Professional Documents
Culture Documents
HEMA1
Uploaded by
marie judimor gomezOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
HEMA1
Uploaded by
marie judimor gomezCopyright:
Available Formats
CLINICAL HEMATOLOGY
RBC ABNORMALITIES
🞂 ERYTHROCYTOSIS AND - denote too many red cells; best defined in
POLYCYTHEMIA relation to hematocrit levels above the
reference range. Primary consequences are
hypervolimia and hyperviscosity.
🞂 ANEMIA - -decreased red cells;
- best defined in reference to a decreased
Hb level, the physiologic consequences and
symptoms are the direct result of the
decreased oxygen carrying capacity of the
blood
Notes:
Conditions associated with anemia or polycythemia can be subdivided into two groups:
➢ ABSOLUTE
o ABSOLUTE ANEMIA – TRUE DECREASE in RCM
o ABSOLUTE POLYCYTHEMIA – TRUE INCREASE in RCM
➢ RELATIVE (secondary to a change in plasma volume) → not true hematologic
disorders
o RELATIVE ANEMIA – there is a FLUID SHIFT from the extravascular to the
intravascular compartment, expanding the plasma volume and diluting RCM
▪ Seen in PREGNANCY and individuals with diseases associated with
HYPERPROTEINEMIA
o RELATIVE POLYCYTHEMIIA – is the result of DECREASE PLASMA VOLUME;
RCM is normal;
▪ Seen in conditions associated with DEHYDRATION
POLYCYTHEMIA
- Is the term used to refer to an increased concentration of erythrocytes
(erythrocytosis) in the circulating blood that is above normal for gender and age.
- S/S: ruddy complexion, headache, dizziness
1. ABSOLUTE POLYCYTHEMIA
• TRUE INCREASED in RCM
• RCM:
• Hematocrit:
• Other lab tests: RBC count Increased, Hemoglobin Increased
TWO KINDS:
i. PRIMARY POLYCYTHEMIA (POLYCYTHEMIA VERA)
- Aka: POLYCYTHEMIA RUBRA VERA, VAGUEZ OSLER
SYNDROME, ERYTHREMIA
- Part of the Chronic myeloproliferative disorder
- Cause: Unknown
- Lab eval:
▪ EPO: normal to decreased
▪ WBC and PLATELET COUNT: Increased
ii. SECONDARY POLYCYTHEMIA
- Cause: due to:
▪ PHYSIOLOGIC RESPONSE TO SYSTEMIC HYPOXIA
i. High altitude
ii. Pulmonary disease
iii. CVD
iv. Alveolary hypoventilation
v. Hemoglobinopathy
vi. Tobacco
▪ RENAL DISEASE and EXTRA RENALTUMORS
Lab eval:
-
▪ EPO: normal to increased
▪ WBC and PLATELET count: normal
2. RELATIVE POLYCYTHEMIA
• Increased RBC concentration due to DECREASED PLASMA VOLUME
• RCM:
• Hct:
• Causes:
TEMPLATE 07//CLINICAL HEMATOLOGY // 1
CLINICAL HEMATOLOGY
i. result of DEHYDRATION secondary to diarrhea, vomiting, excess sweating,
increased vascular permeability (burns and anaphylaxis), or the use of
diuretics.
ii. Anxiety and stress → STRESS SYNDROME, SPURIOUS
ERYTHROCYTOSIS, GAISBOCK’S SYNDROME
ANEMIA
What is anemia?
1. Anemia is considered to be present if the hemoglobin concentration of the red blood cells
(RBCs) or the packed cell volume of RBCs (hematocrit) is below the lower limit of the 95%
reference interval for the individual’s age, gender, and geographical location.
2. Anemia is physiologically defined as a condition in which the circulating blood lacks the ability
to adequately oxygenate body tissues. Anemia may be a sign of an underlying disorder.
a. Dilutional anemia with normal or increased total red cell mass may occur with
pregnancy, macroglobulinemia, and splenomegaly.
b. Some anemias have more than one pathogenetic mechanism and go through more
than one morphological state, such as blood loss anemia. In the case of accelerated
red cell destruction, hemolysis in excess of the ability of the marrow to replace these
losses occurs.
The presence or absence of clinical features can be considered under four major headings:
1. Speed of onset: Rapidly progressive anemia causes more symptoms than anemia of slow
onset because there is less time for adaptation in the cardiovascular system and in the 02
dissociation curve hemoglobin
2. Severity: Mild anemia often produces no symptoms or signs but these are usually present
when the hemoglobin is less than 9-10 g/dL
3. Age: The elderly tolerate anemia less well than the young because of the effect of lack of
oxygen on organs when normal cardiovascular compensation (increased cardiac output caused
by increased stroke volume and tachycardia) is impaired.
4. Hemoglobin 02 dissociation curve: This adaptation is particularly marked in some anemia
which either affect red cell metabolism directly (e.g. the anemia of pyruvate kinase deficiency
which causes a rise in 2,3-DPG concentration in the red cells) or which are associated with a
low affinity hemoglobin (e.g. Hb S).
Signs
General signs:
1. Pallor of mucous membranes which occurs if the hemoglobin level is less than 9 - 10 g/dL.
Conversely, skin color is not a reliable sign.
2. A hyperdynamic circulation may be present with tachycardia, a bounding pulse, cardiomegaly
and a systolic flow murmur especially at the apex. Particularly in the elderly, features of
congestive heart failure may be present. Retinal hemorrhages are unusual.
Specific signs are associated with particular types of anemia:
1. Koilonychia ’spoonnails’ with iron deficiency
2. Jaundice with hemolytic or megaloblastic anemia
3. Leg ulcers with sickle cell and other hemolytic anemia
4. Bone deformities with thalassemia major and other severe congenital hemolytic anemia
Symptoms
1. Shortness of breath particularly on exercise
2. Weakness
3. Lethargy
4. Palpitation
5. Headaches
In older subjects:
1. Cardiac failure
2. Angina pectoris or intermittent claudication or confusion may be present
3. Visual disturbances because of retinal hemorrhages may complicate very severe anemia,
particularly of rapid onset
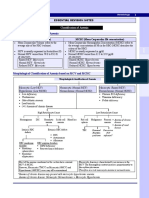
CLASSIFICATIONS OF ANEMIA
1. MORPHOLOGIC CLASSIFICATION OF ANEMIA
TEMPLATE 07//CLINICAL HEMATOLOGY // 2
CLINICAL HEMATOLOGY
a. which was originally proposed by Wintrobe, categorizes anemia by the size of the
erythrocytes. The major limitation of such a classification is that it tells nothing about
the etiology or reason for the anemia.
MICROCYTIC, NORMOCYTIC MACROCYTIC,
HYPOCHROMIC NORMOCHROMIC NORMOCHROMIC
IRON DEFICIENCY DEFECTIVE FORMATION OF THE MEGALOBLASTIC:
THALASSEMIA BLOOD CELLS OR THE PRESENCE ✓ VITAMIN B12
ANEMIA OF CHRONIC OF TUMOR CELLS IN THE BONE DEFICIENCY
DISEASE (SOME CASES) MARROW: o Pernicious
SIDEROBLASTIC ✓ APLASTIC ANEMIA anemia
ANEMIA ✓ LEUKEMIA o Vegetarian diet
✓ HODGKIN’S DISEASE o Taperworm
✓ MM infection
✓ LEUKOERYTHROBLASTOSIS o Sprue/
✓ METATASTATIC CANCER Steatorrhea
✓ ANEMIA ASSOCIATED (malabsorption
WITH RENAL AND syndrome)
ENDROCRINE DISEASE ✓ FOLIC ACID
✓ ANEMIA ASSOCIATED DEFICIENCY
WITH INFLAMMATORY o Sprue/
DISEASE Steatorrhea
ABNORMAL HEMOGLOBIN , o Pregnancy
INCREASED DESTRUCTION OF o Some dietary
deficiency
RBCs
✓ CERTAIN ACQUIRED H.A. Non-megaloblastic:
✓ PNH ✓ ALCOHOLISM
✓ SICKLE CELL ANEMIA ✓ LIVER DISEASE
✓ HDN
✓ ANEMIA OF CHRONIC RENA
INSUFFICIENCY
2. PATHOPHYSIOLOGICAL ANEMIA/ ANEMIA ACCORDING TO CAUSE
3 major categories:
1. BLOOD LOSS: Acute or Chronic
2. IMPAIRED RED CELL PRODUCTION
a. Due to BM DAMAGE, INFILTRATION, ATROPHY
i. Aplastic anemia
ii. Leukemia
iii. Lymphoma
iv. Leukoerythroblastosis
v. Multiple myeloma
vi. Myelofibrosis
vii. Pure red cell aplasia
b. Due to DECREASED ERYTHROPOIETIN
i. Anemia of chronic disease (inflammatory process)
ii. Chronic renal disease
iii. Hypothyroidism
c. Due to VITAMIN AND MINERAL DEFICIENCIES
i. IDA
ii. Megaloblastic anemia (Vitamin B12, Folic acid deficiency)
d. Due to DEFECT IN GLOBIN SYNTHESIS
i. THALASSEMIA
e. Due to IRON OVERLOAD
i. Hemochromatosis
ii. Sideroblastic anemia
f. Due to INEFFECTIVE ERYTHROPOIESIS
i. Congenital dyserythropoietic anemia
3. HEMOLYTIC ANEMIA–Accelerated red cell destruction (hemolysis in excess of
the ability of the marrow to replace these losses)
TEMPLATE 07//CLINICAL HEMATOLOGY // 3
CLINICAL HEMATOLOGY
I. INHERITED HEMOLYTIC ANEMIA/ INTRINSIC HEMOLYTIC ANEMIA
→INTRINSIC DEFECTS within the RBC – means patients RBCs would not survive
when transfused to a normal recipient.
a. STRUCTURAL MEMBRANE DEFECTS
i. Spheroctysosis
ii. Elliptocytosis
iii. Acanthocytosis
iv. Stomatocytosis
v. Xerocytosis
vi. Rh null disease
b. ERYTHROCYTE ENZYME DEFECTS
i. G6PD
ii. PK
iii. Glutathione reductase deficiency
c. DEFECTS OF THE HEMOGLOBIN MOLECULE
i. Hb C disorder
ii. Hb S-C disorder
iii. Hb S-S disorder (sickle cell anemia)
iv. Thalassemia
II. ACQUIRED HEMOLYTIC ANEMIA/ EXTRINSIC HEMOLYTIC ANEMIA
→ factor outside the erythrocyte acts on it
→Extrinsic defects in the red blood cell – means life span of normal red cells would
be decreased if they were transfused into the patients but patient’s red cells
survive normally if given to a normal recipient
a. NON-IMMUNE ACQUIRED HEMOLYITIC ANEMIAS
i. CHEMICALS, DRUGS, VENOMS
1. Aniline Copper (Wilson disease)
2. Lead from gasoline or paint Naphthalene (found in moth
balls)
3. Nitrobenzene
4. Phenacetin
5. Phenol derivatives
6. Resorcinol
7. Sulfonamides
ii. INFECTIOUS MICROORGANISMS
1. Bacteria: Clostridium sp., cholera, E. coli O157:H7, typhoid
fever
2. Protozoa: Leishmania, malaria (Plasmodium sp.),
toxoplasmosis
iii. PHYSICAL AGENTS
1. Severe burns
iv. TRAUMATIC AND MICROANGIOPATHIC HEMOLYTIC ANEMIAS
1. Disseminated intravascular coagulation
2. E. coli O157:H7 Hemolytic uremic syndrome
3. Prosthetic cardiac valves
4. Thrombotic thrombocytopenic purpura
b. IMMUNE ACQUIRED HEMOLYTIC ANEMIA
i. AUTOIMMUNE HEMOLYTIC ANEMIAS
1. Associated with warm-type antibodies
2. Associated with cold-type antibodies
3. Associated with both warm- and cold-type antibodies
ii. ISOIMMUNE HEMOLYTIC ANEMIAS
1. Hemolytic disease of the fetus and newborn (HDFN)
2. Rh incompatibility ABO incompatibility
iii. DRUG-INDUCED HEMOLYTIC ANEMIA
1. Adsorption of immune complexes to red cell membrane
2. Adsorption of drug to red cell membrane
3. Induction of autoantibody to drugs
4. Nonimmunological adsorption of immunoglobulin to red
blood cell membrane
MICROCYTIC, HYPOCHROMIC ANEMIA
1. IRON DEFICIENCY ANEMIA
- Most common micro, hypo anemia
- IDA can be a primary condition due to blood loss or inadequate iron intake.
TEMPLATE 07//CLINICAL HEMATOLOGY // 4
CLINICAL HEMATOLOGY
- It may also be a secondary condition due to a disease process or conditions that deplete iron
stores, such as GI bleed or pregnancy.
- IDA will manifest itself as a microcytic, hypochromic process, where the red cells are small
and deficient in hemoglobin
- The CBC will be characterized by a low red count, hemoglobin, hematocrit, MCV, and MCHC.
IRON INTAKE AND IRON ABSORPTION
- Iron is one of the most abundant metals in the world, yet IDA continues to be one the most
prominent nutritional disorders worldwide.
- Operational iron consists of iron used for oxygen binding and biochemical reactions. In
humans, most operational iron is found in the heme portion of hemoglobin or myoglobin.
- Following the oral intake of iron in the ferric (Fe3+) state, stomach secretions reduce the iron
to the ferrous (Fe2+) state. Conversion of ferric to ferrous iron requires gastric acid and is
facilitated by ascorbic acid. Stomach secretions, referred to as reducing agents include
glutathione, ascorbic acid, and sulfhydryl groups of proteins and digestion products.
