Professional Documents
Culture Documents
AMEP 371201 Adaptations of Clinical Teaching During The Covid 19 Pandemi
Uploaded by
Lasha ChakhvadzeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AMEP 371201 Adaptations of Clinical Teaching During The Covid 19 Pandemi
Uploaded by
Lasha ChakhvadzeCopyright:
Available Formats
Advances in Medical Education and Practice Dovepress
open access to scientific and medical research
Open Access Full Text Article
ORIGINAL RESEARCH
Adaptations of Clinical Teaching During
the COVID-19 Pandemic: Perspectives
Advances in Medical Education and Practice downloaded from https://www.dovepress.com/ on 08-Dec-2022
of Medical Students and Faculty Members
Adla Bakri Hassan 1 , Amgad El-Agroudy 1 , Mohamed Hany Shehata 2,3
, Maryam Abdulla Almoawda 4 ,
Hani Salem Atwa 5,6
1
Department of Internal Medicine, College of Medicine and Medical Sciences, Arabian Gulf University, Manama, Kingdom of Bahrain; 2Department of
Family and Community Medicine, College of Medicine and Medical Sciences, Arabian Gulf University, Manama, Kingdom of Bahrain; 3Department of
Family Medicine, Faculty of Medicine, Helwan University, Cairo, Egypt; 4Medical Intern, Salmaniya Medical Complex, Manama, Kingdom of Bahrain;
5
Department of Medical Education, College of Medicine and Medical Sciences, Arabian Gulf University, Manama, Kingdom of Bahrain; 6Medical
Education Department, Faculty of Medicine, Suez Canal University, Ismailia, Egypt
Correspondence: Hani Salem Atwa, Department of Medical Education, College of Medicine and Medical Sciences, Arabian Gulf University, Manama,
For personal use only.
Kingdom of Bahrain, Tel +973 35635809, Email hanysma@agu.edu.bh; doctorhani2000@yahoo.com
Background: The COVID-19 pandemic had serious implications on medical schools’ programs that necessitated lots of adaptations of
teaching, learning, and assessment to guarantee continuity of education in medical schools. Our study aimed to evaluate perspectives of
clerkship students and faculty members regarding clinical teaching adaptations implemented during the COVID-19 pandemic.
Methods: A descriptive, cross-sectional, survey-based study was conducted and targeted 5th and 6th year clerkship students and full-
and part-time clinical faculty. The survey explored (1) perception of the degree of contribution of implemented adaptations to student
achievement of expected clinical competencies, (2) degree of confidence regarding students’ achievement of expected clinical
competencies through such adaptations, and (3) perception of the effect of implemented educational adaptations on students’ learning.
Descriptive statistics were used, and statistical significance level was set at p < 0.05.
Results: The survey exhibited high internal consistency. Both students and faculty members felt that most of the adaptations had
moderate to high contribution to student achievement of expected clinical competencies. On a 5-point scale, the highest score was
given by faculty members to “Interpretation of investigations” (3.93±0.84) while the lowest scores were given by faculty members
(3.10±1.21) and students (2.57±1.36) to “Performing clinical procedures”. Students and faculty members agreed that the adaptations
had positive effect on students’ learning except for the statement “Students were able to easily monitor their academic progress” where
students gave less scores than faculty members, with a statistically significance difference (p=0.029).
Conclusion: Students and faculty members had similar perspectives regarding the implemented adaptations and their impact and
contribution to student learning and achievement of the basic clinical competencies. Both of them agreed on the need for and
importance of the implemented adaptations. Our findings recommend such adaptations during the times of crises, which can be
conducted through integrating online teaching with face-to-face teaching.
Keywords: COVID-19 pandemic, educational adaptations, medical clerkship
Background
The coronavirus disease 2019 (COVID-19) has rapidly transitioned into a worldwide pandemic. The impact of such
development on medical education was so powerful and unexpected, and led to serious implications and raises countless
questions for the medical schools.1–5 In the current COVID-19 pandemic, some hospitals suspended medical students
from attending clinical rounds. This suspension extended to more hospitals as the COVID-19 pandemic continued to
develop, which led to clinical medical students receiving reduced exposure in different specialties, causing a detrimental
effect to medical students’ performance and competency.6–9
Advances in Medical Education and Practice 2022:13 883–892 883
Received: 17 April 2022 © 2022 Hassan et al. This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.
Accepted: 8 August 2022 php and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License (http://creativecommons.org/licenses/by-nc/3.0/). By accessing the
work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For
Published: 17 August 2022 permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms (https://www.dovepress.com/terms.php).
Hassan et al Dovepress
E-learning satisfaction levels were better among developed countries compared to developing countries. While a USA
study found that overall student performance with respect to generating and researching learning issues was similar
between online and in-person problem based-learning (PBL) sessions,10 another study from Pakistan and KSA found that
the majority of participants agreed that E-learning was satisfactory in acquiring knowledge, however not effective in
acquiring clinical and technical skills and revealed that as the COVID-19 lockdown eases, there will be a need for
improvement in the methods employed in E-learning and more blended learning among healthcare students is
recommended.11 Some adopted new educational system that would be safe and sustainable in the long run.12 In some
medical schools, the medical students seemed to be satisfied and adapted to digitalization, but they also seemed to think
that their teachers would enhance their digital competencies during the pandemic. Therefore, faculties of medicine need
to digitalize their approaches rapidly and adequately to teaching.13
Perspectives of medical students from two countries (Germany and Australia) were found to be different, thus,
differences between countries could reflect cultural differences or variations in the overt and hidden satisfaction of medical
students, hence educational interventions may be needed to improve students’ confidence and sense of competence.14
The situation is more complex for some clerkships or final year medical students who are in the process of sitting their
final assessments. Some medical schools have reduced clinical exposure in the weeks coming up to their final exams to
reduce the risk of contracting the virus.15,16 Others such as United Kingdom, took a different approach and allowed students
exposure and stated that there was a surge in medical student volunteers to support medical staff working on the frontlines.17
As the change to E-learning is increasingly used during the COVID-19 pandemic, the impact of this change on the
medical students at the College of Medicine and Medical Sciences, Arabian Gulf University (CMMS-AGU) is not
known. Our current study aimed to evaluate perceptions of 5th and 6th year medical students and clinical faculty members
towards clinical teaching adaptations implemented by the CMMS-AGU staff during the COVID-19 era.
Materials and Methods
Type of Study
A descriptive, cross-sectional, survey-based study.
