Professional Documents
Culture Documents
Hematology Pathology - 003) Acute Lymphoblastic Leukemia (ALL) (Notes)
Uploaded by
hasanatiya41Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hematology Pathology - 003) Acute Lymphoblastic Leukemia (ALL) (Notes)
Uploaded by
hasanatiya41Copyright:
Available Formats
Last edited: 5/7/2023
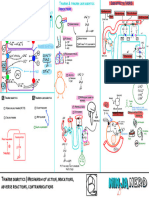
ACUTE LYMPHOBLASTIC LEUKEMIA (ALL)
Acute Lymphoblastic Leukemia (ALL) Medical Editor: Aldrich Christiandy and Jude Loyola
OUTLINE
I) PATHOPHYSIOLOGY AND II) DIAGNOSTIC APPROACH III) TREATMENT
CLINICAL FEATURES (A) CBC WITH PBS (A) SYSTEMIC CHEMOTHERAPY
(A) HEMATOPOIESIS PATHWAY (B) BONE MARROW BIOPSY (B) INTRATHECAL CHEMOTHERAPY
(B) CAUSES OF INCREASED (C) IMMUNOPHENOTYPING (C) ADVANCED THERAPIES
LYMPHOBLASTS (D) GENETIC STUDIES (D) COMPLICATIONS
(C) EFFECTS OF INCREASED LYMPHOBLASTS IN (E) TESTS FOR LEUKEMIC INFILTRATION IV) APPENDIX
BONE MARROW V) REVIEW QUESTIONS
(D) EFFECTS OF INCREASED LYMPHOCYTES IN
VI) REFERENCES
BLOOD AND TISSUES
I) PATHOPHYSIOLOGY AND CLINICAL FEATURES
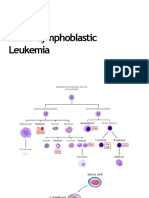
(A) HEMATOPOIESIS PATHWAY
Normal hematopoiesis pathway Pathology
Hematopoiesis is the production of blood cells In ALL, there’s a problem with B-lymphoblast and T-
o Happens in red bone marrow lymphoblast differentiation
Stem cell that generates all blood cells → o Gets stuck in the division stage and can’t differentiate
hemocytoblast (pluripotent stem cell) to become functional T cells and B cells
Continue replicating and dividing without dying
1) Myeloid stem cell o So we end up with
In the presence of Decreased functional T cells and functional B cells
o Erythropoietin → red blood cell Tons of T lymphoblasts and B lymphoblasts
o Thrombopoietin (TPO) → platelet
o Colony-stimulating factor (CSF) → myeloblast
And then myeloblast, in the presence of other colony-
stimulating factors and interleukins, will become
granulocytes
o Neutrophil
o Eosinophil
o Basophil
2) Lymphoid stem cell
→ Lymphoblast
o B-lymphoblast → B-cells (B-lymphocyte)
Go to lymph nodes
o T-lymphoblast → T-cell (T-lymphocyte)
Differentiate in the thymus
Go to lymph nodes
Acute Lymphoblastic Leukemia (ALL) Hematology Pathology: Note #3. . 1 of 11
(B) CAUSES OF INCREASED LYMPHOBLASTS
(1) Chemoradiation (2) Genetic
Causes DNA mutation (i) Down syndrome (trisomy 21)
o Gene has gained the capacity to continue to
replicate without the cell dying Associated with AML and ALL
Causes tons of DNA replication without the cell dying (ii) Translocation
o End up with a massive amount of T lymphoblast and
B lymphoblast 1) t(12;21)
o Without completely becoming differentiated, T cell We have chromosomes 12 and 21
and B cell And we swap some of the genetic material
o Form weird fusion gene → gains the capacity to
(3) Infection
continue to keep replicating and dividing without
Human T-lymphotropic virus (HTLV) dying
o Associated with T-cell ALL Common in children
So, we have 2 types of ALL o So, this translocation is more common
o T lymphoblast (20%) 2) t(9;22)
Remember HTLV as the cause
o B lymphoblast (80%) We have chromosomes 9 and 22
We swap some of the genetic material
o We get the Philadelphia chromosome
Fusion gene → BCR-ABL gene
Common in adults
o Less common
o But it’s important to be able to determine this
Due to different treatment regiment
Remember, these fusion genes gain the capacity to
continue to allow for excessive amounts of DNA
replication without the cell dying
2 of 11 Hematology Pathology: Note #3. Acute Lymphoblastic Leukemia (ALL)
(C) EFFECTS OF INCREASED LYMPHOBLASTS IN BONE MARROW
T lymphoblasts and B lymphoblasts are populated within bone marrow due to
o Chemoradiation causing mutations
o Genetic abnormalities associated with
Trisomy 21 (Down syndrome)
Translocations
• Cause weird fusion genes that cause excessive DNA replication
• Evade apoptosis and become immortal
o Human T-cell lymphotropic virus
Epidemiology
o B cell ALL (80%) VS T cell ALL (20%)
Lymphoblasts populate in the bone marrow and cause a lot of problems
