Professional Documents
Culture Documents
Cartilage 2021
Uploaded by
Nhi SV. Phan Ngọc YếnCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cartilage 2021
Uploaded by
Nhi SV. Phan Ngọc YếnCopyright:
Available Formats
C H A P T E R
HYALINE CARTILAGE
Matrix
7 Cartilage
129
130
FIBROCARTILAGE 134
CARTILAGE FORMATION, GROWTH, & REPAIR 134
Chondrocytes 132
SUMMARY OF KEY POINTS 136
Perichondrium 133
ELASTIC CARTILAGE 133 ASSESS YOUR KNOWLEDGE 136
C artilage is a tough, durable form of supporting con-
nective tissue, characterized by an extracellular
matrix (ECM) with high concentrations of GAGs and
proteoglycans, interacting with collagen and elastic fibers.
Structural features of its matrix make cartilage ideal for a vari-
tissue, chondrocytes exhibit low metabolic activity. Cartilage
also lacks nerves.
The perichondrium (Figure 7–2) is a sheath of dense
connective tissue that surrounds cartilage in most places,
forming an interface between the cartilage and the tissues sup-
ety of mechanical and protective roles within the adult skel- ported by the cartilage. The perichondrium harbors the blood
eton and elsewhere (Figure 7–1). supply serving the cartilage and a small neural component.
Cartilage ECM has a firm consistency that allows the Articular cartilage, which covers the ends of bones in movable
tissue to bear mechanical stresses without permanent dis- joints and which erodes in the course of arthritic degenera-
tortion. In the respiratory tract, ears, and nose, cartilage tion, lacks perichondrium and is sustained by the diffusion of
forms the framework supporting softer tissues. Because of oxygen and nutrients from the synovial fluid.
its resiliency and smooth, lubricated surface, cartilage pro- As shown in Figure 7–1, variations in the composition of
vides cushioning and sliding regions within skeletal joints the matrix characterize three main types of cartilage: hyaline
and facilitates bone movements. As described in Chapter 8, cartilage, elastic cartilage, and fibrocartilage. Important fea-
cartilage also guides development and growth of long bones, tures of these are summarized in Table 7–1.
both before and after birth.
Cartilage consists of cells called chondrocytes
(Gr. chondros, cartilage + kytos, cell) embedded in the ECM › ›› MEDICAL APPLICATION
which, unlike connective tissue proper, contains no other cell Many genetic conditions in humans or mice that cause defec-
types. Chondrocytes synthesize and maintain all ECM com- tive cartilage, joint deformities, or short limbs are due to
ponents and are located in matrix cavities called lacunae. recessive mutations in genes for collagen type II, the aggre-
The physical properties of cartilage depend on electro- can core protein, the sulfate transporter, and other proteins
static bonds between type II collagen fibrils, hyaluronan, required for normal chondrocyte function.
and the sulfated GAGs on densely packed proteoglycans.
Its semirigid consistency is attributable to water bound to the
negatively charged hyaluronan and GAG chains extending
from proteoglycan core proteins, which in turn are enclosed ››HYALINE CARTILAGE
within a dense meshwork of thin type II collagen fibrils. The Hyaline (Gr. hyalos, glass) cartilage, the most common of the
high content of bound water allows cartilage to serve as a three types, is homogeneous and semitransparent in the fresh
shock absorber, an important functional role. state. In adults, hyaline cartilage is located in the articular sur-
All types of cartilage lack vascular supplies and chon- faces of movable joints, in the walls of larger respiratory pas-
drocytes receive nutrients by diffusion from capillaries in sages (nose, larynx, trachea, bronchi), in the ventral ends of ribs,
surrounding connective tissue (the perichondrium). In some where they articulate with the sternum, and in the epiphyseal
skeletal elements, large blood vessels do traverse cartilage to plates of long bones, where it makes possible longitudinal bone
supply other tissues, but these vessels release few nutrients to growth (Figure 7–1). In the embryo, hyaline cartilage forms the
the chondrocytes. As might be expected of cells in an avascular temporary skeleton that is gradually replaced by bone.
129
07_Mescher_ch07_p129-137.indd 129 19/03/21 2:39 PM
130 CHAPTER 7 ■ Cartilage
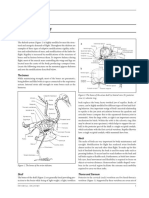
FIGURE 7–1 Distribution of cartilage in adults.
Cartilage in external ear
Extracellular matrix
Epiglottis Cartilages in nose Lacuna
Larynx (with chondrocyte)
Lung
Trachea
Articular cartilage
Perichondrium
of a joint
Costal cartilage 180x
b Hyaline cartilage
Cartilage of
intervertebral disc
Respiratory tract cartilages Perichondrium
in the lungs, trachea,
Elastic fibers
and larynx Pubic symphysis Lacunae
(with chondrocytes)
Extracellular matrix
80x
c Elastic cartilage
Meniscus (padlike
fibrocartilage in
Lacunae
knee joint)
(with chondrocytes)
Extracellular matrix
Collagen fibers
Articular cartilage Hyaline cartilage
of a joint Fibrocartilage
80x
Elastic cartilage
a d Fibrocartilage
(a) There are three types of adult cartilage distributed in many prominent. The photomicrographs show the main features of
areas of the skeleton, particularly in joints and where pliable (b) hyaline cartilage, (c) elastic cartilage, and (d) fibrocartilage.
support is useful, as in the ribs, ears, and nose. Cartilage sup- Dense connective tissue of perichondrium is shown here with
port of other tissues throughout the respiratory tract is also hyaline and elastic cartilage.
