Professional Documents
Culture Documents
MTAP Hema 1 W7 FINAL
Uploaded by
Caleb Joshua MendozaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
MTAP Hema 1 W7 FINAL
Uploaded by
Caleb Joshua MendozaCopyright:
Available Formats
HEMATOLOGY
LECTURE 01 ORIENTATION AND FUNCTIONS OF BLOOD
6. Enumerate and discuss the different special hematologic
Introduction tests.
HEMOGLOBIN 101 Seminar Topics (Week 2)
CYTOCHEMICAL STAINS IN HEMATOLOGY
FUNCTION OF BLOOD - Used in tertiary laboratory
- Hemoglobin - Expensive tests
- How is hemoglobin synthesized/catabolized - Proper training is required
- How is hemoglobin used for the transport of oxygen - Used for the diagnosis of leukemias and anemias (ei.
Myeloperoxidase, Leukocyte Alkaline Phosphatase,
DYSHEMOGLOBINEMIA Esterase, Sudan Black B, etc.)
- Dyshemoglobin compounds that are significant in blood
diseases AUTOMATION IN HEMATOLOGY
- Carboxyhemoglobin, methemoglobin, sulfhemoglobin 5 basic principles of automation
Current Impedance
IRON KENETICS Electrical impedance
- How iron is being recycled in the body Cytochemical differentiation
- How iron is stored in the body Light Scatter
- Different tests related to iron used in the diagnosis of Flow Cytometry (combination of the previous principles)
certain blood disorders (ei. Anemia) - Common automation principles in hematology
- Serum iron, serum ferritin, total iron binding capacity - Discuss how each principle determine the number of cells
in a blood sample, hematocrit, hemoglobin and
METHODS OF HEMOGLOBIN DETERMINATION differentiation of white blood cells.
- Gravimetric
- Chemical COAGULATION AND HEMOSTASIS
- Gasometric - Coagulation Cascade
- Colorimetric - Test used in coagulation
HEMOGLOBIN CATABOLISM (BREAKDOWN OF HEMOGLOBIN) SPECIAL TOPICS
- Breakdown of globin chains - composed of amino acids
that are being recycled VERIFICATION OF HEMATOLOGY ANALYZERS
- Breakdown of heme (NOTE: only protoporphyrin IX is Delivered at the PAMET Scientific Conference in Pangasinan
removed from the body) Importance: Acc. to ISO 15189 (guideline for the accreditation of
clinical laboratories) and
OXYHEMOGLOBIN DISSOCIATION CURVE CLSI – dictates the verification of the hematology analyzers
- Diseases/conditions that will shift the dissociation curve
- Significance: provides an idea on how the primary function QUALITY CONTROL PLANNING AND SIGMA METRICS IN THE
of hemoglobin is being utilized by the body – to transport HEMATOLOGY LABORATORY
oxygen and carbon dioxide Delivered at the PAMET Scientific Conference in Pangasinan and
Baguio/Benguet, Mt. Province Chapters
SPECIAL HEMATOLOGIC TESTS
Learning objectives on Hematology Series Part 2:
- Tests that are not routinely used in hematology and some 1. Discuss the principles of testing and clinical significance of the
of the tests are already obsolete different cytochemical stains used in hematology
- Test are still important because it may be requested for 2. Explain the principles of automation in Hematology
rare blood dyscrasias 3. Discuss the coagulation cascade
4. Explain how automated analyzers in hematology are verified
Learning Objectives on Hematology Lecture Series Part 1: 5. Discuss quality control planning and then apply sigma metrics
1. Explain the different functions of blood. as a quality control tool in hematology (protect your dignity and
2. Discuss the characteristics and synthesis of hemoglobin license in the future)
and the clinical significance of iron kinetics.
3. Discuss the properties and clinical significance of the
different dyshemoglobins.
4. Apply the principles and procedures of the different
methods for hemoglobin determination.
5. Explain the principles of the oxyhemoglobin dissociation
curve and the catabolism of hemoglobin.
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 1
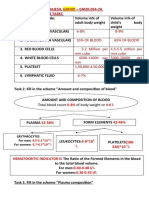
FUNCTIONS OF BLOOD BLOOD CLOTTING
Mediated by platelets as well as the coagulation factors present in
Blood is a specialized connective tissue – it originates from the plasma.
parenchyma cells, in the embro and the fetus.
It contains formed elements in an extra cellular matrix (ECM). BODY TEMPERATURE
In the environment, if the temperature is hot, the temperature inside
GAS TRANSPORT the body is much hotter
- Transport O2 from the lung to the different parts of the body - Since the blood is constantly going around the body
and to collect CO2 to bring it out of the system (revolving), the heat inside the body and body organs is
- During respiration CO2 is produced → respiration will brought to the superficial areas of the body (i.e., arms,
happen while tissues will need oxygen legs, face, torso)
- The warm blood inside the body that continuously
ACID/BASE LEVELS circulates around is carried outside the body (i.e., skin) →
- Maintains acid/ base levels by hemoglobin (has a buffer perspiration (due to condensation) maintains the
system in itself maintains acidity and alkalinity by way of temperature inside and outside the body.
maintaining pH levels)
- Normal pH of blood: 7.35 – 7.45 (Slightly alkaline) OSMOTIC PRESSURE
- Bloods cells has the affinity for the acid dye because the Also known as oncotic pressure
acidic component of blood cell is alkaline - We are talking about the function of albumin and certain
- pH changes based on respiration, amount of oxygen in the proteins in the blood to maintain osmotic/oncotic pressure.
blood and acid. - Why water does not immediately enter the blood circulation
- Hemoglobin → brings O2 to the tissues → CO2 goes (e.g., when drinking water)? This is because of osmotic
inside the blood pressure.
Note: CO2 does not need red blood cells to be transported - The maintenance of the protein component (albumin) of
but only water (plasma is made up of 92% water). It is the blood maintains osmotic pressure. Basically, this
oxygen that needs hemoglobin to be transported because it amount of solute is maintained by this amount of solvent.
is non-water soluble. If CO2 is dissolved in water, it - If the amount of albumin decreases, the amount of water
produces carbonic acid which decreases the pH = increase also decreases, and vice versa. But if the amount of
acidity. albumin is normal, water will not simply enter the blood.
IMMUNE RESPONSE
WBCs are made to combat infectious agents by way of immune
response.
2 types of lymphocytes in the body:
1. B-cells: involved in the production of antibodies and also
involved in humoral immunity.
2. T-cells: responsible for phagocytosis (direct cell killing) and
also involved in cellular immunity.
- Neutrophils are involved in bacterial infection because
they engulf bacterial cells. Neutrophils can only survive for
9-12 days because we are at constant exposure to
infectious agents.
- On a daily average, more than 3,000 types of bacteria,
fungal cells and viruses are breathed in every time we
breathe.
- Neutrophils are suicidal meaning if these cells have
engulfed a bacterial cell, it will release lytic agents within
and lysing itself together with the bacterial cells and
eventually turns into pus cells (manifestation of anti-
inflammation/infection).
- Pus cells are blood cells that have destroyed their
cytoplasm with no distinct morphological characteristic but
contains granules.
- Eosinophils are involved in parasitic infections.
Eosinophils have the Major Basic Protein (MBP) which is
responsible for anti-parasitic activity, killing the parasites.
- Any type of parasitic infection, the eosinophils increase in
number.
- If in case the infectious load of parasite is low, this is
because of the presence or increase of eosinophils.
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 2
LECTURE 01 Hemoglobin 101
hemoglobin Salt bridges will bind the globin chains
Major component of red blood cells together
Blood can carry very little oxygen through plasma, because Lead to more O2 deposited to your
oxygen is nonwatery soluble, thus it requires hemoglobin to Hgb
be transported. O2 down, 2,3, - DPG also down
o Other References: 2-3% of oxygen is found in
plasma. 97% of oxygen in blood is bound to HEMOGLOBIN SYNTHESIS
hemoglobin
o Sir AJ: 0.3% plasma 99.7% hemoglobin Mitochondrion
Hemoglobin is required to carry oxygen around 65% - developing erythroblasts
If the body had to depend upon dissolved oxygen in the 35% - reticulocytes
plasma to supply oxygen to the cells, the heart would have Derived from succinyl CoA + glycine
to pump 140 liters per minute – instead of 4 liters per Remnants of heme production
minute, leading to an increased cardiac output o FEP
o Decreased RBC Decreased Hemoglobin o Ferritin
Decreased Oxygen Increased Cardiac Output Main function: O2 transport
(one of the complications of anemia) o 1.34 mL of O2/g Hgb
Each red blood cells can carry about 1 million molecules of o 401 mL of O2/g iron
oxygen Heme synthesis:
Arterial Blood (oxygenated blood): Hemoglobin is 97% - Protoporphyrin IX
saturated with oxygen when it leaves the lungs - Iron
Venous Blood (Deoxygenated blood): Under resting o 90% of the iron that we use is recycled iron
conditions, hemoglobin is about 75% saturated with oxygen o 10% diet
when it returns to the heart Two pathways:
o Increased physical activity increases metabolic Globin: via the ribosomes
activity in tissues, leading to increased Heme: via the synthesis between the cytosol (cytoplasm)
respiration to provide more oxygen to the tissues and mitochondria
Blood through perfusion is able to collect oxygen from the o 2 components in a developing RBC where heme
lungs is being produced
Blood cells are made up of two components Succinyl CoA
o Hemoglobin: solution inside the cells Glycine
o Membrane: holds or encases the hemoglobin
Video 2 | Hemoglobin 101
• Iron is important for affinity.
• Without iron, there will be no O2 affinity.
• What regulates the affinity?
o 2,3, - DPG
Transient resident (pag kailangan,
anjan sya WOW NAOL)
o Not because iron is present, doesn’t mean that it
will automatically bind to O2.
o Salt bridge: responsible for binding the globin
chains
o (+) 2,3, - DPG >> salt bridges will be broken s
down = lesser affinity of O2 to Hgb
Ex. Increased physical activity
Increased need for O2 by the tissues
Needs more O2 because your muscles
are undergoing metabolism and
respiration
2,3, - DPG will have to be produced by
Luebering Rapoport shunt of the
Embden Meyerhof pathway
After release of 2,3, - DPG, O2 will be
released from the Hgb [It will hold the
globin chains to release the O2]
After resting >> lower respiration >>
lower body temperature >> O2 will now
stabilize b/n blood and the tissues
2,3, - DPG goes down
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 3
Oxidized Ferric state = produce hemiglobin/methemoglobin
*Start with Succinyl CoA
*Heme synthesis starts and ends inside the mitochondria 1 hemoglobin molecule is made up of 4 globin chains
*Most enzymes are found in the cytoplasm 2 beta
2 alpha
Yellow part: mitochondria *binding is always Beta 2 alpha 1 ; Beta 1 alpha 2
White part: cytoplasm
Protoporphyrin IX will bind to Iron in the presence of Video 3 | Hemoglobin 101
Ferrochelatase to form HEME
Heme goes out of the cytoplasm >> looks for globin chains IRON METABOLISM
>> form Hgb
Storage iron – liver
Succinyl CoA + Glycine >> dALA goes outside and P.H.UCs Ferritin
>> Protoporphyrinogen III o Iron + apoferritin
Hemosiderin
1 RBC can carry 1 million molecules of Hgb o Non water soluble
o 1 molecule of Hgb carries 4 molecules of O2 Iron absorption
o Ex. If 250 000 molecules x 4 = 1M O2 Duodenum and jejunum
o Intestinal mucosal cells will oxidise it to its ferric
state
o Mediated by hephaestin (protein on the
basolaminal enterocyte membrane of the GIT
paryicularly the small intestine – responsible for
oxidizing iron as it exits the enterocyte and into the
blood stream)
o Once it is oxidized, the iron is now ready for
plasma transport carried by a specific protein
known as apotransferrin.
o Once the iron binds, the molecule is now known
as transferrin.
o Apotransferrin binds to molecules of ferric iron.
