Professional Documents
Culture Documents
8.3 Acute Kidney Injury - March 16 - Dr. Austria.
Uploaded by
Jess PeltraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
8.3 Acute Kidney Injury - March 16 - Dr. Austria.
Uploaded by
Jess PeltraCopyright:
Available Formats
INTERNAL MEDICINE ACUTE KIDNEY INJURY
AY 2021-2022
NICKSON AUSTRIA, M.D.
Renal Module 03/16/2022
2. AKD
TOPIC OUTLINE a. Transition point of varying Crea and UO for <3
I. Definition mos.
3. CKD
II. KDIGO Criteria and Staging for AKI Diagnosis
a. Kidney damage for > 3mos as defined by
III. Epidemiology structural or functional abnormalities
IV. Etiology and Pathophysiology b. with or without decreased GFR irrespective of
a. Prerenal Azotemia cause
b. Intrinsic Renal Parenchymal Disease c. Kidney damaged is ascertained by GFR and
c. Postrenal Obstruction albuminuria
V. History and Physical Examination d. CKD is staged 1-5 by GFR (based on crea or
crystatin and A1 to A3 by albuminuria.
a. Urine Findings
b. Serum Labs KIDNEY BASICS
c. Imaging ● Filters around 1700L of blood per day to produce around
d. Biopsy 1L of concentrated urine
e. Biomarkers ● Maintains homeostasis
VI. Complications ● Chief regulator of fluid balance, pH, electrolytes,
VII. Treatment endocrinologic, hematologic, immunomodulatory
functions.
a. Renal Replacement Therapy
● Structurally complex
● Basic unit: NEPHRON
LEARNING OBJECTIVES ● Best to appreciate it in 4 morphologic components
1. Discuss acute kidney disorders in terms of: ○ glomerulus
a. Epidemiology ○ Tubules
○ interstitium
b. Etiology (causes)
○ vasculature
c. Clinical Presentation
d. Diagnosis MECHANISMS OF KIDNEY INJURY
● Pre renal : hypotension, excessive fluid loss, shock,
LEGEND: volume depletion, CHF, liver cirrhosis
Clinical Guide ● Renal: Glomerular, tubular/ iterstitial, vascular
PPT Lecturer Book ● Post renal: obstruction distal to the kidneys,
Correlation/SGDs Questions
nephrolithiasis, cancers, prostatic enlargement etc.
● ❖
II. KDIGO CRITERIA AND STAGING FOR AKI
I. DEFINITION DIAGNOSIS
● Impairment of kidney filtration and excretory fxn over
days to weeks causing retention of nitrogenous and other
waste products
● Increase in SCr conc. Often associated w/ redxn in urine
vol
● Clinical dx, NOT a structural one
SPECTRUM OF KIDNEY DISEASE
1. AKI
a. Sudden loss of kidney function generally
occurring with in hours to days resulting in the
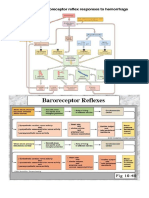
retention of metabolic waste products, Fig 1. Staging of AKI
dysregulation of fluids, electrolytes and *also found in Appendix figure 5
acid-base homeostasis.
Stage 1 Rise in Crea 1.5 - 1.9 fold (7 days or 0.3 III. EPIDEMIOLOGY
mg/dl in 48hrs; OU <0.5ml/kg/hr for 6 hrs ● AKI increases risk for worsening CKD
● Px who survived and recovered from episode of severe
Stage 2 2.0-2.9 fold OU <0.5ml/kg/hr for >12 hrs. AKI requiring dialysis has increased risk for later
development of dialysis-requiring ESRD
Stage 3 >3x or Crea >4.0mg/dl with an acute ● Common causes of community-acquired AKI: vol
increase of >0.5 mg/dL; UO <0.3 mg/kg/hr depletion, HF, ADR, UT obstruction, malignancy
for > 24 hrs or anuria >12hrs
INTERNAL MEDICINE ACUTE KIDNEY INJURY
● Common causes of hospital acquired: sepsis, major ● RBF = 20% of CO
surgical procedure, critical illness following HF or liver ● Mediators of renal vasoconstriction + salt and water
failure, nephrotoxic medication administration reabsorption in response to decreased circulating vol/
CP: angiotensin II, myogenic reflex, tubuloglomerular
IV. ETIOLOGY AND PATHOPHYSIOLOGY feedback
● Factors inhibiting autoregulatory response: hyalinosis
and myointimal hyperplasia from long-standing HTN/old
● 3 categories: prerenal azotemia, intrinsic renal age/ atherosclerosis, CKD, NSAIDs, ACE-I, ARBs, advanced
parenchymal ds., post-renal obstruction liver ds (hepatorenal syndrome)
b. Intrinsic Renal Parenchymal Disease
INTRINSIC AKI
- Can be classified as damage to any of the 4 regions:
glomerular, tubular, interstitial and vascular.