› ›› MEDICAL APPLICATION collagen fibrils are barely discernible. Most of the collagen in
hyaline cartilage is type II, although small amounts of minor
Osteoarthritis, a chronic condition that commonly occurs dur- collagens are also present.
ing aging, involves the gradual loss or changed physical proper- Aggrecan (core protein 250 kDa), with approximately
ties of the hyaline cartilage that lines the articular ends of bones 150 GAG side chains of chondroitin sulfate and keratan sul-
in joints. Joints that are weight-bearing (knees, hips) or heavily fate, is the most abundant proteoglycan of hyaline cartilage.
used (wrist, fingers) are most prone to cartilage degeneration. Hundreds of these proteoglycans are bound noncovalently by
Fragments released by wear-and-tear to the articular cartilage link proteins to long polymers of hyaluronan, as shown sche-
trigger secretion of matrix metalloproteinases and other factors matically in Figure 7–2a and discussed in Chapter 5. These
from macrophages in adjacent tissues, which exacerbate dam- proteoglycan complexes biºnd further to the surface of type II
age and cause pain and inflammation within the joint. collagen fibrils (Figure 7–2a). Water bound to GAGs in the
proteoglycans constitutes up to 60%-80% of the weight of
fresh hyaline cartilage.
Matrix Another important component of cartilage matrix is the
The dry weight of hyaline cartilage is nearly 40% collagen structural multiadhesive glycoprotein chondronectin. Like
embedded in a firm, hydrated gel of proteoglycans and struc- fibronectin in other connective tissues, chondronectin binds
tural glycoproteins. In routine histology preparations, the pro- specifically to GAGs, collagen, and integrins, mediating the
teoglycans make the matrix generally basophilic and the thin adherence of chondrocytes to the ECM.
07_Mescher_ch07_p129-137.indd 130 19/03/21 2:39 PM
Hyaline Cartilage 131
FIGURE 7–2 The structure of cartilage matrix and cells.
C H A P T E R
Proteoglycan
Perichondrium
Hyaluronan
Perichondrial
fibroblast
Type II
7
collagen fibril
Cartilage ■ Hyaline Cartilage
Chondroblast
Cartilage
Interterritorial
matrix
Hyaluronan
Link protein Chondrocyte
Core protein
Chondroitin sulfate Territorial
matrix
Collagen (type II)
a b
(a) A schematic representation of the most abundant molecules (b) A diagram of the transitional area between the perichondrium
in cartilage matrix shows the interaction between type II colla- and the cartilage matrix. Fibroblast-like progenitor cells in the
gen fibrils and proteoglycans linked to hyaluronan. Link proteins perichondrium give rise to larger chondroblasts, which divide
noncovalently bind the protein core of proteoglycans to the linear and differentiate as chondrocytes. These functional cells produce
hyaluronan molecules. The chondroitin sulfate side chains of the matrix components and exist in lacunae surrounded by the matrix.
proteoglycan electrostatically bind to the collagen fibrils, forming The ECM immediately around each lacuna, called the territorial
a cross-linked matrix. The circled area is shown larger in the lower matrix, contains mostly proteoglycans and sparse collagen; that
part of the figure. Physical properties of these matrix components more distant from lacunae, the interterritorial matrix, is richer in
produce a highly hydrated, pliable material with great strength. collagen and may be less basophilic.
Approximately 75% of the wet weight of hyaline cartilage is water.
TABLE 7–1 Important features of the major cartilage types.
Hyaline Cartilage Elastic Cartilage Fibrocartilage
Main features of the Homogeneous, with type II collagen Type II collagen, aggrecan, and Type II collagen and large areas
extracellular matrix and aggrecan darker elastic fibers of dense connective tissue with
type I collagen
Major cells Chondrocytes, chondroblasts Chondrocytes, chondroblasts Chondrocytes, fibroblasts
Typical arrangement Isolated or in small isogenous groups Usually in small isogenous groups Isolated or in isogenous groups
of chondrocytes arranged axially
Presence of Yes (except at epiphyses and articular Yes No
perichondrium cartilage)
Main locations or Many components of upper respiratory External ear, external acoustic Intervertebral discs, pubic
examples tract; articular ends and epiphyseal meatus, auditory tube; epiglottis and symphysis, meniscus, and certain
plates of long bones; fetal skeleton certain other laryngeal cartilages other joints; insertions of tendons
Main functions Provides smooth, low-friction surfaces Provides flexible shape and support Provides cushioning, tensile
in joints; structural support for of soft tissues strength, and resistance to
respiratory tract tearing and compression
07_Mescher_ch07_p129-137.indd 131 19/03/21 2:39 PM
132 CHAPTER 7 ■ Cartilage
Staining variations within the matrix reflect local differ- the matrix. In living tissue, chondrocytes fill their lacunae
ences in its molecular composition. Immediately surrounding completely.