Iron recycling
If NO iron: Protoporphyrin IX Salvage iron from the dying cells
Bone marrow will produce RBC as long as there is hypoxia Largest percentage of recycled iron: from RBCs; senscent
(detected by the kidneys – production of EPO) RBCs ingested by macrophages in the spleen
↑ EPO = RBC produced Not yet senescent RBCs: due to increased hemolytic
What if no iron? Ex. Iron-deficiency anemia reactions coming from either pathologic or physiologic
o No iron = produce FEP (Free Erythrocyte reactions
Protoporphyrin) Iron from Hgb has to be recycled
o FEP = an analyte being determined among iron- Hgb is first degraded with the iron >> ferritin
deficiency anemia patients In the blood vessels, the macrophages posses ferroportin in
o ↑ FEP = no iron; diagnostic of IDA their membrances that allow macrophages to be iron
What if iron overload? exporters so that they can be salvaged into usable iron for
o Sideroblastic anemia use by other cells.
o Low EPO = iron overload o Mediated by a substance produced by the liver
o Ferritin = storage iron; goes back to the liver = Hepcidin
(stored there for future use) o Responsible for regulating the absorption of iron
o ↑ absorption from the GIT may lead to iron
• 1.34 mL of O2/g Hgb overload
o Collect 100 mL of arterial blood Life-threatening
o Contains 15g of Hgb Liver damage
o Hgb concentration is 15g/dL Heart disease
o 15g/100mL Diabetes
o 15 x 1.34 = 20mL of O2 is present per 100 mL of o Regulator molecule that will determine the activity
blood of ferroportin (responsible for the absorption of
iron)
PORPHYRIN RING o Hephaestin will be involved in absorption of iron
At the core of the molecule is porphyrin ring which holds an When needed, iron is eventually
iron atom. released from the mucosal cells and
An iron containing porphyrin is termed a heme. then binds to transferrin developing
This iron atom is the site of oxygen binding. RBCs through ferric transferrin
Should always be in the Ferrous state membrane receptors
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 4
• After releasing iron into the Hemochromatosis
bone marrow, the transferrin Disease which causes your body to absorb too much iron
receptor will complex then from the food that you eat
move back to the cell Too much iron can be dangerous >> life-threatening
membrane and return to the because it can be stored
plasma.
• Only the excess iron will be Sideroblastic anemia
incorporated into the Result of a deffect in an X-linked recessive gene
transferrin and return to the ALAS 2: makes an enzyme which is essential in the
liver. production of heme (O2 carrying portion of the Hgb
o Important: regulatory mechanism b/n the molecule)
absorption of iron in the body Ferrochelatase: absense of ALAS 2 will
iron transport make a deficiency in an enzyme
o Hephaestin responsible for produxn of heme
Decreased O2 carrying capacity of the
65-68% of total body iron is found in HGB as hemoglobin Hgb molecule
iron Serum iron: decreased
18% - form of ferritin and hemosiderin found in the liver Because most of the iron being supplied
10% - myoglobilin iron in muscles to the BM for erythrocyte production is
o Peroxidase not being taken in
o Catalase Iron return back to the liver or in the
o Cytochrome plasma
o Riboflavin enzymes Charactrized by the presence of iron granules present
Iron is important for the functionality of hemoglobin around the mitochondria of precurser cells of red cells;
*transferrin is measured indirectly by TIBC
*test for tranferrin not always readily available
Several blood disorders that may detedted with the use of
iron panel tests
1. SERUM IRON
measure of iron content in serum
affected by diurnal variations
Iron intake and acute phase responses will actually be
affected by diurnal variation
Limited utility in assessment of overall iron status
Still used in the computation of transferrin saturation
Decreased:
IDA – anemia because of deficiency of
iron
ACD – iron in the bodyis sufficient but it
is stored in the form of ferritin or preipheral membance of RBCs
hemosiderin; not releaased in the serum Thalassemia: decreased globin synthesis
• Compensatory mechanism of
our in cases of inflammatory PCT
reactions or infectious Group of acquired and familial disorders in which the activity
diseases of the heme synthetic enzyme uroporphyrinogen
• In the (+) of infectious decarboxylase is deficient
diseases in our body, will Same with SDA; missing enzyme that is responsible for
trigger our body to restrict the binding or synthesis of protoporphyrin IX
release of iron. Stored in the Less amount of protoporphyrin IX that is
form of ferritin or hemosiderin. supposed to bind iron
• Therefore, there will be an Eventually, decrease synthesized heme
apparent decrease in the Increase in serum iron because it is not
serum iron because it is not being used
released by the body to deter • Vitamin B12 deficiency
the growth of mcgs. Inappropriate of RBC due to problems with normal nuclear
maturation
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 5
2. SERUM FERRITIN Hemoglobin compounds
Good indicator of the total body iron stores • Oxyhemoglobin – type of hemoglobin that is bound to
Major storage form of iron • Carboxyhemoglobin
Low levels: diagnostic of IDA o Cherry Red
<100ug/L does not always exlude iron-deficiency o Increased affinity for O2
Feritin: acute phase reactant that can be increased in o Level in smokers: 5-15% (0.5% in non-smokers)
inflammatory states (ex. Liver disease, malignancies) o 10% - impairs judgement
Elevated: iron overload o Greater than 40% - fatal
Transferrin Saturation: test required for iron overload o Tests (absorption band: 576 nm)
Only decreased in cases of IDA Gas chromatography
Palmer’s
3. Transferrin Iron Saturation Percentage Sunderman’s
Usually computed as the percent of transferrins carrying Dithionate
capacity that is saturated with iron • Methemoglobin
For every molecule of transferrin, only 1/3 is occupied by o Chocolate brown
iron. 2/3 a reserve for more iron to bind o Remedies
Formula: serum iron/TIBC x 100 Methemoglobin reductase
Decreased Saturation system/diaphorase
IDA Glutathione reductase system
ACD o Absorption band: 630 nm using KCN
Any type of inflammation o Methemoglobinemia
Useful test for the assessmemt of high ferritin Acquired – exposure to oxidants
High ferritin below 45% especially among women or below (antimalarial drugs, sulfonamides,
50% among men is more likely secondary to another cause aniline dyes, nitrate-rich food stuff)
Inherited – NADH mthemoglobin
4. Total Iron Binding Capacity (TIBC) reductase system def
Indirect measure of transferrin levels Inherited Hgb M amino acid substitutes
Transferrin levels are increased in the setting of ion
deficiency as well as in pregnancy, also in cases of estrogen
administration
Decreases
Inflammation
Chronic liver disease
Malnutrition
Absence of iron >> transferrin is increased
Because it is the body’s compensatory
mechanism for the lack of iron
5. Hemoglobin
Mostly anemia, therefore decreased
*Hemochromatosis, PCT, African Siderosis
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 6
LECTURE 02 DYSHEMOGLOBIN: hemoglobin derivatives and their associated disorders
o Rural areas have lesser levels of carbon
HEMOGLOBIN
monoxide
• Normal hemoglobin is produced with no problems • One spot test
regarding globin chain synthesis nor substitution of o Procedure:
amino acids within globin chain or structural problems Hemolyze 0.5 mL of whole blood with
with the globin chain 20 mL distilled water
• Thalassemia: problems in globin chain synthesis Add 1mL of NaOH, 1.0 mol/L
• Hemoglobinopathies: problem in amino acids or o Result:
structure of globin chain Brown blood: Normal
Light Cherry Red Blood: >20%
OXYHEMOGLOBIN AND DEOXYHEMOGLOBIN Carboxyhemoglobin
• Quantitation of CO (absorption band: 576 nm)
• Oxyhemoglobin – with oxygen; oxygen is being o Gas chromatography
transported by hemoglobin as O2 is non-water soluble, o Spectrophotometry
meaning it needs a transport molecule • Other Tests
• Deoxyhemoglobin – hgb with no oxygen o Palmer’s
o Sunderman’s
CARBAMINOHEMOGLOBIN o Dithionite
• hgb with carbon dioxide
• carbon dioxide that first binds with an amino group, then Effects of Treatment on Laboratory Results
to hemoglobin
• co2 cannot bind to hgb without amino group • It requires administration of high levels of Oxygen
• hgb can only transport 5% on Carbon Dioxide, the • Hyperbaric Oxygen Chamber
remaining 95% is transported by plasma and the water o Patients are exposed to 600x oxygen as
present in RBC compared to the normal environment;
• Plasma can only transport 3% of Oxygen o Oxygen plasma can be maximized from 0.3%
• Carbon Dioxide is water soluble so it doesn’t need to 3%
hemoglobin, it can easily dissolve in the plasma • As long as there is no brain damage, carbon monoxide
poisoning has no long-term effect as long as the patient
receives proper and prompt treatment
PATHOLOGIC HEMOGLOBIN COMPOUNDS
METHEMOGLOBIN
CARBOXYHEMOGLOBIN
• Hemoglobin derivative that binds to carbon monoxide METHEMOGLOBIN (Hemiglobin or Hi)
• Normally found in blood at less than 1% of Total Produced when the iron component of blood is oxidized
Hemoglobin from the ferrous state to the ferric state
• Hemoglobin has 200-250 times greater affinity to Normally, 0.5 - 3% of hgb in blood is converted to
Carbon Monoxide (CO) than Oxygen (O2) methemoglobin daily
• Carbon monoxide is an colorless, odorless gas that NADH-methemoglobin reductase (diaphorase) enzyme
when encountered even in small percentages can is present in erythrocytes to counter the normal
prevent the oxygen transport of many hemoglobin production of methemoglobin
molecules. It can lead to asphyxiation
METHEMOGLOBIN REDUCTION
Symptoms and Physical Findings Requires a properly functioning Embden-Meyerhof
pathway to produce NADH, which is the main source for
• The skin may turn bright cherry red with increasing electron donation in the reduction process
levels of carboxyhemoglobin The electron is transferred from NADH to the
• Exposure and Effect Methemoglobin Reductase and then to an erythrocyte
10% impairs judgement; some may undergo cytochrome before being used in the actual heme
dizziness or fainting reduction
>40% Fatal
50-70% Asphyxiation Hb+3 ----------------------------------------------------------------- Hb+2
(NADH NAD) e- Met Hb Reductase Cytochrome
Laboratory Findings and Correlation with Disease
• Level in smokers: 5-15%
• Non-smokers: 0-5%
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 7
Treatment may not be necessary since there are no
other clinical abnormalities than cyanotic appearance
Laboratory Findings and Correlation with Disease
Peripheral Blood Film
Denatured hemoglobin demonstrates Heinz bodies due
to the ingested toxins
Require special stains
Diaphorase Enzyme Screening Test
Rapid
Specific enzyme assays for use with prepare
hemolysates are also available
Methemoglobin Quantitation
Absorbance at 630 to 635 nm
Potassium cyanide (KCN) is added to a prepared
hemolysate which is converts methemoglobin to
cyanmethemoglobin (does not absorb at 632nm)
The concentration of methemoglobin is proportional to
the amount of cyanmethemoglobin produced in the
METHEMOGLOBINEMIA reaction
Results
Elevated erythrocyte methemoglobin concentrations due o Abnormal: >1.5 % methemoglobin
to inability to adequately reduce methemoglobin o Methemoglobin due to toxic substances: 10 to
Can cause cyanosis < 70%
Clinical Manifestations: few and generally mild o Untreated diaphorase deficiency: 15-30%
Rarely inherited; there are five inherited Hemoglobin M
variants, that cause methemoglobinemia Other Findings
Usually acquired Patients with methemoglobinemia can cause a slight
Treatment: Patients respond to therapeutic doses of compensatory erythrocytosis and a slight left shit in the
methylene blue (except patients with Hb M disorder). O2 dissociation curve. Erythrocyte survival is normal
o Cyanotic Normal Skin Color
Remedies
Inherited Methemoglobinemia Methemoglobin reductase system/diaphorase
Inherited NADH-methemoglobin reductase enzyme Glutathione reductase system
deficiency or Diaphorase Deficiency Vitamin E (alpahatocopherol) is an antioxidant which
The deficiency does not adequately reduce prevents the oxidation of iron from ferrous to ferric state
methemoglobin even with sufficient NADH levels Injection of methylene blue reducing agent
produced by Embden-Meyerhof pathway o Methylene blue donated electron to the
Patients respond to Methylene Blue Treatment enzyme NADPH-methemoglobin reductase ,
leading to the reduction of Methylene blue to
Acquired Methemoglobinemia Leukomethylene blue
May be caused by ingested or absorbed substances o Leukomethylene blue nonenzymatically reduce
o Antimalarial drugs methemoglobin