● MC causes: sepsis, ischemia, nephrotoxins
● Contributors: inflammation, apoptosis, altered regional
perfusion
1. Sepsis-Associated AKI
a. Can complicate as much as 50% of severe sepsis
b. Usually occurs with hypotension
c. Damage mediated by inflammatory cytokines
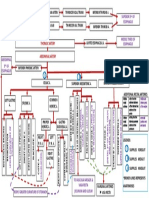
Fig 2. AKI etiology leading to loss of autoregulation
d. Initially: afferent vasodilation and release of NO
a. Prerenal Azotemia etc.
PRE- RENAL AKI e. Later: severe vasoconstriction and
- Decreased effective circulatory volume (shock, hypoperfusion and reduction in GFR.
hypovolemia) -> norepinephrine, angiotensin, f. Most cases in setting of hemodynamic collapse
vasopressin release -> Salt and water reabsorption -> requiring vasopressor support
blood shunts to critical organs g. Hemodynamic efx of sepsis (generalized
- Afferent artery vasoconstriction -> down regulation in vasodilation) decreases GFR
vasodilatory agents (PG, NO, kallikreins and kinins) h. Efferent arteriole vasodilation, renal
- Reverse: TG feedback via the macula densa can work to vasoconstriction from SNS activation/ RAAS/
preserve GFT i states of hypotension but limited to the vasopressin/ endothelin, endothelial damage
nature of the systemic condition resulting to thrombosis, permeability, and
- Key concept: autoregulation activation of ROS which injure renal tubular
- Kidneys are very altruistic organs. cells
- insults occur before the kidneys and hence is more 2. Ischemia-Associated AKI
related to systemic issues. a. Apart from receiving 10% of resting energy
- Absence of damage to the kidney structure/ parenchyma consumption
itself b. Outer medulla – most susceptible to ischemic
- Results in the retention of nitrogenous wastes (azotemia) damage
- Seen as reductions in the renal plasma flow and c. Ischemia alone in healthy kidney is NOT
decreased intraglomerular hydrostatic pressure. sufficient to cause severe AKI
- Should reverse with resumption of renal blood flow. d. AKI more common if ischemia is with CKD or
- May progress to intrinsic renal injury if not managed coexisting insults (sepsis, nephrotoxic drugs,
properly. rhabdomyolysis, etc)
Common causes: hypovolemia, decreases ECV (CHF/ Cirrhosis) e. Prerenal azotemia and ischemia associated AKI
Dysregulation: NSAIDS RAS blockers. = from renal hypoperfusion
f. Post-op AKI: significant blood loss/ intraop
● MC AKI hypotension; RF being CKD, old age, DM, CHF,
● Inadequate renal plasma flow and intraglomerular ER procedures
hydrostatic P to support normal glomerular filtration g. Burns/ Acute Pancreatitis: extensive fluid losses
● Hypovolemia, dec. CO, NSAIDs, Angiotensin II inhibitors in the extracellular compartment
● Prolonged prerenal azotemia may lead to ischemic injury h. Microvascular diseases leading to ischemia:
(acute tubular necrosis) thrombotic microangiopathies, scleroderma,
● No parenchymal damage atheroembolic ds.
● Rapidly reversible upon normalization of parenchymal
blood and intraglomerular hemodynamics
AOYANG, ASILO, CATIBOG, DOLOR, HERNANDEZ, JUSTINIANO, MARALIT 2 of 6
INTERNAL MEDICINE ACUTE KIDNEY INJURY
i. Large vessel ds: renal artery dissection, V. HISTORY AND PHYSICAL EXAMINATION
thromboembolism, thrombosis, renal v.
● Prerenal azotemia: vomiting, diarrhea, glycosuria
compression/ thrombosis causing polyuria, diuretics, NSAIDs, ACE-I, ARBs,
orthostatic hypotension, tachycardia, reduced JVP,
decreased skin turgor, dry mucosa, congestive HD, liver
failure
● Interstitial AKI: extensive vascular ds., asymmetric
kidneys, livedo reticularis, emboli to legs, sepsis,
medications, recent blood transfusion, injuries,
chemotherapy, infection, pruritic rash (AIN = fever, rash,
arthralgias)
● Postrenal AKI: nocturia + urinary hesitancy/frequency
(prostatic ds.), nephrolithiasis, pelvic/paraaortic
malignancy, colicky flank pain radiating to groin (ureteric
obs.)
