Professional Documents
Culture Documents
Tissue Biochemistry Chapter
Uploaded by
Maria Arshad0 ratings0% found this document useful (0 votes)
43 views25 pagesbiochemistry of tissues
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentbiochemistry of tissues
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
43 views25 pagesTissue Biochemistry Chapter
Uploaded by
Maria Arshadbiochemistry of tissues
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 25
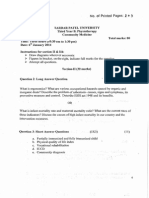
Tissue Biochemistry
DPT 4th Semester
INTRODUCTION
Extracellular Matrix (ECM) are collection of extracellular molecules secreted
by cells that provides structural and biochemical support to the surrounding
cells. They are substances containing Collagen, Elastin, Proteoglycans,
Glycosaminoglycans and fluid produced by the cells they are embedded.
They fill the spaces between the cells in a tissue protecting them and holding
them together. They are the natural support Structures of the cells. The
extracellular matrix may be semifluid or rigidly solid and hard as in bone.
Each type of connective tissue in animals has a type of ECM: collagen fibers
and bone mineral comprise the ECM of bone tissue; reticular fibers and
ground substance comprise the ECM of loose connective tissue; and blood
plasma is the ECM of blood. Some common function of the Extracellular
Matrix includes cell adhesion; cell-to-cell communication and cell
differentiation.
PHYSICAL STRUCTURES OF THE
EXTRACELLULAR MATRIX
• They may be semifluid or rigidly solid and hard as in bone.
• They are network of proteins and carbohydrates that surrounds the
cells and fill the intercellular spaces.
• They are composed of an interlocking mesh of Fibrous proteins and
Glycosaminoglycans (GAGs).
COMPOSITION OF THE EXTRACELLULAR
MATRIX.
Because multicellularity evolved independently in different
multicellular lineages, the composition of ECM varies between
multicellular structures. However, the two main Classes of molecules
that make up the Extracellular Matrix are Fibrous Proteins and
Proteoglycans, other molecules include Water, Electrolytes and
Minerals. These Components are produced and organized by the Cells
that are embedded within them. They Fibroblast (Fiber making cells)
are commonly charged with this responsibility. There are four principles
classes of Fibrous Protein found in the Extracellular Matrix namely;
Collagen, Elastin, Fibronectin and Laminin. Proteoglycans are composed
of Protein core surrounded by long chains of Starch-like molecules
called Glycosaminoglycans (GAG). Let’s take a look at these Molecules.
COLLAGEN
Collagens are strong stretch resistant
fibers that provide tensile strength to the
tissues. They are the most
abundant proteins in the
human body and are the
principle constituent of the
tendons and ligament. They
are also known to provide
support to the skin and help
in wound healing.
ELASTINS
Elastin is a stretchy and resilient
protein that gives elasticity to the
tissues, allowing them to stretch
when needed and then return to
their original state. They are
useful in blood vessels,
the lungs, and skin and these
tissues contain high amounts of
Elastin. They are synthesized
by fibroblasts and smooth
muscle cells.
FIBRONECTIN
Fibronectins are glycoprotein that connect cells with collagen fibers in the
Extracellular Matrix, allowing cells to move through the Matrix. Fibronectins
bind collagen and cell surface integrins,
causing a reorganization of the
cell’s cytoskeleton to facilitate cell movement.
Fibronectins are secreted by cells in an unfolded,
inactive form. Binding to integrins unfolds
Fibronectin molecules, allowing them to form
dimers so that they can function properly.
Fibronectins also help at the site of tissue injury by binding to platelets
during blood clotting and facilitating cell movement to the affected area
during wound healing.
LAMININ
Laminins are proteins found in the basal laminae of virtually all
animals. They form sheet-like network that serves as the “glue”
between dissimilar tissues. They also assist in cell adhesion.
Laminins bind other ECM components such as collagens,
nidogens, and entactins. Laminin
are the principle proteins in the
basement membrane. Basement
membranes are sheet-like
depositions of ECM on which
various epithelial cells rest
Glycosaminoglycan
• Glycosaminoglycans are large complexes of negatively charged
heteropolysaccharides chains
• They have the ability to bind large amount of water. Thereby,
producing the gel like matrix that form the basis of ECM.
• They are generally associated with small amount of protein, forming
proteoglycans ,which typically consist of 95% of carbohydrate.
Importance of glycosaminoglycans
• The hydrated glycosaminoglycans serve as a flexible support for the
ECM .
• They interact with the structural and adhesive protein ,and as a
molecular sieve , influencing movement of material through the ECM.
• The viscous , lubricating properties of mucous secretion also result
from the presence of glycosaminoglycans ,which led to the original
naming of these compounds as mouco polysaccharides.
• Glycosaminoglycans binds with water produces gel like matrix form
the basis body ground substance which along with fibrous structural
proteins such as collagen and elastin , and adhesive proteins such as
fibronectin ,make up the extracellular matrix.
