Professional Documents
Culture Documents
MEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th Edition
Uploaded by
MeryPinkihanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th Edition
Uploaded by
MeryPinkihanCopyright:
Available Formats
1434 SECTION 11 Problems Related to Movement and Coordination
rest and is aggravated by emotional stress or increased concen- sion) or backward (retropulsion). Assessment of postural insta-
tration. The hand tremor is described as “pill rolling” because bility includes the “pull test,” in which the examiner stands
the thumb and forefinger appear to move in a rotary fashion as behind the patient and gives a tug backward on the shoulder,
if rolling a pill, coin, or other small object. Tremor can also causing the patient to lose his or her balance and fall backward.
involve the diaphragm, tongue, lips, and jaw but rarely causes In addition to the motor signs of PD, many nonmotor symp-
shaking of the head. toms are common. They include depression, anxiety, apathy,
Unfortunately, in many people a benign essential tremor is fatigue, pain, constipation, impotence, and short-term memory
mistakenly diagnosed as PD. Essential tremor occurs during impairment. Sleep problems are common in patients with PD
voluntary movement, has a more rapid frequency than parkin- and include difficulty staying asleep at night, restless sleep,
sonian tremor, and is often familial. nightmares, and drowsiness or sudden sleep onset during
Rigidity. Rigidity, the second sign of the triad, is the increased the day.18
resistance to passive motion when the limbs are moved through
their range of motion. Parkinsonian rigidity is typified by cog- Complications
wheel rigidity, or a jerky quality, as if there were intermittent As the disease progresses, complications increase. These include
catches in the movement of a cogwheel, when the joint is moved motor symptoms (e.g., dyskinesias [spontaneous, involuntary
passively. Sustained muscle contraction causes the rigidity and movements], weakness, akinesia [total immobility]), neurologic
consequently elicits complaints of muscle soreness; feeling tired problems (e.g., dementia), and neuropsychiatric problems (e.g.,
and achy; or pain in the head, the upper body, the spine, or the depression, hallucinations, psychosis). As PD progresses, it
legs. Another consequence of rigidity is slowness of movement often results in a severe dementia, which is associated with an
because it inhibits the alternating of contraction and relaxation increase in mortality.
in opposing muscle groups (e.g., biceps and triceps). As swallowing becomes more difficult (dysphagia), malnu-
Bradykinesia. Bradykinesia is particularly evident in the trition or aspiration may result. General debilitation may lead
loss of automatic movements, which is secondary to the physi- to pneumonia, urinary tract infections, and skin breakdown.
cal and chemical alteration of the basal ganglia and related Orthostatic hypotension may occur in some patients and,
structures in the extrapyramidal portion of the CNS. In the along with loss of postural reflexes, may result in falls or other
unaffected patient, automatic movements are involuntary and injury.22
occur subconsciously. They include blinking of the eyelids,
swinging of the arms while walking, swallowing of saliva, self- Diagnostic Studies
expression with facial and hand movements, and minor move- Because there is no specific diagnostic test for PD, the diagnosis
ment of postural adjustment. is based on the history and the clinical features. A firm diagnosis
The patient with PD does not execute these movements and can be made only when at least two of the three signs of the
lacks spontaneous activity. This accounts for the stooped pos- classic triad are present: tremor, rigidity, and bradykinesia. The
ture, masked face (deadpan expression), drooling of saliva, and ultimate confirmation of PD is a positive response to antipar-
shuffling gait ( festination) that are characteristic of a person kinsonian drugs. Research is ongoing regarding the role of
with this disease. The posture is that of a slowed “old man” genetic testing and MRI in diagnosing patients with PD.23
image, with the head and trunk bent forward and the legs con-
stantly flexed (Fig. 59-9). Collaborative Care
Postural instability is common. Patients may complain of Because PD has no cure, collaborative care focuses on relieving
being unable to stop themselves from going forward (propul- the symptoms (Table 59-17).
