Professional Documents
Culture Documents
Parathyroid Gland Anatomy and Function
Uploaded by
Ella OrtegaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Parathyroid Gland Anatomy and Function
Uploaded by
Ella OrtegaCopyright:
Available Formats
1 MLS 418 - LECTURE 2ND SEMESTER | S.Y.
2021-2022
PARATHYROID GLAND PARATHYROID HORMONE
ANATOMY AND HISTOLOGY • Function: Increase serum calcium
• the parathyroid gland is located posteriorly to the • Secreted by parathyroid glands (chief cells)
thyroid gland ▪ rapid response to reduced calcium
• flattened and oval in shape situated external to the (minutes)
thyroid gland but within the pre-tracheal fascia • Polypeptide
• most individuals have four (4) parathyroid glands but ▪ 84 amino acid residues (9,500 Da)
variation in number may occur (some have 2 or 6) • Operates in tissues via the cAMP second messenger
• superior thyroid artery - supply blood for superior • Net effect: increased total/ionized calcium
parathyroid gland ▪ Negative feedback: lowers PTH secretion
• inferior thyroid artery – supply blood for inferior
parathyroid gland
REGULATION
• Happens in the parathyroid cell
• Calcium binds to a receptor (calcium-sensing
receptor) coupled to a G protein
▪ activation of phospholipase C (PLC)
• PLC converts phosphoinositides to inositol
triphosphate (IP3) and diacylglycerol (DAG)
• IP3 - releases calcium from internal stores
• DAG - stimulates protein kinase C (PKC) activation
▪ Calcium/PKC: inhibited PTH release and
synthesis
• Follicles – circular part with colloid inside
• INCREASED SERUM CALCIUM:
o Increased serum calcium will result in
negative feedback to bring lower the calcium
levels
o Calcium binds to the calcium-sensor receptor,
coupled with G protein
o The complex will activate phospholipase C to
• Parathyroid gland is composed of two cells:
inhibit the parathyroid hormone secretion
o Chief cells - responsible for the production
• DECREASED SERUM CALCIUM:
of parathyroid hormone
o Low level of calcium will not attach to the
o Oxyphil cells - responsible for the
calcium-sensor receptor, which will remain
production of PTH-RP or parathyroid
inactivated
hormone-related protein
o Therefore, parathyroid hormone secretion
will be stimulated
BSMLS 3I - Page | 1
• Conclusion: smaller peptides are released in the
o Calcium-sensor activation will result in circulation.
parathyroid inhibition • PTH-related peptide (PTH-rP)
o Calcium-sensor inactivation will result in o produced by tumors
o parathyroid stimulation ▪ lung, breast, kidney, and other
solid tissues
• Effects of PTH: (increase Ca2+) o 141 AA (shares the same homology with
o increase in kidney calcium resorption PTH in the first 13 AA)
o increase in bone calcium resorption o same PTH receptor/functions (increase
o increase vitamin D secretion in kidney serum calcium)
▪ results in gut calcium absorption o present in patients with malignancy-
associated hypercalcemia
FUNCTIONS DISEASES
HYPERCALCEMIA
• Increased serum calcium
• Common causes:
o Hyperparathyroidism
o Malignancy-associated: PTH-rp
o Vitamin D intoxication
o Hypercalcemia in granulomatous disorders
o Milk-alkali syndrome/Burnett syndrome
PRIMARY HYPERPARATHYROIDISM
• Primary: the organ that produces the hormone has
the problem
• The problem is within the parathyroid gland
• Excessive secretion of PTH with no stimulus and no
response to negative feedback
• Caused by: parathyroid adenoma, hyperplasia,
carcinoma
• Increased calcium (high risk of heart problems,
atherosclerosis, osteoporosis, kidney stones)
o Calcium will be lodged or stored in your
coronary arteries or in your blood vessels.