- Most of the iron passes from the stomach to the duodenum and upper jejunum, where it
can be absorbed readily
- The first line of iron supply is the mononuclear phagocyte system
- Iron and globin are recycled as a result of red cell senescence
Iron balance is regulated by several conditions:
1. The amount of iron ingested
2. The amount of iron absorbed
3. Red blood cell formation using recycled and new iron
4. Iron stores, and
5. Iron loss through blood loss or other sources
Two broad types of dietary iron
1. NonHeme iron: Approximately 90% of iron from food is in the ferric (Fe3+) state, which must
be converted to the ferrous (Fe2+) state in order to be absorbed.
- Sources: beans, clams, vegetables
2. Heme iron: The other 10% of dietary iron is in the form of heme iron
- Sources: derived primarily from the hemoglobin and myoglobin of meat.
Iron in Storage
1. Ferritin: Found in liver, spleen, skeletal muscle, bone marrow
2. Hemosiderin: Found in excreted urine
Enhancers of Iron Absorption
Vitamin C Vinegar
Pickles Alcohol
Soy sauce Orange juice doubles the absorption of nonheme iron
Inhibitors of Iron Absorption
Coffee The tannin in tea decreases it by 75%.
Oregano bran, polyphenols, oxalates
Milk phytates, vegetable fiber, , and phosphates
Foods With High Iron Value
Clams Pinto beans Tofu
Soybeans Liver Packaged oatmeal
Lentils Garbanzo beans
Iron Transport
- Iron is transported in the plasma bound to transferrin
- Transferrin is a plasma protein synthesized by the liver, which has high affinity for ferric (Fe3+)
iron. Each molecule of transferrin can carry up to two iron atoms.
Iron Indices
Four values are used to describe body iron status:
1. Serum iron: measure the total amount of iron in the serum with a normal value of 50 to
150 µg/L
2. Serum transferrin or total iron binding capacity: The TIBC measures the availability of
iron binding sites on the transferrin molecule. The reference range, 250 to 450 µg/L, value
is elevated in iron deficient patients but subject to fluctuations in patients who use oral
contraceptives or have liver disease, chronic infections, or nephrotic syndrome.
TEMPLATE 07//CLINICAL HEMATOLOGY // 5
CLINICAL HEMATOLOGY
3. Transferrin saturation (% saturation): is derived as the product of the serum iron
concentration divided by the TIBC and multiplied by 100. The normal value is 20% to 50%.
4. Serum ferritin: One of the MOST SENSITIVE INDICATORS OF IRON STORES, with a
normal value of 20 to 250 µg/L for men and 10 to 120 µg/L for women
The development of IDA is a three-stage process:
1. Stage I: Continuum of iron depletion from the marrow (Prussian blue stain will show
absence of iron). Continuum - continuous sequence in which adjacent elements are not
perceptibly different from each other, although the extremes are quite distinct.
2. Stage II: Iron deficient erythropoiesis
3. Stage III: Finally, a frank case of IDA in the peripheral circulation
Stages of Iron Deficiency Anemia Matched to Diagnostic Signals
Stage 1: Iron Stores Depleted. Test for
1. Absence of stainable bone marrow iron
2. Decreased serum ferritin level
3. Increased TIBC
Stage 2: Iron-Deficient Erythropoiesis. Test for
1. Slight microcytosis
2. Slight decreased hemoglobin
3. Decreased transferrin saturation
Stage 3: Iron Deficiency Anemia. Test for
1. Decreased serum iron
2. Decreased serum ferritin
3. Increased TIBC
4. Decreased transferring saturation
Causes of Iron Deficiency
Decreased Iron Intake Inadequate dietary iron
Decreased Iron Achlorhydria
Absorption Gastric resection
Celiac disease (gluten-sensitive enteropathy)
Pica
Increased Iron Loss Gastrointestinal blood loss:
Neoplasms
Erosive gastritis due to nonsteroidal anti-inflammatory drugs
Peptic ulcer disease
Erosive esophagitis
Inflammatory bowel disease (Crohn’s disease, ulcerative
colitis)
Diverticular disease
Hemorrhoids
Meckel’s diverticulum
Infections: hookworm, schistosomiasis
Excessive menstrual blood flow
Frequent blood donation
Hemoglobinuria:,
paroxysmal nocturnal hemoglobinuria
malfunctioning artificial heart valve
Hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber
syndrome) Hemodialysis
Idiopathic pulmonary hemosiderosis
Runner’s anemia
Increased Iron Infancy
Requirements Pregnancy
Lactation
Clinical Features
- In general, the symptoms of iron deficiency anemia are those of anemia of any cause: fatigue,
dyspnea on exertion, and dizziness.
- There are a few signs and symptoms that are relatively unique to iron deficiency anemia,
TEMPLATE 07//CLINICAL HEMATOLOGY // 6
CLINICAL HEMATOLOGY
1. “spoon” fingernails
2. glossitis (atrophy of the papillae of the tongue, with burning or soreness)
3. ulcerations or fissures at the corners of the mouth (angular stomatitis)
4. dysphagia due to esophageal webs or strictures.
- The combination of dysphagia, angular stomatitis, and hypochromic anemia has been called
the PLUMMER-VINSON OR PATERSON-KELLY SYNDROME.
- PICA is the habitual consumption of unusual substances. Food pica is the compulsive eating
of one kind of food, often crunchy foods such as celery, potato chips, carrots, or raw potatoes.
Specific examples of pica:
a. Geophagia (consumption of earth or clay),
b. Pagophagia (ice), and
c. Amylophagia (laundry starch): Laundry starch and clay can impair iron absorption.
Laundry starch is also extremely poor in iron, so if starch constitutes a significant
proportion of caloric intake, the diet is likely to be deficient in iron.
Laboratory Findings in Iron Deficiency
Blood Count Microcytic, hypochromic red cells if Hgb <12 g/dL (men), < 10 g/dL
(women)
Leukopenia possible
Platelets high with active bleeding
Reticulocytes lower than expected for degree of anemia
Bone Marrow Erythroid hyperplasia
Stainable iron very low or absent
Other Serum iron very low, Total iron-binding capacity high, percent of
saturation very low
Serum ferritin < 10 ng/mL: The single most efficient test to assess body
iron stores
Free erythrocyte protophorphyrin high
RBC survival time slightly low
RDW high (Anisocytosis)
2. SIDEROBLASTIC ANEMIA
- Group of disorders characterized by abnormalities of heme metabolism.
- Diagnostic feature is the presence of nucleated red cells with iron granules (ringed
sideroblasts) in the marrow and the appearance of a DIMORPHIC PERIPHERAL BLOOD
PICTURE, found particularly in the primary types.
- RDW is increased
- Hypercellular - BM shows an increased erythropoietic activity
- Reticulocyte count not elevated
Classification of Sideroblastic Anemia
I. Inherited – Rare sex-linked; adolescence; anemia is generally severe with hematocrit
level of approximately 20%; marked increase of storage iron
II. Acquired
1. Primary (idiopathic) (Myelodysplasias) - more common; adults above 50 years of age;
hematocrit level approximately 25 – 30%; Adequate to abundant iron but unable to
incorporate it into hemoglobin; enters the developing red cell but accumulates in the
perinuclear mitochondria of normoblasts
2. Secondary
a. Associated with other myeloproliferative syndromes (leukemias, polycythemia
vera)
b. Pyridoxine-deficient or responsive anemia
b.1. Vitamin B6 deficiency
b.2. Drugs: isoniazid, cycloserine
b.3. Alcoholism
c. Disorders of hemoglobin synthesis
c.1. Folate deficiency, B12 deficiency
c.2. Lead poisoning
c.3. Erythropoietin porphyria
3. LEAD POISONING
- Adults, lead exposure is usually occupational.
- Children, most common is pica. Children are also sensitive to the lead levels in polluted
atmospheres.
TEMPLATE 07//CLINICAL HEMATOLOGY // 7
CLINICAL HEMATOLOGY
- Lead depresses enzyme activity at the beginning, middle, and end of heme synthesis.
Defective delta-aminolevulinic dehydrase activity causes delta-ALA to accumulate.
- Coproporhyrin metabolism is depressed and the insertion of ferrous iron to protoporhyrin is
inhibited because lead also inhibits heme synthetase.
- Laboratory findings:
o Basophilic stippling
o Elevated red cell protoporhyrin levels→best laboratory test for quantifying lead
toxicity.
4. ANEMIA OF CHRONIC DISEASE AND INFLAMMATION:
- The anemia of chronic disease or the anemia of inflammation is one of the most common
anemias in hospital populations and second only to iron deficiency in terms of frequency.
- Anemia of chronic disease is quite common among certain illnesses lasting longer than 1 to 2
months, especially those with infection, noninfectious inflammation, or malignancy.
- Patients with the anemia of chronic disease will show a borderline low red cell count,
hemoglobin, and hematocrit, a slightly low MCV, and a nor-mal MCHC.
- The peripheral smear will be essentially normal with slight variation in size and chroma.
- Serum iron will be low, serum ferritin will be normal or increased, and serum TIBC will be
decreased. Although this is NOT the profile for a patient with IDA, in both conditions the
patient will have a low serum iron.
- The main pathogenesis of the anemia of chronic disease appears to be the effects of
cytokines on erythropoiesis. They impair the proliferation and differentiation of erythroid
precursors, diminish erythropoietin production, and decrease the bone marrow response to
erythropoietin.
- They also affect iron metabolism by increasing the retention of it in the bone marrow stores
and by decreasing its availability for erythroid precursors (iron is blocked from reaching
erythroid precursors because of impaired release from macrophages).
- Few individuals require a blood transfusion for treatment of their anemia.
- Hepcidin is linked to the immune response and has been identified as a regulator of iron
transit.
Conditions Leading to Anemia of Inflammation or Anemia of Chronic Disease
1. Collagen vascular disease
2. Rheumatoid arthritis
3. Chronic renal disease
4. Thyroid disorders
5. Malignancies
6. Inflammatory bowel disease
MUST KNOW!
Differential Diagnosis of Hypochromic Microcytic Anemia
SERUM SERUM RD
ANEMIA TIBC FEP HbA2 HbF
IRON FERRITIN W
Iron Deficiency Low High Low High N N-L High
Alpha-Thalassemia High N High N N Low
Beta-Thalassemia High N High N High High High
(varies
)
Anemia of Chronic Disease Low Low High High N N N
Sideroblastic Anemia High N High Low N N High
MACROCYTIC, NORMOCHROMIC ANEMIA
The macrocytic anemias are a morphological classification of anemias that have an MCV of greater
than 100 fL. There are several causes but they can be broadly subdivided into:
✓ megaloblastic (dramatically increased >130 Fl)
✓ non-megaloblastic (~100–110 fL).
Macrocytic Anemia: Megaloblastic versus Non-Megaloblastic
MEGALOBLASTIC ANEMIA NON-MEGALOBLASTIC ANEMIA
Folate deficiency Liver disease
Cobalamin deficiency Myelodysplasia
TEMPLATE 07//CLINICAL HEMATOLOGY // 8
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
Antifolate drugs Reticulocytosis
Cancer chemotherapy Hypothyroidism
Alcoholism
Chronic Obstructive Pulmonary Disease
(COPD)
Causes of Megaloblastic anemia:
1. Vitamin B12 deficiency
2. Folate deficiency
3. Abnormalities of Vitamin B12 or Folate metabolism (e.g. transcobalamin deficiency, nitrous
oxide, antifolate drugs)
4. Other defects of DNA synthesis
a. Congenital enzyme deficiencies (e.g. orotic aciduria)
Orotic aciduria: The best known example of congenital deficiency of one or other
enzyme concerned in purine or pyrimidine synthesis that can cause megaloblastic anemia
identical in appearance to that caused by a deficiency of B12 or folate.
b. Acquired enzyme deficiencies (e.g. alcohol, therapy with hydroxyurea, cytosis arabinoside)
Vitamin B12 and Folate: Nutritional aspects
Vitamin B12 Folate
Normal daily dietary intake 7 – 30 µg 200 – 250 µg
Main foods Animal produce only Most, especially liver, green and yeast
(meat, eggs, milk, and
cheese)
Absorption Site Ileum Duodenum and jejunum
Mechanism Intrinsic factor* Conversion of
methyltetrahydrofolate
Limit 2 – 3 µg/day 50 – 80% of dietary content
Transport in plasma Most bound to haptocorrin; Weakly bound to albumin
TC essential for cell uptake
Major intracellular Methyl- and Reduced polyglutamate derivatives
physiological forms deoxyadenosylcobalamin
Usual therapeutic form Hydroxycobalamin Folic (Pteroylglutamic) acid
1. VITAMIN B12
TRANSPORT: the transcobalamins
1. Haptocorrin - most B12 in plasma is bound to this transport protein, (previously called
transcobalamin I). This is a glycoprotein largely synthesized by granulocytes and
macrophages. Vitamin B12 levels in serum bound to haptocorrin does not transfer to
marrow; it appears to be functionally “dead”.
2. Transcobalamin - Vitamin B12 is absorbed into portal blood where it becomes attached to
this plasma-binding protein (TC, previously called transcobalamin II) which delivers B12
to bone marrow and other tissues.
a. TC deficiency causes MEGALOB LASTIC ANEMIA because of failure of B12
to enter marrow (and other cells) from plasma but the SERUM B12 LEVEL
IN TC DEFICIENCY IS NORMAL.
ABSORPTION
Two mechanisms for cobalamin absorption :
1. Passive absorption occurring equally through buccal, duodenal, and ileal mucosa; it is rapid
but extremely inefficient, <1% of an oral dose is absorbed by this process.
2. The other major cobalamin transport protein in plasma is TC II. This is synthesized by liver
and by other tissues, including macrophages, ileum, and endothelium. It normally carries
only 20–60 ng of cobalamin per liter
MECHANISM:
1. Dietary cobalamin is released from protein
complexes by enzymes in the stomach,
duodenum, and jejunum; it combines
rapidly with a salivary glycoprotein that
belongs to the family of cobalamin-binding
proteins known as HAPTOCORRINS
TEMPLATE 07//CLINICAL HE MATOLOGY // KENNETH ART CLOSA NARAG, RMT 9
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
2. In the intestine, the HC is digested by
pancreatic trypsin and the cobalamin
transferred to IF. Intrinsic Factor is a
glycoprotein, is synthesized and secreted
by the gastric parietal cells of the
mucosa in the fundus region and body of
the stomach, and its secretion parallels
that of hydrochloric acid.
