Professional Documents
Culture Documents
Endocrinology Pathology - 007) Cushing's Syndrome (Notes)
Uploaded by
hasanatiya41Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Endocrinology Pathology - 007) Cushing's Syndrome (Notes)
Uploaded by
hasanatiya41Copyright:
Available Formats
Last edited: 3/31/2023
CUSHING'S SYNDROME
Cushing's Syndrome Medical Editor: Jude Loyola
OUTLINE
I) PATHOPHYSIOLOGY III) DIAGNOSTIC APPROACH
(A) CORTISOL PATHWAY (A) SCREENING TESTS
(B) EFFECTS IN DIFFERENT ORGAN SYSTEMS (B) ACTH LEVEL
(C) EXCEPTIONS TO CUSHING’S SYNDROME (C) HIGH DOSE DEXAMETHASONE SUPPRESSION TEST
II) CUSHING’S SYNDROME & (D) CRH STIMULATION TEST
(E) IMAGING STUDIES
CUSHING’S DISEASE
(A) CUSHING’S SYNDROME IV) TREATMENT
(B) CUSHING’S DISEASE V) APPENDIX
VI) REVIEW QUESTIONS
VII) REFERENCES
I) PATHOPHYSIOLOGY
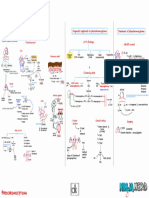
(A) CORTISOL PATHWAY (B) EFFECTS ON DIFFERENT ORGAN SYSTEMS
(1) Sympathetic Nervous System and the
Cardiovascular System
Figure 2. Effects of increased cortisol in the SNS and CVS.
Lateral gray horns innervate the viscera
↑↑cortisol
↑↑SNS stimulation → ↑↑NE release from the lateral gray
horns to the viscera
Figure 1. Cortisol pathway.
(i) Effects of SNS stimulation:
Hypothalamus produces CRH → ↑ACTH production from
the anterior pituitary (+) β-1 adrenergic receptors of the conducting system
ACTH → ↑cortisol production from the zona fasciculata and contractile muscles of the heart
(1) Cushing’s Syndrome vs Cushing’s Disease
(+) ⍺-1 receptors of the vessels → ↑↑SVR
Cushing’s Syndrome
o ↑↑cortisol from tumors or hyperplasia o Hypertension that does NOT respond to >3
Cushing’s Disease hypertension
o ↑↑ACTH from pituitary causes
Therefore,
↑↑ Cortisol upregulates both β1 and ⍺1 receptors of
the heart and vasculature → amplifies the response
Cushing's Syndrome ENDOCRINE PATHOLOGY: Note #7. 1 of 7
(2) Immune System
↑↑cortisol suppress the margination response →
neutrophils cannot stick to the vessel wall → ↑↑WBC in
the bloodstream
o Margination: neutrophils slide along the vessel wall
and squeeze through the wall (called diapedesis) to
fight off pathogens
↑↑cortisol suppress T-cell response → (-) T-cell proliferation
↑↑cortisol inhibits Ab production of plasma cells
Therefore,
↑↑Cortisol increases the risk for infection,
especially fungal infection
Figure 3. Effects of increased cortisol in the immune system.
(3) Endocrine/Metabolic
(i) Liver
(iii) Adipose Tissue (iv) Proteins
(+) proteolysis and (-) collagen
synthesis (see Figure 5)
o Break down proteins in muscles,
connective tissues, and bone
tissues to convert them to glucose
Results in:
o Muscle atrophy (especially in proximal muscles)
o Osteopenia → osteoporosis → fractures
Due to the breakdown of collagen in bones
o Thin skin = abdominal striae (Fig 8),
ecchymoses, slow wound healing
Collagen is heavy in the dermis to
provide tensile strength →
thickness, and integrity of the skin
Figure 4. Diabetogenic effect of increased
cortisol in the liver and pancreas. Figure 5. Effects of increased cortisol in the
adipose tissue and proteins.
