Professional Documents
Culture Documents
09 Muscarinic Antagonists (Notes) Atf
Uploaded by
Anuki TodriaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
09 Muscarinic Antagonists (Notes) Atf
Uploaded by
Anuki TodriaCopyright:
Available Formats
AfraTafreeh.
com
Last edited: 9/16/2022
AUTONOMIC PHARMACOLOGY | MUSCARINIC ANTAGONISTS
Autonomic Pharmacology | Muscarinic Antagonists Medical Editor: Gerard Jude Loyola
OUTLINE
I) CHOLINERGIC PHYSIOLOGY (C) QUATERNARY AMINES
(A) ACETYLCHOLINE-RELEASING III) ANTICHOLINERGIC TOXICITY
NEURONS (A) SYMPTOMS
II) TYPES OF MUSCARINIC ANTAGONISTS (B) CAUSES
(A) MUSCARINIC RECEPTORS (C) ANTIDOTE
(B) TERTIARY AMINES IV) REVIEW QUESTIONS
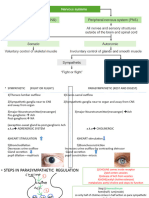
I) CHOLINERGIC PHYSIOLOGY
Table 1. Effects of acetylcholine in different organs.
(A) ACETYLCHOLINE-RELEASING NEURONS
NEURONS/ REMARKS
ORGANS
Basal ganglia Controlled by a balance of dopamine and
acetylcholine
In certain diseases, there is alteration in
the balance leading in alteration of
movement
Emetic center or Found in the medulla
the vomiting Contains a lot of muscarinic receptors
center Controls our vomiting response
Triggered by vestibular dysfunction,
stretching or irritation of particular factors
in the GI tract or higher level of
functioning
Eye Pupil: Causes pupil constriction
Ciliaris: Causes contraction of ciliaris
o Pulls the angle where the aqueous
humor → increases aqueous humor
drainage
Lens: Causes lens accommodation
Lacrimal and Stimulation causes lacrimation (↑tear
salivary glands production) and salivation (↑salivary
production)
CN VII (lacrimal gland)
CN IX (salivary gland)
Vagus nerve Heart: Works on the bundle system (SA
node, AV node) to slow down HR and CO
o To conserve energy for resting and
digesting
Smooth muscle bronchiole:
Bronchoconstriction
Liver: Increase bile release which is
involved in digestion
Stomach: Increase motility and secretions
Skin There is sympathetic neurons but they
Figure 1. Effects of cholinergic neurons in different organs.
release acetylcholine
Anticholinergic drugs act like a parasympatholytic; Involved in sweating
o Trying to inhibit the parasympathetic nervous system
Sacral nerves Supplies the lower abdomen (bladder +
(S2-S4) lower parts of the colon)
Acetylcholine-releasing neurons, muscarinic and nicotinic
Bladder: Causes contraction of the
receptors in the CNS:
detrusor muscle → urination
Lower GIT: Increases GI motility
(1) Summary of cholinergic effects:
Regulates movements Decrease HR and CO
Induce vomiting Bronchoconstricts
Constricts pupil Increase bile secretion
Increase aqueous drainage Increase GI motility and secretion
Accommodation of the lens Increase sweating
Increase lacrimation and salivation Induce urination
Autonomic Pharmacology | Muscarinic Antagonists PHARMACOLOGY: NOTE #9. 1 of 5
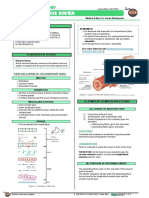
II) TYPES OF MUSCARINIC ANTAGONISTS
(A) MUSCARINIC RECEPTORS
Figure 2. Inhibitory (left) and stimulatory (right) muscarinic receptors.
