Professional Documents
Culture Documents
Blood Vessels and Blood Pressure
Uploaded by
IAhmad QasimOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Blood Vessels and Blood Pressure
Uploaded by
IAhmad QasimCopyright:
Available Formats
Last edited: 11/9/2021
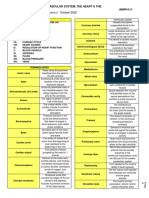
10. BLOOD VESSEL CHARACTERISTICS
Cardiovascular: Blood Vessel Characteristics Medical Editor: Mariel Antoinette L. Perez
OUTLINE II) DIFFERENT TYPES OF VESSELS
1. Elastic Conducting Arteries
I) COURSE OF BLOOD VESSEL CIRCULATION
2. Muscular Distributing Arteries
II) DIFFERENT TYPES OF VESSELS
3. Arterioles
III) ARTERIES
4. True Capillaries
IV) VEINS
5. Venules
V) APPENDIX
6. Veins
VI) REVIEW QUESTIONS
VII) REFRENCES
Table 1. Arteries vs Veins
Arteries Veins
I) COURSE OF BLOOD VESSEL CIRCULATION
Blood flow Away from the Away from the
Arterial Course direction heart heart
o Heart → Elastic artery → Muscular artery → Arteriole Pressure High Low
→ Capillaries High Low
Venous Course Except Except
Oxygen
o Capillaries → Venules → Veins → Heart
content
Note: Capillaries and Venules will be further discussed
in Ninja Nerd’s Microcirculation video.
A nice mnemonic to remember:
Arteries: Away from the heart
Veins: Vack to the heart
III) ARTERIES
Table 2. Muscular Arteries vs Elastic Arteries
FEATURES MUSCULAR ARTERIES ELASTIC ARTERIES
Large vessels
Characteristics Smaller of Medium-sized vessels
Nearest to the heart
Diameter 6mm (due to thick tunica media) Ranges from 1-1.5cm
Structure Less elastic lamina → less elasticity Lots of elastic lamina → more elasticity
Absorbs and dampens high-pressure blood from heart’s ventricles
Delivers blood to specific organs
- Stretches during systole to take on high systolic
pressure
Functions Regulates blood flow to target organs
- Recoils during diastole
- Vasoconstriction
Maintains relatively constant pressure gradient despite heart’s
- Vasodilation
high-pressure pumping action [Tucker, et al.]
Renal artery Pulmonary Trunk
Femoral artery Aorta (prime example)
Examples Gonadal artery
Mesenteric artery
Inferior phrenic artery
(1) Arterioles (2) True Capillaries
Very small vessels with a diameter of around 35 µm Diameter of 8-10 µm
Feed the capillary bed where true capillaries come from Exchange vessels
High Resistance Vessels o Main significance of capillaries
o Develop the most resistance to blood flow o Designed for exchange of different substances (e.g.,
Pre-capillary sphincters gases, nutrients, hormones, wastes)
o Smoot muscle layer wrapped around arterioles or the
capillary bed Tunica Intima
o When the SNS innervates them, it causes them to o Inner lining with simple squamous epithelial cells
constrict
Basement membrane/ Basal lamina
SNS = Sympathetic Nervous System
o Connective tissue layer wrapped around the
This makes the arterioles high resistance vessels
capillaries
o Depending on where it’s located, it may have
intracellular clefts, fenestration pores, tight junctions,
or pericytes
Figure 1.1 Arteries
Blood Vessel Characteristics CARDIOVASCULAR PHYSIOLOGY : Note #10 1 of 3
IV) VEINS (B) VARICOSE VEINS
5mm in diameter
Designed to be lower pressure systems
o 5-10 mmHg
Thin tunica media
Main Function: Capacitance or reservoir vessels
Large lumen
o Occupies large volume of blood Figure 1.2 Varicose veins
o 70% of all the body’s blood at any given instance Tortuous, dilated, twisted, and/or enlarged blood vessels
Decreased smooth muscle Valves can become incompetent and leaky
o Not great at pushing blood up towards heart
Process
(A) FOUR SPECIALTIES OF THE VEIN
Since the vein is not a high-pressure system, it must
develop some adaptations to get blood back up against
gravity despite the decreased smooth muscle
(1) Valves of tunica interna
Tunica interna is an endothelial cell lining that fold
inwards to form valves
o Valves help prevent the blood from going back down Common in the following:
o Blood is pushed up Some blood that circulates o Calves: varicose veins
back down pushes the valve close prevent blood May be caused by standing for a long time
from flowing into the inferior portion of the vein o Testes: varicoceles
o Prevents pooling of blood Particularly the left testes
Causes varicose veins • left gonadal vein comes up with renal artery
and turns to put blood into the IVC
(2) Muscular Milking
o IVC: Inferior Vena Cava
Veins are usually near muscles • blood leads to backflow into the testes
Slow process of muscular contraction that squeezes the • right gonadal vein goes straight to the IVC
blood vessels and push the blood upward May lead to inflammation and in some cases,
infertility
(3) Respiratory Pump
o Anus: hemorrhoidal veins
Breathing increases thoracic cavity volume can push Hemorrhoids
on some lower vessels and help the blood push upward Accumulated pressure due to various scenarios
o Helps increase blood flow from the lungs and back to • E.g., high pressure straining, forcing to go to
the heart the bathroom, sitting for long periods of time
o Helps push blood flow from the lower systemic veins
back up to the heart
(4) Sympathetic Tone
2 of 3 CARDIOVASCULAR PHYSIOLOGY: Note #10 BLOOD VESSEL CHARACTERISTICS
V) APPENDIX
Figure 1.3. Summary of Blood Vessel Characteristics
VI) REVIEW QUESTIONS VII) REFRENCES
● Tucker, W. D. (2021, August 11). Anatomy, Blood Vessels. U.S.
1) Which of the following is considered the largest
National Library of Medicine. Retrieved September 10, 2021, from
blood vessel? https://www.ncbi.nlm.nih.gov/books/NBK470401/.
a) Elastic Conducting Arteries ● Le T, Bhushan V, Sochat M, Chavda Y, Zureick A. First Aid for
b) Muscular Distributing Arteries the USMLE Step 1 2018. New York, NY: McGraw-Hill Medical; 2017
● Mancini MC. Heart Anatomy. In: Berger S Heart Anatomy. New
c) Arterioles York, NY: WebMD.https://emedicine.medscape.com/article/905502-
d) Veins overview.
● Hill M. Cardiovascular System - Heart Histology.
2) Which of the following is not a specialty feature of a https://embryology.med.unsw.edu.au/embryology/index.php/Cardiov
vein? ascular_System_-_Heart_Histology.
a) Valves of tunica externa ● McCorry LK. Physiology of the Autonomic Nervous System. Am
J Pharm Educ .2007; 71(4): p.78. doi: 10.5688/aj710478.
b) Muscular Milking ● Standring S. Gray's Anatomy: The Anatomical Basis of Clinical
c) Respiratory Pump Practice. Elsevier Health Sciences; 2016
d) Sympathetic Tone ● Leslie P. Gartner, James L. Hiatt. Color Textbook of Histology.
New York (NY): Grune & Stratton Inc.; 2006
3) All of the following are features of a varicose vein, ● U. S. National Institutes of Health, National Cancer Institute. NIH
SEER Training Modules - Classification & Structure of Blood
except:
Vessels.
a) Tortuous https://training.seer.cancer.gov/anatomy/cardiovascular/blood/classi
b) Constricted fication.html.
c) Twisted ● Ostenfeld E, Flachskampf FA. Assessment of right ventricular
volumes and ejection fraction by echocardiography: from geometric
d) Enlarged approximations to realistic shapes.. Echo research and practice
.2015; 2(1): p.R1-R11. doi: 10.1530/ERP-14-0077.
● Maceira AM, Prasad SK, Khan M, Pennell DJ. Reference right
ventricular systolic and diastolic function normalized to age, gender
and body surface area from steady-state free precession
CHECK YOUR ANSWERS
cardiovascular magnetic resonance.. Eur Heart J .2006; 27(23):
p.2879-88. doi: 10.1093/eurheartj/ehl336.
● Marieb EN, Hoehn K. Anatomy & Physiology. Hoboken, NJ:
Pearson; 2020.
● Boron WF, Boulpaep EL. Medical Physiology.; 2017.