o Increased osteoclastic activity
o Calcium may be stored in your kidneys
• Bone • Hereditary factors (complex endocrine tumor)
o osteoblast stimulation to produce RANKL* o Combination with other carcinoma of the
which will activate RANK in osteoclasts body!
o (end point: increased bone resorption and o Multiple endocrine neoplasia type 1: (PPP)
increased calcium/osteoporosis risk) ▪ parathyroid, pituitary, pancreas
▪ There will be osteoclastic activity; tumors
where our bone loses Calcium o Multiple endocrine neoplasia type 2A:
towards the blood (TPH)
o RANKL: receptor activator of nuclear factor ▪ thyroid cancer,
ĸB ligand pheochromocytoma (adrenal
o When PTH is stimulated PTH will be gland), hyperparathyroidism
released to the blood and will have a target (parathyroid)
tissue in your bone. In your bone your PTH
stimulates osteoclastic activity bone is OTHER CAUSES OF HYPERCALCEMIA
resorbed which releases calcium in the VITAMIN D INTOXICATION
bloodstream. • Increased calcium absorption in the intestines,
o Increases serum calcium increased bone resorption
• Kidneys
o increased urine excretion of phosphates, HYPERCALCEMIA IN GRANULOMATOUS DISORDERS
calcium reabsorption in the nephron, • Sarcoidosis patients
vitamin D activation o Sacroidosis = an inflammatory disorder that
o Decreases serum phosphate affects multiple organs in the body; px will
have a severe respiratory distress because
PTH LABORATORY METHODS of inflammation in lung parenchyma
• Measurement of intact PTH (using 2 antibodies that o Most common affected organ: lungs and
measure the N-terminal and C-terminal) other organ system
o Using ELISA • Unregulated generation of vitamin D in
o Intact parathyroid hormone is biologically granulomatous tissues
active in its form, however the half-life of o Producing increased amount of vitamin D =
intact parathyroid hormone is only less than hypercalcemia
4-minutes.
o The kidneys and liver will clear the intact MILK-ALKALI SYNDROME
parathyroid hormone rapidly and it will be • In peptic ulcer patients
cleaved into different fragments, and these
LABAN RMT! - Page | 2
• Increased calcium absorption/absorbable alkali • Cardiac anomaly, abnormal facial feature / fasci
(antacids/calcium carbonate) (hooded eyes, relatively long face, small and low-set
o Calcium carbonate is very rampant ears), thymic hypoplasia (px prone to infection), cleft
nowadays because some patients will take palate, hypocalcemia,
this as prophylaxis for osteoporosis • DiGeorge syndrome, also known as 22q11.2 deletion
o Taking too much calcium carbonate or syndrome, is a syndrome caused by the deletion of a
antacids from peptic ulcer disease will cause small segment of chromosome 22.
Milk-alkali syndrome • Common in young individual who have recurrent
• Can be a manifestation of hypercalcemia, infection
hypocalciuria, alkalosis, azotemia, and soft tissue
calcification PSEUDOHYPOPARATHYROIDISM
• aka Albright hereditary osteodystrophy
• genetic disorder where the body fails to respond to
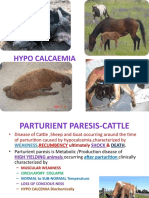
HYPOCALCEMIA PTH
• Causes: o Parathyroid hormone resistancy
o Decreased PTH production/secretion o Body do not respond to PTH