Study Setting and Context
This study was conducted at the College of Medicine and Medical Sciences, Arabian Gulf University (CMMS-AGU),
Manama, Bahrain, during the academic year 2020/2021. During the COVID-19 pandemic and imposition of major restrictions
on clinical teaching in hospitals and other training sites, the CMMS-AGU has planned and implemented several adaptations of
clinical teaching that were extensively used to guarantee continuity of training and guarantee that the students are exposed to at
least the minimum clinical experience. Such adaptations included: live online lectures, live case discussion sessions, posting
recorded lectures on Moodle® or OneDrive®, using social medica platforms (eg, WhatsApp® for communication of
information and materials by students and faculty, online team-based learning tutorials, web-based clinical simulated patient
(DxR®), online role playing and discussion of clinical cases, decreasing the number of days students go to hospitals,
decreasing the time students spend inside the ward for bedside teaching, decreasing the number of students in groups of
bedside teaching (≤5), and using the medical simulation center for physical examination and procedural clinical training.
Sampling
Study Population
The study targeted the 5th and 6th year medical clerkship students, in addition to the full- and part-time clinical faculty
who teach those students.
Sample Size
The study used a convenient sample of both clinical faculty members (including both genders, all academic ranks, and all
clinical departments) and medical students (including both genders, different nationalities, and major clerkship rotations). The
total number of faculty members who responded to the survey within the given timeframe (two weeks) was 42 (27%), while
the total number of medical students who responded to the survey within the given timeframe (two weeks) was 97 (22%).
884 https://doi.org/10.2147/AMEP.S371201 Advances in Medical Education and Practice 2022:13
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Hassan et al
Instrument
survey was devised by the researchers according to the steps of a) reviewing the relevant literature and similar studies, b)
development and revision of the form was devised by the researchers according to the steps of a) reviewing the relevant
literature and similar studies, b) development and revision of the survey by all researchers, and c) piloting on a few
students.
The survey was divided into three sections. The first section addressed the implemented educational adaptations and
the perception of faculty members and students of the degree of contribution of such adaptations to student achievement
of the expected clinical competencies. This section adopted a 4-point scale ranging from “Major Contribution” to “No
Contribution”. The second section addressed the expected clinical competencies and the degree of confidence the
respondents had regarding students’ achievement of such competencies. This section adopted a 5-point scale, ranging
from “Highly Confident” to “Highly Unconfident”. The third section addressed the perception of students and faculty
members of the effects of implemented educational adaptations on students’ learning. This section adopted a 5-point
scale, ranging from “Strongly Agree” to “Strongly Disagree”.
Two versions were prepared; one for the faculty members and another for the students.
Suitability of the developed survey for use was assessed through validity and reliability studies. Reliability was
explored through measuring Cronbach’s alpha to assess its internal consistency. Face and content validity were
established through revision by three experts from the Medical Education Unit at the CMMS-AGU, who indicated
a few modifications in the form of linguistic corrections, reformulation of two items, and deletion of an item that had the
same meaning of another item.
Data Collection
The survey form was converted into an electronic format using Google Forms and distributed to the target population
through different communication platforms (like was converted into an electronic format using Google Forms and
distributed to the target population through different communication platforms (like WhatsApp® groups and official
e-mails). Each respondent was given the chance to respond only once. The survey was open for data collection for two
weeks.
Data Analysis
The Statistical Package for the Social Sciences (SPSS) for Windows, version 25 (SPSS Inc., USA) was used for data
analysis. Descriptive statistics were used. Means (and standard deviations) and frequencies were calculated. Parametric
tests have been used, where means were compared for faculty members and medical students through two-sample t-test,
while frequencies were compared through Fisher’s exact test. The calculated probability of less than 5% (p < 0.05) was
considered as the cut-off point for statistical significance.
Ethical Approval
The study was approved by the Research and Ethics Committee (REC) of the College of Medicine and Medical Sciences,
Arabian Gulf University (Approval #: E030-PI-12/20). All participants were given the option of not to respond to the
survey without any consequences. Completion of the survey form was considered as a consent to participate in the study.
Results
Table 1 shows that the internal consistency of the entire survey and its Sections 2 and 3 was excellent (α ≥ 0.9), while
only Section 1 showed an acceptable internal consistency (α = 0.782).
Table 2 shows that most of the faculty respondents were males (64.3%). Faculty came from five clinical departments,
and the majority of them (88.1%) came from Internal Medicine and Surgery Departments. Regarding their academic
ranks, around two-thirds of the faculty (64.3%) were tutors and lecturers, while the remaining one-third were full,
associate, and assistant professors. The majority of the faculty respondents (81%) were part-timers.
Advances in Medical Education and Practice 2022:13 https://doi.org/10.2147/AMEP.S371201
885
DovePress
Powered by TCPDF (www.tcpdf.org)
Hassan et al Dovepress
Table 1 Reliability Study of the Survey
Section No. of Items Cronbach’s Alpha
Section 1: Degree of contribution of different adaptations 11 0.782
Section 2: Degree of confidence in achievement of learning outcomes 8 0.900
Section 3: Perception of the implemented adaptations 10 0.966
Total Survey 29 0.949
Table 2 Demographic Characteristics of Faculty Respondents
Variable No. %
Gender:
Male 27 64.3%
Female 15 35.7%
Total 42 100%
Department:
Internal Medicine 19 45.2%
Surgery 18 42.9%
Pediatrics 3 7.1%
Obstetrics and Gynecology 1 2.4%
Family and Community Medicine 1 2.4%
Total 42 100%
Academic Rank:
Full Professor 4 9.5%
Associate Professor 3 7.1%
Assistant Professor 8 19%
Lecturer 12 28.6%
Tutor 15 35.7%
Total 42 100%
Contract Type:
Full-time 8 19%
Part-time 34 81%
Total 42 100%
Table 3 shows that the majority of the student respondents were females (82.5%). More than half of them (55.7%)
were Bahraini, while the remaining percentage were from other nationalities. The higher percentage of students who
responded to the survey (40.2%) was from Surgery rotation, followed by Internal Medicine (21.6%) and Family and
Community Medicine (20.6%) rotations.
886 https://doi.org/10.2147/AMEP.S371201 Advances in Medical Education and Practice 2022:13
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Hassan et al
Table 3 Demographic Characteristics of Student Respondents
Variable No. %
Gender:
Male 17 17.5%
Female 80 82.5%
Total 97 100%
Nationality:
Bahrain 54 55.7%
Kuwait 23 23.7%
Saudi Arabia 10 10.3%
Oman 7 7.2%
Other Arab Citizens Living in GCC 3 3.1%
Total 97 100%
Clerkship Rotation:
Surgery 39 40.2%
Internal Medicine 21 21.6%
Family and Community Medicine 20 20.6%
Pediatrics 11 11.3%
Obstetrics and Gynecology 6 6.2%
Total 97 100%
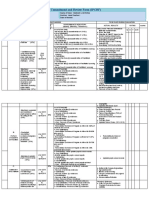
Table 4 shows that both faculty members and students felt that most of the adopted educational adaptations had
moderate to high degree of contribution to student achievement of the expected clinical competencies. There were no
statistically significant differences between faculty members and students regarding their perception of the degree of
contribution of all adaptations except “Online team-based learning tutorials” (p = 0.031) and “Web-based clinical
simulated patient (DxR®)” (p = 0.000), where faculty members were more to the side of moderate to high degree of
contribution.