a. Urine Findings
3. Nephrotoxin-Associated AKI
a. Contrast Agents: iodinated contrast (contrast
nephropathy), high-dose gadolinium for MRI,
oral Na phosphates, bowel purgatives
b. Antibiotics: vancomycin, aminoglycosides,
amphotericin B, Acyclovir, Foscarnet,
Pentamidine, Tenofovir, Cidofovir, Penicillin,
Cephalosporin, Quinolones, Sulfonamides,
Rifampin
c. Chemo-drugs: Cisplatin, carboplatin, ifosfamide,
bevacizumab
d. Toxic agents: ethylene glycol, Melamine, Fig 3. Urine findings in AKI
Aristolochic acids
e. Endogenous Toxins: myoglobin, hemoglobin, ● Complete anuria causes: complete UT obs., RA occlusion,
uric acid, myeloma chains overwhelming septic shock, severe ischemia, severe
f. Other causes of acute tubulointerstitial disease proliferative GN/ vasculitis
leading to AKI: allergic response causing acute ● Oliguria: obs., nephrotoxicity, TIN
tubulointerstitial nephritis ● Anuria (<400mL/day): severe sepsis/ shock
● Heme + w/o RBC: rhabdomyolysis/ hemolysis
4. Glomerulonephritis ● Prerenal AKI: hyaline casts
a. Involves glomerular podocytes, mesangial cells, ● ATN: muddy brown cast w/ tubular epithelial cells
endothelial cells ● GN: >20% RBCs dysmorphic, RBC casts; heavy
b. Compromised filtration barrier and blood flow proteinuria (>1g/day or 3.5 g nephrotic)
w/in renal circulation ● AIN: urine eosinophils
c. Less common cause of AKI ● Ethylene glycol toxicity: Ca oxalate crystalluria
d. Can respond to tx w/ immunosuppressants/ ● TLS: uric acid crystalluria
therapeutic plasma exchange
b. Serum Labs
c. Postrenal Obstruction
● Serial SCr monitoring (prerenal azotemia should return
● Normally unidirectional flow of urine is blocked partially promptly to normal upon correction of hemodynamic
or totally stat)
● Increased retrograde hydrostatic P w/ interference to ● CBC: anemia (multifactorial), elevated WBC (sepsis),
glomerular filtration thrombocytopenia w/ schistocytes (TTP), eosinophilia
● Preservation of urine output may be misleading in hiding (AIN)
postrenal partial obstruction ● Hyperkalemia, hyperphosphatemia, hypocalcemia
● MC: bladder neck obstruction ● TLS: hyperkalemia, hyperphosphatemia, hypocalcemia,
● Hemodynamic alterations triggered by abrupt increase in hyperuricemia
intratubular P (initial hyperemia from afferent arteriolar ● ABG: acidosis + high anion gap
vasodilation followed by intrarenal vasoconstriction from ● Myeloma: low anion gap (high anionic protein released
the generation of angiotensin II, thromboxane A2, from myeloma)
vasopressin, and reduction in NO production) ● Ethylene glycol tox: osmolal gap in serum Osm
AOYANG, ASILO, CATIBOG, DOLOR, HERNANDEZ, JUSTINIANO, MARALIT 3 of 6
INTERNAL MEDICINE ACUTE KIDNEY INJURY
● ANA, anti-dsDNA, ANCA, complement levels, o Complicate acid-base and potassium imbalance
cryoglobulins in px’s w/ other causes of acidosis (sepsis,
diabetic ketoacidosis, resp acidosis)
c. Imaging ● Hyperphosphatemia + Hypocalcemia
● Ultrasound o Rhabdomyolysis, TLS, hemolysis
o Useful in postrenal AKI o Hypocalcemia: perioral paresthesia, muscle
o Finding: dilation of collecting system, cramps, seizures, carpopedal spasm, prolonged
hydroureteronephrosis QT-i
o Absence of radiologic abnormalities in vol ● Bleeding
depletion, retroperitoneal fibrosis, encasement o Direct hema efx from uremia
w/ tumor, early obs. o Decreased erythropoiesis and pltlt dysfxn
o Differentiate CKD from AKI (CKD = small kidney ● Infections
usually <8cm o Common precipitant of AKI
o Enlarged CKD kidney: DM, HIV nephropathy, o Dreaded complication of AKI
infiltrative ds., AIN o Impaired host immunity esp in ESRD
o Avoid: MRI w/ Gadolinium contrast ● Cardiac Complications
(nephrogenic systemic fibrosis) o Arrhythmias, pericarditis, effusion
● Malnutrition
d. Biopsy o From severely hypercatabolic state in AKI
● If AKI cause is NOT apparent on Hx, PE labs, imaging
● Diagnostic and prognostic evaluation VII. TREATMENT
● If the ff are unlikely: Prerenal azotemia, postrenal AKI, ● Volume Mgt
ischemic AKI, nephrotoxic AKI o Address hypovolemia (be cautious about pulmo
● If ff are considered: GN, vasculitis interstitial nephritis, edema)
myeloma, TTP/ HUS, allograft dysfxn o Restrict fluids and Na