(+) gluconeogenesis and (+) lipolysis = break down
glycogenolysis → ↑↑glucose = triglycerides in the fat tissue to free FA Fig 6. Moon facies in Cushing's syndrome.
hyperglycemia and glycerol
o Called the diabetogenic effect of (+) fat redistribution
cortisol o Cortisol only has an intracellular
o Gluconeogenesis: taking non- receptor
carbohydrates (amino acids, o Takes adipose from the extremities
glycerol, odd-chain FA) and and redistributes them to the
converting them to glucose central portion of the body →
o Glycogenolysis: break down moon facies (Figure 6), buffalo
glycogen into glucose hump (Figure 7), abdominal
obesity Fig 7. Buffalo hump in Cushing's syndrome.
(ii) Pancreas
(-) insulin production (see Figure 4)
Fig 8. Abdominal striae from Cushing's syndrome.
(4) Reproductive
↑↑cortisol → (-) GnRH production in the pituitary
Figure 9. Reproductive effects of increased cortisol.
2 of 7 ENDOCRINE PATHOLOGY: Note #7. Cushing's Syndrome
(C) EXCEPTIONS TO CUSHING’S SYNDROME
Recall the two reasons for ↑↑cortisol in Cushing’s:
o From ↑↑ACTH → Cushing’s disease
o From ↑↑cortisol production by the adrenal
regardless of ACTH → Cushing’s syndrome
(1) Acne and Hirsutism
Either of the following is ONLY seen in Cushing’s
↑↑ACTH → ↑androgens in females = acne and hirsutism Disease (d/t a pituitary tumor), NOT in Cushing’s
o Not due to ↑cortisol syndrome
o Seen likely in patients with a pituitary tumor o Acne and hirsutism due to ↑androgens
o Hyperpigmentation due to ↑MSH
Figure 10. Acne and hirsutism seen in patients with Cushing’s
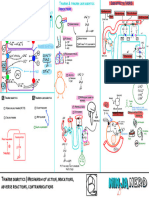
disease. Fig 11. Exceptions to signs and symptoms of Cushing's syndrome.
(2) Hyperpigmentation
↑↑ACTH → ↑melanocyte-stimulating hormone (MSH) →
(+) melanocytes in the skin → ↑melanin production →
hyperpigmentation
II) CUSHING’S SYNDROME & CUSHING’S DISEASE
(A) CUSHING’S SYNDROME (B) CUSHING’S DISEASE
Figure 12. Cushing's syndrome.
Primary Hypercortisolism Figure 13. Cushing's disease.
(1) Causes: (1) Cause:
Tumor of the adrenal gland Pituitary adenoma or small cell lung cancer →
o Adenoma or carcinoma ↑↑ACTH → acts on the adrenal cortex (zona fasciculata)
→ ↑↑cortisol
Iatrogenic
o Small cell lung CA is the most common ectopic
Chronic corticosteroid use
ACTH-producing cancer
o From autoimmune diseases such as rheumatoid arthritis
o Other ectopic locations:
o Corticosteroids > cortisol
Renal cell CA
Recall that corticosteroids act like cortisol
Pancreatic islet tumor
Eventually, the adrenal gland can atrophy →
↓cortisol production The problem is NOT on the adrenal cortex
o No negative feedback with pituitary adenoma
↑↑cortisol → negative feedback to the pituitary gland →
(-) ACTH production = ↓↓ACTH
Cushing's Syndrome ENDOCRINE PATHOLOGY: Note #7. 3 of 7
III) DIAGNOSTIC APPROACH
(A) SCREENING TESTS
Needs 2 out of 3 of the following tests to be positive = Cushing’s
It does not differentiate Cushing’s disease and Cushing’s syndrome
(1) Low Dose Dexamethasone (2) Urinary Cortisol (24-hour) (3) Late Night Salivary Cortisol
Suppression Test
Figure 15. 24-hr urinary cortisol.
Figure 14. Low-dose dexamethasone Collect urine over 24 hours → Figure 16. Late-night salivary cortisol
suppression test. test.
measure cortisol levels, whether
Giving the patient 1 mg high or low Measuring cortisol levels in the
dexamethasone should suppress (+) Cushing’s: ↑↑cortisol → runs saliva
ACTH production → (-) cortisol through the blood and is filtered (+) Cushing’s: ↑↑cortisol in the
production = ↓cortisol level by the kidneys → ↑↑cortisol in saliva
Patients with (+) pituitary or the urine
adrenal tumor (Cushing’s) will It does NOT differentiate
NOT respond to this test → Cushing’s disease and Cushing’s
↑↑cortisol after 1-mg syndrome
dexamethasone
(B) ACTH LEVEL (C) HIGH-DOSE DEXAMETHASONE SUPPRESSION
TEST
Figure 18. High-dose dexamethasone suppression test.
