Professional Documents
Culture Documents
(Ofi) Respiratory System
Uploaded by
Pimpam0 ratings0% found this document useful (0 votes)
6 views12 pagesCopyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views12 pages(Ofi) Respiratory System
Uploaded by
PimpamCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 12
RESPIRATORY SYSTEM -done MUSCES OF RESPIRATION ACCESSORY MUSCLES Shortness of Breath
• Muscles of the thoracic cage • Scalene Chest Pain with Breathing
• Diaphragm • Sternocleidomastoid Past History of Respiratory Infection
MODULE 1: ANATOMY AND PHYSIOLOGY • Trapezius Smoking History
• Pectoralis Environmental Exposure
PRIMARY FUNCTIONS SECONDARY FUNCTIONS • Rectus abdominis Self-Care Behaviors
• Provides O2 for oxygen • Facilitates sense of smell PHYSICAL ASSESSMENT
metabolism in the tissues. • Produces speech FACTORS AFFECTING VENTILATION AND RESPIRATION Posterior Thorax and Lungs
• Removes CO2, the waste • Maintains acid-base balance • Air pressure A. Inspection
product of cellular metabolism • Maintains body water balance • O2, CO2 & H ion concentrations • Color
• Maintains heat balance • Airway resistance • Spine and mobility and any structural deformity
• Lung compliance • Symmetry of the posterior chest and posture and mobility of the
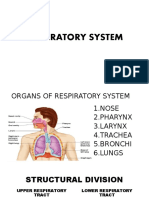
UPPER RESPIRATORY TRACT LOWER RESPIRATORY TRACT • Lung elasticity thorax on respiration
• Nose • Trachea • Alveolar surface tension • Note any bulges or retractions of the costal interspaces on
• Sinuses • Mainstem Branchi respiratory movement
- Pulmonary ventilation depends on the • Note the anteroposterior diameter in relation to the lateral
• Pharynx • Bronchioles
AIR PRESSURES volume changes within the thoracic cavity. diameter of the chest
• Larynx •Alveolar Ducts and Alveoli
- Pressures present in the thoracic cavity. B. Palpation
• Glottis/ Epiglottis • Lungs
2 phases of pulmonary ventilation: • Identify any areas of tenderness, masses and inflammation
• Pleural Membranes
• inspiration • Palpate the ribs for symmetry, mobility and tenderness and the
• expiration spine for tenderness and vertebral position
LUNG VOLUMES AND CAPACITIES
• Check for symmetric chest expansion
• Amount of air breathe during a quiet breathing; 500 ml - Respiratory changes in the medulla
• Check the tactile fremitus
- Tidal Volume O2, CO2 and H ion oblongata and pons of the brain and by
C. Percussion
concentrations the chemoreceptors located in the
• Amount of extra air inhaled beyond TV; 2000-3000 ml • Percuss the entire lung fields
medulla, carotid and aortic bodies.
- Inspiratory Reserve Volume • Assess diaphragmatic
-friction encountered as gases move along
extra air that can be exhaled after a forced breath; 1200 ml D. Auscultation
the respiratory passageway, by
- Expiratory Reserve Volume • Assess breath sounds
constriction of the passageways, by
• Assess voice sounds
• Amount of air moved on deepest inspiration and expiration; 3000- AIRWAY RESISTANCE accumulations of mucus or infectious
E. Inspection
5000 ml material and by tumors.
• Inspect for symmetry of the thorax, ribs and clavicles
- Vital Capacity - as resistance increases, gas flow
• Inspect skin color, lesions, hair distribution and note width of
• Maximum amount of air an individual can inspire after a normal decrease,
costal angle
expiration; 2500-3500 ml - The distensibility of the lungs.
• Note manner of breathing and any signs of respiratory difficulty
- Inspiratory Capacity - decreased by factors that decrease the
• Assess the respiratory rate, depth and symmetry
LUNG COMPLIANCE elasticity of the lungs, block the
• Amount of air that cannot be forcefully expired; 1000-1200 ml respiratory passageways or interfere with Anterior Thorax and Lungs
- Residual Volume the movement of the rib cage. A .Inspection
• Amount of air that remains in the alveoli even if the lung has • Inspect for symmetry of the thorax, ribs and
collapsed maybe because of trauma; 40% of RV ASSESSMENT clavicles
- Minimal Air • Inspect skin color, lesions, hair distribution and note width of
costal angle
• Total Lung Capacity INTERVIEW ASSESSMENT
• Note manner of breathing and any signs of respiratory difficulty
Cough
• Assess the respiratory rate, depth and symmetry
Sputum Production
B. Palpation Post-Procedure Nursing Care: - urge to cough, flushing, nausea or a salty taste
• General Palpation - Transport specimen stat - emergency equipment available
• Symmetrical Chest Expansion - Mouth care Post-Procedure:
• Assess Tactile Fremitus -A non-invasive test that registers arterial O2 - vital signs/ no BP taking for 24 hours in the affected extremity
C. Percussion PULSE Saturation (SaO2) - monitor peripheral neurovascular status
D. Auscultation OXIMETRY -Normal Values: 95-100% - encourage increase oral fluid intake/ IVF
• Assess Breath Sounds -Alert hypoxemia before clinical signs occur - assess for bleeding and dye reaction
• Assess Voice Sounds Procedure: -Also known as PLEURAL TAP.
TONE DESCRIPTION - a sensor is placed: finger, toe, nose or earlobe THORACENTESIS - Insertion of a hollow needle or similar
Flat soft intensity, high pitch, short duration - do not select an extremity with an impediment to blood flow instrument into the pleural cavity of the chest
*bones, large pleural effusion in order to drain pleural fluid, pus or air
Dull medium intensity, medium pitch and < 91% - immediate treatment Pre-Procedure:
duration SaO2 is < 85% - hypo-oxygenation - informed consent
*liver, pneumonia, tumor, pleural SaO2 is < 70% - life threatening situation - vital signs
effusion BRONCHOSCOPY -Visual examination of the larynx, trachea and - CXR or UTZ prior to the procedure
Resonance loud intensity, low pitch, long duration bronchi with a bronchoscope. - NPO if patient will receive sedation, otherwise local anesthesia is
*normal lung Pre-Procedure: given
Hyperresonance very loud, low pitch, longer duration - informed consent - assess coagulation studies
*emphysema, pneumothorax - NPO prior - upright position
- assess coagulation studies - do not cough, breathe deeply or move during the procedure
- remove dentures/ eyeglasses Post-Procedure:
MODULE 2: LAB & DIAGNOSTIC TESTS - prepare suction - vital signs/ respiratory status
- sedatives as ordered - pressure dressing
• Chest X-ray • Thoracentesis - have resuscitation equipment available - assess site for bleeding and crepitus
• Sputum Collection • Lung Biopsy Post-Procedure: - monitor for signs of complications
• Pulse Oximetry • Ventilation Perfusion Scan - vital signs -Indicated if CXR, CT-Scan or bronchoscopy
• Bronchoscopy • Skin tests - high-fowler's position LUNG BIOPSY have failed to identify the cause of pulmonary
• Pulmonary Angiography • Arterial Blood Gas Analysis (ABG) - assess gag reflex lesions
• Pulmonary Function Tests - monitor for bloody sputum Pre-Procedure:
- monitor respiratory status - informed consent
CHEST X-RAY - Information on the anatomic location and
- monitor for complications: bronchospasm, bronchial perforation, - NPO post NOC (midnight)
appearance
crepitus, dysrhythmia, fever, hemorrhage, hypoxemia and - CXR and blood studies
Pre-Procedure Nursing Care:
pneumothorax - anesthetic
- Remove jewelries and other metal objects
- notify MD if complications occur - pressure during insertion and aspiration
- Assess ability to inhale and hold breath
- Insertion of a fluoroscopy via the antecubital - analgesics and sedatives as ordered
- Question regarding pregnancy or possibility of pregnancy
PULMONARY or femoral vein into the pulmonary artery - keep calm and quiet
SPUTUM - Obtained by expectoration, tracheal ANGIOGRAPHY - Involves iodine, radiopaque, contrast Post-Procedure:
COLLECTION suctioning or bronchoscopy. material - vital signs
Pre-Procedure Nursing Care: Pre-Procedure: - pressure dressing
- Determine specific purpose - NPO/ Vital Signs - monitor for bleeding and respiratory distress
- Early morning sterile specimen - assess coagulation studies and renal system functioning - monitor for complications
- Rinse mouth with water prior to collection - establish an open line/ IV - CXR
- Take several deep breaths and then cough forcefully - administer sedation
- Collect specimen before giving antibiotics - client must lie still during the procedure
Types: - Pulmonary function laboratory citirizine
- Fine needle - common - Nose clip is applied to unsedated client then Act on the cough-control dextromethorphan
- Transbronchial PULMONARY breathes into a spirometer or body center in the medulla to codeine
- Open biopsy FUNCTION plethysmograph Antitussives suppress the cough benzonatate
VENTILATION -Determines the patency of the pulmonary TESTS - Using measured lung volumes, respiratory reflex.