o Use of diuretics
e. Biomarkers o Low dose dopa : NO BENEFIT
● BUN + Crea = biomarkers of glomerular filtration, NOT ● Electrolytes
tissue injury; suboptimal for dx of actual parenchymal o Acidosis: target pH > 7.2 (HCO3 15 mmol/L)
damage; slow to rise after kidney injury o Avoid overcorrection (metabolic alkalosis,
● Kidney Injury Molecule – 1 (KIM-1) = expressed in prox hypocalcemia, hypokalemia, vol overload)
tubular cells injured by ischemia/ nephrotoxins o Hyperphosphatemia: phosphate binders ( Ca
● Neutrophil Gelatinase Associated Lipocalin (NGAL/ carbonate, alum hydroxide, etc)
lipocalin-2/ siderocalin) = highly upregulated after ● Anemia
inflammation/ kidney injury w/in 2 hrs of cardiopulmo o NOT improved by EPO
bypass assoc. AKI o Replace blood loss
o Uremic bleeding: desmopressin or estrogen
o GI prophylaxis: PPIs / H2 receptor blockers
VI. COMPLICATIONS
● Malnutrition
● Uremia o Inadequate nutrition: starvation ketoacidosis
o Elevated BUN and protein catabolism
o BUN has LITTLE direct toxicity if <100 mg/dL o Excessive nutrition: nitrogenous waste
o At higher levels = mental stat changes, bleeding generation and worsening azotemia
● Hypervolemia o KDIGO Guideline on total energy intake of px w/
o Expansion of extracellular fluid vol AKI: 20-30 kcal/kg/day
o Impaired salt and H20 excretion o Protein intake based on AKI severity
● Hypovolemia ▪ Noncatabolic AKI w/o need for
o Polyuria accompanying AKI recovery (osmotic dialysis: 0.8-1.0g/kg/day
diuresis from retained urea) ▪ Px on dialysis: 1.0-1.5g/kg/day
● Hyponatremia ▪ Hypercatabolic w/ RRT: max
1.7g/kg/day
o From administration of excessive hypotonic
crystalloid/ isotonic dextrose sol’n in pc with
dysfunctional kidneys unable to regulate
electrolyte balance
● Hyperkalemia
o Most feared
o Fatal arrhythmias
● Acidosis
o Metabolic acidosis + elevated anion gap
AOYANG, ASILO, CATIBOG, DOLOR, HERNANDEZ, JUSTINIANO, MARALIT 4 of 6
INTERNAL MEDICINE ACUTE KIDNEY INJURY
a. Renal Replacement Therapy
● Indications: mgt fails to control vol overload,
hyperkalemia, acidosis, toxic ingestions, severe
complications of uremia (asterixis, pericardial
rub/effusion, encephalopathy, uremic bleeding)
● Late initiation: risk of avoidable vol, electrolyte, metabolic
complications of AKI
● Early Initiation: infection, bleeding, hypotension,
procedural complications from IV lines and invasive
procedures
● Diffusive clearance: small solutes removed across
semipermeable membrane down conc gradient
● Convective clearance: solutes removed along w/
movement of plasma
1. Hemodialysis
a. Vascular access: femoral, IJV, Subclavian vein
b. Intermittent, diffusive and convective
c. 3-4 hrs/day, 3-4x/wk
d. Most common form of RRT
e. Complications: hypotension (may perpetuate
AKI)
2. Continuous Renal Replacement Therapy (CRRT)
a. Convective (Continuous Venous Hemofiltration)
b. Diffusive (continuous venous hemodialysis)
3. Slow low efficiency dialysis (SLED)
a. Extended daily dialysis
b. Blood flow and dialysate flow are higher than
CVVHD but tx time reduced to </=12 hrs
4. Peritoneal Dialysis
a. Use temporary intraperitoneal catheter
b. Dialysate sol’n instilled into and removed from
peritoneal cavity at regular intervals in order to
achieve diffusive and convective clearance of
solutes across peritoneal membrane
c. Dextrose dialysate sol’n
d. Continuous, convective and diffusive
e. May NOT be sufficient in hypercatabolic px due
to inherent limitations in dialysis efficacy
Guide Questions
1. How much urine per day to be considered anuric
2. When will you think of interstitial/tubular kidney
disease as opposed to prerenal azotemia
a. 500 mOsm/L urine osmolality
b. 300 mOsm/L urine osmolality
3. Regarding #2, why is that the answer?
4. Why is the S3 segment prone to ischemia?
5. Where do you expect to find ischemia first?
a. Cortex
b. Medulla
Answers: </=400mL/day, B, if the interstitium and tubules are already affected, the
ability of the kidney to concentrate urine will be impaired resulting to a dilute urine, It
is the most metabolically active where most NaCl and H20 are reabsorbed, B
References:
● Dr. Austria’s Slides
● Jameson, J., Kasper, D., Longo, D. … Loscalzo, J. (2018).