each chondrocyte, the ECM is relatively richer in GAGs than Because cartilage matrix is avascular, chondrocytes
collagen, often causing these areas of territorial matrix to respire under low-oxygen tension. Hyaline cartilage cells
stain differently from the intervening areas of interterritorial metabolize glucose mainly by anaerobic glycolysis. Nutrients
matrix (Figures 7–2b and 7–3). from the blood diffuse to all the chondrocytes from the carti-
lage surface, with movements of water and solutes in the carti-
Chondrocytes lage matrix promoted by intermittent tissue compression and
decompression during body movements. The limits of such
Cells occupy relatively little of the hyaline cartilage mass. At diffusion define the maximum thickness of hyaline cartilage,
the periphery of the cartilage, young chondrocytes or chon- which usually exists as small, thin plates.
droblasts have an elliptic shape, with the long axes parallel
to the surface (Figure 7–3). Deeper in the cartilage, they are
round and may appear in groups of up to eight cells that origi- › ›› MEDICAL APPLICATION
nate from mitotic divisions of a single chondroblast and are
In contrast to other forms of cartilage and most other tissues,
called isogenous aggregates. As the chondrocytes become
hyaline cartilage is susceptible to partial or isolated regions of
more active in secreting collagens and other ECM compo-
calcification during aging, especially in the costal cartilage
nents, the aggregated cells are pushed apart and occupy sepa-
adjacent to the ribs. Calcification of the hyaline matrix, accom-
rate lacunae.
panied by degenerative changes in the chondrocytes, is a com-
Cartilage cells and matrix may shrink slightly during
mon part of the aging process and in many respects resembles
routine histologic preparation, resulting in both the irreg-
endochondral ossification by which bone is formed.
ular shape of the chondrocytes and their retraction from
FIGURE 7–3 Hyaline cartilage.
P
P
C C
M
M
C
P
a b
(a) The upper part of the photo shows the perichondrium (P), an (b) The thin region of hyaline cartilage shown here has perichon-
example of dense connective tissue consisting largely of type I drium (P) on both sides and shows larger lacunae containing
collagen. Among the fibroblastic cells of the perichondrium are isogenous groups of chondrocytes (C) within the matrix (M). Such
indistinguishable mesenchymal stem cells. There is a gradual groups of two, four, or more cells are produced by mitosis; the
transition and differentiation of cells from the perichondrium to cells will separate into individual lacunae as they begin to secrete
the cartilage, with some elongated fibroblast-like cells becoming matrix. Territorial matrix immediately around the chondrocytes is
larger and more rounded as chondroblasts and chondrocytes (C). more basophilic than interterritorial matrix farther from the cells.
These are located within lacunae surrounded by the matrix (M) (X160; H&E)
which these cells secreted. (X200; H&E)
07_Mescher_ch07_p129-137.indd 132 19/03/21 2:39 PM
Elastic Cartilage 133
Chondrocyte synthesis of sulfated GAGs and secretion of perichondrium, which is essential for the growth and main-
proteoglycans are accelerated by many hormones and growth tenance of cartilage (Figures 7–2b and 7–3). The outer region
C H A P T E R
factors. A major regulator of hyaline cartilage growth is the of the perichondrium consists largely of collagen type I fibers
pituitary-derived protein called growth hormone or somato- and fibroblasts, but an inner layer adjoining the cartilage
tropin. This hormone acts indirectly, promoting the endocrine matrix also contains mesenchymal stem cells that provide a
release from the liver of insulin-like growth factors, or somato- source for new chondroblasts that divide and differentiate into
medins, which directly stimulate the cells of hyaline cartilage. chondrocytes.
7
› ›› MEDICAL APPLICATION ››ELASTIC CARTILAGE
Cartilage ■ Elastic Cartilage
Cells of cartilage can give rise to either benign (chondroma) or
Elastic cartilage is essentially similar to hyaline cartilage
slow-growing, malignant (chondrosarcoma) tumors in which
except that it contains an abundant network of elastic fibers in
cells produce normal matrix components. Chondrosarcomas
addition to a meshwork of collagen type II fibrils (Figures 7–4
seldom metastasize and are generally removed surgically.
and 7–1c), which give fresh elastic cartilage a yellowish color.
With appropriate staining, the elastic fibers usually appear as
Perichondrium dark bundles distributed unevenly through the matrix.
Except in the articular cartilage of joints, all hyaline car- More flexible than hyaline cartilage, elastic cartilage is
tilage is covered by a layer of dense connective tissue, the found in the auricle of the ear, the walls of the external auditory
FIGURE 7–4 Elastic cartilage.
a b
The chondrocytes (C) and overall organization of elastic cartilage flexibility to this type of cartilage. The section in part b includes
are similar to those of hyaline cartilage, but the matrix (M) also perichondrium (P) that is also similar to that of hyaline cartilage.
contains elastic fibers that can be seen as darker components (a) X160; Hematoxylin and orcein. (b) X180; Weigert resorcin and
with proper staining. The abundant elastic fibers provide greater van Gieson.