o Taking so much space in the bone marrow
o Taking all the nutrients that are needed for red blood cell and platelet production
So, these cell lines become affected, and their production is dropped due to
o Decreased space
o Decreased nutrients available for them to continue to undergo their production process
(1) Increased lymphoblast → decreased functional (3) Thrombocytopenia (low platelet)
white blood cells We could see this on CBC showing low levels of platelet
Platelets are supposed to clog up holes in blood
Aren’t able to perform normal functions below
vessels if they’re broken or ripped up
o Fight off pathogens
o If we can’t do this, we’ll bleed through those holes
→ release cytokines
Develop little bruising on the skin → Petechiae
→ promote an inflammatory reaction
Bigger one → purpura
→ fight off infection
Even bigger one → ecchymosis
High risk of infections o Or bleeding
o One of the higher mortality causes Nose bleeding
o They may present with Gingival bleeding
Pneumonia GI bleeding
Urinary tract infection (UTI)
Look for features of
Cellulitis
Bruising
(2) Anemia (low red blood cell) o Petechiae (Diameter ≤ 3mm)
o Purpura (Diameter 3-10mm)
Dropping the amount of red blood cells causes
o Ecchymosis (Diameter > 10mm)
anemia
Anemia would be evident if we got CBC and showed low Bleeding
numbers of red blood cell o Epistaxis
Clinical features o Gingival bleeding
o GI bleeding
1) Pallor
o Decreased hue of the skin (4) Bone pain
o If red blood cell is oxygenated properly and has
Increased lymphoblast → compensate and expand to
enough of them
make space for these lymphoblasts
They should give a pinky-reddish hue to the skin
Distension and activation of pain receptors and
2) Fatigue, dyspnea nerves → Bone pain
o Remember, red blood cells are supposed to supply o May present with limping
O2 to tissues o Or complaining of particular bone pain in the areas
o To help us to be able to perform normal functions where red bone marrow is present
(producing energy)
Acute Lymphoblastic Leukemia (ALL) Hematology Pathology: Note #3. . 3 of 11
(D) EFFECTS OF INCREASED LYMPHOCYTES IN BLOOD AND TISSUES
We know that B lymphoblasts and T lymphoblasts are made particularly within the bone marrow
They should get pushed into the bloodstream → supposed to go to some organs
(1) Liver and spleen → hepatosplenomegaly (3) Meninges → meningeal leukemia
Deposit lymphoblasts cause hepatosplenomegaly Unique and important to differentiate between AML
The liver and spleen are getting bigger and ALL
o Taking up a lot of spaces within the GI tract → o Deposit into meninges → meningeal leukemia
Compress stomach and bowels Present with features of meningitis
Food is supposed to go through without any o Headache
compression or restriction o Photophobia
o Now we have things compressing GI organs like o Phonophobia
the stomach and bowels o Nausea/vomiting
Not going to be able to push food along easily o Focal neural deficits
These will cause o Altered mental status
• Nausea/vomiting
• Abdominal fullness The cranial nerve that moves through and around the
area of the meninges, especially CN VI
(2) Lymph nodes → lymphadenopathy o Lots of deposition into meninges and
compressing cranial nerve → cranial nerve palsy
B cells and T cells naturally go into lymph nodes Specifically, CN VI → CN VI palsy
Deposit lots of them cause lymphadenopathy o If CN VI isn’t able to work
o May see in any lymphocyte-predominant leukemia Can’t abduct the eye
o May see this within the cervical region or other areas Related to extraocular movement
of the body
Generally, it’s a large, non-painful (non-tender) type of
swollen lymph node
4 of 11 Hematology Pathology: Note #3. Acute Lymphoblastic Leukemia (ALL)
QUICK RECAP
Depositing into the liver and spleen causes big swelling
Lymphadenopathy
o Large, non-painful, non-tender type of swollen lymph node
Meningeal leukemia presents with
o Meningitis
o Cranial nerve palsy, specifically CN VI palsy
Inability to abduct the eye
(1) Testicular enlargement (3) Leukostasis
