Professional Documents
Culture Documents
299.08 - Renal Pathology) Chronic Kideny Disease (CKD)
Uploaded by
AnishilOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
299.08 - Renal Pathology) Chronic Kideny Disease (CKD)
Uploaded by
AnishilCopyright:
Available Formats
Last edited: 11/12/2021
CHRONIC KIDNEY DISEASE (CKD)
Chronic Kidney Disease (CKD) Medical Editor: Donya Moslemzadeh
OUTLINE Mesangial cells
Interglomerular
I) INTRODUCTION Extraglomerular
II) CAUSES
o part of Juxtaglomerular complex
III) PATHOPHYSIOLOGY & CLINICAL FEATUERES
IV) DIAGNOSIS Overall function of Mesangial cells is protection of
V) TREATMENT Kidneys
VI) APPENDIX o Phagocytosis and Endocytosis
VII) REVIEW QUESTIONS o Structural Support
VIII) REFERENCES o Secretion of TGF-B and other Cytokines
o Etc.
I) INTRODUCTION
Juxtaglomerular Complex
Components
(i) Juxtaglomerular cells
Modified smooth muscle cells located in the
afferent arterioles
Renin Synthesis
(ii) Macula Densa
Monitors the NaCl concentration within the lumen
of the DCT
(iii) Extraglomerular Mesangial cells
Autoregulation of Blood flow
Afferent arteriole → Brings blood in
Efferent arteriole → Drains blood
(B) BASIC KIDNEY FUNCTIONS
Waste removal
o Drugs, Urea, Creatinine, etc.
Water balance
Electrolyte Balance
Figure 1. Structure of the Renal Corpuscle and the structures
o Ca2+, Na+, K+, PO43-
associated with it [Ross & Pawlina, 2015]
Acid-Base Balance
(A) REVIEW OF THE IMPORTATN KIDNEY Hormones
STRUCTURES o Erythropoietin
Nephron
(C) DEFINITIONS
Definition
Acute Kidney Injury, AKI
o Structural and Functional unit, o Abrupt Decrease in Renal Function
o composed of Renal Corpuscle and Renal Tubule
Chronic Kidney Disease, CKD
(i) Renal Corpuscle o ↓ Renal Function ≥ 3 months
o The renal corpuscle contains the filtration apparatus o ↓↓ Glomerular Filtration Rate =GFR (< 90)
of the kidney=Glomerular filtration barrier → 3
components
i. Glomerular Endothelium
ii. Glomerular Basement Membrane, GBM
iii. Visceral layer of Bowman's capsule
o Function: Filters fluid and produce ultrafiltrate
(ii) Renal Tubule
o Segments:
Proximal Convoluted Tubule
Loop of Henle
Distal Convoluted Tubule (DCT)
Connecting Tubule and collecting duct
o Function:
resorbs and secretes substances from the
ultrafiltrate, producing urine
Chronic Kidney Disease (CKD) RENAL PATHOLOGY: NOTE #8. 1 of 15
II) CAUSES
(A) HYPERTENSION (B) DIABETES
Second most common cause Most Common Cause
= Diabetic Nephropathy
Mechanism:
Mechanism:
High BP
(i) N.E.G
Non Enzymatic Glycosylation (also called Glycation) :
Consistent High BP o Glucose in the blood
(ii) Arteriolosclerosis
o Mesangial cells = Supportive cells o Diabetic Patients
Very sensitive to low O2
o Hyaline → protein deposition
o Atherosclerotic → fat deposition
(iii) Glomerulosclerosis
o arteriolosclerosis of the Efferent arteriole
(iv) Tubular Disease
o Arteriolosclerosis of the Efferent arteriole
Kimmelstiel-Wilson nodules[Klatt, n.d.]
= Nodular glomerulosclerosis
Nodules of pink hyaline material form in regions of
glomerular capillary loops in the glomerulus. This is due
to a marked increase in mesangial matrix from damage
as a result of non-enzymatic glycosylation of proteins.
2 of 15 RENAL PATHOLOGY: NOTE #8. Chronic Kidney Disease (CKD)
(C) GLOMERULONEPHRITIS Glomerulosclerosis [AMBOSS, 2021]
A scarring of the renal glomeruli with deposition of
3 common cause
rd
extracellular matrix, which leads to impaired glomerular
Various Types filtration and proteinuria. Can occur in a segmental
pattern (e.g., in focal segmental glomerulosclerosis) or
o Secondary to autoimmune disease ,Lupus,
nodular pattern (e.g., in diabetic nephropathy).