o Sulfonamides Blue family of Kentucky
o Drugs of abuse In US, they are cyanotic, and they are injected with
o Aniline dyes (fresh dye on shoes) methylene blue reducing agent due to their system
o Nitrate-rich water and foods deficiency
o Common aromatic chemicals
Patients also respond to methylene blue treatment
Inherited Hemoglobin M Methemoglobinemia
There are five Hb M variants caused by amino acid
substitutions in the globin chains
The amino acid substitutions in globin chains directly
affect the heme group, causing it to enter the ferric or
oxidized state
Patients do not respond to methylene blue
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 8
SULFHEMOGLOBIN
Oxidation derivative of hemoglobin that cannot carry
oxygen
Exposure to certain drugs and chemicals
o Acetanilid, phenacetin, sulfonamides
Sulfur containing drugs that may lead
to binding of sulfur to hemoglobin
Sulfur has the same affinity with oxygen but once sulfur
has bound to hgb, oxygen cannot bind to hgb anymore,
leading to cyanosis
Once sulfhemoglobin is formed it cannot be converted
back to a functional hemoglobin
IrreversibleA
Mauve-lavender blood
Absorption band: 618 nm
Symptoms and Physical Findings
Excessive sulfhemoglbin concentration hardly exceed
20% in the blood
Not life threatening and is generally benign
Cyanosis is the only significant effect
Laboratory Findings and Correlation with Disease
Sulfhemoglobin quantitation
o Examines hemolysate for a distinct, broad
increase in the absorption curve in the range of
600 to 620 nm
Treatment
o Removal of the offending agent
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 9
LECTURE 03 Methods of Hemoglobin Determination
Gravimetric colorimetric
• Crude method Visual Methods
• Used for mass blood donations – because of simplicity of
the test ACID HEMATIN METHOD
o Basis of donor’s acceptance to donate
Sinks or stays in the middle:
QUALIFIED
Floats: DEFFERED
PROCEDURE
1. Place 500mL Copper Sulphate (CuSO4) Solution in a 1L
beaker Comparator
2. Adjust the CuSO4 by adding water until its specific gravity blocks
is 1.050, 1.052 or 1.053
3. Place a drop a patient’s blood observe if it floats or
sinks
RESULTS
FLOAT: SG is less than the CuSO4
SINK: SG is greater than the CuSO4
STAYS IN THE MIDDLE: equal SG
Specific Gravity Corresponding HgB conc PROCEDURE:
1.050 - 1. Add acid hematin to the hemometer tube (0.1 N HCl) up to
1.052 - the 2-mark
1.053 12.5 g/dL 2. Add 20 uL blood
1.055 13.5 g/dL 3. Mix with glass stirrer or applicator stick
4. Place the tube in the hemometer set
Note: The SG of the sample is directly proportional to the HgB 5. Add drops of distilled water – for every drop, stir the soln
content of the blood until the color of the solution is the same as the comparator
block (endpoint)
Gasometric 6. Check the level of the soln – this is now the level of HgB
• Indirect measure for HgB ALKALI HEMATIN METHOD
o measure O2 to determine the level of HgB
o 1.34 mL 02/g HgB • Same procedure as Acid hematin
o Difference: reagent is 1 N Sodium hydroxide
• Specimen: arterial blood
o The sample should be ~97% oxygenated • Standardization method: Gibbson/Harisson method
Example: 100 mL of blood with 20.1 mL of oxygen Photometric Method (Medical)
20.1 𝑚𝑚𝑚𝑚 • Direct HgB determination
= 𝟏𝟏𝟏𝟏 𝒈𝒈 𝒐𝒐𝒐𝒐 𝑯𝑯𝑯𝑯𝑯𝑯⁄𝟏𝟏𝟏𝟏𝟏𝟏 𝒎𝒎𝒎𝒎 𝒐𝒐𝒐𝒐 𝒃𝒃𝒃𝒃𝒃𝒃𝒃𝒃𝒃𝒃 • Reference method
1.34
• Principle is also used by hematology analyzers
Chemical o Cyanmethemoglobin reagent dilute blood
• Indirect measure lyse red cells read spectrophotometrically
o Measures iron to determine the level of HgB
o ICSH: 3.47 mg Fe/g HgB DRABKIN’S METHOD/CYANMETHEMOGLOBIN METHOD
ICSH – International Committee for • Most common manual method
standardization in Hematology • Drabkins reagent
• Involves lysing of blood cells measure iron in the o Potassium ferricyanide + Potassium cyanide +
hemolysate sodium bicarbonate + surfactant
Cyanide is slowly replaced by Sodium
lauryl sulfate
• Cyanide is hazardous
PRINCIPLE: Drabkins reagent converts hemoglobin to
methemoglobin cyanmethemoglobin (orange in color; Abs: 540
nm in spectrophotometer)
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 10
[RODAKS]
1. Create a standard curve, using a commercially available
Note: cyanmethemoglobin standard.
• The absorbance of cyanmethemoglobin is directly a. When a standard containing 80 mg/dL of
proportional to the hemoglobin concentration. hemoglobin is used, the following dilutions should
• Sulfhemoglobin can’t measured by this method since it be made:
is not converted to cyanmethemoglobin
PROCEDURE
[Sir Aj’s]
1. 5 ml of Drabkin’s reagent is placed in a tube
2. Dispense 20 uL of blood
3. Mix incubate for 15 mins at 37OC
4. Read against a standard
dilution by adding 0.02 mL (20 mL) of blood to 5 mL of
b. Transfer the dilutions to cuvettes. Set the cyanmethemoglobin reagent. The pipette should be rinsed
wavelength on the spectrophotometer to 540 nm thoroughly with the reagent to ensure that no blood
and use the blank to set to 100% transmittance. remains.
c. Using semilogarithmic paper, plot percent 4. Cover and mix well by inversion or use a vortex mixer. Let
transmittance on the y-axis and the hemoglobin stand for 10 minutes at room temperature to allow full
concentration on the x-axis. The hemoglobin conversion of hemoglobin to cyanmethemoglobin
concentrations of the control and patient samples 5. Transfer all of the solutions to cuvettes. Set the
can be read from this standard curve spectrophotometer to 100% transmittance at the
d. A standard curve should be set up with each new wavelength of 540 nm, using cyanmethemoglobin reagent
lot of reagents. It also should be checked when as a blank
alterations are made to the spectrophotometer 6. Using a matched cuvette, continue reading the %
2. Controls should be run with each batch of samples. transmittance of the patient samples and record the values
Commercial controls are available 7. Determine the hemoglobin concentration of the control
3. Using the patient’s whole blood anticoagulated with EDTA samples and the patient samples from the standard curve
or heparin or blood from a capillary puncture, make a 1:251
SOURCES OF ERROR IN DRABKIN’S METHOD
Effect Resolution
Drabkin’s reagent is sensitive to light Store in a brown/amber bottle or in a dark
place
High WBC count (>20x 109/L) Centrifuge reagent-sample solution and
Turbidity false high result
High platelet count (>700 x 109/L) supernatant measured
Lipemia Corrected by adding 0.01 ml of patient’s
Turbidity false high result plasma to 5 mL cyanmethemoglobin used
as reagent blank
Presence of Hb S and Hb C Make 1:2 dilution with water and multiplying
Resistant to hemolysis turbidity
the results from the standard curve by 2
Presence of abnormal globulins in patients Add 0.1 g of potassium carbonate to
with plasma cell myeloma or Waldenstorm cyanmethemoglobin reagent
macroglobulinemia
Globulins may precipitate in the reagent
Note: Commercial cyanmethemoglobin
reagent are now modified to contain potassium
carbonate
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 11
Lecture 04 Hemoglobin dissociation
Oxygen dissociation curve (01)
Figure 1.0 The oxygen affinity of hemoglobin is depicted by the
Oxygen dissociation curve (ODC). The fractional saturation of
hemoglobin (y axis) is plotted against the concentration of oxygen
measured as the PO2 (x axis). At a pH of 7.4 and an oxygen tension
(PO2) of 26 mmHg, hemoglobin is 50% saturated with oxygen (red
line). The curve shifts in response to temperature, CO2, O2, 2,3-
BPG concentration, and pH. When the curve shifts left (light blue
line), there is increased affinity of Hb for O2. When the curve shifts
right (dark blue line), there is decreased affinity of Hb for O2
[McKenzie, 3rd ed]
SUMMARY
LEFT SHIFT [R] RIGHT SHIFT [T]
↑ O2 ↓ O2 (to tissues)
↑ pH (No HCO3 & H2CO3) ↓ pH
↓ CO2 ↑ CO2 (to blood)
↓ 2,3-BPG (No Release) ↑ 2,3-BPG
↓ H+ ↑ H+
↓ Temperature ↑ Temperature
[At resting phase] [↑ Metabolism = ↑ respiration]
Other Blood Functions 3. 2,3-Biphosphoglycerate (2,3-BPG)
1. Thermoregulation . 2,3-BPG affects oxygen-binding affinity by binding in a
QFR #1: How does the blood regulate the temperature of the body? small central cavity of deoxygenated hemoglobin. This shifts
The heat of the internal organs will perfuse in blood and will the equilibrium towards deoxy-hemoglobin. The presence of
later disseminate and distribute that heat throughout the acids leads to increased H+ and a reduction in pH. This
body, from the core to the surface and vice versa. By promotes formation of the deoxy form of hemoglobin,
changing the blood flow to the skin, the body can control shifting the oxygen dissociation curve to the right, promoting
heat exchange at its surface with its surroundings oxygen release to actively respiring tissues. At high altitude,
2. Immunologic function (WBCs) when oxygen in the atmosphere is scarce because the air is
3. Hemostasis “thinner,” production of 2,3-BPG is greatly increased,
4. pH Buffer helping hemoglobin to release more of its bound oxygen. It
takes about 24 hours for 2,3-BPG levels to rise, and over
Factors that affect Hemoglobin affinity for Oxygen longer periods of time, the levels continue to increase as part
of the acclimation effect. The 2,3-BPG production is one
[Hematology 1- Module 3: Hemoglobin]
1. Partial pressure of oxygen reason that athletes train at high altitudes to increase their
aerobic capacity. Interestingly, 2,3-BPG does not bind to
If the oxygen dissociation curve shifts to the left, a patient with
fetal hemoglobin. This results in tighter binding of oxygen
arterial and venous PO2 levels in the reference intervals (80 to
100 mm Hg arterial and 30 to 50 mm Hg venous) will have a
relative to maternal hemoglobin, giving the developing fetus
higher percent oxygen saturation and a higher affinity for better access to oxygen from the mother's bloodstream.
oxygen than a patient for whom the curve is normal. With a shift
in the curve to the right, a lower oxygen affinity is seen. 4. Temperature
Tissues of the human body that are actively undergoing high
2. pH of blood metabolic rates produce excess amounts of thermal energy
The pH of blood affects the shifting of the oxygen dissociation as a waste product. Through heat transfer, the thermal
curve either to the left or to the right. This is explained by the energy diffuses to the blood in nearby capillaries. When the
Bohr effect which explains the lower affinity of hemoglobin for thermal energy reaches the blood stream, it increases the
oxygen due to increases in the partial pressure of carbon average kinetic energy of the molecules within the plasma
dioxide (CO2) which eventually decreases the blood pH. thereby resulting to higher temperature. Higher temperature
Whenever the human body undergoes increased cellular in the blood is interpreted by the body that cells are working
respiration, such as in strenuous physical activities, there is also harder thus requiring more oxygen to keep them going. In
an increase in metabolic activity within the tissues involved response to higher temperature, the Hb decrease its affinity
resulting in the production of CO2 as a metabolic waste product. for oxygen to facilitate delivery to the tissues. Thus,
To transport CO2 through the venous blood, it diffuses into the increased temperature in the blood shifts the oxygen
red blood cells combining with water to form carbonic acid dissociation curve to the right such as when tissues are
(H2CO3). This reaction is facilitated by the enzyme, carbonic
actively engaged in physical activity, these tissues would
anhydrase. The carbonic acid will then dissociate to release H+
require and eventually receive more O2.
and bicarbonate (HCO3-). The increase in H+ due to this
reaction decreases the blood pH as explained by the Bohr effect
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 12
5. Carbon dioxide
CO2 is a waste product of cellular respiration. As discussed earlier, CO2 diffuses from the tissues to red cells to form H2CO3 which dissociates
to H+ and HCO3- resulting to a shift of the curve to the right. Once the red cells reach the lungs, O2 will diffuse into the deoxygenated Hb
resulting to release of H+ that will combine with HCO3- to form H2CO3 which in turn will dissociate to water and CO2 where the latter will
diffuse out of the cells and eventually expelled by the lungs. This phenomenon is explained by the Haldane effect which describes the binding
of oxygen to Hb which promotes the release of CO2
2,3 BPG Binding to Hemoglobin
PRINCIPLE:
Oxygen interacts weakly with heme iron, and the two
can dissociate easily. As O2 is released by hemoglobin
in the tissues, the heme pockets narrow and restrict
entry of O2, and the space between the β-chains
widens and 2,3-BPG binds again in the central cavity.