Not as common as meningeal leukemia Way more common in AML than in ALL
o But this is something to think about Tons of blast cells stuck within the bloodstream
o Occlude the blood flow
AML vs. ALL
o Block the circulation to brain tissues, causing
Biggest features to differentiate from AML Stroke
o Lymphadenopathy Headache
o Meningeal leukemia o Blockage of pulmonary vessels causing
o Testicular enlargement Hypoxemia
Dyspnea
We can rarely see splenomegaly in AML
o But not that common o Block the retina vessel
o Hepatosplenomegaly is more commonly seen in Vision change or vision loss
ALL than in AML o Block off the drainage vein of the penis
Priapism
(4) Tumor lysis syndrome
(2) Thymus (T-cell ALL only) → thymic enlargement
High tumor burden (massive amount of
Only see this in T-cell ALL lymphoblasts)
Thymus sits on the top of the heart o Present and stuck in capillaries and popping open
o T lymphoblasts deposit in the thymus o Getting chemotherapy and busting the cell open
o Thymus will get larger → Thymic enlargement Releasing K+, PO43- , uric acid
Compressing these structures o May get acute kidney injury associated with this
1) Trachea and bronchi → Dyspnea and stridor May see this in AML and ALL
2) Esophagus → dysphagia
3) Superior vena cava → SVC syndrome
o We have subclavian and internal jugular veins
draining into the brachiocephalic vein, → drains into
the superior vena cava
o Symptoms
Very large neck vein
Enlargement of veins with blue discoloration
• Chest
• Face
• Arms
Acute Lymphoblastic Leukemia (ALL) Hematology Pathology: Note #3. . 5 of 11
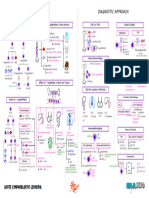
II) DIAGNOSTIC APPROACH
(A) CBC WITH PBS (B) BONE MARROW BIOPSY
Figure 4. Bone marrow biopsy reveals hypercellular bone
Figure 1. CBC shows anemia, thrombocytopenia, and marrow with >20% lymphoblasts.
increased lymphoblasts.
Definitive diagnostic test
General screening test Take a chunk of the bone marrow which then shows
o Tell us the effect of crowding of lymphoblast on the hypercellular BM with >20% lymphoblasts
bone marrow o Highly diagnostic of ALL
(1) Effect of Lymphoblast Crowding on CBC:
↓↓CBC = anemia
↓↓platelets = thrombocytopenia
↑↓mature WBCs
o Very variable; sometimes you have leukopenia or
leukocytosis
↑↑lymphoblasts
o On PBS, there is evidence of ↑↑lymphoblasts
o In AML, there is ↑↑myeloblast with Auer rods
Figure 5. Lymphoblasts on bone marrow biopsy.
Figure 2. PBS shows lymphoblasts indicating acute
lymphoblastic leukemia.
Figure 3. PBS showing myeloblasts with their characteristic
Auer rods (Raj & Mehta, 2022).
6 of 11 Hematology Pathology: Note #3. Acute Lymphoblastic Leukemia (ALL)
(C) IMMUNOPHENOTYPING (D) GENETIC STUDIES
To determine the specific chromosomal abnormality in
ALL because it affects the management
(1) Cytogenetics
Figure 7. Cytogenetics shows different chromosomal
Figure 6. Flow cytometry and immunohistochemistry can abnormalities in ALL.
determine which ALL subtype is present. Taking the nuclear material and then checking for any
To determine the subtype of ALL chromosomal abnormality
Is there a specific type of molecule present in lymphoblast (12:21)t
that is not seen in myeloid stem cells? o Associated with children
o More common
(1) Immunohistochemistry
(9:22)t or the Philadelphia chromosome
Checks for specific proteins inside the lymphoblasts o Associated with adults
Lymphoblasts = Tdt (+) and MPO (-) o Less common
o MPO (myeloperoxidase) is only seen in myeloblasts o Involves a very specific treatment process !!
(2) Flow Cytometry (2) PCR
What kinds of CD proteins are present on the surface of
the cells?
Checks for specific proteins outside the lymphoblasts =
CD proteins
o The type of CD determines whether it is a B-cell or a
T-cell
Running these cells through a column and putting Abs
that bind to these proteins, and lighting them up
More beneficial in ALL than AML
(i) T-lymphoblast (T-ALL)
Highly suggestive if there is CD2-CD8 Figure 8. PCR reveals the BCR-ABL fusion gene, which may
o Most important is CD3 indicate a different treatment regimen for ALL.