rheumatoid arthritis
o Secondary to Infections like HIV, Hepatitis
Mechanism (D) POLYCYSTIC KIDNEY DISEASE
Antigen-Antibody complex Inherited disorder
multiple cysts in the kidneys
2 Types:
o Autosomal Dominant Polycystic Kidney Disease
(ADPKD)
Glomerular Endothelium o Autosomal Recessive Polycystic Kidney Disease
Glomerular Basement Membrane, GBM
Visceral layer of Bowman's capsule Mechanism:
• Contains Visceral Epithelial cells = o Cysts
Podocytes
↓ O2 Delivery to the tubular cells
↑ damage to GBM
↓Blood flow
(E) ACUTE KIDNEY INJURY
Prolonged AKI
Frequent AKIs over time
Prostaglandins
Mechanism of NSAIDs
o Acts on COX enzyme
Chronic Kidney Disease (CKD) RENAL PATHOLOGY: NOTE #8. 3 of 15
III) PATHOPHYSIOLOGY & CLINICAL FEATUERES
(A) ELECTROLYTE ABNORMALITIES (B) WATER IMBALANCE
Mechanism :
↓GFR
Lungs
Cardiovascular System
• Hypertension
Lower Extremities
• Peripheral Edema
Another mechanism that cause edema
o Albuminuria
• Pulmonary Edema
• Peripheral Edema
Albumin creates osmotic gradient to keep water in
(1) K+ and PO43- the vessels
Kidneys normally excrete two ions
o Potassium K+
o Phosphate PO43-
Hyperkalemia
o ↓GFR → ↓Excretion of K+→ Hyperkalemia
o Tubular damage → ↓Excretion of K+→ Hyperkalemia
Hyperphosphatemia
o ↓GFR →↓Excretion PO43- → Hyperphosphatemia
(2) Ca2+
Proximal Convoluted tubular cells Produce
Hypocalcemia
o ↓Kidney function
(3) Na+
Variable depending on the severity of CKD
Beginning → Stages Water retention → ↓sodium
Very Low GFR → Unable to Excrete Sodium
4 of 15 RENAL PATHOLOGY: NOTE #8. Chronic Kidney Disease (CKD)
(C) UREMIA (D) HORMONE IMBALANCE
Azotemia= Urea buildup without any organ damage (1) Erythropoietin
Uremia = Urea elevation with organ damage
Proximal Convoluted tubular cells
Clinical Features of Uremia
Encephalopathy
o Asterixis = Flapping Tremor
o Seizure
o Coma
o Fatigue CKD
o Nausea/vomiting o Damage of Proximal convoluted tubular cells
Uremic Pericarditis / Pericardial effusion
o Urea deposition in the pericardium
o Inflammation of the pericardium
o Normocytic and Normochromic Anemia
Uremic Frost
o Urea secreted in the sweat
Coagulopathy
o Uremia
Chronic Kidney Disease (CKD) RENAL PATHOLOGY: NOTE #8. 5 of 15
(2) Renin (3) PTH
CKD Vitamin D Synthesis:
o Renal Damage
o In skin
UV exposure
7 -Dehydrocholesterol → cholecalciferol (D3)
o liver
25-Hydroxylase
o kidney
1α-Hydroxylase
Renin-Angiotensin-Aldosterone-ADH System
Components of RAAAS
Renin
o Enzyme produced by the kidneys
Angiotensinogen
o Protein produced by the liver §circulates in the blood
Angiotensin-I Figure 2. Vitamin D Metabolism. [ Brunton et al, 2017]
o precursor molecule ↓Kidney function
Angiotensin Converting Enzyme (ACE)
o Mostly Produced by Capillary endothelial cells of the lungs
Angiotensin-II
o Extremely potent vasoconstrictive agent
Production of ANG-II ↓ Ca2+
↓Systemic BP, ↓ Blood Flow to the kidneys
If the kidney’s function was normal then PTH would
Renin converts Angiotensinogen made by the liver into increase the Calcium Reabsorption
Angiotensin-I PTH cannot increase Ca2+ by reabsorption from
Angiotensin-I circulates in the body and goes to lungs kidneys so it affects the bones → stimulate
Angiotensin-I in lungs reacts with Angiotensin Converting Osteoclasts →Bone Resorption → ↑ Ca2+
enzyme (ACE) High Bone turnover may cause various diseases:
ACE converts Angiotensin-I into Angiotensin o Renal Osteodystrophy
o Osteitis cystica fibrosa
Angiotensin-II Effects: o ↑ Risk of Fracture
Vasoconstriction
Angiotensin-II receptors on the vascular smooth muscle
Antidiuretic Hormone ADH
Angiotensin-II Stimulates Posterior Pituitary
Aldosterone
o Steroid Hormone produced by Zona Glomerulosa of the
adrenal medulla
o Angiotensin-II Stimulates Aldosterone Production from
Adrenal Cortex
o Aldosterone initiates K+ Excretion in the Urine
6 of 15 RENAL PATHOLOGY: NOTE #8. Chronic Kidney Disease (CKD)
(E) ACID-BASE IMBALANCE (F) ALBUMIN REGULATION
Mechanism : Mechanism:
↓Kidney function →↑ Albumin Excretion into the
Alpha-Intercalated cells in distal convoluted tubules Urine→↓ Albumin in the blood
and collecting duct
↓ Albumin in the blood
Kidney damage o →3rd spacing of Fluid
o → Stimulate Liver →↑ Protein production
→↑Lipoproteins →↑ TG and ↑LDL →
↓ Kidney function Hyperlipidemia
Third Spacing [UpToDate, 2021]
H+ retention+↑ HCO3- excretion
Third-spacing refers to the process of capillary leak
and extravasation of protein-rich serum into the
interstitial spaces of the soft tissues (e.g., skin, fat,
muscle), organs, deep space cavities (e.g., chest,
abdomen), or retroperitoneum.