Muscarinic receptors are G-protein receptors
(1) Inhibitory receptors (M2R, M4R) (2) Stimulatory receptors (M1R, M3R, M5R)
o Coupled with G-inhibitory proteins o Coupled with G-stimulatory proteins
o Primary organ is the heart o When ACh is released from the post-ganglionic
o When ACh is released from the post-ganglionic neuron, it binds to these stimulatory receptors →
neuron, it binds to M2R or M4R → ↓cAMP → ↓PK → ↑cAMP → ↑PK → ↑contraction, secretion etc.
cell hyperpolarization → ↓HR and CO o Bladder: Causes ↑contractility of the detrusor muscle
Also ↑K efflux → hyperpolarization → ↓HR and CO → ↑urination
o GIT: ↑contractility and secretions
Muscarinic antagonists block the aforementioned
reactions
(B) TERTIARY AMINES
Tertiary amines are lipophilic → easier to cross the BBB → affects the CNS
(1) Atropine
Blocks the muscarinic receptors in the pupil and ciliaris
AfraTafreeh.com
causes pupil dilation and decrease drainage in the
canal shunt
o ↓aqueous humor drainage → blurred vision, and
increase IOP
o !! Be careful to patients with narrow-angle glaucoma
Blocks muscarinic receptors in the lacrimal gland →
↓lacrimation may dry out the eyes
Blocks muscarinic receptors in the salivary gland →
↓salivation
o Indicated in:
Situations where patients drool a lot
Pre-op vs pre-intubation to clear-up upper airway
secretions
Oppose the M2R in the AV and SA node → ↑HR and
↑CO
o First-line for patients with symptomatic bradycardia
Cholinergic agonists (cholinesterase) → cholinergic
crisis
o Atropine as an antidote to cholinergic crisis
(2) Scopolamine
Blocks muscarinic receptor in the emetic center
o When there is a lot of acetylcholine in the emetic
center
o Inhibit vomiting type of process
Indicated in (1) patients with motion sickness (d/t
vestibular dysfunction) or (2) post-operative nausea
and vomiting (PONV)
2 of 5 PHARMACOLOGY: NOTE #9. Autonomic Pharmacology | Muscarinic Antagonists
AfraTafreeh.com
(3) Benztropine & Trihexyphenidyl
Recall that movement is modulated by balance of
dopamine and ACh
In states where there is a massive reduction of dopamine,
acetylcholine may be overpowering
o Can reduce tremors in Parkinson’s by inhibiting
acetylcholine
Recall that in Parkinson’s, the neurons in the
substantia nigra degenerate leading to reduction
in dopamine
o Can alleviate EPS (extrapyramidal symptoms)
caused by antipsychotics in patients who are delirious
or with psychiatric disorders
(4) Oxybutynin, Tolteradine, Solfenacin (5) Dicyclomine & Hyoscyamine
Inhibits contraction in the bladder Indicated in patients have GI spasms or diarrhea
Indicated in patients with urinary incontinence or o Benefits patients with IBS-D → ↓spasms and diarrhea
urgency (overactive bladder) o Recall that IBS has two types:
(1) IBS-C with predominant constipation,
(2) IBS-D with predominant diarrhea
(C) QUATERNARY AMINES
Figure 3. Quaternary amines.
Quaternary amines are hydrophilic → difficulty penetrating the CNS
(1) Glycopyrrolate (2) Ipratropium & Tiotropium
Indicated for patients with a lot of drooling (e.g. cerebral In the bronchioles, ACh promotes bronchoconstriction →
palsy or psychiatric disorders that causes a lot of causes difficulty in ventilation in diseases such as COPD
drooling) and asthma
o Inreased respiratory secretions can clog endotracheal These drugs inhibit bronchoconstriction → better air
tubes → cause pneumonia movement
Helpful in pre-op situation or pre-intubation to clear up Ipratropium: short-acting muscarinic antagonist (SAMA)
respiratory secretions Tiotropium: long-acting muscarinic antagonist (LAMA)
Autonomic Pharmacology | Muscarinic Antagonists PHARMACOLOGY: NOTE #9. 3 of 5
III) ANTICHOLINERGIC TOXICITY
(A) SYMPTOMS (B) CAUSES
Antimuscarinic agents
Tricyclic antidepressants
Antipsychotics
First-gen antihistamines
Belladonna plant
Either these drugs are taken two much or mixed together
can cause anticholinergic toxicity.
(C) ANTIDOTE
Physostigmine
o Cholinergic agonist
o Will do everything opposite of anticholinergic toxicity
Figure 4. Symptoms of anticholinergic toxicity.