PERFUSION airways. capacities are calculated to assess pulmonary -Not given long term
SCAN - 10 ml (air allowed) status (mimic)
*TLC: total volume of lungs at their maximum inflation; TV, IRV, ERV Relaxes the smooth
Pre-Procedure: and RV are used to calculate TLC muscles of the bronchi,
- informed consent *VC: IRV, TV and ERV bronchioles and
- assess allergies to dye, iodine or seafood *IC: TV and IRV Methylyxanthine pulmonary blood vessels
- remove jewelries *Functional Residual Capacity: volume of air left in the lungs after a s by inhibiting the enzyme theophylline
- review breathing methods normal exhalation; ERV and RV phosphodiesterase,
- IV access *Forced Expiratory Volume: amount of air that can be exhaled in -asthma resulting in an increase
- administer sedation 1 sec cAMP, which promotes
- emergency resuscitation equipment *Forced Vital Capacity: amount of air that can be exhaled forcefully bronchodilation
Post-Procedure: and rapidly after maximum air intake Stimulates beta 2 pirbutetol
- monitor reaction to radionuclide *Minute Volume: total amount of air breathe in 1 minute Beta 2 agonist receptors to cause albuterol
- handle body secretions carefully smooth muscles of the
- wash hands carefully with soap and water -bronchodilators
bronchi to relax
- Determine hypersensitivity Mast Cell Prevents the release of Cromolyn sodium
- Should be on the area without excessive body Stabilizer histamine and slow-
hair and dermatitis reacting substances of -
SKIN TESTS - Circle, document the date, time and test site anaphylaxis by bronchoconstriction
- Do not scratch nor wash -given as stabilizing the mast cell
- Assess for induration, erythema and preventive membrane, as a result,
vesiculation the stimulus for
- Tuberculin test/ PPD bronchospasm is
0-4 mm Not significant ✓ ACCUMULATION OF: reduced and
5 mm or greater HIV and close contacts of someone with bronchospasm is
active PTB. Fluids - Pleural effusion relieved
10 mm or greater Normal or mildly impaired immunity. Air - Pneumothorax Mucolytic Liquify and loosen thick Acetylcysteine
ARTERIAL - Measurement of tissue oxygenation, carbon Blood - Hemothorax mucus secretions so that ambroxol
BLOOD GAS dioxide removal and acid base balance. Pus - Empyema -nonproductive they can be
ANALYSIS (ABG) cough expectorated
Obtaining Specimen for ABG: Expectorant Thin mucus so it’s guaifenesin
- Do Allen's Test MODULE 3: DRUGS & SPECIAL PROCEDURES cleared more easily out
- Use heparinized syringe of airways; also soothe
- No bubbles in the syringe mucous membranes in
DRUG MOA EXAMPLE
- Send specimen on ice and occlude needle to prevent air from the respiratory tract
<nasopharyngeal diphenhydramine
coming in the syringe
secretions by blocking (IM/IV)
- Check site for hematoma, bleeding and pain SPECIAL PROCEDURE & DEVICE
Antihistamines the H1 receptors loratadine
(not cause zzz) • Chest tube thoracostomy
• Mechanical ventilator - apnea that is not readily reversible m. Due to loss of the protective reflexes (cough and swallowing)
- A flexible plastic tube is Respiratory Therapies: and loss of the tone of the pharyngeal muscles, which causes the
CHEST TUBE THORACOSTOMY inserted through the side of the • Oxygen therapy tongue to fall back and block the airway.
chest into the pleural space. • Incentive Spirometry
Indications: • Small-Volume Nebulizer (Mini-Nebulizer) Therapy ENDOTRACHEAL - Involves passing an endotracheal tube
- pneumothorax Oxygen therapy - provide adequate transport of oxygen in the INTUBATION through the nose or mouth into the trachea.
- pleural effusion blood while decreasing the work of breathing -PT cant talk.
- empyema and reducing stress on the myocardium. Complications:
Nursing Considerations: - Method of deep breathing that provides - Can occur from pressure exerted by the cuff on the tracheal wall.
- drainage tubing does not kink, loop or blocks pt’s movement. Incentive visual feedback to encourage the patient to - Cuff pressures should be maintained between 20 and 25 mm Hg
- encourage a comfortable position with good body alignment* Spirometry inhale slowly and deeply to maximize lung (24 to 30 cm H2O)
- there is fluctuation or "tidaling" of the fluid in the water seal inflation and prevent or reduce atelectasis. - high cuff pressure can cause: tracheal bleeding, ischemia, and
chamber in wet systems or check the air leak indicator for leaks in Indications: pressure necrosis,
dry systems with one-way valve* - used after surgery, especially thoracic and abdominal surgery, - Low cuff pressure can increase the risk of aspiration pneumonia.
- observe for air leaks in the drainage system - they are indicated by - to promote the expansion of the alveoli - Is a surgical procedure in which an opening
constant bubbling in the water seal chamber or by air leak indicator - to prevent or treat atelectasis is made into the trachea.
in dry systems with a one-way valve* - Handheld apparatus that disperses a TRACHEOSTOMY -The indwelling tube inserted into the
- observe and immediately report rapid and shallow breathing, Small-Volume moisturizing agent or medication such as a trachea is called a tracheostomy tube.
cyanosis, pressure in the chest, subcutaneous emphysema, Nebulizer (Mini- bronchodilator or mucolytic agent, into - after 2 weeks
symptoms of hemorrhage or significant changes in the vital signs Nebulizer) microscopic particles and delivers it to the -lifetime
- the chest tube is removed as directed when the lung has Therapy lungs as the patient inhales. rather than air Complications:
reexpanded* driven. - dislodgement,
- accidental decannulation,
- 3 chambers - a collection chamber, water EMERGENCY MANAGEMENT OF UPPER AIRWAY OBSTRUCTION - bleeding,
seal chamber and wet suction control - pneumothorax,
chamber. • Endotracheal Intubation - air embolism,
• Tracheostomy - aspiration,
Traditional Water *requires that sterile fluid be instilled into - subcutaneous mediastinal emphysema,
Seal (Wet water seal and suction chambers - recurrent laryngeal nerve damage,
CAUSES
Suction) *has positive and negative pressure release - posterior tracheal wall penetration.
a. food particles
valves. Long-term complications:
b. vomitus
*intermittent bubbling indicates that the - airway obstruction from accumulation of secretions
c. blood clots
system is functioning properly. - protrusion of the cuff over the opening of the tube,
d. or anything that obstructs the larynx or trachea.
*additional suction can be added by - infection,
e. enlargement of tissue in the wall of the airway
connecting system to a suction source. - dysphagia,
f. Epiglottitis
MECHANICAL - a positive or negative-pressure breathing - tracheal dilation,
g. obstructive sleep apnea
VENTILATOR device that supports ventilation and - tracheal ischemia, and necrosis.
h. laryngeal edema
oxygenation for a prolonged period of time. Tracheal stenosis may develop after the tube is removed.