Blood Vessel Characteristics CARDIOVASCULAR PHYSIOLOGY : Note #10 3 of 3
Last edited: 10/9/2021
1. TUNIC LAYERS AND TYPES OF CAPILLARIES
Cardiovascular: Tunic Layers and Types of Capillaries Medical Editor: Mariel Antoinette L. Perez
• Sympathetic Nervous system
OUTLINE o Norepinephrine
o Epinephrine
I) TUNIC LAYERS OF BLOOD VESSELS
• Angiotensin II
II) THREE TYPES OF CAPILLARIES
III) APPENDIX • Vasopressin (ADH)
IV) REVIEW QUESTIONS • Endothelin
V) REFRENCES o Vasodilation
Smooth muscles relax → ↑lumen diameter →
I) TUNIC LAYERS OF BLOOD VESSELS ↓Vascular Resistance → ↓Blood Pressure
Stimulators
The layers of an artery and vein are almost the same, the • Nitric Oxide and prostaglandins
only difference is in the thickness of the layers • Atrial Natriuretic peptide
The layers are: • Increased Cellular Activity
o Tunica Interna/Intima o Decreased oxygen (O2)
o Internal Elastic Lamina o Increased carbon dioxide (CO2)
o Tunica Media o Increased protons (H+)
o External Elastic Lamina
o Tunica Externa/Adventitia (D) EXTERNAL ELASTIC LAMINA
(A) TUNICA INTERNA/INTIMA Connective Tissue: Elastic Connective Tissue
Function:
Innermost layer o Allows blood vessels to stretch and recoil when
Has two distinct layers blood is rushing through it
(1) Endothelial Layer Without this ability, can lead to rigidity, hardening,
and/or thickening of vessels
Endothelial Tissue: Simple squamous epithelial cells
Functions: (E) TUNICA EXTERNA/ADVENTITIA
o Keeps blood antithrombotic (prevents clots) Outermost layer
o Acts as barrier between blood and tissue Connective Tissue: Dense Fibrous Irregular
o Controls blood vessel growth Connective tissue
o Can form valves in veins to prevent backflow Function:
(2) Subendothelial Layer o Anchors vessels to surrounding structures
o Not super vascular; has its own blood supply
Connective Tissue: Loose areolar connective tissue Vasa Vasorum
Made of glycogen, and other proteoglycans & proteins • Supplies blood to Tunica Media and Tunica
Function: Adventitia
o Prevents the blowout of the blood vessel • Clinical Correlate: Tertiary Syphilis
o Activates primary Hemostatic plug o Destroys vasa vasorum supply to
(B) INTERNAL ELASTIC LAMINA tunica adventitia; may damage tunica
media thickening and weakening of
Connective Tissue: Elastic Connective Tissue blood vessel risk for aortic aneurysm
Made up of collagen, fibrin, and other proteins o Caused by bacterium Treponema pallidum
Function:
o Allows vessels to stretch and recoil when blood is (F) TUNICA EXTERNA/ADVENTITIA
rushing through it. Table 1. Summary of Differences of Tunic Layers in Arteries
and Veins
Congenital disorders that affect the internal elastic lamina
Marfan Syndrome: usually lack of fibrillin Arteries Veins
Ehlers-Danlos Syndrome: lack of specific type of Tunica Intima No valves Valves
collagen Tunica Media Thicker Thinner
o Both syndromes can increase risk of aortic dissection
Elastic Lamina
or aneurysms
Tunica Externa
(C) TUNICA MEDIA Diameter
Middle layer Veins may have little to no internal/external elastic lamina
Tissue: Smooth Muscle Cells o Due to veins not being high-pressure systems
Under sympathetic innervation They don’t need to be distensible or stretched
o Has vasomotor tone Pressure is only 5-10 mmHg
Without vasomotor tone, blood vessels would
dilate cause neurogenic shock Tunica media is thin
o Sympathetic nerves hasVE aginergic receptors o Due to veins being capacitance/reservoir vessels
Holds 70% of blood
Function: Regulates lumen diameter o Has sympathetic innervation
o Vasoconstriction Can contract, but not as much
smooth muscles contract → ↓lumen diameter →
↑Vascular Resistance → ↑Blood pressure Histologically, veins will have a collapsed lumen
Stimulators
Tunic Layers and Types of Capillaries CARDIOVASCULAR PHYSIOLOGY : Note #11 1 of 3
(B) CONTINUOUS CAPILLARIES
II) THREE TYPES OF CAPILLARIES
Distinguishing Features
Sinusoidal Capillaries o Least permeable
Continuous Capillaries o Small intracellular cleft
Fenestrated Capillaries Exception: blood-brain barrier
(A) SINUSOIDAL CAPILLARIES • No clefts, but have tight junctions that link
endothelial cells together
Distinguishing Features o Contain Pericytes
o Large Intercellular clefts Control endothelial cell growth
Huge gaps between the endothelial cells Cause vasoconstriction
o Most permeable capillary Act as phagocytes for things leaking out of the cell
Allows large proteins and cells to move through o Dependent on transcellular transport
intercellular clefts Can undergo pinocytosis or passive diffusion
E.g., RBCs and albumin can leak out of these • Endothelial cell can form a little endocytic
blood vessels vesicle and take in small solutes (low
Common Locations molecular weight proteins) and undergo
o Spleen – important! transcytosis (the vesicle leaks out) or passive
o Red Bone Marrow diffusion
o Liver Common Locations
o Skin
o Blood Brain Barrier
o Muscles
o Lungs
(C) FENESTRATED CAPILLARIES
Distinguishing Features
o Have medium intracellular clefts
o Fenestration Pores running through endothelial cells
Moderate permeability
Allows small proteins and solutes to pass through
fenestrations and leave the plasma
• But does not allow blood cells to pass
o Endothelial cells can also undergo pinocytosis
o Location:
Kidneys
Endocrine/Exocrine Glands
• Endocrine: ductless glands (uses hormones)
• Exocrine: duct glands
Small intestine
III) APPENDIX
Figure 1. Tunic Layers in a vein (left) and an artery (right)
2 of 3 CARDIOVASCULAR PHYSIOLOGY: Note #11 TUNIC LAYERS AND TYPES OF CAPILLARIES
Figure 2. Summary of Tunic Layers and Types of Capillaries
IV) REVIEW QUESTIONS V) REFRENCES
1) What can you find in the Tunica Adventitia? ● Tucker, W. D. (2021, August 11). Anatomy, Blood Vessels. U.S.
National Library of Medicine. Retrieved September 10, 2021, from
a) Simple squamous epithelial cells https://www.ncbi.nlm.nih.gov/books/NBK470401/.
b) Dense Fibrous Irregular Connective tissue ● Torres-Vázquez, J., Kamei, M., & Weinstein, B. M. (2003).
c) Elastic Connective Tissue Molecular distinction between arteries and veins. Cell and Tissue
Research, 314(1), 43–59. https://doi.org/10.1007/s00441-003-0771-
d) Smooth Muscle Cells 8
● Le T, Bhushan V, Sochat M, Chavda Y, Zureick A. First Aid for
2) Where can you NOT find sinusoidal capillaries? the USMLE Step 1 2018. New York, NY: McGraw-Hill Medical; 2017
a) Spleen ● Mancini MC. Heart Anatomy. In: Berger S Heart Anatomy. New
b) Lungs York, NY: WebMD.https://emedicine.medscape.com/article/905502-
c) Bone Marrow overview.
● Hill M. Cardiovascular System - Heart Histology.
d) Liver https://embryology.med.unsw.edu.au/embryology/index.php/Cardiov
ascular_System_-_Heart_Histology.
3) Which of the following is the least permeable ● Standring S. Gray's Anatomy: The Anatomical Basis of Clinical
capillary? Practice. Elsevier Health Sciences; 2016
a) Sinusoidal ● Leslie P. Gartner, James L. Hiatt. Color Textbook of Histology.
New York (NY): Grune & Stratton Inc.; 2006
b) Continuous
● U. S. National Institutes of Health, National Cancer Institute. NIH
c) Fenestrated SEER Training Modules - Classification & Structure of Blood
d) Pericytes Vessels.
https://training.seer.cancer.gov/anatomy/cardiovascular/blood/classi
fication.html.
● Marieb EN, Hoehn K. Anatomy & Physiology. Hoboken, NJ:
CHECK YOUR ANSWERS Pearson; 2020.
● Boron WF, Boulpaep EL. Medical Physiology.; 2017.
Tunic Layers and Types of Capillaries CARDIOVASCULAR PHYSIOLOGY : Note #11 3 of 3
Last edited: 11/9/2021
1. MICROCIRCULATION
Cardiovascular: Microcirculation Medical Editor: Mariel Antoinette L. Perez
OUTLINE II) NET FILTRATION PRESSURE (NFP)
I) OVERVIEW There are pressure changes through capillaries
II) NET FILTRATION PRESSURE (NFP) NFP
III) ANASTOMOSES = (Forces pushing or pulling OUT of the vessel and
IV) REGULATION OF MICROCIRCULATION into the interstitium) – (Forces pushing or pulling
V) APPENDIX INTO the vessel from the interstitium
VI) REVIEW QUESTIONS
NFP = (HPC + OPC) – (OPC + HPI)
VII) REFRENCES
o NFP on arterial side
= (35 mmHg + 1 mmHg) – (26 mmHg + 0 mmHg)
= +10mmhg
I) OVERVIEW Positive NFP tells us that filtrate is moving out of
Diagram Guide of things discussed in the video lecture the vessel into interstitial space
o Brain: CNS o NFP on venous side
o Lungs = (17 mmHg + 1 mmHg) – (26 mmHg + 0 mmHg)
o Skeletal Muscle Tissue = –8 mmHg
o Blood Vessels Negative NFP tells us that filtrate is moving into a
Arterioles vessel from interstitial space.
Venules Blood is made up of cells and plasma
Capillaries
o Generalized Tissue Cells (A) FORCES PUSHING/PULLING OUT OF VESSEL
o Lymphatic Vessel (1) Capillary Hydrostatic Pressure (HPC)
o Skin Epidermis and Dermis
o Gastrointestinal (GI) Tract Hydrostatic pressure within the capillaries
Pushes filtrate out of the vessel (capillary bed) and into
(A) BLOOD VESSELS the interstitial space
Directly dependent on systolic blood pressure
(1) Terminal Arteriole
o ↑BP → ↑HPC → pushes more filtrate out of the vessel
Gets ready to feed into the capillary bed or AV shunt o ↓BP → ↓HPC → less filtrate pushed out the vessel
(2) Metarteriole Average pressure value
o Arterial side of capillary: 35 mmHg
(3) True Capillaries o Venous side of capillary: 17mmhg
10-100 true capillaries per capillary bed Pressure is lower in venous channels.
Comes off the metarteriole
(2) Interstitial Osmotic Pressure (OPI)
(i) Precapillary Sphincter Pulls filtrate from blood vessel into interstitial space
Ring of smooth muscle tissue right around the true Dependent on proteins in interstitial space
capillaries o E.g., albumin
Controls blood flow of true capillaries ↑albumin in interstitial space
• Constricts: no blood flows
• Dilated: blood can come out ↓albumin in interstitial space
Controlled by Sympathetic Nervous System
(SNS) and other chemicals Average pressure value: 1 mmHg
o There’s usually very few albumin in interstitial spaces
(4) Thorough Fare Channel
(B) FORCES PUSHING/PULLING INTO THE VESSEL
(5) Vascular shunt
Blood flow from metarteriole to Thoroughfare Channel (1) Capillary Osmotic Pressure (OPC)
Arterio-venous anastomose Pulls filtrate from interstitial spaces into blood vessels or
keeps filtrate in the blood vessel.
(6) Post-Capillary Venule
Dependent on proteins in the blood (like albumin)
Drains out the Thoroughfare Channel o E.g., albumin
↑albumin in the blood
(B) PATHWAY
(1) If precapillary sphincters closed: ↓albumin in blood
o Terminal arteriole → metarteriole → thoroughfare
channel → postcapillary venule Average pressure value: 26 mmHg
o Vascular shunt o There’s usually plenty of albumin in the blood
blood flow from metarteriole → thoroughfare
(2) Interstitial Hydrostatic Pressure (IHP)
channel
Pushes filtrate from interstitial space into blood vessels.
(2) If precapillary sphincters open:
Dependent on
o Terminal arteriole → metarteriole → true capillaries → o Volume of filtrate in the interstitial space
thoroughfare channel → postcapillary venule o Function of the lymphatic system that removes
excess filtrate.
MICROCIRCULATION CARDIOVASCULAR PHYSIOLOGY : Note #12 1 of 3
If lymphatics are working well (2) Venous:
Fusion of Vein and vein around a tissue to provide
alternative blood flow if needed
Most abundant and common
If lymphatics are plugged up
Examples
o Median Antecubital vein
A fusion of basilic and axillary vein
Good for blood draws.
Average pressure value: 0 mmHg
o Assuming normal lymphatic function (3) Arterio-Venous
This is a fusion of an arteriole with a venule.
(C) CLINICAL CORRELATES
Examples:
Disease or condition where patient loses a lot of protein in o Vascular shunt at capillary bed
the urine Metarteriole → Thoroughfare channel
o Loss of protein loss of albumin OPC goes down
filtrate gets more pushed out edema (B) CLINICAL CORRELATE: AV MALFORMATION
o E.g., Glomerulonephritis, Nephrotic syndrome, Condition wherein people don’t have true capillaries
hypoalbuminemia, hypoproteinemia o True capillaries dampen the pressure
Cancer caused an occlusion within a lymphatic vessel Without true capillaries, there’s high pressure
o Start backflowing swelling edema from artery straight to the vein
May cause vessels to coil up and rupture
III) ANASTOMOSES Rare condition but common in the brain
Alternative or collateral channels for blood to flow through Treatment: embolization
Fusion of vessels to allow blood to flow through
IV) REGULATION OF MICROCIRCULATION
alternative pathways if needed.