Delirium, alterned mental status → seizures (rarely but
possible)
o Although ACh is involved in regulating movement, it
also affects cognition AfraTafreeh.com
Massive pupil dilation
Blurry vision
o Due to ciliaris not contracting and/or inability of the
lens to accommodate
o !! Contraindicated in patients with narrow-angle
glaucoma (high IOP)
Severe dry eyes and dry mouth
Tachycardia (↑↑↑HR) and hypertension (↑↑↑CO)
Bronchodilation
Little sweating
o Body cannot be cooled down through evaporative
cooling → hyperthermia (↑↑↑T)
Severe constipation
o Due to inadequate GI contraction
o !! Contraindicated in patients with small bowel
obstruction, large bowel obstruction, or ileus
Severe retention
o !! Contraindicated in patients with BPH
4 of 5 PHARMACOLOGY: NOTE #9. Autonomic Pharmacology | Muscarinic Antagonists
AfraTafreeh.com
IV) REVIEW QUESTIONS
1) Sarin is a nerve gas that is an organophosphate
cholinesterase inhibitor. Which agent could be used
as an antidote to sarin poisoning?
a. Pilocarpine
b. Carbachol
c. Atropine
d. Physostigmine.
2) A patient with asthma was prescribed a β2 agonist
for acute relief of bronchospasm, but did not respond
to treatment. Which drug is the most likely next
option for this patient?
a. Benztropine
b. Ipratropium
c. Oxybutynin
d. Physostigmine
3) A 50-year-old male who is noncompliant with
medications was recently diagnosed with COPD. His
physician would like to prescribed an inhaled
anticholinergic that is dosed once or twice daily.
Which drug is most appropriate for this patient?
a. Atropine
b. Ipratropium
c. Tiotropium
d. Trospium
4) Which is the most effective drug for motion sickness
for a person planning to go on a cruise?
a. Atropine
b. Fesoterodine
c. Scopolamine
d. Tropicamide
5) Which drug is useful in treating sinus bradycardia?
a. Atropine
b. Cisatracurium
c. Neostigmine
d. Succinylcholine
Autonomic Pharmacology | Muscarinic Antagonists PHARMACOLOGY: NOTE #9. 5 of 5
You might also like
- Freebie Bundle-50 Pages.Document76 pagesFreebie Bundle-50 Pages.Kia MercadoNo ratings yet
- YopoDocument6 pagesYopotNo ratings yet
- Comprehensive Table of Drugs: Cholinergic Agonists (Parasympathomimetics)Document31 pagesComprehensive Table of Drugs: Cholinergic Agonists (Parasympathomimetics)filchibuffNo ratings yet
- 08 Cholinergic Agonists (Notes) AtfDocument13 pages08 Cholinergic Agonists (Notes) AtfJust CrashedNo ratings yet
- EXCRETORY PHYSIOLOGYDocument6 pagesEXCRETORY PHYSIOLOGYKUMAR SUMITNo ratings yet
- 2.drugs Acting On The EyeDocument19 pages2.drugs Acting On The EyeEman MohamedNo ratings yet
- (OPHTHA) 2.05 Tearing - Rivera PDFDocument5 pages(OPHTHA) 2.05 Tearing - Rivera PDFRachel EstradaNo ratings yet
- Acid-Base Imbalances: Types, Causes, Symptoms & TreatmentsDocument4 pagesAcid-Base Imbalances: Types, Causes, Symptoms & TreatmentsHenric CasimiroNo ratings yet
- Unit 1 Gastro Intestinal SystemDocument53 pagesUnit 1 Gastro Intestinal SystemPlatypus proNo ratings yet
- Guyton GI Chapters 62, 64, 65Document36 pagesGuyton GI Chapters 62, 64, 65Samuel BordohNo ratings yet
- Hypothalamic Pituitary ConnectionDocument3 pagesHypothalamic Pituitary Connectionیوسف رمضانNo ratings yet