07_Mescher_ch07_p129-137.indd 133 19/03/21 2:39 PM
134 CHAPTER 7 ■ Cartilage
canals, the auditory (Eustachian) tubes, the epiglottis, and the
upper respiratory tract. Elastic cartilage in these locations
FIGURE 7–5 Fibrocartilage.
includes a perichondrium similar to that of most hyaline car-
tilage. Throughout elastic cartilage, the cells resemble those of
hyaline cartilage both physiologically and structurally.
››FIBROCARTILAGE C
Fibrocartilage takes various forms in different structures but C
is essentially a mingling of hyaline cartilage and dense connec-
tive tissue (Figures 7–5 and 7–1d). It is found in intervertebral
discs, in attachments of certain ligaments, and in the pubic
symphysis—all places where it serves as very tough, yet cush-
ioning support tissue for bone.
Chondrocytes of fibrocartilage occur singly and often in
aligned isogenous aggregates, producing type II collagen and
other ECM components, although the matrix around these
chondrocytes is typically sparse. Areas with chondrocytes and
hyaline matrix are separated by other regions with fibroblasts
and dense bundles of type I collagen, which confer extra ten- C
sile strength to this tissue (Figure 7–5). The relative scarcity
of proteoglycans overall makes fibrocartilage matrix more aci-
dophilic than that of hyaline or elastic cartilage. There is no
distinct surrounding perichondrium in fibrocartilage.
Intervertebral discs of the spinal column are composed
primarily of fibrocartilage and act as lubricated cushions and
shock absorbers, preventing damage to adjacent vertebrae from
abrasive forces or impacts. Held in place by ligaments, interver-
tebral discs are discussed further with joints in Chapter 8.
Important features of the three major types of cartilage
are summarized in Table 7–1. Fibrocartilage varies histologically in different structures, but
is always essentially a mixture of hyaline cartilage and dense
connective tissue.
››CARTILAGE FORMATION, In a small region of intervertebral disc, the axially arranged
aggregates of chondrocytes (C) are seen to be surrounded by
GROWTH, & REPAIR small amounts of matrix and separated by larger regions with
dense collagen and scattered fibroblasts with elongated nuclei
All cartilage forms from embryonic mesenchyme in the pro- (arrows). (X250; Picrosirius-hematoxylin)
cess of chondrogenesis (Figure 7–6). The first indication
of cell differentiation is the rounding up of the mesenchymal
cells, which retract their extensions, multiply rapidly, and perichondrium (Figure 7–2b). In both cases, the synthesis
become more densely packed together. In general, the terms of matrix contributes greatly to the growth of the cartilage.
“chondroblasts” and “chondrocytes,” respectively, refer to the Appositional growth of cartilage is more important during
cartilage cells during and after the period of rapid prolifera- postnatal development, although as described in Chapter 8,
tion. At both stages, the cells have basophilic cytoplasm rich interstitial growth in cartilaginous regions within long bones
in RER for collagen synthesis (Figure 7–7). Production of the is important in increasing the length of these structures. In
ECM encloses the cells in their lacunae and then gradually articular cartilage, cells and matrix near the articulating sur-
separates chondroblasts from one another. During embryonic face are gradually worn away and must be replaced from
development, the cartilage differentiation takes place primar- within, because there is no perichondrium to add cells by
ily from the center outward; therefore, the more central cells appositional growth.
have the characteristics of chondrocytes, whereas the periph- Except in young children, damaged cartilage undergoes
eral cells are typical chondroblasts. The superficial mesen- slow and often incomplete repair, primarily dependent on
chyme develops as the perichondrium. cells in the perichondrium, which invade the injured area and
Once formed, the cartilage tissue enlarges both by inter- produce new cartilage. In damaged areas, the perichondrium
stitial growth, involving mitotic division of preexisting produces a scar of dense connective tissue instead of forming
chondrocytes, and by appositional growth, which involves new cartilage. The poor capacity of cartilage for repair or regen-
chondroblast differentiation from progenitor cells in the eration is due in part to its avascularity and low metabolic rate.
07_Mescher_ch07_p129-137.indd 134 19/03/21 2:39 PM
Cartilage Formation, Growth, & Repair 135
FIGURE 7–6 Chondrogenesis.
7 C H A P T E R
Cartilage ■ Cartilage Formation, Growth, & Repair
a b c d
The major stages of embryonic cartilage formation, or chondro- various matrix components, which collectively swell with water
genesis, are shown here. and form the very extensive ECM. (d) Multiplication of chondro-
(a) Mesenchyme is the precursor for all types of cartilage. (b) Mito- blasts within the matrix gives rise to isogenous cell aggregates sur-
sis and initial cell differentiation produce a tissue with condensa- rounded by a condensation of territorial matrix. In mature cartilage,
tions of rounded cells called chondroblasts. (c) Chondroblasts are this interstitial mitotic activity ceases and all chondrocytes typically
then separated from one another again by their production of the become more widely separated by their production of matrix.
FIGURE 7–7 Chondrocytes in growing cartilage.
