Professional Documents
Culture Documents
Ca Pharmacology
Uploaded by
88annemariOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ca Pharmacology
Uploaded by
88annemariCopyright:
Available Formats
PHARMACOLOGY potency of an agonist. Ex.
Epinephrine and Phenoxybenzamine
Sources of drugs 2. Enzymes and pumps
Animals = insulin ---- pancreas of cows and pigs (Drug-Enzyme Interaction)
Plants = St. John’s Wort ---- for depression Example: Cholinesterase(ASE=enzyme)
Inorganic compounds Inhibitors
Synthetic = E. coli (Inhibiting Pumps)
Example: Reuptake Inhibitors - impulse
Branches of Pharmacology 3. Chemical Interaction
Pharmacodynamics – Drug binding to receptor 4. Altering metabolic Process
Pharmacokinetics – Body reactions to the drugs
Liberation Pharmacokinetics
Absorption 1. Liberation – release of active ingredients
Distribution 2. Absorption – Blood
Metabolism 3. Distribution
Excretion 4. Metabolism(Biotransformation) – ex. 500mg
Oral – going to liver- from liver release new
Rights of Drug Administration drug 400mg less active also called First Pass
Right Drug Effect
Right Dose 5. Excretion – kidneys, feces, lungs, Skin
Right Patient Routes of Drug Absorption
Right Time 1. Enteral Route - GIT
Right Route Oral, Rectal (fastest route), Nasogastric
2. Parenteral – IV, SQ, IM, ID
Right Documentation
3. Transmucosal – Sublingual, Inhalation, Topical
Right education
Right to refuse
Dose
Right assessment
Amount of drug to be administer
Right Evaluation
Schedule
Frequency, how many doses per day
Pharmacodynamics
Recommended dose
Actions of drug
Right amount + Right schedule
Replacement a missing substance – Insulin,
Critical Concertation
Cortisol. T4, T3.
level of drug in the blood which produces a
Increase Cellular activities – Epinephrine
therapeutic effect.
Depress cellular activities – Beta blockers
Therapeutic Effect
Interfere with growth of a foreign cell -
favorable response after a treatment of any
Antibiotic
kind
Drug actions maybe through
Loading Dose
1. Receptors (Drug-Receptors Interaction)
Initial dose, immediate response
Example: Autonomic Drugs
Agonist – stimulate High than recommended dose
Antagonist: Giving during emergency cases.
Competitive antagonist – Binds to a Half life
same Receptor, Potency of an agonist Time it takes for a drug to become half of its
is reduced. Ex. Diazepam and previously peaked level.
Flumazenil.
Non Competitive antagonist – Binds
to a different receptor, prevent
Dosage forms of Drugs Neurotransmitters
A. Solid Chemicals in the body acting as “Messengers”
1. Tablets: Acetylcholine (ACH)
Scored Muscle contraction
Layered (2 or more chemicals tablet) Memory
Enteric-Coated (tablets not dissolved in Bipolar. Alzheimer’s Disease
stomach but in ab alkaline environment) Norepinephrine and Epinephrine (NE/E)
Chewable – liquid forms are better Catecholamine (NE, E, D) released by
absorbed. nerves in the SNS
Sustained-Release – liberation and Depression
absorption is delayed and not at the same Schizophrenia, Mania.
time. Depression, ADHD
2. Capsule: Dopamine (DOPA)
Hard gel Coordination of impulses and responses
Soft gel Cognitive behavior (thinking, learning,
3. Lozenges reasoning)
Antiseptic action – Destroy the bacteria Schizophrenia, Mania.
Anesthetic action – Relieve pain Depression, Parkinson’s, ADHD
B. Liquid Serotonin (5HT)
1) Syrup For arousal and sleep
Sugar and clear and flavor In preventing depression
For kids Promotes motivation
2) Suspension Chocolate, Banana
Shake before use Schizophrenia, Depression
3) Elixir
Contains alcohol Gamma-aminobutyric Acid (GABA)
Cause drowsiness Inhibitory nerve activity
Avoid driving and operating machine Prevents over excitability or stimulation
C. Topical such as seizure activity
I. Ointment Treat Seizures, anti-convulsant drug
Oil based
For dry lesion Cholinergic Nerves
II. Cream A nerve produces, stores and releases
Water based Acetylcholine (ACH)
Wet lesion Adrenergic Nerves
III. Lotion A nerve producing epinephrine, norepinephrine
Used if the lesion is extensive Produce in the adrenal medulla.
