Professional Documents
Culture Documents
Pain Algorithim 2
Uploaded by
api-662601291Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pain Algorithim 2
Uploaded by
api-662601291Copyright:
Available Formats
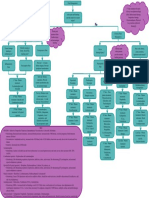
What kind of
pain is the
Self-Limited pain patient Pain the persissts
that occurs as the experiencing? beyond the natural
result of an injury healing Process
Peroperative
Pain
Musculoskeletal
Acute Characteristics:
Beneficial
Characteristics: - Chronic Pain
Persistent or intermittent
Pre-Op: 1 to 2 Adaptive - Pathologic
hours before Protective - Maladaptuve
Is it coming from Is there damage to Clear Cause
surgery. Prevent - Unclear Cause
stimuli causing a the tissues leading First Line
peripheral - Challenging
shark, shocklike to inflammation? Non-Pharm:
sensitization management
pain? Multidisciplinary
- Physchologic
management
Component Neuropathic and physical
Nociceptive Inflammatory Pain exercise
Pain Pain Diabetic
Trigeminal
Intra-Op: During the Peripheral
Neuralgia
operation. Prevent Neuropathy
Second Line
central sensitization due Pharmacologic:
to incisional injury Postherpetic
1st Line: Non-Pharm Fibromyalgia First Line APAP,
Neuralgia
Pharmacologic: NSAIDs
First Line: Duloxetine,
2nd Line: Pharm Carbamazepine How to Prevent: First Line: Pregabalin
Therapy Shingles Non Pharm Third Line
Post-Op: Want to Vaccination (Education Second Line Pharmacologic:
reduce acute pain and Second Line: (shingrix) and Pharmacologic: Weak
further prevent from Oxcarbazepine Psychological TCAs, opioids,
chronic pain (within APAP - for support & antidepressants,
gabapentin,
one week post-op) mild/moderate First Line Exercise!) muscle
venlafaxine
pain Pharmacologic: relaxants
Third Line: Lidocaine
Combination patch
NSAIDs - for Second Line
Therapy Third Line
inflammatory Pharmacologic:
Pharmacologic:
conditions, Duloxetine, Last Line
Second Line Combination
Overall treatments: APAP, watch for Milnacipran, Pharmacologic:
Pharmacologic: Therapy
NSAIDs, Pergabalin, bleeding risks Amytripyline, Strong opioids,
Gabapentin,
Gabapentin, Local Pregabalin, anticonvulsants
Pregabalin,
Anesthetics, Opioids Cyclobenzaprine,
Topical
Opioids - most Tramadol Last Line
Capsaicin, TCAs
effective, start with Pharmacologic:
combo products Opioids
(e.g codeine) Third Line
Third Line Pharmacologic:
Pharmacologic: Gabapentin,
Tramadol SSRIs,
Venlafaxine,
Cannabinoids
KEY:
Monitoring/Safety/AEs
APAP: Acetaminophen
- Many formulations, caution in alcohol use and liver dysfunction, maximum dose 4000mg/day, can cause hepatotoxicty and skin rxns (SJS, TEN, AGEP)
NSAIDs:
- Overall Counseling: Antinflammatory agents, decreased renal clearance, increased BP, increased risk of MI/stroke, avoid in pregnancy (third trimester), nausea, GI
Bleeds
- Non-Selective: Ibuprofen, Indomethacin, Naproxen, Ketorolac
- Counseling: Increased risk of GI bleeds, max of 3200mg/day (Ibuprofen), Risk of CNS effects (Indomethacin), short term use - risk of renal and liver failure
(ketorolac)
- COX-2 Selective: Celecoxib, Diclofenac
- Counseling: Increased MI/stroke
Skeletal Muscle Relaxants: Carisoprodol, Diazepam, Tizanidine, Baclofen, Dantrolene, Chlorzoxazone, Cyclobenzaprine, Methocarbamol, Metaxalone, Orphenadrine
- Monitoring: Can cause CNS depression and have additive effects, should be used short term, should be d/c if ineffective, add risk for polypharmacy
Opioids: Oxycodone, Morphine, Hydrocodone, Fentanyl, etc.