.i. laryngeal carcinoma
Indications:
j. peritonsillar abscess
- continuous decrease in oxygenation (PaO2) MECHANICAL VENTILATOR
k. . thick secretions
- increase in arterial CO2 levels
l. patient with an altered level of consciousness from any cause
- persistent acidosis (decreased pH) TYPES OF MECHANICAL VENTILATOR
- conditions* that lead to respiratory failure • Positive-pressure ventilators
• Noninvasive positive-pressure ventilation (NIPPV) Pressure support - applies a pressure plateau to the airway - Promote Effective Airway Clearance
- inflate the lungs by exerting positive ventilation throughout the patient triggered inspiration. - Prevent Trauma and Infection
POSITIVE-PRESSURE pressure on the airway, pushing air in, Ventilators setting: - Promote Optimal Level of Mobility
VENTILATORS similar to a bellows mechanism, and forcing 1.tidal volume (6-10ml/kg or 4-8ml/kg for patients with ARDS) - Promote Optimal Communication
the alveoli to expand during inspiration. 2.Mode - Promote Coping Ability
NONINVASIVE a.CPAP – Continuous Positive Airway 3.FIO2 - Monitor and Manage Potential Complications
POSITIVE-PRESSURE Pressure 4.Rate
VENTILATION b.BiPAP – Bilevel PositiveAirway Pressure 5.PEEP if applicable MODULE 4: DISORDERS (PART 1)
(NIPPV) 6.Peak inspiratory pressure (PIP) – (Normal – 15-20cmH2O)
- a method of positive-pressure ventilation Increased = increased airway resistance or decrease compliance
UPPER RESPIRATORY TRACT INFECTION (URTI)
that can be given via facemasks that cover
COMPLICATION • Rhinitis
the nose and mouth, nasal masks, or other
• Rhinosinusitis
BiPAP – Bilevel oral or nasal devices such as the nasal pillow • Trauma
• Laryngitis
PositiveAirway (a small nasal cannula that seals around the • Fluid retention
• Acute Pharyngitis (sore throat)
Pressure nares to maintain the prescribed pressure) • Oxygen toxicity
• Tonsillitis and Adenoiditis
- it eliminates the need for endotracheal • Hemodynamic compromise
intubation or tracheostomy and decreases • Obstructive Sleep Apnea (OSA)
• Aspiration
the risk of nosocomial infections such as • Epistaxis (Nosebleed)
• Gastrointestinal ulceration (stress ulcer)
pneumonia. • Laryngeal Obstruction
-Damage to the lungs by positive pressure) can
Indication: BAROTRAUMA occur due to a pneumothorax, subcutaneous • Acute Tracheobronchitis
- acute or chronic respiratory failure emphysema or pneumomediastinum. -inflammation and irritation of the
- acute pulmonary edema VOLUTRAUMA - Damage to the lungs by volume delivered RHINITIS mucous membranes of the nose
- COPD - from one lung to the other). - may be acute or chronic, and allergic or
chronic heart failure nonallergic.
FLUID - can be due to decreased CO, activation of
- sleep-related breathing disorder e.g. OSA RETENTION RAAS Factors:
VENTILATOR MODES a. changes in temperature or humidity
- Can result from high concentrations of
- refers to how breaths are delivered to the patient b. Odors
OXYGEN oxygen (typically < 50%), long durations of
• A/C mode – Assist- control mode TOXICITY oxygen therapy (typically < 24 to 48 hr), c. Infection
• SIMV – synchronized intermittent mandatory ventilation and/or the client’s degree of lung disease.
d. Age
• Pressure support ventilation e. systemic disease
HEMODYNAMIC - can increase thoracic pressure (positive
A/C mode – Assist- - Provides full ventilator support by f. use of over-the-counter (OTC) and prescribed nasal
COMPROMISE pressure), which can result in decreased
control mode delivering a preset tidal volume and decongestants
venous return.
respiratory rate. g. presence of a foreign body.
ASPIRATION - Keep the head of the bed elevated 30° at all
- delivers a preset tidal volume and number May occur with:
times to decrease the risk of aspiration.
of breaths per minute. A. exposure to allergens such as Foods
GASTROINTESTIN - Ulcers can be evident in clients receiving
SIMV – - Between ventilator-delivered breaths, the B. medications
AL ULCERATION mechanical ventilation.
synchronized patient can breathe spontaneously with no C. particles in the indoor and outdoor
(STRESS ULCER )
intermittent assistance from the ventilator on those - Inflammation and congestion, with
mandatory extra breaths. RHINOSINUSITIS thickened mucous secretions filling the
ventilation - Because the ventilator senses patient sinus cavities and occluding the openings.
2 IMPORTANT GENERAL NURSING INTERVENTIONS
breathing efforts and does not initiate a Signs and symptoms:
1. pulmonary auscultation
breath in opposition to the patient’s efforts 1. Rhinorrhea (excessive nasal drainage, runny nose)
2. interpretation of ABG measurements
fighting the ventilator is reduced. 2. Nasal congestion (purulent with bacterial rhinitis)
- Enhance Gas Exchange
3. Sneezing 2. Epstein–Barr virus 2. Penicillins (first line therapy) or cephalosporins
4. Pruritus of the nose, roof of the mouth, throat, eyes and ears 3. herpes simplex virus. 3. Tonsillectomy – treatment of choice for Chronic tonsillitis
5. Headache – if rhinosinusitis is also present - Bacterial infection accounts for the remainder of cases NURSING MANAGEMENT:
Medical Management 1. Provide post-operative care
Bacterial invasion
1.Antihistamines – most common treatment - Continuous nursing observation (immediate postoperative and
↓
2.Oral decongestants – for nasal obstruction recovery periods) because of the risk of hemorrhage
Inflammatory response - pain, fever, vasodilation, edema, tissue
3.Saline nasal spray - Place patient on prone position with head turned to one side –
damage (redness, and swelling in the tonsillar pillars, uvula and
4.Intranasal corticosteroids – severe congestion to allow drainage from mouth and pharynx
soft palate.)
Patient Education: - Apply ice collar to the neck
Clinical Manifestations:
1. Avoid or reduce exposure to allergens and irritants. Educating Patients about Self-care:
1. fiery-red pharyngeal membrane and tonsils
2. Instruct the importance of controlling the environment at home -The patient and family must understand the signs and symptoms
2. lymphoid follicles that are swollen and flecked with white-
and at work. of hemorrhage (Bleeding may occur up to 8 days after surgery).
purple exudate.
3. Review the importance of influenza vaccination each year - older - The nurse instructs the patient about the use of liquid
3. enlarged and tender cervical lymph nodes, and no cough
adults and high risk populations. acetaminophen with or without codeine for pain control.
4. Fever (<38.3°C [101°F])
4. Review hand hygiene technique in case of infection. - Disorder characterized by recurrent
5. Malaise
- an inflammation of the larynx, often episodes of upper airway obstruction and
6. sore throat
LARYNGITIS occurs as a result of voice abuse or OBSTRUCTIVE SLEEP a reduction in ventilation.
Diagnostics:
exposure to dust, chemicals, smoke, and APNEA (OSA) - It is defined as cessation of breathing
1. Rapid antigen detection testing (RADT) - uses swabs that collect
other pollutants or as part of a URI (apnea) during sleep usually caused by
specimen from posterior pharynx and tonsil - 90-95% sensitive
Causes: repetitive upper airway obstruction.