Third-spacing into the soft tissue results in edema,
whereas fluid that leaks from the peritoneal or pleural
surfaces generates ascites or pleural effusion.
Hypoalbuminemia contributes to third-spacing; it is
theorized that the resultant intravascular oncotic
pressure, resulting from hypoalbuminemia, contributes
to the fluid shifting.
Chronic Kidney Disease (CKD) RENAL PATHOLOGY: NOTE #8. 7 of 15
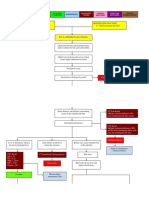
IV) DIAGNOSIS
History of (B) ALBUMINURIA
o Hypertension
o Diabetes Kidney damage marker
o Drugs Predictor of the severity of the disease
≥ 3 months Evidence of Kidney injury Urine analysis → Urine Albumin/Creatinine ratio
Table 2. Severity of the CKD based on albumin creatinine
o Markers → GFR, Albumin
ratio
(A) GFR Severity ACR (mg/g) Description
Normal GFR= 130 and 120 mL/min/1.73 m2 Normal to mildly
Mild <30
Best index of overall kidney function increased
Methods to Estimate GFR Moderate 30-299 Micro-Albuminuria
o Using Creatinine Severe ≥300 Macro-Albuminuria
o Serum cystatin C
Table 1. CKD staging based on GFR.
CKD GFR Description
Stages (mL/min/1.73 m2)
I >90 Normal or High
II 60-89 Mildly decreased
IIIa 45-59 Mildly to Moderately decreased
IIIb 30-44 Moderately to severely decreased
IV 15-29 Severely decreased
V <15 Kidney failure
Figure 3 Prognosis of CKD by GFR and Albuminuria
Category [KDIGO, 2012].
8 of 15 RENAL PATHOLOGY: NOTE #8. Chronic Kidney Disease (CKD)
(C) RENAL ULTRASOUND (E) ADDITIONAL LAB TESTS
(1) Findings: Order BMP =Basic Metabolic Panel
o BMP measures: Glucose, Calcium, Sodium,
o Cysts → Diagnosis of polycystic kidney disease
Potassium, Bicarbonate, Chloride, BUN, Creatinine
(i) Small,
(ii) atrophic, Table 3. Additional Lab Tests for the Diagnosis of CKD.
(iii) fibrotic kidneys z
LAB Test Findings
o ↓perfusion, ↓vascularity (using Doppler Ultrasound)
Calcium Hypocalcemia
Sodium Hyponatremia or Hypernatremia
BMP
Potassium Hyperkalemia
Bicarbonate Low due to acidosis
Creatinine Use to estimate GFR
Phosphate Hyperphosphatemia
RBCs
Hb
Hct
Anemia
MCV
CBC
Normocytic= Normal MCV
MCH
MCHC
(D) RENAL BIOPSY + SEROLOGY WBC
Platelets
To Determine cause and types of Glomerulonephritis
(1) Renal Biopsy Serum Iron
May have Iron deficiency
Studies
Ferritin
Iron associated anemia
(2) Serology Transferrin
TIBC
(i) Antinuclear antibodies
ANA
(screening for Lupus) Bicarbonate
ABG
PaO2 Metabolic Acidosis
(ii) Antineutrophil cytoplasmic autoantibodies SaO2
(ANCA;
for DX of Vasculitis, Goodpasture)
Lipid Panel
TG
(iii) RF (Rheumatoid factor for rheumatoid arthritis) LDL
(iv) Serology for hepatitis virus, and HIV ↑ TG and ↑LDL
HDL
Cholesterol
↑PTH
If Severe CKD and↑↑↑↑PTH →
PTH
Hypercalcemia
Chronic Kidney Disease (CKD) RENAL PATHOLOGY: NOTE #8. 9 of 15
V) TREATMENT
(A) SLOWING THE PROGRESSION OF CKD
Treat the underlying causes
Disease-Modifying Antirheumatic Drug (DMARD)
(1) HTN
Goal of Therapy: BP ≤ 130/80 A group of unrelated medications with
Treatment: immunosuppressive and anti-inflammatory properties
that improve symptoms and prevent further disease
(i) RAAAS inhibitors progression. They are commonly used to treat
rheumatoid arthritis but may also be indicated in other
o ACEI diseases (e.g., malignancies, psoriatic arthritis, systemic
o ARBs lupus erythematosus). [AMBOSS, 2021]
o Potassium sparing diuretics
Table 4. Commonly Used DMARDs. [UpToDate, 2021]
(ii) Decrease H2O Retention
Traditional Biologic Other
o Diuretics
DMARDs DMARDs DMARDs
Loop Diuretics