- Monitoring: Watch for - life threatening respiratory depression, addiction, interactions with alcohol, heat exposure, cytochrome P450 interactions, concomitant use
with MAOIs, tablet crushing (with specific formulations), life threatening QT prolongation, medication errors, nausea, vomiting
Combination Opioids: e.g Hydrocodone & APAP
- Monitoring: Watch for - life threatening respiratory depression, addiction, interactions with alcohol, heat exposure, cytochrome P450 interactions, concomitant use
with MAOIs, tablet crushing (with specific formulations), life threatening QT prolongation, medication errors, nausea, vomiting
Antidepressants
- SSRI: Duloxetine, Milnacipran, Venlafaxine
- Monitoring: Increased bleeding risk, dose adjustments with renal/hepatic impairment
- TCAs: Amitriptyline, Nortriptyline, Desipramine, Imipramine
- Monitoring: Lower doses necessary compared to MDD doses, multiple cardiac/anticholinergic effects
Anticonvulsants: Gabapentin, Pregabalin, Topiramate, Lamotrigine, Carbamazepine
- Monitoring: CNS depressions, risk for impairment, drug rashes, hepatotoxicity, blood dycrasias, bone loss, suicide risk
You might also like
- NCP Post Op PainDocument2 pagesNCP Post Op PainLiz Liwag0% (1)
- Nursing Care Plan For Subconjunctival Hemorrhage OSDocument8 pagesNursing Care Plan For Subconjunctival Hemorrhage OSRosemarie CarpioNo ratings yet
- Antidepressant & Psychedelic Drug Interaction ChartDocument3 pagesAntidepressant & Psychedelic Drug Interaction ChartFred The Nomad100% (2)
- Pain Management AlgorithmDocument1 pagePain Management Algorithmapi-662596662No ratings yet
- Pain Dr. HenryDocument36 pagesPain Dr. Henryreagan setiawanNo ratings yet
- Pad Bundle Ce Final - Presentation ViewDocument60 pagesPad Bundle Ce Final - Presentation ViewJeremy WalleyNo ratings yet
- Pain Daily PracticeDocument30 pagesPain Daily Practicesukasuka azaNo ratings yet
- Treatment of Neuropathic Pain or Post Herpetic PainDocument8 pagesTreatment of Neuropathic Pain or Post Herpetic PainSalwa ZeinNo ratings yet
- Assessment and Management of Chronic Pain Guideline SummaryDocument8 pagesAssessment and Management of Chronic Pain Guideline SummaryBiby AnneNo ratings yet
- NCP Acute PainDocument3 pagesNCP Acute PainBasema HashhashNo ratings yet
- PAiN SYnDrOmEs (Reviewer)Document19 pagesPAiN SYnDrOmEs (Reviewer)Agum, Philip James P.No ratings yet
- Manajemen NyeriDocument27 pagesManajemen Nyerivera100% (1)
- 2021 Update Management Pain (Dokter & Medical)Document30 pages2021 Update Management Pain (Dokter & Medical)Andri MuliaNo ratings yet
- Drug Study On AnestheticsDocument9 pagesDrug Study On AnestheticsKalvinArtRazalanCelebradosNo ratings yet
- E PaediatricsfordoctorsDocument53 pagesE PaediatricsfordoctorsJimmy RahuNo ratings yet
- Nonnarcotic Methods of Pain ManagementDocument1 pageNonnarcotic Methods of Pain ManagementVanessa PasikNo ratings yet
- Manajemen Nyeri Motik RS BhinaDocument36 pagesManajemen Nyeri Motik RS Bhinayn_faisalNo ratings yet
- Pain and Fever in The PharmacyDocument11 pagesPain and Fever in The PharmacyP D SpencerNo ratings yet
- Advance Pain ManagementDocument50 pagesAdvance Pain ManagementAkmal ZaibNo ratings yet
- Dr. Erwin A.D. Nanulaitta, SPKFR - Physical Rehabilitation in Pain ManagementDocument29 pagesDr. Erwin A.D. Nanulaitta, SPKFR - Physical Rehabilitation in Pain ManagementFreade AkbarNo ratings yet
- Penatalaksanaan Nyeri DLL 2018Document14 pagesPenatalaksanaan Nyeri DLL 2018Silvia HandikaNo ratings yet
- General Santos Doctors' Medical School Foundation NCM: 122N Rle ExposureDocument8 pagesGeneral Santos Doctors' Medical School Foundation NCM: 122N Rle Exposurejay kusainNo ratings yet
- Pain & Neuropathic Pain Basics - Reading MaterialDocument13 pagesPain & Neuropathic Pain Basics - Reading MaterialSalim khanNo ratings yet