o Resistance to PTH action • low blood calcium and high phosphate levels
▪ You have a normal level of • characteristics:
parathyroid hormone. However, o short height
our body failed to response to the o short hand bones (bone below the 4th
parathyroid hormone itself finger)
o Deficiency of vitamin D
HYPOPARATHYROIDISM
• Diminished or absent PTH production
• Acquired: neck surgeries/thyroidectomy
o Thyroidectomy: removal of thyroid either
partial or total (entire gland is being
removed)
• Parathyroid gland is situated posterior to thyroid
gland so there is a big chance that your parathyroid
gland can also be transected or can be damaged
during the procedure. That is why patient may take
Calcium supplements after thyroidectomy
• Inherited:
o Defective thymus and parathyroid gland
(DiGeorge syndrome) CATCH 22
o Hereditary autoimmune syndrome:
autoimmune polyglandular deficiency
DiGeorge syndrome is a combination of:
• Cardiac anomaly
o Px may manifest with cardiac problem or
murmur
• Abnormal facial feature or Abnormal fascia
• Thymic hypoplasia
o Px has hypoplastic thymus = poor
differentiation of T cells
o T cells are differentiated in thymus gland
o Without T cells, px may have severe
infection or recurrent infection
• Cleft palate
• Hypocalcemia
o Because of defective parathyroid gland
• Chromosome 22
o Since it is inherited, chromosome 22 is
affected
LABAN RMT! - Page | 3
You might also like
- Pediatric Endocrinology Part 2: Pediatrics 2Document8 pagesPediatric Endocrinology Part 2: Pediatrics 2sarguss14No ratings yet
- VPHY 143 Parathyroid To ThyroidDocument3 pagesVPHY 143 Parathyroid To ThyroidRegulus Fidelis SevillaNo ratings yet
- Calcium MetabolismDocument51 pagesCalcium MetabolismAlan ThomasNo ratings yet
- Calcium Homeostasis HormonesDocument31 pagesCalcium Homeostasis HormonesNoval FebriNo ratings yet
- Calcium Metabolism and Disorders (Hanan)Document169 pagesCalcium Metabolism and Disorders (Hanan)drhananfathyNo ratings yet
- 287 FullDocument4 pages287 FullRye CalderonNo ratings yet
- BMD and DialysisDocument30 pagesBMD and DialysisThe AbyssinicansNo ratings yet
- Parathyroid: Calcium and Vitamin DDocument135 pagesParathyroid: Calcium and Vitamin DPhysiology by Dr RaghuveerNo ratings yet
- PTH Regulation and Hyperparathyroidism GuideDocument39 pagesPTH Regulation and Hyperparathyroidism GuideAris josuaNo ratings yet
- Parathyroid Hormone and Calcium Regulation: By: Abebe TDocument29 pagesParathyroid Hormone and Calcium Regulation: By: Abebe TLidiya TeshomeNo ratings yet
- Parathyroid Hormone PDFDocument120 pagesParathyroid Hormone PDFLaura TapiaNo ratings yet
- Parathormone, CalcitoninDocument14 pagesParathormone, CalcitoninIbrahimNo ratings yet
- Endo Lect - ParathyroidDocument25 pagesEndo Lect - ParathyroiddoctorrfarrukhNo ratings yet
- Calcium and Phosphate MetabolismDocument27 pagesCalcium and Phosphate MetabolismIshaqNo ratings yet
- Hormon Parathyroid: Dr. Nanang Miftah F, SPPDDocument13 pagesHormon Parathyroid: Dr. Nanang Miftah F, SPPDFitri Nur DiniNo ratings yet
- Parathyroid Gland: Clinical Chemistry - 3Document16 pagesParathyroid Gland: Clinical Chemistry - 3Mary Rose BarrigaNo ratings yet