Importance: (A) SKELETAL MUSCLE
o If one vessel is blocked, the anastomoses allow blood
to move through collateral or fusion connection and How does blood flow change in certain circumstances?
still supply the tissue or move blood along. o Someone’s exercising they can get a little sore
Because they might be producing lactic acid
(A) TYPES OF ANASTOMOSES Metabolic acid that can decrease pH
o Produce CO2 H+ can mediate/localize
(1) Arterial:
regulation
Fusion of artery and artery around a tissue to provide Can act on muscle cells muscle cells relax
alternative blood flow if needed o Localized or active hyperemia
Examples
In conclusion, Muscle activity results in:
(i) Coronary circulation o CO2
o H+
o O2
(ii) Circle of Willis o K+
These chemicals cause vasodilation and increase blood
Importance of Anastomoses: flow to muscles when there is increased demand
(B) BRAIN
Increased Mean Arterial Pressure (MAP) in cerebral
vessels
Myogenic Mechanis
o high MAP Stretch of cerebral vessels
o Low MAP No stretching of cerebral vessels
(C) LUNGS
Decreased Oxygen in alveoli
o May be due to obstruction or mucus buildup
o Causes pulmonary arterioles to constrict
(D) GASTROINTESTINAL TRACT AND SKIN
In a fight or flight situation, the SNS is activated.
Figure 1. Circle of Willis
2 of 3 CARDIOVASCULAR PHYSIOLOGY: Note #12 MICROCIRCULATION
V) APPENDIX
Figure 2. Summary of Microcirculation
VI) REVIEW QUESTIONS VII) REFRENCES
● Tucker, W. D. (2021, August 11). Anatomy, Blood Vessels. U.S.
1) A clot in which artery of the Circle of Willis will allow
National Library of Medicine. Retrieved September 10, 2021, from
blood to find an alternative route to flow to? https://www.ncbi.nlm.nih.gov/books/NBK470401/.
a) Basilar artery ● Le T, Bhushan V, Sochat M, Chavda Y, Zureick A. First Aid for
b) Posterior communicating artery the USMLE Step 1 2018. New York, NY: McGraw-Hill Medical; 2017
● Mancini MC. Heart Anatomy. In: Berger S Heart Anatomy. New
c) Internal carotid artery York, NY: WebMD.https://emedicine.medscape.com/article/905502-
d) Anterior cerebral artery overview.
● Hill M. Cardiovascular System - Heart Histology.
https://embryology.med.unsw.edu.au/embryology/index.php/Cardiov
2) Which of the following pressures don’t have the ascular_System_-_Heart_Histology.
same average pressure value for the arterial and ● McCorry LK. Physiology of the Autonomic Nervous System. Am
J Pharm Educ .2007; 71(4): p.78. doi: 10.5688/aj710478.
venous side? ● Standring S. Gray's Anatomy: The Anatomical Basis of Clinical
a) Capillary Hydrostatic Pressure Practice. Elsevier Health Sciences; 2016
b) Interstitial Hydrostatic Pressure ● Leslie P. Gartner, James L. Hiatt. Color Textbook of Histology.
New York (NY): Grune & Stratton Inc.; 2006
c) Capillary Osmotic Pressure ● U. S. National Institutes of Health, National Cancer Institute. NIH
d) Interstitial Osmotic Pressure SEER Training Modules - Classification & Structure of Blood
Vessels.
https://training.seer.cancer.gov/anatomy/cardiovascular/blood/classi
3) Which of the following is directly dependent on fication.html.
systolic blood pressure? ● Ostenfeld E, Flachskampf FA. Assessment of right ventricular
volumes and ejection fraction by echocardiography: from geometric
a) Capillary Hydrostatic Pressure approximations to realistic shapes.. Echo research and practice
b) Interstitial Hydrostatic Pressure .2015; 2(1): p.R1-R11. doi: 10.1530/ERP-14-0077.
c) Capillary Osmotic Pressure ● Maceira AM, Prasad SK, Khan M, Pennell DJ. Reference right
ventricular systolic and diastolic function normalized to age, gender
d) Interstitial Osmotic Pressure and body surface area from steady-state free precession
cardiovascular magnetic resonance.. Eur Heart J .2006; 27(23):
p.2879-88. doi: 10.1093/eurheartj/ehl336.
CHECK YOUR ANSWERS ● Marieb EN, Hoehn K. Anatomy & Physiology. Hoboken, NJ:
Pearson; 2020.
● Boron WF, Boulpaep EL. Medical Physiology.; 2017.
MICROCIRCULATION CARDIOVASCULAR PHYSIOLOGY : Note #12 3 of 3
Last edited: 8/10/2021
1. FUNDAMENTALS OF BLOOD PRESSURE
Fundamentals of Blood Pressure Medical Editor: Dr. Donya Moslemzadeh
● Ions
OUTLINE
o Calcium
I) BLOOD PRESSURE Hypocalcemia → ↑Heart Rate
II) CARDIAC OUTPUT Hypercalcemia → ↓Heart Rate
o Potassium
III) BLOOD FLOW AND VELOCITY Hyperkalemia → ↓Heart Rate
IV) TOTAL PERIPHERAL RESISTANCE ● Drugs
V) TYPES OF BLOOD FLOW ● CO2, O2, H+
● Age & Gender
VI) PERFUSION PRESSURE
VII) SYSTOLIC AND DIASTOLIC BLOOD PRESSURE
(B) STROKE VOLUME
VIII) MEAN ARTERIAL PRESSURE
(SV)= End Diastolic Volume (EDV)- End Systolic Volume
IX) KOROTKOFF SOUNDS (ESV) =70ml
X) REVIEW QUESTIONS ● EDV: Pre-pumping volume in ventricles
XI) REFRENCES o Volume of blood in ventricles before contraction
o Based on venous return and “stretchy” myocardium
● ESV: Post-pumping volume in ventricles
I) BLOOD PRESSURE o Volume of blood in ventricles after contraction
● Blood Pressure = CO (Cardiac output) * TPR (Total o Based on Contractility and Afterload
Peripheral Resistance) ● The most important factors that affect the Stroke
● MAP= CO X PR Volume are Preload, Contractility and Afterload.
● Cardiac Output (CO) is directly Proportional to Blood
(1) Preload
Pressure
● Peripheral Vascular Resistance (PR) is directly ● Definition: Degree of Stretch of ventricular myocardium
Proportional to Blood Pressure ● Blood Volume in the Heart↑ → EDV↑→ Preload↑
● Blood Pressure (BP) is dependent on Blood Volume ● If Preload↑→↑SV
o Blood Volume is directly Proportional to Blood ● If Preload↓→ ↓SV
Pressure ● Factors affecting the Preload:
↑Blood Volume→↑Blood pressure o Venous Return to heart
• Causes: o Muscle Compliance
o Congestive Heart failure o Filling time
o Liver failure o Heart valve malfunction
o Kidney Failure
(2) Contractility
↓Blood Volume→↓Blood Pressure
• Causes: ● Definition: Strength/Force of Ventricular Contraction
o Severe Vomiting or Diarrhea ● ↑Contractility→↑SV
o Diuretics→↑urine output ● ↓Contractility→↓SV
o Hemorrhage ● Factors affecting contractility :
Bleeding externally o Sympathetic Nervous System
Bleeding internally Epi, NE
o Hormones
T3,T4
II) CARDIAC OUTPUT Glucagon
o Ions
● Cardiac Output (CO)= Heart Rate (HR) X Stroke Volume Calcium
(SV) (Check out the Cardiac output video for more Potassium
details) o Drugs
● CO=HR X SV
o HR → Beats/min (3) Afterload
o SV → ml/beat ● Definition: Pressure the ventricles must overcome to push
Volume of blood being ejected in every beat blood from ventricles into arteries (Aorta and Pulmonary
o CO → ml/min trunk).
Volume of blood being pumped out of heart within ● ↑Afterload→↓SV
one minute ● ↓Afterload→↑SV
● Factors That ↑ Afterload
o ↑Vascular resistance in Systemic Circulation
(A) HEART RATE
o Diastolic Hypertension→↑afterload
Factors that affect HR: (Check out the Cardiac output o Atherosclerosis→↑resistance to blood
video for more details) flow→↑afterload
● Sympathetic Nervous System (SNS)→ ↑Heart Rate
● Parasympathetic Nervous System (PSNS) → ↓Heart Rate
● Hormones
o Increased Thyroid Hormone → ↑Heart Rate
o Low Thyroid Hormone → ↓Heart Rate
Fundamentals of BlOod Pressure CARDIOVASCULAR PHYSIOLOGY : Note #1. 1 of 4
IV) TOTAL PERIPHERAL RESISTANCE
● 2 Formulas:
∆ 𝑝𝑝 ∆ 𝑝𝑝
o 𝐹𝐹 = or 𝐶𝐶𝐶𝐶 =
𝑅𝑅 𝑇𝑇𝑇𝑇𝑇𝑇
8η𝑙𝑙
o 𝑅𝑅 =
𝜋𝜋𝑟𝑟 4
8η𝑙𝑙
● Based on Poiseuille’s Equation( 𝑅𝑅 = ) 3 factors affect
𝜋𝜋𝑟𝑟 4
the Resistance:
Figure 1. SV is dependent on Preload, Contractility and o η = Viscosity of Blood
Afterload. o L= Length of Blood Vessel
o r = Radius of the Vessel
III) BLOOD FLOW AND VELOCITY
(A) VISCOSITY OF BLOOD
● Flow→ cm3 / min
● Cardiac Output is equivalent to Blood Flow (F) ● Viscosity is Directly Proportional to Peripheral Vascular
o CO = Volume of blood being pumped out of heart Resistance
within one minute → ml/min ● ↑Viscosity→↑Peripheral Vascular Resistance
o 1ml= 1cm3 o Causes:
Polycythemia (Increased RBCs)
● Velocity of Blood Flow Dehydration→↓plasma volume →
o Velocity = Rate of Blood Flow Hemoconcentration
o Flow and Cross-Sectional area tell us the Velocity of
Blood Flow ● ↓Viscosity→↓Peripheral Vascular Resistance
o Velocity (cm/ min) = Flow (cm3 / min) / Cross sectional o Causes:
area of the blood vessel (cm2) Anemia (Decreased RBCs)
● Flow (CO) is directly proportional to velocity of blood flow (B) LENGTH OF BLOOD VESSEL
o ↑Flow (CO)→↑Velocity of blood flow ● Length of blood vessel is directly proportional to
o ↓Flow (CO)→↓Velocity of blood flow Peripheral Vascular Resistance
● Cross Sectional Area is Inversely Proportional to velocity ● ↑Length of blood vessels→↑Peripheral Vascular
of blood flow (Figure 2). Resistance
o 𝐴𝐴 = 𝜋𝜋𝑟𝑟 2 o Causes:
o ↑Cross Sectional Area→↓velocity of blood flow ↑ weight and/or height
Examples: Adults have long vessels
• Capillaries (Figure 3) ● ↓Length of blood vessels→↓Peripheral Vascular
o Need slow velocity to exchange O2 and Resistance
Nutrients properly o Causes:
o Capillaries → Slowest velocity ↓weight and/or height
o ↓Cross Sectional Area→↑velocity of blood flow Children have short vessels
Examples:
• Large Arteries like Aorta (Figure 3) (C) RADIUS OF VESSEL
o Need High velocity to push lots of blood ● Radius of the blood vessel is the MAJOR determinant of
from heart to everywhere around the body Peripheral Vascular Resistance
o Aorta → Highest velocity ● Radius of blood vessel is INVERSELY proportional to
Peripheral Vascular Resistance
● ↓Vessel Radius→↑Peripheral Vascular Resistance
o Vasoconstriction
Sympathetic Nervous system
• Norepinephrine
• Epinephrine
Angiotensin II
Vasopressin (ADH)
Endothelin
● ↑Vessel radius→↓Peripheral Vascular Resistance
Figure 2. Relationship between Velocity and Cross-Sectional o Vasodilation
Area. Nitric Oxide and prostaglandins
Atrial Natriuretic peptide
Increased Cellular Activity
• Decreased oxygen (O2)
• Increased carbon dioxide (CO2)
• Increased protons (H+)
● Resistance to Blood flow in SERIES
o Example: One artery→ one arteriole → one capillary
→ one venule → one vein
o Not as realistic in human body
o R (total)= R1+ R2+ R3
● Resistance to Blood flow in PARALLEL
o Example: One artery→ multiple arterioles → multiple
capillaries → multiple venules → one vein
o More realistic in human body
Figure 3. Cross-Sectional Area of 1. Aorta, 2. Arteries, 3. o 1/R total= 1/R1 + 1/R2 + 1/R3
Arterioles, 4. Capillaries, 5. Venules, 6. Veins.