Determines which secondary cause of hypercortisolism:
pituitary vs ectopic
Measurement of cortisol after 8 mg of dexamethasone
(+) Pituitary tumor = can suppress ACTH → ↓↓ACTH →
Figure 17. Measurement of ACTH levels. ↓↓cortisol
(+) Ectopic site = continues to produce ACTH →
Done if there is ↑↑cortisol
↑↑ACTH → ↑↑cortisol
Can differentiate between Cushing’s disease and
Cushing’s syndrome
↑↑ACTH = Cushing’s Disease due to a pituitary or
ectopic problem
↓↓ACTH = Cushing’s Syndrome due to adrenal tumor or
iatrogenic
4 of 7 ENDOCRINE PATHOLOGY: Note #7. Cushing's Syndrome
(D) CRH STIMULATION TEST
Figure 19. CRH stimulation test.
Alternative to high-dose dexamethasone test
CRH → (+) ACTH production
(+) Pituitary tumor = hyperresponsive to CRH due to
upregulated CRH receptors → ↑↑↑ACTH → ↑↑↑cortisol
(+) Ectopic site = low to no response to CRH → ↑ACTH
→ ↑cortisol
o ACTH is not low due to its ACTH production capability
(E) IMAGING STUDIES
Pituitary CT/MRI = shows pituitary adenoma
Figure 23. Algorithm for the management of suspected
Cushing's syndrome [Jameson et al, 2018].
IV) TREATMENT
Table 1. The treatment approach to Cushing's is according to
etiology.
Figure 20. Pituitary adenoma in MRI. ETIOLOGY TREATMENT
Adrenal CT/MRI
Pituitary adenoma Transsphenoidal resection
Adrenal adenoma Ketoconazole OR adrenalectomy
Ectopic etiology Chemoradiation OR ketoconazole
Iatrogenic Taper steroid dose
*Ketoconazole can suppress cortisol production
Figure 21. Adrenal adenoma in CT scan.
CT Chest Abdomen and Pelvis = may show small cell
lung CA or renal cell CA
Figure 24. Treatment approaches to Cushing's syndrome.
Figure 22. Small cell lung CA in CT scan.
Cushing's Syndrome ENDOCRINE PATHOLOGY: Note #7. 5 of 7
V) APPENDIX
Table 2. Effects of Hypercortisolism on Different Body Systems.
PATHOPHYSIOLOGY SIGNS AND SYMPTOMS
SNS and CVS ↑↑cortisol → ↑↑activity and sensitivity of SNS: Secondary hypertension
• (+) β-1 AR → ↑↑HR and SV → ↑CO Tachycardia
• (+) ⍺-1 AR → ↑↑SVR → ↑BP
Immune ↑ ↑ cortisol → Infections, especially fungal infections
• (-) margination response of PMNs
• (-) T-cell response
• (-) Ab production of plasma cells
Endocrine/ Liver: ↑ ↑ cortisol → (+) gluconeogenesis and Hyperglycemia → increased risk of
Metabolic glycogenesis diabetes
Pancreas: ↑ ↑ cortisol → (-) insulin production Moon facies, buffalo hump, abdominal
Fat: ↑ ↑ cortisol → (+) lipolysis and (+) fat obesity
redistribution Muscle atrophy, osteopenia
Proteins: ↑ ↑ cortisol → (+) proteolysis and (-) Abdominal striae, ecchymoses, slow
collagen synthesis wound healing
Reproductive ↑↑cortisol → (-) GnRH production in the pituitary → (- ↓libido in males
) FSH and LH Amenorrhea in females
Table 3. Cushing’s Syndrome vs Cushing’s Disease
CUSHING’S SYNDROME CUSHING’S DISEASE
Causes Adrenal adenoma or carcinoma Pituitary adenoma
Chronic exogenous steroid use Small cell lung CA
Renal cell CA, pancreatic islet tumor
Cortisol levels ↑↑ ↑↑
ACTH levels ↓↓ ↑↑
Additional S/Sx (-) Acne and hirsutism
Hyperpigmentation
Table 4. Summary of Diagnostics used in Cushing’s Syndrome.