2. Throat culture
1. isolated infection involving only the vocal cords Risk Factors:
Medical management:
2. gastroesophageal reflux (referred to as reflux laryngitis 1. Obesity – major risk factor
1. Viral pharyngitis – supportive measures
Clinical Manifestations: - a larger neck circumference and increased amounts of
2. Bacterial pharyngitis – penicillin (treatment of choice),
- hoarseness or aphonia (loss of voice) peripharyngeal fat narrow and compress the upper airway.
cephalosporins and macrolides
- severe cough. 2. male gender
Nutritional therapy: - Liquid or soft diet
Medical Management: 3. postmenopausal status
1. resting the voice TONSILLITIS AND - Tonsils frequently serve as the site of 4. advanced age
2. avoiding irritants (including smoking) ADENOIDITIS acute infection (tonsillitis) Pathophysiology:
3. resting and inhaling cool steam or an aerosol. Caused by: pharynx is a collapsible tube that can be compressed by the soft
- Sudden painful inflammation of the GABHS (bacterial) Epstein–Barr virus (viral) tissues and structures surrounding it
ACUTE PHARYNGITIS pharynx, the back portion of the throat Clinical Manifestations:
During sleep
(SORE THROAT) that includes the posterior third of the - sore throat
↓
tongue, soft palate, and tonsils. - Fever
The tone of the muscles of the upper airway is reduced
Causes: - Snoring
↓
1.Group A beta-hemolytic streptococcus (GABHS)/ group A - difficulty swallowing
Reduced diameter of the upper airway
streptococcus (GAS) or streptococcal pharyngitis. - Enlarged adenoids may cause: mouth breathing, earache, draining
↓
2.groups B and G streptococci, Neisseria gonorrhoeae, Mycoplasma ears, frequent colds, bronchitis, foul smelling breath, voice
pneumoniae, Arcanobacteriumhaemolyticum, and HIV (Randel, impairment, and noisy respiration.
Dynamic changes during sleep
2013). Diagnostics:
↓
Pathophysiology: - Primarily clinical
Obstruction
- Viral infection causes most cases of acute pharyngitis - Throat swab culture
Responsible viruses include: Medical Management:
These sleep-related changes may predispose to
1. adenovirus, influenza virus 1.Supportive measures – increase fluid intake, analgesics, salt-water
↓
gargles, rest
Upper Airway collapse PRECIPITATING MECHANISM OF OBSTRUCTION
↓ Nursing Management: EVENT
Apnea 1. Instruct the patient and family about treatments, including the History of allergies; exposure to anaphylaxis
↓ correct and safe use of CPAP, BiPAP, MAD, and oxygen therapy. medications, latex, foods, bee
Repetitive Apneic events - a hemorrhage from the nose stings.
↓ EPISTAXIS - caused by the rupture of tiny, distended Foreign body inhalation / ingestion of meat or
Hypoxia and hypercapnia (NOSEBLEED) vessels in the mucous membrane of any other food items, coin, chewing
Classic Signs and Symptoms (“3S”) area of the nose. gum, balloon fragment
1. snoring - loud Risk factors: Heavy alcohol consumption; Obstruction from tumor
2. sleepiness • Local infections (vestibulitis, rhinitis, rhinosinusitis) heavy tobacco use
3. significant-other report of sleep apnea episodes • Systemic infections (scarlet fever, malaria) Use of ACE inhibit Increased risk of Angioedema of
Symptoms typically progress with increase in weight and aging: • Drying of nasal mucous membranes the mucous membranes
1. Excessive daytime sleepiness • Nasal inhalation of corticosteroids (e.g., beclomethasone) or illicit History of surgery or previous Possible subglottic stenosis
2. Frequent nocturnal awakening drugs (e.g., cocaine) tracheostomy
3. Morning headaches • Trauma (digital trauma, blunt trauma, fracture, forceful nose Clinical Manifestations:
Diagnostics: blowing) - lowered oxygen saturation
1. Clinical features • Arteriosclerosis - use of accessory muscles
2. Polysomnographic find • Hypertension Assessment and Diagnostic Findings:
Medical Management: • Tumor (sinus or nasopharynx) 1.thorough history - can be very useful
- Weight loss, • Thrombocytopenia 2.emergency measures to secure the patient’s airway should not be
- avoidance of alcohol Use of aspirin delayed.
- positional therapy (using devices that prevent patients from Medical Management: Medical Management:
sleeping on their backs) - Depends on the cause and location - Medical management is based on the initial evaluation of the
- oral appliances – e.g. mandibular advancement devices (MADs) - Apply direct pressure patient and the need to ensure a patent airway
Surgical Management: - Nasal decongestants (phenylephrine) vasoconstrictors - allergic reaction = subcutaneous epinephrine and a corticosteroid
1. Simple tonsillectomy - patients with larger tonsils Nursing management: - Ice may be applied to the neck =reduce edema.
2. Uvulopalatopharyngoplasty - resection of pharyngeal soft tissue - monitors the patient’s vital signs - Continuous pulse oximetry
and removal of approximately 15 mm of the free edge of the soft - assists in the control of bleeding - an acute inflammation of the mucous
palate and uvula - provides tissues and an emesis basin to allow the patient to ACUTE membranes of the trachea and the
3. Nasal septoplasty - may be performed for gross anatomic nasal expectorate any excess blood TRACHEOBRONCHITIS bronchial tree, often follows infection of
septal deformities - assess the patient’s airway and breathing the upper respiratory tract.
4. Maxillomandibular surgery - may be performed to advance the Educating Patients about Self-care:
maxilla and mandible forward in order to enlarge the posterior - avoid vigorous exercise for several days Caused by:
pharyngeal region - avoid hot or spicy foods and tobacco (causes vasodilation and 1. Streptococcus pneumoniae, Haemophilus influenzae, or
5. Tracheostomy - relieves upper airway obstruction but has increase the risk of rebleeding) Mycoplasma pneumoniae,or a fungal infection (e.g.,Aspergillus)
numerous adverse effects, including speech difficulties and - avoid forceful nose blowing, straining, high altitudes, and nasal ↓
increased risk of infections. trauma (including nose picking Inflammation of bronchial mucosa
Pharmacologic Therapy: - Applying direct pressure to the nose for 15 minutes ↓
1. Modafinil - to <daytime sleepiness (Downey, 2015) - Obstruction of the larynx because of produces mucopurulent sputum
2. Protriptyline (Triptil) - given at bedtime may increase the edema - is a serious condition that may be
respiratory drive and improve upper airway muscle tone 2. inhalation of physical and chemical irritants = gases, or other air
LARYNGEAL fatal without swift, decisive intervention
3. Medroxyprogesterone acetate (Provera) and acetazolamide contaminants
OBSTRUCTION - It is an occasional cause of death in
(Diamox) used for sleep apnea associated with chronic alveolar ↓
severe anaphylaxis (angioedema).
hypoventilation. cause acute bronchial irritation
BRONCHIAL ASTHMA a. corticosteroids: prednisolone, prednisone
Clinical Manifestations: - Chronic inflammatory disease of the airways that causes airway b. mast cell stabilizers: cromolyn sodium, nedocromil
1. Dry, irritating cough and expectorates a scanty amount of mucoid hyperresponsiveness, mucosal edema and mucus production. c. long acting beta 2 adrenergic agonists: salmeterol (Serevent)
sputum d. leukotriene modifiers/ antileukotrienes: act by interfering with
2. Report of sternal soreness from coughing ETIOLOGY leukotriene synthesis or prevents its binding to receptor sites;
3. fever or chills - Environmental factors interact with inherited factors to produce montelukast (Singulair), zafirlukast (Accolate), zileuton (Zyflo)
4. night sweats the disease. e. methylxanthines: theophylline (Theo-Dur, Slo-bid)
5. headache ASTHMA TRIGGERS INTERVENTIONS FOR AN ACUTE ASTHMA ATTACK
6. General malaise • seasonal allergens: grass, tree, weed, pollens - assess airway patency
7. shortness of breath • perennial allergens: mold, dust, roaches, animal dander - administer humidified oxygen
8. noisy inspiration and expiration (inspiratory stridor and • airway irritants: air pollutants, cold, heat, weather changes, - administer rescue meds
expiratory wheeze) strong odors or perfumes, smoke - monitor respiratory status, pulse oximeter and color
9. purulent (pus-filled) sputum • exercise, stress, emotional upset - initiate IV line
10. blood-streaked secretions - due to mucosal airways irritation. • sinusitis with postnasal drip - prepare for CXR
Medical Management: • medications: aspirin, penicillin, beta blockers - prepare to obtain ABG and serum electrolytes
1. Antibiotic treatment may be indicated depending on the • viral respiratory tract infections NURSING MANAGEMENT
symptoms, sputum purulence, and results of the sputum culture • hyper allergenic food - chest physiotherapy
and sensitivity. ASSSESSMENT - allergen control
2. Antihistamines usually are not prescribed, because they can • cough: non-productive to productive - avoid extremes of temperature
cause excessive drying and make secretions more difficult to • dyspnea - avoid exposure to viral respiratory infection
expectorate. • wheezing - recognize early symptoms
3.Increase Fluid intake • diaphoresis - instruct patient in the administration of medications as treatment
Nursing Management : •mild apprehension and restlessness - adequate rest, sleep and a well-balanced diet
- is usually treated in the home setting • tachycardia and palpitation - adequate fluid intake
1. encourage bronchial hygiene • cyanosis and hypoxia - exercise as tolerated
- increased fluid intake - directed coughing to remove secretions - • hyperventilation
encourage and assist patient to sit up frequently to cough DIAGNOSTIC TESTS COPD
effectively • ABG: respiratory alkalosis to respiratory acidosis; hypoxemia aka Chronic Airflow Limitation
2. emphasize full course of antibiotics • Blood tests: eosinophilia, elevated IgE -Group of diseases including chronic bronchitis and emphysema or
3. rest COMPLICATION a combination of these disorders.