Table 5 shows moderate mean scores for all items for faculty members and students. The mean scores ranged from
2.57 (±1.36) for students regarding “Performing clinical procedures” to 3.93 (±0.84) for faculty members regarding
“Interpretation of investigations”. The perceptions of faculty members and students regarding the degree of confidence
that the students had achieved the basic clinical competencies through the implemented adaptations were similar for all
explored competencies. There was a statistically significant difference (p = 0.032) between faculty members and students
regarding the “Performing clinical procedures” competence.
Table 6 shows moderate mean scores for all statements for faculty members and students. The mean scores
ranged from 2.91 (±1.22) for students regarding the statement “Students were able to easily monitor their academic
progress” to 3.60 (±0.96) for faculty members regarding the statement “Students had sufficient opportunities to
discuss approaches to clinical cases”. The perceptions of faculty members and students regarding the effects of the
implemented adaptations on the students were nearly similar for all statements. There was a statistically significant
difference (p=0.029) between faculty members and students regarding the statement “Students were able to easily
monitor their academic progress”.
Advances in Medical Education and Practice 2022:13 https://doi.org/10.2147/AMEP.S371201
887
DovePress
Powered by TCPDF (www.tcpdf.org)
Hassan et al Dovepress
Table 4 Degree of Contribution of the Educational Adaptations to Student Achievement of the Expected Clinical Competencies from
the Viewpoints of Faculty Members and Students
No. Adaptations Moderate to High Poor or No Sig.
Contribution Contribution (Fisher’s
Exact Test)
Faculty Students Faculty Students
(n=42) (n=97) (n=42) (n=97)
1 Live online lectures 36 (85.7%) 79 (81.5%) 6 (14.3%) 18 (18.6%) 0.631
2 Live case discussion sessions 36 (85.8%) 83 (85.6%) 6 (14.3%) 14 (14.4%) 1.000
® ®
3 Posting recorded lectures on Moodle or OneDrive 28 (66.7%) 57 (58.8%) 14 (33.3%) 40 (41.3%) 0.450
4 Using social media platforms (eg, WhatsApp®) for 34 (81%) 75 (77.3%) 8 (19.1%) 22 (22.7%) 0.823
communication of information and materials by students and
faculty
5 Online team-based learning tutorials 39 (92.8%) 75 (77.3%) 3 (7.2%) 22 (22.7%) 0.031*
®
6 Web-based clinical simulated patient (DxR ) 34 (80.7%) 37 (38.1%) 8 (19%) 60 (61.8%) 0.000*
7 Online role-playing and discussion of clinical cases 35 (83.4%) 76 (78.3%) 7 (16.6%) 21 (21.6%) 0.646
8 Decreasing the number of days students go to hospital 21 (50%) 33 (34.1%) 21 (50%) 64 (65.9%) 0.089
9 Decreasing the time students spend inside the ward for bedside 22 (52.4%) 43 (44.3%) 20 (47.6%) 54 (55.7%) 0.459
teaching
10 Decreasing the number of students in groups of bedside 37 (88%) 85 (87.6%) 5 (11.9%) 12 (12.4%) 1.000
teaching (≤ 5)
11 Using the medical simulation center for physical examination 36 (85.7%) 93 (95.9%) 6 (14.2%) 4 (4.2%) 0.066
and procedural clinical training
Note: *Statistically significant.
Table 5 Degree of Confidence of Faculty Members and Students Regarding Achievement of the Basic Clinical Competencies Through
the Implemented Adaptations
No. Competencies Faculty (n=42) Students (n=97) Sig. (t-test)
Mean (±SD) Mean (±SD)
1 History taking 3.81 (±0.86) 3.71 (±0.97) 0.572
2 Clinical reasoning 3.69 (±0.87) 3.49 (±1.02) 0.281
3 Conducting physical examination 3.38 (±1.08) 3.21 (±1.15) 0.402
4 Performing clinical procedures 3.10 (±1.21) 2.57 (±1.36) 0.032*
5 Interpretation of investigations 3.93 (±0.84) 3.65 (±0.99) 0.092
6 Management of clinical cases 3.64 (±0.96) 3.47 (±1.05) 0.374
7 Communications skills (with patients and their relatives) 3.52 (±1.19) 3.68 (±1.09) 0.453
8 Health promotion and preventive aspects 3.64 (±0.98) 3.66 (±1.04) 0.929
Note: *Statistically significant.
Discussion
This study aimed to evaluate the perceptions of medical faculty members and clerkship students of the adaptations of
clinical teaching implemented by the CMMS-AGU during the COVID-19 pandemic. Such adaptations were extensively
used during the pandemic as the methods of clinical teaching of the clerkship students.
888 https://doi.org/10.2147/AMEP.S371201 Advances in Medical Education and Practice 2022:13
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Hassan et al
Table 6 Students’ and Faculty Members’ Perception of the Effects of Implemented Educational Adaptations
No. Statements Faculty (n=42) Students (n=97) Sig.
Mean (±SD) Mean (±SD) (t-test)
In adapted clinical teaching/learning,
1 Students were actively engaged 3.45 (±1.25) 3.29 (±1.06) 0.431
2 Students had sufficient opportunities to reflect on what they have learned 3.33 (±1.12) 3.11 (±1.05) 0.268
3 Students were able to achieve several clinical competencies 3.19 (±1.19) 3.18 (±1.11) 0.942
4 There were sufficient opportunities to collaborate with other students 3.26 (±1.11) 3.15 (±1.19) 0.620
5 Students had improved skills in accessing and using information 3.57 (±1.02) 3.38 (±1.16) 0.359
6 Students had sufficient opportunities to discuss approaches to clinical cases 3.60 (±0.96) 3.24 (±1.26) 0.071
7 Students were able to improve their clinical reasoning and approach to 3.52 (±1.06) 3.32 (±1.21) 0.346
common clinical problems
8 Assessment of students’ academic progress was accurate 3.29 (±1.17) 3.14 (±1.20) 0.522
9 Students were able to easily monitor their academic progress 3.38 (±1.03) 2.91 (±1.22) 0.029*
10 Faculty members’ feedback on students’ performance was effective 3.48 (±1.15) 3.15 (±1.28) 0.163
Note: *Statistically significant.
Reliability study showed high internal consistency of the utilized survey (α ≥ 0.9), which gives credibility to the
results.
In this study, both faculty members and students felt that most of the educational adaptations had moderate to high
degree of contribution to the student achievement of the expected competencies, except for “Decreasing the number of
days students go to hospital”, “Decreasing the time students spend inside the ward for bedside teaching”, and using the
“Web-based clinical simulated patient (DxR®)” software, where the students felt that these three adaptations did not
contribute much to the achievement of expected competencies. This might be because the clerkship students prefer longer
stays in clinical placements or simulation center for better learning and they believe that computer-based virtual patients
are not enough. This agrees with the findings of Halbert et al,18 who reported that medical students have chosen to remain
on clinical placements, even though they had concerns about their personal safety. Also, this is congruent with a study
from the same university by Atwa et al,6 who reported that both faculty members and medical students were in favor for
face-to-face and blended learning compared to online learning in the clinical context.