o Sodium Intake Restriction → Low-Sodium Diet Etanercept Tofacitinib
Adalimumab Baricitinib
Infliximab
Methotrexate Upadacitinib
(2) Diabetes Certolizumab
Sulfasalazine Golimumab
Goal of Therapy: HbA1c < 6.5% Hydroxychloroquine Anakinra
Treatment: Leflunomide Abatacept
o Insulin Cyclosporine Rituximab
o Antidiabetic drugs Azathioprine
Metformin Tocilizumab
SGLT2 inhibitors Sarilumab
o Weight loss
o Diet Modification
(4) Polycystic Kidney Disease
(3) Glomerulonephritis
Treatment :
Treatment: o Control the secondary HTN and other complications
o Treat the underlying cause (e.g., Autoimmune
May lead to Renal Transplant
diseases, Inflammatory reactions)
o Steroids
o DMARDs (5) Discontinue Nephrotoxins
NSAIDs
Nephrotoxic Agents
10 of 15 RENAL PATHOLOGY: NOTE #8. Chronic Kidney Disease (CKD)
(B) MANAGING THE COMPLICATIONS OF CKD – ELECTROLYTES
May need Renal Replacement Therapy
(2) Hyperphosphatemia
(1) Hyperkalemia
Mechanism:
Mechanism: o ↓GFR →↑PO43- retention
o ↓GFR → ↓Excretion of K+→ Hyperkalemia
Treatment:
Treatment: o Dietary Phosphate Restriction
o Insulin o Phosphate binder
o Short-Acting Beta Agonists (SABA) Sevelamer Hydrochloride
Albuterol
(3) Hypocalcemia
o HCO3-
o Diuretics
Treatment:
Loop
Thiazide o Calcium
o Cation Exchanger o Vitamin D increase the calcium absorption
Sodium polystyrene sulfonate (SPS) (4) Secondary Hyperparathyroidism
o If all failed → dialysis
Mechanism:
o If Severe CKD and ↑↑↑↑PTH → Hypercalcemia
Treatment:
o ↓ PTH production
Cinacalcet
o If Medications Fail → Parathyroidectomy
(C) MANAGING THE COMPLICATIONS OF CKD-HORMONES
(1) Anemia
Target : Hgb 8-10
(a) Mechanism:
o ↓EPO → ↓RBCs
Treatment:
o Synthetic Erythropoietin
(2) Secondary Hypertension
Goal of Therapy: BP ≤ 130/80
(a) Mechanism:
o ↓GFR
o Secondary HTN associated with elevated Renin
Treatment:
o ACEI
o ARBs
o Potassium sparing diuretics
Chronic Kidney Disease (CKD) RENAL PATHOLOGY: NOTE #8. 11 of 15
(D) MANAGING THE COMPLICATIONS OF CKD- (F) MANAGING THE COMPLICATIONS OF CKD-
WATER BALANCE ALBUMINURIA
Mechanism: Mechanism:
o ↑Albumin Excretion
o ↓GFR →↑H2O retention →↑volume overload
Manifestations:
• Pulmonary Edema
• Peripheral Edema Treatment:
• HTN o Proteinuria
ACEI (unknown mechanism)
Treatment: ARBs (unknown mechanism)
o Diuretics
Loop Diuretics Important ACEI and ARBs Side effects in CKD
Thiazide Diuretics patients
Potassium sparing diuretics o ↑ Creatinine
o Sodium Intake Restriction o Hyperkalemia
(G) MANAGING THE COMPLICATIONS OF CKD-
(E) MANAGING THE COMPLICATIONS OF CKD-
DYSLIPIDEMIA
ACIDOSIS
Mechanism: Mechanism:
o ↓ Albumin in the blood
o ↓Ability to excrete H → H retention
+ +
o ↑ HCO3- excretion
o H+ retention+↑ HCO3- excretion → Acidosis
o Acidosis → pH<7.2 → May affect
Cardiac System →↓Cardiac contractility
Electrolyte Abnormalities
Resistance to vasopressors Treatment:
Treatment: o Statins
o Sodium Bicarbonate (H) MANAGING THE COMPLICATIONS OF CKD-
PLATELET DSYFUNCTION
Mechanism:
o Uremia
Treatment:
o DDAVP = Desmopressin
Increase Platelets Activity
12 of 15 RENAL PATHOLOGY: NOTE #8. Chronic Kidney Disease (CKD)
(I) DIALYSIS
Need Dialysis if CKD worsening :
o Exacerbation of following conditions that are
refractory to medical therapies
Acidosis
Electrolyte abnormalities
Intoxication due to drug/waste accumulation
Volume Overload
Uremia
o Continuous reduction of GFR → Stage IV, V
Dialysis may be the bridge to Kidney Transplant
Different types of Dialysis :
o Peritoneal dialysis
o Hemodialysis
VI) APPENDIX
Table 5. Summary of CKD.