(9:22)t → there is a specific fusion gene present called
(ii) B-lymphoblast (B-ALL) BCR-ABL
Highly suggestive if there is CD10, CD19 or CD20 (+) BCR-ABL → treated with tyrosine kinase inhibitors
(TKI)
o BCR-ABL gene hyperactivates tyrosine kinases →
Low numbers indicate T-ALL, ↑↑stimulation and replication
high numbers indicate B-ALL
Acute Lymphoblastic Leukemia (ALL) Hematology Pathology: Note #3. . 7 of 11
(E) TESTS FOR LEUKEMIC INFILTRATION
Figure 9. Different diagnostic modalities for leukocytic infiltration.
Check for leukemic infiltration in the organs
Table 1. Tests or imaging to check for organ involvement in ALL.
Check for features of
meningitis →
CT/MRI
enhancement of
CNS
meninges
Lumbar puncture ↑↑lymphoblasts in CSF
Check for testicular
infiltration of
Testicles Testicular UTS
lymphoblasts resulting
in a testicular mass
(+) thymic enlargement
Thymus Chest Xray or CT → mediastinal widening
and mass effect
Liver
Ultrasound or CT
and/or Hepatosplenomegaly
of the abdomen
Spleen Figure 12. Thymoma from ALL in coronal CT scan.
Figure 10. Cranial MRI showing enhancement of meninges
indicating meningeal leukemia.
Figure 13. Hepatomegaly as seen in abdominal CT scan.
Figure 11. Testicular involvement in ALL as shown in testicular
ultrasound.
8 of 11 Hematology Pathology: Note #3. Acute Lymphoblastic Leukemia (ALL)
III) TREATMENT
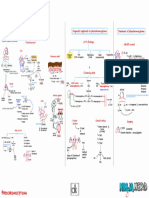
(A) SYSTEMIC CHEMOTHERAPY (C) ADVANCED THERAPIES
Figure 14. Chemotherapeutic regimen for ALL.
Same with AML to start with combination systemic Figure 16. Advanced ALL therapies use TKI or BM transplant.
chemotherapy (1) TKIs
Induction → consolidation → maintenance
o The goal is to reach complete remission Tyrosine kinase inhibitors: imatinib
o Most common agent
Agents: CVADD
o Cyclophosphamide (+) (9:22)t
o Vincristine (+) BCR-ABL gene
o Asparaginase (+/-) (2) Bone Marrow Transplant
o Daunorubicin
o Dexamethasone If patients fail chemotherapy, TKIs, or if there is a poor
prognostic
(B) INTRATHECAL CHEMOTHERAPY (D) COMPLICATIONS
(1) Tumor Lysis Syndrome (TLS)
Figure 17. Tumor lysis syndrome is the most common
Figure 15. Intrathecal chemotherapy for ALL. complication of ALL.
Prophylactic for meningeal leukemia During chemotherapy, leukemic cells pop out and release
o Chemotherapy ↑↑PO4, ↑↑K+, and ↑↑uric acid → causes AKI
o Radiation (+/-)
(i) Treatment
(1) Chemotherapy
IV fluids
Agents: Allopurinol
o Methotrexate (MTX)* o Prevents conversion of purines to uric acid
May be asked in exams
o Cytarabine Rasburicase
o Steroids o Converts uric acid to its non-toxic metabolite
It may be delivered intrathecally: through a lumbar drain
or through the EVD
(2) Radiation (+/-)
Cranial irradiation therapy
Acute Lymphoblastic Leukemia (ALL) Hematology Pathology: Note #3. . 9 of 11
IV) APPENDIX
Liver
V) REVIEW QUESTIONS 7) Which indicates T-ALL in flow cytometry?
a) Tdt (+)
1) Both B-lymphoblasts and T-lymphoblasts migrate b) MPO (-)
into the thymus for differentiation c) CD10 (+)
a) True d) CD3 (+)
b) False
8) What gene translocation is the Philadelphia
2) Which are the etiologies of the increased chromosome? What fusion gene is the result of this
lymphoblasts? (May choose more than 1) translocation?
a) Chromosome 12 and 22 translocation
b) Chemoradiation 9) What agent is used in intrathecal chemotherapy of
c) Cytomegalovirus infection ALL?
d) Down syndrome a) Methotrexate
e) Klinefelter syndrome b) Vincristine
f) Human T-lymphotropic virus infection c) Cyclophosphamide
g) Steven-Johnson syndrome d) All of the above
3) Acute lymphoblastic leukemia can cause anemia and 10) What is the specific therapy for patients who are
thrombocytopenia due to decreased bone marrow positive for the Philadelphia chromosome?
size and decreased nutrients for production a) Methotrexate
a) True b) Imatinib
b) False c) Pembrolizumab
d) Vincristine
4) Superior vena cava syndrome can be found in both
acute lymphoblastic leukemia and acute myeloid 11) What is the most common complication of ALL?
leukemia patients
a) True VI) REFERENCES
b) False
5) The following can be seen in the CBC of patients
● Harrison, T. R., & Kasper, D. L. (2015). Harrison's Principles of
Internal Medicine. McGraw-Hill Medical Publ. Division.
with ALL EXCEPT?
a) Increased lymphoblasts
● Raj, K., & Mehta, P. (2022, March 4). Acute myeloid leukemia.