All other adaptations that focused on transforming theoretical teaching and case discussions to the online mode were
considered to have moderate to high degree of contribution. This agrees with Lal et al,19 who reported students’ preference of
using flipped classroom over Zoom to role-play cases with faculty assessing symptoms and disclosing prognosis.
The current study showed an acceptable degree of confidence among both faculty members and students regarding
achievement of the basic clinical competencies through the implemented adaptations. This was true for all competencies
except “Performing clinical procedures”, where there was a statistically significant difference as the students showed
much less confidence regarding achievement of this competence through the implemented adaptations. This agrees with
the results of similar studies that indicated that online learning is not effective in acquiring technical skills and
procedures.6,11,20,21
Medical students and faculty members perceived that the implemented online educational adaptations, in general, had
favorable educational effects on students’ learning. Among the most important effects was keeping the students actively
engaged during online learning activities. This can be explained by the effectiveness of such adaptations in drawing the
attention of the students and also the willingness of the students to achieve the highest benefit and compensate for the
missed face-to-face sessions. Armstrong-Mensah et al22 found that students were still motivated to learn and to complete
their assessments and assignments on time in distance online learning during the COVID-19 pandemic. Also, Atwa et al6
Advances in Medical Education and Practice 2022:13 https://doi.org/10.2147/AMEP.S371201
889
DovePress
Powered by TCPDF (www.tcpdf.org)
Hassan et al Dovepress
reported in their study that most of the students felt actively engaged in online lessons during the pandemic and they
could also collaborate with other students, which was also found in this study. As well, Kumar et al,23 found that
interactivity among students during online sessions could be maintained, as reported by most of the teachers in their
study. Farrell and Brunton24 indicated that active engagement of students in online learning sessions depends in part on
peer community, an engaging online teacher, and student confidence, which were all implied in our implemented
adaptations.
Regarding the learning opportunities students had during the online adaptations, they included discussing clinical
cases, improved clinical reasoning and approach to common clinical problems, reflect on their learning, and achieve
several clinical competencies. Among the adaptations that led to such learning opportunities are the clinical case
discussions, role-playing of clinical cases, using the medical simulation center, and, to a lesser extent, the use of the web-
based clinical simulated patient (DxR®). Furlan et al25 and Kiesewetter et al26 reported that clerkship students can benefit
from similar web-based case discussion software in increasing their clinical reasoning skills, especially during crises
times and impossibility of training on real patients. Furthermore, a scoping review by Park et al27 showed that most
clinical competencies could be learned online or in the virtual setting, which supports the usefulness of our implemented
adaptations.
One of the important effects of the implemented adaptations was the improved skills of the students in accessing and
using information. This is explained by the increased use of technology in learning and searching for information during
online lessons whenever the students need such information. Li and Lee,28 in their study on computer literacy and online
learning attitude, found that students who attended online courses reported higher computer literacy and ability to retrieve
and use information than those who had not done so. They found also that those students are more willing to participate
in further online courses.
The lowest rated effect by the students was in relation to the ability of the students to easily monitor their academic
progress. This might be because the students were feeling detached from the real contact with their school, teachers, and
peers, and were also feeling that online teaching and learning were not well-structured due to the sudden shift to the
online mode. Almendingen et al,29 in their study on student’s experiences with online teaching during COVID-19
lockdown, found that following the academic progress of the students was affected by several factors including lack of
academic contact with their teachers and their peers, lack of social interaction with their peers, and feeling alone in their
studies. Furthermore, Coffey et al30 reported that their students felt anxious and uncertain regarding their education and
academic progress during remote medical education in clerkships during the COVID-19 pandemic.
We believe that this study would add to the medical education literature as it explored the possible important
adaptations that can be implemented in clinical teaching during crises and suspension of or limited access to clinical
training in hospitals and other clinical training sites.
An important limitation of this study was the small sample size. In addition, strengthening the findings with
qualitative data through in-depth interviews or focus group discussions with the students and faculty members would
have added more value to the study.
Conclusion
This study showed that both clerkship students and faculty members have almost similar perspectives of the impact of
implemented educational adaptations, the degree of contribution such adaptations to student achievement of the expected
clinical competencies, as well as the degree of confidence regarding the achievement of the basic clinical competencies.
Clerkship students and faculty members agreed on the need and importance of the implemented educational adaptations.
The current study can be considered as a piece of evidence that the implemented adaptations are recommended and
are quite applicable through integrating online teaching with on campus teaching in the clerkship years of the under
graduate medical curriculum.
Acknowledgments
We would like to thank all the medical students and faculty members who participated in this study. We also would like
to show our deep gratitude to the administration of our institution for the continuous support and care.
890 https://doi.org/10.2147/AMEP.S371201 Advances in Medical Education and Practice 2022:13
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Hassan et al
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design,
execution, acquisition of data, or analysis and interpretation; took part in drafting, revising or critically reviewing the
article; gave final approval of the version to be published; have agreed on the journal to which the article has been
submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Patil NG, Chan Y, Yan H. SARS and its effect on medical education in Hong Kong. Med Educ. 2003;37(12):1127–1128. doi:10.1046/j.1365-
2923.2003.01723.x
2. Chinelatto LA, Costa TRD, Medeiros VMB. What you gain and what you lose in COVID-19: perception of medical students on their education.
Clinics. 2020;75:e2133. doi:10.6061/clinics/2020/e2133
3. Wilcha RJ. Effectiveness of virtual medical teaching during the COVID-19 crisis: systematic review. JMIR Med Educ. 2020;6(2):e20963.
doi:10.2196/20963
4. Findyartini A, Anggraeni D, Husin JM, Greviana N. Exploring medical students’ professional identity formation through written reflections during
the COVID-19 pandemic. J Public Health Res. 2020;9(1_suppl):jphr–2020. doi:10.4081/jphr.2020.1918
5. Alsoufi A, Alsuyihili A, Msherghi A, et al. Impact of the COVID-19 pandemic on medical education: medical students’ knowledge, attitudes, and
practices regarding electronic learning. PLoS One. 2020;15(11):e0242905. doi:10.1371/journal.pone.02429
6. Atwa H, Shehata MH, Al-Ansari A, et al. Online, face-to-face, or blended learning? Faculty and medical students’ perception during the COVID-19
pandemic: a mixed-method study. Front Med. 2022;9:791352. doi:10.3389/fmed.2022.791352
7. Pan D, Rajwani K. Implementation of simulation training during the COVID-19 pandemic: a New York hospital experience. Simul Healthc.