Thus, as 2,3-BPG concentration increases, the T
configuration of hemoglobin is favored and the
oxygen affinity decreases. [McKenzie, 3rd ed]
Oxyhemoglobin VS Deoxy-hemoglobin
Oxyhemoglobin [R] Deoxy-hemoglobin [T]
Tense or “T” state
Relaxed or R state
2,3 BPG causes a conformational change in hemoglobin shape
O2 can freely enter in the body
because it replaces the salt bridges connecting the globin chains.
Hemoglobin tetramer is fully oxygenated
2,3 BPG is ONLY produced when there is increased need for O2
NO 2,3 BPG (Instead, salt bridges hold α1β1 and α2β2)
NOTE: The tense form incorporates one 2,3-bisphosphoglycerate (2,3-BPG) molecule, bound between the β-globin chains with salt bridges. It is unable to
transport oxygen. As hemoglobin binds oxygen molecules, the α1β1 and α2β2 dimers rotate 15º relative to each other as a result of the change in hydrophobic
interactions at the α1β2 contact point, disruption of salt bridges, and release of 2, 3-BP [Rodak,5th]
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 13
Hemoglobin as a Blood Buffer
OPTIMAL blood pH : 7.40
<7.4 : acidosis
>7.4 : alkalosis
NORMAL pH range: 7.35- 7.45
Buffering System
PRINIPLE :The effect of pH on hemoglobin–oxygen affinity is known as the Bohr effect, an
example of the acid–base equilibrium of hemoglobin that is one of the most important buffer
systems of the body. A molecule of hemoglobin can accept H+ when it releases a molecule of
oxygen. Deoxyhemoglobin accepts and holds the H+ better than oxyhemoglobin. In the tissues,
the H+ concentration is higher because of the presence of lactic acid and CO2. When blood
reaches the tissues, hemoglobin’s affinity for oxygen is decreased by the high H+ concentration,
thereby permitting the more efficient unloading of oxygen at these sites. [McKenzie, 3rd ed]
QFR #2: How does the buffer system work ?
i. During respiration CO2 is produced.
ii. CO2 diffuses in the blood cells and plasma (water)
iii. [CO2 + H2O] : Forms carbonic acid (H₂CO3) in the presence of carbonic
anhydrase [enzyme]
iv. H2CO3 produced in increased amounts will decrease blood pH.
v. Blood will have increased acidity
vi. [HCO3- + H+] : In order to maintain blood pH, some H2CO3 is further converted
into bicarbonates and hydronium ions in the same presence of carbonic
anhydrase [enzyme]
vii. Bicarbonates (HCO3-) will act as the buffering system
viii. HCO3- and H2CO3 will be dissociated in the lungs as H2O and CO2
ix. H2O will be reabsorbed in the system
x. CO2 will be expelled during respiration
Note: CO2 does not require hemoglobin to be transported out of the body. It only needs H2O
because it is water soluble. .
95% of CO2 is transported by the water component of blood and dissolved in the plasma
99.7% of O2 is transported by Hgb.
CHECKPOINT
OXYGEN CONCENTRATION is the same through all levels of the earth at 20% to 21%.
However, the partial pressure of O2 is dependent on elevation.
↑↑ Altitude = ↓ partial pressure = O2 will diffuse harder
↓↓ Altitude (sea level) = ↑ partial pressure = O2 will diffuse easier
INHALED O2 will be decreased by 4% to 5%. Hence, EXHALED O2 will be around 16% to 17%.
Oxygen dissociation CURVE (02)
PRINCIPLE: The oxygen dissociation curve illustrates the relationship between oxygen
saturation of hemoglobin and the partial pressure of oxygen.
In the Normal (N) hemoglobin-oxygen dissociation curve, P50 is the partial
pressure of oxygen (O2) needed for 50% O2 saturation of hemoglobin.
In the Left-shifted (L) curve with reduced P50, it can be caused by decreases
in 2,3-bisphosphoglycerate (2,3-BPG) (e.g., multiple transfusion of stored
blood), H+ ions (raised pH), partial pressure of carbon dioxide (PCO2), and/or
body temperature. A left shifted curve is also seen with hemoglobin F and
hemoglobin variants that have increased oxygen affinity and in alkalosis.
In the Right-shifted (R) curve with increased P50 can be caused by
elevations in 2,3-BPG (e.g., in response to hypoxic conditions such as in high
altitudes), H+ ions (lowered pH), PCO2, and/or temperature. A right-shifted
curve is also seen with pulmonary insufficiency, congestive heart failure, severe
anemia and in the presence of hemoglobin variants that have decreased
oxygen affinity.
[Hematology 1- Module 3: Hemoglobin]
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 14
OXYGEN TRANSPORT
MUST KNOW [Rodak 5th] o ↓↓CO2 and ↓↓ H+ ion
concentrations (higher pH)
The function of hemoglobin is to readily increase oxygen saturation
bind oxygen molecules in the lung, The local fluid flow through the capillary
which requires high oxygen affinity; to network and extracellular spaces of
transport oxygen; and to efficiently living tissue. It is characterized as the
Perfusion
unload oxygen to the tissues, which volumetric flow rate per volume of
Main Hgb requires low oxygen affinity. tissue.
function in O2 o Ex. Obtaining O2 from the lungs
transport During oxygenation, each of the four
heme iron atoms in a hemoglobin CONDITIONS THAT PRODUCE A LEFT SHIFT [R]
molecule can reversibly bind one Lowered body temperature due to external causes.
oxygen molecule. Multiple transfusions of stored blood with depleted 2,3-BPG;
Approximately 1.34 mL of oxygen is alkalosis
bound by each gram of hemoglobin Presence of hemoglobin variants with a high affinity for
Affinity of hemoglobin for oxygen oxygen.
Reflects the amount of oxygen gas Shift to the left indicates a decreased MCV (microcytic).
dissolved in the blood. It primarily [Ciulla]
PO2 / PaO2
measures the effectiveness of the lungs
Partial pressure of in pulling oxygen into the blood stream CONDITIONS THAT PRODUCE A RIGHT SHIFT [R]
Oxygen from the atmosphere. Increased body temperature
NORMAL: 27 mm Hg results in Acidosis
50% oxygen saturation Presence of hemoglobin variants with a low affinity for
LEFT SHIFT : < 27 mm Hg oxygen
RIGHT SHIFT : >27 mm Hg Increased 2,3-BPG concentration in response to hypoxic
conditions, such as :
The amount of oxygen needed to high altitude
P50 pulmonary insufficiency
saturate 50% of hemoglobin
congestive heart failure
Oxygen
Plots the percent oxygen saturation of severe anemia
Dissociation
hemoglobin versus the PO2 Shift to the right indicates an increased MCV (macrocytic).
Curve (ODC)
[Ciulla]
The curve is sigmoidal, which indicates
low hemoglobin affinity for oxygen at MOVEMENT OF O2 FROM BLOOD TO TISSUE
low oxygen tension and high affinity for
Sigmoidal O2 from blood can be transferred into the tissues within the
oxygen at high oxygen tension.
ff conditions:
o At the plateau (75%) O2
o PaO2 of tissue should be lower than blood
dissociation will be more rapid
NOTE: PO2 of blood is p50 = 50% Hgb
The reference interval for arterial saturation.
oxygen saturation is 96% to 100%. Normal range is p50 to p100
o Diffusion: movement of solute from higher to a
LEFT SHIFT : a patient with arterial and lesser concentration.
venous PO2 levels in the reference o Example:
Arterial oxygen intervals (80 to 100 mm Hg arterial and i. Physical activity induces a right shift.
saturation 30 to 50 mm Hg venous) will have a ii. Increased respiration will be observed
higher percent oxygen saturation and as more O2 is used.
a higher affinity for oxygen than a iii. Hence, PaO2 in the muscles will be
patient for whom the curve is normal. decreased.
iv. Diffusion will now occur.
RIGHT SHIFT: Lower oxygen affinity v. CO2 will move to the blood stream and
will be converted to H2CO3 and later
A shift in the curve due to a change in into HCO3. These byproducts will be
pH (or hydrogen ion concentration) ‘ transferred into the lungs
It facilitates the ability of hemoglobin to vi. HCO3 and H2CO3 is converted to CO2
exchange oxygen and carbon dioxide and H2O
Bohr effect
(CO2) vii. H2O is absorbed ; CO2 is expelled
o ↑↑CO2 and ↑↑ H+ ion
concentrations (lower pH)
decrease oxygen saturation
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 15
SAMPLE SCENARIOS 4. Which of the following is associated with a "shift to the left"
1. PHYSICAL ACTIVITY in the oxygen dissociation curve of hemoglobin [CIULLA]
a. Decreased pH and elevated temperature
o Increased unloading O2 into the tissues
b. Decreased oxygen affinity
o ↓ PaO2
c. Decreased oxygen release
o ↓ SpO2 d. Presence of 2,3-bisphosphoglycerate (2,3-BPG)
o Results to a hypoxic tissue
5. A "shift to the left," when used to describe a cell
2. >1,500m ABOVE SEA LEVEL [Baguio] population, refers to: [CIULLA]
o PaO2 is 100 mmHg a. Increased cells in the blood due to a redistribution of
o PaO2 in lungs: 40 mmHg blood pools
o Inhalation of O2 at this altitude will result to a decreased b. An increase in immature blood cells following release
PaO2. From 100 mmHg it will be diffused into 80 mmHg of bone marrow pool
o Compensatory mechanism: ↑ RBC production ↑ O2 c. A cell production "hiatus" or gap
o DID YOU KNOW: d. A higher percentage of lymphocytes than neutrophils
Living at places such as Baguio increases your
hematocrit level by 2 to 3 points. 6. In the normal hemoglobin-oxygen dissociation curve, what
Congestion is commonly observed when travelling percentage of oxygen is released to the tissues when PO2
from high altitude places to the lowlands. It is averages 40 mmHg? [BOC]
commonly manifested through “rosy cheeks” hihi a. 75%
3. SEA LEVEL b. 25%
o PaO2 is 140 mmHg c. 100%
o PaO2 in lungs: 40 mmHg d. 50%
o Diffusion of O2 in the lungs will be from a high to a low
concentration 7. What would the hemoglobin-oxygen dissociation curve
o Inhalation of O2 at this altitude will result to a decreased depict in a patient exhibiting clinical signs of alkalosis?
PaO2. From 140 mmHg it will be diffused into 120 mmHg [BOC]
a. normal
4. >10,000 m ABOVE SEA LEVEL [Mt. Everest] b. shift to the left
o PaO2 is 40 mmHg c. shift to the right
o PaO2 in lungs: 40 mmHg d. none of the above
o Inhalation of O2 at this altitude will result to a decreased
PaO2. From 40 mmHg it will be diffused into 20 mmHg 8. What would the hemoglobin-oxygen dissociation curve
o Thin O2 levels cause hypoxic situations. It can initially be depict in a patient exhibiting clinical signs of acidosis?
manifested through fainting. [BOC]
a. normal
NOTE: b. shift to the left
A decrease in the PO2 is due to the admixture of other forms of c. shift to the right
gases d. none of the above
REVIEW QUESTIONS 9. One of the most important buffer systems of the body is
[Rodak, Ciulla, BOC, McKenzie, Module ] the: [McKenzie]
1. Which of the following forms of hemoglobin molecule has a. chloride shift
the lowest affinity for oxygen? [Rodak] b. Bohr effect
a. Tense c. heme–heme interaction
b. Relaxed d. ODC
2. Using the normal hemoglobin-oxygen dissociation curve in 10. When the H+ concentration in blood increases, the oxygen
Figure 1 for reference, predict the position of the curve when affinity of hemoglobin [McKenzie]
there is a decrease in pH. [Rodak] a. Increases
a. Shifted to the right of normal with decreased oxygen b. is unaffected
affinity c. decreases
b. Shifted to the left of normal with increased oxygen d. cannot be measured
affinity
c. Shifted to the right of normal with increased oxygen 11. During exercise, the oxygen affinity of hemoglobin is
affinity [McKenzie]
d. Shifted to the left of normal with decreased oxygen a. Increased in males but not females
affinity b. decreased due to production of heat and lactic acid
c. unaffected in those who are physically fit
3. How does hyperventilation affect the behavior of d. affected only if the duration is more than 1 hour
hemoglobin in response to the imbalance in the levels of
oxygen and carbon dioxide in the body? [Module, QFR]
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 16
12. The oxygen dissociation curve in a case of chronic
carboxyhemoglobin poisoning would show [McKenzie]
a. a shift to the right
b. b . a shift to the left
c. c . a normal curve
d. d . decreased oxygen affinity
13. An aerobics instructor just finished an hour of instruction.
Blood is drawn from her for a research study, and the oxygen
dissociation is measured. What would you expect to find?