This TEM of fibrocartilage shows chondrocytes with abundant are both present in fibrocartilage. Chondrocytes in growing hya-
RER actively secreting the collagen-rich matrix. Bundles of colla- line and elastic cartilage have more prominent Golgi complexes
gen fibrils, sectioned in several orientations, are very prominent and synthesize abundant proteoglycans in addition to collagens.
around the chondrocytes of fibrocartilage. Collagen types I and II (X3750)
07_Mescher_ch07_p129-137.indd 135 19/03/21 2:39 PM
136 CHAPTER 7 ■ Cartilage
Cartilage SUMMARY OF KEY POINTS
■■ Cartilage is a tough, resilient type of connective tissue that struc- Elastic Cartilage
turally supports certain soft tissues, notably in the respiratory ■■ Elastic cartilage generally resembles hyaline cartilage in its chondro-
tract, and provides cushioned, low-friction surfaces in joints. cytes and major ECM components, but its matrix includes abundant
■■ Cells of cartilage, chondrocytes, make up a small percentage of elastic fibers, visible with special stains, which increase the tissue’s
the tissue’s mass, which is mainly a flexible mass of extracellular flexibility.
matrix (ECM). ■■ Elastic cartilage provides flexible support for the external ear as well
■■ Chondrocytes are embedded within lacunae surrounded by the as certain structures of the middle ear and larynx; it is always sur-
ECM. rounded by perichondrium.
■■ Cartilage ECM typically includes collagen as well as abundant
proteoglycans, notably aggrecan, which bind a large amount of Fibrocartilage
water. ■■ Fibrocartilage contains varying combinations of hyaline cartilage
■■ Cartilage always lacks blood vessels, lymphatics, and nerves, but it in small amounts of dense connective tissue.
is usually surrounded by a dense connective tissue perichondrium ■■ Histologically, it consists of small chondrocytes in a hyaline matrix,
that is vascularized. usually layered with larger areas of bundled type I collagen with
■■ There are three major forms of cartilage: (1) hyaline cartilage, scattered fibroblasts.
(2) elastic cartilage, and (3) fibrocartilage. ■■ Fibrocartilage provides very tough, strong support at tendon inser-
tions and in intervertebral discs and certain other joints.
Hyaline Cartilage
■■ The ECM of hyaline cartilage is homogenous and glassy, rich Cartilage Formation, Growth, & Repair
in fibrils of type II collagen and aggrecan complexes with bound ■■ All forms of cartilage form from embryonic mesenchyme.
water. ■■ Cartilaginous structures grow by mitosis of existing chondro-
■■ The ECM has less collagen and more proteoglycan immediately blasts in lacunae (interstitial growth) or formation of new chon-
around the lacunae, producing slight staining differences in this droblasts peripherally from progenitor cells in the perichondrium
territorial matrix. (appositional growth).
■■ Chondrocytes occur singly or in small, mitotically derived isog- ■■ Repair or replacement of injured cartilage is very slow and
enous groups. ineffective, due in part to the tissue’s avascularity and low
■■ Perichondrium is usually present, but not at the hyaline cartilage metabolic rate.
of articular surfaces or the epiphyses of growing long bones.
Cartilage ASSESS YOUR KNOWLEDGE
1. The molecular basis for the shock absorbing properties of cartilage 5. What is the source of the mesenchymal progenitor cells activated for
involves which of the following? the repair of hyaline cartilage of accident-damaged costal cartilages?
a. Electrostatic interaction of proteoglycans with type IV collagen a. Perichondrium
b. Ability of glycosaminoglycans to bind anions b. Adjacent loose connective tissue
c. Noncovalent binding of glycosaminoglycans to protein cores c. Bone of the adjacent rib(s) and sternum
d. Sialic acid residues in the glycoproteins d. Chondrocytes of the injured cartilage
e. Hydration of glycosaminoglycans e. Stem cells circulating with blood
2. What distinguishes cartilage from most other connective tissues? 6. How does articular cartilage differ from most other hyaline cartilage?
a. Its extracellular matrix is rich in collagen. a. It undergoes mainly appositional growth.
b. Its predominant cell type is a mesenchymal derivative. b. It contains isogenous groups of chondrocytes.
c. Its predominant cell type secretes both fibers and proteoglycans. c. It lacks a perichondrium.
d. It lacks blood vessels. d. Its matrix contains aggrecan.
e. It functions in mechanical support. e. It is derived from embryonic mesenchyme.
3. Which feature is typical of elastic cartilage? 7. Which step occurs first in chondrogenesis?
a. Primary skeletal tissue in the fetus a. Appositional growth
b. No identifiable perichondrium b. Conversion of chondroblasts to chondrocytes
c. Found in intervertebral discs c. Formation of mesenchymal condensations
d. Most widely distributed cartilage type in the body d. Interstitial growth
e. Collagen is mainly type II e. Secretion of collagen-rich and proteoglycan-rich matrix
4. Which area in cartilage is relatively collagen-poor and
proteoglycan-rich?
a. Fibrocartilage
b. Territorial matrix
c. Epiphyseal plate
d. Interterritorial matrix
e. Perichondrium
07_Mescher_ch07_p129-137.indd 136 19/03/21 2:39 PM
Cartilage Formation, Growth, & Repair 137
8. Osteoarthritis is characterized by the progressive erosion of articu- 10. A 66-year-old man who suffered from severe osteoarthritis is
lar cartilage. The matrix metalloproteinases involved in this erosion referred to an orthopedic surgeon for replacement of his right knee.