2 of 4 CARDIOVASCULAR PHYSIOLOGY: Note #1. Fundamentals of BlOod Pressure
V) TYPES OF BLOOD FLOW This Narrowed lumen‚→ ↓Diameter BUT Really
INCREASES the velocity across the narrowed
● Blood flow is dependent on Reynolds equation (Re) area →↑ Reynolds number → ↑Turbulence
● Re= Density of blood X Diameter of vessel X velocity of Can be heard as a Bruit with stethoscope
blood flow/ Viscosity of Blood o Aortic Stenosis, → Stiff valves create a disturbance in
𝑑𝑑𝑑𝑑𝑑𝑑�
● 𝑅𝑅𝑅𝑅 = 𝜂𝜂 the normal flow pattern and can produce this chaotic
o d = Diameter flow pattern
o v = Velocity The Stiff valves‚ → ↓Diameter BUT Really
o ρ = Density INCREASEs the velocity across the valve‚ →
o η = Viscosity ↑Reynolds number‚→↑Turbulence
Can be heard as a murmur with a stethoscope
● Density, Diameter and Velocity are Directly Proportional
o Anemia →↓Viscosity‚→↑Reynolds
with Reynolds Number
Number‚→↑Turbulence
o ↑Density, Diameter and Velocity→↑ Reynolds Number
o ↓Density, Diameter and Velocity→↓Reynolds Number Also, Anemia reflexively Increases Cardiac
Output‚→↑Flow‚→↑ velocity‚→↑ Reynolds
● Viscosity is Inversely proportional to Reynolds Number number‚→↑turbulence
o ↑Viscosity→↓Reynolds Number
o ↓Viscosity→↑Reynolds Number
● High Re → Turbulent Flow
● Low Re → Laminar Flow
(A) LAMINAR FLOW
● Laminar Flow= Streamlining= Normal Flow
● Definition: Layered flow pattern
● Highest velocity flows in the
center of the blood vessel
● Lowest velocity flows near walls
of the blood vessel
● Laminar Flow is Silent.
● No effect on resistance
● Pressure↑ → Laminar Flow ↑ (Figure 3)
Figure 5. Turbulent Flow
VI) PERFUSION PRESSURE
● ∆ 𝑝𝑝 = 𝑀𝑀𝑀𝑀𝑀𝑀 − 𝐶𝐶𝐶𝐶𝐶𝐶
● Central Venus pressure = Right atrial pressure → so
small = 3–8 mm Hg
o Pressure that tries to bring the blood toward the heart
● ∆ 𝑝𝑝 ≅ 𝑀𝑀𝑀𝑀𝑀𝑀
VII) SYSTOLIC AND DIASTOLIC BLOOD
PRESSURE
Figure 4. Laminar Flow (A) SYSTOLIC BLOOD PRESSURE (SBP)
● Pressure in the arteries exerted by the ventricles during
contraction or systole
(B) TURBULENT FLOW ● Normal SBP: 120mmHg
● Definition: Chaotic flow pattern (B) DIASTOLIC BLOOD PRESSURE (DBP)
● As a result of turbulent flow ● Pressure in the arteries during ventricular relaxation or
o Flow decreases Diastole
o Perfusion Pressure increases ● Normal DBP: 80mmHg
∆ 𝑝𝑝↑
o 𝑅𝑅↑↑ =
𝐹𝐹 ↓ (C) PULSE PRESSURE
o Resistance increases
● Pulse Pressure= SBP-DBP
● Physiological Causes: ● Normal PP: 40mmHg
o Vasoconstriction narrows lumen ● Wide Pulse Pressure (>>>40) →due to ↑SV
and may create this Chaotic flow o Examples:
pattern Anemia→↑SV to increase more blood delivery to
o High Velocities in large vessels like the Aorta may compensate for ↓Hemoglobin in RBCs→↓less
create this Chaotic flow pattern oxygen delivered to tissues because of anemia
o Arterial Bifurcation points may create this Chaotic Hyperthyroidism→↑Contractility→↑SV
flow pattern Aortic regurgitation→↑blood regurgitation into
● Pathological Causes: ventricle→↓Diastolic Blood
o Atherosclerotic Plaque/Thrombus →can narrow pressure→↑EDV→↑Preload→↑SV
vessel lumen‚ → may create this Chaotic flow pattern ● Narrow Pulse Pressure (<<<40) → due to Decreased SV
o Examples:
Fundamentals of BlOod Pressure CARDIOVASCULAR PHYSIOLOGY : Note #1. 3 of 4
Systolic Congestive Heart Failure→↓SV Formulas:
Cardiac Tamponade → restricts filling of ● 𝐵𝐵𝐵𝐵 = 𝐶𝐶𝐶𝐶 × 𝑇𝑇𝑇𝑇𝑇𝑇 , 𝑀𝑀𝑀𝑀𝑀𝑀 = 𝐶𝐶𝐶𝐶 × 𝑇𝑇𝑇𝑇𝑇𝑇
heart→↓EDV→↓preload→↓SV ● 𝐶𝐶𝐶𝐶 = 𝐻𝐻𝐻𝐻 × 𝑆𝑆𝑆𝑆
● 𝐹𝐹𝐹𝐹𝐹𝐹𝐹𝐹 = 𝐶𝐶𝐶𝐶
VIII) MEAN ARTERIAL PRESSURE ● 𝑉𝑉𝑉𝑉𝑉𝑉𝑉𝑉𝑉𝑉𝑉𝑉𝑉𝑉𝑉𝑉 𝑜𝑜𝑜𝑜 𝐵𝐵𝐵𝐵𝐵𝐵𝐵𝐵𝐵𝐵 𝐹𝐹𝐹𝐹𝐹𝐹𝐹𝐹 = 𝐹𝐹𝐹𝐹𝐹𝐹𝐹𝐹 ⁄𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶𝐶 𝑠𝑠𝑠𝑠𝑠𝑠𝑠𝑠𝑠𝑠𝑠𝑠𝑠𝑠𝑠𝑠𝑠𝑠 𝑎𝑎𝑎𝑎𝑎𝑎𝑎𝑎
𝟏𝟏
● ∆𝑝𝑝 = 𝑀𝑀𝑀𝑀𝑀𝑀 − 𝐶𝐶𝐶𝐶𝐶𝐶, ∆𝑝𝑝 ≅ 𝑀𝑀𝑀𝑀𝑀𝑀
● 𝑴𝑴𝑴𝑴𝑴𝑴 = 𝑫𝑫𝑫𝑫𝑫𝑫 + 𝑷𝑷𝑷𝑷 ● ∆𝑝𝑝 = 𝐹𝐹𝐹𝐹𝐹𝐹𝐹𝐹 × 𝑅𝑅 (𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟𝑟)
𝟑𝟑
● MAP= Cardiac Output (CO) X Peripheral Vascular ● 𝑅𝑅 = 8𝜂𝜂𝜂𝜂 ⁄𝜋𝜋𝑟𝑟 4
Resistance (PR) 1 2
● 𝑀𝑀𝑀𝑀𝑀𝑀 = 𝑆𝑆𝑆𝑆𝑆𝑆 + 𝐷𝐷𝐷𝐷𝐷𝐷, 𝑀𝑀𝑀𝑀𝑀𝑀 = 𝐷𝐷𝐷𝐷𝐷𝐷 + 𝑃𝑃𝑃𝑃
1
3 3 3
● Normal MAP: 93mmHg
● 𝑃𝑃𝑃𝑃 = 𝑆𝑆𝑆𝑆𝑆𝑆 − 𝐷𝐷𝐷𝐷𝐷𝐷
● This pressure tells us how well we are perfusing 𝑑𝑑𝑑𝑑𝑑𝑑�
(Delivering O2 and Nutrients) a tissue ● 𝑅𝑅𝑅𝑅 = 𝜂𝜂
● ↓MAP→↓perfusion to tissue
o Examples: Very important to know about ↓MAP
↓MAP→↓perfusion of Brain tissue →Ischemia → X) REVIEW QUESTIONS
damage tissue
↓MAP→↓perfusion to Kidney→ Ischemia → In which of the following types of blood vessels will
damage tissue flow be the slowest?
↓MAP→↓perfusion to Liver→ Ischemia→ damage a. Arteries
tissue b. Arterioles
c. Capillaries
● ↑MAP→↑ perfusion to tissue
d. Venules
o Examples
e. Veins
Norepinephrine and Epinephrine
→↑contractility→↑SV→↑ CO→↑MAP
Which of the following statements will be true about
Intravenous fluids→↑blood volume→↑MAP
the measured velocity of blood flow?
Norepinephrine and epinephrine
a. It is higher in the capillaries than the arterioles.