[McKenzie]
a. shift to the left
b. a shift to the right
c. no shift
d. an increased oxygen affinity
14. In the lungs, a hemoglobin molecule takes up two oxygen
molecules. What effect will this have on the hemoglobin
molecule? [McKenzie]s
a. It will increase oxygen affinity.
b. It will narrow the heme pockets blocking entry of
additional oxygen.
c. The hemoglobin molecule will take on the tense
structure.
d. The center cavity will expand, and 2,3-BPG will enter
Answer Key:
1.a 2.a 3. 4.c 5.b 6.b 7.b
8.c 9.b 10.c 11.b 12.b 13.b 14.a
RATIONALIZATION
Question # 3 : Hyperventilation causes acute hypocapnia resulting
in cerebral vasoconstriction, hypocalcemia, a shift in the oxygen–
hemoglobin dissociation curve, and reduced oxygen delivery.
Symptoms include lightheadedness, dizziness, faintness,
paresthesias, and altered consciousness. Acute hyperventilation
will result in an acute respiratory alkalosis and cause a left shift in
the oxyhemoglobin dissociation curve
Question # 4 : A "shift to the left" in the oxygen dissociation
curve of hemoglobin means that a higher percentage of
hemoglobin will retain more of its oxygen at a given pressure.
Thus affinity will be greater and oxygen delivery will be reduced.
[CIULLA]
Question # 5 : A "shift to the left" means an increase in immature
neutrophilic cells in the blood caused by bone marrow release of
cells in response to infection or tissue damage. A redistribution of
the blood pools because of emotional or physical stimuli is
characterized by an increased WBC count without a left shift. A
cell "hiatus" refers to a population of cells in which there is a gap
in the normal maturation sequence. A cell hiatus is most often
seen in acute leukemia, in which there are many blasts and a few
mature cells but no intermediate stages. [CIULLA]
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 17
LECTURE 06 Special hematological tests
WINTROBE
Erythrocyte sedimentation rate
The common anticoagulant is double oxalate
• Erythrocyte Sedimentation Rate (ESR) – is a non-specific The Wintrobe method uses the Wintrobe tube.
indicator of inflammation. MICROMETHOD (LANDAU)
3 FACTORS AFFECTING ESR Often used for infants
Uses sodium citrate as the specimen
RBC The ESR must be setup within 4 hours of collection of
o dependent on how the RBCs will be able to form rouleaux or to blood, otherwise it may cause variations in the test result
pack or to be attached to one another making them heavier. In
a simple analogy, it is like stacking several coins and letting STAGES OF ERYTHROCYTE SEDIMENTATION
them fall in a bucket of water. o Rouleaux formation – first 10 minutes
Coins that are stacked together will settle faster than o Sedimentation of RBCs in plasma – next 40 minutes
those that are not attached to each other/separated. o Packing/settling of RBCs – last 10 minutes
In terms of the RBC, the zeta potential which results
from the negatively charged sialic acid groups on the CLINICAL SIGNIFICANCE:
red cell membrane is responsible for affecting the
INCREASED
results of ESR particularly the rouleaux formation of
RBC Pregnancy
A decrease in the zeta potential of RBC will make them Anemia among females
near negative, near neutral, or near positive in terms of Macrocytosis
their electroneutrality on the plasma membrane. Technical errors (e.g., tilted ESR tubes)
Changes on the electroneutrality of RBCs will allow Seen in elevated fibrinogen and gamma-globulin levels
them to attach to one another and form rouleaux. in cases of infection and inflammation
Factors that affect the zeta potential: Fibrinogen and Malignancy
Gamma-globulins = ↓ decrease the zeta potential of Acute myocardial infarction
RBCs = ↑ rouleaux formation = ↑ ESR Multiple myeloma
PLASMA Waldenstrom’s macroglobulinemia
DECREASED
o components in plasma that would affect ESR.
Factors in plasma that affect ESR: Presence of acute Extremely high WBC count
phase proteins (e.g., beta-2-macroglobulin, alpha-1- RBC anomalies:
antitrypsin, and others) which are responsible for Spherocytosis
decreasing the viscosity of plasma. Acanthocytosis
The role of plasma in ESR is very important because Microcytosis
the viscosity or the lesser viscosity of plasma will affect Some of these cells will not allow rouleaux
the rest. formation to take place
↑ viscosity of plasma will deter sedimentation of blood May result in dilution problems (e.g., inadequate mixing
cells while ↓ viscosity of plasma (less viscous) will allow of the sample and anticoagulant)
rapid sedimentation of red cells May also be seen in hyperalbuminemia,
Presence of acute phase proteins in the plasma hypofibrinogenemia, hypogammaglobulinemia, and
especially in cases of inflammation → decrease the certain dysproteinemias.
viscosity of plasma → faster sedimentation of RBCs
The presence of high levels of albumin or Zeta sedimentation ratio
hyperalbuminemia → increase the viscosity of o Measurement of the ease with which the RBC are able to
plasma → slow sedimentation of RBCs sediment under standardized cycle of compaction and
TECHNICAL dispersion stress with the use of zetafuge.
Shaking or vibrations on the table = ↑ ESR Zetafuge – a centrifuge which thins capillary tubes in a
Tilting of the tube = ↑ ESR vertical position in 4 x 45 sec. cycles
Dilution factors = ↑ or ↓ ESR
METHODS:
WESTERGREN/MODIFIED WESTERGREN/DISPETTE
The usual specimen used for these methods is sodium
citrate treated blood
For the modified Westergren method the anticoagulant
used is modified by adding 2mL of EDTA + 0.5mL
either sodium citrate or NSS before diluting it in
blood.
The common tube used is the Westergren tube for the
Zetacrit
Westergren method with a total length of 300mm, while
ZSR = Hct/Zct
the graduations is only 200mm. The internal bore of the
tube is 2.5mm ± 0.15mm.
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 18
Correction for anemia (patient with anemia will drastically
affect ESR whether or not there is inflammation will most COMPUTATIONS:
likely be high) RELATIVE RETICULOCYTE COUNT
NV: 41-54% commonly expressed in the laboratory
Advantages: # 𝑜𝑜𝑜𝑜 𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟 𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐
𝑅𝑅𝑅𝑅𝑅𝑅 = × 100
o Easier to fill capillary tubes compared to ESR 1000 𝑅𝑅𝑅𝑅𝑅𝑅
o Less sample needed
o Unaffected by anemia ABSOLUTE RETICULOCYTE COUNT
the actual count of reticulocytes in the sample
Reticulocyte count 𝐴𝐴𝐴𝐴𝐴𝐴 = 𝑅𝑅𝑅𝑅𝑅𝑅 𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐 × 𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅 𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅 𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐 (𝑖𝑖𝑖𝑖 𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑)
o Measure of the bone marrow’s effective erythropoietic activity
o NV:
CORRECTED RETICULOCYTE COUNT
o Adults – 0.5 -2.5%
o Infant – 2- 6% also known as reticulocyte index or hematocrit correction –
in most laboratories, retic count is expressed as the RI/HC
Relative Retic count (%), the percentage of Done when the patient has ↓ hematocrit
𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅 𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅 𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐 × 𝑞𝑞𝑞𝑞𝑞𝑞𝑞𝑞𝑞𝑞𝑞𝑞𝑞𝑞𝑞𝑞 𝑜𝑜𝑜𝑜 𝑝𝑝𝑝𝑝𝑝𝑝𝑝𝑝𝑝𝑝𝑝𝑝𝑝𝑝 𝐻𝐻𝐻𝐻𝐻𝐻
reticulocyte count in relation to the total red blood 𝐶𝐶𝐶𝐶𝐶𝐶 =
𝑁𝑁𝑁𝑁𝑁𝑁𝑁𝑁𝑁𝑁𝑁𝑁 𝐻𝐻𝐻𝐻𝐻𝐻 [0.45]
cell count of the patient
↑ reticulocyte count may indicate hemolysis, in RETICULOCYTE PRODUCTION INDEX
some follow up samples it may result to response
Also known as the second correction/Shift correction
to treatment for IDA 𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶 𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅𝑅 𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐
𝑅𝑅𝑅𝑅𝑅𝑅 =
𝑚𝑚𝑚𝑚𝑡𝑡𝑢𝑢𝑢𝑢𝑢𝑢𝑢𝑢𝑢𝑢𝑢𝑢𝑢𝑢 𝑡𝑡𝑡𝑡𝑡𝑡𝑡𝑡 𝑖𝑖𝑖𝑖 𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑 𝑜𝑜𝑜𝑜 𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟
METHODS: 𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑 𝑜𝑜𝑜𝑜 𝑡𝑡ℎ𝑒𝑒 𝐻𝐻𝐻𝐻𝐻𝐻
GLASS SLIDE METHOD (Stains are used) Hct = 0.35- 0.39 – maturation time = 1.5 days
1. Dry/Schilling Hct = 0.25- 0.34 – maturation time = 2 days
Brilliant Cresyl Blue or the reference stain - new Hct = 0.15- 0.24 – maturation time = 2.5 days
methylene blue N (NMBN) to dry on a surface of Hct = < 0.15 – maturation time = 3 days
the glass slide→ once the stain is dry on the glass
slide, put one drop of blood and overlay a coverslip SOURCES OF ERROR
→ incubate for 10-15 mins under a wet preparation o Recent blood transfusion
(covered in a petri dish) → view under the o Proper specimen handling, preparation and transport (viability
microscope (10 fields HPF/OIF) of RBCs are very important; fresh samples should be collected
2. Wet (create a blood smear out of the solution) and should be processed/prepared right away)
Stain is still wet when supravital staining with o Red cell inclusions mistaken for reticulocytes
NMBN/BCB Heinz bodies (usually prepared via supravital staining)
Adding equal amounts of blood with NMBN/BCB → Howell-Jolly bodies
incubate for 5 mins (inside the clinical lab Pappenheimer bodies
incubation is 10-15 mins at 37⁰C for better uptake
of the stain) → place one drop of the mixture of
blood and stain in a glass slide → let it dry→
examine under the microscope
Note: supravital – staining while the cells are living;
not yet fixed
CALIBRATED MILLER DISK
o Reticulocyte (%) = Total Retic count in square A ×
100/Total RBC in square B × 9
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 19
LE CELL PREPARATION
• Detect presence of LE cell for diagnosis of SLE
• LE Cell
o Neutrophil that engulfed antibody-coated nucleus of another cell due to the production of antinuclear antibodies.
o Discovered by Malcolm Hargraves, Helen Richmond and Robert Morton (1948).