2021;16(1):46. doi:10.1097/SIH.0000000000000535
8. Servin-Rojas M, Olivas-Martinez A, Dithurbide-Hernandez M, et al. Impact of the COVID-19 pandemic on the clinical training of last year medical
students in Mexico: a cross-sectional nationwide study. BMC Med Educ. 2022;22(1):1–8. doi:10.1186/s12909-021-03085-w
9. Dziurka M, Machul M, Ozdoba P, et al. Clinical training during the COVID-19 pandemic: experiences of nursing students and implications for
education. Int J Env Res Public Health. 2022;19(10):6352. doi:10.3390/ijerph19106352
10. Coiado OC, Yodh J, Galvez R, Ahmad K. How COVID-19 transformed problem-based learning at Carle Illinois college of medicine. Med Sci
Educ. 2020;1–2. doi:10.1007/s40670-020-01063-3
11. Abbasi MS, Ahmed N, Sajjad B, et al. E-Learning perception and satisfaction among health sciences students amid the COVID-19 pandemic. Work.
2020;67(3):549–556. doi:10.3233/wor-203308
12. Althwanay A, Ahsan F, Oliveri F, et al. Medical education, pre- and post-pandemic era: a review article. Cureus. 2020;12(10):e10775. doi:10.7759/
cureus.10775
13. Loda T, Löffler T, Erschens R, Zipfel S, Herrmann-Werner A. Medical education in times of COVID-19: German students’ expectations – a cross-
sectional study. PLoS One. 2020;15(11):e0241660. doi:10.1371/journal.pone.0241660
14. Gilligan C, Loda T, Junne F, et al. Medical identity; perspectives of students from two countries. BMC Med Educ. 2020;20(1):420. doi:10.1186/
s12909-020-02351-7
15. Lara S, Foster CW, Hawks M, Montgomery M. Remote assessment of clinical skills during COVID-19: a virtual, high-stakes, summative pediatric
objective structured clinical examination. Acad Pediatr. 2020;20(6):760–761. doi:10.1016/j.acap.2020.05.029
16. Shehata MH, Kumar AP, Arekat MR, et al. A toolbox for conducting an online OSCE. Clin Teach. 2021;18(3):236–242. doi:10.1111/tct.13285
17. Rainbow S, Dorji T. Impact of COVID-19 on medical students in the United Kingdom. Germs. 2020;10(4):240–243. doi:10.18683/
germs.2020.1210
18. Halbert JA, Jones A, Ramsey LP. Clinical placements for medical students in the time of COVID-19. Med J Aust. 2020;213(2):69–69.e1.
doi:10.5694/mja2.50686
19. Lal A, Bell G, Curseen K, Kavalieratos D. Teaching telepalliative care: an elective rotation for medical students during the COVID-19 pandemic.
J Palliat Med. 2021;24(3):318–319. doi:10.1089/jpm.2020.0643
20. Arja SB, Fatteh S, Nandennagari S, Pemma SSK, Ponnusamy K, Arja SB. Is emergency remote (Online) teaching in the first two years of medical
school during the COVID-19 pandemic serving the purpose? Adv Med Educ Pract. 2022;13:199–211. doi:10.2147/AMEP.S352599
21. Wallace D, Sturrock A, Gishen F. “You’ve got mail!”: clinical and practical skills teaching re-imagined during COVID-19. Future Healthc J.
2021;8(1):e50–e53. doi:10.7861/fhj.2020-0231
22. Armstrong-Mensah E, Ramsey-White K, Yankey B, Self-Brown S. COVID-19 and distance learning: effects on Georgia state university school of
public health students. Front Public Health. 2020;8:576227. doi:10.3389/fpubh.2020.576227
23. Kumar AP, Al Ansari AM, Shehata MH, et al. Evaluation of curricular adaptations using digital transformation in a medical school in arabian gulf
during the COVID-19 pandemic. J Microsc Ultrastruct. 2020;8(4):186–192. doi:10.4103/jmau.jmau_87_20
24. Farrell O, Brunton J. A balancing act: a window into online student engagement experiences. Int J Educ Technol High Educ. 2020;17(1):1–9.
doi:10.1186/s41239-020-00199-x
25. Furlan R, Gatti M, Menè R, et al. A natural language processing-based virtual patient simulator and intelligent tutoring system for the clinical
diagnostic process: simulator development and case study. JMIR Med Inform. 2021;9(4):e24073. doi:10.2196/24073
26. Kiesewetter J, Sailer M, Jung VM, et al. Learning clinical reasoning: how virtual patient case format and prior knowledge interact. BMC Med Educ.
2020;20(1):73. doi:10.1186/s12909-020-1987-y
Advances in Medical Education and Practice 2022:13 https://doi.org/10.2147/AMEP.S371201
891
DovePress
Powered by TCPDF (www.tcpdf.org)
Hassan et al Dovepress
27. Park H, Shim S, Lee YM. A scoping review on adaptations of clinical education for medical students during COVID-19. Prim Care Diabetes.
2021;15(6):958–976. doi:10.1016/j.pcd.2021.09.004
28. Li LY, Lee LY. Computer literacy and online learning attitude toward GSOE students in distance education programs. High Educ Stud. 2016;6
(3):147–156. doi:10.5539/hes.v6n3p147
29. Almendingen K, Morseth MS, Gjolstad E, Brevik A, Torris C. Student’s experiences with online teaching following COVID-19 lockdown: a mixed
methods explorative study. PLoS One. 2021;16(8):e0250378. doi:10.1371/journal.pone.0250378
30. Coffey CS, MacDonald BV, Shahrvini B, Baxter SL, Lander L. Student perspectives on remote medical education in clinical core clerkships during
the COVID-19 pandemic. Med Sci Educ. 2020;30(4):1577–1584. doi:10.1007/s40670-020-01114-9
Advances in Medical Education and Practice Dovepress
Publish your work in this journal
Advances in Medical Education and Practice is an international, peer-reviewed, open access journal that aims to present and publish research
on Medical Education covering medical, dental, nursing and allied health care professional education. The journal covers undergraduate
education, postgraduate training and continuing medical education including emerging trends and innovative models linking education,
research, and health care services. The manuscript management system is completely online and includes a very quick and fair peer-review
system. Visit http://www.dovepress.com/testimonials.php to read real quotes from published authors.