Fig 4. Management of AKI Harrison’s principles of internal medicine (20th edition).
New York, New York: McGraw-Hill Education.
AOYANG, ASILO, CATIBOG, DOLOR, HERNANDEZ, JUSTINIANO, MARALIT 5 of 6
INTERNAL MEDICINE ACUTE KIDNEY INJURY
APPENDIX
Fig 5. Staging of AKI
AOYANG, ASILO, CATIBOG, DOLOR, HERNANDEZ, JUSTINIANO, MARALIT 6 of 6
You might also like
- Medical Terminology - Prefixes, Suffixes, Root WordsDocument9 pagesMedical Terminology - Prefixes, Suffixes, Root Wordssooperstarx2171% (7)
- Lab - 18 (Gizmo) Senses SEDocument8 pagesLab - 18 (Gizmo) Senses SEJack50% (4)
- CCRN-PCCN Review RenalDocument11 pagesCCRN-PCCN Review RenalGiovanni MictilNo ratings yet
- Paeds Crack Notes-1Document111 pagesPaeds Crack Notes-1Ashutosh Krishna JadhavNo ratings yet
- ccpc15 Principles Renal Clearance Acute Kidney Renal Replacement WorkbookDocument22 pagesccpc15 Principles Renal Clearance Acute Kidney Renal Replacement WorkbookJeremy Hampton67% (3)
- Understanding Chronic Kidney Disease: A guide for the non-specialistFrom EverandUnderstanding Chronic Kidney Disease: A guide for the non-specialistRating: 4 out of 5 stars4/5 (3)
- Chronic Kidney DiseaseDocument6 pagesChronic Kidney DiseaseAndrea GuidoteNo ratings yet
- 8.4 Chronic Kidney Disease - March 17 - Dra. BasilanDocument9 pages8.4 Chronic Kidney Disease - March 17 - Dra. BasilanJess PeltraNo ratings yet
- Aki CR 1Document3 pagesAki CR 1AmeldaNo ratings yet
- Acut Kidney InjuryDocument12 pagesAcut Kidney InjuryorriNo ratings yet
- QweqDocument7 pagesQweqJackieNo ratings yet
- AKI Perioperatif 3Document6 pagesAKI Perioperatif 3Kevin JohanesNo ratings yet
- MRCP Course Handbook 2022Document140 pagesMRCP Course Handbook 2022Nada KhanNo ratings yet
- CHRONIC KIDNEY DISEASE GUIDEDocument9 pagesCHRONIC KIDNEY DISEASE GUIDECorazon Arellano RamosNo ratings yet
- Slide NephrologyDocument19 pagesSlide Nephrologyandirio7486No ratings yet
- Acute Kidney InjuryDocument5 pagesAcute Kidney InjuryisnaazmutNo ratings yet
- Nephrology DR ZeinabDocument101 pagesNephrology DR ZeinabZeinab Muhammad100% (1)
- Ea0039ep55 EposterDocument1 pageEa0039ep55 EposterMiftakhul HudaNo ratings yet
- INFECTIOUS CASE - SGD 8Document91 pagesINFECTIOUS CASE - SGD 8PARADISE JanoNo ratings yet
- The Definition of Acute Kidney Injury and Its Use in PracticeDocument12 pagesThe Definition of Acute Kidney Injury and Its Use in PracticeErwin SiahaanNo ratings yet
- AKI and CKDDocument73 pagesAKI and CKDzaw wai aungNo ratings yet
- Review Sheet-Introduction FinalDocument11 pagesReview Sheet-Introduction FinalsammyNo ratings yet
- Understanding Chronic Kidney Disease (CKDDocument48 pagesUnderstanding Chronic Kidney Disease (CKDyohannesNo ratings yet
- 2022 Clinthera S1T5 Aki PDFDocument4 pages2022 Clinthera S1T5 Aki PDFmedicoNo ratings yet
- Acute Kidney Injury HarrisonsDocument13 pagesAcute Kidney Injury HarrisonsDan Angelo TemplonuevoNo ratings yet
- Acute Kidney Injury: Current Concepts and New Insights: Key WordsDocument5 pagesAcute Kidney Injury: Current Concepts and New Insights: Key WordsIHNo ratings yet
- Medical MasterClass MRCP Part 2 Nephrology 2010 ElzohrykDocument82 pagesMedical MasterClass MRCP Part 2 Nephrology 2010 ElzohrykSagvan HajaniNo ratings yet
- Low-Flow Acute Kidney InjuryDocument11 pagesLow-Flow Acute Kidney InjuryJuan Manuel Lopez VargasNo ratings yet
- Aki Vs CKD: Consultant NephrologistDocument35 pagesAki Vs CKD: Consultant NephrologistFreeburn SimunchembuNo ratings yet
- Management of Patients With Renal DisordersDocument14 pagesManagement of Patients With Renal DisordersJhosita Flora LarocoNo ratings yet
- ATN Post NephrectomyDocument3 pagesATN Post NephrectomyUrologi Januari21No ratings yet