TEST RESULTS AND INTERPRETATION
Screening Tests
Low Dose Dexamethasone Measure cortisol levels after 1 mg of ↑↑cortisol = Cushing’s
Suppression Test dexamethasone
Urinary Cortisol Measure urine cortisol over 24 hours ↑↑cortisol = Cushing’s
Late Night Salivary Cortisol Measure cortisol in the saliva ↑↑cortisol = Cushing’s
Other Tests
ACTH Measurement of ACTH ↑↑ACTH = Cushing’s disease
↓↓ACTH = Cushing’s syndrome
High Dose Dexamethasone Measure cortisol levels after 8 mg of ↑↑cortisol = Pituitary tumor
Suppression Test dexamethasone ↓↓cortisol = Ectopic tumor
CRH Stimulation Test Alternative to high-dose ↑↑↑cortisol = Pituitary tumor
dexamethasone test ↑cortisol = Ectopic tumor
Measures cortisol after CRH *cortisol from pituitary tumor >>> cortisol from
administration → stimulates ACTH ectopic tumor
6 of 7 ENDOCRINE PATHOLOGY: Note #7. Cushing's Syndrome
VI) REVIEW QUESTIONS VII) REFERENCES
1) Which of the following causes Cushing’s disease? ● Loscalzo, J., Fauci, A. S., Kasper, D. L., Hauser, S. L., Longo, D. L.,
& Jameson, J. L. (2022). Harrison's Principles of Internal Medicine.
a) Exogenous steroid use McGraw Hill.
b) Adrenal adenoma
c) Renal cancer
d) Pituitary adenoma
2) Which manifestation can differentiate between
Cushing’s syndrome and Cushing’s disease in the
following patients with high cortisol?
a) Indented streaks on the abdomen
b) Hirsutism on a woman
c) Fat deposition on the central portion of the body
d) Bruising on the upper and lower extremities
3) The following are screening tests for Cushing
syndrome EXCEPT:
a) Low-dose dexamethasone test
b) High-dose dexamethasone test
c) Urinary cortisol
d) Salivary cortisol
4) What is the next step once hypercortisolism is
established?
a) Measure the patient’s ACTH
b) Order cranial and CAP CT scan
c) Give 1 mg of dexamethasone to see if ACTH can be
suppressed
d) Test whether CRH stimulates ACTH production
5) How much dexamethasone should be administered
to determine ACTH suppression in secondary
hypercortisolism?
a) 1 mg
b) 8 mg
c) 100 mcg
d) 800 mcg
6) Which of the following does NOT match their
treatment modality?
a) Pituitary adenoma: transsphenoidal resection
b) Adrenal adenoma : adrenalectomy
c) Exogenous steroids: ketoconazole administration
d) None of the above
7) What PE findings can suggest Cushing’s in a 30-
year-old man who complains of polyuria, polydipsia,
and symmetric joint pains on the elbow and hands?