IV. Patch Dopaminergic Nerves
Apply over dry and none a nerve producing dopamine.
irritation areas
Rotate sites – irritation Autonomic Nervous System
Includes two neurotransmitters:
Nervous System
Norepinephrine and Acetylcholine
Two Branches:
1. Sympathetic – Adrenergic Nervous System.
Ex. NE=Adrenaline
2. Parasympathetic – Cholinergic
Ex. Acetylcholine
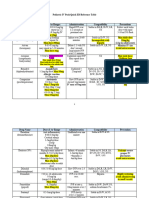
ANS Sympathetic Parasympathetic Cholinergic agonist to BV = vasodilation
Response to: + HR, - HR, Contractility Adrenergic antagonist to GIT = diarrhea
Heart Contractility
Lungs, Bronchus RR – Bronchoconstriction OR: Atropine – Anticholinergic drug
Bronchodilation
Lessen the secretion
Pupils Dilate: Mydrasis Constrict: Meiosis Decrease risk of aspiration
GIT (blood flow, Constipation Diarrhea
motility, ADRENERGIC
secretions) (receptor)
Kidney - Urine formed + urine formed Alpha (a) Beta (B)
Blood flow
Urinary Bladder Relax Contract A1 A2 B1 B2
Sphincter Contract Relax
Detrusor Urinary CNS Nerve Heart Lungs
muscle Retention of Emptying of bladder Bladder Membrane +HR, bronchodilati
Urine Sphincter – decrease NE +contractility on
Blood Vessels Vasoconstriction Vasodilation Closes: Release
Retention Potassium
( smooth
Weakens Enters Cell -
muscle)
SNS antiarrhythm
ic
PSNS
Sympathetic = SNS = Adrenergic Blood Vessels Pancreas Kidney Uterus -
Agonist = stimulate - decrease +Renin relaxation
Vasoconstricti insulin Release,
Mimetic = copy on release. increase BP
Sympathomimetic to bronchus = increase HR Hyperglycem
ia
Sympathomimetic to GIT = bronchodilation
Iris – Dilation: BV of heart,
Sympathomimetic to bladder = retention Mydriasis Lung &
Sympathomimetic to BV = vasoconstriction Skeletal
Sympathomimetic to blood flow = decrease muscle -
vasodilation
Liver –
Parasympathomimetic to GIT = Diarrhea Glycogenolysi
Parasympathomimetic to BV = vasodilation s
Hyperglycemi
Parasympathomimetic to pupils = meiosis a
Parasympathomimetic to bronchus =
bronchoconstriction AGONIST
Parasympathetic = PSNS = Cholinergic Alpha 1 Adrenergic Agonist
Antagonist = Block
Lytic = block, Destroy, Dissolve Phenylephrine
Decongestant
Sympatholytic to pupils = meiosis Allergic rhinitis – vasoconstriction – blood flow
Sympatholytic to BV = vasodilation decrease – reduce o2 and nutrients to cells –
Sympatholytic to bladder = emptying Shrink
Sympatholytic to heart = decrease HR Eye exam
Sympatholytic to bronchus = bronchoconstriction Midodrine
DOC for orthostatic hypotension
Parasympatholytic to pupils = mydriasis
Vasoconstriction – increases TPR – Increase BP
Parasympatholytic to GIT = constipation
Adrenergic agonist to heart = increase HR
Alpha 2 Adrenergic Agonist Alfuzosin
Urinary bladder Emptying bladder BPH
Clonidine (Catapres) Tamsulosin
Decrease BP For BPH
Methyldopa
Beta Adrenergic Blockers Drugs
Beta 1 Adrenergic Agonist Indications:
Use for HPNde. HRdec. BP
Dobutamine Use for ANGINA: -O2 supply, +O2 demand,
Synthetic dopamine Goal: +O2 suppy, -O2 demand
CHF (congested heart failure) Decrease HR workload of heart decreaseO2
Sympathomimetic drug demand decreaseO2 supply increase
Side effects: palpitation, hypertension MI
Supraventricular Arrhythmia, Atrial FIB
Beta 2 Adrenergic Agonists CHF (cautious)
Decrease HRdecrease workload of
Albuterol/Salbutamol heartincrease of contraction
Bronchodilation Anxiety (Propranolol)
used for Asthma, COPD Tremors and palpitationdecrease HR
Side effect: Palpitation, tremors (B2> B1) Migraine
Open-Angle Glaucoma (Betaxol, Timolol)
Terbutaline Side Effects Contraindication Nursing M.