C H A P T E R
primarily act on which matrix component? He had been actively involved in both high school and intercolle-
a. Aggrecan giate football and had continued running until about the age of 45
b. Link proteins as a form of relaxation and exercise. With the patient’s permission,
c. Network-forming collagen the removed joint is used by investigators performing a proteomic
d. Fibril-forming collagen analysis of different joint tissues. The meniscus was found to contain
e. Chondronectin almost exclusively type I collagen and aggrecan was undetectable.
What is the most likely explanation for this result?
9. A 28-year-old woman visits the family medicine clinic complaining of
7
a. The meniscus normally consists of dense regular connective tis-
loss of the sense of smell, nosebleeds, problems with swallowing, and sue, which contains primarily type I collagen.
Cartilage ■ Cartilage Formation, Growth, & Repair
hoarseness. She admits to “casual, social use” of cocaine on a regular b. The meniscus normally consists of fibrocartilage, which contains
basis since her sophomore year of college. A complete examination of only type I collagen.
her nose with a speculum and otoscope shows severe rhinitis (inflam- c. The meniscus had undergone repeated rounds of repair due to
mation). There is also perforation and collapse of the nasal cartilage wear-and-tear during which its hyaline cartilage component was
resulting in a “saddle nose” deformity. Erosions in the enamel of her replaced by dense connective tissue.
front teeth are noted. The breakdown of the nasal cartilage releases d. Osteoarthritic injury in the knee resulted in the chondrocytes of
collagen fibers primarily of which type? the meniscus switching from expression of genes for type II col-
a. Type I lagen to type I collagen.
b. Type II e. Elastic cartilage is normally replaced by fibrocartilage during
c. Type III aging and this process can be accelerated by exercise.
d. Type IV
e. Type VII
Answers: 1e, 2d, 3e, 4b, 5a, 6c, 7c, 8d, 9b, 10c
07_Mescher_ch07_p129-137.indd 137 19/03/21 2:39 PM
You might also like
- Cranial Vault As A Tensegrity Structure by ScarrDocument21 pagesCranial Vault As A Tensegrity Structure by ScarrTensegrity Wiki100% (1)
- Ankit Pathak: Business AnalystDocument3 pagesAnkit Pathak: Business AnalystBibhuPrakashDasNo ratings yet
- Landscape Architecture: Elements of Garden DesignDocument7 pagesLandscape Architecture: Elements of Garden Designtwinkle4545No ratings yet
- Joint Structure and FunctionDocument87 pagesJoint Structure and Functionjay shah90% (21)
- Cisco Start CatalogDocument4 pagesCisco Start CatalogqntttNo ratings yet
- BUKU 1 HistologiDocument36 pagesBUKU 1 HistologiSewa ScribdNo ratings yet
- Histo Lec Module 4 BookDocument32 pagesHisto Lec Module 4 Bookchuchu lalaNo ratings yet
- Synovialjointslab PDFDocument7 pagesSynovialjointslab PDFmariNo ratings yet
- Safari - Feb 21, 2024 at 12:17 PM 2Document1 pageSafari - Feb 21, 2024 at 12:17 PM 2syansyncNo ratings yet
- CartilageDocument4 pagesCartilageNicole DragoneNo ratings yet
- HISTO LAB Week 1 Bone and CartilageDocument4 pagesHISTO LAB Week 1 Bone and CartilageJennie WatanabeNo ratings yet
- Chapter 7 (Cartilage)Document5 pagesChapter 7 (Cartilage)Jovilyn SilongaNo ratings yet
- Cartilago ArticularDocument8 pagesCartilago ArticularManuel Azael Rodríguez CigalaNo ratings yet
- 1.2 Cartilage and BoneDocument27 pages1.2 Cartilage and BonePema GaleyNo ratings yet
- CARTILAGEDocument24 pagesCARTILAGEEdzeal Bruan JrNo ratings yet
- EDR Kartilago 2018Document20 pagesEDR Kartilago 2018Artha CimutNo ratings yet
- Cartilage: Histology Dr. BernalDocument4 pagesCartilage: Histology Dr. BernalA18- Jessa Mae DayagNo ratings yet
- 08 Cartilage Summary2017Document2 pages08 Cartilage Summary2017Dan ChoiNo ratings yet
- Chapter 7 - CartilageDocument17 pagesChapter 7 - CartilageREMAN ALINGASANo ratings yet
- Zoo115 (Histo) Exer4 (Cart&Bone) EditedDocument6 pagesZoo115 (Histo) Exer4 (Cart&Bone) EditedChristi Lorraine LayogNo ratings yet