- The Tibial Tuberosity Is A Bony Prominence Located On The Anterior 2Document3 pagesThe Tibial Tuberosity Is A Bony Prominence Located On The Anterior 2Iqtader hoque khan AkibNo ratings yet
- Patho PneumoniaDocument2 pagesPatho Pneumoniaailyne_galicia100% (2)
- Zoology 120: Visceral Effector Receptor Effect of Sympathetic Stimulation Effect of Parasympathetic Stimulation EyeDocument2 pagesZoology 120: Visceral Effector Receptor Effect of Sympathetic Stimulation Effect of Parasympathetic Stimulation EyecarllNo ratings yet
- Drug StudyDocument4 pagesDrug StudyPauline BelbisNo ratings yet
- Pharma Super TableDocument87 pagesPharma Super TableMarton Emile DesalesNo ratings yet
- Neuromuscular Blocking DrugsDocument4 pagesNeuromuscular Blocking DrugsNix14No ratings yet
- Functional Anatomy and Physiology of Domestic Animals (PDFDrive) (1) (1) - 403-407Document5 pagesFunctional Anatomy and Physiology of Domestic Animals (PDFDrive) (1) (1) - 403-407chairunnisaNo ratings yet
- Chapter 32 NotesDocument4 pagesChapter 32 NotesMariah Jane TaladuaNo ratings yet
- 2 - Pharmacology of Drugs Acting On The Eye (Updated)Document22 pages2 - Pharmacology of Drugs Acting On The Eye (Updated)loubnarymNo ratings yet
- Pharmacology - Section 05 - Cholinergic Transmission 1 (Cholinomimetics and Antimuscarinics)Document5 pagesPharmacology - Section 05 - Cholinergic Transmission 1 (Cholinomimetics and Antimuscarinics)Pathalee ThalpavilaNo ratings yet
- NMJ PharmacologyDocument3 pagesNMJ PharmacologyRebecca MarshallNo ratings yet
- Direct Acting Muscarinic AgonistDocument6 pagesDirect Acting Muscarinic AgonistDeia ArahmanNo ratings yet
- Direct Acting Muscarinic AgonistDocument6 pagesDirect Acting Muscarinic AgonistDeia ArahmanNo ratings yet
- Direct Acting Muscarinic AgonistDocument6 pagesDirect Acting Muscarinic AgonistDeia ArahmanNo ratings yet
- Phara MacDocument7 pagesPhara Macshubhamyaduvanshi422No ratings yet
- Assessment Nursing Diagnosis Scientific Explaination Planning Implementation Rationale EvaluationDocument5 pagesAssessment Nursing Diagnosis Scientific Explaination Planning Implementation Rationale EvaluationDiana MuañaNo ratings yet
- 2010 2physDocument12 pages2010 2physlahiruwan123No ratings yet
- Drug StudyDocument14 pagesDrug Studysyd1975% (8)
- Nervous TissueDocument42 pagesNervous TissueKatherineVoNo ratings yet
- MO - Question PaperDocument13 pagesMO - Question PaperSonu SahooNo ratings yet
- Expert Opinion On Pharmacotherapy: The Role of Nitric Oxide in Penile ErectionDocument13 pagesExpert Opinion On Pharmacotherapy: The Role of Nitric Oxide in Penile ErectionwizuraihakimroyNo ratings yet
- Pcap PathoDocument2 pagesPcap PathoLardel CarayNo ratings yet
- 299.08 - Renal Pathology) Chronic Kideny Disease (CKD)Document15 pages299.08 - Renal Pathology) Chronic Kideny Disease (CKD)AnishilNo ratings yet
- Cholinergic Agents: Cholinergic Receptors Types of Receptor Muscarinic Receptor Nicotinic ReceptorDocument4 pagesCholinergic Agents: Cholinergic Receptors Types of Receptor Muscarinic Receptor Nicotinic ReceptorDonkeyManNo ratings yet
- SEO Excretion TitleDocument12 pagesSEO Excretion TitleNisha JodhanNo ratings yet
- Parasym Pathetic Nervous System Symp Atheti C Nervo Us Syste MDocument3 pagesParasym Pathetic Nervous System Symp Atheti C Nervo Us Syste MLj CruzNo ratings yet