- MacroMinerals: Calcium, Phosphorus, Potassium, Sodium, Chloride, and MagnesiumDocument9 pagesMacroMinerals: Calcium, Phosphorus, Potassium, Sodium, Chloride, and MagnesiumDerek AtienzaNo ratings yet
- Endocrinology Contd IDocument3 pagesEndocrinology Contd IMaybelle Acap PatnubayNo ratings yet
- Hypercalcemia in Dogs Emergent Care Diagnostics and TreatmentsDocument8 pagesHypercalcemia in Dogs Emergent Care Diagnostics and Treatmentstarilubis277No ratings yet
- Drugs Affecting Calcium Balance: Harsh Vinayak Roll No. 39 Mbbs 2 Yr Student BATCH 2019 Rdasmc, AyodhyaDocument24 pagesDrugs Affecting Calcium Balance: Harsh Vinayak Roll No. 39 Mbbs 2 Yr Student BATCH 2019 Rdasmc, AyodhyaA2Z GyanNo ratings yet
- Calcium, Phosphate and MagnesiumDocument46 pagesCalcium, Phosphate and Magnesiumkiedd_04100% (3)
- Hyper PTHDocument46 pagesHyper PTHJulian TaneNo ratings yet
- Lect 9 Parathyroid Gland-1Document30 pagesLect 9 Parathyroid Gland-1warda farooqNo ratings yet
- Parathyroid HormoneDocument120 pagesParathyroid HormoneLaura TapiaNo ratings yet
- Calcium and PhosphateDocument35 pagesCalcium and PhosphateSULEIMAN OMARNo ratings yet
- Calcium Metabolism & Calcium Metabolism DisordersDocument45 pagesCalcium Metabolism & Calcium Metabolism Disorderstrisya arthaputriNo ratings yet
- Share Market Report 6Document13 pagesShare Market Report 6Nithish DevadigaNo ratings yet
- Cc2 l7 Other GlandsDocument2 pagesCc2 l7 Other GlandsRose Denisse EstrellaNo ratings yet
- Parathyroid DisordersDocument37 pagesParathyroid DisordersMannat ZaidiNo ratings yet
- Parathyroid Hormone: DR Pramod Kumar Asstt. Professor Department of Veterinary Physiology Bihar Veterinary College, PatnaDocument19 pagesParathyroid Hormone: DR Pramod Kumar Asstt. Professor Department of Veterinary Physiology Bihar Veterinary College, PatnasanathNo ratings yet
- Calcium and PhosphorusDocument34 pagesCalcium and Phosphorus075 Keerthighaa SNo ratings yet
- Study Guide For Calcium and Phosphate MetabolismDocument74 pagesStudy Guide For Calcium and Phosphate MetabolismMohammad MamunuzzamanNo ratings yet
- Calcium & Phosphorus Metabolism: Regulation of Levels, Absorption & FunctionsDocument90 pagesCalcium & Phosphorus Metabolism: Regulation of Levels, Absorption & FunctionsSriya Saatwika ReddyNo ratings yet
- Calcium, Phosphate and Vitamin D MetabolismDocument25 pagesCalcium, Phosphate and Vitamin D MetabolismRendy LectusNo ratings yet
- Parathyroid Hormone: Shahab Ullah Khan Ayub Medical CollegeDocument28 pagesParathyroid Hormone: Shahab Ullah Khan Ayub Medical CollegeDr KhanNo ratings yet
- Calcium and PhosphateDocument49 pagesCalcium and Phosphatehaidernadhem57No ratings yet
- Calcium & Phosphate MetabolismDocument36 pagesCalcium & Phosphate MetabolismMustafa KhandgawiNo ratings yet
- NotesDocument1 pageNotesGerard JameroNo ratings yet
- Bone Markers - FinalDocument79 pagesBone Markers - FinalSparrowNo ratings yet
- chronic kidney disease bmdDocument2 pageschronic kidney disease bmdapi-734449276No ratings yet
- MineralsDocument22 pagesMineralsLovely Pardilla TorillaNo ratings yet
- Men1, Gi Endo Cam304 2019 J.burgessDocument27 pagesMen1, Gi Endo Cam304 2019 J.burgessJeffrey XieNo ratings yet
- Minerals c 4Document40 pagesMinerals c 4Jasmine sindhooNo ratings yet