Used in asthma and COPD Bradycardia Monitor HR Hold if HR
Used in premature labor: Tocolytic <60/min
Hypotension Monitor BP Hold if BP
Isosuxprine <90/60
Tocolytic mmHg
Bronchoconstriction Monitor BS Avoid
asthma,
ANTAGONIST
COPD
Hypoglycemia Monitor BS Caution in
Alpha Adrenergic Antagonist
DM
Impotence
Phentolamine
Use for hypertensive crisis due to: Beta 1-Selective Adrenergic Blockers Drugs
Pheochromocytoma (tumor in adrenal medulla, Bisoprolol, Betaxolol
increase NE cause Hypertension) and MAOI’s Esmolol
(MAO break down NE)
Acebutolol, Atenolol
Metoprolol
Alpha 1 Adrenergic Antagonist
Propanolol
Prazosin
Use for tachycardia and tremors in
Blood vessels vasodilation decrease TPR
hypertyroidism
Hypertension
Doxazosin & Terazosin
CHOLINERGIC receptors
Blood Vessel Vasodilation decrease TPR
HPN
Muscarinic Agonist to Pupils = Meiosis
Urinary Bladder Emptying bladder BPH Antinicotinic to Bladder = retention
(Benign Prostatic hypertrophy)
CHOLINERGIC (Receptors)
Muscarinic Nicotinic
M1 M2 M3 M4 M5 N1 or N2 or Nn
Nm
CNS Heart Smooth CNS CNS NMJ Autonomic
Muscle Ganglia
Gastric
Parietal CNS
Cells
Adrenal
Autono Medulla
mic
Ganglia
Myasthenia Gravis
Autoimmune Antibody Antigen (foreign
body)
Attacking receptors
Paralysis – descending paralysis
Sign & Symptoms
Ptosis = initial sign. Check palpebral fissure
Diplopia – Double vision
Mask like facial expression
Dysphagia - Risk for aspiration
Weakening of Laryngeal Muscles
Respiratory Muscle Weakness - lead to
respiratory arrest. Prepare at bedside
tracheostomy set
Nursing Priorities
Airway, Dysphagia (aspiration), Immobility
Treatment:
Neostigmine
Pyridostigmine
Edrophonium – Chloride (tensilon) for
diagnostic
Diagnostic Test:
Tensilon Test: Edrophonium Chloride
(Cholinergic drug), IV
MYASTHENIC CHOLINERGIC
CRISIS CRISIS
S/Sx Weakness, Weakness,
paralysis Paralysis
Cause Under dose of Overdose of
cholinergic drug cholinergic drug
Tx Cholinergic Anticholinergic
drugs drugs (
Atropine)
You might also like
- Addicted to Energy Deficit - Your Neuroscience Based Guide to Restrictive Eating DisordersFrom EverandAddicted to Energy Deficit - Your Neuroscience Based Guide to Restrictive Eating DisordersNo ratings yet
- PharmaDocument5 pagesPharmaIrish RonquilloNo ratings yet
- PharmacologyDocument7 pagesPharmacologyIrish RonquilloNo ratings yet
- Pharmacology NotesDocument21 pagesPharmacology NotesmariaNo ratings yet
- PHARMACOLOGYDocument21 pagesPHARMACOLOGYAllisson BeckersNo ratings yet
- Pharmacology (Laden Saleh) FinalDocument235 pagesPharmacology (Laden Saleh) FinalLaden SalehNo ratings yet
- PharmacologyDocument5 pagesPharmacologyCassandra NicoleNo ratings yet
- Nootropics - Smart Drugs Cheat Sheet: by ViaDocument6 pagesNootropics - Smart Drugs Cheat Sheet: by ViaRajaNo ratings yet
- Pharmacology Week 2 Cheat Sheet: by ViaDocument4 pagesPharmacology Week 2 Cheat Sheet: by ViaVijungcoNo ratings yet