3. The IF-cobalamin complex passes to the
ileum, where IF attaches to a specific
receptor (cubilin) on the microvillus
membrane of the enterocytes.
4. The cobalamin-IF complex enters the ileal
cell where IF is destroyed. After a delay of
~6 hours, the cobalamin appears in portal
blood attached to transcobalamin (TC)
II. Between 0.5 and 5.0 µg of cobalamin
enters the bile
There are three regions of the stomach: the fundus and the body, both of which contain acid-
secreting gastric parietal cells and pepsinogen-secreting zymogenic cells, and the antrum, which
contains gastrin-producing cells.
CAUSES OF VITAMIN B12 DEFICIENCY
1. Malabsorption (Most Common)
a. Pernicious anemia: loss of IF production and gastric acid
b. Gastrectomy: loss of IF production and gastric acid
c. Crohn’s disease or Inflammatory Bowel Disease (IBD): loss of absorption in terminal
ileum
d. Resection of terminal ileum: loss of absorption by specific IF-B12 receptors
e. Pancreatic insufficiency: inability to digests R-binders off of B12
f. Blind loop syndrome: bacterial overgrowth; bacteria compete for B12
g. Congenital deficiency of intrinsic factor (rare)
h. Fish tapeworm (Diphyllobothrium latum): competition for B12
i. Zollinger-Ellison syndrome: impaired B12 absorption but no megaloblastic anemia;
hypersecretion of gastric juice which interferes the binding of B12 to IF
j. Imerslund’s syndrome: inherited as autosomal recessive trait; Vitamin B12 is bound to
IF but there is deficiency of the receptor site in the terminal ileum.
2. Dietary Deficiency
a. Strict vegans
b. Infants breast-fed by vegetarian mothers
3. Congenital Deficiency of Transcobalamin (Rare)
Notes: PERNICIOUS ANEMIA
- Classic or “Addisonian” Pernicious anemia is megaloblastic anemia due to
autoimmune chronic gastritis with destruction of the gastric parietal cells.
- Pernicious anemia is not synonymous with megaloblastic anemia; it is a subset of
megaloblastic anemia.
- Achlorhydria, the absence of hydrochloric acid (HCl) in the stomach, is an important
finding in pernicious anemia. An absence of free HCl in gastric fluid is a universal feature of
this form of megaloblastic anemia. Achlorhydria results from atrophy of the parietal cells of
the stomach.
- The LDH is significantly increased owing to the increased intramedullary destruction of
megaloblastic bone marrow cells.
- Patients with pernicious anemia may have serum antibodies against gastric parietal cells
(anti–parietal cell antibodies) or antibodies against intrinsic factor (anti-IF antibodies).
7 Clinical “P”s of Pernicious Anemia
1. Pancytopenia
2. Peripheral neuropathy
3. Posterior spinal column neuropathy
4. Pyramidal tract signs
5. Papillary (tongue) atrophy
6. pH elevation (gastric fluid)
7. Psychosis (megaloblastic psychosis)
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 10
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
SCHILLING TEST
• The standard method to diagnose pernicious anemia, once cobalamin deficiency is
confirmed.
• Radiolabeled cobalamin is given orally, a large dose of unlabeled B12 is given
intramuscularly, and urine is collected for 24 hours.
• The amount of radioactivity in the urine indicates how much B12 was absorbed
orally.
o B12 of <6% in the urine = MALABSORPTION OF B12.
o If the initial value is abnormal →SECOND STAGE is performed in which intrinsic
factor is given together with the labeled B12.
o Increase in the amount of B12 absorbed during the second stage of the Schilling test
= PERNICIOUS ANEMIA.
2. FOLIC ACID
- Folic (pteroylglutamic) acid is a yellow, crystalline, water-soluble substance. Humans are
unable to synthesize the folate structure and thus require preformed folate as a vitamin.
- Folic acid is abundant in vegetables, fruit, cereals, and dairy products. Folic acid is heat labile,
and much is destroyed by cooking.
- The primary dietary source for folic acid is fresh uncooked fruits and vegetables.
Causes of Folate Deficiency
Inadequate Diet (Most common) Rare Causes
Alcoholism Hemodialysis
Lack of fresh fruits and vegetables Antiepileptic drugs
Malabsorption (Less common) Antifolate drugs
Gluten-sensitive enteropathy (celiac Increased requirements
sprue)
Tropical sprue Chronic hemolytic anemia
Extensive small bowel resection Psoriasis
Inflammatory Bowel Disease (regional Pregnancy
enteritis)
Oral contraceptives (Uncommon)
Exposure to nitrous oxide (N2O)
LABORATORY ABNORMALITIES IN MEGALOBLASTIC ANEMIA
1. There is ASYNCHRONY between the age of the nuclear material and the age of the
cytoplasm, but this can best be appreciated by making a serious comparison of the nuclear
and cytoplasmic material in megaloblastic precursor cells versus normoblastic precursor cells.
2. Decreased hemoglobin
3. Increased MCV (often ≥120 fL)
4. Oval macrocytes
5. Leukopenia
6. Hypersegmented neutrophils
a. ˃5 nuclear lobes in any cell
b. ≥5% of neutrophils have 5 nuclear lobes
7. Thrombocytopenia
8. Increased lactic dehydrogenase (LD)
9. Increased bilirubin
10. Decreased haptoglobin
11. Bone marrow
a. Megaloblasts (enlarged erythrocyte precursors with immature nuclear chromatin)
b. The marrow is hypercellular with erythroid hyperplasia and M:E ratio of 1:1 to 1:3 (Normal
is 3:1)
c. Giant bands and metamyelocytes
Laboratory Diagnosis of Megaloblastic Anemias
TEST COBALAMIN DEFICIENCY FOLATE DEFICIENCY
Serum cobalamin Decreased Usually normal
Serum Folate Normal to increased Decreased
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 11
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
Erythrocyte folate Decreased Decreased
Serum methylmalonic acid Increased Normal
Serum homocysteine Increased Increased (Moderately)
NORMOCYTIC, NORMCHROMIC ANEMIA
1. APLASTIC ANEMIA
• Aplastic anemia indicates pancytopenia in the presence of a hypocellular (aplastic)
bone marrow
PATHOPHYSIOLOGY OF APLASTIC ANEMIA
• Caused by a failure of hematopoietic stem cells. Failure may be due to an abnormality of
the hematopoietic stem cells themselves or to some factor that suppresses or destroys them.
• It is important to distinguish aplastic anemia from other causes of pancytopenia such
as myelodysplasia, megaloblastic anemia, and acute leukemia, among others.
• In APLASTIC ANEMIA, the cells that are present are normal or have only mild morphologic
abnormalities. The presence of nucleated or abnormally shaped erythrocytes (other
than mild macrocytosis), hypersegmented neutrophils or other abnormal leukocytes,
immature cells, or megakaryocyte fragments strongly points to a disorder other than
aplastic anemia.
Causes of Aplastic Anemia
A. FAMILIAL
1. FANCONI’S ANEMIA
2. DYSKERATOSIS CONGENITA
3. SCHWACHMAN-DIAMOND SYNDROME (aplastic anemia with pancreatic insufficiency)
INHERITED (CONSTITUTIONAL) VARIANTS OF APLASTIC ANEMIA
There are two types of congenital (primary) aplastic anemia:
1. FANCONI'S ANEMIA: is autosomal recessive, and characterized as having microencephaly,
skin hyperpigmentation (brown), short stature, skeletal disorders, renal anomalies, and/or
mental retardation.
2. Estren–Dameshek syndrome: Estren– Dameshek syndrome has the same hematologic
features as Fanconi’s but without the physical abnormalities.
FANCONI’S ANEMIA
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 12
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
- The most common (approximately two-thirds of cases) of aplastic anemia.
- A rare and often fatal inherited disease in which the bone marrow fails to produce red blood
cells, white blood cells, platelets, or a combination of these cells.
- The clinical picture of Fanconi’s anemia is variable and can include pancytopenia, skeletal
abnormalities, neurologic abnormalities, and physical abnormalities.
- A characteristic feature of Fanconi’s anemia is INCREASED CHROMOSOMAL FRAGILITY.
Chromosomes show spontaneous breaks, gaps, rearrangements, reduplications, and
exchanges.
- Diagnosis: The main diagnostic test is culturing the patient’s lymphocytes in diepoxybutane
or mitomycin C and demonstrating increased chromosomal instability.
NOTES:
Pancytopenia
- Means a disorder in which all 3 blood elements (red blood cells, white blood cells and platelets)
are decreased than normal.
Other Constitutional Aplastic Anemias
1. SCHWACHMAN-DIAMOND SYNDROME
- Is an inherited disorder characterized by exocrine pancreatic deficiency,
pancytopenia, skeletal changes
2. DYSKERATOSIS CONGENITA
- Consists of mucocutaneous abnormalities with variable hematologic disorders.
- The mucocutaneous changes include reticulated pigmentation of skin in the upper
body, mucosal leukoplakia, and dystrophic changes in the nails.
B. ACQUIRED
1. Chemicals and toxins: BENZENE, INSECTICIDES (DDT, PARATHION,
CHLORDANE), ARSENIC
2. Medications: CHEMOTHERAPY DRUGS, CHLORAMPHENICOL, PHENYBUTAZONE,
ANTICONVULSANTS, CARBAMAZEPINE, CLONAZIPRIL, GOLD COMPOUNDS,
ORAL HYPOGLYCEMIC AGENTS
3. IONIZING RADIATION
4. Viral infections: HEPATITIS, EPSTEIN-BARR VIRUS, HIV, CMV, DENGUE,
PARVOVIRUS B19
5. Miscellaneous: PREGNANCY, AUTOIMMUNE DISORDERS (DIFFUSE
EOSINOPHILIC FASCIITIS)
6. Idiopathic
a. Approximately 70% of acquired aplastic anemia cases are IDIOPATHIC.
(Rodak, 2012)"
2. PURE RED CELL APLASIA
- Pure red cell aplasia (PRCA) is defined as anemia with an absence of erythroid
precursors in the bone marrow.
- In contrast with aplastic anemia, granulocyte precursors and megakaryocytes are
preserved in PRCA.
1. CONGENITAL HYPOPLASTIC ANEMIA (DIAMOND-BLACKFAN ANEMIA)
- Congenital hypoplastic anemia (CHA) is heterogeneous in clinical features, pattern of
inheritance, and associated anomalies.
- It probably represents several different conditions, with the common feature of onset
during infancy.
- Differential Diagnosis
- The most important differential diagnosis is CHA versus transient erythroblastopenia of
childhood (TEC).
Characteristics CHA TEC
Age of onset Usually <1 year Usually ˃1 year
Family history Sometimes present Absent
MCV Frequently elevated Normal
RBC precursors in BM Absent or decreased Absent or decreased
Fetal Hgb Increased Normal
RBC i Antigen Present Absent
RBC adenosine deaminase Elevated Normal
activity
2. ACQUIRED PURE RED CELL APLASIA
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 13
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
- Acquired pure red cell aplasia (PRCA) can be divided into primary (idiopathic) and
secondary types.
- Most cases of primary acquired PRCA appear to be caused by an IgG antibody that inhibits
proliferation and/or maturation of erythroid progenitor cells.
Acquired
1. Primary
2. Secondary
a. Thymoma
b. Hematologic malignancies: CML, non-Hodgkin’s lymphomas, Hodgkin’s disease, others
c. Non-hematologic malignancies
d. Infections: parvovirus B19, EBV, adult T-cell lymphocytotrophic virus, hepatitis,
mumps, CMV, Mycoplasma pneumoniae
e. Autoimmune hemolytic anemia
f. Collagen vascular diseases: SLE, rheumatoid arthritis
g. Drugs and chemicals
h. Pregnancy
i. Severe renal failure
j. Severe malnutrition
k. Miscellaneous
3. CONGENITAL DYSERYTHROPOIETIC ANEMIAS
- Congenital dyserythropoietic anemias (CDAs) are a group of conditions characterized by
anemia and erythroid hyperplasia in the bone marrow, with ineffective erythropoiesis
The three described types are as follows:
A. CONGENITAL DYSERYTHROPOIETIC ANEMIA TYPE I
- A characteristic feature is internuclear bridges between erythroblasts. The cause is
unknown.
B. CONGENITAL DYSERYTHROPOIETIC ANEMIA TYPE II is also known as HEMPAS
(Hereditary Erythroblastic Multinuclearity with a Positive Acidified Serum test).
- It is the most common type of CDA..
- The characteristic feature is that acidified serum from approximately 30% of normal people
lyses CDA type II cells but do not hemolyze in the sugar water test. Unlike paroxysmal
nocturnal hemoglobinuria (PNH), the patient’s own serum does not cause hemolysis.
- The bone marrow shows erythroid hyperplasia; many late erythroid precursors are
binucleate, with occasional multinucleate cells but with no megaloblastic changes. On
electron microscopy there are two layers to the cell membrane.
- The red cells in this disorder contain the blood group antigen, i, on them, termed the
HEMPAS antigen.
C. CONGENITAL DYSERYTHROPOIETIC ANEMIA TYPE III
-is the rarest of the CDAs.
4. MYELOPHTHISIC ANEMIAS
- Fibrosis of the bone marrow, usually accompanied by a characteristic blood smear picture
called leukoerythroblastosis, can occur as:
o primary hematologic disease→ myelofibrosis or myeloid metaplasia
o secondary hematologic disease→ myelophthisis.