- Pain and NeuralgiaDocument51 pagesPain and NeuralgiaAndika WigunaNo ratings yet
- CH12AnalgesiaLabor (9 AgustuDocument27 pagesCH12AnalgesiaLabor (9 AgustuAnonymous FX2NVrd4c2No ratings yet
- Acute Periopertive Pain Management (Sby)Document87 pagesAcute Periopertive Pain Management (Sby)Adam KurniaNo ratings yet
- Neuropathic PainDocument40 pagesNeuropathic PainHasmirahNo ratings yet
- Bahan SharingDocument40 pagesBahan SharingkfcrajanyaayamNo ratings yet
- Pain - Post Partum MotherDocument2 pagesPain - Post Partum Motherulrikov91% (11)
- Mixed Pain Jainuri Erik Pratama-1Document37 pagesMixed Pain Jainuri Erik Pratama-1Trie WulandariNo ratings yet
- Subjective Data: Objective Data: - Well Appearing But Independent Nursing Interventions: - Review Intraoperative Desired Outcome. Goal Met. Patient Was Able ToDocument3 pagesSubjective Data: Objective Data: - Well Appearing But Independent Nursing Interventions: - Review Intraoperative Desired Outcome. Goal Met. Patient Was Able ToMariel GamaloNo ratings yet
- Manajemen Nyeri Dengan DexketoprofenDocument27 pagesManajemen Nyeri Dengan Dexketoprofenmaya santiNo ratings yet
- Drug StudyDocument3 pagesDrug Studymarichelle plazaNo ratings yet
- Nalbuphine NubainDocument1 pageNalbuphine NubainB PNo ratings yet
- Pain ManagementDocument7 pagesPain ManagementHazel ZullaNo ratings yet
- Marquina Chronic Neuro PainDocument63 pagesMarquina Chronic Neuro PainLukasNo ratings yet
- Current Concept For Management of Neuropathic PainDocument55 pagesCurrent Concept For Management of Neuropathic Painmpm8471No ratings yet
- DS - 3rd RotDocument8 pagesDS - 3rd Rotalamillodemarkbsn3No ratings yet
- NCP 2Document2 pagesNCP 2marohunkNo ratings yet
- Management NyeriDocument49 pagesManagement NyeriYuke ArmikaNo ratings yet
- Balanced AnalgesicDocument37 pagesBalanced AnalgesicGia Bảo Thụy NguyễnNo ratings yet
- WIM Pain ManagementDocument34 pagesWIM Pain ManagementSugiono brinabimoNo ratings yet
- Pain Science in Practice - What Is Pain Neuroscience Part 2Document3 pagesPain Science in Practice - What Is Pain Neuroscience Part 2MathildeNo ratings yet
- Peran Akupunktur Medik Pada Kasus NyeriDocument155 pagesPeran Akupunktur Medik Pada Kasus NyeriSilvia HandikaNo ratings yet
- Opioid AnalgesicsDocument25 pagesOpioid AnalgesicscchatrumaNo ratings yet
- Perioperative Pain Management - Bali 2019Document55 pagesPerioperative Pain Management - Bali 2019Joko WowNo ratings yet
- Drug StudyDocument7 pagesDrug StudyBoss SaligumbaNo ratings yet
- Assessment Nursing Diagnosis Scientific Explanation Planning Implementation Rationale EvaluationDocument3 pagesAssessment Nursing Diagnosis Scientific Explanation Planning Implementation Rationale EvaluationNurse NotesNo ratings yet
- Drug StudyDocument3 pagesDrug StudyFrances Katherine GarciaNo ratings yet
- Beri151216 w1Document1 pageBeri151216 w1Lunatiku TraderNo ratings yet
- Panel Nyeri Blok 2.5Document28 pagesPanel Nyeri Blok 2.5HAFIZH CAHYA ARYANSYAHNo ratings yet
- Management Acute PainDocument110 pagesManagement Acute PainjohannesNo ratings yet
- Assessment Explanation of The Problem Objective Nursing Intervetion Rationale EvaluationDocument2 pagesAssessment Explanation of The Problem Objective Nursing Intervetion Rationale EvaluationSALWANo ratings yet
- Know Acute Pain-Standard Slide-Approve For Use - DR - ZuhadDocument42 pagesKnow Acute Pain-Standard Slide-Approve For Use - DR - Zuhadteguh cahyonoNo ratings yet
- Mixed Pain DR Novi Irawan SPSDocument25 pagesMixed Pain DR Novi Irawan SPSnovi irawanNo ratings yet
- Preemptive Analgesia in Oral Surgery (Pain Vaccination) - A ReviewDocument27 pagesPreemptive Analgesia in Oral Surgery (Pain Vaccination) - A ReviewAshish DadhaniaNo ratings yet