Submit your manuscript here: http://www.dovepress.com/advances-in-medical-education-and-practice-journal
892 DovePress Advances in Medical Education and Practice 2022:13
Powered by TCPDF (www.tcpdf.org)
You might also like
- Free Online Business Model Canvas TemplateDocument120 pagesFree Online Business Model Canvas TemplateYahya Rizki100% (2)
- Grade 10 Math Textbook Principles of MathematicsDocument4 pagesGrade 10 Math Textbook Principles of MathematicsDebi0% (2)
- OECD Learning Compass 2030 Concept Note SeriesDocument146 pagesOECD Learning Compass 2030 Concept Note SeriesNguyen Nhu Ngoc NGONo ratings yet
- Selecting and Using Instructional ResourcesDocument23 pagesSelecting and Using Instructional ResourcesMaria Victoria Padro100% (1)
- DLL Empowerment Technologies Week 1Document3 pagesDLL Empowerment Technologies Week 1Brynard Garbosa100% (2)
- The Future of Education and SkillsDocument23 pagesThe Future of Education and SkillsHelena VelezNo ratings yet
- BTECLevel 3 National Engineering Teaching Resource Pack Unit 2Document29 pagesBTECLevel 3 National Engineering Teaching Resource Pack Unit 2princedotty0% (1)
- Academic Cover LettersDocument5 pagesAcademic Cover Letterscoxo_designNo ratings yet
- Emerging Trends in EducationDocument11 pagesEmerging Trends in Educationdanie chasesaNo ratings yet
- Diplomacy Development Security in The Information Age PDFDocument152 pagesDiplomacy Development Security in The Information Age PDFLasha ChakhvadzeNo ratings yet
- List of TrainingsDocument4 pagesList of TrainingsQazi TauseefNo ratings yet
- 11 BEED Teaching Mathematics in The Primary GradesDocument9 pages11 BEED Teaching Mathematics in The Primary Gradesdave puertollanoNo ratings yet
- Alhamad 2023Document10 pagesAlhamad 2023Juan Carlos FloresNo ratings yet
- Amep 6 407Document14 pagesAmep 6 407agung triskoNo ratings yet
- COVID-19 Vaccination Acceptance and Its Associated Factors Among The Iraqi Population: A Cross Sectional StudyDocument13 pagesCOVID-19 Vaccination Acceptance and Its Associated Factors Among The Iraqi Population: A Cross Sectional StudyJijesh NambiarNo ratings yet
- Sources of Stress and Coping Behaviors Among Nursing Students Throughout Their First Clinical TrainingDocument7 pagesSources of Stress and Coping Behaviors Among Nursing Students Throughout Their First Clinical Trainingاحمد العايديNo ratings yet
- Ksu 2017Document7 pagesKsu 2017AHMED HNo ratings yet
- Effect of Dates in Late Pregnancy On The Duration of Labor in Nulliparous WomenDocument5 pagesEffect of Dates in Late Pregnancy On The Duration of Labor in Nulliparous Womendewi lilisNo ratings yet
- Farmaceuticos Instruindo EnfermagemDocument8 pagesFarmaceuticos Instruindo EnfermagemPhilipe VieiraNo ratings yet
- Attitude On Clinical Pharmacy Training: The Case of Haramaya University, EthiopiaDocument8 pagesAttitude On Clinical Pharmacy Training: The Case of Haramaya University, EthiopiaAychluhm TatekNo ratings yet
- Health Nursing DissertationDocument7 pagesHealth Nursing DissertationsamNo ratings yet
- Knowledge and Perception About Epidemiology Among Pharmacy StudentsDocument7 pagesKnowledge and Perception About Epidemiology Among Pharmacy StudentsArwinda NugraheniNo ratings yet
- Educationalinterventiontoimprove GoodDocument8 pagesEducationalinterventiontoimprove Gooderine5995No ratings yet
- Blended Learning' As An Effective Teaching and Learning Strategy in Clinical Medicine: A Comparative Cross-Sectional University-Based StudyDocument6 pagesBlended Learning' As An Effective Teaching and Learning Strategy in Clinical Medicine: A Comparative Cross-Sectional University-Based StudyAnonymous GOUaH7FNo ratings yet
- The Effect of Study Preparation On Test Anxiety AnDocument7 pagesThe Effect of Study Preparation On Test Anxiety AnjuneldelmundoNo ratings yet
- Towards Pharmaceutical Care Services in Saudi Arabia Personal Experience 2376 0419 1 E116Document2 pagesTowards Pharmaceutical Care Services in Saudi Arabia Personal Experience 2376 0419 1 E116Hamad AlshabiNo ratings yet
- Health Science Students Attitude of Using Educational Simulation in SaudiDocument9 pagesHealth Science Students Attitude of Using Educational Simulation in SaudiVictoriano MendezNo ratings yet
- Exploring The Challenges of Clinical EducationDocument8 pagesExploring The Challenges of Clinical EducationVlarah Alondra LiponNo ratings yet
- Amep 208874 Relationship Between Study Habits and Academic Achievement IDocument7 pagesAmep 208874 Relationship Between Study Habits and Academic Achievement IRoyce IbuanNo ratings yet
- Effect of Self-Directed Learning On Nursing Students' Readiness, Perception and Performance in SudanDocument10 pagesEffect of Self-Directed Learning On Nursing Students' Readiness, Perception and Performance in SudanZilbran BerontaxNo ratings yet
- JMedLife 12 075Document9 pagesJMedLife 12 075nurazizahj9No ratings yet
- Analysis of The Third-Grade Curriculum For Health Subjects: Application of Health Education Curriculum Analysis ToolDocument8 pagesAnalysis of The Third-Grade Curriculum For Health Subjects: Application of Health Education Curriculum Analysis ToolBIO FloraNo ratings yet
- A Journey Across An Unwelcoming Field A Qualitative Study Exploring The Factors Influencing Nursing Students Clinical EducationDocument6 pagesA Journey Across An Unwelcoming Field A Qualitative Study Exploring The Factors Influencing Nursing Students Clinical EducationKusrini Kadar SyamsalamNo ratings yet
- Perceptions On Reciprocal Peer Teaching Among Medical StudentsDocument11 pagesPerceptions On Reciprocal Peer Teaching Among Medical StudentsAmmarah OmerNo ratings yet
- Al-Shahrani A M, Miskeen E, (2021)Document7 pagesAl-Shahrani A M, Miskeen E, (2021)Phong Triệu LêNo ratings yet
- Effect of High Fidelity Simulation On Self Satisfaction and Self Confidence Among Nursing StudentsDocument8 pagesEffect of High Fidelity Simulation On Self Satisfaction and Self Confidence Among Nursing Studentsاحمد العايديNo ratings yet
- AUA India Brochure - 2021 - 22Document12 pagesAUA India Brochure - 2021 - 22Bharath ReddyNo ratings yet
- Healthcare SimulationDocument8 pagesHealthcare SimulationcatsdeadnowNo ratings yet