PROTEOGLYCANS
Proteoglycans are a combination of
proteins and Glycosaminoglycans.
Glycosaminoglycans (GAGs)
are carbohydrate polymers and are
usually attached to extracellular matrix
proteins to form Proteoglycans.
Proteoglycans have a net negative
charge that attracts positively charged
sodium ions (Na+), which attracts water
molecules via osmosis, keeping the ECM
and resident cells hydrated.
Proteoglycans may also help to trap and
store growth factors within the ECM
MACHANICAL PROPERTIES OF THE
EXTRACELLULAR MATRIX
The ECM can exist in varying degrees of stiffness and elasticity, from
soft brain tissues to hard bone tissues, the elasticity of the ECM can
differ by several orders of magnitude. This property is primarily
dependent on collagen and elastin concentration, and it has recently
been shown to play an influential role in regulating numerous cell
functions. Cells can sense the mechanical properties of their
environment by applying forces and measuring the resulting backlash.
This plays an important role because it helps regulate many important
cellular processes including cellular contraction, cell migration, cell
proliferation, differentiation and cell death (apoptosis).
Bone & its ECM
• What is bone for?
• Support - bones make up a structural framework for the body, and
provide attachment sites for muscles.
• Protection - protection of internal organs - i.e. brain, heart and lungs,
• Assisting movement.
• Mineral homeostasis - the bone is a store for calcium and
phosphorus
• Blood cell production - takes place in the bone marrow.
What is bone made up of?
• Bone is a strong, flexible and semi-rigid supporting tissue. It can
withstand compression forces, and yet it can bend. Like cartilage, and
other types of connective tissue, bone is made up
of Cells and Extracellular matrix:
• Cells - which in bone are called osteoblasts and osteocytes, (osteo -
bone). There are also two other cell types: osteoprogenitor
cells and osteoclasts.
ECM of Bone
• Extracellular matrix, which is made up of an organic matrix (30%) containing
proteoglycans (but less than cartilage), glycosaminoglycans, glycoproteins, osteonectin
(anchors bone mineral to collagen) and osteocalcin (calcium binding protein). There are
collagen fibres (mostly type I (90%), with some type V). Only 25% of bone is water.
Almost 70% of bone is made up of bone mineral called hydroxyapatite.
• Before the extracellular matrix is calcified, the tissue is called osteoid (bone-
like) tissue. When the concentrations of calcium and phosphate ions rise high enough,
they are deposited into the extracellular matrix, and the bone calcifies. Impaired
calcification (i.e. in diseases such as rickets) leads to higher levels of osteoid tissue than
normal. Calcification occurs only in presence of collagen fibers - salts crystallize in the
spaces between the fibers, then accumulate around them.
• Bone is resistant to bending, twisting, compression and stretch. It is hard, because it is
calcified, and the collagen fibers help the bone to resist tensile stresses. If you dissolve
away the calcium salts of bone, then the bone becomes rubbery because of the collagen
fibers which are left behind.
Types of bone:
• The first bone formed at any site is woven (or primary) bone, but this is soon replaced
by lamellar bone. In woven bone the collagen fibres are random. In lamellar bone, the
collagen fibres have become re-modelled to become more parallel - in layers.
• There are two types of mature bone:
• 1. Compact - which is found in the shafts of long bones (in the diaphyses). This makes up
80% of all bone.
• 2. Spongy (cancellous) bone - which is found at the ends of long bones (in the epiphysis).
This makes up 20% of all bone. This type of bone contains red bone marrow and a
network of bony trabeculae.
• A 'periosteum' is found on the outside of bone. This is a dense fibrous layer, where
muscles insert. It contains bone forming cells. It is not found in the regions of bone
covered by articular cartilage.
• The endosteum is the name given to the tissue that lines the inner surfaces of bones.
Growth and nourishment of bone.
• Unlike cartilage, bone has a very good blood supply. Bone is riddled with blood
capillaries. The central cavity contains blood vessels and is a storage for bone
marrow. All of the osteocytes in bone are within 0.2mm of a capillary. The tissue
fluid from the capillary reaches the osteocytes though canaliculi.
• There are two ways in which bone can grow:
• Endochondral - formation of bone onto a temporary cartilage model or scaffold.
• Intramembranous - formation of bone directly onto fibrous connective tissue.
There is no intermediate cartilage stage. This type of ossification occurs in a few
specialised places such as the flat bones of skull (i.e. parietal bone), mandible,
maxilla and clavicles. Mesenchyme cells differentiate into osteoprogenitor cells,
then into osteoblasts, which secrete the bone matrix. Once the osteoblasts are
embedded in the bone matrix, they are known as osteocytes.
Teeth & its ECM
• Dental pulp is an unmineralized oral tissue composed of soft connective tissue, vascular,
lymphatic and nervous elements that occupies the central pulp cavity of each tooth. Pulp
has a soft, gelatinous consistency. The majority of pulp (75-80%) is water. Aside from the
presence of pulp stones, found pathologically within the pulp cavity of aging teeth, there
is no inorganic component in normal dental pulp. There are a total of 32 pulp organs in
adult dentition. The pulp cavities of molar teeth are approximately four times larger than
those of incisors.