- Generalidades de La Rabdomiolisis: Dra. Kelly Ortiz Villarreal Residente I Medicina InternaDocument13 pagesGeneralidades de La Rabdomiolisis: Dra. Kelly Ortiz Villarreal Residente I Medicina Internadantheman123No ratings yet
- Injuria Renală Acută CorectatDocument6 pagesInjuria Renală Acută CorectatCaraiman LarisaNo ratings yet
- 0800-0840 AKI Nephrology Review Internist2023 2Document58 pages0800-0840 AKI Nephrology Review Internist2023 2Jay Kittichoke PipatdumkoengNo ratings yet
- Integrated Therapeutics IiDocument165 pagesIntegrated Therapeutics IiSalahadinNo ratings yet
- Canine Chronic Kidney Disease Current Diagnostics & Goals For Long-Term ManagementDocument7 pagesCanine Chronic Kidney Disease Current Diagnostics & Goals For Long-Term ManagementJuni ClaudiaNo ratings yet
- Jurnal CKDDocument7 pagesJurnal CKDJuni ClaudiaNo ratings yet
- CellularDocument21 pagesCellularLoreth Aurea OjastroNo ratings yet
- Module A Compiled Samplex 2020Document47 pagesModule A Compiled Samplex 2020DeepbluexNo ratings yet
- Acute Kidney Injury Etd Nov-Dec HPSF Sem 6 2022Document22 pagesAcute Kidney Injury Etd Nov-Dec HPSF Sem 6 2022Harry James Potter James PotterNo ratings yet
- SIMCLEX Renal and Genitourinary DisordersDocument7 pagesSIMCLEX Renal and Genitourinary DisorderssandraNo ratings yet
- Lecture 6.1. Acute Kidney InjuryDocument39 pagesLecture 6.1. Acute Kidney InjurykrisnadewirahadiNo ratings yet
- Module 5Document31 pagesModule 5xtnreyesNo ratings yet
- NCM 118 - CCN - THEORY - MidtermsDocument19 pagesNCM 118 - CCN - THEORY - MidtermsSTEFFANIE VALE BORJANo ratings yet
- KDIGO Stage Serum CR Urine Output Criteria GFR (Step Up Mentions It) RIFLE (Risk/ Injury/Failure/Loss/END Stage Renal Disease) Stage 1Document11 pagesKDIGO Stage Serum CR Urine Output Criteria GFR (Step Up Mentions It) RIFLE (Risk/ Injury/Failure/Loss/END Stage Renal Disease) Stage 1Zahra AlaradiNo ratings yet
- Management of Acute Kidney Injury: Core Curriculum 2018Document13 pagesManagement of Acute Kidney Injury: Core Curriculum 2018Kholida NabilaNo ratings yet
- Renal Failure: An OverviewDocument28 pagesRenal Failure: An OverviewaburisyaNo ratings yet
- Diagnostic Approach To Chronic Kidney DiseaseDocument3 pagesDiagnostic Approach To Chronic Kidney DiseaseBlomblom Pow00No ratings yet
- Carotid-Cavernous Fistule: Case SeriesDocument46 pagesCarotid-Cavernous Fistule: Case SeriesaditzNo ratings yet
- Jurnal Aki 2018Document13 pagesJurnal Aki 2018Arief TricahyonoNo ratings yet
- Kdoki y KdigoDocument24 pagesKdoki y KdigoIsrael Armida SodanargNo ratings yet
- Chronic Kidney DiseaseDocument6 pagesChronic Kidney DiseaseOmaima AlhaikiNo ratings yet
- GU Blackboard OutlineDocument15 pagesGU Blackboard Outlinedlneisha61No ratings yet
- (MED 2) S04 T02 Acute Kidney InjuryDocument16 pages(MED 2) S04 T02 Acute Kidney InjurySheila Lyn LacsonNo ratings yet
- Feline Acute Kidney Injury. 2. Approach To Diagnosis, Treatment and PrognosisDocument9 pagesFeline Acute Kidney Injury. 2. Approach To Diagnosis, Treatment and PrognosisMartín QuirogaNo ratings yet
- C370 Lecture 1 Lecture Notes Part 2Document54 pagesC370 Lecture 1 Lecture Notes Part 2Yan Mui ChanNo ratings yet
- Prevent and Manage AKIDocument29 pagesPrevent and Manage AKImdonnyyuniarpratamaNo ratings yet
- Guidelines On The Management of Abnormal Liver Blood TestsDocument15 pagesGuidelines On The Management of Abnormal Liver Blood TestsYasser AlghrafyNo ratings yet
- NGAL Feature in CLI April-May 2009 IssueDocument4 pagesNGAL Feature in CLI April-May 2009 IssueKaycsa AdrianaNo ratings yet