- PHARMACOLOGY Week 1Document13 pagesPHARMACOLOGY Week 1Bee LeriosNo ratings yet
- Pharmacology LecDocument37 pagesPharmacology LecAIRA BIANCA B. MANALANGNo ratings yet
- PharmacologyDocument20 pagesPharmacologyKan JiNo ratings yet
- Irritability: Figure 1: MimosaDocument5 pagesIrritability: Figure 1: MimosaSabita SinghNo ratings yet
- Levetiracetam Drug StudyDocument2 pagesLevetiracetam Drug Studykaycelyn jimenez50% (2)
- Pharma Trans 1 PHARMA, TOXI, DYNA, THERADocument7 pagesPharma Trans 1 PHARMA, TOXI, DYNA, THERAFiel Virata 許慧安No ratings yet
- Drug Study 5Document4 pagesDrug Study 5Butts McgeeNo ratings yet
- Pharmacology in NursingDocument1 pagePharmacology in NursingJessa Mae Barquilla100% (1)
- (LEGMED-FM-PPT) 2.04b Dangerous Drugs PDFDocument134 pages(LEGMED-FM-PPT) 2.04b Dangerous Drugs PDFAl Giorgio SyNo ratings yet
- Notes of Control and CoordinationDocument6 pagesNotes of Control and CoordinationVipul BullaNo ratings yet
- Basic PharmacologyDocument32 pagesBasic PharmacologyJames PerianayagamNo ratings yet
- Forchem Chapter 6Document3 pagesForchem Chapter 6Russelie MarianoNo ratings yet
- Autacoids PharmacologyDocument47 pagesAutacoids PharmacologyZora DNo ratings yet
- Clinical Veterinary PharmacologyDocument4 pagesClinical Veterinary PharmacologyLaureece Salm ApduhanNo ratings yet
- Antiemetic Drugs: PHR Sangita ShakyaDocument26 pagesAntiemetic Drugs: PHR Sangita ShakyaCurex QANo ratings yet
- Drug Delivery System: IntroductionDocument4 pagesDrug Delivery System: IntroductionPamelaFNo ratings yet
- Drug Study: Atropine: RecommendedDocument6 pagesDrug Study: Atropine: RecommendedShara Lailanie A. AzisNo ratings yet
- PHARMAfdDocument7 pagesPHARMAfdJobelle AcenaNo ratings yet
- DRUG EDUCATION and VICE MIDTERMSDocument14 pagesDRUG EDUCATION and VICE MIDTERMSCATHLEENE MAYNE BELIRANNo ratings yet
- Drugs and Alcohol AbuseDocument12 pagesDrugs and Alcohol AbuseSaumya GopalNo ratings yet
- Pharmacodynamics BDS97Document42 pagesPharmacodynamics BDS97Dr.U.P.Rathnakar.MD.DIH.PGDHM100% (2)
- 7779087Document65 pages7779087MohamedNo ratings yet
- Drug Induced VomitingDocument5 pagesDrug Induced VomitingnimasNo ratings yet
- Drug ClassificationDocument8 pagesDrug ClassificationMachi CamzNo ratings yet
- I. Drug Study: Drug Mechanism of Action Indications Contraindication Side Effects Nursing ConsiderationsDocument3 pagesI. Drug Study: Drug Mechanism of Action Indications Contraindication Side Effects Nursing Considerationscyn yana0723No ratings yet
- Multi Functional Drugs - A Novel Concept For Psycho PharmacologyDocument3 pagesMulti Functional Drugs - A Novel Concept For Psycho Pharmacologyrocsa11No ratings yet
- Practical PharmacologyhjhjhDocument9 pagesPractical PharmacologyhjhjhMonzer AchtarNo ratings yet
- Doxofylline Drug StudyDocument2 pagesDoxofylline Drug StudyArabelle GO67% (3)