CKD
Decreased Kidney function for three or more months
Definition
Hypertension
Diabetes
Glomerulonephritis
Causes
Polycystic Kidney Disease
NSAID Overuse
Prolonged/ Recurrent AKI
Electrolyte Abnormalities Hyperkalemia
Hyperphosphatemia
Hypocalcemia
Water Imbalance Pulmonary Edema
o ↓H2O filtration Hypertension
o Albuminuria Peripheral Edema
Uremia Nervous System
o Encephalopathy
Asterixis
Pathophysiology & Clinical Features
Seizure
Coma
Cardiovascular System
o Uremic Pericarditis
Skin
o Uremic Frost
Platelets
o ↑ Risk of Bleeding
Hormone Imbalance Anemia
o EPO
o Renin Secondary Hypertension
o PTH
Secondary Hyperparathyroidism → CKD-related Bone Diseases
o Renal Osteodystrophy
o Osteitis cystica fibrosa
o Fractures
Acid-Base Imbalance Metabolic Acidosis
Albumin Imbalance Albuminuria → Hypoalbuminemia
o 3rd Spacing of fluids → Edema
o Hyperlipidemia
Additional Lab Tests
D
GFR
i
Chronic Kidney Disease (CKD) RENAL PATHOLOGY: NOTE #8. 13 of 15
CKD
Albumin o CBC
Ultrasound o BMP
Biopsy o ABG
Serology o Iron Studies
o Lipid Panel
o PTH
Slowing the progression of CKD HTN ACEI
ARBs
Diuretics
Low Sodium Intake
DM Insulin
Antidiabetic Drugs
Weight Loss
Diet Modification
Glomerulonephritis Steroids
DMARDs
PKD Treat Secondary HTN
Renal Transplant
Discontinue e.g., NSAIDs
Nephrotoxins
Managing the Complications Hyperkalemia
Insulin
Short-Acting Beta Agonists (SABA)
o Albuterol
HCO3-
Diuretics
o Loop
o thiazide
Cation Exchanger
Treatment
o Sodium polystyrene sulfonate (SPS)
If all failed → dialysis
Hyperphosphatemia Dietary Phosphate Restriction
Phosphate binder
o Sevelamer Hydrochloride
Hypocalcemia Calcium
Vitamin D
Secondary Cinacalcet
Hyperparathyroidism Parathyroidectomy
Anemia EPO
Volume Overload Diuretics
Low Sodium Intake
Acidosis Sodium Bicarbonate
Albuminuria ACEI
ARBs
Dyslipidemia Statins
Platelet Dysfunction DDAVP
Dialysis Exacerbation of following conditions that are refractory to medical therapies
o Acidosis
o Electrolyte abnormalities
o Intoxication due to drug/waste accumulation
o Volume Overload
o Uremia
Continuous reduction of GFR → Stage IV, V
14 of 15 RENAL PATHOLOGY: NOTE #8. Chronic Kidney Disease (CKD)
VII) REVIEW QUESTIONS
1) All the following conditions can cause CKD except:
a) Diabetes
b) Hypertension
c) Acute Kidney Injury less than 40 days
d) Polycystic kidney disease
2) The use of angiotensin-converting enzyme (ACE)
inhibitors is beneficial in patients with
a) Hypertension
b) Albuminuria
c) Hyperkalemia
d) A and B
3) The most common cause of CKD is
a) Diabetes
b) Hypertension
c) Glomerulonephritis
d) Polycystic Kidney Disease
4) A common marker of CKD is
a) Rash
b) Hematuria
c) Proteinuria
d) Bacteremia
5) Which statement is not true about the managing of
CKD complications:
a) Cation exchangers can be used to treat
Hyperkalemia.
b) Anemia in CKD patients is treated with Iron
Supplements only.
c) ARBs should Use cautiously in CKD patients with
Albuminuria.
d) Calcium and Vitamin D supplements can be used in
CKD patients with Hypocalcemia.
CHECK YOUR ANSWERS
VIII) REFERENCES
● Brunton, L., Knollman, B., & Hilal-Dandan, R. (2017). Goodman
and Gilman’s The Pharmacological Basis of Therapeutics, 13th
Edition. McGraw-Hill Education.
● AMBOSS: medical knowledge platform for doctors and students.
(n.d.). Amboss. Retrieved 2021, from https://www.amboss.com/
● UpToDate: Evidence-based Clinical Decision Support. (n.d.).
UpToDate.Com. Retrieved 2021, from
https://www.wolterskluwer.com/en/solutions/uptodate
● Ross, M. H., & Pawlina, W. (2015). Histology: A Text and Atlas:
With Correlated Cell and Molecular Biology (7th ed.). Lippincott
Williams & Wilkins.
● Klatt, E. C. (n.d.). Renal Pathology. The Internet Pathology
Laboratory for Medical Education. Retrieved November 12, 2021,
from https://webpath.med.utah.edu/RENAHTML/RENAL027.html
● Lab Tests Online. (n.d.). Patient Education on Blood, Urine, and
Other Lab Tests. Retrieved August 22, 2021, from
https://labtestsonline.org/
● Le, T., Bhushan, V., & Sochat, M. (2021). First Aid for the
USMLE Step 1 2021, Thirty First Edition (31st ed.). McGraw-Hill
Education / Medical.
● Gabriel, D. (2019). USMLE Step 2 CK: A Student-to-student
Guide (Clinical Knowledge) (10th ed.). Independently published.
● Papadakis, M., McPhee, S., & Rabow, M. (2019). CURRENT
Medical Diagnosis and Treatment 2020 (59th ed.). McGraw-Hill
Education / Medical.