- Anatomy - Physiology (Chapter 6 - Skeletal System)Document39 pagesAnatomy - Physiology (Chapter 6 - Skeletal System)Avi ZychNo ratings yet
- Cartilage 2024Document23 pagesCartilage 2024rand200507No ratings yet
- The Basic Science of Articular Cartilage: Structure, Composition, and FunctionDocument8 pagesThe Basic Science of Articular Cartilage: Structure, Composition, and FunctionMonica J Ortiz PereiraNo ratings yet
- Biomechanics of The Flexor TendonsDocument21 pagesBiomechanics of The Flexor TendonsAlejandro PAEZ MONTESNo ratings yet
- Histology 4 Cartilage and BoneDocument61 pagesHistology 4 Cartilage and BoneAbdul RahmanNo ratings yet
- CartilagoDocument40 pagesCartilagoIlham DwiNo ratings yet
- Tendon Injuries - EFORT Open ReviewsDocument23 pagesTendon Injuries - EFORT Open ReviewsAvram GeorgievNo ratings yet
- HistoPath (Lect #4) TransDocument2 pagesHistoPath (Lect #4) TransSherlyn Giban InditaNo ratings yet
- Biomekanik Iv FDC 2020Document23 pagesBiomekanik Iv FDC 2020Nadhia FitriaNo ratings yet
- Histology of Cartilage and BoneDocument15 pagesHistology of Cartilage and BoneDorcus PriyaNo ratings yet
- Cartilage ReviewDocument4 pagesCartilage ReviewClyde BaltazarNo ratings yet
- Internal Anatomy: Skeletal SystemDocument6 pagesInternal Anatomy: Skeletal SystemkarlpdmNo ratings yet
- Lecture: Histology of Cartilage and BoneDocument49 pagesLecture: Histology of Cartilage and BoneStreet Fhigteer AgitatorNo ratings yet
- Biomechanics and Biomaterials in Orthopedic SurgeryDocument11 pagesBiomechanics and Biomaterials in Orthopedic SurgeryManiventhan NachimuthuNo ratings yet
- Combination of Chondrocytes and Chondrons Improves Extrac - 2021 - Journal of orDocument8 pagesCombination of Chondrocytes and Chondrons Improves Extrac - 2021 - Journal of orAkirajane De GuzmanNo ratings yet
- CartilageDocument29 pagesCartilageMASHAL ABDINo ratings yet
- Kirkendall 2007Document5 pagesKirkendall 2007raden chandrajaya listiandokoNo ratings yet
- Skeletal SystemDocument2 pagesSkeletal SystemReslie Joy SerranoNo ratings yet
- C6-Skeletal SystemDocument5 pagesC6-Skeletal SystemLorrine MagramoNo ratings yet
- CartilageDocument37 pagesCartilageFiraol DiribaNo ratings yet
- Support and Movement: I. Human SkeletonDocument9 pagesSupport and Movement: I. Human SkeletonShahzaib AhmedNo ratings yet
- CartilageDocument3 pagesCartilageعلي المحترفNo ratings yet
- Periodontal Ligament: Ganesh Ganji 2 Year PGDocument34 pagesPeriodontal Ligament: Ganesh Ganji 2 Year PGNareshNo ratings yet
- Chapter 6 ANATOMY AND PHYSIOLOGYDocument6 pagesChapter 6 ANATOMY AND PHYSIOLOGYAngela Mae MeriñoNo ratings yet
- Biomechanics of CartilageDocument14 pagesBiomechanics of CartilageYusraNo ratings yet
- CartilageDocument20 pagesCartilageDoctora NourhanNo ratings yet
- Bone Tissue and The Skeletal System: (Hyaline) CartilageDocument3 pagesBone Tissue and The Skeletal System: (Hyaline) CartilageMae CanlasNo ratings yet
- Normal Bone Anatomy and PhysiologyDocument9 pagesNormal Bone Anatomy and PhysiologyindrapratisthaNo ratings yet
- Biomecanica Del Cartilago ArticularDocument43 pagesBiomecanica Del Cartilago ArticularJosue AcostaNo ratings yet
- Skeletal System1Document1 pageSkeletal System1Elisha DienteNo ratings yet
- Flash Cards 2Document7 pagesFlash Cards 2Brian Ernesto Leal NievesNo ratings yet
- Role of RANKL-RANK-osteoprotegerinDocument7 pagesRole of RANKL-RANK-osteoprotegerinsebastian BarrigaNo ratings yet
- Histo Trans 1.4 - Cartilage and BoneDocument6 pagesHisto Trans 1.4 - Cartilage and BonePim AramNo ratings yet
- CH8 Bone: Medullary CavitiesDocument9 pagesCH8 Bone: Medullary Cavitiesdanny olulanaNo ratings yet
- CartilageDocument26 pagesCartilageAbdi Asiis Omar MohamedNo ratings yet
- HISTO - 6 Muscular Tissue (Complete)Document10 pagesHISTO - 6 Muscular Tissue (Complete)Chynna Dela RosaNo ratings yet
- Periodontal LigamentDocument103 pagesPeriodontal Ligamentanukbhatgmail.com anukbhatgmail.comNo ratings yet
- Skeletal MusclesDocument20 pagesSkeletal MusclesDeshmukh KrishnaNo ratings yet