- NCM 118 - Lesson 15 (Chronic Renal Failure and Dialysis)Document7 pagesNCM 118 - Lesson 15 (Chronic Renal Failure and Dialysis)Bobby Christian DuronNo ratings yet
- Acute Kidney Injury and Kidney Replacement Therapy in AdultsDocument7 pagesAcute Kidney Injury and Kidney Replacement Therapy in Adultsjsali9210No ratings yet
- Current Challenges with their Evolving Solutions in Surgical Practice in West Africa: A ReaderFrom EverandCurrent Challenges with their Evolving Solutions in Surgical Practice in West Africa: A ReaderNo ratings yet
- Case for SGDDocument1 pageCase for SGDJess PeltraNo ratings yet
- Net Notes AuditoryDocument8 pagesNet Notes AuditoryJess PeltraNo ratings yet
- Lateral Region Simplified For TransDocument4 pagesLateral Region Simplified For TransJess PeltraNo ratings yet
- Net Notes CardioDocument9 pagesNet Notes CardioJess PeltraNo ratings yet
- Blood FlowDocument1 pageBlood FlowJess PeltraNo ratings yet
- Chapter 4 - The Motor and Somatosensory Pathways and Approach To Weakness and Sensory LossDocument11 pagesChapter 4 - The Motor and Somatosensory Pathways and Approach To Weakness and Sensory LossJess PeltraNo ratings yet
- Chapter 4 - Postoperative CareDocument14 pagesChapter 4 - Postoperative CareJess PeltraNo ratings yet
- Complications Associated With Surgical Treatment of Congenital Intrinsic Duodenal ObstructionDocument4 pagesComplications Associated With Surgical Treatment of Congenital Intrinsic Duodenal ObstructionJess PeltraNo ratings yet
- Chapter 26 - HeadacheDocument9 pagesChapter 26 - HeadacheJess PeltraNo ratings yet
- 9.2.2 The Fetal Patient - Fetal Assessment - April 05 - Dra. MeerDocument3 pages9.2.2 The Fetal Patient - Fetal Assessment - April 05 - Dra. MeerJess PeltraNo ratings yet
- Chapter 9 - The Brainstem and Cranial NervesDocument8 pagesChapter 9 - The Brainstem and Cranial NervesJess PeltraNo ratings yet
- CPG Early and Locally Advanced Non-Small-Cell LungDocument6 pagesCPG Early and Locally Advanced Non-Small-Cell LungJess PeltraNo ratings yet
- COVID-19 Life EventsDocument30 pagesCOVID-19 Life EventsJess PeltraNo ratings yet
- Malignant Skin Disorders-HandoutDocument5 pagesMalignant Skin Disorders-HandoutJess PeltraNo ratings yet
- Y3 Immunologic DsesDocument65 pagesY3 Immunologic DsesJess PeltraNo ratings yet
- Surgery of The SkinDocument66 pagesSurgery of The SkinJess PeltraNo ratings yet
- HPAxis 3rd (Autosaved)Document29 pagesHPAxis 3rd (Autosaved)Jess PeltraNo ratings yet
- Histology: Male Reproductive SystemDocument24 pagesHistology: Male Reproductive SystemJess PeltraNo ratings yet
- Pregnancy Complication - HypertensionDocument37 pagesPregnancy Complication - HypertensionJess PeltraNo ratings yet
- Urologic Conditions Surgery GuideDocument6 pagesUrologic Conditions Surgery GuideJess PeltraNo ratings yet
- 8.2 Inguinal Hernias, PUV, and VUR - March 14 - Dr. Gellido & Dr. LawenkoDocument8 pages8.2 Inguinal Hernias, PUV, and VUR - March 14 - Dr. Gellido & Dr. LawenkoJess PeltraNo ratings yet
- Therapeutic Notes BKDocument1 pageTherapeutic Notes BKJess PeltraNo ratings yet
- Pemeriksaan Tensi Sesuai AHADocument1 pagePemeriksaan Tensi Sesuai AHAdhita octrianiNo ratings yet
- 8.5 Renal Cell Ca & Urothelial Ca - Mar 21 - Dra. de LaraDocument9 pages8.5 Renal Cell Ca & Urothelial Ca - Mar 21 - Dra. de LaraJess PeltraNo ratings yet
- PHYSICS OF VISION AND REFRACTIONDocument5 pagesPHYSICS OF VISION AND REFRACTIONJess PeltraNo ratings yet
- Cubital Tunnel Syndrome: Causes, Symptoms and TreatmentDocument18 pagesCubital Tunnel Syndrome: Causes, Symptoms and TreatmentJess PeltraNo ratings yet
- Edukasyon Sa Pagpapakatao Curriculum Guide Grade 1-10Document3 pagesEdukasyon Sa Pagpapakatao Curriculum Guide Grade 1-10Jess PeltraNo ratings yet