→↑vasoconstriction→↑resistance to blood
b. It is higher in the veins than in the venules.
flow→↑MAP
c. It is higher in the veins than the arteries.
d. It falls to zero in the descending aorta during
IX) KOROTKOFF SOUNDS
diastole.
● Definition: The sounds you hear when measuring the e. It is reduced in a constricted area of a blood vessel.
blood pressure via Auscultatory method.
● Measuring Blood Pressure via Auscultatory Method
o Wrap the blood pressure cuff → Inflate the cuff → cuff CHECK YOUR ANSWERS
pressure >> SBP (stopping the blood flow) → deflate
the cuff gradually→ tapping and swishing
sounds=Korotkoff sounds→ the first pulse XI) REFRENCES
sound=SBP → continue deflating → when there is no
constriction and blood flows freely → sound ● Marieb, E. N., & Hoehn, K. N. (2012). Human Anatomy &
Physiology (9th Edition) (Marieb, Human Anatomy &
disappear = DBP Physiology) (9th ed.). Pearson.
● Hall, J. H. E., & Hall, M. M. H. E. (2020). Guyton and Hall
Textbook of Medical Physiology (Guyton Physiology) (14th ed.).
Elsevier.
● AMBOSS: medical knowledge platform for doctors and students.
(n.d.). Amboss. Retrieved August 9, 2021, from
https://www.amboss.com/us/
● Barrett, K., Barman, S., Boitano, S., & Reckelhoff, J. (2017).
Ganong’s Physiology Examination and Board Review (1st ed.).
McGraw-Hill Education / Medical.
Figure 6. Auscultatory method for measuring systolic and
diastolic arterial pressures. [Hall & Hall, 2020]
4 of 4 CARDIOVASCULAR PHYSIOLOGY: Note #1. Fundamentals of BlOod Pressure
Last edited: 8/16/2021
14. BLOOD PRESSURE REGULATION- HYPOTENSION
Cardiovascular: Blood Pressure Regulation- Hypotension Medical Editor: Donya Moslemzadeh
OUTLINE BARORECEPTOR REFLEX
Response to Low Blood Pressure:
I) INTRODUCTION When Pressure is Low→ ↓ stretch on vessel wall→ ↓
II) BARORECEPTORS
stretch of sensory nerve endings of
III) RENAL REGULATION OF BLOOD PRESSURE
Aortic Sinus and Carotid Sinus→ ↓
IV) HIGHER BRAIN CENTERS’ EFFECT ON BLOOD
PRESSURE activation of mechanically gated Na+
V) REVIEW QUESTIONS channels→ ↓ Na+ enters nerve
VI) REFRENCES endings→ ↓ action potentials are carried
down Glossopharyngeal and Vagus
sensory fibers→ Medulla→ Nucleus
I) INTRODUCTION Tractus Solitarius (NTS)
Nucleus Tractus Solitarius (NTS)
Hypotension o This is a relay center
Definition: Low Blood Pressure o ↓ signals from the Vagus and Glossopharyngeal
o Systolic Blood Pressure (SBP)< 100mmHg nerve
Normal Blood Pressure [UpToDate 2021] NTS→ (-) Cardiac Inhibitory Center in medulla
o Systolic Blood Pressure: < 120 NTS→ (+) Cardio acceleratory Center in Medulla
o Diastolic Blood Pressure: < 80 NTS→ (+) Vasomotor Center in Medulla
Compensation mechanisms in response to Hypotension:
o Baroreceptor reflex
o Renin-Angiotensin- Aldosterone System
Formulas & Relations:
𝐵𝐵𝐵𝐵 = 𝐶𝐶𝐶𝐶 × 𝑇𝑇𝑇𝑇𝑇𝑇
𝐶𝐶𝐶𝐶 = 𝐻𝐻𝐻𝐻 × 𝑆𝑆𝑆𝑆
𝑅𝑅 = 8𝜂𝜂𝜂𝜂 ⁄𝜋𝜋𝑟𝑟 4
↑Heart rate→↑CO
↓Heart Rate→↓CO
↑EDV→↑SV→↑CO
↓EDV→↓SV→↓CO
↑ESV→↓SV→↓CO
↓ESV→↑SV→↑CO
↑Preload→↑SV→↑CO
↓Preload→↓SV→↓CO
↑Contractility→↑ SV→↑ CO
↓Contractility→↓SV→↓CO
↑Afterload→↓SV→↓CO
↓Afterload→↑SV→↑CO
Figure 1. Baroreceptor Reflex.
↓Vessel Radius→↑Peripheral Vascular Resistance
↑Vessel radius→↓Peripheral Vascular Resistance
(1) Cardio Inhibitory Center
= Dorsal Nucleus Vagus
II) BARORECEPTORS Connected with the Parasympathetic Nervous System
Inhibited due to Low Blood Pressure signal coming
Definition: Stretch-sensitive nerve endings located in: through Sensory afferent fibers of CN X and CN IX to the
NTS
o Aortic Arch
Around Aortic Arch there is Aortic Sinus that is (2) Cardio Acceleratory Center
sensitive to pressure changes. Connected with the Sympathetic Nervous System
Aortic Sinus are innervated by sensory fibers of Stimulated due to Low Blood Pressure signal coming
Cranial Nerve X (Vagus nerve) through Sensory afferent fibers of CN X and CN IX to the
o Bifurcation of Common Carotid Artery NTS
Around Bifurcation there is Carotid sinus that are o Activates Sympathetic Nervous system→
sensitive to Pressure changes ↑Norepinephrine release→ stimulates Beta 1
Carotid Sinus are innervated by sensory fibers of Receptors on nodal cells→ ↑HR→ ↑Cardiac Output→
Cranial Nerve IX (Glossopharyngeal Nerve) ↑Blood pressure
SA node, AV node
• NE → B1 receptors → Gs-protein → AC →
cAMP →PKA → Phosphorylation of
Ca2+channel → opens → Ca2+ flows in → HR↑
→ CO ↑ → BP↑
Blood Pressure Regulation- Hypotension CARDIOVASCULAR PHYSIOLOGY : Note #14. 1 of 4
o Activates Sympathetic Nervous system→ III) RENAL REGULATION OF BLOOD PRESSURE
↑Norepinephrine release→ stimulates Beta 1
Receptors on contractile cells→ ↑Contractility→ The kidneys act both directly and indirectly to regulate
↑Stroke volume→ ↑Cardiac output→ ↑Blood pressure Blood pressure [Marieb].
Myocardium (contractile unit) Direct Renal Mechanism
• NE → B1 receptors → Gs-protein→ AC → o ↓Systemic BP (SBP<100mmhg) →↓Hydrostatic
cAMP → PKA → phosphorylation of Ca2+ Pressure in Glomerulus→↓GFR→↓ Urine output
channel → opens → Ca2+ flows in → more (Oliguria) → ↑Blood Volume→ ↑BP
cross bridge formation → increase Indirect Renal Mechanism
contraction→ SV↑ → CO ↑ → BP↑ o Renin-Angiotensin-Aldosterone System
RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM
RAAS is stimulated in 3 ways: [Boron]
Decreased systemic blood pressure (Sympathetic effect
on JG cells)
a. ↓BP→↑sympathetic Nervous system→↑B1 activity
on Juxtaglomerular cells in the Afferent arteriole of
glomerulus→↑renin released→↑Renin Angiotensin
Aldosterone ADH Axis Activity
Decreased NACL Concentration at the Macula Densa
a. ↓BP→↓GFR→↓ Na+ and Cl- levels in tubules→
stimulates Macula Densa cells in distal convoluted
Tubule→ ↑release PGE2→ stimulates
Juxtaglomerular cells in the Afferent arteriole of
Figure 2. Beta-1 Adrenergic Receptor Mechanism.
glomerulus to release Renin and trigger
vasodilation of afferent arterioles→ ↑GFR to
maintain some degree of urine output despite ↓BP
(3) Vasomotor Center
Decreased Renal Perfusion Pressure (renal
Connected with the Sympathetic Nervous system
baroreceptors)
Stimulated due to Low Blood Pressure signal coming
a. ↓BP→ ↓Blood Flow to the kidneys → Stimulate JG
through Sensory afferent fibers of CN X and CN IX to the
cells →↑renin released→↑Renin Angiotensin
NTS
Aldosterone ADH Axis Activity
o Activates Sympathetic Nervous system→
↑Norepinephrine release→ stimulates alpha-1
Receptors on smooth muscle cells (Tunica Media) in (1) Production of Angiotensin-II
arterioles→ ↑vasoconstriction of arterioles→
Components:
↓Vessel diameter→ ↑Resistance→ ↑Blood pressure
o Renin
o Activates Sympathetic Nervous system→
Enzyme produced by the kidneys
↑Norepinephrine release→ stimulates alpha-1
o Angiotensinogen
Receptors on smooth muscle cells in venules→
Protein produced by the liver
↑Vasoconstriction of venules→ ↓Vessel diameter→
circulates in the blood
↑Resistance→ ↑Blood pressure→ ↑ venous return to
o Angiotensin-I
heart→ ↑Preload→ ↑Stroke volume→ ↑Cardiac
precursor molecule
output→ ↑Blood pressure
o Angiotensin Converting Enzyme (ACE)
Mostly Produced by Vascular endothelial cells of
the lungs
o Angiotensin-II
↓Systemic BP→ stimulates Juxtaglomerular cells which
are pressure receptors in the Afferent arteriole of
glomerulus in the kidney release Renin which converts
Angiotensinogen made by the liver into→ Angiotensin-I
reacts with→ Angiotensin Converting enzyme (ACE)
which converts Angiotensin-I→ Angiotensin-II
(2) Angiotensin-II action Pathways
(i) Vasoconstriction
Angiotensin-II receptors on the Tunica Media of the
Figure 3. Alpha-1 Receptor Mechanism. Arterioles
Angiotensin-II stimulates Vasoconstriction of Systemic
Adrenal Medulla Arterioles→↓Vessel Diameter→ ↑Resistance→ ↑BP
Activated Sympathetic Nervous system → Adrenal
Medulla → Chromaffin Cells → ↑ production of (ii) ↑Blood Volume- Aldosterone
Epinephrine (80%) and Norepinephrine (20%) →
Beta-1 and Alpha-1 receptors→ ↑HR, ↑Contractility, Aldosterone
↑vasoconstriction →↑Blood pressure o Steroid Hormone produced by Zona Glomerulosa of
the adrenal medulla
Angiotensin-II Stimulates Aldosterone Production
from Adrenal Cortex→ Aldosterone ↑Na+ and
H20 reabsorption in Distal Convoluted Tubules of
kidney→ ↑ Blood Volume→ ↑BP
2 of 4 CARDIOVASCULAR PHYSIOLOGY: Note #1. Blood Pressure Regulation- Hypotension
Mechanism of Action of Aldosterone
o Acts on Distal Convoluted Tubules Protective mechanism of kidneys to maintain
o Aldosterone binds to the intracellular receptor→ GFR
activate specific Genes → ↑production of 3 Proteins
Na+ Channels o ↓BP→↓GFR→↓ Na+ and Cl- levels in tubules →
• More Na+ flows to the cells stimulates Macula Densa cells in distal
convoluted Tubule→ ↑release PGE2→
K+ Channels
stimulates Juxtaglomerular cells in the Afferent
• More K+ flows out of the cells to the Distal arteriole of glomerulus to release Renin and
Convoluted Tubules trigger vasodilation of afferent arterioles→ ↑GFR
Na+ / K+ / ATPase Pump (on Basolateral to maintain some degree of urine output despite
Membrane) ↓BP
• 3 Na+ reabsorbed to the circulation in
exchange of 2 K+ o ↑↑↑↑ Angiotensin-II levels→↑Vasoconstriction of
o H2O follows Na+ back to the circulation efferent arteriole of Glomerulus in
kidneys→↓blood flow leaving the glomerular
(iii) ↑Blood Volume- ADH capillaries→↑ hydrostatic pressure in the
glomerulus→↑GFR
ADH =Anti-Diuretic Hormone= Vasopressin
Supraoptic nucleus (specials cells in the Hypothalamus)
→ Posterior Pituitary glands→ ADH release
o Angiotensin-II Stimulates Posterior Pituitary→ ↑ADH
release→ ↑water reabsorption in Collecting duct of IV) HIGHER BRAIN CENTERS’ EFFECT ON BLOOD
kidneys→ ↑Blood Volume→ ↑BP PRESSURE
Mechanism of Action of ADH Higher Brain centers that can influence the blood
o Acts on 2 locations in the nephron pressure
Collecting duct o Cerebral Cortex
Distal Convoluted Tubules o Hypothalamus
o ADH binds to V2-Receptore (Gs-Protein) → AC → o Limbic Nuclei
cAMP → PKA → Phosphorylation vesicles containing
Stimulated as a response to Stress, Emotions, etc.