Retrieved from BMJ Best Practice:
b) Decreased RBC https://bestpractice.bmj.com/topics/en-us/274
c) Increased platelets
d) Increased leukocytes
6) What is the definitive diagnostic test for ALL?
a) PBS
b) Bone marrow biopsy
c) CT scan
d) Flow cytometry
10 of 11 Hematology Pathology: Note #3. Acute Lymphoblastic Leukemia (ALL)
Acute Lymphoblastic Leukemia (ALL) Hematology Pathology: Note #3. . 11 of 11
You might also like
- Hematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Notes)Document8 pagesHematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Notes)hasanatiya41No ratings yet
- Acute Leukemia HandoutDocument10 pagesAcute Leukemia Handoutnonie jacobNo ratings yet
- AML, CML, ALL, CLL, HemophiliaDocument7 pagesAML, CML, ALL, CLL, HemophiliaJamara Kyla Dela CruzNo ratings yet
- 1 Acute LeukemiaDocument14 pages1 Acute Leukemiaسمير هزاعNo ratings yet
- Acute Lymphoblastic Leukemia - LecturioDocument17 pagesAcute Lymphoblastic Leukemia - LecturioCornel PopaNo ratings yet
- Acute Lymphoblastic LeukemiaDocument27 pagesAcute Lymphoblastic LeukemiaMahalakshmi PalanisamiNo ratings yet
- Chapter 13 Neoplastic Proliferations of White CellsDocument16 pagesChapter 13 Neoplastic Proliferations of White CellsOmar100% (1)
- Tutorial: Section A: Multiple Choice Question (Mcqs T/F)Document7 pagesTutorial: Section A: Multiple Choice Question (Mcqs T/F)Harith AsriNo ratings yet
- Hoffbrands Haematology Online MCQSDocument29 pagesHoffbrands Haematology Online MCQSATHUMANI JUMBENo ratings yet
- Anemia Lectures From Doll Very Well Covered in Pathoma Coberly Plasma Cell DyscrasiasDocument19 pagesAnemia Lectures From Doll Very Well Covered in Pathoma Coberly Plasma Cell DyscrasiasTeehee JonesNo ratings yet
- Unit 4 Study Guide PathoDocument10 pagesUnit 4 Study Guide Pathoangieswenson100% (1)
- Leukemia Myeloproliferation, Myelodysplasia: Lita Septina Peyakit Dalam FK UMSUDocument47 pagesLeukemia Myeloproliferation, Myelodysplasia: Lita Septina Peyakit Dalam FK UMSUJr SparkNo ratings yet
- Acute Lymphoblastic LeukemiaDocument5 pagesAcute Lymphoblastic LeukemiavnykumalasariNo ratings yet
- (Romanian Journal of Internal Medicine) Acute Lymphocytic Leukemia in Adults. Pathologic Features and PrognosisDocument6 pages(Romanian Journal of Internal Medicine) Acute Lymphocytic Leukemia in Adults. Pathologic Features and PrognosisPepeeNo ratings yet
- Molecular Basis of Acute LeukemiaDocument31 pagesMolecular Basis of Acute LeukemiaVivek SharmaNo ratings yet
- CancerDocument20 pagesCancerManisha DasNo ratings yet
- How I Treat Essential ThrombocythemiaDocument12 pagesHow I Treat Essential ThrombocythemiaJicko Street HooligansNo ratings yet
- IT 9 - Hematology Malignancy - NDDocument93 pagesIT 9 - Hematology Malignancy - NDDesi MawarniNo ratings yet
- El Husseinys Essentials of Hematology OncologyDocument114 pagesEl Husseinys Essentials of Hematology Oncologymedokidz7No ratings yet
- Hematology QuestionsDocument13 pagesHematology QuestionsGlazel TulaganNo ratings yet
- Managing The Client With Leukemia: Module DescriptionDocument10 pagesManaging The Client With Leukemia: Module DescriptionMelodia Turqueza GandezaNo ratings yet
- Managing The Client With Leukemia: Module DescriptionDocument10 pagesManaging The Client With Leukemia: Module DescriptionMelodia Turqueza GandezaNo ratings yet
- Leukocytic Disorders QuizDocument3 pagesLeukocytic Disorders QuizJana LacuestaNo ratings yet
- Leukemia: Dr. Suhaemi, SPPD, FinasimDocument96 pagesLeukemia: Dr. Suhaemi, SPPD, Finasimwie_wie_wieNo ratings yet
