet
- Gen BioDocument86 pagesGen BioPaul MagbagoNo ratings yet
- NARRATIVE REPORT PSI JacuDocument9 pagesNARRATIVE REPORT PSI Jaculemar aribalNo ratings yet
- MennaDocument7 pagesMennaDr. Mohammad JamaliNo ratings yet
- Antenatal Assessment of Fetal Well Being: DR - Abdulkarim Ahmed MohamudDocument46 pagesAntenatal Assessment of Fetal Well Being: DR - Abdulkarim Ahmed MohamudPeterNo ratings yet
- Embryology, Types of EggDocument21 pagesEmbryology, Types of EggHoney krishnaNo ratings yet
- JH Cerilles State College Western Mindanao State University: Odessa Bugarin, MNDocument5 pagesJH Cerilles State College Western Mindanao State University: Odessa Bugarin, MNNicole ArandingNo ratings yet
- DMD Skin Sciences - Email Consultation Form (CSM - New Patient) JOSHUA FLORODocument21 pagesDMD Skin Sciences - Email Consultation Form (CSM - New Patient) JOSHUA FLOROJoshua Diaz FloroNo ratings yet
- 1.menstrual CycleDocument7 pages1.menstrual CycleAyenachew AyelikNo ratings yet
- Uterine Therapeutics: by Henry MintonDocument48 pagesUterine Therapeutics: by Henry MintonSravs Pandu100% (1)
- NCM 107 Rle 2Document2 pagesNCM 107 Rle 2Patricia RamosNo ratings yet
- New England Journal Medicine: The ofDocument10 pagesNew England Journal Medicine: The ofSuwandi ChangNo ratings yet
- Lai Wagner For The Womb 2011-1Document5 pagesLai Wagner For The Womb 2011-1Arlene Culagbang GuitguitinNo ratings yet
- Hipothalamus & HipofisisDocument42 pagesHipothalamus & HipofisisONe's IwanNo ratings yet
- Controversies Practice Changers in Ob-GynDocument57 pagesControversies Practice Changers in Ob-GynVirginia AbalosNo ratings yet
- Hormonal Contraceptives in CanadaDocument3 pagesHormonal Contraceptives in CanadaNida Saghir AhmedNo ratings yet
- Be A Voice. Not An EchoDocument13 pagesBe A Voice. Not An EchoJohanna A. DefelesNo ratings yet
- STI - HerpesDocument1 pageSTI - HerpesDanii LuvNo ratings yet