• status asthmaticus -Characterized by progressive airflow limitations into and out of the
• respiratory failure lungs, elevated airway resistance, irreversible lung distention and
DISORDERS (ADULT) • pneumonia ABG imbalance.
• Bronchial Asthma • Empyema • atelectasis
• COPD • ARDS • dehydration RISK FACTORS
- Chronic Bronchitis • CO Poisoning MEDICAL MANAGEMENT • exposure to tobacco smoke
- Emphysema • Histoplasmosis 1. Quick-relief medications • passive smoking
• Bronchiectasis • Sarcoidosis a. Short acting beta adrenergic agonists: albuterol (Proventil, • occupational exposure - ambient air pollution
• Pneumonia • Occupational Lung Diseases Pneumoconioses Ventolin), metaproterenol sulfate (Alupent), terbutaline sulfate • efficiency of alpha1 antitrypsin
-Pneumoconioses (Bricanyl) CHRONIC BRONCHITIS
b. anticholinergics: ipatropium bromide (Atrovent) Inflammation of the bronchi leading to increased mucus
c. systemic corticosteroids: prednisone production, chronic cough and eventual scarring of the bronchial
2. Long-acting control medications lining
Thickening due to excessive Consistent destruction of the - loss of elastic fibers causes collapse of small bronchioles and air
Presence of productive cough for at least 3 months in each of two mucus plug formation and alveoli and alveolar walls. trapping in the aveoli at the end of expiration
consecutive years rigidity of bronchi. MEDICAL MANAGEMENT
A. Pharmacologic Interventions
ASSESSMENT Narrowing of air passages. Enlargement of acini. 1. Bronchodilators
- productive cough -- relieve bronchospasm and reduce airway obstruction by
- dyspnea on exertion Reduction in the alveolar allowing increased O2 distribution throughout the lungs and
- hypercapnia diffusing space and some tissue improving alveolar ventilation
- cyanosis CHRONIC BRONCHITIS changes. - administered via MDI, USN, Oral
- anorexia and generalized body malaise a. beta 2 adrenergic agonists: act on the the beta 2 adrenoceptors
- pulmonary hypertension PULMONARY EMPHYSEMA in the smooth muscles of the airways and cause bronchodilation;
- polycythemia ASSESSMENT enhance mucus clearance and improve the endurance of
- recurrent RTI • dyspnea on exertion • wheezing respiratory muscles; albuterol (Proventil, Ventolin), metaproterenol
• productive cough • weight loss sulfate (Alupent)
EMPHYSEMA • barrel chest • orthopnea b. anticholinergics: block the cholinergic receptors located in the
abnormal and permanent distention of the air spaces beyond the • hyperresonant sound • use of accessory muscles larger airways resulting in bronchodilation; ipratropium bromide
terminal bronchioles, with destruction of the overdistended walls of • circumoral cyanosis • neck vein distention (Atrovent)
the alveoli • digital clubbing • pitting peripheral edema c. methylxanthines: enhance mucociliary clearance, stimulate the
• cor pulmonale central respiratory drive and improve lung function during sleep;
the end stage of a process that has progressed slowly for many DIAGNOSTICS aminophylline (Phyllocontin), theophylline (Slobid, Theo-Dur)
years - ABG: decreased PO2, increased PCO2 ( Respiratory acidosis, 2. Corticosteroid
TYPES hypoxemia) - shorten recovery time, improve lung function and decrease
1. Centriacinar/ Centrilobular - CXR: reveals consolidation and hyperinflation hypoxemia
- the most common type; occurs most commonly in smoker - PFTs: FEV1/FVC ratio of less than 70% - ex. beclomethasone (Beclo-vent, Vanceril); budesonide
- destruction in the bronchioles, usually in the upper lung regions COMPLICATIONS (Turbuhaler, Pulmicort)
- spreads peripherally but the alveolar sac remains intact • pneumothorax 3. Antimicrobial Agents
2. Panacinar/ Panlobular • respiratory failure 4. Mucolytics/ Expectorants/ Antitussives
- destruction of the entire alveolus and most commonly involves • pneumonia B. Oxygen Therapy
the lower portions of the lungs • chronic atelectasis - improve survival and quality of life in hypoxemic clients
- seen in individuals with AAT deficiencies • cor pulmonale - patients with chronic hyprecapnia may be O2 sensitive, their
SCHEMATIC DIAGRAM OF COPD RISK REDUCTION PaCO2 levels may rise when given with supplemental oxygen,
PREDISPOSING FACTORS PRECIPITATING FACTORS -Smoking cessation leading to:
Chronic irritation to the airflows of the lungs EFFECTS OF SMOKING CO2 Narcosis: suppression of the CNS and significant lethargy
Infiltration of lymphocytes, The elastin and fiber network of - nicotine constricts terminal bronchioles which < airflow in and NURSING MANAGEMENT
macrophages and the alveoli are broken. out of the lungs. 1. Monitor VS
polymorphonuclear leukocytes - CO is smoke binds with hemoglobin and < its O2-carrying capacity 2. Administer decreased Oxygen concentration
in the mucosal areas. - Irritants in smoke cause increased mucus secretion by the mucosa 3. Monitor pulse oximetry
of the bronchial tree and swelling of the mucosal lining, impairing 4. Provide respiratory treatments and chest physiotherapy
Vasodilation, congestion and As a compensatory mechanism, airflow. 5. Teach pursed-lip breathing techniques
edema of the bronchial mucosa. the alveoli are enlarged and the - irritants in smoke inhibit ciliary action and subsequently destroy it 6. Record the color, amount and consistency of sputum
walls are damaged. with time, smoking leads to the destruction of elastic fibers in the 7. Suction if necessary
lungs. 8. Monitor weight
9. Provide small, frequent feedings, high in calorie and protein with CLASSIFICATION - refers to the pulmonary consequences resulting from entry of
supplements 1. According to Nature of Acquisition endogenous* or exogenous substances into the lower airway
10. Force fluids unless contraindicated 2. According to Lung Involvement - most common form is bacterial infection from aspiration of
11. High fowler's position, leaning forward 3. According to Location and Radiologic Appearance bacteria that normally reside in the upper airways
12. Adhere to activity limitations ACCORDING TO NATURE OF ACQUISITION - most common pathogens: S. Pneumoniae, H. Influenzae and S.