- 3 NCP FinalDocument7 pages3 NCP FinalJames PanlaanNo ratings yet
- Pain Science in PracticeDocument4 pagesPain Science in PracticeIan PeroniNo ratings yet
- Perioperative Pain ManagementFrom EverandPerioperative Pain ManagementFelicia CoxNo ratings yet
- Assessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsFrom EverandAssessment of Pain Management in Anaesthesia Practice among Nurse AnaesthetistsNo ratings yet
- Johnson County Drug SweepDocument10 pagesJohnson County Drug SweepFOX59/CBS4No ratings yet
- Med Card PregabalinDocument1 pageMed Card PregabalinTaylor NicholNo ratings yet
- Drugs FOR Psychiatric & Neurologic Disorders: Clonazepam (Klonopin, Rivotril) Midazolam (Versed, Dormicum)Document5 pagesDrugs FOR Psychiatric & Neurologic Disorders: Clonazepam (Klonopin, Rivotril) Midazolam (Versed, Dormicum)Noriko MatsumotoNo ratings yet
- Prescription MedicationsDocument3 pagesPrescription MedicationsCarla PulgarNo ratings yet
- Quick Reference Guide April 2019 PDFDocument2 pagesQuick Reference Guide April 2019 PDFAaron ShokarNo ratings yet
- Literatur Jurnal PDFDocument5 pagesLiteratur Jurnal PDFEga Ayu PrastikaNo ratings yet
- Tradamol Drug InformationDocument1 pageTradamol Drug InformationJohnny ZinzNo ratings yet
- Drugs Acting On Central Nervous SystemDocument11 pagesDrugs Acting On Central Nervous SystemVidhi MehtaNo ratings yet
- NyeriDocument1 pageNyeriIlmiyatul MuhimmahNo ratings yet
- Mapeh-9health Q2 Summative-TestDocument2 pagesMapeh-9health Q2 Summative-TestRojegarmil LagoNo ratings yet
- Test Bank For Drugs Society and Human Behavior 16th EditionDocument11 pagesTest Bank For Drugs Society and Human Behavior 16th Editionjohnflorescdjrfwqxzs100% (30)
- Anti Psychotic DrugsDocument2 pagesAnti Psychotic DrugscalfornianursingacadNo ratings yet
- KIMED - HSA ANALGESIKvDocument21 pagesKIMED - HSA ANALGESIKvKuni RofiatyNo ratings yet
- Lista de Precios 2019: Alvarez Martinez HaydeeDocument2 pagesLista de Precios 2019: Alvarez Martinez HaydeeedgarNo ratings yet
- StimulantsDocument4 pagesStimulantsLinh-Trang NguyenNo ratings yet
- Common Types of DrugsDocument8 pagesCommon Types of DrugsFELIX Mary Ann G.No ratings yet
- Multi Functional Drugs - A Novel Concept For Psycho PharmacologyDocument3 pagesMulti Functional Drugs - A Novel Concept For Psycho Pharmacologyrocsa11No ratings yet
- Classification CNS, NSAIDsDocument15 pagesClassification CNS, NSAIDsAkmalNo ratings yet
- Model Paper Set-B Medicinal Chemistry-I Bp402T: Section A MM 75 1. Attempt All Questions in Brief. 10 X 1 20Document1 pageModel Paper Set-B Medicinal Chemistry-I Bp402T: Section A MM 75 1. Attempt All Questions in Brief. 10 X 1 20SwarnA TamtaNo ratings yet
- Normal Reçete Ile Kontral Tabi ListeDocument4 pagesNormal Reçete Ile Kontral Tabi Listefurkan.aras000No ratings yet
- PreparateDocument2 pagesPreparateVasile LozinschiiNo ratings yet
- Classification of DrugsDocument57 pagesClassification of Drugsmark alvin rufoNo ratings yet
- PSYCHOPHARMACOLOGYDocument2 pagesPSYCHOPHARMACOLOGYJulia Rae Delos SantosNo ratings yet
- Antidepressant MCQs Group 2Document4 pagesAntidepressant MCQs Group 2Ayesha Ayesha100% (1)
- Normal Reçete İle Verilmesi Gereken İzlemeye Tabi İlaç ListesiDocument4 pagesNormal Reçete İle Verilmesi Gereken İzlemeye Tabi İlaç ListesicanankeNo ratings yet
- Different Kinds of Drugs and Its EffectsDocument13 pagesDifferent Kinds of Drugs and Its EffectsSapo KurtNo ratings yet
- Amphetamine and Its RoleDocument1 pageAmphetamine and Its RoleConleyHillNo ratings yet
- Drugs of AbuseDocument1 pageDrugs of AbuseAigerim SuiindikovaNo ratings yet
- Psychotherapeutic Drugs: Pam Pam LamDocument7 pagesPsychotherapeutic Drugs: Pam Pam Lamchubbygunny_29776413No ratings yet