- Basic Concepts of Hematology MalignanciesDocument5 pagesBasic Concepts of Hematology MalignanciesViolet MillerNo ratings yet
- Acute Lymphoblastic LeukaemiaDocument9 pagesAcute Lymphoblastic LeukaemiaAdams ZarawuNo ratings yet
- Acute Lymphoblastic LeukaemiaDocument19 pagesAcute Lymphoblastic LeukaemiaRo RyNo ratings yet
- Non-Hodgkin'S Lymphoma: Oliveros Francis!!!!!!!!!!!!!!!!!Document48 pagesNon-Hodgkin'S Lymphoma: Oliveros Francis!!!!!!!!!!!!!!!!!francis00090No ratings yet
- White Blood Cell Disorders: Neoplastic Diseases of The BloodDocument81 pagesWhite Blood Cell Disorders: Neoplastic Diseases of The BloodMiguel Cuevas Dolot100% (1)
- Answers - Haematological Malignancies Digital Images QuizDocument4 pagesAnswers - Haematological Malignancies Digital Images Quizcande casanasNo ratings yet
- Hematology - PathophysiologyDocument28 pagesHematology - Pathophysiologyjmosser100% (2)
- Limfoma Maligna FinalDocument50 pagesLimfoma Maligna FinalAulia Ayu PuspitaNo ratings yet
- Survey and Summary How Does DNA Break During Chromosomal Translocations?Document13 pagesSurvey and Summary How Does DNA Break During Chromosomal Translocations?Daniel ALNo ratings yet
- Acute Monocytic Leukemia and Acute Lmphocytic Leukemia: OccurrenceDocument12 pagesAcute Monocytic Leukemia and Acute Lmphocytic Leukemia: OccurrenceAngelo Jude CobachaNo ratings yet
- Laboratory Evaluation of ThrombophiliaDocument7 pagesLaboratory Evaluation of ThrombophiliaAmine CHAHIDNo ratings yet
- HS202 Pathology ExamDocument6 pagesHS202 Pathology ExamJulio dR AltavasNo ratings yet
- T5-Haematological MalignanciesDocument27 pagesT5-Haematological Malignanciesdanielnsy28No ratings yet
- Case 2 (Mantle Cell Lymphoma)Document3 pagesCase 2 (Mantle Cell Lymphoma)gaber 230No ratings yet
- 20 Lymphoid and Plasma Cell NeoplasmsDocument12 pages20 Lymphoid and Plasma Cell NeoplasmsDaphne Hernaez100% (1)
- Quiz Hematology Oncology Part 2 of 2Document60 pagesQuiz Hematology Oncology Part 2 of 2MedShare100% (5)
- LNs HNDocument190 pagesLNs HNNinna Isabel VictorioNo ratings yet
- Hematology 1 LeukemiaDocument140 pagesHematology 1 LeukemiamaryantoinetteriveraNo ratings yet
- LeukemiaDocument91 pagesLeukemiaShadin SNo ratings yet
- Leukemia: Defintion: Leukemias Are Diseases in Which Localised or Generalised Proliferation orDocument12 pagesLeukemia: Defintion: Leukemias Are Diseases in Which Localised or Generalised Proliferation orsharon victoria mendezNo ratings yet
- Leukemia AcuteDocument7 pagesLeukemia AcutefallstarrNo ratings yet
- Haematologic MalignanciesDocument18 pagesHaematologic MalignanciesMukesh SahooNo ratings yet
- Anatomy: Hem Atolog YDocument94 pagesAnatomy: Hem Atolog YaamirNo ratings yet
- 6.7 Acute and Chronic Leukemias - Feb 11 - Dra. CaliwaganDocument14 pages6.7 Acute and Chronic Leukemias - Feb 11 - Dra. CaliwaganJCAsssssiloNo ratings yet
- Pathogenesis of Non-Hodgkin's Lymphoma: Ournal of Linical NcologyDocument9 pagesPathogenesis of Non-Hodgkin's Lymphoma: Ournal of Linical NcologyZullymar CabreraNo ratings yet
- Lypmhomas PDFDocument4 pagesLypmhomas PDFVerónica Guadalupe Dimayuga HernándezNo ratings yet
- Tutors CBL Long Case 2 LeukaemiaDocument4 pagesTutors CBL Long Case 2 LeukaemiaRayNo ratings yet
- Case Study On Acute Lymphocytic/Lymphoblastic LeukemiaDocument22 pagesCase Study On Acute Lymphocytic/Lymphoblastic LeukemiaLilian Linogao86% (21)
- Red Blood Cells..: Erythropoiesis.Document10 pagesRed Blood Cells..: Erythropoiesis.lubna aloshibiNo ratings yet