This ANA or LE factor which is present in serum actually destroys the nuclear protein and neutrophils eventually will
phagocytose the antibody coated nuclear material
• Smears
LE Cell
a. Zimmer & Hargraves
i. Macerate the blood clots using
mortar and pestle and the wire sieve • Homogenous nuclear material that are presumed
ii. Allow the clotted blood to pass to have been antibody coated already which are now
through the sieve by slowly phagocytosed by nuclear material of a neutrophil
macerating it • LE cell has already been lysed so it is more
iii. the maceration will actually homogenous
introduce the trauma to the WBCs if • often mistaken as TART CELLS
Blood clot preparation the ANA is present, this will trigger
the production of antibodies and Tart cell
then eventually the ANA will coat
some of the nuclear materials of the
WBCs the triggered neutrophils
will then phagocytose this antibody
coated nuclear material
b. Magath & Winkle
• Heterogenous nucleus
• Tart cells are not always clinically significant but then
it is seen in cases of infections or inflammations
• There is just an adjacent cells near another nuclear
material
LE cell: phagocytosed
Tart cell: no phagocytosis
Rotary/ Zinkam & Conley
Defibrinated method
Slide method Snapper & Nathan
Capillary tube method Mudick
• Serologic
DNP – use of latex beads that have been coated of deoxyribonucleic proteins. If agglutination happens then it is usually interpreted as a
positive test for the presence of ANA or the LE cell
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 20
ANTI-NUCLEAR ANTIBODY TEST
Detects ANA in patients adhering to reagent test cells forming distinct fluorescence pattern
Types of substrates
• Rat liver
• Multiblock substrates (combination of mouse stomach + rat liver + rat kidney)
Standard substrate before
• Hep-2: increased sensitivity
• Substrate being used now
• Cultured cells of laryngeal squamous cell carcinoma
• they are usually available commercially in the form of prefixed on glass slide drop the blood of the Px
on the glass slide where Hep 2 was prefixed Interpret
Interpretation
• Qualitative
POSITIVE/ negative
• Quantitative
o Last dilution with a (+) result is the titer
o Reporting:
-/+
Titer
Type of substrate
IF-ANA Pattern of fluorescence
Homogenous: - Characterized by total nuclear fluorescence due to antibodies that are derive
against the nucleoprotein
- Common in SLE, drug induced-SLE
Peripheral - Fluorescence occurs at the edges of nucleus in a shaggy appearance, the anti-
dna antibodies cause this pattern
- Common in SLE, and systemic sclerosis
Speckled - Result from antibodies that are directed against different nuclear antigens.
- They are often seen in SLE, mixed connective tissue diseases, systemic
sclerosis, Sjogren syndrome, polymyositis
Nucleolar - Results from antibody directed against a specific RNA configuration of the
nucleolus or an antibody that is specific for proteins that are necessary for
maturation of nucleolar RNA
- Systemic sclerosis, pyomyositis
Additional notes:
IF-ANA was introduced by George Friou (1957)
One of the widely used test for the diagnosis of not only SLE but most connective tissue diseases such as SLE,
polymyositis, dermatomyositis, Sjogren syndrome, lupoid hepatitis, rheumatoid arthritis
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 21
OSMOTIC FRAGILITY TEST
• Diagnosis of Hereditary Spherocytosis/ Hereditary Elliptocytosis
• Result of test may also be increased in hereditary stomatocytosis
• Principle
o Heparinized WB is added to decreasing concentration
of NaCl then incubated at RT or at 37ºC
• Incubated OFT
o 2nd method of OFT
o OFT that has been incubated at RT that will show normal
results are followed up with incubation
at 37ºC for 24 hrs.
o If the same results come out, the Px is interpreted as having normal OF
o Increase fragility: diagnostic of hereditary spherocytosis
• Prepare decreasing concentration of salt solutions (it depends on the procedure but usually it starts with 0.90 which is NSS)
• To the 0.9 NSS add several drops of distilled water to decrease the concentration of the NSS
• NSS is 0.90, you are going to add 1 drop of water to make it 0.75 2 drops on 0.65 tube 3 drops on 0.60, etc.
• The drop of distilled water will tend to decrease the concentration of salt in the solution.
• As we all know most cells survive or there is no osmosis that will happen if you are going to incubate blood in 0.9 NaCl but if you are going
to decrease the conc of NaCl, there will be a tendency for osmosis to happen because there will now be a movement of the solvent which is
water from an area of lesser conc. to greater conc.
o the water from the tubes will tend to go into the RBCsIf red blood cells are spherocytic, they cannot accommodate water anymore
easily lyse
When we are talking about OFT: it is about red blood cells that are not fragile, it means they are strong to invite more water
The larger the amt. of the red cell membrane or the surface area in relation to the size of the cell, the more the fluid the cell is able
to absorb or invite before they are able to rupture
DECREASED Reticulocytes
OFT Certain types of anemia (cells in IDA, thalassemic cells, sickle cell anemia)
After splenectomy when target cells are present
( liver disease, polycythemia vera, hemoglobinopathies)
Hemoglobinopathies: where you see target cells, so target cells are able to invite more
fluid because they are actually flat cells.
INCREASED Spherocytosis
OFT Elliptocytosis
Stomatocytosis
- These cells are in their maximum capacity in terms of solvent volume within the RBCs.
That’s the reason why when you incubate them in LISS, they will easily lyse
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 22
SICKLE CELL STUDIES
• Sickle cells: cells that are products of the presence of Hemoglobin S
• Sickle cell disease
o Either Sickle Cell Anemia (SCA)/ Sickle Cell Trait (SCT)
Sickle Cell Anemia - A phenomenon whereby you inherit both hemoglobin S genes from both parents
(SCA) - Px suffering from SCA: 80-100% Hgb S or homozygous inheritance
- Sickling phenomenon may lead to infections, dehydrations and hemolytic anemia also the excruciating
pain that may be suffered by patients
Sickle Cell Trait - Inherited disorder leading to the production of hemoglobin S but the inheritance is only from 1 parent
(SCT) - 20-40% inheritance of Hgb S
- No health issues
- Patients who are resistant to malarial infections
- More difficult to diagnose
o Inherited disorder
o Production of Hgb
• Sickling phenomenon
o Only happens in temporary state of hypoxia just like when they are infected with the malarial parasite
The malarial parasite will not be able to survive in this type of cells because they are devoid of oxygen as well as of
potassium.
Under temporary state of hypoxia, the cells assumed sickling phenomenon (rigid shape or the sickle shape) which leads
to blockage of blood vessels causing excruciating pain among the patients
o HgbS: arises from an altered or mediated S gene. This differs compared to Hgb A1 by one amino acid substitution. Just a mutation of
the beta-globin chain which contain 146 amino acids Hgb S production.
This single amino acid substitution which is actually valine substituting glutamic acid in the 6th position of the 146 AA
chain of the beta globin chain of the hgb Hgb S sickling phenomenon
Laboratory Methods
a. Scriver and Waugh: Sealed WB method Other sickling hemoglobin
Procedure Hgb CHARLEM
i. In order for temporary state of hypoxia to be initiated Hgb STRAVIS
ii. tie a rubber band around the finger that you are going to Hgb CZINGUINCHOR
puncture until the finger becomes lightly cyanotic
iii. perform finger puncture
iv. place drop of blood on slide and make a blood smear
v. stain with Wright stain
vi. look for sickle cells
b. Daland and Castle: Na metabisulphite method
Direct smear method
Procedure
i. Do finger puncture
ii. Mix a drop of blood with a drop of Na metabisulphite
- Na metabisulphite: deep oxygenating reagent which
will remove the oxygen from blood
iii. Make a smear of the sample
iv. Stain with wright stain
v. Look for sickle cells
Sickle cells: diagnostic for Sickle Cell Anemia
Dithionite solubility test
- Not commonly use
Turbidimetric - Uses dithionite solubility reagent
- Increase turbidity due to the presence of Hgb S is interpreted as positive
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 23
HAM TEST ● Normal: RBCs do not lyse in LISS particularly a sugar
● Also known as Acid serum test / PNH test/ Serum lysis water solution which contain 9 to 10 ug sugar/100mL water
test ● If positive, confirm with Ham test
● Discovered by Dr. Thomas Hale Ham
- He demonstrated that RBCs in PNH were lysed KLEIHAUER-BETKE TEST
by the complement when normal serum is ● Measures fetal Hgb transferred from fetus to an Rh (-)
acidified or activated by alloantibodies mother’s bloodstream or amount of fetomaternal
● A reliable test for the diagnosis of PNH hemmorrhage
● PNH (Paroxysmal Nocturnal Hemoglobinuria) ● Acid elution - mother’s cells only
- Acquired clonal disorder or the RBCs of the - Pale staining
patient are abnormally sensitive to lysis by **Fetal cells: bright pink
complement present in the plasma ● To determine dose of Rh Ig
- Increased complement sensitivity of RBC - Prevent Rh antibodies
membrane
PRINCIPLE OF KLEIHAUER-BETKE TEST
- Signs & symptoms:
● Adult hemoglobin but NOT fetal hemoglobins are soluble in
➢ Hemoglobinuria during sleep
a citrate buffer with pH 3.2 and will elute out of the RBCs
➢ Jaundice
● After acid elution the ff. are seen
➢ Hemosiderinuria
● (+) Result: Lysis of RBCs in acidified serum samples with Maternal cells Pale staining
patient cell but is not present with normal cell
Fetal cells Bright pink
PRINCIPLE OF HAM TEST - Resistant to an acid
● Exposure of patient red cells to normal acidified serum at solution
lytic pH (6.5 to 7.0)
● Sample: EDTA-treated blood ● Used to determine the dose of Rhogam or Rh
immunoglobulin that will be given to the mother to prevent
the production of Rh antibodies
● Maternal blood is fixed on a slide w/ 80% ethanol
→treatment with citrate phosphate buffer → staining with
hematoxylin and eosin →fetal cells are stained; maternal
cells appear as light “O” cells → computation
● Computation:
𝑵𝑵𝑵𝑵. 𝒐𝒐𝒐𝒐 𝒇𝒇𝒇𝒇𝒇𝒇𝒇𝒇𝒇𝒇 𝒄𝒄𝒄𝒄𝒄𝒄𝒄𝒄𝒄𝒄 𝑭𝑭𝑭𝑭𝑭𝑭𝑭𝑭𝑭𝑭 𝒃𝒃𝒃𝒃𝒃𝒃𝒃𝒃𝒃𝒃 𝒗𝒗𝒗𝒗𝒗𝒗𝒗𝒗𝒗𝒗𝒗𝒗
=
𝑵𝑵𝑵𝑵. 𝒐𝒐𝒐𝒐 𝒂𝒂𝒂𝒂𝒂𝒂𝒂𝒂𝒂𝒂 𝒄𝒄𝒄𝒄𝒄𝒄𝒄𝒄𝒄𝒄 𝑴𝑴𝑴𝑴𝑴𝑴𝑴𝑴𝑴𝑴𝑴𝑴𝑴𝑴𝑴𝑴 𝒃𝒃𝒃𝒃𝒃𝒃𝒃𝒃𝒃𝒃 𝒗𝒗𝒗𝒗𝒗𝒗𝒗𝒗𝒗𝒗𝒗𝒗
● It is assumed that 1 fetal cells = 20 mL mother’s blood
volume
BONE MARROW STUDIES
CAUSES OF FALSE-POSITIVE RESULT IN HAM TEST
INDICATIONS
1. Use of old serum of the patient
● Evaluation of:
2. Recent transfusion of blood to the patient
- Specimen cellularity or types of cells present in
Note:
the bone marrow
● Verification method: Heated serum of the patient can also
- Marrow architecture or make-up and
be used at 56 degrees Celsius
cytochemistry of the bone marrow
● Heating the sample at 56 degrees Celsius inactivates the
● Utilized in chromosomal culture and determination of the
complement hence there will be no hemolysis both in the
cellular makeup of the components of the bone marrow
control and the PNH patient
● Disease/s that are diagnosed using this method:
SUGAR WATER SCREENING TEST - Leukemia
● Also a test for PNH
METHODS OF COLLECTION
● Whole blood is mixed with sugar water solution or low ionic
1. Aspiration
strength solution ➜ incubate at room temperature - Jamshidi needle: special needle where
percutaneous aspiration of a bone marrow is
Low ionic strength solution performed
● Promotes binding of complement components (C3) to RBC
surface
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 24
Common sites of percutaneous
aspiration NITROBLUE TETRAZOLIUM TEST (NBT)
● aka “Neutrophil reduction test”
Adults ● Posterior iliac crest ● Test that distinguishes bacterial infection and CGD
● Spinous processes of the ribs
Bacterial Infection Reduction of NBT to formazan
● Vertebra
● Sternum CGD (Chronic No reduction of NBT to
- Not always used due Granulomatous Disease) formazan
to its location being ** Formazan - black dye
near to the heart
Metabolic defects of
neutrophils
Infants ● Head of the tibia
SPECIMEN
● Heparinized whole blood
2.
Biopsy
PROCEDURE
- Open trephine
● Involves making of smear of blood that was incubated with
- Sample of the core of the bone marrow is
NBT dye
obtained
- Usual site of collection: Posterior iliac crest / hip
bone Reduction ● Presence of black colored
METHODS OF EXAMINATION (NBT➜ Formazan) neutrophils
1. Smear Preparation
No reduction ● Normal neutrophils
Thin direct ● Aka “Imprint”
smear ● Usually done on glass Note: This test is not performed if the patient’s neutrophil count is
slides low. Hence, it is only performed if neutrophilia is present in the
● Usually stained with smear.