13. Prevent infections A. Community Acquired Pneumonia Aureus
- occurs in the community setting or within the first 48 hours after ACCORDING TO LUNG INVOLVEMENT
BRONCHIECTASIS hospitalization. A. Segmental Pneumonia - one or more segments of the lungs are
- Chronic irreversible dilation of the bronchi and bronchioles. Types: affected
- Develops when bronchial walls are weakened by chronic A1. Streptococcal/ Pneumococcal Pneumonia: most common; B. Lobar Pneumonia - one or more entire lobes are affected
inflammatory changes in the bronchial mucosa and occurs most greatest incidence in the elderly and COPD patients; CA - C. Bilateral Pneumonia - lobes in both lungs are affected
often after recurrent inflammatory conditions. Streptococcus Pneumoniae ACCORDING TO LOCATION AND RADIOLOGIC APPEARANCE
PREDISPOSING FACTOS A2. Haemophilus Influenzae: affects the elderly and patients in A. Bronchopneumonia (Bronchial PN)
- airway obstruction long term care facilities - involves the terminal bronchioles and alveoli
- diffuse airway injury A3. Legionnaire's Disease: greatest incidence in smokers and B. Interstitial (Reticular) Pneumonia
- pulmonary infections or complications of such genetic disorders immunosuppressed; CA - Legionella Pneumophilia - involves inflammatory responses within lung tissue surrounding
(CF) A4. Mycoplasma Pneumonia: occurs most often in older children the air spaces and vascular structures rather than the air passages
ASSESSMENT and young adults; CA - Mycoplasma Pneumoniae themselves
- chronic cough with purulent sputum A5. Viral Pneumonia: caused by influenza virus types A, B, C. Alveolar (Acinar) Pneumonia
- fever parainfluenza, cytomegalovirus and coronavirus - there is fluid accumulation in the lung's distal air spaces
- hemoptysis B. Hospital Acquired Pneumonia D. Necrotizing Pneumonia
- fatigue and weakness - aka Nosocomial Pneumonia - causes death of a portion of lung tissue surrounded by viable
- clubbing of fingers - the onset of pneumonia symptoms > 48 hours after admission in tissue.
MANAGEMENT patients with no evidence of infection at the time of admission. ASSESSMENT
- promotion of bronchial drainage Types: - productive cough: pathognomonic sign
- antimicrobial therapy B1. Pseudomonal PN: occurs in debilitated patients, on prolonged - greenish to rusty sputum
- bronchodilators intubation or with tracheostomy; CA Pseudomonas Aeruginosa - dyspnea
- management of fatigue and malnutrition B2. Staphylococcal PN: occurs thru inhalation of the organism or via - tachypnea
- prevention of infection blood; caused by misuse or overuse of antimicrobial agents; CA - orthopnea
Staphylococcus Aureus - fever, chills, anorexia, generalized body malaise
PNEUMONIA B3. Klebsiella PN: occurs in alcoholics, elderly, those with DM and - anorexia and weight loss
-inflammation of lung parenchyma leading to pulmonary chronic lung diseases; CA Klebsiella Pneumoniae - pleuritic friction rub* and crackles
consolidation as alveoli are filled with exudates. C. Pneumonia in Immunocompromised Host - cyanosis
- occurs with the use of corticosteroids, chemotherapy, nutritional DIAGNOSTICS
PREDISPOSING FACTORS
depletion, use of broad-spectrum antibiotics, AIDS, genetic immune - CXR: consolidation
- age
disorders and long term advanced life-support therapy - Sputum GS, C & S: determines causative agent and drugs that are
- smoking
Types: effective
- air pollution
C1. Pneumocystis PN (PCP): observed in immunocompetent hosts - CBC: increased WBC* and ESR*
- prolonged immobility
and is often an initial AIDS-defining symptom; CA - Pneumocystis - ABG: decreased PO2
- immunosuppression
Jiroveci COMPLICATIONS
- chronic disease states
C2. Fungal PN: greatest incidence in immunocompromised and - shock and respiratory failure
- URTI
neutropenic patients; CA - Aspergillus Fumigatus - atelectasis
MODE OF TRANSMISSION
D. Aspiration Pneumonia - pleural effusion
- respiratory droplets through person-to-person contact
- superinfection - drain pleural cavity and achieve complete lung reexpansion - hypoxemia
MANAGEMENT - needle aspiration, CTT, open chest drainage via thoracotomy - sudden and progressive pulmonary edema
- macrolides: azithromycin (Zithromax), clarithromycin - administration of antibiotics DIAGNOSTICS
- fluoroquinolones: levofloxacin (Levaquin) - Decortication - ABG: respiratory acidosis with hypoxemia or respiratory alkalosis
- cephalosporins: cefuroxime (Zinacef) NURSING MANAGEMENT due to hyperventilation followed by metabolic acidosis
- beta lactamase inhibitors: co-amoxiclav (Augmentin) - monitor breath sounds - CXR: shows diffuse, bilateral and rapid progressing interstitial or
- antipyretics - semi-fowler's/ high- fowler's alveolar infiltrates
mucolytics/ expectorants - encourage coughing and DBE INTERVENTIONS
- O2 therapy - assist with promotion of lung drainage and lung reexpansion - identify and treat the underlying cause
NURSING MANAGEMENT - administer O2
- enforce CBR - force fluids (2-3 L/day) ACUTE RESPIRATORY DISTRESS SYNDROME (ARDS) - high fowler's/ prone
- institute pulmonary toilet: DBE, coughing exercises, chest - aka Adult Respiratory Distress Syndrome - prepare for intubation or mechanical ventilation using PEEP
physiotherapy, turning and repositioning, postural drainage - a form of acute respiratory failure that occurs as a complication of - administer diuretics, anticoagulants or corticosteroids as
- diet: increase CHO or calories, CHON and Vitamin C some other conditions, caused by a diffuse lung injury and leads to prescribed.
- position: semi-fowlers extravascular lung fluid.
-the major site of injury is the alveolar capillary membrane. CO POISONING
EMPYEMA -the interstitial edema causes compression and obliteration of the - CO is a colorless, odorless and tasteless gas that has an affinity for
- An accumulation of thick, purulent fluid within the pleural space. terminal airways and leads to reduced lung volume and compliance. hgb 200 x greater than O2.
CAUSES RISK FACTORS ASSESSMENT
- bacterial PN or lung abscess - sepsis - neurological injuries - 1-10%: impaired visual acuity
- penetrating chest trauma - fluid overload - burns - 11-20%: flushing, headache
- hematogenous infection of the pleural space - shock -drug ingestion - 21-30%: nausea and impaired dexterity
- trauma - inhalation of toxic substances - 31-40%: vomiting, dizziness and syncope
- nonbacterial infections
PHASES - 41-50%: tachypnea and tachycardia
- iatrogenic causes (post-thoracic surgery, thoracentesis)
• One: injury reduces normal blood flow to the lungs; platelets - > 50%: coma and death
ASSESSMENT
aggregate and release histamines, serotonins and bradykinins. INTERVENTIONS
• fever • Decreased/absent breath sound
• Two: released substances inflame and damage the alveolar - remove victim from exposure
• night sweats • Anorexia
capillary membrane increasing capillary permeability; fluids then - administer O2
• pleural pain
shift into the interstitial space. - monitor VS and CO level
• Cough
• Dyspnea • Three: capillary permeability increases and proteins and fluids - assess the need for basic life support
• weight loss leak out, increasing interstitial osmotic pressure thus causing
• dullness on percussion pulmonary edema. HISTOPLASMOSIS
• decreased fremitus • Fourth: decreased blood flow and fluids in the alveoli damage - a pulmonary fungal infection caused by Histoplasma capsulatum
NURSING MANAGEMENT surfactant and impair the cell's ability to produce more; the alveoli which lives in the moist soil of appropriate chemical composition
- monitor breath sounds then collapse, hence impairing gas exchange. such as:
- semi-fowler's/ high- fowler's • Fifth: oxygenation is impaired but CO2 easily crosses the alveolar a. mushroom cellars
- encourage coughing and DBE capillary membrane and is expired; blood O2 and CO2 are low; b. floors of chicken houses and bat caves
- assist with promotion of lung drainage and lung re expansion pulmonary edema worsens and inflammation leads to fibrosis; gas c. in bird droppings (starlings, pigeons and blackbirds)
exchange is further impeded. - transmission occurs by inhalation of the spores
DIAGNOSTICS
- endemic to the Central America, India and Cyprus
- CXR: reveals pleural exudates ASSESSMENT
- CBC: elevated WBC - tachypnea
- dyspnea ASSESSMENT
- Chest CT/ Thoracentesis under UTZ guidance
MEDICAL MANAGEMENT - decreased breath sounds
- dyspnea, fever and chills, chest and joint pains, productive cough, OCCUPATIONAL LUNG DISEASES: PNEUMOCONIOSES - respiratory failure
fatigue, anorexia and weight loss - Refers to nonneoplastic alteration of the lung resulting from - lung cancer
DIAGNOSITICS inhalation of mineral or inorganic dust leading to its deposition in MANAGEMENT
- histoplasmin skin test (+) the lungs. - eliminate toxic substances
- ABG: PO2 -Progresses to pulmonary fibrosis and parenchymal changes. - supportive therapy since symptoms are already irreversible
- CXR: pulmonary infiltrates -maybe asymptomatic but advanced disease is often accompanied - control infection.