- MDT 100 Study GuideDocument7 pagesMDT 100 Study GuideSatori NoëlNo ratings yet
- Acute Lymphoblastic Leukaemia ArticleDocument10 pagesAcute Lymphoblastic Leukaemia ArticleDiego Fernando Ortiz TenorioNo ratings yet
- Faculty of Medicine Department of Molecular and Medical Genetics Typical Exam Tests Genetics 1Document9 pagesFaculty of Medicine Department of Molecular and Medical Genetics Typical Exam Tests Genetics 1adehkordiNo ratings yet
- The LeukemiasDocument52 pagesThe Leukemiasمصطفي خندقاوي100% (1)
- Fast Facts: Leukemia: From initial gene mutation to survivorship supportFrom EverandFast Facts: Leukemia: From initial gene mutation to survivorship supportNo ratings yet
- Endocrine Physiology) 15. Adrenal Medulla - Catecholamines - KeyDocument1 pageEndocrine Physiology) 15. Adrenal Medulla - Catecholamines - Keyhasanatiya41No ratings yet
- Endocrinology Pathology - 007) Cushing's Syndrome (Notes)Document7 pagesEndocrinology Pathology - 007) Cushing's Syndrome (Notes)hasanatiya41No ratings yet
- Endocrinology Pathology - 009) Pheochromocytoma (Illustrations - Key)Document1 pageEndocrinology Pathology - 009) Pheochromocytoma (Illustrations - Key)hasanatiya41No ratings yet
- Orthopedic DisordersDocument15 pagesOrthopedic Disordershasanatiya41No ratings yet
- Reumato and EndocrineDocument106 pagesReumato and Endocrinehasanatiya41No ratings yet
- Neurology LectureDocument48 pagesNeurology Lecturehasanatiya41No ratings yet
- 010 - Cardiovascular Physiology) Cardiovascular Cardiac CycleDocument3 pages010 - Cardiovascular Physiology) Cardiovascular Cardiac Cyclehasanatiya41No ratings yet
- CardiologyDocument43 pagesCardiologyhasanatiya41No ratings yet
- Hematology& Onco LectureDocument66 pagesHematology& Onco Lecturehasanatiya41No ratings yet
- Development & Growth Nutrition & Behavioral DisordersDocument27 pagesDevelopment & Growth Nutrition & Behavioral Disordershasanatiya41No ratings yet
- Cardiovascular Pharmacology) 09 Thiazide Diuretics - KeyDocument1 pageCardiovascular Pharmacology) 09 Thiazide Diuretics - Keyhasanatiya41No ratings yet
- 057 - Endocrinology Physiology) OvulationDocument4 pages057 - Endocrinology Physiology) Ovulationhasanatiya41No ratings yet
- Pharmacology Basics - 016) Drugs For Heart Failure (Notes - Q&A)Document3 pagesPharmacology Basics - 016) Drugs For Heart Failure (Notes - Q&A)hasanatiya41No ratings yet
- Hematology Pathology - 003) Acute Lymphoblastic Leukemia (ALL) (Illustrations - Key)Document1 pageHematology Pathology - 003) Acute Lymphoblastic Leukemia (ALL) (Illustrations - Key)hasanatiya41No ratings yet
- Vasculitis PPT NotesDocument14 pagesVasculitis PPT Noteshasanatiya41No ratings yet
- Hematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Illustrations - Key)Document1 pageHematology Pathology - 006) Chronic Myeloid Leukemia (CML) (Illustrations - Key)hasanatiya41No ratings yet
- Hematology Pathology - 005) Chronic Lymphocytic Leukemia (CLL) (Illustrations - Key)Document1 pageHematology Pathology - 005) Chronic Lymphocytic Leukemia (CLL) (Illustrations - Key)hasanatiya41No ratings yet
- 342 - Hematology Physiology) Erythropoiesis Red Blood Cell FormationDocument6 pages342 - Hematology Physiology) Erythropoiesis Red Blood Cell Formationhasanatiya41No ratings yet
- Engineering CAR-T Cells To Activate Small-MoleculeDocument24 pagesEngineering CAR-T Cells To Activate Small-MoleculeKudelko MatNo ratings yet