- ParathyroidDocument2 pagesParathyroiddhaineyNo ratings yet
- Calcium MetabolismDocument19 pagesCalcium MetabolismShabariNath R NairNo ratings yet
- Disorders of Calcium, Inorganic Phosphate and Magnesium Metabolism 1Document62 pagesDisorders of Calcium, Inorganic Phosphate and Magnesium Metabolism 1IiiNo ratings yet
- Calcium Homeostasis HormonesDocument8 pagesCalcium Homeostasis HormonesRoua SafwatNo ratings yet
- Biochemical Markers of Bone Metabolism PPT LectureDocument89 pagesBiochemical Markers of Bone Metabolism PPT LectureNeil Vincent De AsisNo ratings yet
- Milk FeverDocument78 pagesMilk FeverAsif AliNo ratings yet
- CalciumDocument77 pagesCalciumRhaffy RapaconNo ratings yet
- Endocrine Part 2 DRAFTDocument6 pagesEndocrine Part 2 DRAFTPreeti Joan BuxaniNo ratings yet
- Breast Milk BiochemistryDocument6 pagesBreast Milk Biochemistry365 DaysNo ratings yet
- Ca Phosphate MetaDocument77 pagesCa Phosphate MetanivethaseshaNo ratings yet
- Hormones of Parathyroid and Regulation of Blood Calcium LevelDocument9 pagesHormones of Parathyroid and Regulation of Blood Calcium Levelriskyy1No ratings yet
- Feedback Mechanism ActivityDocument9 pagesFeedback Mechanism ActivityRohan BhatiaNo ratings yet
- 06-Calcium Phosphate Metabolism-NewDocument16 pages06-Calcium Phosphate Metabolism-NewBassimkhalil AbdallahNo ratings yet
- Calcium HomeostasisDocument10 pagesCalcium Homeostasiszsf8m52ky4No ratings yet
- A Simple Guide to Hyperparathyroidism, Treatment and Related DiseasesFrom EverandA Simple Guide to Hyperparathyroidism, Treatment and Related DiseasesNo ratings yet
- Fast Facts: Deficit di piruvato chinasi per pazienti e sostenitori: Una rara malattia genetica che colpisce I globuli rossi Informazioni + assunzione del controllo = migliore risultatoFrom EverandFast Facts: Deficit di piruvato chinasi per pazienti e sostenitori: Una rara malattia genetica che colpisce I globuli rossi Informazioni + assunzione del controllo = migliore risultatoNo ratings yet
- Hema Quiz RatioDocument20 pagesHema Quiz RatioElla OrtegaNo ratings yet
- Quizzes RationaleDocument22 pagesQuizzes RationaleElla OrtegaNo ratings yet
- Errors and The CBC Result 2.0Document43 pagesErrors and The CBC Result 2.0Ella OrtegaNo ratings yet
- Histo QuizDocument1 pageHisto QuizElla OrtegaNo ratings yet
- Microscopic Analysis of Urine SedimentsDocument21 pagesMicroscopic Analysis of Urine SedimentsElla OrtegaNo ratings yet
- Antihuman Globulin TestsDocument6 pagesAntihuman Globulin TestsElla OrtegaNo ratings yet
- Chloride, Bicarbonate and LactateDocument25 pagesChloride, Bicarbonate and LactateElla OrtegaNo ratings yet
- Chloride, Bicarbonate and LactateDocument32 pagesChloride, Bicarbonate and LactateElla OrtegaNo ratings yet
- 2.2 - Weak D AntigenDocument3 pages2.2 - Weak D AntigenElla OrtegaNo ratings yet
- Cleft Lip and Cleft PalateDocument16 pagesCleft Lip and Cleft Palatemacuka08100% (3)
- 18 - OET Online Test 4Document22 pages18 - OET Online Test 4DHARA MODI100% (1)
- Gambling Addiction PowerpointDocument11 pagesGambling Addiction PowerpointEK200620No ratings yet
- Subarachnoid Hemorrhage With AneurysymDocument30 pagesSubarachnoid Hemorrhage With AneurysymmunaNo ratings yet