Drug Therapy. Drug therapy for PD is aimed at correcting
the imbalance of neurotransmitters within the CNS. Antipar-
Blank facial Forward tilt
to posture kinsonian drugs either enhance the release or the supply of DA
expression
(dopaminergic) or antagonize or block the effects of the overac-
tive cholinergic neurons in the striatum (anticholinergic) (see
Fig. 59-7). Levodopa with carbidopa (Sinemet) is often the first
Slow, monotonous,
slurred speech drug used. Levodopa is a chemical precursor of DA and can
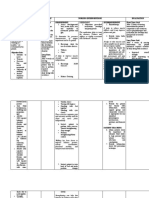
TABLE 59-17 COLLABORATIVE CARE
Tremor Parkinson’s Disease
Diagnostic
• History and physical examination
• Tremor, rigidity, and bradykinesia
• Positive response to antiparkinsonian drugs
Short, shuffling gait • MRI
• Rule out side effects of phenothiazines, reserpine,
benzodiazepines, haloperidol
Collaborative Therapy
• Antiparkinsonian drugs (see Table 59-18)
• Deep brain stimulation
• Ablation surgery
FIG. 59-9 Characteristic appearance of a patient with Parkinson’s disease.
You might also like
- Everything You Need to Know About Parkinson's DiseaseDocument17 pagesEverything You Need to Know About Parkinson's DiseaseAlexandra BădescuNo ratings yet
- Joaquin Farias - Intertwined - How To Induce Neuroplasticity (2012)Document154 pagesJoaquin Farias - Intertwined - How To Induce Neuroplasticity (2012)Shwanseb100% (2)
- Neurological ExaminationDocument216 pagesNeurological Examinationkid_latigo100% (4)
- Parkinson's DiseaseDocument38 pagesParkinson's DiseaseSofie Dee100% (8)
- DR A.A.Ayu Meidiary, SPS: Department of Neurology, Sanglah General Hospital, Udayana University DenpasarDocument47 pagesDR A.A.Ayu Meidiary, SPS: Department of Neurology, Sanglah General Hospital, Udayana University DenpasarKertiasihwayanNo ratings yet
- A Simple Guide to Parkinson's Disease and Related Brain ConditionsFrom EverandA Simple Guide to Parkinson's Disease and Related Brain ConditionsNo ratings yet
- Parkinson DiseaseDocument10 pagesParkinson DiseaseparthibaneNo ratings yet
- Parkinson's DiseaseDocument11 pagesParkinson's Diseaseleeyan2wenty6100% (3)
- Uworld - PSYCHIATRYDocument24 pagesUworld - PSYCHIATRYNikxyNo ratings yet
- Key Homoeopathic Remedies GuideDocument114 pagesKey Homoeopathic Remedies GuideHussain Kaisrani100% (1)
- Cognitive MedsDocument2 pagesCognitive MedsRNStudent1100% (1)
- Drug Study - LevetiracetamDocument3 pagesDrug Study - LevetiracetamCath Bril100% (4)
- ACETIC ACID REMEDIESDocument55 pagesACETIC ACID REMEDIESEngr Syed Numan ShahNo ratings yet
- Anxiety NCPDocument2 pagesAnxiety NCPAnaleah MalayaoNo ratings yet
- Cerebral Palsy: Signs & Symptoms / Pathophysiology / Drug Studies / Ncps / Health TeachingsDocument22 pagesCerebral Palsy: Signs & Symptoms / Pathophysiology / Drug Studies / Ncps / Health TeachingsGeoffrey Sintaan RiveraNo ratings yet
- Pain in Parkinson's Disease: Blair Ford, MDDocument6 pagesPain in Parkinson's Disease: Blair Ford, MDMaria RamosNo ratings yet
- Parkinson's Disease-Diagnosis & TreatmentDocument9 pagesParkinson's Disease-Diagnosis & Treatmentvivek_win95100% (1)
- Alprazolam Mechanism, Indications, Adverse Effects, Nursing ResponsibilitiesDocument2 pagesAlprazolam Mechanism, Indications, Adverse Effects, Nursing ResponsibilitiesGrape JuiceNo ratings yet