The pathophysiology has three distinct features:
1. Proliferation of fibroblasts in the marrow space (myelofibrosis);
2. The extension of hematopoiesis into the long bones and into extramedullary sites, usually the
spleen, liver, and lymph nodes (myeloid metaplasia); and
3. Ineffective erythropoiesis
5. DISORDERS RELATED TO HEMOGLOBIN BIOSYNTHESIS
A. DISORDERS OF HEME (PORPHYRIN) SYNTHESIS
PORPHYRIA
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 14
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
- A primary abnormality in porphyrin biosynthesis leads to excessive accumulation and
excretion of porphyrins or their precursors by the biliary and/or renal route.
- Porphyria is derived from the Greek word, porphyra, which means purple. The purple-red
pigment (porphyrins) is responsible for the wine-red color characteristic of porphyric
urine.
- PBG is normally excreted in small amounts in urine; however, it appears in significantly
elevated amounts in acute intermittent porphyria, which may be detected by testing the urine
with Ehrlich’s aldehyde reagent.
- Historically, hereditary porphyria affected many members of the royal houses of Stuart, Queen
of Scots, several royal members exhibited classic symptoms of variegate porphyria.
- Porphyrias can be classified based on various characteristics:
1. Clinical presentation (acute versus chronic)
2. Source of enzyme deficiency
3. Site of enzyme deficiency in the heme biosynthetic pathway
Types of Porphyria:
A. Inherited
1. CONGENITAL ERYTHROPOIETIC PORPHYRIA (GUNTHER’S DISEASE)
- Causes cutaneous photosensitivity and is one of the rarer types of porphyria.
- There is decreased production of :
▪ uroporphyrinogen III cosynthetase, which then results in an
overproduction of uroporphyrinogen I
- Most characteristic is an increased excretion of uroporphyrinogen I in the urine which
may be pink to deep burgundy in color.
2. PORPHYRIA CUTANEA TARDA
- It is manifested clinically by sensitivity to light and to minor trauma with
resultant skin lesions and scarring.
- It is caused by a decreased production of:
▪ uroporphyrinogen decarboxylase.
- The urine is generally reddish or brownish in color and contains increased amounts
of uroporhyrin I
3. ERYTHROPOIETIC PROTOPORPHYRIA
- It is caused by a decreased activity of :
▪ heme ferrochelatase (heme synthetase), resulting in increased
concentrations of protoporphyrin IX in the feces.
- The red blood cells also contain a marked increased in protophorphyrin IX and will
show fluorescent cytoplasm.
4. ACUTE INTERMITTENT HEPATIC PORPHYRIA
- It is caused by a deficiency in:
▪ uroporphyrinogen I synthetase, and is the most common of the
inherited porphyrias.
5. HEREDITARY COPROPORPHYRIA
- Resembles acute intermittent hepatic porphyria.
- It is caused by a decrease in:
▪ coproporphyrinogen oxidase, which results in the increased amounts of
coproporphyrin III in the urine and feces and accumulation in the liver.
6. VARIEGATE PORPHYRIA
- The clinical symptoms are those similar to porphyria cutanea tarda. It is caused by a
deficiency in:
▪ protoporphyrinogen oxidase.
B. Acquired
- An acquired form has been found that is caused by exposure to halogenated aromatic
hydrocarbons
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 15
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
B. DISORDERS OF IRON METABOLISM
IRON OVERLOAD
- Too much iron accumulates in HH, porphyria cutanea tarda, and the iron-loading anemias, for
example, hemolytic dyserythropoietic, myelodysplastic, and aplastic anemias.
- In primary overload disorders, iron absorption from a normal diet is increased due to inherited
alteration in factors that control iron uptake and retention.
- In comparison, secondary iron overload may arise in patients with chronic disorders or
erythropoiesis or hemolytic anemias, for example, sideroblastic anemia as a consequent of
iron therapy due to excessive dietary or supplement ingestion of iron or from multiple RBC
transfusions.
1. SIDEROBLASTIC ANEMIA (Notes on Microcytic, Hypochromic Anemia)
2. HEREDITARY HEMOCHROMATOSIS
- In contrast to iron overload caused by various conditions or disorders (e.g., multiple
transfusions, alcohol abuse, or hepatocellular carcinoma), HH is a genetic error of
metabolism that produces inappropriately increased (twofold to threefold greater
than normal) GI absorption of iron.
Classification and Characteristics
1. HEREDITARY HEMOCHROMATOSIS
- It is inherited as autosomal recessive trait. The disease is often referred to as “bronze
diabetes”; bronze colored skin pigmentation from melanin deposits in the skin
exposed to sunlight.
2. JUVENILE HEMOCHROMATOSIS
- Caused by HEMOJUVELIN (HJV) MUTATIONS (TYPE 2A) share the same phenotype
as that of patients with mutations that disrupt the hepcidin gene (HAMP, type 2B).
- Membrane hemojuvelin positively modulates the iron regulator hepcidin. Type 2B
is related to HAMP and the production of hepcidin. It is characterized by hepcidin deficiency
and severe iron overload.
- No or very low hepcidin activation is the hallmark of juvenile hemochromatosis.
Hepcidin: a liver-produced peptide hormone is the master regulatory hormone of systemic
iron metabolism. The interaction of hepcidin with the plasma iron transporter, ferroportin,
coordinates iron acquisition with iron utilization and storage.
3. TRANSFERRIN RECEPTOR 2(TFR2)HEMOCHROMATOSIS is a different form of the
disease that usually appears in midlife.
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 16
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
- This form is associated with mutation in TFR2, the gene encoding transferrin receptor
2, found on human chromosome 7q22.
4. FERROPORTIN DISEASE related to the SLC40A1 gene that encodes for ferroportin
- This form of the disorder differs from the others in that it is inherited in an autosomal
dominant pattern and is associated with increased iron in macrophages of mononuclear
phagocytic system. This form also differs because it lacks linkage to the HLA locus.
Treatment: Treatment can be by therapeutic phlebotomy or iron chelation therapy. Removal
of one unit (450 mL) of whole blood once or twice weekly is the safest and most effective way of
removing iron from the body. Each unit of blood contains approximately 250 mg of iron. In patients
with transfusion-dependent anemia, chelation is the only option for effective iron removal.
6. HEMOGLOBIN DEFECTS (HEMOGLOBINOPATHIES)
- Encompass a heterogeneous group of disorders associated with genetic mutations in both the
alpha-globin and beta-globin genes.
Classification of Hemoglobinopathies
I. Structural hemoglobinopathies—hemoglobins with altered amino acid sequences that result
in deranged function or altered physical or chemical properties
A. Abnormal hemoglobin polymerization—HbS
B. Altered O2 affinity
1. High affinity—polycythemia
2. Low affinity—cyanosis, pseudoanemia
C. Hemoglobins that oxidize readily
1. Unstable hemoglobins—hemolytic anemia, jaundice
2. M hemoglobins—methemoglobinemia, cyanosis
II. Thalassemias—defective biosynthesis of globin chains
A. α Thalassemias
B. β Thalassemias
C. δβ, ϒδβ, αβThalassemias
III. Thalassemic hemoglobin variants—structurally abnormal Hb associated with co-inherited
thalassemic phenotype
A. HbE
B. Hb Constant Spring
C. Hb Lepore
IV. Hereditary persistence of fetal hemoglobin— persistence of high levels of HbF into adult life
V. Acquired hemoglobinopathies
A. Methemoglobin due to toxic exposures
B. Sulfhemoglobin due to toxic exposures
C. Carboxyhemoglobin
D. HbH in erythroleukemia
E. Elevated HbF in states of erythroid stress and bone marrow dysplasia
A. SICKLE CELL ANEMIA (HEMOGLOBIN S)
- Hemoglobin S (sickle hemoglobin) is the most common hemoglobinopathy worldwide.
- Sickle cell trait provides a survival advantage over individuals with normal hemoglobin in
regions where malaria, P. falciparum, is endemic. Sickle hemoglobin impairs malaria growth.
Sickle cell trait does not provide absolute protection, but individuals are more likely to survive
the acute illness.
Pathophysiology:
- The abnormality in Hb S is substitution of valine for
- glutamic acid at the sixth amino acid position (6 Glu → Val).
- Deoxygenated hemoglobin S tends to polymerize into long rigid structures, which distort the
cell into the characteristic sickle shape. Anything that causes deoxygenation of
hemoglobin predisposes to sickling, including hypoxia, acidosis, and increased
temperature.
HOMOZYGOUS HEMOGLOBIN S (SICKLE CELL ANEMIA): The severity of illness in sickle cell
anemia (HEMOGLOBIN SS) is highly variable and can vary even within families.
Complications of Sickle Cell Disease
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 17
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
Complication Consequences
Vaso-occlusion Painful crises: extremities (bones and joints);
abdomen; aseptic necrosis of femoral heads
Painful crises are the most common type of crisis
and are believed to be caused by occlusion of small
blood vessels, with consequent infarction of tissues.
“hand-foot syndrome or dactylitis” in young children
Autosplenectomy Increased susceptibility to infection, particularly S.
pneumonia
Cerebrovascular accidents Strokes are a major cause of morbidity in sickle cell
disease, occurring in 5 to 8% of patients by the age of
14 years.
Aplastic crises due to parvovirus B19 Acute exacerbation of anemia; Acute parvovirus B19
infection infection causes a transient halt in production of
erythrocytes, which usually lasts about 5 to 7 days.
Infarction of renal medulla Inability to concentrate urine; infarction of papillae;
hematuria
Vaso-occlusion in and infarction of Priapism and impotence
corpora cavernosa
Chronic hemolysis Bilirubin gallstones
Leg ulcers
Proliferative retinopathy Intraocular hemorrhage; retinal detachment (more
common in hemoglobin SC)
Cardiomyopathy
Acute chest syndrome (acute lung The second most common cause of
syndrome) hospitalization (after vasoocclusive crises) and
causes approximately 25% of the deaths from sickle
cell disease.
Infections Infections are the most common cause of death in
sickle cell disease
Drug Therapy
1. Hydroxyurea
- A cytostatic agent; a ribonucleotide reductase inhibitor, stimulates the production of Hb F
but suppresses bone marrow production. Fetal hemoglobin is a potent inhibitor of the
polymerization of deoxyhemoglobin S.
- The exact mechanism of action of hydroxyurea remains uncertain. Hydroxyurea therapy
can ameliorate the clinical course of sickle cell anemia in some adults with three or more
painful crises per year.
- In addition to moderating acute painful episodes, hydroxyurea has been demonstrated to
reduce the frequency of hospitalizations and the need for blood.
SICKLE CELL SYNDROMES
HETEROZYGOUS HEMOGLOBIN S (SICKLE TRAIT)
- People who are heterozygous for hemoglobin are generally asymptomatic, have a normal
blood hemoglobin level and complete blood count (CBC), and have a normal life
span.
Sickle β –Thalassemia
- The inheritance of the sickle gene from one parent and a β-thalassemia gene from the other
results in the compound heterozygous state: sickle β-thalassemia.
Sickle-C Disease (Hemoglobin SC)
- The patients have only Hb S and C, with an absence of Hb A and normal or increased levels
of Hb F.
B. OTHER HEMOGLOBINOPATHIES
HEMOGLOBIN C DISEASE
- Hemoglobin C is the second most common hemoglobinopathy in the United States and the
third
- most common worldwide.
- Like hemoglobin S, hemoglobin C is thought to have arisen as a response to malaria.
- Hemoglobin C has a substitution of lysine for glutamic acid at the sixth amino acid of the globin
chain. Like hemoglobin S, hemoglobin C is capable of polymerizing into crystals when
deoxygenated.
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 18
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
-
HEMOGLOBIN E DISEASE
- Like hemoglobins S and C, hemoglobin E is thought to have arisen as a consequence of
malaria.
- It has substitution of lysine for glutamic acid at position 26 of the β globin chain (26
Glu→Lys).
- Heterozygous hemoglobin E is clinically silent. The blood hemoglobin level is normal, but there
is mild microcytosis and prominent target cells on the blood smear.
- The most significant clinical syndrome associated with hemoglobin E is the double
heterozygous state for hemoglobin E and β-thalassemia, which presents as
thalassemia major.
-
HEMOGLOBIN H DISEASE
- The disease most frequently results from an absence of three of the four α-globin genes.
- Supravital staining with brilliant cresyl blue reveals multiple fine, deeply stained deposits (“golf
ball” cells) caused by precipitation of aggregates of β-globin chains.
HEMOGLOBIN D DISEASE
- Hemoglobin D is actually a heterogeneous group of β-globin chain mutations.
- The most significant variant is DLos Angeles (also known as DPunjab). It is significant because
heterozygotes for both hemoglobin S and DLos Angeles have a sickling illness resembling sickle
cell anemia.
HEMOGLOBIN G DISEASE
- Hemoglobin G is also heterogeneous and includes both α and β globin chain mutations.
- The most common hemoglobin G variant in the United States is GPhiladelphia which is an α chain
mutation that occurs in African Americans.
- Hemoglobin G is not usually associated with significant anemia or other clinical problems;
hemoglobin G does not interact with hemoglobin S.
- The electrophoresis pattern of hemoglobin G is similar to that of hemoglobin D.
HEMOGLOBIN LEPORE, [α2(δβ)2]
- Hemoglobin Lepore is a fusion protein caused by a crossing over between the genes
for the δ globin and the β globin chains.
SUMMARY:
MUST KNOW!!!!
Hgb S
Hgb C
Hgb E
Hgb D
C. THE THALASSEMIAS
- Characterized by a QUANTITATIVE ABNORMALITY OF GLOBIN CHAIN SYNTHESIS.
- The genetic mutation in thalassemia results in the absence of mRNA production from the
involved gene, production of a nonfunctional mRNA, or production of an unstable
mRNA that is prematurely degraded. The end result is decreased synthesis of the involved
globin chain.
- Thalassemias are, as a group, probably the most common genetic diseases in the world.