Chronic Kidney Disease (CKD) RENAL PATHOLOGY: NOTE #8. 15 of 15
You might also like
- Aspects of Cell RegulationFrom EverandAspects of Cell RegulationG. H. BourneNo ratings yet
- OS 206 Renal PhysiologyDocument9 pagesOS 206 Renal Physiologyalphius_mendoza100% (1)
- Presentation I PC II RENALDocument58 pagesPresentation I PC II RENALSuhayb CumarNo ratings yet
- Endocrinology Pathology - 007) Cushing's Syndrome (Notes)Document7 pagesEndocrinology Pathology - 007) Cushing's Syndrome (Notes)hasanatiya41No ratings yet
- A Level Yr 2 Module 5: Communication, Homeostasis and EnergyDocument52 pagesA Level Yr 2 Module 5: Communication, Homeostasis and EnergyDanielNo ratings yet
- APP Level 4 Renal Review ORIGKEYDocument6 pagesAPP Level 4 Renal Review ORIGKEYnandiNo ratings yet
- Pruebas de Función RenalDocument10 pagesPruebas de Función RenalTito AboNo ratings yet
- 041 - Endocrinology Physiology) Antidiuretic Hormone (ADH)Document3 pages041 - Endocrinology Physiology) Antidiuretic Hormone (ADH)یوسف رمضان100% (1)
- Glial Cells: Astrocytes, Oligodendrocytes and Their Key FunctionsDocument7 pagesGlial Cells: Astrocytes, Oligodendrocytes and Their Key FunctionsGavin MuhammadNo ratings yet
- Clinical Chemistry 2 Liver FunctionsDocument5 pagesClinical Chemistry 2 Liver FunctionsJen NovaNo ratings yet
- EXCRETORY PHYSIOLOGYDocument6 pagesEXCRETORY PHYSIOLOGYKUMAR SUMITNo ratings yet
- 8.3 Acute Kidney Injury - March 16 - Dr. Austria.Document6 pages8.3 Acute Kidney Injury - March 16 - Dr. Austria.Jess PeltraNo ratings yet
- Excretory Products and Their Elimination Diagram+Matching BasedDocument31 pagesExcretory Products and Their Elimination Diagram+Matching Basedshivamkumarbgs724No ratings yet
- Aubf Lec 2 Trans 2Document4 pagesAubf Lec 2 Trans 2Aj MondejarNo ratings yet
- EndotelinaDocument77 pagesEndotelinaMateo MendozaNo ratings yet
- Lec15 - Renal SystemDocument3 pagesLec15 - Renal SystemGeorge Constante Valiente-SebastianNo ratings yet
- LIVERDocument3 pagesLIVERHanna MaraeNo ratings yet
- 052 - Endocrinology Physiology) Adrenal Gland OverviewDocument2 pages052 - Endocrinology Physiology) Adrenal Gland Overviewیوسف رمضانNo ratings yet
- Technique NotesDocument297 pagesTechnique NotesyangNo ratings yet
- 1 RaynerCh01Document11 pages1 RaynerCh01kayamasakuuNo ratings yet
- Renal Pathology Acute Kidney Injury AKIDocument14 pagesRenal Pathology Acute Kidney Injury AKIPranav PunjabiNo ratings yet
- Generalidades de La Rabdomiolisis: Dra. Kelly Ortiz Villarreal Residente I Medicina InternaDocument13 pagesGeneralidades de La Rabdomiolisis: Dra. Kelly Ortiz Villarreal Residente I Medicina Internadantheman123No ratings yet
- Ninja Nerd AnemiaDocument13 pagesNinja Nerd AnemiaAndra Bauer100% (3)
- Renal Physiology IDocument15 pagesRenal Physiology IJubilee Christiene Ang100% (1)
- 0320 Histology II Consitt: o Dual Blood SupplyDocument8 pages0320 Histology II Consitt: o Dual Blood SupplyYvonne ChuehNo ratings yet
- Glomerular DiseasesDocument24 pagesGlomerular DiseasesBarda GulanNo ratings yet
- Efficacy of Platelet Gel in Reconstructive Bone Surgery: M F, MD P D, MD I F, S D M D G, MD R A, MDDocument3 pagesEfficacy of Platelet Gel in Reconstructive Bone Surgery: M F, MD P D, MD I F, S D M D G, MD R A, MDAnsh Veer ChouhanNo ratings yet
- Diureticos y El RiñonDocument8 pagesDiureticos y El RiñonIrving MeraNo ratings yet
- 1 RaynerCh01Document11 pages1 RaynerCh01Bima Sena Arya YudhaNo ratings yet
- Kidney Anatomy and Function OverviewDocument13 pagesKidney Anatomy and Function OverviewHannah Grace GalinatoNo ratings yet
- 09 Muscarinic Antagonists (Notes) AtfDocument5 pages09 Muscarinic Antagonists (Notes) AtfAnuki TodriaNo ratings yet
- Lechner 2017Document8 pagesLechner 2017farisNo ratings yet
- Sure UnsureDocument20 pagesSure Unsureohemgee wowNo ratings yet
- Excretory Products and Their EliminationDocument2 pagesExcretory Products and Their Eliminationadtydv007No ratings yet