- BIPERIDENDocument3 pagesBIPERIDENDenise GabatoNo ratings yet
- Parkinson's DiseaseDocument24 pagesParkinson's DiseaseVimal KumarNo ratings yet
- University of The Southern Caribbean Maracas Royal Road, Maracas, St. JosephDocument12 pagesUniversity of The Southern Caribbean Maracas Royal Road, Maracas, St. JosephTISHANNA GLASSGOWNo ratings yet
- Subiaga Antiparkinsonismmuscle-RelaxantsDocument15 pagesSubiaga Antiparkinsonismmuscle-RelaxantsNicole ObispoNo ratings yet
- DTSCH Arztebl Int-113-0061Document10 pagesDTSCH Arztebl Int-113-0061ayuNo ratings yet
- PD Presentation PINKAN PDFDocument71 pagesPD Presentation PINKAN PDFMartga Bella RahimiNo ratings yet
- Psychotherapeutic AgentsDocument2 pagesPsychotherapeutic AgentsjustinahorroNo ratings yet
- Movement Disorders: Akinetic-Rigid SyndromesDocument8 pagesMovement Disorders: Akinetic-Rigid SyndromesMarwan M.No ratings yet
- Eps and NMSDocument12 pagesEps and NMSNaomi OraengNo ratings yet
- NCA2 Almo Neuro Part 2Document6 pagesNCA2 Almo Neuro Part 2Pebbles PangilinanNo ratings yet
- Movement Disorders GuideDocument23 pagesMovement Disorders GuideBrendan O'HareNo ratings yet
- Activity 4 F PsychiaLab DrugStudyDocument36 pagesActivity 4 F PsychiaLab DrugStudyVinz OñoNo ratings yet
- Clarisse B. Cerame - Drug Study - PsychopharmacologyDocument5 pagesClarisse B. Cerame - Drug Study - PsychopharmacologyClarisse Biagtan CerameNo ratings yet
- Antipsychotics 1Document41 pagesAntipsychotics 1fahad rustam100% (1)
- Https Emedicine - Medscape.com Article 1831191-PrintDocument59 pagesHttps Emedicine - Medscape.com Article 1831191-PrintNoviatiPrayangsariNo ratings yet
- ACTIVITY 14. 1. Drugs Affecting The CNS Mechanism of Action Indications Adverse Effects Important Nursing ConsiderationsDocument19 pagesACTIVITY 14. 1. Drugs Affecting The CNS Mechanism of Action Indications Adverse Effects Important Nursing ConsiderationsPatricia Dianne RuizNo ratings yet
- Parkinson's DiseaseDocument26 pagesParkinson's DiseaseDarwin CauilanNo ratings yet
- Gaines K Adjunctive Therapy in PD The Role of Rasagiline Neuropsych Dis and Treat 2012 V2Document10 pagesGaines K Adjunctive Therapy in PD The Role of Rasagiline Neuropsych Dis and Treat 2012 V2Dany RockNo ratings yet
- Week 6 - Antiparkinsonism AgentsDocument18 pagesWeek 6 - Antiparkinsonism AgentsDino MicaNo ratings yet
- ParkinsonDocument2 pagesParkinsongoyaNo ratings yet
- Pysche OSCE - EPSE ExaminationDocument1 pagePysche OSCE - EPSE ExaminationAmber WangNo ratings yet
- Anti-Parkinsonian Drugs: Lecturer: Sir Mark Angelo Cristino - 24 March 2022Document6 pagesAnti-Parkinsonian Drugs: Lecturer: Sir Mark Angelo Cristino - 24 March 2022Marimiel PagulayanNo ratings yet
- Parkinsons Disease PDFDocument32 pagesParkinsons Disease PDFRaymund Christopher Dela PeñaNo ratings yet
- Update On The Diagnosis and Management of Parkinson's DiseaseDocument6 pagesUpdate On The Diagnosis and Management of Parkinson's DiseaseAsniar RNo ratings yet
- Surgical Therapies For Parkinson DiseaseDocument13 pagesSurgical Therapies For Parkinson DiseaseAnali Durán CorderoNo ratings yet
- RISPERIDONE Iloilo Doctor's College Nursing Responsibilities for RisperidoneDocument9 pagesRISPERIDONE Iloilo Doctor's College Nursing Responsibilities for RisperidoneColeen Mae CamaristaNo ratings yet