- Adobe Scan Jan 14, 2024Document12 pagesAdobe Scan Jan 14, 2024Rian LoeyNo ratings yet
- A. General Anatomy: The Digestive SystemDocument19 pagesA. General Anatomy: The Digestive SystememeredinNo ratings yet
- OS 206 Renal PhysiologyDocument9 pagesOS 206 Renal Physiologyalphius_mendoza100% (1)
- Sistem Pencernaan Fiswanman 2020Document61 pagesSistem Pencernaan Fiswanman 2020SHABRINA LAILINo ratings yet
- Nursing Care Plan for Clear Airway GoalDocument9 pagesNursing Care Plan for Clear Airway GoalSkyerexNo ratings yet
- Hastings 2003Document13 pagesHastings 2003Miriam LópezNo ratings yet
- ANS Pharmacology Edited LastDocument84 pagesANS Pharmacology Edited LastTadela MengashaNo ratings yet
- Pathophysiology: Etiology: Salmonella, Shigella, Staphylococcus, Campylobacter Jejuni, ClostridiumDocument5 pagesPathophysiology: Etiology: Salmonella, Shigella, Staphylococcus, Campylobacter Jejuni, ClostridiumHanna La MadridNo ratings yet
- Enteric Nervous SystemDocument5 pagesEnteric Nervous Systemmehdi mafakheriNo ratings yet
- Adrenergic Agonists Classification and EffectsDocument15 pagesAdrenergic Agonists Classification and EffectsSeema YadavNo ratings yet
- Vestibular Physiology: Functions and ReflexesDocument4 pagesVestibular Physiology: Functions and ReflexesShruthi DanielNo ratings yet
- Pharma Super TableDocument56 pagesPharma Super TableMarco Paulo Reyes NaoeNo ratings yet
- Autonomic Nervous SystemDocument17 pagesAutonomic Nervous SystemKC PalattaoNo ratings yet
- Overactive Bladder - Concept-Map - Jesoro - JM - P. - 2BSN2Document2 pagesOveractive Bladder - Concept-Map - Jesoro - JM - P. - 2BSN2Jane Mae JesoroNo ratings yet
- Class: History:: Pharm-07A1 Pharm-04B6 Pharm-97A12Document3 pagesClass: History:: Pharm-07A1 Pharm-04B6 Pharm-97A12Ben PiperNo ratings yet
- The Urinary System & Fluid BalanceDocument8 pagesThe Urinary System & Fluid BalanceMarianne DugosNo ratings yet
- Directacting - Cholinergic - Agonists Faxrh3 lYVFRoQ 74189Document1 pageDirectacting - Cholinergic - Agonists Faxrh3 lYVFRoQ 74189Aya AmerNo ratings yet
- Cholinergic Drugs - TablesDocument7 pagesCholinergic Drugs - TablesThuan Tăng NguyenNo ratings yet
- Spotters Answers For Git & RenalsDocument1 pageSpotters Answers For Git & Renalsgiridurai05No ratings yet
- Whatsapp: +1 (402) 235-1397Document312 pagesWhatsapp: +1 (402) 235-1397Khushi RNo ratings yet
- Vestibular DisorderDocument22 pagesVestibular DisorderSumbal SalikNo ratings yet
- Drug StudyDocument6 pagesDrug StudyLizli LoredoNo ratings yet
- The Inner Ear: Including Otoneurology, Otosurgery, and Problems in Modern WarfareFrom EverandThe Inner Ear: Including Otoneurology, Otosurgery, and Problems in Modern WarfareNo ratings yet
- Cellular Mechanism for Calcium Transfer and HomeostasisFrom EverandCellular Mechanism for Calcium Transfer and HomeostasisGeorge Jr. NicholsRating: 5 out of 5 stars5/5 (1)
- Celecoxib Drug Study WWW RNpedia ComDocument3 pagesCelecoxib Drug Study WWW RNpedia ComAngelou MortosNo ratings yet
- Bioequivalence dossier requirementsDocument22 pagesBioequivalence dossier requirementsdeepakmaramwarNo ratings yet
- Teratogenic DrugsDocument8 pagesTeratogenic DrugsMudrekaNo ratings yet
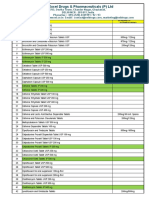