- Smartphone medical app use in clinical training of medical studentsDocument6 pagesSmartphone medical app use in clinical training of medical studentsPicu Arya PrabudiNo ratings yet
- Barriers To Occupational Therapy Fieldwork Education in Iran: The Perspectives of Fieldwork Educators and StudentsDocument6 pagesBarriers To Occupational Therapy Fieldwork Education in Iran: The Perspectives of Fieldwork Educators and StudentsNataliaNo ratings yet
- Study Habits of Highly Effective Medical StudentsDocument7 pagesStudy Habits of Highly Effective Medical StudentscastillojessNo ratings yet
- Amep 259557 Perceived Stress Among Iranian Nursing Students in A ClinicaDocument7 pagesAmep 259557 Perceived Stress Among Iranian Nursing Students in A ClinicaMarianne CoracheaNo ratings yet
- Ijgm 13 77Document12 pagesIjgm 13 77DⒶrk OtⒶkuNo ratings yet
- CoursesDocument2 pagesCoursesapi-586042393No ratings yet
- Identifikasi Tantangan Ke Babak Klinis Yang Baik Studi Kelompok Terarah Guru MedisDocument12 pagesIdentifikasi Tantangan Ke Babak Klinis Yang Baik Studi Kelompok Terarah Guru MedisMarisaNo ratings yet
- Community Medicine Study GuideDocument78 pagesCommunity Medicine Study GuideNasir HussainNo ratings yet
- Perceptions of Pharmacy and Other Health Professional Students Toward Interprofessional EducationDocument8 pagesPerceptions of Pharmacy and Other Health Professional Students Toward Interprofessional EducationLitera HusadaNo ratings yet
- Faktor 2 QCDocument13 pagesFaktor 2 QCwi bowoNo ratings yet
- 1 s2.0 S2452301116300700 Main 1Document11 pages1 s2.0 S2452301116300700 Main 1uiolNo ratings yet
- Hanfesa, 2020Document8 pagesHanfesa, 2020nurrahmasia raraNo ratings yet
- Ijwh-14-517 TiruyeDocument11 pagesIjwh-14-517 TiruyeDaraaswanNo ratings yet
- Health Literacy Pada InfluenzaDocument8 pagesHealth Literacy Pada Influenzahairun hairunNo ratings yet
- Hamza ThesisDocument45 pagesHamza ThesisShanoo AmeerNo ratings yet
- The Evaluation of The Learning by Clinical Reasoning Among Students of 3RD Year of Medicine - Faculty of Medicine and Pharmacy of MarrakeshDocument6 pagesThe Evaluation of The Learning by Clinical Reasoning Among Students of 3RD Year of Medicine - Faculty of Medicine and Pharmacy of MarrakeshIJAR JOURNALNo ratings yet
- Perspective of Postgraduate Medical Students on the need for Foundation Course After the Admission in Postgraduate Medical CollegeDocument3 pagesPerspective of Postgraduate Medical Students on the need for Foundation Course After the Admission in Postgraduate Medical CollegeBIOMEDSCIDIRECT PUBLICATIONSNo ratings yet
- The Mental Health of Healthcare Workers in The COVID-19 Pandemic: A Systematic ReviewDocument12 pagesThe Mental Health of Healthcare Workers in The COVID-19 Pandemic: A Systematic ReviewAnjas Berlyanta Fitra RamadhaniNo ratings yet
- QU Bulletin 2012 - Health Colleges-Final PDFDocument371 pagesQU Bulletin 2012 - Health Colleges-Final PDFomarNo ratings yet
- Assessment of Educational Environment For Interns Using Postgraduate Hospital Educational Environment Measure (PHEEM)Document12 pagesAssessment of Educational Environment For Interns Using Postgraduate Hospital Educational Environment Measure (PHEEM)Maryam AzizNo ratings yet
- Content ServerDocument10 pagesContent ServersyarifaNo ratings yet
- Pharm D-2023-24 - 301123Document63 pagesPharm D-2023-24 - 301123quratulainansari839No ratings yet
- Medical Student Performance Evaluation For جيرخلا مسا ماعلاريدقتلا / وينوي) وأ (ربمسيد ةعفدلاDocument6 pagesMedical Student Performance Evaluation For جيرخلا مسا ماعلاريدقتلا / وينوي) وأ (ربمسيد ةعفدلاeolhc rezarfNo ratings yet
- Padilla - The Lived Experience of Nurses Caring For Patients With COVID-19 in Iran: A Phenomenological StudyDocument8 pagesPadilla - The Lived Experience of Nurses Caring For Patients With COVID-19 in Iran: A Phenomenological StudyNicole PadillaNo ratings yet
- The Effect of Patient Safety Education On Undergraduate Nursing Students Patient Safety CompetenciesDocument6 pagesThe Effect of Patient Safety Education On Undergraduate Nursing Students Patient Safety CompetenciesRandom HNo ratings yet
- Anxiety and Its Association WiDocument12 pagesAnxiety and Its Association WiWiyar HoldingNo ratings yet
- AUA India Brochure 2022 23Document12 pagesAUA India Brochure 2022 23Salim NooriNo ratings yet
- Impact of Students Useof Technologyon TheirlearningachievementsDocument5 pagesImpact of Students Useof Technologyon TheirlearningachievementsLee-Ann LimNo ratings yet
- College of Pharmacy OverviewDocument21 pagesCollege of Pharmacy OverviewTuấn HuỳnhNo ratings yet
- RCSI Bahrain Develops Healthcare LeadersDocument22 pagesRCSI Bahrain Develops Healthcare LeadersIoana GusatuNo ratings yet
- Medical Student Syndrome Bjmp-2019-12-1-A003: British Journal of Medical Practitioners January 2019Document6 pagesMedical Student Syndrome Bjmp-2019-12-1-A003: British Journal of Medical Practitioners January 2019Nabila AjmaliaNo ratings yet
- Jeehp 17 08 PDFDocument9 pagesJeehp 17 08 PDFEllismarNo ratings yet
- Pharmacist with experience in hospitals and community pharmaciesDocument1 pagePharmacist with experience in hospitals and community pharmaciesoalnatour osama al-natourNo ratings yet
- Comprehensive Healthcare Simulation: Mastery Learning in Health Professions EducationFrom EverandComprehensive Healthcare Simulation: Mastery Learning in Health Professions EducationNo ratings yet
- SoMEP 2020 - PDF 84684244Document174 pagesSoMEP 2020 - PDF 84684244Lasha ChakhvadzeNo ratings yet
- MSAR Application Transfer Policies 07.13.23Document11 pagesMSAR Application Transfer Policies 07.13.23Lasha ChakhvadzeNo ratings yet
- Cureus 0014 00000024280Document7 pagesCureus 0014 00000024280Lasha ChakhvadzeNo ratings yet
- UoS Student Transfer PolicyDocument3 pagesUoS Student Transfer PolicyLasha ChakhvadzeNo ratings yet
- Ime 01 00004Document5 pagesIme 01 00004Lasha ChakhvadzeNo ratings yet
- View of Experiences of A London Medical Student in The COVID-19 Pandemic - International Journal of Medical StudentsDocument2 pagesView of Experiences of A London Medical Student in The COVID-19 Pandemic - International Journal of Medical StudentsLasha ChakhvadzeNo ratings yet