RED CELL ZINC PROTOPORPHYRIN TEST
- Wright’s stain
● Confirmatory diagnosis of Iron Deficiency Anemia
or;
(IDA)
- Hematoxylin &
Eosin ➢ IDA: there is decreased iron that would be taken
up by precursor cells of RBCs → meaning the
Particle smear ● The sample is crushed mature RBCs may have increased free
between two glass slides erythrocyte protoporphyrin → since there is no
● Either the aspirate or the iron we look for the free radicals scavenger zinc
biopsy bone marrow → there will be increased zinc free erythrocyte
collection method is used protoporphyrin present in the RBCs → presence
of zinc protoporphyrin will react with the
Concentrate ● Aka “Buffy coat smear” protofluor reagent which will be detected using
smear ● Sample is obtained from the protofluor-Z-Hematofluorometer
the buffy coat layer
➢ Result: Increased zinc protoporphyrin →
Note: In bone marrow studies, the most recommended or indicates IDA
best stain are: (1) Wright’s stain (smear) and (2) H & E ● Screening for lead poisoning
stain (histologic samples) ● Protoflour-Z-Hematofluorometer
2. Histologic - Uses Protoflour reagent
● Usually done for histologic examinations of bone
GEL ELECTROPHORESIS
marrow sample
● In Hgb electrophoresis, the red cell lysate is subjected to
● Fixative: Zenker’s
electrical fields under alkaline or acidic pH
● Stain: Hematoxylin & Eosin
● Alkaline gel → Cellulose acetate
CRITERIA THAT INDICATE PROPER COLLECTION OF BONE ● Acidic gel → Citrate agar
MARROW SAMPLES ● This can be carried out in a:
1. Presence of 1 to 3% of fat cells - Filter paper
- Absence of fats indicates dry tap or improper - Cellulose acetate membrane
marrow collection - Starch gel
2. Presence of 5 to 8% of nucleated RBCs - Citrate gel
- Agarose gel
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 25
●
The separation of different Hgbs is dependent on the
Region Hemoglobin Present
charge of Hgb molecule
● Change in the amino acid composition of the globin chains Alkaline gel electrophoresis
will result in the alteration of the charge of Hgb molecule →
leading to a change in the speed of migration of the Hgb Top band (farthest from Hb H
molecule origin: H lane) Hb I
**fastest to migrate
● This test if for the diagnosis of different Hgb variant
METHODS J Lane Hb J
Hb Bart’s and Hb N are
pH between Hb J and Hb H lanes
1. Cellulose 8.2 to 8.6 ● Hgb is negatively A Lane Hb A
Acetate at an charged and will F Lane Hb F
alkaline pH migrate toward the
anode (+) S Lane Hb S
● Most common pH: 8.4 Hb D
Hb G
2. Citrate Agar 6.0 to 6.2 ● Confirmation for Hb Lepore
Electrophoresi variant hemoglobins
C Lane Hb C
s ● Differentiate
Hb E
- S from D and G Hb O
- C from E, O ARAB Hb A2
and CHARLEM Hb S/G hybrid
Carbonic anhydrase band Hb G2
(faint) Hb A2
**band nearest the origin Hb CS
Acid gel electrophoresis
- Used to differentiate Hgb S from Hgb D and G since in
alkaline gel Hgb S, D, G, are all found in S lane.
Top band (farthest from Hb C
origin)
C Lane
S Lane Hb S
Note: Hgb S is more clinically significant than Hgb D and Hgb G. Hb S/G hybrid
Hence, further test using citrate agar must be performed to separate Hb O and Hb H are between S
Hgb S from Hgb D and G. If Hgb S is still present it is indicative of the and A lanes
presence of Hgb S.
Note: Hgb S is the fastest in
acid gel electrophoresis as
compared to alkaline gel
electrophoresis
A Lane Hb A
Hb E
Hb A2
Hb D
Hb G
Hb Lepore
Hb J
Hb I
Hb N
Hb H
MIGRATION OF VARIOUS HEMOGLOBIN BANDS IN ALKALINE
GEL AND ACID GEL ELECTROPHORESIS F Lane Hb F
● Different hemoglobins will migrate at different speed Hb Hope
Hb Bart’s
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 26
HIGH-PERFORMANCE LIQUID CHROMATOGRAPHY ANION EXCHANGE MICROCHROMATOGRAPHY
Weak cation exchange column system; a sample of RBC Detection of hemoglobin A2 levels
lysate buffer is injected into the system → application of Elevated levels indicate beta thalassemia
mobile phase (the hemoglobin variants can interact (homozygous/trait)
between the stationary phase and mobile phase) → the heading
eluted hemoglobin with different hemoglobin variant will be TEST FOR UNSTABLE HEMOGLOBIN
detected by light absorbance
Unstable hemoglobins (globin mutations)
The time required for the hemoglobin variants to elute is
o Hemoglobin variants with amino acid deletion or
referred to as retention time (for each hemoglobin variant
substitutions have weakened the binding forces
there is a specific retention time that would differentiate it
to maintain the hemoglobin structure
from the others)
Mutations may lead to precipitation of
o Identification of more hemoglobin variants that
hemoglobin (decrease solubility →
were not detected by gel electrophoresis
precipitation→ decreases the survival
Disadvantage
time of the RBC)
o Carry-over of specimen – when HPLC is used
o Inherited as autosomal dominant disorder
and the first specimen with sickle cell disease a
o May lead to anemia with reticulocytosis
small peak will be seen at the S window in the
o Mostly with mild compensated anemia/ mild
next specimen that can lead to diagnostic
reticulocytosis – may show sever chronic
confusion and the sample to be rerun or it may
hemolysis with splenomegaly and jaundice
also result to false positive result
Some have severe hemolytic type of
anemia
Approximate Retention Times of Various Hemoglobins in o Example
HPLC Analysis Hemoglobin H (homotetramer of beta
Approximate Hemoglobin globin chains), Hemoglobin Bart’s
Retention (homotetramers of gamma globin
Time (Min) chains), hemoglobin M, hemoglobin
0.7 (Peak 1) Acetylated Hb F, Hb H, Hb Bart’s, bilirubin Köln, Hemoglobin Zurich –
1.1 Hb F hemoglobins usually seen in α-
1.3 (Peak 2) Hb A1c, Hb Hope thalassemia
1.7 (Peak 3) Aged Hb A (Hb A1d), Hb J, Hb N, Hb I
2.5 Hb A, Hb S1c
ISOPROPANOL PRECIPITATION TEST
3.7 Hb A2, Hb E, Hb Lepore, Hb S1d
3.9-4.2 Hb D, Hb G Detection of unstable hemoglobins
4.5 Hb S, Hb A20, Hb C1c Normal: Hgb precipitation in a 17% isopropanol solution
Hb O Arab has a broad range from 4.5 to 5 after about 40 mins
min Unstable hgbs begin to precipitate in 5 mins and show
4.6-4.7 Hb G2 heavy flocculation in 20 mins
4.9 Hb C (preceding the main peak is a small
peak, Hb C1d), HEAT STABILITY TEST
Hb S/G hybrid, Hb CS (three peaks: 2_3%) Mix then heat hemolysate and buffer (TRIS buffer –
maintain buffer at pH 7.2) at 50 ⁰C
Hydrophobic bond/ force are weakened → decrease
stability of hemoglobin molecule
Under controlled conditions, unstable hemoglobins will
precipitate while stable hemoglobins will remain in the
solution
Interpretation: unstable Hgbs precipitate within 60 mins and
heavy flocculation is seen at 120 mins, normal result show
minimal flocculation
Sample used: EDTA treated whole blood
HEINZ BODY PREPARATION
Most unstable hemoglobins may show precipitated
hemoglobins in RBCs and the most commonly
encountered manifestation is Heinz bodies
Prevention of oxidation of hemoglobin – 2 aspects that
X axis – retention time (mins) should not be oxidized
Y axis – light absorbance (manifest the peak of the elution time of the 1. Iron in the heme molecule
different hemoglobins) 2. Sulfide group in the globin molecule - oxidation will result to
precipitated hemoglobins and will only occur when the
glycolytic enzymes were able to prevent the oxidation →
Heinz body formation (late sign of oxidative damage;
represents the degradation products of hemoglobin)
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 27
Usually seen in post splenectomy patients, chemical
poisoning, drug toxicity, G6PD deficiency BASOPHIL COUNT
Specimen: heparinized/EDTA – treated whole blood COOPER & CRUICKSHANK
Crystal violet/ methyl violet – supravital staining Stain: Toluidine blue (metachromatic stain that stains the
Acetylphenylhydrazine heparin component basophils) – heparin
May lead to hemolytic anemia because it may hinder the Basophil color: purple red
flexibility and deformability of the RBCs → RBC passing
through microvasculature = bite cells/ rupture of the RBC NEUTRAL RED STAIN
→hemolysis
Supravital staining technique; stains the heparin and
↑ Heinz bodies in the circulation = Heinz body hemolytic
histamine components of basophils
anemia
Basophil color: Red
HEMOGLOBIN H PREPARATION # 𝑜𝑜𝑜𝑜 𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐 /𝑚𝑚𝑚𝑚3 = 𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐 𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐 × 𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑𝑑 𝑓𝑓𝑓𝑓𝑓𝑓𝑓𝑓𝑓𝑓𝑓𝑓
Detect presence of four β in α-thalassemia × 𝑣𝑣𝑣𝑣𝑣𝑣𝑣𝑣𝑣𝑣𝑣𝑣 𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐𝑐 𝑓𝑓𝑓𝑓𝑓𝑓𝑓𝑓𝑓𝑓𝑓𝑓
Hgb H precipitates (multiple pale staining greenish blue
spherical inclusions) when exposed to BCB or NMBN; can
be mistaken as Howell jolly body/ reticulocytes
Specimen: EDTA-treated blood
3 drops of BCB + 3 drops of EDTA treated blood →
incubate for 2 hours at 37⁰C → create a smear→ air
dry→ examine under the microscope (OIO)
In hemoglobin H disease about 10% of the cells or more
will develop inclusions
.01%-1% may be seen in α-thalassemia trait and
myelodysplastic syndrome
ASCORBATE-CYANIDE SCREENING TEST
Non-specific screening procedure for detecting deficiencies
in the pentose phosphate pathway (PPP)
(+): G-6-PDH deficiencies
Incubate blood with ascorbate-cyanide
LOBE CELL COUNT
EOSINOPHIL COUNT
Use of special hemocytometer (Fuchs Rosenthal counting
chamber/ Speirs levy counting chamber)
Diluting fluid: propylene glycol or distilled water
Stain/Dye: eosin, flusin
Acetone may be used to prevent the lysis of eosinophils
Most common methods used are method by Pilot,
Friedman method and Randolph Method
Clinical Significance:
Eosinophilia - found in parasitism and allergies
Eosinopenia – seen in hyperadrenalism (Cushing syndrome)
EOSINOPHIL DEPRESSION TEST/ THORN TEST
Utilizes eosinophil count
Antiquated test for adrenal function
Collection of 2 blood samples; 1st collect Fasting Blood
Sample → after the first collection, 25mg of
adrenocorticotropic hormone (ACTH) will be administered
(IM) to the px→ after 4 hours, 2nd sample is collected →
perform eosinophil count on both samples
Hyperadrenalism and hypoadrenalism may be distinguish
with the use of this test
Normal result: 50% decrease in the original eosinophil
count
o No decrease in the original eosinophil count is
manifested by hypoadrenalism
o No decrease in the second sample -
hypoadrenalism/ Addison’s disease