- Liver Cirrhosis Care PlanDocument3 pagesLiver Cirrhosis Care PlanWendy EscalanteNo ratings yet
- ProbabilityDocument49 pagesProbabilityKaveh ArabpourNo ratings yet
- Ipsc LectureDocument36 pagesIpsc LectureGuleRia ShiVani0% (1)
- Foundations in Microbiology: TalaroDocument68 pagesFoundations in Microbiology: Talaromertx013No ratings yet
- Biopsychosocial Model of Health and DiseaseDocument7 pagesBiopsychosocial Model of Health and DiseaseMary Romaine Dela PasionNo ratings yet
- Activity 5 TitrationDocument1 pageActivity 5 TitrationPorcha PacsayNo ratings yet
- AlbinismDocument10 pagesAlbinismTapash GopeNo ratings yet
- Production of Transgenic Goats Expressing Human Coagulation Factor IX in The Mammary Glands After Nuclear Transfer Using Transfected Fetal Fibroblast CellsDocument9 pagesProduction of Transgenic Goats Expressing Human Coagulation Factor IX in The Mammary Glands After Nuclear Transfer Using Transfected Fetal Fibroblast CellsMaira QuintanaNo ratings yet
- Premature Rupture of MembranesDocument4 pagesPremature Rupture of MembranesNikko Pabico67% (3)
- Haematopoiesis: Jump To Navigation Jump To SearchDocument16 pagesHaematopoiesis: Jump To Navigation Jump To SearchHashim uddinNo ratings yet
- Co Ip and IpDocument77 pagesCo Ip and IpTaufikNo ratings yet
- Renal Drug ExcretionDocument15 pagesRenal Drug ExcretionSatwika EkanandaNo ratings yet
- A Mechanism-Based Approach To Physical Therapist Management of PainDocument13 pagesA Mechanism-Based Approach To Physical Therapist Management of PainLuis Eduardo Cabezas MirandaNo ratings yet
- BIOL 2905 Quiz 2 Immunology BasicsDocument6 pagesBIOL 2905 Quiz 2 Immunology BasicsShafeeq ZamanNo ratings yet
- COVID 19 Origin Paper PreproofDocument19 pagesCOVID 19 Origin Paper PreproofSANDEEP REDDYNo ratings yet
- Karyotyping Gizmo Digital 2023Document5 pagesKaryotyping Gizmo Digital 2023zackdagoat404 0No ratings yet
- Sy Compdiv1 Genes - t1Document9 pagesSy Compdiv1 Genes - t1Shreeya GanjiNo ratings yet
- Care of The Elderly: "Roles of The Nurses To Resolve Geriatric Syndrome"Document42 pagesCare of The Elderly: "Roles of The Nurses To Resolve Geriatric Syndrome"Tino PriyudhaNo ratings yet
- Final Capstone PaperDocument15 pagesFinal Capstone Paperapi-478784238No ratings yet
- Definitive Guide To Red Light Therapy PhotobiomodulationDocument10 pagesDefinitive Guide To Red Light Therapy PhotobiomodulationDavid Jenkins0% (2)
- IVMS - General Pathology, Inflammation NotesDocument19 pagesIVMS - General Pathology, Inflammation NotesMarc Imhotep Cray, M.D.No ratings yet
- Stuttering and Second Language LearnersDocument12 pagesStuttering and Second Language Learnersapi-324980546100% (1)
- Voltage, The Key To Rebuilding You LifeDocument33 pagesVoltage, The Key To Rebuilding You LifeLodan Ranue100% (3)
- Physiology of Pain Pathways and Who Pain LadderDocument38 pagesPhysiology of Pain Pathways and Who Pain LadderSai TejeswiNo ratings yet
- 2019 Maxicare Plus Standard - SMALL - WithVAT - 50kDocument16 pages2019 Maxicare Plus Standard - SMALL - WithVAT - 50kLew WallaceNo ratings yet
- Pseudomonas and Bacillus) As GreatDocument3 pagesPseudomonas and Bacillus) As Greatichi senriNo ratings yet
- Fragile X Syndrome EssayDocument4 pagesFragile X Syndrome Essayapi-338677507No ratings yet
- Transfusion-Related Acute Lung Injury: HistoryDocument20 pagesTransfusion-Related Acute Lung Injury: HistoryBladimir CentenoNo ratings yet
- Nursing Care Plan For Down SyndromeDocument20 pagesNursing Care Plan For Down SyndromeMuhammad Jefri LukmanNo ratings yet