- UK Medical Schools Come Together To Respond To The Coronavirus Pandemic - Medical Schools CouncilDocument5 pagesUK Medical Schools Come Together To Respond To The Coronavirus Pandemic - Medical Schools CouncilLasha ChakhvadzeNo ratings yet
- Entry Requirements Document 2022 DigitalDocument90 pagesEntry Requirements Document 2022 DigitalLasha ChakhvadzeNo ratings yet
- Acc 57 736Document8 pagesAcc 57 736Lasha ChakhvadzeNo ratings yet
- OECD Report 69096873-EnDocument476 pagesOECD Report 69096873-EnMuratHan588No ratings yet
- Covid 19 Initial Guidance For ProvidersDocument11 pagesCovid 19 Initial Guidance For ProvidersLasha ChakhvadzeNo ratings yet
- OECD Work Education Skills Policy Products Services For CountriesDocument9 pagesOECD Work Education Skills Policy Products Services For CountriesClaudia TeoodorescuNo ratings yet
- Folkneri. DatviDocument55 pagesFolkneri. DatviLasha ChakhvadzeNo ratings yet
- Bbeca162 enDocument384 pagesBbeca162 enLasha ChakhvadzeNo ratings yet
- Gsas Cvs and Cover LettersDocument31 pagesGsas Cvs and Cover LettersSardar Haroon KhanNo ratings yet
- Expo Ida (2015) 549050 enDocument24 pagesExpo Ida (2015) 549050 enLasha ChakhvadzeNo ratings yet
- Theatre Articles in GeorgianDocument12 pagesTheatre Articles in GeorgianLasha ChakhvadzeNo ratings yet
- OECD Future of Education and Skills 2030: Conceptual Learning FrameworkDocument15 pagesOECD Future of Education and Skills 2030: Conceptual Learning Framework4nn1shNo ratings yet
- Rules For The Evaluation of Academic B.A and M.A Degrees Awarded by Foreign Institutions of Higher Education (The Rachlevsky Rules)Document7 pagesRules For The Evaluation of Academic B.A and M.A Degrees Awarded by Foreign Institutions of Higher Education (The Rachlevsky Rules)Lasha ChakhvadzeNo ratings yet
- Education Diplomacy Brief: The New Era of Global Education GovernanceDocument5 pagesEducation Diplomacy Brief: The New Era of Global Education GovernanceLasha ChakhvadzeNo ratings yet
- Aacrao 2015 Annual MeetingDocument12 pagesAacrao 2015 Annual MeetingLasha ChakhvadzeNo ratings yet
- Cremonini, Epping, Westerheijden C12DW012 Publicatie Inqaahe - Case - Study - Report-Final-0201Document36 pagesCremonini, Epping, Westerheijden C12DW012 Publicatie Inqaahe - Case - Study - Report-Final-0201Lasha ChakhvadzeNo ratings yet
- EU Higher Education As Soft Power in Neighbouring Countries: A Projection of Influence by Compelling MeansDocument28 pagesEU Higher Education As Soft Power in Neighbouring Countries: A Projection of Influence by Compelling MeansLasha ChakhvadzeNo ratings yet
- Final Report 28-7-09Document46 pagesFinal Report 28-7-09Lasha ChakhvadzeNo ratings yet
- Education - The Neglected Tool of Indian DiplomacyDocument15 pagesEducation - The Neglected Tool of Indian DiplomacyLasha ChakhvadzeNo ratings yet
- Part 3Document19 pagesPart 3jayrald cruzada100% (2)
- Chapter 2Document8 pagesChapter 2Zyrome Jen HarderNo ratings yet
- 2014 Annual ReportDocument95 pages2014 Annual ReportMithunNo ratings yet
- GE 5 Module 2Document12 pagesGE 5 Module 2Glenda RadasaNo ratings yet
- Use of Information and Communication Technologies As A Medium For Education in AlbaniaDocument7 pagesUse of Information and Communication Technologies As A Medium For Education in AlbaniapferradaNo ratings yet
- Position Paper Teaching and Learning With TechnologyDocument3 pagesPosition Paper Teaching and Learning With Technologyapi-29566828783% (6)
- Chapter 5 VR, AR and MRDocument22 pagesChapter 5 VR, AR and MRZerihun BekeleNo ratings yet
- Synopsys: This Chapter Is Devoted To The Issues of Changing TheDocument12 pagesSynopsys: This Chapter Is Devoted To The Issues of Changing TheKhushi JoshiNo ratings yet
- Lily Forward Planning Document 2Document2 pagesLily Forward Planning Document 2api-250171106No ratings yet
- Dissertation: A Grounded Theory of Trauma-Informed Online LearningDocument4 pagesDissertation: A Grounded Theory of Trauma-Informed Online LearningSuzanne ReinhardtNo ratings yet
- ASCC R&D Platforms (Future of Education) Regional Online Forum - Concept Note For Participants - BLDocument5 pagesASCC R&D Platforms (Future of Education) Regional Online Forum - Concept Note For Participants - BLVictor LabotanoNo ratings yet
- WHTC Curriculum For Website 2018 19Document43 pagesWHTC Curriculum For Website 2018 19Mychannel Mdx BrentNo ratings yet
- Students embrace online learning despite challenges of MCODocument3 pagesStudents embrace online learning despite challenges of MCOFardiana EdrinaNo ratings yet
- Frustrated Pupils 'Bored by Their Factory Schools': NB You May Use Any Letter More Than OnceDocument1 pageFrustrated Pupils 'Bored by Their Factory Schools': NB You May Use Any Letter More Than OncePhạm ThắngNo ratings yet
- Evaluating Impact: Turning Promises Into EvidenceDocument16 pagesEvaluating Impact: Turning Promises Into Evidenceakyadav123No ratings yet
- CBT Presentation TM1Document7 pagesCBT Presentation TM1Bong Bayron Encarnacion Jr.No ratings yet
- The Introduction To E Learning Education Essay: Research Question/AimDocument6 pagesThe Introduction To E Learning Education Essay: Research Question/AimAsad RazaNo ratings yet
- Edukasyong Pantahanan at Pangkabuhayan: Florencia S.MiñasDocument109 pagesEdukasyong Pantahanan at Pangkabuhayan: Florencia S.Miñasmarivicgrimpula3124No ratings yet
- A Study On The Effectiveness of Online Teaching in Pharmacy Education From Teacher and Student Perspectives During The COVID-19 PandemicDocument5 pagesA Study On The Effectiveness of Online Teaching in Pharmacy Education From Teacher and Student Perspectives During The COVID-19 PandemicAbbyNo ratings yet
- IPCRF Performance Review SummaryDocument4 pagesIPCRF Performance Review SummaryDolly UcagNo ratings yet
- The Quest For Critical Thinking Framework in ELT Hamzah Puadi IlyasDocument24 pagesThe Quest For Critical Thinking Framework in ELT Hamzah Puadi IlyasBERNARD RICHARD NAINGGOLANNo ratings yet
- Probation Report 2015 s1Document6 pagesProbation Report 2015 s1api-296874431No ratings yet