o Drastic decrease of more than 50% in the second
sample – hyperadrenalism (Cushing’s syndrome)
COLLATED BY: ♣ ♠ ♥ ♦ Hematology 1 28
You might also like
- Preclinical Physiology Review 2023: For USMLE Step 1 and COMLEX-USA Level 1From EverandPreclinical Physiology Review 2023: For USMLE Step 1 and COMLEX-USA Level 1No ratings yet
- Hema Transes 1Document13 pagesHema Transes 1Nico LokoNo ratings yet
- MCQS FOR DIPLOMA HAEMATOLOGYDocument11 pagesMCQS FOR DIPLOMA HAEMATOLOGYSAMMY91% (11)
- Plasma Physiology (1-2020) by DR Khaled A AbulfadleDocument9 pagesPlasma Physiology (1-2020) by DR Khaled A AbulfadleUzama Binu AliNo ratings yet
- MLS305 Hema Lab PrelimsDocument11 pagesMLS305 Hema Lab PrelimsEvanka BaguistanNo ratings yet
- HEMA-LEC-COVER2COVERDocument61 pagesHEMA-LEC-COVER2COVERPrincheska TallaNo ratings yet
- Clinicalenzymology 220623200711 Deeb284aDocument8 pagesClinicalenzymology 220623200711 Deeb284aRahul guptaNo ratings yet
- BloodDocument127 pagesBloodyapyihao2No ratings yet
- Human Physiology Objectives WAPT 2022Document15 pagesHuman Physiology Objectives WAPT 2022ExcelNo ratings yet
- Mod 1Document26 pagesMod 1SEAN MELNOR LOSBAÑESNo ratings yet
- Presentation On Project Report: Practical in Biochemistry, Pathology and MicrobiologyDocument33 pagesPresentation On Project Report: Practical in Biochemistry, Pathology and Microbiologybharathi novalNo ratings yet
- The Measurement of Serum Osmolality and Its Application To Clinical Practice and Laboratory: Literature ReviewDocument8 pagesThe Measurement of Serum Osmolality and Its Application To Clinical Practice and Laboratory: Literature ReviewAkbar TaufikNo ratings yet
- Hema Lec Trans PrelimDocument28 pagesHema Lec Trans PrelimSarah EugenioNo ratings yet
- HematopoiesisDocument32 pagesHematopoiesisRenad AlharbiNo ratings yet
- Functions of Blood in 40 CharactersDocument29 pagesFunctions of Blood in 40 CharactersShobhit GajbhiyeNo ratings yet
- M5 AnaphyLec DigestDocument15 pagesM5 AnaphyLec DigestLaedyn Faye IsipNo ratings yet
- Introduction To Hematology-1Document44 pagesIntroduction To Hematology-1Sri DurgaNo ratings yet
- Assignment ProteinDocument15 pagesAssignment ProteinAnnabela Dewi Amor ValentinaNo ratings yet
- Plasma Proteins by U.Sivakumar: 1 PhysiologyDocument23 pagesPlasma Proteins by U.Sivakumar: 1 PhysiologyAkash JaatNo ratings yet
- Introduction To HematologyDocument2 pagesIntroduction To HematologyMary Joy HersaliaNo ratings yet
- What is Blood and its ConstituentsDocument16 pagesWhat is Blood and its Constituentseman el saeedNo ratings yet
- Microscopic Identification of BloodstainsDocument5 pagesMicroscopic Identification of BloodstainsNormalyn Andres MacaysaNo ratings yet
- BloodDocument32 pagesBloodPushpa AdhikariNo ratings yet
- Rate of Reticulocyte Release Rate of Removal of Spent Rbcs by Spleen & LiverDocument4 pagesRate of Reticulocyte Release Rate of Removal of Spent Rbcs by Spleen & Liverraiansuyu2495gmail.comNo ratings yet
- 7 5 16 Physiology of Red Blood CellsDocument72 pages7 5 16 Physiology of Red Blood CellsJoshua NyazonNo ratings yet
- Introduction to Common Clinical Lab TestsDocument4 pagesIntroduction to Common Clinical Lab TestsPrincess EscandalloNo ratings yet
- Blood: A. Erythrocytes or Red Blood Cells (RBCS) B. Leukocytes or White Blood Cells (WBCS) C. Thrombocytes or PlateletsDocument10 pagesBlood: A. Erythrocytes or Red Blood Cells (RBCS) B. Leukocytes or White Blood Cells (WBCS) C. Thrombocytes or PlateletsVictor HechanovaNo ratings yet
- Hematology: AbbreviationsDocument5 pagesHematology: AbbreviationsReyven Niña DyNo ratings yet
- BloodDocument70 pagesBloodbookaccountNo ratings yet
- Plasma Proteins: Functions and Clinical ImportanceDocument72 pagesPlasma Proteins: Functions and Clinical Importancereuben kwotaNo ratings yet
- Final PrelimsDocument13 pagesFinal PrelimsLesly Marie LaxamanaNo ratings yet
- Lesson 1-2Document5 pagesLesson 1-2Lesly Marie LaxamanaNo ratings yet
- HaematologyDocument260 pagesHaematologydatitox100% (1)
- Introduction To HematologyDocument2 pagesIntroduction To HematologyJohn Rick OrineNo ratings yet
- VSP-UG-1 (Blood)Document70 pagesVSP-UG-1 (Blood)Samartha SamdarshiNo ratings yet
- Mtap Hema MergedDocument86 pagesMtap Hema MergedAndrea Faye MONTERONANo ratings yet
- Selective B2-Adrenergic Agonists:: Mode of ActionDocument9 pagesSelective B2-Adrenergic Agonists:: Mode of ActionAda JoraimiNo ratings yet
- Midterm Topics Hema 1 LecDocument37 pagesMidterm Topics Hema 1 Lec4jzbxz64kqNo ratings yet
- Haemostatic Activity of Ethamsylate and Aminocaproic Acid Adsorbed Poly@-Hydroxyethyl Methacrylate) ParticlesDocument6 pagesHaemostatic Activity of Ethamsylate and Aminocaproic Acid Adsorbed Poly@-Hydroxyethyl Methacrylate) ParticlesKovacs Ferenc DavidNo ratings yet
- Week 9 Blood (P) Lecture 1Document18 pagesWeek 9 Blood (P) Lecture 1Fathimath iba AhmedNo ratings yet
- BloodDocument6 pagesBloodCrazy StrangerNo ratings yet
- 8 Blood ChemistryDocument10 pages8 Blood ChemistryAlexandra DalisayNo ratings yet
- Clinical Centrifuge Sample Prep Application Note ANCFGCLINICALBENCHDocument8 pagesClinical Centrifuge Sample Prep Application Note ANCFGCLINICALBENCHabasNo ratings yet
- Name - Soni Ritika Rajesh, Group - GM20-054-2A Physiology Week 03 TasksDocument10 pagesName - Soni Ritika Rajesh, Group - GM20-054-2A Physiology Week 03 TasksRitika SoniNo ratings yet
- Red Blood Cells "Best Module Ever"Document4 pagesRed Blood Cells "Best Module Ever"Jose Emmanuel Dolor100% (1)
- PHY LE 2 Finals ReviewerDocument22 pagesPHY LE 2 Finals Reviewerroxanne.viriNo ratings yet
- Human Histology Lecture on Blood Components and FunctionsDocument4 pagesHuman Histology Lecture on Blood Components and FunctionsJazyl TanNo ratings yet
- Blood Physiology GuideDocument14 pagesBlood Physiology GuideRimsha MustafaNo ratings yet
- 2 - Midterrm MLSPDocument5 pages2 - Midterrm MLSPAllen Rivera ReyesNo ratings yet
- Physiology-1: Chapter 1: Autonomic Nervous SystemDocument34 pagesPhysiology-1: Chapter 1: Autonomic Nervous SystemMustafa SaßerNo ratings yet
- Chapter 4 Blood Coagulation and Coagulation Disorders _32f6d4d0c67589df3863ad91f445f357Document27 pagesChapter 4 Blood Coagulation and Coagulation Disorders _32f6d4d0c67589df3863ad91f445f357daisysintszwaiNo ratings yet
- L - 28-Composition and Function of Blood. ( (L32) )Document28 pagesL - 28-Composition and Function of Blood. ( (L32) )Turky TurkyNo ratings yet
- Blood Composition and FunctionsDocument94 pagesBlood Composition and FunctionsNikita SebastianNo ratings yet
- Physiology I Blood & Immunity: 1-PlasmaDocument12 pagesPhysiology I Blood & Immunity: 1-Plasmanadine azmyNo ratings yet
- Blood Module I - Pallor, Swelling & FeverDocument20 pagesBlood Module I - Pallor, Swelling & FeverEdward XiamNo ratings yet
- PBBS502 Lecture3 Blood ProteinsDocument10 pagesPBBS502 Lecture3 Blood ProteinsleahbayNo ratings yet
- Hematology ReviewerDocument12 pagesHematology ReviewerPatty RomeroNo ratings yet
- Hematologia Del RatónDocument17 pagesHematologia Del RatónRodrigo Ignacio Gacitúa OpazoNo ratings yet
- Bioc416 PDFDocument53 pagesBioc416 PDFrJ100% (2)
- Blood and Bloodstains: Harry Danny L. Aspillaga Instructor Forensic Chemistry and ToxicologyDocument50 pagesBlood and Bloodstains: Harry Danny L. Aspillaga Instructor Forensic Chemistry and ToxicologyHarry Danny AspillagaNo ratings yet
- Understanding Lab Values : InstructionsDocument9 pagesUnderstanding Lab Values : InstructionssinnetrbNo ratings yet
- NSSBIO3E SB1B Ch08 e PDFDocument60 pagesNSSBIO3E SB1B Ch08 e PDFr6 obiNo ratings yet
- Your Dog's Lab Tests DecodedDocument3 pagesYour Dog's Lab Tests DecodedUmesh GopalanNo ratings yet
- Study Data Reviewer's Guide: LDCP, Inc. Study LDCP-0242-005Document15 pagesStudy Data Reviewer's Guide: LDCP, Inc. Study LDCP-0242-005anon_181306460No ratings yet
- Training Resources: Unicel DXH 800 Coulter Cellular Analysis System Training ResourcesDocument56 pagesTraining Resources: Unicel DXH 800 Coulter Cellular Analysis System Training ResourcesHadi BitarNo ratings yet
- BLOODDocument5 pagesBLOODSora TensaiNo ratings yet
- Complete Blood Picture ReportDocument1 pageComplete Blood Picture Reportvanitha vemulaNo ratings yet
- LPL - Pasricha Diagnostics & Ultrasound ClinicDocument4 pagesLPL - Pasricha Diagnostics & Ultrasound ClinicJohnnieNo ratings yet
- Differential White Blood Cell CountDocument20 pagesDifferential White Blood Cell CountNada hasan100% (2)
- Aplastic Anemia Case Study FINALDocument53 pagesAplastic Anemia Case Study FINALMatthew Rich Laguitao Cortes100% (6)
- Immune System GlossaryDocument4 pagesImmune System GlossaryLorena Lévano BastoNo ratings yet
- HEMATOLOGYDocument36 pagesHEMATOLOGYMA. ANDREA NICOLE BITOINNo ratings yet
- HeamatologyDocument45 pagesHeamatologypikachuNo ratings yet
- Key Elements of Immunity: SpecificityDocument9 pagesKey Elements of Immunity: SpecificityParth KulkarniNo ratings yet
- Platelet Diluting Fluid ProcedureDocument1 pagePlatelet Diluting Fluid ProcedureJohnree A. EvangelistaNo ratings yet
- Hema Summary NotesDocument42 pagesHema Summary NotesJustine Joy Remotigue MantosNo ratings yet
- Microscopic Examination of Urine LectureDocument21 pagesMicroscopic Examination of Urine LectureDiana IliescuNo ratings yet
- Immuno Notes LectureDocument30 pagesImmuno Notes LectureSteph TabasaNo ratings yet
- Spots For Hematology PracticalDocument17 pagesSpots For Hematology PracticalPhysiology by Dr RaghuveerNo ratings yet
- MLT MCQDocument13 pagesMLT MCQRamesh Rangu88% (8)
- What Is LeukopeniaDocument8 pagesWhat Is LeukopeniaMustafa AlmasoudiNo ratings yet
- White Blood Cells and Its Disorders: Key PointsDocument24 pagesWhite Blood Cells and Its Disorders: Key PointsskNo ratings yet
- Bone Marrow Hematopoiesis ReviewDocument7 pagesBone Marrow Hematopoiesis ReviewMarc ViduyaNo ratings yet
- Manish 1Document1 pageManish 1Manish kumarNo ratings yet
- He Hematologic System: Bone MarrowDocument5 pagesHe Hematologic System: Bone MarrowPatricia Mae Loyola FerrerNo ratings yet
- Pneumonia Case StudyDocument49 pagesPneumonia Case StudyJohn Paul Farofil Reproto100% (3)
- HPCT-1-Intro To General Pathology PDFDocument6 pagesHPCT-1-Intro To General Pathology PDFRochellane Ramos PlasabasNo ratings yet
- Anaphy Midterm Notes (The Blood Summary)Document4 pagesAnaphy Midterm Notes (The Blood Summary)Zosia Sage100% (1)
- Blood Group 3Document29 pagesBlood Group 3Hamirie JoshuaNo ratings yet