- Renal Physiology FunctionsDocument15 pagesRenal Physiology Functionskang seulgi can set me on fire with her gaze aloneNo ratings yet
- Unit Exam #1: Blood Vessels: B.) Advanced Glycation End ProductsDocument85 pagesUnit Exam #1: Blood Vessels: B.) Advanced Glycation End ProductsCherry RahimaNo ratings yet
- Urinary System Functions and AnatomyDocument4 pagesUrinary System Functions and AnatomyBrent SantosNo ratings yet
- HL Topic 11.3 KidneyDocument6 pagesHL Topic 11.3 KidneyPraveenNo ratings yet
- SEO Excretion TitleDocument12 pagesSEO Excretion TitleNisha JodhanNo ratings yet
- (PED2) 3.03 Pediatric Hematology - Castro (Final V.2)Document25 pages(PED2) 3.03 Pediatric Hematology - Castro (Final V.2)Sam MataNo ratings yet
- 1 s2.0 S0168365921001826 MainDocument11 pages1 s2.0 S0168365921001826 MainhsiyangtNo ratings yet
- 13 HemostasisDocument38 pages13 HemostasissiratelNo ratings yet
- Renal Pathology GuideDocument10 pagesRenal Pathology GuideMonique BorresNo ratings yet
- Importance of Ca in The BodyDocument30 pagesImportance of Ca in The BodyMushtaaq Bintu MaxamuudNo ratings yet
- Pathology 5.01.1 Kidney I - Dr. MesinaDocument14 pagesPathology 5.01.1 Kidney I - Dr. MesinaShaira Aquino VerzosaNo ratings yet
- Acute Kideny Injury and Chronic Renal FailureDocument55 pagesAcute Kideny Injury and Chronic Renal FailurehisslNo ratings yet
- Page of 1 3 Renal Histology & Function Renal Biology L1Document3 pagesPage of 1 3 Renal Histology & Function Renal Biology L1Fazreena EleenaNo ratings yet
- Chapter 8 Transport in Mammals - Lecture NotesDocument10 pagesChapter 8 Transport in Mammals - Lecture Notesapi-3728508100% (2)
- Rass & Paw Renal PracticeDocument20 pagesRass & Paw Renal PracticeNabeel ShahzadNo ratings yet
- Acute Kidney Injury: Mohammad RudiansyahDocument80 pagesAcute Kidney Injury: Mohammad Rudiansyahshrt gtNo ratings yet
- Special Pathology Solved KMU SEQs by RMC StudentsDocument145 pagesSpecial Pathology Solved KMU SEQs by RMC StudentsAamir Khan0% (1)
- The Pathology Associated With Diabetic RetinopathyDocument8 pagesThe Pathology Associated With Diabetic RetinopathyVivi DeviyanaNo ratings yet
- Pathophysiology - Obstructive JaundiceDocument3 pagesPathophysiology - Obstructive JaundiceAbigail Lonogan0% (1)
- Exercise 3.1 - Nuclides-1Document1 pageExercise 3.1 - Nuclides-1Rinalyn AsuncionNo ratings yet
- Kelompok Bhs Inggrtios .Id - enDocument16 pagesKelompok Bhs Inggrtios .Id - enAgustinusNo ratings yet
- NCERT Solution For Class 11 Biology Chapter 19 Excretory Products and Their EliminationDocument6 pagesNCERT Solution For Class 11 Biology Chapter 19 Excretory Products and Their EliminationHafiz HussainNo ratings yet
- MBBS - 1022 - Ysiology - TP1 (January-2024) - January-2024 (Apr-24)Document3 pagesMBBS - 1022 - Ysiology - TP1 (January-2024) - January-2024 (Apr-24)Zammam Hashim MecciNo ratings yet
- VSP-UG-7 (Kidney - Excretory System)Document50 pagesVSP-UG-7 (Kidney - Excretory System)6qhx62pr42No ratings yet
- 1 - The Urinary System and Fluid Balance - de Veyra - Silvano&tajalaDocument12 pages1 - The Urinary System and Fluid Balance - de Veyra - Silvano&tajalaMika SaldañaNo ratings yet
- The Urinary System Kidneys: Calcitriol - Active Form of Vitamin D, Circulates As A HormoneDocument10 pagesThe Urinary System Kidneys: Calcitriol - Active Form of Vitamin D, Circulates As A HormonemasorNo ratings yet
- Problem 3.12 Study Guide 1 Causes of Renal Failure 1. Discuss The Causes of Acute (Pre-Renal, Renal and Post-Renal) and Chronic Renal FailureDocument48 pagesProblem 3.12 Study Guide 1 Causes of Renal Failure 1. Discuss The Causes of Acute (Pre-Renal, Renal and Post-Renal) and Chronic Renal FailureAnishilNo ratings yet
- Normal CXRsDocument19 pagesNormal CXRsAnishilNo ratings yet
- Pacific Access CategoryDocument1 pagePacific Access CategoryAnishilNo ratings yet
- Evaluation of 2018 SQ and Pac Pre Departure Settlement Information Pilot Final Report 08-01-0Document64 pagesEvaluation of 2018 SQ and Pac Pre Departure Settlement Information Pilot Final Report 08-01-0AnishilNo ratings yet