AQ-II → ↑ express of AQ-II on the membrane → ↑
reabsorption of H2O
(iv) ↑Blood Volume- Thirst Center Influence of Higher Brain Center
Thirst Center Reflexes that regulate blood pressure are integrated in
o Angiotensin-II→↑ Hypothalamic thirst center the medulla oblongata of the brain stem. Although the
activity→↑consumption of water→↑absorption across cerebral cortex and hypothalamus are not involved in
GIT→ ↑ Blood Volume→ ↑ BP routine controls of blood pressure, these higher brain
centers can modify arterial pressure via relays to the
(v) ↑Blood Volume- Kidney medullary centers.
For example, the fight-or-flight response mediated by the
Angiotensin-II→↑ Na+, Cl- and H20 reabsorption in hypothalamus has profound effects on blood pressure.
Proximal Convoluted Tubules of kidney→ ↑ Blood (Even the simple act of speaking can make your blood
Volume→ ↑ BP pressure jump if the person you are talking to makes you
anxious.) The hypothalamus also mediates the
redistribution of blood flow and other cardiovascular
responses that occur during exercise and changes in
body temperature. [Marieb & Hoehn, 2012, p. 707]
Figure 4. Sites of Action of ADH, Aldosterone and Angiotensin-
II on a Nephron.
Figure 5. Levels of ANS control. (Marieb & Hoehn, 2012, p.
538)
Blood Pressure Regulation- Hypotension CARDIOVASCULAR PHYSIOLOGY : Note #14. 3 of 4
Figure 6. Physiologic response to low blood pressure.
V) REVIEW QUESTIONS
Renin is not released in response to which of the In the normal operation of the arterial baroreceptor
following? [Khan Academy | Free Online Courses, Lessons & Practice, n.d.] reflex, a cardiovascular disturbance that lowers
a. Detection of low plasma electrolyte levels by macula mean arterial pressure will evoke a decrease in
densa cells [Mohrman & Heller, 2018]
a. Detection of low blood pressure by baroreceptor a. baroreceptor firing rate
cells b. sympathetic nerve activity
b. Detection of low glomerular filtrate electrolyte levels c. heart rate
by macula densa cells d. total peripheral resistance
c. Innervation by sympathetic nerve cells e. myocardial contractility
In general, normal kidneys tend to retain sodium
Which of the following accurately describes a and fluid in the body whenever [Mohrman & Heller, 2018]
function of angiotensin-II? [Khan Academy | Free Online Courses, a. arterial pressure is high
Lessons & Practice, n.d.]
b. parasympathetic nerve activity is high
a. Acts on the pituitary to increase secretion of c. sympathetic nerve activity is high
aldosterone d. plasma aldosterone levels are low
b. Acts on smooth muscle cells lining blood vessels e. plasma renin levels are low
decreasing resistance to blood flow CHECK YOUR ANSWERS
c. Acts on nephrons to increase water retention in the
blood VI) REFRENCES
d. Acts on the adrenal glands to increase secretion of
● Marieb, E. N., & Hoehn, K. N. (2012). Human Anatomy &
ADH Physiology (9th Edition) (Marieb, Human Anatomy &
Physiology) (9th ed.). Pearson.
● Hall, J. E., & Hall, M. E. (2020). Guyton and Hall Textbook of
Medical Physiology (Guyton Physiology) (14th ed.). Elsevier.
Which of the following is least likely to trigger the ● AMBOSS: medical knowledge platform for doctors and students.
release of ADH from the posterior pituitary gland? (n.d.). Amboss. Retrieved August 9, 2021, from
[Khan Academy | Free Online Courses, Lessons & Practice, n.d.] https://www.amboss.com/us/
● Boron, W. F., & Boulpaep, E. L. (2016). Medical Physiology (3rd
a. Increase in angiotensin-II plasma concentration ed.). Elsevier.
b. Decrease in blood pressure ● Mohrman, D. E., & Heller, L. J. (2018). Cardiovascular
c. High blood volume Physiology (9th ed.). McGraw-Hill Education / Medical.
● UpToDate: Evidence-based Clinical Decision Support. (n.d.).
d. Decrease in sodium concentration in glomerular
Uptodate. Retrieved August 16, 2021, from
filtrate http://www.uptodate.com/index
● Khan Academy | Free Online Courses, Lessons & Practice.
(n.d.). Khan Academy. Retrieved August 16, 2021, from
https://www.khanacademy.org/
4 of 4 CARDIOVASCULAR PHYSIOLOGY: Note #1. Blood Pressure Regulation- Hypotension
Last edited: 8/16/2021
15. BLOOD PRESSURE REGULATION- HYPERTENSION
Cardiovascular: Blood Pressure Regulation- Hypertension Medical Editor: Donya Moslemzadeh
OUTLINE BARORECEPTOR REFLEX
Response to High Blood Pressure:
I) INTRODUCTION
II) BARORECEPTORS
When Pressure is HIGH→ ↑stretch on
III) RENAL REGULATION
vessel wall→ ↑ stretch of sensory nerve
IV) ATRIAL NATRIURETIC PEPTIDE (ANP)
V) REFRENCES endings of Aortic Sinus and Carotid
Sinus→ ↑ activation of mechanically
gated Na+ channels→ ↑ Na+ enters
nerve endings→ ↑ action potentials are
carried down Glossopharyngeal and
I) INTRODUCTION Vagus sensory fibers→ Medulla→ Nucleus Tractus
Solitarius (NTS)
Hypertension
Definition: High Blood Pressure Nucleus Tractus Solitarius (NTS)
o Systolic Blood Pressure, SBP>140mmHg o This is a relay center
o Diastolic Blood Pressure, DBS >90mmHg o Signals from the Vagus and glossopharyngeal nerve
Normal Blood Pressure [UpToDate] NTS→ (+) Cardiac Inhibitory Center in medulla
o Systolic Blood Pressure: < 120 NTS→ (-) Cardio acceleratory Center in Medulla
o Diastolic Blood Pressure: < 80 NTS→ (-) Vasomotor Center in Medulla
Physiological response to Hypertension
o Baroreceptor reflex
o Inhibition of Renin-Angiotensin- Aldosterone System
Formulas & Relations: Vasomotor center has 2 important areas:
𝐵𝐵𝐵𝐵 = 𝐶𝐶𝐶𝐶 × 𝑇𝑇𝑇𝑇𝑇𝑇
𝐶𝐶𝐶𝐶 = 𝐻𝐻𝐻𝐻 × 𝑆𝑆𝑆𝑆 1) C1 is for constriction of the
𝑅𝑅 = 8𝜂𝜂𝜂𝜂 ⁄𝜋𝜋𝑟𝑟 4 vessels, activated when the
blood pressure is low and
inhibited when the blood
↑Heart rate→↑CO
pressure is high
↓Heart Rate→↓CO
↑EDV→↑SV→↑CO
2) A1 is for vasodilation of the
↓EDV→↓SV→↓CO
vessels , activated when
↑ESV→↓SV→↓CO
the blood pressure is high and inhibited when
↓ESV→↑SV→↑CO
the blood pressure is low
↑Preload→↑SV→↑CO
↓Preload→↓SV→↓CO
↑Contractility→↑ SV→↑ CO
↓Contractility→↓SV→↓CO
↑Afterload→↓SV→↓CO
↓Afterload→↑SV→↑CO
↓Vessel Radius→↑Peripheral Vascular Resistance
↑Vessel radius→↓Peripheral Vascular Resistance
II) BARORECEPTORS
Definition: Stretch-sensitive nerve endings
Location:
o Aortic Arch
Around Aortic Arch there is Aortic Sinus that is
sensitive to pressure changes.
Aortic Sinus are innervated by sensory fibers of
Cranial Nerve X (Vagus nerve)
o Bifurcation of Common Carotid Artery
Around Bifurcation there is Carotid sinus that are
sensitive to Pressure changes Figure 1. Baroreceptor reflex in High BP.