- DR. THOMAS COOLEY AND DR. PEARL LEE described the first cases of thalassemia disease
in North America in 1925.
NOTES:
- A microcytic anemia that is not due to iron deficiency is most likely THALASSEMIA
.The first step after identification of a microcytic anemia is to check the serum ferritin or serum
iron/transferrin/transferrin saturation.
The decrease in globin chain synthesis has two consequences
1. Decreased hemoglobin synthesis, resulting in anemia and microcytosis
2. Aggregation of the excess free globin chains produced by the non-thalassemic gene (α
chains in the case of β-thalassemia; β chains in the case of α -thalassemia). The aggregates
of unpaired globin chains attach to and damage the erythrocyte cell membrane, resulting in
hemolysis.
Complications of Thalassemias
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 19
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
1. Chronic anemia: Chronic anemia causes growth retardation, delayed sexual maturation,
cardiac dilatation and congestive heart failure, decreased work capacity, and all of the other
complications associated with chronic anemia.
2. Marked expansion of the bone marrow: The bone marrow becomes greatly expanded
due to marked erythroid hyperplasia. Widening of the diploic spaces in the skull gives a
characteristic “crewcut” or “hair on end” appearance on radiographs. Hypertrophy of the
frontal bones results in frontal bossing. Hypertrophy of the maxillae results in prominent
cheeks and dental malocclusions, giving a characteristic “chipmunk” facies. Thinning of the
cortex of the vertebrae and long bones results in fractures.
3. Extramedullary hematopoiesis causes ENLARGEMENT OF THE SPLEEN AND LIVER. Foci
of extramedullary hematopoiesis may occur in soft tissues (myeloid tumors), and paravertebral
masses may cause spinal cord compression.
4. IRON OVERLOAD: There is chronic hyperabsorption of iron by the gastrointestinal tract,
driven by the chronic erythropoiesis, and this is exacerbated by RBC transfusions. Iron
deposition in the heart causes cardiomyopathy and cardiac arrhythmias. Deposition in the liver
causes portal fibrosis and may result in hepatic cirrhosis. Patients with hepatic cirrhosis are at
risk of developing hepatocellular carcinoma (hepatoma).
5. CHRONIC HEMOLYSIS: Chronic hemolysis causes splenomegaly, hepatomegaly, and
bilirubin gallstones. Hypersplenism may develop, increasing transfusion requirements.
α-Thalassemia
- Most cases of α-thalassemia are due to deletions in the α globin genes.
- There are two genes for the α globin chain on chromosome 16; the mutation may involve only
one or both α genes on each chromosome.
1. Single-gene mutation (-α /αα ): Clinically silent, without microcytosis or anemia
2. Two-gene mutation (- α /- α or - - αα; α -thalassemia minor or α -thalassemia
trait ): Mild microcytic anemia; serious complications are uncommon
3. Three-gene mutation (- -/- α; hemoglobin H disease): Moderately severe,
microcytic anemia. The excess chains precipitate as γ4 tetramers (hemoglobin H).The
clinical picture is variable; patients may or may not have splenomegaly, iron overload,
and the skeletal complications seen in severe thalassemia.
4. Four-gene mutation (- - / - - hydrops fetalis): Incompatible with life. Most
pregnancies spontaneously terminate prematurely. Those infants that survive to
delivery have gross anasarca and usually die of congestive heart failure shortly after
birth. There is a high incidence of maternal preeclampsia during the pregnancy.
Note:
Hemoglobin constant spring
- An unusual form of the silent carrier state, has one deletion and represents an
mRNA termination defect.
- It is a hemoglobin formed from the combination of two structurally abnormal α chains, each
elongated by 31 amino acids at the carboxy-terminal end, and two normal β chains. The
homozygous state is phenotypically similar to mild a -thalassemia.
β-Thalassemia
- There is a single gene for the β globin chain on chromosome 11. Most mutations in β-
thalassemia are single-nucleotide substitutions. The mutation may result in a complete lack of
β chain synthesis (β 0-thalassemia) or a decrease in β chain synthesis (β +-thalassemia).
- Unlike α-thalassemia, the majority of genetic lesions are point mutations rather than gene
deletions. These mutations may be within the gene complex itself or in promoter or enhancer
regions.
- Children develop characteristic “chipmunk” facies due to maxillary marrow hyperplasia and
frontal bossing.
The β-thalassemias have been divided into three main clinical syndromes:
1. β -Thalassemia minor: Heterozygosity for β-thalassemia results in a mild clinical syndrome
designated β-thalassemia minor. The hemoglobin and the MCV are mildly or moderately
decreased (hemoglobin ~9–12 g/dL and MCV ~65–75 fL), and the patient has few symptoms
or complications.
2. β-Thalassemia major (Cooley’s anemia): Homozygosity for β-thalassemia results in a
severe clinical syndrome characterized by severe anemia and microcytosis (hemoglobin ~3–5
g/dL and MCV <65 fL), total or near total absence of Hb A, marked ineffective erythropoiesis,
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 20
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
marked expansion of the bone marrow with skeletal complications, splenomegaly, and iron
overload due to hyperabsorption of iron.
3. β-Thalassemia intermedia: β-Thalassemia intermedia is homozygous β-thalassemia that is
not transfusion dependent. It is genetically and clinically heterogeneous. The hemoglobin is
intermediate between β-thalassemia major and minor (~6–9 g/dL), as is the incidence of
clinical complications.
(A fourth category, β-thalassemia minima, is sometimes added for patients who have a normal
CBC but are identified as having β-thalassemia based on screening or family studies.)
Diagnosis of Hemoglobinopathies
1. HEMOGLOBIN ELECTROPHORESIS - The most common method used to diagnose
hemoglobinopathies which separates hemoglobins based on differences in size and
electrical charge.
a. ALKALINE ELECTROPHORESIS
- Has an alkaline ph (8.6)
- This method of separating hemoglobin fractions is based on the principle that
hemoglobin molecules in an alkaline solution have a net negative charge
and move toward the anode in an electrophoretic system.
- Those with a greater electrophoretic mobility than hemoglobin A at pH 8.6 are
classified as the fast hemoglobins.
- Examples of fast hemoglobins are Bart’s hemoglobin and the two fastest
variants, hemoglobin H and hemoglobin I.
- Hemoglobin C is the slowest common hemoglobin.
- Various media, such as paper, cellulose acetate, or starch blocks, and different
buffers may be used for electrophoresis.
- This technique separates the hemoglobin fractions S, F, A, C, and A2
b. Citrate Agar Electrophoresis
- This process takes place at an acid pH (6.1)
- In this method, hemoglobins are separated on the basis of a complex interaction
between hemoglobin, agar, and citrate buffer ions.
- Electrophoresis in citrate agar at an acid pH (acid citrate electrophoresis) is used to
separate hemoglobins that migrate to the same position on alkaline
electrophoresis (hemoglobin S from hemoglobin D or G; hemoglobin C from
hemoglobin O or E).
2. Kleihauer Betke
- A procedure commonly used to determine the amount of fetal blood that has
mixed with maternal blood following delivery.
- This test involves acid denaturation of hemoglobin.
- Result:
o Fetal haemoglobin (Hgb F) →resists denaturation
o Adult hemoglobin → sensitive to acid denaturation
- Elevated levels of hemoglobin F can be seen in beta-thalassemia, a form of anemia, and
paroxysmal nocturnal hemoglobinuria (PNH).
3. Chromatography
- Quantitation of hemoglobin A can be accomplished by cation exchange mini column
chromatography.
4. SICKLE CELL TESTS:
a. SODIUM DITHIONITE TEST/ SOLUBILITY TEST
i. Screening procedure for HgbS or any sickling
ii. Reagents:
1. Saponin- haemolytic agent
2. Sodium dithionite – reducing agent
3. Potassium phosphate-strong buffer
iii. (+) result: TUBIDITY (HgbS)
b. SOSIUM METABISULFITE/ SICKLING TEST
i. Formation of SICKLE SHAPED RED CELLS (+HgbS) upon contact with sodium
metabisulfite (reducing agent)
5. ISOPROPANOL TEST and HEAT PRECIPITATION TEST
a. For UNSTABLE HEMOGLOBINS
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 21
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
• If you are going to order hemoglobin electrophoresis, the patient should not have been transfused
for at least 90 days before the test is performed because transfused blood may make interpretation
of the electrophoresis difficult. Hemoglobin electrophoresis on infants can also be difficult to interpret
because of the physiologic elevation in fetal hemoglobin (hemoglobin F).
1. CELLULOSE ACETATE
- +
2. CITRATE AGAR
- +
7.HEMOLYTIC ANEMIAS
a. INHERITED HEMOLYTIC DISORDERS (intrinsic hemolytic anemia )
b. ACQUIRED HEMOLYTIC DISORDERs in which a factor outside the erythrocyte acts on it (extrinsic
hemolytic anemia)
INTRAVASCULAR EXTRAVASCULAR
Site of destruction of Within blood cells Spleen or liver
erythrocytes
Mechanism Activation of complement IgM Cell-mediated phagocytosis of
or IgG IgM-or IgG-coated cells
Laboratory findings Hemoglobinuria Positive DIRECT
Hemosiderinuria ANTIGLOBULIN TEST
Notes:
The main laboratory features of intratravascular hemolysis are as follows.
1. Hemoglobinemia and hemoglobinuria
2. Hemosiderinuria (iron storage protein in the spun deposit of urine)
3. Methemalbuminemia (detected spectrophotometrically by Schumm’s test).
INHERITED HEMOLYTIC ANEMIA
Etiology: Inherited hemolytic disorders may affect the basic membrane structure, the erythrocytic
enzymes, or the hemoglobin molecules within the red cell.
Examples of Inherited Hemolytic Anemias
A. Structural Membrane Defects
Hereditary spherocytosis Hereditary xerocytosis
Hereditary ellipitocytosis Rhnull disease
Hereditary stomatocytosis
B. Erythrocytic Enzyme Defects
G6PD deficiency Glutathione reductase
Pyruvate kinase deficiency Hexokinase
C. Defects of the Hemoglobin Molecule
Hb C disorder Hb S-S disorder (sickle cell anemia)
Hb S-C disorder Thalassemia
A. STRUCTURAL MEMBRANE DEFECT
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 22
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
Pathophysiology
- Structural proteins, forming the erythrocyte skeleton, are α and β-spectrin, actin, and protein
4.1
- Red cell band 3 is the major integral membrane protein that regulates exchange and
facilitates the transfer of CO2 from tissues to lungs.
- Ankyrin is the major connecting protein that links the membrane skeleton to the membrane
bilayer
.,
Mutations in any of the genes coding for the major membrane proteins can
1. Alter the amount or function of the expressed proteins
2. Compromise the integrity of the membrane
3. Contribute to abnormal erythrocyte morphology
HEREDITARY SPHEROCYTOSIS (HS)
- Results from the loss of erythrocytic membrane surface, as vesicles, due to decreased
membrane proteins linked to spectrin-ankyrin-band 3 associations and weak contacts between
spectrin and the negatively charged lipids of the inner half of the membrane bilayer.
- Hereditary spherocytosis (HS) is the most common inherited hemolytic anemia in
people of Northern European descent.
- the majority of cases result from mutations in the gene for ankyrin.
- The fundamental cause in most cases of HS is defective vertical attachment between the
phospholipid bilayer and the cytoskeleton scaffold, thus, the cell has a decreased surface-
area-to-volume ratio, which changes the shape of the cell from discoid to spherocyte.
- Spherocytes have reduced cellular flexibility. Spherocytic cells demonstrate an abnormal
permeability to sodium ion (Na+), causing an influx of sodium at 10 times the normal rate.
- Cholelithiasis, or the presences of gallstones, is a common complication of patients
with HS and occurs with greatest frequency in adolescents and young adults.
Laboratory investigations:
OSMOTIC FRAGILITY TEST
- Measure the ability of the red cell to take up fluid without lysing.
- The primary factor affecting OFT is the shape of RBCs (depends on the volume, surface area,
and functional state of RBC membrane)
o CODOCYTE=
o SPHEROCYTE=
- Specimen: HEPARINIZED BLOOD or DEFIBRINATED BLOOD
o Heparin must mantains blood pH at 7.4 which is required for the test
- Principle:
o Whole blood is added to varying concentration of buffered NaCl solution and allowed
to incubate at RT.
o The amount of HEMOLYSIS in each salne concentration is determined.
o IF RBCS are placed in an ISOTONIC SOLUTION (0.85% NaCl), fluid will neither enter
nor leave the RBC
o IF RBCs are placed in a HYPOTONIC SOLUTION, fluied enters the RBC until either
ruptures or an equilibrium is reached.
- RESULTS:
o First tube (trace hemolysis in the supernatant) = determined the beginning of
hemolysis
o First tube having the highest concentration of NaCl in which hemolysis is complete=
determined complete hemolysis
o Normally, hemolysis should be completed in 0.3 % NaCl, and beginning hemolysis
should not occur in a concentration over 0.45 % NaCl
Treatment
- The principal form of treatment is splenectomy although this should not be performed unless
clinically indicated because of anemia or gallstones because of the risk of post-splenectomy
sepsis, particularly in early childhood.
HEREDITARY ELLIPTOCYTOSIS (HE)
- Hereditary elliptocytosis is due to defective horizontal stability in the cytoskeleton. Most
cases are caused by mutations in spectrin, resulting in impaired assembly of the spectrin
tetramers. Since the spectrin tetramer assembly is defective, the cytoskeleton is less rigid and
more easily deformed.
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 23
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
SOUTH-EAST ASIAN OVALOCYTOSIS
- Variant of HE; common in Melanesia, Malaysia, Indonesia and the Philippines and is
caused by a nine amino acid deletion at the junction of the cytoplasmic and
transmembrane domains of the band 3 protein
HEREDITARY PYROPOIKILOCYTOSIS
- a subset of common hereditary elliptocytosis HE, seen primarily in blacks.