- Satyanand Sahu (Narcotic and Non - Narcotic Analgesic)Document44 pagesSatyanand Sahu (Narcotic and Non - Narcotic Analgesic)Satyanand SahuNo ratings yet
- Drug Addiction: Physical Dependence Is A State of Adaptation of The Organism To The Presence of The Drug and IsDocument9 pagesDrug Addiction: Physical Dependence Is A State of Adaptation of The Organism To The Presence of The Drug and IsMehar KhanNo ratings yet
- Drugs FOR Psychiatric & Neurologic Disorders: Clonazepam (Klonopin, Rivotril) Midazolam (Versed, Dormicum)Document5 pagesDrugs FOR Psychiatric & Neurologic Disorders: Clonazepam (Klonopin, Rivotril) Midazolam (Versed, Dormicum)Noriko MatsumotoNo ratings yet
- Lecture 2 DrugDocument6 pagesLecture 2 DrugDuran JustineNo ratings yet
- Drug LiteratureDocument3 pagesDrug LiteratureAng, Rico GabrielNo ratings yet
- Dangerous Drugs ReportDocument17 pagesDangerous Drugs ReportAngela PototNo ratings yet
- Pharmacology - PrelimsDocument9 pagesPharmacology - PrelimsLou KristofferNo ratings yet
- Pharma Module 3Document65 pagesPharma Module 3Amy LuglugNo ratings yet
- PcolDocument3 pagesPcolkimkaigel6No ratings yet
- Reviewer Psychia FinalsDocument28 pagesReviewer Psychia FinalsTherese PagayNo ratings yet
- Intro + Pharmacodynamics 2Document46 pagesIntro + Pharmacodynamics 2Dana E AbuqaudNo ratings yet
- 1 Semester: Anti-Migraine Agents Are Used To Treat Migraine HeadachesDocument26 pages1 Semester: Anti-Migraine Agents Are Used To Treat Migraine HeadachesMARY BERNADETTE EGANANo ratings yet
- Pharma NotesDocument38 pagesPharma NotesJose Luis AlmonedaNo ratings yet
- A Brain On Cannabinoids The Role of Dopamine in Reward SeekingDocument14 pagesA Brain On Cannabinoids The Role of Dopamine in Reward SeekingJoão MaiaNo ratings yet
- Barbiturates: Presented by Rasel Mahbub & Ananta SutradharDocument24 pagesBarbiturates: Presented by Rasel Mahbub & Ananta SutradharfarihazmiNo ratings yet
- Clinical PharmacologyDocument51 pagesClinical PharmacologyNARESH JANDIALNo ratings yet
- Repeated Administration: Drug Mechanisms Drug EffectsDocument13 pagesRepeated Administration: Drug Mechanisms Drug EffectsAbraham WalkthewokNo ratings yet
- Unit #1 IntroductionDocument22 pagesUnit #1 IntroductionSaima VictorNo ratings yet
- Jornal Homeopatia HagilDocument4 pagesJornal Homeopatia HagilViviane CollodaNo ratings yet
- Sedative and HypnoticsDocument37 pagesSedative and Hypnoticsprajyot khedekarNo ratings yet
- Vii. Drug Study: Parkinsonis M. Pheochrom Ocytoma (Risk of Hypertensiv e Crisis)Document5 pagesVii. Drug Study: Parkinsonis M. Pheochrom Ocytoma (Risk of Hypertensiv e Crisis)Darwin AndalNo ratings yet
- Ncma216 PrelimDocument44 pagesNcma216 Prelimroldanmarygrace023No ratings yet
- Ilegal DrugsDocument40 pagesIlegal DrugsCabagan IsabelaNo ratings yet
- Tot 3 indicatii-de prescris - копияDocument1 pageTot 3 indicatii-de prescris - копияRenata ProsutinskaiaNo ratings yet