- CBC: increased WBC by disability and premature death.
MEDICAL MANAGEMENT -The effects of inhaling these materials depend on:
- antifungal agents - composition of the substance
itraconazole - its concentration and ability to initiate an immune response
amphotericin B (Fungizone): nephrotoxicity and hypokalemia - its irritating properties
- corticosteroids - the duration of exposure
- mucolytic/ expectorants - the individual's response or susceptibility to the irritant
NURSING MANAGEMENT TYPES
- administer O2 Silicosis
- administer antiemetics, antihistamines, antipyretics and - caused by inhalation of silica dust in mining, quarrying, tunneling
corticosteroids as prescribed operations, glass manufacturing, stone-cutting, pottery, soap,
- encourage coughing and DBE polish and filter manufacturing
- semi-fowler's position Signs and Symptoms:
- force fluids - acute: dyspnea, fever, cough, weight loss
- CBR - chronic: hypoxemia, severe airflow obstruction and right sided
- instruct client to spray area with water before sweeping barn and heart failure
chicken coops Asbestosis
- spray breeding places - characterized by diffuse pulmonary fibrosis from the inhalation of
asbestos dust during asbestos mining and manufacturing,
SARCOIDOSIS shipbuilding, demolition and roofing
- a multisystem, granulomatous disease of unknown etiology. Signs and Symptoms:
ASSESSMENT - progressive dyspnea, persistent dry cough, mild to moderate chest
- night sweats, fever, weight loss, cough, skin nodules, polyarthritis pain, anorexia, weight loss, malaise, crackles, clubbing of fingers
DIAGNOSTICS Coal Worker's Pneumoconiosis
- Kveim test: sarcoid node antigen in injected intradermally and - aka "Black Lung Disease"
- includes a variety of lung diseases found in coal workers who have
causes a local nodular lesion in about 1 month
inhaled coal dust (mixture of coal, kaolin, mica and silica) over the
- CXR/ CT Scan: hilar adenopathy and disseminated miliary and
years
nodular lesions in the lungs
Signs and Symptoms:
- Transbronchial/ Open Biopsy: shows noncaseating granulomas
- chronic cough and sputum production, dyspnea, coughing up of
MANAGEMENT
sputum with varying amounts of black fluid (melanoptysis)
- administer corticosteroids to control symptoms
- monitor temperature
PNEUMOCONIOSES
- force fluids
- provide adequate rest periods COMPLICATIONS
- encourage small, nutritious meals - pulmonary tuberculosis
- cor pulmonale
You might also like
- Respiratory TransesDocument4 pagesRespiratory TransesAriane Shane BidoNo ratings yet
- Johnson Jerry Alan Chinese Medical Qigong Therapy Vol 5-141-160Document20 pagesJohnson Jerry Alan Chinese Medical Qigong Therapy Vol 5-141-160toanbauNo ratings yet
- Medical Surgical Nursing Module 11Document26 pagesMedical Surgical Nursing Module 11weissNo ratings yet
- Mechanics of RespirationDocument78 pagesMechanics of Respirationnirilib100% (4)
- Respiratory System Notes - KEYDocument3 pagesRespiratory System Notes - KEYjoy100% (1)
- Respiratory System QuizDocument2 pagesRespiratory System Quizapi-281108263100% (1)
- ... 2 Finals Pulmonary PhysiologyDocument9 pages... 2 Finals Pulmonary PhysiologyELIZABETH GRACE AMADOR100% (1)
- 2803NRS Acute Nursing Practice Exam NotesDocument18 pages2803NRS Acute Nursing Practice Exam NotesGrace CallowNo ratings yet
- Nasal Physiology and Pathophysiology PDFDocument610 pagesNasal Physiology and Pathophysiology PDFRahat tanvirNo ratings yet
- NCM112OFI Prelims Respi and CardioDocument17 pagesNCM112OFI Prelims Respi and CardioTrisha Julienne CuaNo ratings yet
- Nayli Bio SBP 2019 EseiDocument5 pagesNayli Bio SBP 2019 EseiEqis AlfiesyaNo ratings yet
- Functions of The Respiratory SystemDocument10 pagesFunctions of The Respiratory Systemadelina.jianu9991No ratings yet
- Nurs 13 Week 2Document20 pagesNurs 13 Week 2cheskalyka.asiloNo ratings yet
- Anatomy and Physiology of The Respiratory SystemDocument14 pagesAnatomy and Physiology of The Respiratory SystemAmore BuenafeNo ratings yet
- Physiology Of: RespirationDocument51 pagesPhysiology Of: RespirationDr. R. PeriasamyNo ratings yet
- MC 1B 11 Respiratory System DisordersDocument9 pagesMC 1B 11 Respiratory System DisordersjambyNo ratings yet
- Ch. 29 StudyDocument6 pagesCh. 29 StudyPaige Nicole GauthreauxNo ratings yet
- Respiratory System HandoutDocument11 pagesRespiratory System HandoutJohn Carlo SantiagoNo ratings yet
- Assessment of The Thorax and LungsDocument9 pagesAssessment of The Thorax and LungsJasmin MolanoNo ratings yet
- Midterm 3 Anatomy PDFDocument364 pagesMidterm 3 Anatomy PDFaidanNo ratings yet
- Thorax and LungsDocument2 pagesThorax and LungsHNo ratings yet
- The Respiratory SystemDocument22 pagesThe Respiratory System5130022035 ARINA DINANANo ratings yet
- Respiratory SystemDocument6 pagesRespiratory SystemChelsie NicoleNo ratings yet
- Thorax & LungsDocument14 pagesThorax & LungsRed MontemayorNo ratings yet
- Oxygenation-AnaPhysio HanakoRN PDFDocument69 pagesOxygenation-AnaPhysio HanakoRN PDFHanako Sasaki AranillaNo ratings yet
- NCM103j OXYGENATIONDocument4 pagesNCM103j OXYGENATIONTamara RomuarNo ratings yet
- Oxygenation Respiration: Hypoxia Is A Condition in Which The Body or A Region ofDocument3 pagesOxygenation Respiration: Hypoxia Is A Condition in Which The Body or A Region ofMarissa AsimNo ratings yet
- Respiratory SystemDocument2 pagesRespiratory SystemjuliamaesimbreNo ratings yet
- 1 Mechanics of Breathing PDFDocument38 pages1 Mechanics of Breathing PDFEkrem VarlikNo ratings yet
- Respiratory KeypointsDocument11 pagesRespiratory KeypointsShahina ShayneNo ratings yet
- Respiratory System: Functional Anatomy, VentilationDocument50 pagesRespiratory System: Functional Anatomy, VentilationRevanth VejjuNo ratings yet
- S - Assessment of The Thorax 2Document2 pagesS - Assessment of The Thorax 2Queen RiquezNo ratings yet
- 112 NotesDocument9 pages112 NotesDawnmurph Dharlene Wag-eNo ratings yet
- Reviewer in Anatomy PhysiologyDocument50 pagesReviewer in Anatomy PhysiologyAuthor - SanNo ratings yet