- It is manifested in infancy or early childhood as a severe hemolytic anemia with significant
poikilocytosis.
- One consequence is decreased thermal stability of the spectrin proteins (hence the
term “pyro,” meaning fire).
- Spectrin proteins from patients with HPP denature at approximately 45°C, whereas spectrin
from normal individuals denatures at approximately 49°C.
HEREDITARY STOMATOCYTOSIS
- Can be seen in the genetic hemoglobin defect, thalassemia, and in lead poisoning, HS, and
alcoholic cirrhosis.
- The cellular appearance stems from a cation abnormality, because the erythrocytes contain
increased sodium (Na+) and decreased potassium (K+). Because the intracellular
osmolality is exceeded and the intracellular concentration of cations increases, water enters
the cell and overhydrated erythrocytes take on the appearance of stomatocytes or
erythrocytes with a mouth-like opening.
- Osmotic fragility and autohemolysis are increased. Autohemolysis is partially
corrected with glucose and adenosine triphosphate (ATP).
- Splenectomy yields variable responses.
HEREDITARY XEROCYTOSIS
- Is a permeability disorder.
- In vitro, the thermal instability of spectrin suggests a defect in qualitative spectrin abnormality.
- The net loss of intracellular K exceeds the passive Na+ influx, yielding a net Na+ gain. This
causes the red cell to dehydrate.
- The osmotic fragility test is abnormal, especially after incubation. Autohemolysis is
increased and the hemolysis is not corrected with glucose.
Rhnull Disease
- Rhnull disease, or Rh deficiency syndrome, is a rare hereditary disorder causing mild,
compensated chronic hemolytic anemia.
- This disorder is associated with stomatocytosis, spherocytosis, and the deletion of all
Rh-Hr determinants including the Landsteiner-Weiner (LW) antigen from the red
blood cells.
- Many of the red blood cells are spheroidal or stomatocytic.
- Hemoglobin F levels are often elevated.
ACANTHOCYTOSIS
- Dense contracted or spheroidal red blood c ells with multiple thorny projections or spicules.
- Acanthocytes are prevalent in two very different constitutional disorders: abetalipoproteinemia
and spur cell anemia.
- Abetalipoproteinemia is a rare derangement of lipid metabolism resulting from a genetic
inability to synthesize apolipoprotein B (apoB), the protein that coats chylomicrons.
SPUR CELL HEMOLYTIC ANEMIA
- This form of acanthocyte-associated hemolytic anemia is seen in patients with established
alcoholic cirrhosis.
- Hemolysis usually becomes severe and may necessitate maintenance transfusions.
- Other causes of acanthocytosis can include neonatal hepatitis, infantile pyknocytosis,
the McLeod blood group, and severe malnutrition (e.g., anorexia nervosa).
NEUROACANTHOCYTOSIS
- Neuroacanthocytosis (NA) is a heterogeneous group of neurodegenerative disorders
associated with acanthocytosis in peripheral blood. Clinically, NA is characterized by a
combination of neurobehavioral changes. The cause of the disorder is unknown, but recent
evidence is increasing that the erythrocytic membrane is defective, with major integral
membrane protein band 3 being reported in a few cases.
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 24
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 25
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
ERYTHROCYTE MEMBRANE DEFECTS
PROTEINS HEMATOLOGIC TREATMENT
DISORDER INHERITANCE
INVOLVED MANIFESTATIONS
Hereditary Autosomal dominant Ankyrin most Spherocytes; increased osmotic Folic acid;
spherocytosis (HS) (majority) common; β spectrin, fragility; majority have mild to splenectomy for
α spectrin, band 3 moderate anemia but may have severe cases
Autosomal recessive protein, others exacerbations; autosomal recessive
HS is usually due to cases more severe
mutations in the α
spectrin gene
Hereditary Autosomal dominant α spectrin most Elliptocytes; majority None in majority of
elliptocytosis common asymptomatic, without anemia; cases
(HE) occasional severe anemia in
infancy
Hereditary Hereditary recessive α spectrin most Microcytosis, poikilocytosis, RBC Splenectomy
pyropoikilocytosis common fragments; moderate to severe
(HPP) anemia
Spherocytic Autosomal dominant Unknown Moderate hemolytic anemia; Splenectomy for
elliptocytosis elliptocytes and spherocytes on severe cases
smear; increased osmotic fragility
Southeast Asian Autosomal dominant Band 3 protein No hemolysis or anemia; increased None
ovalocytosis resistance to malarial infection
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 26
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 27
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
B. ERYTHROCYTIC ENZYME DEFECTS
- Erythrocytic enzyme defects are inherited.
- The anemias in this group are caused by deficiencies of
1. Glucose-6-phosphate dehydrogenase (G6PD)
2. Pyruvate kinase (PK)
3. Methemoglobin reductase
GLUCOSE-6-PHOSPHATE DEHYDROGENASE (G6PD DEFICIENCY)
- resistance to Falciparum malaria.
- Glucose 6-phosphate dehydrogenase (G6PD) is a housekeeping enzyme critical in the redox metabolism
of all aerobic cells and the most common aerobic erythrocyte enzyme deficiency.
- Glucose-6-Phosphate Dehydrogenase is the first enzyme in the hexose monophosphate shunt, which is
required to generate the reduced form of nicotinamide adenine dinucleotide phosphate (NADPH). NADPH is
required for the regeneration of glutathione by the enzyme glutathione reductase.
G6PD
Glucose-6-phosphate +NADP 6-phosphogluconate +NADPH
- An excess intermediate product, oxidized glutathione, accumulates in the red cell because of the absence of
NADPH and forms insoluble complexes with hemoglobin that result in Heinz body formation. This damages
the cell, resulting in hemolysis.
- The aggregates of oxidized hemoglobin are plucked out of the cell by the spleen, resulting in characteristic
“bite” or “blister” cells.
- The level of G6PD is HIGHEST IN RETICULOCYTES and declines with increasing age of the red cell.
- In normal cells, the half-life of the enzyme is approximately 62 days.
Clinical features: the main syndromes that occur are as follows.
1. Acute hemolytic anemia in response to oxidant stress, e.g. drugs, fava beans or infections. The acute
hemolytic anemia is caused by rapidly developing intravascular hemolysis with hemoglobinuria.
2. Neonatal jaundice
3. Rarely, a congenital non-spherocytic hemolytic anemia.
Agents that may cause hemolytic anemia in glucose-6-phosphate dehydrogenase (G6PD) deficiency
1. Infections and other acute illnesses (e.g, diabetic ketoacidosis)
2. Fava beans (possibly other vegetables): Uncooked fava beans are a notorious cause of hemolysis in
patients with G6PD Mediterranean (favism).
3. Drugs
Unsafe DRUGS:
Acetanilid Primaquine
Furazolidine Sulfa antibiotics
Nalidixic Acid Thiazolsulfone
Naphthalene Toluidine blue
Nitrofurantoin Trinitrotoluene
Phenazopyridine Doxorubicin
Phenylhydrazine
TEST:
ASCOBATE CYANIDE SCREENING TEST:
• NONSPECIFIC TEST detecting the deficiencies in HMP/PPP: G6PD def, GLUTATHIONE PEROXIDASE,
GLUTATHIONE REDUCTASE
• Reagents: Na carbonate, Na cyanide
• Normal: red
• Abn/Enz deficient: BROWN
G6PD FLUORESCENT SCREENING
• Normal: MAXIMUM FLUORESCENCE at 10 minsa
• Abn (G6PD def): Little or no fluorescence
PYRUVATE KINASE DEfiCIENCY
- Pyruvate kinase (PK) deficiency is the second most common RBC enzymopathy and the most common
enzyme deficiency in the Embden-Meyerhof (glycolytic) pathway.
- However, it is far less common than G6PD deficiency. It occurs most commonly in people of Northern European
and Mediterranean descent.
- Jaudice is usual and gallstones frequent. Frontal bossing may be present. The blood film shows poikilocytosis
and distorted “prickle” cells, particularly post-splenectomy.
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 28
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
METHEMOGLOBIN REDUCTASE DEFICIENCY
- Hemoglobin that is oxidized from the ferrous to the ferric valency state is called methemoglobin. Approximately
1% of circulating hemoglobin in normal individuals is methemoglobin.
- Hereditary deficiency of the enzyme NADH-methemoglobin reductase results in increased levels of
methemoglobin.
- A deficiency in the enzyme, also called NADH diaphorase, can result from inheritance of an autosomal
recessive trait or in conjunction with hemoglobin M disease, or as a result of exposure to toxic substances or
various drugs.
- The predominant clinical manifestation of methemoglobin reductase deficiency is cyanosis because the
methemoglobin cannot carry oxygen to the tissues.
Other Red Blood Cell Enzyme Deficiencies
Glucosephosphate isomerase deficiency: causes an abnormality in anaerobic glycolysis and is the third most common
red blood cell enzyme deficiency
HEMATOLOGIC OTHER
ENZYME INHERITANCE
MANIFESTATIONS MANIFESTATIONS
Glucose Autosomal Neonatal
phosphoisomerase recessive hyperbilirubinemia;
Hemolytic anemia of
variable severity
Gluthathione Autosomal Hemolytic anemia Metabolic acidosis
synthetase recessive
Hexokinase Autosomal Hemolytic anemia
recessive
Phosphofructokinase Autosomal Hemolytic anemia Glycogen storage
recessive disease
Aldolase Autosomal Hemolytic anemia Glycogen storage
recessive disease
Phosphoglycerokinase X-linked Hemolytic anemia Mental retardation;
myoglobinuria
Triosephosphate Autosomal Hemolytic anemia Progressive neurologic
isomerase recessive abnormalities
Pyrimidine 5’ Autosomal Hemolytic anemia with
nucleotidase recessive prominent basophilic
stippling
ACQUIRED HEMOLYTIC ANEMIA
Etiology: Acquired hemolytic anemias can be classified according to the agent or condition responsible for inducing
the hemolysis. A major distinction exists between acute hemolysis of red cells, which results from damage done
directly to the cell membrane, and hemolytic anemias caused by immunologic responses.
Examples of Agents and Conditions Associated With Acquired Hemolytic Anemias
A. CHEMICALS, DRUGS, VENOMS
Aniline Nitrobenzene
Copper (Wilson disease) Phenacetin
Lead from gasoline or paint Phenol derivatives
Naphthalene (found in moth balls) Resorcinol and Sulfonamides
B. MICROORGANISMS
Bacteria: Clostridium sp., cholera, E. coli O157:H7, typhoid fever
Protozoa: Leishmania, malaria (Plasmodium sp.), toxoplasmosis
C. IMMUNE MECHANISMS (ANTIBODIES)
Autoimmune anemia due to cold- Idiopathic
reactive antibodies
Cold hemagglutinin disease Secondary
Idiopathic or secondary Lymphoproliferative disorders (CLL, malignancies,
systemic lupus erythematosus, viruses)
Paroxysmal cold hemoglobinuria Hemolytic disease of the fetus and newborn (HDFN)
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 29
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
Autoimmune anemia due to warm- Incompatible blood transfusion
reactive antibodies
Drug induced Paroxysmal nocturnal hemoglobinuria
D. AGENTS
Severe burns
E. TRAUMATIC AND MICROANGIOPATHIC HEMOLYTIC ANEMIAS
Disseminated intravascular coagulation Prosthetic cardiac valves
E. coli O157:H7 Thrombotic thrombocytopenic purpura (TTP)
Hemolytic uremic syndrome
Acquired hemolytic anemias
- the acquired hemolytic anemias (with one exception) involve abnormalities that are extrinsic to the
erythrocyte. The exception to the acquired = extrinsic rule is Paroxysmal Nocturnal Hemoglobinuria
(PNH), which is an acquired genetic lesion resulting in increased susceptibility of red blood cells (RBCs) to
hemolysis by the complement cascade.
- the clues that with an acquired hemolytic anemia are an INCREASED RETICULOCYTE COUNT (or
reticulocyte production index), INCREASED BILIRUBIN AND LACTIC DEHYDROGENASE , and
DECREASED HAPTOGLOBIN
IMMUNE HEMOLYTIC ANEMIAS
- The easiest way to approach the immune hemolytic anemias is to divide them according to the mechanism of
hemolysis and the type of mediating antibody:
1. Direct complement-mediated (intravascular) hemolysis versus phagocytosis by
macrophages of the reticuloendothelial system (extravascular hemolysis)
Immune hemolytic anemias can be further divided into:
AUTOIMMUNE HEMOLYTIC ANEMIAS
Associated with warm-type antibodies
Associated with cold-type antibodies
Associated with both warm- and cold-type antibodies
ISOIMMUNE HEMOLYTIC ANEMIAS
Hemolytic Disease of the fetus and newborn (HDFN)
Rh incompatibility
ABO incompatibility
DRUG-INDUCED HEMOLYTIC ANEMIA
Adsorption of immune complexes to red cell membrane
Adsorption of drug to red cell membrane
Induction of autoantibody to drugs
Non-immunological adsorption of immunoglobulin to red blood cell membrane
A. COLD-REACTIVE IMMUNE HEMOLYTIC ANEMIA
- Cold-reactive immune hemolytic anemia is generally mediated by IgM antibodies that react maximally at
approximately 4 to 18°C.
- IgM antibodies may cause intravascular hemolysis if the antibody is present in high titer; more often hemolysis
is extravascular, predominantly in the liver.
- IgM antibodies are large and can bridge the distance between two RBCs; thus, IgM antibodies by themselves
are able to agglutinate RBCs. (In contrast, IgG antibodies are smaller and alone are not able to agglutinate
RBCs.)
- There are many causes of cold-reactive immune hemolytic anemia. Most of these fall into the category of
cold agglutinin disease. Cold agglutinin disease, in turn, is divided into primary (idiopathic) and
secondary forms. Cold-reactive immune hemolytic anemia is less common than the warm-reacting type,
accounting for approximately 10 to 20% of immune hemolytic anemias.