- Anti Parkinsonian Drugs 09Document26 pagesAnti Parkinsonian Drugs 09yara baNo ratings yet
- Clinical Pharmacy & Therapeutics 1 Case Study on Parkinson's DiseaseDocument13 pagesClinical Pharmacy & Therapeutics 1 Case Study on Parkinson's DiseaseJenesis Cairo CuaresmaNo ratings yet
- Extrapyramidal Symptoms - StatPearls - NCBI BookshelfDocument6 pagesExtrapyramidal Symptoms - StatPearls - NCBI BookshelfFitrah RahmadhaniNo ratings yet
- Parkinson's Disease Guide: Causes, Symptoms and TreatmentDocument16 pagesParkinson's Disease Guide: Causes, Symptoms and TreatmentNab MughalNo ratings yet
- Pharma Lab. Activity 2Document55 pagesPharma Lab. Activity 2Majestic RavenNo ratings yet
- Parkinson19 PDFDocument6 pagesParkinson19 PDFLorenaNo ratings yet
- NeurologiaDocument67 pagesNeurologiastevenNo ratings yet
- MEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionDocument1 pageMEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionMeryPinkihanNo ratings yet
- Rivotril DrugDocument2 pagesRivotril DrugMery Ong BenitezNo ratings yet
- Extrapyramidal Symptom AssessmentDocument6 pagesExtrapyramidal Symptom AssessmentJNo ratings yet
- YAWAADocument10 pagesYAWAAZyrene CapulongNo ratings yet
- Group 7-Parkinson's DiseaseDocument1 pageGroup 7-Parkinson's DiseaseKamal Talukder KabboNo ratings yet
- Parkinson S Disease Epidemiology,.9Document5 pagesParkinson S Disease Epidemiology,.9bacharelado2010No ratings yet
- Parkinsons Disease Copy 3Document41 pagesParkinsons Disease Copy 3Raghad AbbadyNo ratings yet
- JOURNAL READING-Epilepsy-RidhaDocument22 pagesJOURNAL READING-Epilepsy-RidhaUlul Azmi AdnanNo ratings yet
- Anti ParkinsonsDocument4 pagesAnti ParkinsonsMichaela BernadasNo ratings yet
- Understanding Sleep Disorders in ParkinsonismDocument1 pageUnderstanding Sleep Disorders in ParkinsonismYusni NaniNo ratings yet
- Drug StudyDocument27 pagesDrug StudyMariefer EsplagoNo ratings yet
- Parkison DiseaseDocument36 pagesParkison Diseaseabenezer g/kirstosNo ratings yet
- PARKINSON DiseaseDocument40 pagesPARKINSON DiseaseJM MARQUEZNo ratings yet
- Haloperidol PDFDocument1 pageHaloperidol PDFAda AlvarezNo ratings yet
- Sensory Aspects of Movement Disorders: ReviewDocument13 pagesSensory Aspects of Movement Disorders: ReviewFirdauzi Devi ArimbiNo ratings yet
- Pharmacology: Reviewer For Final Exam: Nervous SystemDocument18 pagesPharmacology: Reviewer For Final Exam: Nervous Systempatty janeNo ratings yet
- QuizlewwwDocument90 pagesQuizlewwwnaimNo ratings yet
- MEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionDocument1 pageMEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionMeryPinkihanNo ratings yet
- MEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionDocument1 pageMEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionMeryPinkihanNo ratings yet
- MEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionDocument1 pageMEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionMeryPinkihanNo ratings yet
- Managing Chronic Neurologic Problems Like Parkinson's DiseaseDocument1 pageManaging Chronic Neurologic Problems Like Parkinson's DiseaseMeryPinkihanNo ratings yet
- MEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionDocument1 pageMEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionMeryPinkihanNo ratings yet
- MEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionDocument1 pageMEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionMeryPinkihanNo ratings yet
- MEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionDocument1 pageMEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionMeryPinkihanNo ratings yet
- Clinical Opioid Withdrawal Scale Cows - 2Document1 pageClinical Opioid Withdrawal Scale Cows - 2thidingNo ratings yet
- 2015 Movement DisordersDocument567 pages2015 Movement DisordersAndreea Raluca CimpoiNo ratings yet
- Parkinson's Disease Stage of Parkinson's DiseaseDocument2 pagesParkinson's Disease Stage of Parkinson's DiseaseRaRa PRawitaNo ratings yet
- Holmes' tremor from cerebellar lesionsDocument7 pagesHolmes' tremor from cerebellar lesionsIan Luis Flores SaavedraNo ratings yet
- Clinical Approach To Tremor in ChildrenDocument6 pagesClinical Approach To Tremor in Childrenveerraju tv100% (1)
- Energies Alterations and Chakras Energies Deficiencies As Underlying Cause of Essential TremorsDocument9 pagesEnergies Alterations and Chakras Energies Deficiencies As Underlying Cause of Essential TremorsasclepiuspdfsNo ratings yet
- Case of Cerebellar Ataxia and TremorsDocument2 pagesCase of Cerebellar Ataxia and TremorsBacean Aurel IoanNo ratings yet
- Neurological Disorders in Older Adults: Types, Symptoms & PreventionDocument20 pagesNeurological Disorders in Older Adults: Types, Symptoms & PreventionAlyssa NicoleNo ratings yet
- Disease DetectionDocument17 pagesDisease DetectionBharat DedhiaNo ratings yet
- 1.2 General Survey, Vital Signs, and SkinDocument7 pages1.2 General Survey, Vital Signs, and SkinC1 - RAZALAN NICKA JOYNo ratings yet
- Myoclonus With DementiaDocument8 pagesMyoclonus With DementiaSantosh DashNo ratings yet
- Practical Use of The MDS-UPDRS EditDocument56 pagesPractical Use of The MDS-UPDRS EditSafitri MuhlisaNo ratings yet
- Presentation FinalDocument26 pagesPresentation FinalDr THOMAS KINGSLEY MDNo ratings yet
- James Parkinson's Disease: Signs, Symptoms, and Physiotherapy ManagementDocument25 pagesJames Parkinson's Disease: Signs, Symptoms, and Physiotherapy ManagementArko duttaNo ratings yet
- Neurology TerminologyDocument5 pagesNeurology TerminologyMuhammad asif samiNo ratings yet
- Tremor Ease 1Document15 pagesTremor Ease 1Matthew WalkerNo ratings yet
- Cardiovascular Chest Pain GuideDocument5 pagesCardiovascular Chest Pain GuidefilchibuffNo ratings yet
- The Ethical Aspects of ICT Implants in The Human Body - Tb21dec - Ict - enDocument87 pagesThe Ethical Aspects of ICT Implants in The Human Body - Tb21dec - Ict - enGovernment-Slave-4-UNo ratings yet
- 09#gyro Grip Culinary AbstractDocument3 pages09#gyro Grip Culinary Abstractkumaramartya11No ratings yet
- FGFKSJHGFKHSFGKJHSDGLDocument11 pagesFGFKSJHGFKHSFGKJHSDGLyannajsdhfjskdhfjkshjfhNo ratings yet
- Insights Into Pathophysiology From Medication-Induced TremorDocument10 pagesInsights Into Pathophysiology From Medication-Induced TremoradindaNo ratings yet
- Clinical Pearls in Tremor and Other Hyperkinetic MovimentDocument7 pagesClinical Pearls in Tremor and Other Hyperkinetic Movimentrafael rocha novaesNo ratings yet