- Gen BioDocument15 pagesGen BioCAMILLE JELLA ALZOLANo ratings yet
- Module 10: Respiratory: Increasing Size of LungsDocument5 pagesModule 10: Respiratory: Increasing Size of LungsjunquelalaNo ratings yet
- Anaphy Week4 Respiratory-SystemDocument13 pagesAnaphy Week4 Respiratory-SystemMarc QuireNo ratings yet
- NCM103 - 2016 - Lecture2 - Response To Altered Respiratory FunctionDocument128 pagesNCM103 - 2016 - Lecture2 - Response To Altered Respiratory FunctionrimeoznekNo ratings yet
- The Respiratory SystemDocument61 pagesThe Respiratory SystemLuna JadeNo ratings yet
- Respiratory SystemDocument30 pagesRespiratory SystemaadhyagattiNo ratings yet
- Bio CH8 F4 Studywithadmin PDFDocument16 pagesBio CH8 F4 Studywithadmin PDFMUHAMMAD FAREEZ HAIKAL MOHD SHAIFUDDINNo ratings yet
- Anaphy-Respiratory HandoutDocument7 pagesAnaphy-Respiratory HandoutAEGEL DARO TORRALBANo ratings yet
- RP 1 PDFDocument9 pagesRP 1 PDFObsa AbrahimNo ratings yet
- (Unit 6) m.02 Physiology of The Nose and Paranasal SinusesDocument6 pages(Unit 6) m.02 Physiology of The Nose and Paranasal Sinusesjustme12345mNo ratings yet
- Respiratorio-Openstax Biology2e ch39Document43 pagesRespiratorio-Openstax Biology2e ch39ANo ratings yet
- Oxygenation and SuctioningDocument7 pagesOxygenation and Suctioningkrysteljen052002No ratings yet
- Medsurg Reviewer (Prelim)Document71 pagesMedsurg Reviewer (Prelim)JOANA MARIE MAE SANTOS BASILIONo ratings yet
- Respiratory System I. FunctionDocument6 pagesRespiratory System I. Functionjgcriste100% (3)
- Respiratory SystemDocument8 pagesRespiratory SystemSJane FeriaNo ratings yet
- Respiratory System and Its Treatment Modalities PDFDocument1 pageRespiratory System and Its Treatment Modalities PDFAdri SinclaireNo ratings yet
- Respiratory System LecDocument49 pagesRespiratory System LecStef FieNo ratings yet
- Oxygen Therapy and NebulizationDocument9 pagesOxygen Therapy and NebulizationArun Roa DanielNo ratings yet
- Functions of The Respiratory Passage WaysDocument14 pagesFunctions of The Respiratory Passage WaysArgon BoronNo ratings yet
- Respiratory Disorders (Completed)Document55 pagesRespiratory Disorders (Completed)Czejan Rae TabaranzaNo ratings yet
- Respiratory SystemDocument36 pagesRespiratory Systemسارة عبد الكاظم مكطوفNo ratings yet
- Physio Topic 6 RespiratoryDocument4 pagesPhysio Topic 6 RespiratoryJames FabioNo ratings yet
- Form 4 Revision QuizDocument80 pagesForm 4 Revision QuizEnvira LeeNo ratings yet
- (Highlight Ni Dean) : Diagnostic ExamsDocument16 pages(Highlight Ni Dean) : Diagnostic Examsfiel borataNo ratings yet
- 12 - Respiratory PhysiologyDocument62 pages12 - Respiratory PhysiologyRohit K YNo ratings yet
- Ms Lec 2 Respiratory SystemDocument11 pagesMs Lec 2 Respiratory SystemLabinnah MoresNo ratings yet
- Chapter 11 Gas Exchange in Humans 23-24Document127 pagesChapter 11 Gas Exchange in Humans 23-24Huraiza AsifNo ratings yet
- Gen Physiology - Transes 9Document3 pagesGen Physiology - Transes 9karmylle andradeNo ratings yet
- Drugs Acting On The Respiratory System Respiratory System: Lung ComplianceDocument9 pagesDrugs Acting On The Respiratory System Respiratory System: Lung ComplianceAdiel CalsaNo ratings yet
- Infection at A Glance.: Upper Respiratory Tract Infection S.O.P D.A.V .VDocument7 pagesInfection at A Glance.: Upper Respiratory Tract Infection S.O.P D.A.V .VdeepuNo ratings yet
- Lung Dissection Lab ReportDocument10 pagesLung Dissection Lab ReportSantiago MacíasNo ratings yet
- Anatomy Chapter 23 Respiratory SystemDocument86 pagesAnatomy Chapter 23 Respiratory SystemLagunamedical PharmacyNo ratings yet
- Pulmonology 3 COPD (Completed)Document6 pagesPulmonology 3 COPD (Completed)Benjamin NgNo ratings yet
- Class Lesson - Lesson 2. Respiratory SystemDocument18 pagesClass Lesson - Lesson 2. Respiratory Systemshellers24No ratings yet
- Methacholine Challenge TestDocument8 pagesMethacholine Challenge TestHafiz Hari NugrahaNo ratings yet
- CARE PLAN For BRONCHIECTASISDocument8 pagesCARE PLAN For BRONCHIECTASISCecil MonteroNo ratings yet
- Cambridge International Examinations Cambridge International Advanced Subsidiary and Advanced LevelDocument16 pagesCambridge International Examinations Cambridge International Advanced Subsidiary and Advanced LevelMena YasserNo ratings yet
- Bronchi 0Document52 pagesBronchi 0Jennifer DixonNo ratings yet
- Anatomy of Lung Segment Sem 3 Week 2Document2 pagesAnatomy of Lung Segment Sem 3 Week 2miftahuldursinaNo ratings yet
- Impaired Gas Exchange NCPDocument3 pagesImpaired Gas Exchange NCPMae Denn LabordoNo ratings yet
- Asthma: Assessment, Diagnosis, and Treatment Adherence: Gerri KaufmanDocument8 pagesAsthma: Assessment, Diagnosis, and Treatment Adherence: Gerri KaufmandessyNo ratings yet
- Respiratory PhysiologyDocument38 pagesRespiratory PhysiologyskNo ratings yet
- Chatburn - Fundamentals of MVDocument313 pagesChatburn - Fundamentals of MVJesus Alonso Hernandez ANo ratings yet
- Critical Care Medicine OutlineDocument76 pagesCritical Care Medicine OutlineMiss KNo ratings yet
- Steam Inhalation ProcedureDocument6 pagesSteam Inhalation ProcedureSujatha J Jayabal100% (2)
- Makalah Bhs Inggris Sistem RespirasiDocument13 pagesMakalah Bhs Inggris Sistem RespirasiDewa Ayu Made FebriariNo ratings yet
- The EMERGENCY SEVERITY INDEXDocument4 pagesThe EMERGENCY SEVERITY INDEXWindyNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanKoleen KirstenNo ratings yet
- Field Resuscitation of Newborn CalvesDocument2 pagesField Resuscitation of Newborn Calvesapi-262327869100% (1)
- 112 NotesDocument9 pages112 NotesDawnmurph Dharlene Wag-eNo ratings yet
- Cpap - A Gentle VentilationDocument24 pagesCpap - A Gentle VentilationrobystwnNo ratings yet
- Name: Jake Yvan G. Dizon Year Level: BSN IIIDocument2 pagesName: Jake Yvan G. Dizon Year Level: BSN IIIJake Yvan DizonNo ratings yet
- CH 21Document19 pagesCH 21Lisa Evitt CoxNo ratings yet
- COPD Treatment, DiagnoseDocument8 pagesCOPD Treatment, Diagnoseaghamohsin1No ratings yet