- Normal CXRsDocument19 pagesNormal CXRsAnishilNo ratings yet
- Pac Registration Guide For Fiji and TongaDocument18 pagesPac Registration Guide For Fiji and TongaAnishilNo ratings yet
- Nihaal Sidhant Chand UU114 Report FinalDocument33 pagesNihaal Sidhant Chand UU114 Report FinalAnishilNo ratings yet
- Problem 3.12 Study Guide 1 Causes of Renal Failure 1. Discuss The Causes of Acute (Pre-Renal, Renal and Post-Renal) and Chronic Renal FailureDocument48 pagesProblem 3.12 Study Guide 1 Causes of Renal Failure 1. Discuss The Causes of Acute (Pre-Renal, Renal and Post-Renal) and Chronic Renal FailureAnishilNo ratings yet
- Eye HXDocument2 pagesEye HXAnishilNo ratings yet
- Meningitis HXDocument2 pagesMeningitis HXAnishilNo ratings yet
- Anatomi Dan Fisiologi GinjalDocument32 pagesAnatomi Dan Fisiologi GinjalAlamul Huda100% (1)
- Thyroid Diseases in Pregnancy PMK HandoutDocument12 pagesThyroid Diseases in Pregnancy PMK HandoutWikrom Keng WromKiNo ratings yet
- Lab ValuesDocument4 pagesLab ValuespninthemakinNo ratings yet
- Adrenal CortexDocument8 pagesAdrenal CortexEdward XiamNo ratings yet
- AIPMT 2013 Code W1 Question PaperDocument43 pagesAIPMT 2013 Code W1 Question PaperNageswarNo ratings yet
- Infertility TreatmentDocument9 pagesInfertility TreatmentNur Farizah ZuhaidiNo ratings yet
- Daftar Harga Distributor Per Mei 2023Document10 pagesDaftar Harga Distributor Per Mei 2023martinNo ratings yet
- Askari Lab, Gojra RD.: Reference BillDocument1 pageAskari Lab, Gojra RD.: Reference Billmeer haadiNo ratings yet
- 10 31 Concept MapDocument1 page10 31 Concept Mapapi-725271439No ratings yet
- Diabetes InsipidusDocument8 pagesDiabetes InsipidusNader Smadi100% (5)
- HypothalamusDocument38 pagesHypothalamuscmabdullahNo ratings yet
- Evaluation of Hypoglycemia: & Insulin Autoimmune Syndrome (Hirata Disease)Document15 pagesEvaluation of Hypoglycemia: & Insulin Autoimmune Syndrome (Hirata Disease)Anonymous B3J9sWNo ratings yet
- SNDT Women's University Syllabus - Bachelors in PharmacyDocument101 pagesSNDT Women's University Syllabus - Bachelors in Pharmacysunil_vaman_joshiNo ratings yet
- CC CCCCC: Y CCC CCCC CCCCC CCCC CCC CCCCCCCCCC CC CDocument3 pagesCC CCCCC: Y CCC CCCC CCCCC CCCC CCC CCCCCCCCCC CC CRachel Ann BatayolaNo ratings yet
- Royal Alexandra Hospital For Children: Policy & Procedures ManualDocument73 pagesRoyal Alexandra Hospital For Children: Policy & Procedures ManualDivya NarayanNo ratings yet
- Case ReportDocument10 pagesCase ReportFika Wilda AnggraeniNo ratings yet
- ImedclerksDocument389 pagesImedclerksWest AfricaNo ratings yet
- Cushings Ebook PDFDocument53 pagesCushings Ebook PDFvalisiano100% (1)
- NBHS1112 Biochemistry/ Biokimia May Semester 2022Document16 pagesNBHS1112 Biochemistry/ Biokimia May Semester 2022amu tha100% (1)
- Types of Progestins in Birth Control PillsDocument4 pagesTypes of Progestins in Birth Control PillsBrenda LiawNo ratings yet
- AcromegalyDocument24 pagesAcromegalycsngiuNo ratings yet
- Multiple-Choice Questions: Chapter 45 Hormones and The Endocrine SystemDocument15 pagesMultiple-Choice Questions: Chapter 45 Hormones and The Endocrine SystemshasagailNo ratings yet
- Hormonal ContraceptionDocument13 pagesHormonal ContraceptionAnuradha RoopchandNo ratings yet
- Principles of Clinical EndocrinologyDocument127 pagesPrinciples of Clinical EndocrinologyMNo ratings yet
- B.Barnes - Thyroid GlandDocument8 pagesB.Barnes - Thyroid GlandoptinNo ratings yet
- Congenital Kidney Anomalies and Cystic DiseasesDocument4 pagesCongenital Kidney Anomalies and Cystic DiseasesEMILY N CRUZ-VARGASNo ratings yet
- Pathophysiology 30 00029Document12 pagesPathophysiology 30 00029Fernando MartinezNo ratings yet
- CHAPTER 2 Science Form 4Document59 pagesCHAPTER 2 Science Form 4Lopak TikeNo ratings yet
- AP Biology Endocrine Systems-0Document14 pagesAP Biology Endocrine Systems-0Aamer AlmansourNo ratings yet
- Nilai Normal TorchDocument3 pagesNilai Normal Torchirma RDNo ratings yet