a) Increased blood pressure
b) Increased fat on the sides of the face
c) Tachycardia
d) All of the above
Cushing's Syndrome ENDOCRINE PATHOLOGY: Note #7. 7 of 7
You might also like
- Unit Exam #1: Blood Vessels: B.) Advanced Glycation End ProductsDocument85 pagesUnit Exam #1: Blood Vessels: B.) Advanced Glycation End ProductsCherry RahimaNo ratings yet
- 299.08 - Renal Pathology) Chronic Kideny Disease (CKD)Document15 pages299.08 - Renal Pathology) Chronic Kideny Disease (CKD)AnishilNo ratings yet
- APP Level 4 Renal Review ORIGKEYDocument6 pagesAPP Level 4 Renal Review ORIGKEYnandiNo ratings yet
- Stent Restenosis 2Document13 pagesStent Restenosis 2Ela MihNo ratings yet
- Adrenal Gland Cortisol AtfDocument4 pagesAdrenal Gland Cortisol Atf2ymyccmvfcNo ratings yet
- MBBS - 1023 - Physiogy - TP2 (January-2024) - January-2024 (Apr-24)Document3 pagesMBBS - 1023 - Physiogy - TP2 (January-2024) - January-2024 (Apr-24)Zammam Hashim MecciNo ratings yet
- Technique NotesDocument297 pagesTechnique NotesyangNo ratings yet
- Cell, Blood and Muscle PhysiologyDocument5 pagesCell, Blood and Muscle PhysiologyMaheen AnwaarNo ratings yet
- Collins On 2007Document12 pagesCollins On 2007Davy JonesNo ratings yet
- AV UWorld EOs (Rough Draft) - Data - Subject LandscapeDocument139 pagesAV UWorld EOs (Rough Draft) - Data - Subject Landscapesaeedfadaly1No ratings yet
- Update On Colchicine, 2017: RheumatologyDocument8 pagesUpdate On Colchicine, 2017: RheumatologyAdriani HartantoNo ratings yet
- Sepsis-Syok Septik 5-12-15Document36 pagesSepsis-Syok Septik 5-12-15Titi Nur IndrawatiNo ratings yet
- Pathology Board Exam QuestionsDocument7 pagesPathology Board Exam Questionschristinejoan100% (1)
- GP Micro SEQ PDFDocument16 pagesGP Micro SEQ PDFhaddi awanNo ratings yet
- Importance of Ca in The BodyDocument30 pagesImportance of Ca in The BodyMushtaaq Bintu MaxamuudNo ratings yet
- The Cardiovascular Effects of CocaineDocument13 pagesThe Cardiovascular Effects of CocaineRoberto López Mata100% (1)
- 2012 Circadian Rhythm Disruption in Cancer BiologyDocument12 pages2012 Circadian Rhythm Disruption in Cancer BiologyArmando AldanaNo ratings yet
- ConnexinpptDocument47 pagesConnexinpptDivya DarbarNo ratings yet
- 052 - Endocrinology Physiology) Adrenal Gland OverviewDocument2 pages052 - Endocrinology Physiology) Adrenal Gland Overviewیوسف رمضانNo ratings yet
- Hematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Notes)Document8 pagesHematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Notes)hasanatiya41No ratings yet
- 5 - Adrenergic AgonistsDocument15 pages5 - Adrenergic AgonistsSeema YadavNo ratings yet
- Sepsis-Syok Septik 5-12-15Document36 pagesSepsis-Syok Septik 5-12-15Titi Nur IndrawatiNo ratings yet
- Bakteriemia, Sepsis Dan Syok Septik: DR Putra Hendra SPPD UnibaDocument33 pagesBakteriemia, Sepsis Dan Syok Septik: DR Putra Hendra SPPD UnibaTondy HarahapNo ratings yet
- Clinpath-04.-Disorders of Hemostasis and Blood CoagulationDocument11 pagesClinpath-04.-Disorders of Hemostasis and Blood CoagulationCharisse Angelica MacedaNo ratings yet
- Coronary Collateral Function Long After Drug-Eluting Stent ImplantationDocument13 pagesCoronary Collateral Function Long After Drug-Eluting Stent ImplantationJorge Peregrino BragaNo ratings yet
- Im-Crohn - S Dse Pathophysiology (Final)Document3 pagesIm-Crohn - S Dse Pathophysiology (Final)TrisNo ratings yet
- Hemostasis and Thrombosis: OutlineDocument11 pagesHemostasis and Thrombosis: OutlineManila MedNo ratings yet