Causes of Cold-Reactive Immune Hemolytic Anemia
1. COLD AGGLUTININ DISEASE
a. Primary
b. Secondary
b.1. Infections
b.2. Autoimmune disorders
b.3. Lymphoproliferative disorders
Primary (Idiopathic) Cold Agglutinin Disease
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 30
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
- Occurs with no obvious precipitating cause. It usually occurs in older individuals (peak age about 70 years)
and is more common in women than men. The course is usually chronic, lasting for months or years.
- The anemia associated with idiopathic cold agglutinin disease is usually modest; the main symptoms are
related to agglutination of erythrocytes on exposure to cold rather than the anemia. Agglutination occurs
in the fingers, toes, nose, and ears and causes cyanosis of those areas (acrocyanosis).
- Some patients have a lymphoproliferative disorder such as chronic lymphocytic leukemia (CLL),
Waldenström’s macroglobulinemia, or non-Hodgkin’s lymphoma.
- The antibody is monoclonal, usually IgM with kappa light chain (IgM). Primary cold agglutinin disease thus
represents a monoclonal gammopathy.
Secondary Cold Agglutinin Disease
- Cold agglutinin disease (CAD) is most often related to infections, primarily Mycoplasma pneumoniae
or Epstein-Barr virus (EBV) (infectious mononucleosis).
- It can occasionally occur with other viral infections (adenovirus, cytomegalovirus, rubella, mumps, HIV),
bacterial infections (Legionella, Escherichia coli, Listeria), malaria, syphilis, and others.
- The patients are usually young and otherwise healthy. The onset is abrupt, usually as the infection is
resolving. The patients present with pallor, jaundice, and the other signs of acute hemolytic anemia.
Massive acute intravascular hemolysis and acute renal failure may occur but are fortunately rare.
- The antibodies are polyclonal and usually directed against the “I/i blood group”. The antibody is usually
IgM and binds to red cells best at 4°C. IgM antibodies are highly efficient at fixing complement and both
intravascular and extravascular hemolysis can occur.
Laboratory Testing:
1. The direct antiglobulin test (DAT or direct Coombs’ test) tests for antibody or complement on the
patient’s RBCs. The direct antiglobulin test uses the patient’s cells and adds a reagent serum.
- It is performed by adding antibodies directed against either human IgG, complement components, or both
(the antiglobulin or Coombs’ reagent) to the patient’s RBCs and seeing if the cells agglutinate.
- If there is IgG or complement on the surface of the RBCs, then the added antibodies will cause the cells
to agglutinate (positive DAT). If there is no IgG or complement on the RBC surface, the cells will not
agglutinate.
- In cold agglutinin disease, there is complement on the patient’s RBCs but no immunoglobulin.
2. The antibody screen (also called indirect antiglobulin test or indirect Coombs’ test) tests for
unexpected anti-erythrocyte antibodies in the patient’s serum. The patient’s serum is added to panels of
reagent red cells.
- After the cells and serum have incubated, the cells are washed and an antiglobulin reagent is added. If
there are unexpected antibodies in the patient’s serum, the reagent cells will agglutinate; otherwise, the
reagent cells do not agglutinate.
- Unexpected antibodies are those that should not be present in a normal person; for example, antibodies
against the A or B blood group antigens would be expected in a person who lacks those antigens.
Antibodies against other RBC agents would be unexpected.
- In cold agglutinin disease, there is usually an unexpected antibody in the patient’s serum that reacts best
at cold temperatures.
2. PAROXYSMAL COLD HEMOGLOBINURIA (PCH)
➪ Do not confuse cold agglutinins with cryoglobulins. Cold agglutinins are antibodies that cause agglutination
of erythrocytes at cold temperatures. Cryoglobulins are antibodies that aggregate at cold temperatures (no
erythrocytes involved).
- It is caused by a peculiar biphasic IgG antibody that reacts and fixes complement at cold temperatures.
After rewarming, the complement cascade goes to completion with formation of the membrane attack complex
and intravascular hemolysis due to complement lysis.
- The antibody has been designated the Donath-Landsteiner antibody and is usually directed against the “P”
blood group antigen.
- Syphilis used to be the most common cause, but now most cases occur in children, and are related to viral
infection (measles, measles vaccine, mumps, adenovirus, EBV, cytomegalovirus) or Mycoplasma
pneumoniae. Occasional cases are related to systemic lupus erythematosus (SLE).
- Paroxysmal cold hemoglobinuria is a relatively common cause of acute hemolytic anemia in children
➪ Warning: Do not confuse paroxysmal cold hemoglobinuria (PCH) with paroxysmal nocturnal hemoglobinuria
(PNH).
Three clinical forms of Paroxysmal cold hemoglobinuria:
1. An acute form that follows an infection
2. A chronic form associated with tertiary or congenital syphilis
3. A chronic idiopathic form.
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 31
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
B. WARM-REACTIVE IMMUNE HEMOLYTIC ANEMIA
- More common than the cold reactive variant (at least 70% of immune hemolytic anemias).
- It can be primary (idiopathic), secondary to a wide variety of different conditions, or drug-related. The
idiopathic variety is more common in women and the older population.
Pathophysiology
- The antibody is usually a “panagglutinin,” meaning that the patient’s antibody will react with virtually all
cells. In most cases, the antibody appears to be recognizing some antigen in the Rh blood group system,
although it is usually impossible to define a specific antigenic reactivity.
- The antibody is almost always an IgG. Occasionally, an IgA or IgM antibody will be seen along with the IgG
or, exceptionally, alone. When the cells are coated with IgG and complement (C3d, the degraded fragment
of C3) or complement alone, red cell destruction occurs more generally in the RE system.
- Red cell destruction is primarily by phagocytosis by splenic macrophages. In many cases, the phagocytosis is
partial rather than complete;
Clinical features
- The disease may occur at any age, in both sex and presents as a hemolytic anemia of varying severity.
- The spleen is often enlarged. The disease tends to remit and relapse. It may occur alone or in association
with other diseases, or arise in some patients as a result of methyldopa therapy.
- When associated with idiopathic thrombocytopenic purpura (ITP), which is a similar condition affecting
platelets, it is known as Evans’ syndrome.
Causes of Warm-Reactive Immune Hemolytic Anemia
1. Primary (Idiopathic)
2. Secondary
a. Infections
b. Autoimmune disorders: SLE, Rheumatoid arthritis
c. Lymphoproliferative disorders: CLL, non-Hodgkin’s lymphomas, myeloma
d. Hodgkin’s lymphoma
e. Thymoma
f. Ovarian dermoid cyst or teratoma
g. Carcinomas
h. Hypogammaglobulinemia
i. AIDS
3. Drug related
C. DRUG-RELATED IMMUNE HEMOLYTIC ANEMIA
- Drugs and medications are common causes of immune hemolytic anemia (~10–20% of cases).
- The hemolysis is almost always of the warm-reactive type.
- It is common for patients on a variety of medications to develop a positive DAT; however, actual hemolysis is
rare.
Three mechanisms of drug-related immune hemolytic:
1. Drug adsorption (penicillin) type
- The drug binds tightly to the RBC surface, and an antidrug antibody reacts with the drug that is bound to
the red cell.
- The DAT is positive for IgG, with or without complement.
- Hemolysis is usually extravascular in the spleen; rarely, there may be intravascular hemolysis if the
antibody fixes complement. The hemolysis is usually subacute, not severe.
2. Neoantigen (formerly called immune complex) type
- There is a complex of drug and antidrug antibody, which binds to an antigen on the red cell. The antibody
can be either IgM or IgG and is often complement fixing.
- The antibody often has relatively low avidity; it binds to the complex on the cell membrane, fixes
complement, and then dissociates from the cell surface.
- The DAT is therefore positive for complement but usually not for immunoglobulins.
- Hemolysis is usually intravascular, often sudden and severe, and maybe associated with acute renal
failure. The reaction may occur with low doses of the medication.
- Medications that can cause this type of reaction include cephalosporin antibiotics, quinine, quinidine, and
stibophen.
3. Autoimmune (-methyldopa) type
- Methyldopa (Aldomet) is capable of inducing an autoimmune reaction.
- The antibody is directed against a red cell antigen, not against the drug itself.
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 32
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
- The characteristics are similar to those of idiopathic warm-reactive immune hemolytic anemia.
- The DAT is positive for IgG with or without complement and may be positive even in the absence of the
drug. The antibody screen may be positive.
- A similar reaction can be seen with levodopa and procainamid
NON-IMMUNE ACQUIRED HEMOLYTIC ANEMIAS
A. Mechanical Trauma
1. Malfunctioning mechanical heart valve
2. “March hemoglobinuria”
- Can occur during long marches or marathons, resulting from erythrocytes being crushed in the
capillaries of the soles of the feet as they pound against the surface.
- This can be prevented by wearing thicker socks and softer-soled shoes.
3. Microangiopathic hemolytic anemias (sometimes called thrombotic microangiopathies ):
thrombotic thrombocytopenic purpura (TTP), hemolytic-uremic syndrome (HUS), preeclampsia/eclampsia,
malignant hypertension, disseminated intravascular coagulation (DIC)
- Fibrin strands form within the capillaries, slicing erythrocytes into fragments as they pass through.
B. Acanthocytosis
1. Hereditary abetalipoproteinemia
2. End-stage liver disease
3. Severe starvation, anorexia nervosa
C. Severe Hypophosphatemia
1. Intravenous hyperalimentation lacking phosphorous supplementation
2. Severe starvation
3. Alcoholism
4. Prolonged therapy with phosphate-binding antacids
D. Wilson’s disease; copper poisoning
- Due to a mutation in the gene for ceruloplasmin, a copper transport protein. Patients accumulate excessive
amounts of copper in their tissues, particularly the liver. Some patients with Wilson’s disease develop an
abrupt onset of hemolysis due to sudden release of copper from the liver.
- Excess inorganic copper damages RBC membranes, disrupts cellular metabolism, and accelerates the
oxidation of hemoglobin, all of which result in decreased cell survival.
- Hemolytic episodes tend to occur relatively early in the course of Wilson’s disease, often in the patient’s
twenties, and may be the initial symptomatic manifestation of the disease.
- Hemolytic episodes are usually transient and self-limited but may be recurrent and severe.
E. Oxidative drugs or chemicals
- Examples of drugs that have been implicated include sulfonamides, phenazopyridine (Pyridium),
nitrofurantoin (Furadantin), phenacetin, and cisplatin.
- Chemicals that have been implicated in hemolysis include chlorates, nitrates, naphthalene
(mothballs), methylene blue, and others.
- Treatment is to stop the drug or exposure and provide support as necessary.
F. Severe burns
G. Venoms
1. Brown recluse spider
2. Snakes (cobras)
H. Infections
1. Direct infection of erythrocytes: malaria, babesiasis, bartonellosis, trypanosomiasis
2. Clostridium perfringens septicemia
3. Other: gram-positive and gram-negative septicemia, leptospirosis, Borrelia, others
PAROXYSMAL NOCTURNAL HEMOGLOBINURIA (PNH)
- PNH is a rare, acquired, clonal disorder of marrow stem cells in which there is deficient synthesis of the
glycosylphosphatidylinositol (GPI) anchor, a structure that attaches several surface proteins to the cell
membrane.
- It results from mutations in the X chromosome gene coding for phosphatidylinositol glycan protein A
(PIG-A) which is essential for the formation of the GPI anchor.
- The lack of surface molecules decay-activating factor (DAF, CD55) and membrane inhibitor of reactive
lysis (MIRL, CD59) render red cells sensitive to lysis by complement and the result is chronic intravascular
hemolysis.
- Chronic intravascular hemolysis of PNH is mediated by the alternative pathway of complement.
Diagnosis of PNH
- The traditional diagnostic tests are the :
o SUCROSE HEMOLYSIS TEST /SUGAR WATER TEST
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 33
CLINICAL HEMATOLOGY PREPARED BY: KENNETH ART CLOSA NARAG, RMT
▪ SCREENING
▪ Based on the principle that sucrose provides a medium of low ionic strength and promotes
binding of complememt to RBCs
▪ (+) hemolysis
o ACIDIFIED SERUM TEST
▪ CONFIRMATORY
▪ Based on the principle that acidified serum activates complement by the alternative pathway
▪ (+) hemolysis
- Demonstration of a decreased expression of GPI-anchored proteins on RBCs or leukocytes by flOW
CYTOMETRY has been shown to be more sensitive than either of these tests.