- Trường Đại Học Y Khoa Phạm Ngọc Thạch: Name: ClassDocument45 pagesTrường Đại Học Y Khoa Phạm Ngọc Thạch: Name: ClassĐoàn Tuấn KhôiNo ratings yet
- ND PrioritizationDocument1 pageND PrioritizationBea Dela Cena50% (2)
- Atypical PsychosisDocument10 pagesAtypical Psychosistsurmeli100% (1)
- Pregnant Over 40Document31 pagesPregnant Over 40Daniel Andre S. SomorayNo ratings yet
- Sleep and Sleep Disorders in The Menopausal Transition - BAKERDocument23 pagesSleep and Sleep Disorders in The Menopausal Transition - BAKERlucasaguiar1996No ratings yet
- Musculoskeletal ICD-10-CM Coding Tip Sheet: Overview of Key Chapter 13 UpdatesDocument3 pagesMusculoskeletal ICD-10-CM Coding Tip Sheet: Overview of Key Chapter 13 UpdatesAneez Malik100% (1)
- Cumulative NCLEX Test May 2023Document29 pagesCumulative NCLEX Test May 2023Julie Ann100% (2)
- Drug Study AmoxicillinDocument3 pagesDrug Study AmoxicillinJanzelvine Lee MontenegroNo ratings yet
- Case Pres NCP ProperDocument3 pagesCase Pres NCP ProperMyraNo ratings yet
- PEDIATRIC SURGERY - A Comprehensive Textbook For africa.-SPRINGER NATURE (2019) - 631-827Document197 pagesPEDIATRIC SURGERY - A Comprehensive Textbook For africa.-SPRINGER NATURE (2019) - 631-827adhytiyani putriNo ratings yet
- Delirium Pathophysiology: Multiple Neurotransmitter AbnormalitiesDocument2 pagesDelirium Pathophysiology: Multiple Neurotransmitter AbnormalitiesMikeVDCNo ratings yet
- Protozoa. Sporozoa. Haemosporidia (The Malaria Parasites)Document22 pagesProtozoa. Sporozoa. Haemosporidia (The Malaria Parasites)Sharan MurugaboopathyNo ratings yet
- Drugs of Choice for CNS, Blood, GIT, Endo & Chemo /TITLEDocument9 pagesDrugs of Choice for CNS, Blood, GIT, Endo & Chemo /TITLESHAKEEL1991No ratings yet
- DR Franciscus Ginting - Sepsis PIN PAPDI Surabaya WS-051019-DikonversiDocument82 pagesDR Franciscus Ginting - Sepsis PIN PAPDI Surabaya WS-051019-DikonversiDea LudjenNo ratings yet
- Prepration of The Isolation UnitDocument43 pagesPrepration of The Isolation UnitGayatri MudliyarNo ratings yet
- Tratament 5Document5 pagesTratament 5Razvan Cristian RotaruNo ratings yet
- Nebulization TherapyDocument3 pagesNebulization TherapyGemalie KadilNo ratings yet
- TENS relieves pain through peripheral and central mechanismsDocument6 pagesTENS relieves pain through peripheral and central mechanismsAdam ForshawNo ratings yet
- Preliminary Study To Identify Severe From Moderate Cases of COVID-19 Using Combined Hematology ParametersDocument15 pagesPreliminary Study To Identify Severe From Moderate Cases of COVID-19 Using Combined Hematology Parameterstrisna amijayaNo ratings yet
- H 12 PlmpilukDocument7 pagesH 12 PlmpilukSofiNo ratings yet
- Treatment of Cutaneous Larva Migrans: Eric CaumesDocument4 pagesTreatment of Cutaneous Larva Migrans: Eric CaumesElva PatabangNo ratings yet
- Drug StudyDocument7 pagesDrug StudyKynaWeeNo ratings yet
- ATLS Notes PDFDocument46 pagesATLS Notes PDFTilly Mandal100% (3)
- Nursing Care PlanDocument9 pagesNursing Care PlanjmichaelaNo ratings yet
- Further Practice-W11.1Document5 pagesFurther Practice-W11.1Binh Pham Thanh0% (3)
- Procedures Skin Tag RemovalDocument5 pagesProcedures Skin Tag RemovalIrvan Dwi FitraNo ratings yet