- AACE Clinical Case Reports: Kyrstin L. Lane, MD, Ari Weinreb, MD, Kira Chow, MD, Jane Weinreb, MDDocument2 pagesAACE Clinical Case Reports: Kyrstin L. Lane, MD, Ari Weinreb, MD, Kira Chow, MD, Jane Weinreb, MDShuaib AhmedNo ratings yet
- Endocrinology Pathology - 008) Hyperaldosteronism (Notes)Document7 pagesEndocrinology Pathology - 008) Hyperaldosteronism (Notes)hasanatiya41No ratings yet
- 13 Antihypertensive Drugs (Notes) AtfDocument24 pages13 Antihypertensive Drugs (Notes) AtfFeven AbrahamNo ratings yet
- Special Pathology Solved KMU SEQs by RMC StudentsDocument145 pagesSpecial Pathology Solved KMU SEQs by RMC StudentsAamir Khan0% (1)
- 041 - Endocrinology Physiology) Antidiuretic Hormone (ADH)Document3 pages041 - Endocrinology Physiology) Antidiuretic Hormone (ADH)یوسف رمضان100% (1)
- Hematologic DysfuncyionDocument96 pagesHematologic DysfuncyionJason OgalescoNo ratings yet
- Hemostasis and Platelet FunctionDocument17 pagesHemostasis and Platelet FunctionUzama Binu AliNo ratings yet
- Fisiopatología Shock 1987Document14 pagesFisiopatología Shock 1987Alejo ZubietaNo ratings yet
- 1 s2.0 S0092867422004007 Main PDFDocument16 pages1 s2.0 S0092867422004007 Main PDFPrecious IJNo ratings yet
- Path IA PapersDocument9 pagesPath IA PapersPOOVIZHI SNo ratings yet
- Chapter 03 - Inflammation and Tissue RepairDocument7 pagesChapter 03 - Inflammation and Tissue RepairJo100% (2)
- 316 Week 7 CTDocument21 pages316 Week 7 CTandrea villanuevaNo ratings yet
- 5 - Adrenal Insufficiency (Notes)Document7 pages5 - Adrenal Insufficiency (Notes)Meng BekNo ratings yet
- SSLC Examination March 2023 Biology Answer Key / Hints (English Medium)Document3 pagesSSLC Examination March 2023 Biology Answer Key / Hints (English Medium)nihalnihal43849No ratings yet
- Cell Lab Report PosterDocument1 pageCell Lab Report Posterapi-633883722No ratings yet
- Where Hypertension Happens: CommentariesDocument4 pagesWhere Hypertension Happens: CommentariesIlvita MayasariNo ratings yet
- 2 AnsDocument97 pages2 AnsMahmoud AboudNo ratings yet
- Disorders of The Lymph Circulation: Their Relevance To Anaesthesia and Intensive CareDocument8 pagesDisorders of The Lymph Circulation: Their Relevance To Anaesthesia and Intensive CareKenesaNo ratings yet
- Patho Previous Year PaperDocument31 pagesPatho Previous Year PaperVishal KumarNo ratings yet
- MedCosmos Surgery - MCQ - General SurgeryDocument167 pagesMedCosmos Surgery - MCQ - General SurgeryEmmanuel DanielsNo ratings yet
- Bakteriemia, Sepsis Dan Syok SeptikDocument36 pagesBakteriemia, Sepsis Dan Syok Septikdiah stanyaNo ratings yet
- Peptic Ulcer and GERD: Chiao-Hsiung ChuangDocument58 pagesPeptic Ulcer and GERD: Chiao-Hsiung ChuangMK CameraNo ratings yet
- Sq. Epithelial CellsDocument3 pagesSq. Epithelial Cellselvie21No ratings yet
- Multiple Organ Dysfunction SyndromeDocument4 pagesMultiple Organ Dysfunction SyndromeJenny SisonNo ratings yet
- Transverse Myelitis AtfDocument3 pagesTransverse Myelitis AtfRishi VermaNo ratings yet
- Rheumatology Quiz.8Document2 pagesRheumatology Quiz.8Ali salimNo ratings yet
- Journal of Medical Case Reports: Adrenocortical Oncocytic Neoplasm Presenting With Cushing's Syndrome: A Case ReportDocument5 pagesJournal of Medical Case Reports: Adrenocortical Oncocytic Neoplasm Presenting With Cushing's Syndrome: A Case Reportlala_bojaNo ratings yet
- 347 - Hematology Physiology) Hemostasis Coagulation CascadeDocument6 pages347 - Hematology Physiology) Hemostasis Coagulation Cascadehasanatiya41No ratings yet
- Loukov 2018Document9 pagesLoukov 2018Jonathan Billy ChristianNo ratings yet