Carotid Sinus are innervated by sensory fibers of
Cranial Nerve IX (Glossopharyngeal Nerve)
Blood Pressure Regulation- Hypertension CARDIOVASCULAR PHYSIOLOGY : Note #15. 1 of 4
(1) Cardio- Inhibitory Center (3) Vasomotor Center
= Dorsal Nucleus Vagus Part of the Sympathetic Nervous system
Part of Parasympathetic Nervous System Inhibited due to Low Blood Pressure signal coming
Stimulated due to High Blood Pressure signal coming through Sensory afferent fibers of CN X and CN IX to the
through Sensory afferent fibers of CN X and CN IX to the NTS
NTS o Inhibits Sympathetic Nervous system→
Activates Parasympathetic Nervous system→ ↓Norepinephrine release→ ↓ stimulation of alpha-1
↑Acetylcholine release→ stimulates M2-Receptors on Receptors on smooth muscle cells (Tunica Media) in
nodal cells→ ↓HR→ ↓Cardiac Output→ ↓Blood pressure arterioles→ Vasodilation of arterioles→ ↑Vessel
o Right Vagus → SA node diameter→ ↓Resistance→↓Blood pressure (Diastolic
o Left Vagus → AV node Blood Pressure)
No innervation to myocardium from the Vagus Nerve
Changing Total Peripheral Resistance= Changing
M2 Receptor → Gi → Inhibits AC → ↓cAMP → ↓PKA → Diastolic Blood Pressure
inhibits Ca2+ channels→ ↓ Ca2+→ Hyperpolarization
M2 Receptor → βi and γi → Activates K+ Channels → K+
Adrenal Medulla
leaking out of the cell → Hyperpolarization Inhibited Sympathetic Nervous system → Adrenal
Medulla → Chromaffin Cells →↓production of
Epinephrine (80%) and Norepinephrine (20%) →
↓↓ Stimulation Beta-1 and Alpha-1 receptors→ ↓HR,
↓Contractility, Vasodilation →↓Blood pressure
III) RENAL REGULATION
The kidneys act both directly and indirectly to regulate
Blood pressure: [Marieb & Hoehn, 2012]
Direct Renal Mechanism
o The direct renal mechanism alters blood volume
independently of hormones. When either blood
volume or blood pressure rises, the rate at which fluid
Figure 2. M2 Receptor mechanism. filters from the bloodstream into the kidney tubules
speeds up. In such situations, the kidneys cannot
reabsorb the filtrate rapidly enough, and more of it
leaves the body in urine. As a result, blood volume
Good to Know: and blood pressure fall. [Marieb & Hoehn, 2012]
o ↑↑ Systemic BP (SBP>140mmhg) → ↑Hydrostatic
Chronotropy: Any influence on Heart Rate [AMBOSS]] Pressure in Glomerulus→ ↑GFR→ ↑Urine output→
o Positive Chronotropic action ↓Blood Volume→ ↓BP
SNS→ NE, Epi → ↑HR Indirect Renal Mechanism
o Negative Chronotropic action
o Renin-Angiotensin-Aldosterone System
PSNS → Ach → ↓HR
Inotropy: Any influence on Myocardial contraction
[AMBOSS] RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM
o Positive Inotropic action
SNS → NE, Epi → ↑Contractility (1) Production of Angiotensin-II
o Negative Inotropic action →↓ Contractility
Components:
o Renin
Enzyme produced by the kidneys
o Angiotensinogen
Protein produced by the liver
(2) Cardio- Acceleratory Center circulates in the blood
Part of Sympathetic Nervous System o Angiotensin-I
Inhibited due to High Blood Pressure signal coming Precursor molecule
through Sensory afferent fibers of CN X and CN IX to the o Angiotensin Converting Enzyme (ACE)
NTS Mostly Produced by Vascular endothelial cells of
the lungs
o Inhibits Sympathetic Nervous system→ o Angiotensin-II
↓Norepinephrine release→ ↓Stimulation of Beta 1
(2) Angiotensin-II Action Pathways
Receptors on nodal cells (SA & AV nodes) →↓HR→
↓Cardiac Output→ ↓Blood pressure (i) Vasoconstriction
o Inhibits Sympathetic Nervous system→
↓Norepinephrine release→ inhibits Beta 1 Receptors o Angiotensin-II receptors on the Tunica Media of the
on contractile cells→ ↓Contractility→ ↓Stroke Arterioles
volume→ ↓Cardiac output→ ↓Blood pressure o Angiotensin-II stimulates Vasoconstriction of Systemic
Arterioles→↓Vessel Diameter→ ↑Resistance→ ↑BP
2 of 4 CARDIOVASCULAR PHYSIOLOGY: Note #1. Blood Pressure Regulation- Hypertension
(ii) ALDOSTERONE IV) ATRIAL NATRIURETIC PEPTIDE (ANP)
o Steroid Hormone Produced by Zona Glomerulosa of Definition: A peptide hormone released from atrial
the adrenal medulla myocytes in response to increased stretch on the atrium
o Angiotensin-II Stimulates Aldosterone Production
[AMBOSS]
from Adrenal Cortex→ Aldosterone ↑Na+ and H20 Natriuretic= Producing Salty Urine
reabsorption in Distal Convoluted Tubules of kidney→
↑ Blood Volume→ ↑BP Response to High Blood Pressure
↑↑ BP→ Stretches atrial chambers→ stimulates release
o Mechanism of Action of Aldosterone of Atrial Natriuretic Peptide (ANP)→ ↓Renin Angiotensin
Acts on Distal Convoluted Tubules Aldosterone ADH Axis
Aldosterone binds to the intracellular receptor→
activate specific Genes → ↑production of 3 ANP→ ↓Angiotensin II pathways
Proteins
(i) Vasodilation
Na+ Channels
o ANP blocks Angiotensin II→ ↑Vasodilation of
o More Na+ flows to the cells
Systemic Arterioles→↑Diameter→↓Resistance→↓BP
K+ Channels
o More K+ flows out of the cells to the Distal (ii) Decrease blood volume
Convoluted Tubules
o ANP→↓Angiotensin II→↓Aldosterone Production
Na+ / K+ / ATPase Pump (on Basolateral Membrane)
from Adrenal Cortex→↓Na+ and H20 reabsorption in
o 3 Na+ reabsorbed to the circulation in
Distal Convoluted Tubules→↓Blood Volume→↓BP
exchange of 2 K+
H2O follows Na+ back to the circulation
o ANP→↓Angiotensin II→↓ADH release from Posterior
(iii) ADH Pituitary→↓water reabsorption in Collecting
duct→↓Blood Volume→↓BP
o ADH =Anti-Diuretic Hormone= Vasopressin
o Supraoptic nucleus (specials cells in the
o ANP→↓Angiotensin II→↓Hypothalamic thirst center
Hypothalamus) → Posterior Pituitary glands→
activity→↓consumption of water→↓absorption across
Release of ADH
GIT→↓Blood Volume→↓BP
o Angiotensin-II Stimulates Posterior Pituitary→ ↑ADH
release→ ↑water reabsorption in Collecting duct of
o ANP→↓Angiotensin II→↓Na+ and H20 reabsorption in
kidneys→ ↑Blood Volume→ ↑BP
Proximal Convoluted Tubules→↓Blood Volume→↓BP
o Mechanism of Action of ADH
Acts on 2 locations in the nephron ↓Na+ and H20 reabsorption→ ↑ Urine output = Polyuria
• Collecting duct
• Distal Convoluted Tubules
ADH binds to V2-Receptore (Gs-Protein) → AC →
cAMP → PKA → Phosphorylation vesicles
containing AQ-II → ↑ express of AQ-II on the
membrane → ↑ reabsorption of H2O
(iv) Thirst Center
o Angiotensin-II→↑ Hypothalamic thirst center
activity→↑consumption of water→↑absorption across
GIT→ ↑ Blood Volume→ ↑ BP
(v) Kidney
o Angiotensin-II→↑ Na+, Cl- and H20 reabsorption in
Proximal Convoluted Tubules of kidney→ ↑ Blood
Volume→ ↑ BP
(3) Response to High Blood Pressure
↑↑Systemic BP (SBP>140mmhg)→ ↓ Renin Angiotensin
Aldosterone ADH Axis
↑↑ BP→ ↓ Juxtaglomerular cell activity in the Afferent
arteriole of glomerulus→ ↓ Renin release
↑↑ BP→ ↓sympathetic nervous system activity→↓B1
activity on Juxtaglomerular cells in the Afferent arteriole
of glomerulus→ ↓Renin release Figure 3. Sites of action of ADH, Aldosterone, Angiotensin-II
↑↑ BP→ ↑GFR→ ↑Na+ and Cl- levels in tubules Macula and ANP on a nephron.
Densa cells in distal convoluted Tubules→ ↓release of
PGE2→ ↓Juxtaglomerular cell activity in the Afferent
arteriole of glomerulus→ ↓release of Renin
Blood Pressure Regulation- Hypertension CARDIOVASCULAR PHYSIOLOGY : Note #15. 3 of 4
Figure 4. Physiologic Responses to High Blood Pressure.
V) REFRENCES
● Marieb, E. N., & Hoehn, K. N. (2012). Human Anatomy &
Physiology (9th Edition) (Marieb, Human Anatomy &
Physiology) (9th ed.). Pearson.
● Hall, J. E., & Hall, M. E. (2020). Guyton and Hall Textbook of
Medical Physiology (Guyton Physiology) (14th ed.). Elsevier.
● AMBOSS: medical knowledge platform for doctors and students.
(n.d.). Amboss. Retrieved August 9, 2021, from
https://www.amboss.com/us/
● Boron, W. F., & Boulpaep, E. L. (2016). Medical Physiology (3rd
ed.). Elsevier.
● Mohrman, D. E., & Heller, L. J. (2018). Cardiovascular
Physiology (9th ed.). McGraw-Hill Education / Medical.
● UpToDate: Evidence-based Clinical Decision Support. (n.d.).