- Drug AbuseDocument13 pagesDrug AbuseLydah Trina RodriguezNo ratings yet
- Daftar Obat BPJSDocument2 pagesDaftar Obat BPJSNurtaty lamba sangganiNo ratings yet
- Pediatric IV Push Quick ED Reference TableDocument4 pagesPediatric IV Push Quick ED Reference TableTayyab RazaNo ratings yet
- ZavzpretDocument21 pagesZavzpretNeethu Anna StephenNo ratings yet
- Ati Pharmacology Study GuideetsyDocument49 pagesAti Pharmacology Study GuideetsyKarima Jones100% (4)
- Rko Puskesmas 2022 Fix OkeDocument39 pagesRko Puskesmas 2022 Fix OkeFormanNo ratings yet
- Pharmacology A ReviewDocument13 pagesPharmacology A ReviewCheriz LukbanNo ratings yet
- Stok Amp Per 17.09.2022Document70 pagesStok Amp Per 17.09.2022Inna TrissNo ratings yet
- Food and Drug Interactions NotesDocument8 pagesFood and Drug Interactions NotesSUDHEER SNo ratings yet
- Nama Zat Aktif BSO Dan Kekuatan Nama Produk (Merk Produsen Amatidin AsiklovirDocument1 pageNama Zat Aktif BSO Dan Kekuatan Nama Produk (Merk Produsen Amatidin AsiklovirGustika AzharNo ratings yet
- Act 2 NotesDocument3 pagesAct 2 NotesNina CasasNo ratings yet
- Management of MedicationDocument9 pagesManagement of MedicationAnirban RoyNo ratings yet
- Antibiotic Renal DoseDocument13 pagesAntibiotic Renal DoseKhor Chin PooNo ratings yet
- Form Stock Opname 2016Document69 pagesForm Stock Opname 2016Windi Astika YuniartiNo ratings yet
- Padmaja Devi - FEMALE - 62 Yrs APJ1.0013308310 1779459Document2 pagesPadmaja Devi - FEMALE - 62 Yrs APJ1.0013308310 1779459John DaveNo ratings yet
- HARGA Apotek Al LatifDocument12 pagesHARGA Apotek Al LatifMarogi Al AnsorianiNo ratings yet
- Spesialit Asma, Batuk, DekongestanDocument4 pagesSpesialit Asma, Batuk, DekongestanS AnindahYaniNo ratings yet
- Classification of Drugs Based On PreparationDocument4 pagesClassification of Drugs Based On PreparationMile ArsicNo ratings yet
- Artificialsnr 1 XyDocument440 pagesArtificialsnr 1 XyAnonymous diiOgjtNo ratings yet
- Drugs That May Cause Mental ConfusionDocument2 pagesDrugs That May Cause Mental ConfusionohnoitsjohnnyNo ratings yet
- Artikuj Pa 20%Document30 pagesArtikuj Pa 20%Beso BurrjaNo ratings yet
- M6 Pharmaceutical LabelsDocument23 pagesM6 Pharmaceutical Labelscbun22222No ratings yet
- Daftar Obat & BMHP Hampir EdDocument2 pagesDaftar Obat & BMHP Hampir EdIshma Yasmin NabillaNo ratings yet
- DocumentDocument146 pagesDocumentotoongulalaNo ratings yet
- Shop - Hemiacosmetics Topical Hair Loss SolutionsDocument1 pageShop - Hemiacosmetics Topical Hair Loss SolutionsYAZLi iNo ratings yet
- DesoxypipradrolDocument4 pagesDesoxypipradrolMarcNo ratings yet
- Sympathomimetics Physical MCQDocument4 pagesSympathomimetics Physical MCQMohamed MoustafaNo ratings yet
- Chapter 021 QuestionsDocument29 pagesChapter 021 QuestionsPrecilou Cutanda100% (1)
- GP MCQ 11Document4 pagesGP MCQ 11Marta MoreiraNo ratings yet