- U1 l1 Basic Concepts of SetsDocument39 pagesU1 l1 Basic Concepts of SetsJess PeltraNo ratings yet
- Nephrology and Urology MCQsDocument111 pagesNephrology and Urology MCQsAhMad MaGdyNo ratings yet
- The Heart Has Several Pacemakers Known As Autonomic FociDocument1 pageThe Heart Has Several Pacemakers Known As Autonomic FociAnonymous mLYupGyNNo ratings yet
- BIO2A03-Respiration Lecture NotesDocument67 pagesBIO2A03-Respiration Lecture NotesJeevikaGoyalNo ratings yet
- Pacemaker Learning Package: Paula Nekic CNE Liverpool Hospital ICU January 2016Document46 pagesPacemaker Learning Package: Paula Nekic CNE Liverpool Hospital ICU January 2016Zahangir Kabir AshikNo ratings yet
- Lymphatic SystemDocument2 pagesLymphatic Systemmeg leeNo ratings yet
- 6th Class General Science Chapter 2Document2 pages6th Class General Science Chapter 2Shahid MahmoodNo ratings yet
- How Animals SurviveDocument69 pagesHow Animals SurviveMichael Daryl GalsimNo ratings yet
- Chapter 19 - Nutritional Needs of A NewbornDocument8 pagesChapter 19 - Nutritional Needs of A NewbornMerenisa LiminNo ratings yet
- Class 11 Biology Sheet - 1Document4 pagesClass 11 Biology Sheet - 1Vidya SajitNo ratings yet
- 4 Human Anatomy and Physiology (2220004)Document4 pages4 Human Anatomy and Physiology (2220004)Shrinidhi AcharyaNo ratings yet
- Guided Notes Respiratory SystemDocument3 pagesGuided Notes Respiratory Systemapi-280337641No ratings yet
- Autonomic Nervous SystemDocument40 pagesAutonomic Nervous SystemmarciaNo ratings yet
- Food Classes: FAT Water Vitamins, Minerals, & Roughage ProteinDocument25 pagesFood Classes: FAT Water Vitamins, Minerals, & Roughage Proteinuminoriah80% (5)
- Cerebellum: John H. Martin, Ph.D. Center For Neurobiology & Behavior Columbia UniversityDocument21 pagesCerebellum: John H. Martin, Ph.D. Center For Neurobiology & Behavior Columbia UniversitySasikala MohanNo ratings yet
- COVID-19 Case Study InsightsDocument43 pagesCOVID-19 Case Study InsightsElena Cariño De Guzman100% (1)
- CH 4take Home Test - Chapter 4 Integumentary SystemDocument5 pagesCH 4take Home Test - Chapter 4 Integumentary SystemKatieNo ratings yet
- Liver Cirrhosis PowerPointDocument12 pagesLiver Cirrhosis PowerPointFrancis Adrian100% (2)
- Heart CH 12 PDFDocument65 pagesHeart CH 12 PDFGabriel Tafalla100% (1)
- Anatomy For Beginners 2 - CirculationDocument18 pagesAnatomy For Beginners 2 - CirculationDefy R PradentyNo ratings yet
- Neurotransmitter Release and ProcessDocument14 pagesNeurotransmitter Release and ProcessRain TolentinoNo ratings yet
- The Lymphatic System and Body Defenses ExplainedDocument57 pagesThe Lymphatic System and Body Defenses ExplainedJulia Stefanel PerezNo ratings yet
- BSC Immunology Course Sylibus - Updated 1st Sem. 2022-2023Document3 pagesBSC Immunology Course Sylibus - Updated 1st Sem. 2022-2023Basma MohamedNo ratings yet
- Pengaruh Pijat Laktasi Terhadap Produksi ASI Pada Ibu Menyusui Di Kelurahan Sendang Sari Kabupaten Asahan Tahun 2019Document7 pagesPengaruh Pijat Laktasi Terhadap Produksi ASI Pada Ibu Menyusui Di Kelurahan Sendang Sari Kabupaten Asahan Tahun 2019MAS 16No ratings yet
- Lesson Plan ScienceDocument7 pagesLesson Plan ScienceAnonymous JCLBQh0eNo ratings yet
- Physiology of The Digestive System: Column A Column BDocument4 pagesPhysiology of The Digestive System: Column A Column BJonash MoralesNo ratings yet
- Tissue WorksheetDocument4 pagesTissue WorksheetFAITH ALBAÑEZNo ratings yet
- CMDA STUDENTS EXAMDocument9 pagesCMDA STUDENTS EXAMEwaoluwa AribaNo ratings yet
- Luteinizing HormoneDocument8 pagesLuteinizing HormoneSaba MalikNo ratings yet