Uptodate. Retrieved August 16, 2021, from
http://www.uptodate.com/index
4 of 4 CARDIOVASCULAR PHYSIOLOGY: Note #1. Blood Pressure Regulation- Hypertension
You might also like
- Cardiovascular System ReviewerDocument7 pagesCardiovascular System ReviewerVictoria Ellex TiomicoNo ratings yet
- 013 Cardiovascular Physiology Blood Vessel CharacteristicsDocument3 pages013 Cardiovascular Physiology Blood Vessel CharacteristicsTtNo ratings yet
- Blood Vessel (Student)Document148 pagesBlood Vessel (Student)Jerkin Razhed Postanes100% (1)
- 01 - Overview of The Cardiovascular Physiology - ACPDocument6 pages01 - Overview of The Cardiovascular Physiology - ACPMavic VillanuevaNo ratings yet
- Hematology Pathology - 002) CBC - Approach To Polycythemia (Notes)Document4 pagesHematology Pathology - 002) CBC - Approach To Polycythemia (Notes)Aro DanaNo ratings yet
- HaematologyDocument28 pagesHaematologyfh fgNo ratings yet
- CARDIAC TAMPONADE: MONITORING AND MANAGING PRESSURE ON THE HEARTDocument2 pagesCARDIAC TAMPONADE: MONITORING AND MANAGING PRESSURE ON THE HEARTkathzheinNo ratings yet
- (PED2) 3.03 Pediatric Hematology - Castro (Final V.2)Document25 pages(PED2) 3.03 Pediatric Hematology - Castro (Final V.2)Sam MataNo ratings yet
- Acls PDFDocument2 pagesAcls PDFKyrie Diosabeth TumbagaNo ratings yet
- 157 - Metabolism Physiology) Regulation of GlycolysisDocument4 pages157 - Metabolism Physiology) Regulation of Glycolysissaranya sankarNo ratings yet
- ECG - NotesDocument33 pagesECG - NotesNaveen ChandanNo ratings yet
- Understanding Arrhythmias and ECG Interpretation GuideDocument17 pagesUnderstanding Arrhythmias and ECG Interpretation GuideAngel HannahNo ratings yet
- CP RBC DisorderDocument15 pagesCP RBC DisorderDETECTIVE CONANNo ratings yet
- Glycogenolysis AtfDocument3 pagesGlycogenolysis AtfDivyaa VisvalingamNo ratings yet
- 2 - Renal PhysiologyDocument8 pages2 - Renal PhysiologyKunware TropaNo ratings yet
- Resting Membrane, Graded, Action Potentials AtfDocument4 pagesResting Membrane, Graded, Action Potentials AtfdaphneNo ratings yet
- Urinary SystemDocument9 pagesUrinary SystemCUESCANO, CRISTEL G. BSMT 2-ANo ratings yet
- CVS, Respi Heent ExamDocument8 pagesCVS, Respi Heent ExamDranreb Berylle MasangkayNo ratings yet
- BPH Thalamustudy PDFDocument5 pagesBPH Thalamustudy PDFputriNo ratings yet
- The Abdominal OrgansDocument56 pagesThe Abdominal OrgansAjeng FikihNo ratings yet
- The-Cardiovascular-System Notes MariebDocument7 pagesThe-Cardiovascular-System Notes MariebLol lolNo ratings yet
- 1 Digestive System DevelopmentDocument3 pages1 Digestive System DevelopmentDianne IgnacioNo ratings yet
- Anatomy of Thoracic WallDocument27 pagesAnatomy of Thoracic WallSamuel Pola Karta Sembiring100% (1)
- Osce PDFDocument51 pagesOsce PDFAlfonso PeñarroyaNo ratings yet
- Anatomy of BladderDocument10 pagesAnatomy of BladderKiran tyraNo ratings yet
- Mechanism of MicturitionDocument4 pagesMechanism of MicturitionGerardLum100% (2)
- MTHISTO100 Lesson 2 Excretory SystemDocument9 pagesMTHISTO100 Lesson 2 Excretory SystemJaeri HuangNo ratings yet
- 1 The Electrical Activity of The HeartDocument2 pages1 The Electrical Activity of The HeartRickertsNo ratings yet
- Femoral EmbolectomyDocument13 pagesFemoral EmbolectomyAndrea Aji SanayaNo ratings yet
- Akut AbdomenDocument24 pagesAkut AbdomenSelingkuhan neptunusNo ratings yet
- NeigeDocument26 pagesNeigeAchmad Nur AffendickNo ratings yet
- Hereditary Spherocytosis and Hereditary ElliptocytosisDocument40 pagesHereditary Spherocytosis and Hereditary ElliptocytosisJosh Matthew RosalesNo ratings yet
- MicturitionDocument29 pagesMicturitionHifza Anjum KhanNo ratings yet
- Cardiac CycleDocument35 pagesCardiac CycleEnuga Applegate100% (1)
- Histology of Kidney, Ureter and BladderDocument28 pagesHistology of Kidney, Ureter and Bladderkhairul_azhar_27No ratings yet
- 3-Major Veins of The BodyDocument26 pages3-Major Veins of The BodyTJPlayz100% (1)
- Cardiovascular System WordDocument18 pagesCardiovascular System WordLapitan Jared Anne S.No ratings yet
- Blood Vessel Characteristics AtfDocument3 pagesBlood Vessel Characteristics AtfMariaNo ratings yet
- The Vascular SystemDocument7 pagesThe Vascular SystemMiguel GumatayNo ratings yet
- Lecture 29 30Document8 pagesLecture 29 30vinnie0905No ratings yet
- Histologi KardiovaskularDocument32 pagesHistologi KardiovaskularMochammad Fariz AmsalNo ratings yet
- Ch09 - Notes - e 2Document7 pagesCh09 - Notes - e 21A22 LI SIU MAN 李兆旻100% (1)
- Cvs BdsDocument142 pagesCvs BdsDr Dhiren Kumar PandaNo ratings yet
- Biology Chapter 5Document13 pagesBiology Chapter 5Shahzaib AhmedNo ratings yet
- Histology Department Circulatory Systems SlidesDocument54 pagesHistology Department Circulatory Systems SlidesAdinda Rizki RamadhaniNo ratings yet
- Intro CVSDocument23 pagesIntro CVSumerjicNo ratings yet
- CH 11 Vessels PDFDocument10 pagesCH 11 Vessels PDFIbra TutorNo ratings yet
- Cardiovascular or Circulatory SystemDocument3 pagesCardiovascular or Circulatory SystemALEXIS MOIRAH CALIGAGANNo ratings yet
- Hhis 211 - Week 9 - Lecture - The Circulatory SystemDocument2 pagesHhis 211 - Week 9 - Lecture - The Circulatory Systemkyle LuNo ratings yet
- Circulatory System PDFDocument5 pagesCirculatory System PDFNibshian Dela RosaNo ratings yet
- 'Aliah's Cardiovascular SystemDocument45 pages'Aliah's Cardiovascular SystemLuqman Al-Bashir FauziNo ratings yet
- Cardiovascular System.Document37 pagesCardiovascular System.Wajahat FaizNo ratings yet
- Anaphy Chapter 21 Blood Vessels and Circulatory Doran Mls 1 FDocument12 pagesAnaphy Chapter 21 Blood Vessels and Circulatory Doran Mls 1 FayenaNo ratings yet
- Chap +5+Cardiovascular+SyDocument39 pagesChap +5+Cardiovascular+SySalman MasriNo ratings yet
- AP10-Cardio-Blood VesselsDocument13 pagesAP10-Cardio-Blood VesselsPay per PrintNo ratings yet
- 3 Cardiovascular PhysiologyDocument79 pages3 Cardiovascular PhysiologyJose Luna100% (2)
- Chapter 11Document4 pagesChapter 11Nona PeriarceNo ratings yet
- Sistem KV - PPT (Document121 pagesSistem KV - PPT (Bio Rizki MaulanaNo ratings yet
- Circulatory SystemDocument15 pagesCirculatory SystemaggyNo ratings yet
- 1.08 - The Cardiovascular System, The Heart & The Blood VesselsDocument9 pages1.08 - The Cardiovascular System, The Heart & The Blood Vessels13PLAN, SENTH RUEN, ANo ratings yet
- Chapter - 13 - Cardiovascular - Responses - Exercise Physiology For Health Fitness and PerformanceDocument32 pagesChapter - 13 - Cardiovascular - Responses - Exercise Physiology For Health Fitness and Performanceec16043No ratings yet
- ANP 1105 Blood VesselsDocument72 pagesANP 1105 Blood VesselsMathios TigerosNo ratings yet
- Maternal Cardiovascular and Hemodynamic Adaptations To PregnancyDocument13 pagesMaternal Cardiovascular and Hemodynamic Adaptations To PregnancyAnchalia ChandrakumaranNo ratings yet
- Arterial Waveform Analysis For The AnesthesiologistDocument11 pagesArterial Waveform Analysis For The AnesthesiologistNaser ElsuhbiNo ratings yet
- Fundamentals of Cardiology For The USMLE and General Medics PDFDocument287 pagesFundamentals of Cardiology For The USMLE and General Medics PDFMaria Patitu100% (2)
- Chap+12+CO, VRegul+Fall11 1Document17 pagesChap+12+CO, VRegul+Fall11 1Drbee100% (1)
- Hypercapnia: Neus Fabregas, Juan Fernández-CandilDocument12 pagesHypercapnia: Neus Fabregas, Juan Fernández-CandilGone WaysNo ratings yet
- 9 Anaesthetic Considerations For Laparoscopic Surgery in Neonates and Infants: A Practical ReviewDocument13 pages9 Anaesthetic Considerations For Laparoscopic Surgery in Neonates and Infants: A Practical Reviewdiomer123No ratings yet
- Untitled19 PDFDocument19 pagesUntitled19 PDFElizabeth LeonNo ratings yet
- Table Respiration RateDocument1 pageTable Respiration Ratereal_septiady_madrid3532No ratings yet
- Early Post-Operative Pulmonary Hypertension Management in The ICUDocument34 pagesEarly Post-Operative Pulmonary Hypertension Management in The ICUari wijayantiNo ratings yet
- Physiology Cardiovascular Physiology NotesDocument13 pagesPhysiology Cardiovascular Physiology Noteshedayatamin44No ratings yet
- Inhalational AnesthesiaDocument96 pagesInhalational AnesthesiaNachee PatricioNo ratings yet
- Integrated Control of The Cardiovascular SystemDocument5 pagesIntegrated Control of The Cardiovascular SystemPatricia SanchezNo ratings yet
- Full download book Neurology Neonatology Questions And Controversies Neonatology Questions Controversies Pdf pdfDocument41 pagesFull download book Neurology Neonatology Questions And Controversies Neonatology Questions Controversies Pdf pdfzelma.lansberry528100% (12)
- Fluid Status and Fluid Responsiveness PDFDocument8 pagesFluid Status and Fluid Responsiveness PDFGiselle BaiãoNo ratings yet
- 1st Year PhysiologyDocument15 pages1st Year PhysiologyMaheen AnwaarNo ratings yet
- Vascular Technology 1000 Multiple Choice QuestionsDocument196 pagesVascular Technology 1000 Multiple Choice Questionssaimum9092% (13)
- Hypertension Thesis 2Document19 pagesHypertension Thesis 2Nica MangampatNo ratings yet
- Fluid Therapy and The Microcirculation in Health and Critical IllnessDocument11 pagesFluid Therapy and The Microcirculation in Health and Critical IllnessAdote DrmNo ratings yet
- Uterine Blood Flow During Supine Rest and Exercise in Late PregnancyDocument9 pagesUterine Blood Flow During Supine Rest and Exercise in Late PregnancyMD Luthfy LubisNo ratings yet
- Cor Pulmonale ReDocument35 pagesCor Pulmonale ReFabb NelsonNo ratings yet
- Physiology of The Lateral Decubitus Position and One-Lung VentilationDocument31 pagesPhysiology of The Lateral Decubitus Position and One-Lung VentilationDebasis Sahoo100% (1)
- Hemodynamics The Study of The Movement of Blood and The Physical Principles Governing This MovementDocument46 pagesHemodynamics The Study of The Movement of Blood and The Physical Principles Governing This MovementwayneNo ratings yet
- VasoactivosDocument8 pagesVasoactivosrogelio cruzNo ratings yet
- Porth2014 Apa 2018 Disorder of Blood Pressure RegulationDocument27 pagesPorth2014 Apa 2018 Disorder of Blood Pressure RegulationMumtaz MaulanaNo ratings yet
- Surgery ManualDocument444 pagesSurgery Manualnoor hishamNo ratings yet
- Exercise Physiology Lab ReportDocument11 pagesExercise Physiology Lab Reportapi-253201402No ratings yet
- Understanding The Haemodynamics of HypertensionDocument12 pagesUnderstanding The Haemodynamics of Hypertensionrichard pucheNo ratings yet
- 5.vital Signs-1Document89 pages5.vital Signs-1Abdella UmerNo ratings yet