- An Overview of IsDocument10 pagesAn Overview of Ismo82No ratings yet
- Target Organs of The Thyroid AtfDocument4 pagesTarget Organs of The Thyroid AtfRidwan PermanaNo ratings yet
- Appendicitis Meningitis: Vascular Cellular Response The Inflammatory Process RepairDocument10 pagesAppendicitis Meningitis: Vascular Cellular Response The Inflammatory Process RepairYaff DthNo ratings yet
- Endocrine Physiology) 15. Adrenal Medulla - Catecholamines - KeyDocument1 pageEndocrine Physiology) 15. Adrenal Medulla - Catecholamines - Keyhasanatiya41No ratings yet
- Reumato and EndocrineDocument106 pagesReumato and Endocrinehasanatiya41No ratings yet
- Neurology LectureDocument48 pagesNeurology Lecturehasanatiya41No ratings yet
- Endocrinology Pathology - 009) Pheochromocytoma (Illustrations - Key)Document1 pageEndocrinology Pathology - 009) Pheochromocytoma (Illustrations - Key)hasanatiya41No ratings yet
- Orthopedic DisordersDocument15 pagesOrthopedic Disordershasanatiya41No ratings yet
- Hematology& Onco LectureDocument66 pagesHematology& Onco Lecturehasanatiya41No ratings yet
- CardiologyDocument43 pagesCardiologyhasanatiya41No ratings yet
- 057 - Endocrinology Physiology) OvulationDocument4 pages057 - Endocrinology Physiology) Ovulationhasanatiya41No ratings yet
- Cardiovascular Pharmacology) 09 Thiazide Diuretics - KeyDocument1 pageCardiovascular Pharmacology) 09 Thiazide Diuretics - Keyhasanatiya41No ratings yet
- 010 - Cardiovascular Physiology) Cardiovascular Cardiac CycleDocument3 pages010 - Cardiovascular Physiology) Cardiovascular Cardiac Cyclehasanatiya41No ratings yet
- Hematology Pathology - 005) Chronic Lymphocytic Leukemia (CLL) (Illustrations - Key)Document1 pageHematology Pathology - 005) Chronic Lymphocytic Leukemia (CLL) (Illustrations - Key)hasanatiya41No ratings yet
- Development & Growth Nutrition & Behavioral DisordersDocument27 pagesDevelopment & Growth Nutrition & Behavioral Disordershasanatiya41No ratings yet
- Vasculitis PPT NotesDocument14 pagesVasculitis PPT Noteshasanatiya41No ratings yet
- Hematology Pathology - 003) Acute Lymphoblastic Leukemia (ALL) (Illustrations - Key)Document1 pageHematology Pathology - 003) Acute Lymphoblastic Leukemia (ALL) (Illustrations - Key)hasanatiya41No ratings yet
- Hematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Illustrations - Key)Document1 pageHematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Illustrations - Key)hasanatiya41No ratings yet
- Hematology Pathology - 003) Acute Lymphoblastic Leukemia (ALL) (Notes)Document11 pagesHematology Pathology - 003) Acute Lymphoblastic Leukemia (ALL) (Notes)hasanatiya41No ratings yet
- Hematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Notes)Document8 pagesHematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Notes)hasanatiya41No ratings yet
- 342 - Hematology Physiology) Erythropoiesis Red Blood Cell FormationDocument6 pages342 - Hematology Physiology) Erythropoiesis Red Blood Cell Formationhasanatiya41No ratings yet
- Effect of Education On HRQoL - EQ5D CutoffDocument9 pagesEffect of Education On HRQoL - EQ5D CutoffTrang HuyenNo ratings yet
- Epidemiology and Pathophysiology of Diverticular Disease: August 2009Document7 pagesEpidemiology and Pathophysiology of Diverticular Disease: August 2009kuro hanabusaNo ratings yet
- Prevalence of Pneumonia and Factors Associated Among Children 259 Months Old in Wondo Genet District Sidama Zone SNNPR Ethiopia - PDDocument7 pagesPrevalence of Pneumonia and Factors Associated Among Children 259 Months Old in Wondo Genet District Sidama Zone SNNPR Ethiopia - PDMusainah FeisalNo ratings yet