- Special CT-Cartilage and BoneDocument21 pagesSpecial CT-Cartilage and BoneJaniah AllaniNo ratings yet
- Chapter 3: The Skeletal System - Arthrology: Reading: Moore, Dalley, & Agur ObjectivesDocument12 pagesChapter 3: The Skeletal System - Arthrology: Reading: Moore, Dalley, & Agur ObjectivesVarsha SNo ratings yet
- Colágeno en Salud y EnfermedadDocument7 pagesColágeno en Salud y EnfermedadJair NavarroNo ratings yet
- Advanced farriery knowledge: A study guide and AWCF theory course companionFrom EverandAdvanced farriery knowledge: A study guide and AWCF theory course companionNo ratings yet
- Suprachoroidal Space InterventionsFrom EverandSuprachoroidal Space InterventionsShohista SaidkasimovaNo ratings yet
- East Coast Yacht's Expansion Plans-06!02!2008 v2Document3 pagesEast Coast Yacht's Expansion Plans-06!02!2008 v2percyNo ratings yet
- Human Rights RapDocument4 pagesHuman Rights Rapapi-264123803No ratings yet
- List of Affilited CollegesDocument28 pagesList of Affilited Collegesuzma nisarNo ratings yet
- An Introduction To Uhde Oil & Gas: Thyssenkrupp Uhde - Engineering With IdeasDocument40 pagesAn Introduction To Uhde Oil & Gas: Thyssenkrupp Uhde - Engineering With IdeasHany FathyNo ratings yet
- Once Upon A Time A Hawk Feels in Love With A HenDocument2 pagesOnce Upon A Time A Hawk Feels in Love With A HenJeffri Aritonang100% (1)
- Writing Task 2 - Discussion - Opinion EssayDocument7 pagesWriting Task 2 - Discussion - Opinion EssayTonNo ratings yet
- Short VowelDocument3 pagesShort VowelNidzar ZulfriansyahNo ratings yet
- Lindsey Position PaperDocument14 pagesLindsey Position PaperRamil DumasNo ratings yet
- SaviorKitty - (Seven Deadly Sins Series 4) PrideDocument48 pagesSaviorKitty - (Seven Deadly Sins Series 4) PrideMarife LuzonNo ratings yet
- Japanese ScriptDocument67 pagesJapanese ScriptBrat_princeNo ratings yet
- 2017 - Hetherington - Physiology and Behavior - Understanding Infant Eating BehaviourDocument8 pages2017 - Hetherington - Physiology and Behavior - Understanding Infant Eating BehaviourJuan P. CortésNo ratings yet
- IFAS - Presentation - S2Document21 pagesIFAS - Presentation - S2Abinash BiswalNo ratings yet
- ObliCon Reviewer SMDocument111 pagesObliCon Reviewer SMJessa Marie BrocoyNo ratings yet
- Syllabus (Economic Analysis For Business)Document5 pagesSyllabus (Economic Analysis For Business)S TMNo ratings yet
- Indian Knowledge SystemDocument7 pagesIndian Knowledge Systempooja.pandyaNo ratings yet
- Chapter 9 Formulation of National Trade Policies: International Business, 8e (Griffin/Pustay)Document28 pagesChapter 9 Formulation of National Trade Policies: International Business, 8e (Griffin/Pustay)Yomi BrainNo ratings yet
- Gehman Mennonite Church: Let's Walk With Jesus Personally, Locally, and GloballyDocument1 pageGehman Mennonite Church: Let's Walk With Jesus Personally, Locally, and GloballyGehman Mennonite ChurchNo ratings yet
- CHAPTER - 7 Managing Growth and TransactionDocument25 pagesCHAPTER - 7 Managing Growth and TransactionTesfahun TegegnNo ratings yet
- Bernardo Carpio - Mark Bryan NatontonDocument18 pagesBernardo Carpio - Mark Bryan NatontonMark Bryan NatontonNo ratings yet
- Commercial V Social Veil LiftingDocument3 pagesCommercial V Social Veil LiftingMuhammad Aaqil Umer MemonNo ratings yet
- Ec04c0a5 en GBDocument3 pagesEc04c0a5 en GBd228835No ratings yet
- How Does Texting Worsens Our Vocabulary & Writing Skills ?Document10 pagesHow Does Texting Worsens Our Vocabulary & Writing Skills ?Manvi GoelNo ratings yet
- Extended AbstractDocument4 pagesExtended Abstractadi_6294No ratings yet
- Preparation and Practice Answer KeyDocument16 pagesPreparation and Practice Answer KeyHiệp Nguyễn TuấnNo ratings yet
- FY EDC 2020 Decor-Combinations en EASTDocument14 pagesFY EDC 2020 Decor-Combinations en EASTCristian VasileNo ratings yet
- Please DocuSign Youssef ADMISSIONS FORM W ATDocument5 pagesPlease DocuSign Youssef ADMISSIONS FORM W ATyoussefkhalfaoui30No ratings yet
- Kelompok 1 Recount TextDocument11 pagesKelompok 1 Recount TextElvina RahmayaniNo ratings yet