TEMPLATE 07//CLINICAL HEMATOLOGY // KENNETH ART CLOSA NARAG, RMT 34
You might also like
- Anemia in TropicsDocument7 pagesAnemia in TropicsAsnaafii BantiiNo ratings yet
- MEDSEM2LE4 Approach To AnemiaDocument19 pagesMEDSEM2LE4 Approach To AnemiaAndrea Ann MagpayoNo ratings yet
- Abnormal HBDocument55 pagesAbnormal HBtofyNo ratings yet
- Hemolytic AnemiaDocument81 pagesHemolytic AnemiaL3mi DNo ratings yet
- HaematologyDocument62 pagesHaematologyManmeet SNo ratings yet
- Hemato 2Document54 pagesHemato 2toot aliNo ratings yet
- Ha I by AbdifatahDocument109 pagesHa I by AbdifatahAbdifatah AhmedNo ratings yet
- Hemolytic AnemiaDocument99 pagesHemolytic AnemiaSagar Chandrakant Mhetre100% (3)
- How To Interpret HEMATOLOGY Test ResultsDocument36 pagesHow To Interpret HEMATOLOGY Test Resultssylvia haryantoNo ratings yet
- M.03 Hemolytic AnemiaDocument5 pagesM.03 Hemolytic AnemiaRaymund AldabaNo ratings yet
- 1 Erythrocytic DisordersDocument6 pages1 Erythrocytic DisorderschippaiqweqweNo ratings yet
- Disorders of Red Blood: CellsDocument4 pagesDisorders of Red Blood: CellsIberisNo ratings yet
- Anemia: Dr. Tanbira Alam MBBS, M.PhilDocument22 pagesAnemia: Dr. Tanbira Alam MBBS, M.Philsatvindar_muNo ratings yet
- Hemolytic Anemia-Pediatric MasterDocument62 pagesHemolytic Anemia-Pediatric MasterPedia 2020No ratings yet
- Anemia DIC NotesDocument6 pagesAnemia DIC NotesJeanna ChongNo ratings yet
- Macrocytic AnemiaDocument49 pagesMacrocytic AnemiaANo ratings yet
- Hematology System Problems WorksheetDocument7 pagesHematology System Problems WorksheetJennNo ratings yet
- Anemia OsamaDocument57 pagesAnemia Osamaosamafoud7710No ratings yet
- Introduction To Hemolytic Anemia OkDocument26 pagesIntroduction To Hemolytic Anemia OkNayana M RNo ratings yet
- Hemolytic Anemia Inherited: Hematologi-Onkologi Division Child Departement - Fkusu/RshamDocument56 pagesHemolytic Anemia Inherited: Hematologi-Onkologi Division Child Departement - Fkusu/RshamMarcelliaNo ratings yet
- Systematic Plan For The Diagnosis of AnaemiaDocument31 pagesSystematic Plan For The Diagnosis of AnaemiaAriyike OmoobaNo ratings yet
- Anemia OsamaDocument57 pagesAnemia Osamaosamafoud7710No ratings yet
- Finals Week 10Document8 pagesFinals Week 10MARIE NELLIE MOSTRADONo ratings yet
- HEMADocument44 pagesHEMAJilycamae COSMODNo ratings yet
- Subject: Anemia - Defects of Red Blood Cell Membrane Production Discipline: PhysiopathologyDocument30 pagesSubject: Anemia - Defects of Red Blood Cell Membrane Production Discipline: PhysiopathologyCristina Teodora BerbecaruNo ratings yet
- Hematologic SystemDocument39 pagesHematologic SystemESPINOSA JHANNANo ratings yet
- Anaemia: What Is Anemia?Document21 pagesAnaemia: What Is Anemia?Rashed ShatnawiNo ratings yet
- Physiology Group 2Document58 pagesPhysiology Group 2Akinmade AyobamiNo ratings yet
- BMLT Class Note On Anemia ClassificationDocument2 pagesBMLT Class Note On Anemia ClassificationSubhasish BarikNo ratings yet
- Normocytic AnemiaDocument16 pagesNormocytic AnemiaPaula ArayaNo ratings yet
- SBRC HematologyOncology 1Document80 pagesSBRC HematologyOncology 1dalia khamoNo ratings yet
- Hemolytic Anemias and Acute Blood Loss: AnemiaDocument4 pagesHemolytic Anemias and Acute Blood Loss: AnemiaAjay Pal NattNo ratings yet
- Quick Notes - ANEMIADocument3 pagesQuick Notes - ANEMIAWispy NotesNo ratings yet
- Approach To Blood and Hemopoietic DiseasesDocument168 pagesApproach To Blood and Hemopoietic DiseasesAgung CahyonoNo ratings yet
- Anemia and Red Blood Cell Disorder Lecture by Dr. Rosales (Nov 6, 2017)Document7 pagesAnemia and Red Blood Cell Disorder Lecture by Dr. Rosales (Nov 6, 2017)Ian Gabrielle Mercado CuynoNo ratings yet
- Anemia Its Laboratory DiagnosisDocument146 pagesAnemia Its Laboratory DiagnosisCh M MushahidNo ratings yet
- Lecture 2 - Clinical Pathology - AnemiaDocument56 pagesLecture 2 - Clinical Pathology - AnemiaSamuel GitongaNo ratings yet
- Anemia Approach S.elyaDocument51 pagesAnemia Approach S.elyaAnonymous JqvBHcsYrENo ratings yet
- Anemia IntroductionDocument40 pagesAnemia IntroductionRazaz AdilNo ratings yet
- Sickle Cell Disease ManagementDocument23 pagesSickle Cell Disease ManagementAndrew SilungweNo ratings yet
- Anemia HemolitikDocument37 pagesAnemia HemolitikBintang Ruth Cecilia FebrinaNo ratings yet
- Hemolytic AnemiasDocument59 pagesHemolytic AnemiasRajesh darlingNo ratings yet
- Anemia: Bariq. J .Hassan Wael MohanDocument34 pagesAnemia: Bariq. J .Hassan Wael MohanhaiderNo ratings yet
- Ceva de HematoDocument5 pagesCeva de HematoPana NicolaeNo ratings yet
- AnemiaDocument16 pagesAnemiaAaron GarciaNo ratings yet
- PANCYTOPENIADocument51 pagesPANCYTOPENIAResmyNo ratings yet
- Blood Disorders Seminar No 7Document142 pagesBlood Disorders Seminar No 7Hysum Mushtaq100% (1)
- Davao Doctors College Medical Laboratory Science Department Student Notes: Hema 1 Warm Autoimmune Hemolytic AnemiaDocument3 pagesDavao Doctors College Medical Laboratory Science Department Student Notes: Hema 1 Warm Autoimmune Hemolytic AnemiaMichelle San Miguel FeguroNo ratings yet
- BloodDocument142 pagesBloodChelleyOllitroNo ratings yet
- SGL 2 (Hemolytic Anemia & Hemoglobinopathies)Document53 pagesSGL 2 (Hemolytic Anemia & Hemoglobinopathies)raman mahmudNo ratings yet
- Califmed00232 0012Document5 pagesCalifmed00232 0012Vale SportsNo ratings yet
- Nephrotic and Nephritic Syndrome: Med5010 LectureDocument65 pagesNephrotic and Nephritic Syndrome: Med5010 LectureFreeburn Simunchembu100% (1)
- Polycythemia Vera ReportDocument31 pagesPolycythemia Vera ReportAdrianNo ratings yet
- Anaemia - OverviewDocument3 pagesAnaemia - OverviewAqsa YounisNo ratings yet
- Haemolytic Anemia: Dr. Sookun Rajeev K (MD) Dept of General Medicine Anna Medical CollegeDocument11 pagesHaemolytic Anemia: Dr. Sookun Rajeev K (MD) Dept of General Medicine Anna Medical CollegeshravaniNo ratings yet
- AnemiaDocument26 pagesAnemiaJoel CanenciaNo ratings yet
- Patho FinaaaaalllDocument15 pagesPatho FinaaaaalllIvin SajithNo ratings yet
- 3-T and Sicke Cell Disease 2016Document68 pages3-T and Sicke Cell Disease 2016ThaveeshaLindsayWhiteNo ratings yet
- Approach To Hemolytic AnemiaDocument63 pagesApproach To Hemolytic AnemiaSarath Menon R100% (2)
- Dna Polymorphism and Human IdentificationDocument5 pagesDna Polymorphism and Human Identificationmarie judimor gomezNo ratings yet
- IMMUNOASSAYDocument31 pagesIMMUNOASSAYmarie judimor gomezNo ratings yet
- LibraryDocument2 pagesLibrarymarie judimor gomezNo ratings yet
- Thesis QuestionaireDocument3 pagesThesis Questionairemarie judimor gomezNo ratings yet
- Research MCNPDocument57 pagesResearch MCNPmarie judimor gomezNo ratings yet
- Tumor ImmunologyDocument15 pagesTumor Immunologymarie judimor gomezNo ratings yet
- Hema 1 ErythropoiesisDocument20 pagesHema 1 Erythropoiesismarie judimor gomezNo ratings yet
- Library Collection InventoryDocument1 pageLibrary Collection Inventorymarie judimor gomezNo ratings yet
- Library Inventory CollectionDocument2 pagesLibrary Inventory Collectionmarie judimor gomezNo ratings yet
- Library ActivityDocument2 pagesLibrary Activitymarie judimor gomezNo ratings yet
- TTL 1 Prelims Handouts Part1Document15 pagesTTL 1 Prelims Handouts Part1marie judimor gomezNo ratings yet
- Lesson 1 Introduction To TTLDocument38 pagesLesson 1 Introduction To TTLmarie judimor gomezNo ratings yet
- Ces Library InventoryDocument1 pageCes Library Inventorymarie judimor gomezNo ratings yet
- FECALYSISDocument21 pagesFECALYSISmarie judimor gomezNo ratings yet
- Assessmen T Diagnosi S Planning Intervention S Rational E Evaluatio NDocument3 pagesAssessmen T Diagnosi S Planning Intervention S Rational E Evaluatio Nmarie judimor gomezNo ratings yet
- Anti-Terrorism Is UnconstitutionalDocument5 pagesAnti-Terrorism Is Unconstitutionalmarie judimor gomezNo ratings yet
- Anemia - AmbossDocument10 pagesAnemia - AmbossGuga XachidzeNo ratings yet
- Clinical Pathology MCQs and Ansewrs PDFDocument29 pagesClinical Pathology MCQs and Ansewrs PDFAmeer MattaNo ratings yet
- Drug Treatment of AnemiasDocument29 pagesDrug Treatment of AnemiasKashmalaNo ratings yet
- Management of Aplastic Anemia in PregnancyDocument4 pagesManagement of Aplastic Anemia in PregnancyAhmad NajmiNo ratings yet
- Physiology: Under Graduate MaterialsDocument416 pagesPhysiology: Under Graduate Materialskrithika sathishNo ratings yet
- Practical Pediatric HematologyDocument350 pagesPractical Pediatric Hematologylovelots1234100% (5)
- Types of Anaemia and How To Remember Them: With Sophie BroughtonDocument28 pagesTypes of Anaemia and How To Remember Them: With Sophie BroughtonurtikikeNo ratings yet
- Samplex Aug2021-Dec2021Document162 pagesSamplex Aug2021-Dec2021Christian TayagNo ratings yet
- A Diagnostic Approach To Macrocytic AnemiaDocument87 pagesA Diagnostic Approach To Macrocytic AnemiaRathod arvinNo ratings yet
- POIKILOCYTESDocument8 pagesPOIKILOCYTESGail IbanezNo ratings yet
- Haematology: Normal Sequence of Development of Cells of Haematopoietic SystemDocument71 pagesHaematology: Normal Sequence of Development of Cells of Haematopoietic SystemMaxamed AadanNo ratings yet
- Workineh Case Studyy 1Document17 pagesWorkineh Case Studyy 1HABTAMU MOLLANo ratings yet
- Harr 5th EdDocument15 pagesHarr 5th EdTrixia UrsuaNo ratings yet
- Hematology 1 Module and Laboratory MannualDocument255 pagesHematology 1 Module and Laboratory MannualPALATTAO, AUBRIE L. BSMT2-8No ratings yet
- Hematology Week 8Document3 pagesHematology Week 8Rose Neil LapuzNo ratings yet
- Anemia DX TXDocument2 pagesAnemia DX TXProsanjit MajumderNo ratings yet
- 8 Morphology and InclusionsDocument31 pages8 Morphology and InclusionsLian Marie ViñasNo ratings yet
- SEPTEMBER 6, 2021 Hematology Assessment: Characteristic FeaturesDocument23 pagesSEPTEMBER 6, 2021 Hematology Assessment: Characteristic FeaturesChristian John V. CamorahanNo ratings yet
- Lee EllenCLPC Spring 2017 - CBC ColorDocument13 pagesLee EllenCLPC Spring 2017 - CBC ColorChristine Joy MolinaNo ratings yet
- Anaemia: DR Adjugah J. U. B. Med Sci (Physiology), MBBS, FMCFM, Mph. Consultant Family PhysicianDocument78 pagesAnaemia: DR Adjugah J. U. B. Med Sci (Physiology), MBBS, FMCFM, Mph. Consultant Family PhysicianAkwu AkwuNo ratings yet
- Atlas of Clinical HematologyDocument146 pagesAtlas of Clinical HematologyMaath Khalid100% (11)
- What Is Vitamin B12 Good For: Vitamins Vitamin B Niacin Folic Acid Vitamin B12Document75 pagesWhat Is Vitamin B12 Good For: Vitamins Vitamin B Niacin Folic Acid Vitamin B12Nanda SuchirNo ratings yet
- Journal Homepage: - : IntroductionDocument12 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- RBCDocument26 pagesRBCPriyanka RameshNo ratings yet
- Macrocytic AnemiaDocument48 pagesMacrocytic AnemiaMONo ratings yet
- April 25, 2007 SNB Questions: ND RD RD TH RD TH TH TH TH TH TH TH TH TH TH THDocument36 pagesApril 25, 2007 SNB Questions: ND RD RD TH RD TH TH TH TH TH TH TH TH TH TH THAnna Dianelli Masicap82% (11)
- Anemia GravisDocument35 pagesAnemia GravisMufthifina AulahaqNo ratings yet
- Diagnosis of AnemiaDocument14 pagesDiagnosis of AnemiaAnggie AnggriyanaNo ratings yet
- Hematology Mudit Khanna PDFDocument40 pagesHematology Mudit Khanna PDFSylvia DiamondNo ratings yet
- Classification of Anemia OkDocument60 pagesClassification of Anemia OkAnonymous 7CnBF0cjNo ratings yet
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (5)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (39)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (84)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeFrom EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeRating: 4.5 out of 5 stars4.5/5 (3)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (44)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (267)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- I Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionFrom EverandI Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionNo ratings yet
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (39)
- The Fun Habit: How the Pursuit of Joy and Wonder Can Change Your LifeFrom EverandThe Fun Habit: How the Pursuit of Joy and Wonder Can Change Your LifeRating: 4.5 out of 5 stars4.5/5 (19)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- The Story of Philosophy: The Lives and Opinions of the Greater PhilosophersFrom EverandThe Story of Philosophy: The Lives and Opinions of the Greater PhilosophersNo ratings yet