- Clinical Neurorestorative Therapeutic Guidelines For Spinal Cord InjuryDocument5 pagesClinical Neurorestorative Therapeutic Guidelines For Spinal Cord InjuryLau FloresNo ratings yet
- "Dying To Be Thin" Outline: INFORMATIVE SPEECH Sample Outline Using TOPICAL StructureDocument4 pages"Dying To Be Thin" Outline: INFORMATIVE SPEECH Sample Outline Using TOPICAL StructureZack CruzNo ratings yet
- Comprehension Quiz12345answersDocument3 pagesComprehension Quiz12345answersLamaNo ratings yet
- Safety Practices in Outdoor RecreationDocument39 pagesSafety Practices in Outdoor RecreationJen E.No ratings yet
- Adverse Drug ReactionsDocument34 pagesAdverse Drug ReactionsYanaNo ratings yet
- Introduction - CPR PerspectiveDocument62 pagesIntroduction - CPR PerspectiveImtiaz AhmadNo ratings yet
- Drug Levothyroxine SodiumDocument2 pagesDrug Levothyroxine SodiumSrkocher0% (1)
- Tiếng Anh chuyên ngành YDocument2 pagesTiếng Anh chuyên ngành YHuynhbanghia10sinhNo ratings yet
- Multiple Sclerosis Nursing Care PlanDocument4 pagesMultiple Sclerosis Nursing Care PlanCHRISTIE MONTANONo ratings yet
- MHRS 48 Medical Examination FormDocument6 pagesMHRS 48 Medical Examination FormImroz AhmedNo ratings yet
- 2019 ALS 1 Manual V4 FinalDocument53 pages2019 ALS 1 Manual V4 FinalyusupNo ratings yet
- 34 Original - Effectiveness of Betadine Vs Normal Saline in Catheter Care For Prevention of Catheter Associated Urinary TractDocument4 pages34 Original - Effectiveness of Betadine Vs Normal Saline in Catheter Care For Prevention of Catheter Associated Urinary TractM EhabNo ratings yet
- Pro68-01 Manual Urin Micro SOP1Document19 pagesPro68-01 Manual Urin Micro SOP1mcurskmNo ratings yet
- Colostomy Care: Sital B Sharma MSC Nursing Part I Con, NBMCDocument39 pagesColostomy Care: Sital B Sharma MSC Nursing Part I Con, NBMCShetal Sharma100% (1)
- CPH-LEC Chapter 2Document18 pagesCPH-LEC Chapter 2John Vincent TacalNo ratings yet
- Healthy U-One Bank One Plan - Health Bouquet Final - 22 JulDocument35 pagesHealthy U-One Bank One Plan - Health Bouquet Final - 22 JulAyushi AgarwalNo ratings yet
- Hematology: Mohamad H Qari, MD, FRCPADocument49 pagesHematology: Mohamad H Qari, MD, FRCPASantoz ArieNo ratings yet
- Chapter 5 (Fundamentals of Cavity Preparation) Choose The Most Suitable AnswerDocument13 pagesChapter 5 (Fundamentals of Cavity Preparation) Choose The Most Suitable AnswerAbo QadeerNo ratings yet
- Monasteries Meditation Centres Sri Lanka2013 PDFDocument23 pagesMonasteries Meditation Centres Sri Lanka2013 PDFeberalejandroNo ratings yet
- Laparoscopic Liver ResectionDocument111 pagesLaparoscopic Liver ResectionTeodora-Valeria Tolan100% (1)
- Avian Influenza (AI) : Synonyms DefinitionDocument16 pagesAvian Influenza (AI) : Synonyms DefinitionDr-Hassan Saeed100% (1)
- Council 2016 AnswerDocument44 pagesCouncil 2016 AnsweralicNo ratings yet
- Classification Pathophysiology Diagnosis and ManagDocument10 pagesClassification Pathophysiology Diagnosis and ManagHeru SetiawanNo ratings yet
- Types of Sensory DisabilitiesDocument3 pagesTypes of Sensory DisabilitiesElijahNo ratings yet
- Psoriasis Soap - Psorolin Soap For Dry Skin and PsoriasisDocument2 pagesPsoriasis Soap - Psorolin Soap For Dry Skin and Psoriasisjrkresearch researchNo ratings yet
- Nursing Role and Nursing Care During Pregnancy ComplicationsDocument21 pagesNursing Role and Nursing Care During Pregnancy Complicationsvienny kayeNo ratings yet
- Emerging and Reemerging InfectionDocument1 pageEmerging and Reemerging InfectionKurt Bryan CortezNo ratings yet