- Top selling medicines and discounts by manufacturerDocument12 pagesTop selling medicines and discounts by manufacturerfarmasi pikNo ratings yet
- ANA 2022 Poster Kaminski A Phase 3 Study Evaluating SatralizumabDocument1 pageANA 2022 Poster Kaminski A Phase 3 Study Evaluating SatralizumabMarco Antonio KoffNo ratings yet
- Vee Excel Drugs & Pharmaceuticals product catalogDocument10 pagesVee Excel Drugs & Pharmaceuticals product catalogSingh PushpanjaliNo ratings yet
- SkinTesting BeforeAntibiotic Administration Is There A Scientific BasisDocument3 pagesSkinTesting BeforeAntibiotic Administration Is There A Scientific Basiskamari mohamedNo ratings yet
- STOCK OBAT 7okt22Document5 pagesSTOCK OBAT 7okt22Klinik AlbucasisNo ratings yet
- Clindamycin Drug StudyDocument2 pagesClindamycin Drug StudyArthur Christopher CorpuzNo ratings yet
- Benzos Factsheet2011Document4 pagesBenzos Factsheet2011tech1322No ratings yet
- High Blood Pressure in Acute Ischaemic Stroke - Broadening Therapeutic HorizonsDocument7 pagesHigh Blood Pressure in Acute Ischaemic Stroke - Broadening Therapeutic HorizonsSergio Gutierrez VidalNo ratings yet
- Solution 1Document3 pagesSolution 1mabarcauNo ratings yet
- Ob2rle Sas 20Document10 pagesOb2rle Sas 20Aira Mae R. AndradaNo ratings yet
- Clinical Ocular Toxicology - FraunfelderDocument371 pagesClinical Ocular Toxicology - Fraunfelderelias misael montero ramirez100% (1)
- Catálogo de ProdutosDocument20 pagesCatálogo de ProdutosjessicayukiNo ratings yet
- Community Herbal Monograph On Achillea Millefolium L., D51Document7 pagesCommunity Herbal Monograph On Achillea Millefolium L., D51Miroslav IlicNo ratings yet
- Stock 15 FebDocument15 pagesStock 15 FebnaelarizqiNo ratings yet
- Common Drug Side Effects - Drug Interactions - Elderly - Primary Care - 2017Document8 pagesCommon Drug Side Effects - Drug Interactions - Elderly - Primary Care - 2017opulgarNo ratings yet
- Drug Study DiazepamDocument1 pageDrug Study DiazepamjolibeecaldonaNo ratings yet
- Pfizer OverviewDocument1 pagePfizer OverviewAkashNo ratings yet
- Single Dose Bioequivalence Study of Two Rivaroxaban Tablet Formulations Administered Orally After Being Crushed and SuspDocument5 pagesSingle Dose Bioequivalence Study of Two Rivaroxaban Tablet Formulations Administered Orally After Being Crushed and SuspAnonymous p8uXRS6JNo ratings yet
- CefuroximeDocument5 pagesCefuroximeRJ JOHNNo ratings yet
- Jurnal Data P4GN 2011 - Edisi 2012 - ENDocument179 pagesJurnal Data P4GN 2011 - Edisi 2012 - ENAnti NarkobaNo ratings yet
- Xanax Information-Sheet 2018-002Document2 pagesXanax Information-Sheet 2018-002Alexa HuffmanNo ratings yet
- Unit 3, Novel Drug Delivery Systems, B Pharmacy 7th Sem, Carewell PharmaDocument33 pagesUnit 3, Novel Drug Delivery Systems, B Pharmacy 7th Sem, Carewell Pharmaayush pathak100% (1)
- DrugsDocument18 pagesDrugsdantacNo ratings yet
- Tatalaksana ARV - Efek Samping - IRIS - Monitoring Terapi - PEPDocument95 pagesTatalaksana ARV - Efek Samping - IRIS - Monitoring Terapi - PEPtriiNo ratings yet
- Skills Math WorksheetDocument4 pagesSkills Math WorksheetBrennan MaguireNo ratings yet
- Advantage of FDC Atozet-Sv - EditDocument31 pagesAdvantage of FDC Atozet-Sv - EditSuardy Ciayadi100% (1)