• The pulp cavity extends down through the root of the tooth as the root canal which
opens into the periodontium via the apical foramen. The blood vessels, nerves etc. of
dental pulp enter and leave the tooth through this foramen. This sets up a form of
communication between the pulp and surrounding tissue - clinically important in the
spread of inflammation from the pulp out into the surrounding periodontium.
• Developmentally and functionally, pulp and dentin are closely related. Both are products
of the neural crest-derived connective tissue that formed the dental papilla.
Components of dental pulp
Components of dental pulp
• CELLS (odontoblast, fibroblast,undifferentiated cell, macrophage,
dendritic cell)
• FIBERS AND GLYCOPROTEIN (collagen type I, III, no elastic fiber,
fibronectin)
• GROUND SUBSTANCES (glycosaminoglycans, chondroitin sulfate
• proteoglycan)
• BLOOD VESSELS, NERVES, LYMPH VESSELS
The principle cells of the pulp:
• Odontoblasts (The most distinctive cells of the dental pulp).
• Fibroblast (The function is to form and maintain pulp matrix).
• Undifferentiated mesenchymal cells (Represents the pool from
which the connective tissues of the pulp are derived).
• Macrophages (Involved in the elimination of dead cells).
• Immunocompetent cells (Lymphocytes & Dendritic cells).
Collagen in dental pulp
• Concentration varies from species to species, 32% in human pulp.
• Higher content in the middle and apical pulp.
• Total collagen decreases with age.
• Interestingly high level of collagen type III. (43%) : vascular content,
tissue extensibility (cf. Elastin)
• Absence of elastin .
Adhesive glycoproteins in dental pulp
• Fibronectin found in predentine NOT mature dentine.
• Fibronectin present in pulp and dental papilla.
• Fibroblasts synthesize pulpal fibronectin.
• Fibronectin is expressed during reparative dentinogenesis.
Glycosaminoglycans in dental pulp
• Chondroitin sulfate, dermatan sulfate, hyaluronic acid present.
• Amount of uronic acid decreases with age
• Total GAG decreases with reduced dentinogenic activity
• Decorin may involve in mineral nucleation at the mineralization front.
You might also like
- IPMR Biochemistry Fourth SemesterDocument83 pagesIPMR Biochemistry Fourth Semestertwity 1No ratings yet
- DPT Colleges of PakistanDocument24 pagesDPT Colleges of PakistanAli Bin AsimNo ratings yet
- Tissue BiochemistryDocument40 pagesTissue BiochemistryZahid MehmoodNo ratings yet
- Handbook of Endocrine Research TechniquesFrom EverandHandbook of Endocrine Research TechniquesFlora de PabloNo ratings yet
- Medical Ionization: Iontophoresis DR - Saira DDocument22 pagesMedical Ionization: Iontophoresis DR - Saira DAnonymous -No ratings yet
- Talent Management Case Studies NokiaDocument1 pageTalent Management Case Studies NokiakamsudhakarbalaNo ratings yet
- Water Borne Diseases: Summyia Siddique (PT) MSCPPTDocument17 pagesWater Borne Diseases: Summyia Siddique (PT) MSCPPThfyfvgskfajNo ratings yet
- Muhammad Wajid: Institute of Pharmacy Gulab Devi Educational Complex, LahoreDocument31 pagesMuhammad Wajid: Institute of Pharmacy Gulab Devi Educational Complex, LahoreAhmed ImranNo ratings yet
- The YMCA Bench Press Test.10Document4 pagesThe YMCA Bench Press Test.10katerinaNo ratings yet
- Osteogenesis Imperfecta: Osteogenesis Muscle Mass LigamentDocument7 pagesOsteogenesis Imperfecta: Osteogenesis Muscle Mass Ligamentlionella12No ratings yet
- Sangeetha Loganathan Angeliza ArciagaDocument57 pagesSangeetha Loganathan Angeliza ArciagaSangeetha LoganathanNo ratings yet
- Privatization of KESCDocument25 pagesPrivatization of KESCFahad Khalil0% (2)
- SZABIST's 4-Year BE Mechatronics ProgramDocument6 pagesSZABIST's 4-Year BE Mechatronics ProgramAhmar Hayat KhanNo ratings yet
- Introduction To CNS Pharmacology KFU 1Document24 pagesIntroduction To CNS Pharmacology KFU 1Peter HarrisNo ratings yet
- Community Based Rehabilitation: A.ThiruppathiDocument47 pagesCommunity Based Rehabilitation: A.ThiruppathiSri Charan ReddyNo ratings yet
- E1 Introduction To Community Medicine and Principles of EpidemiologyDocument39 pagesE1 Introduction To Community Medicine and Principles of EpidemiologyTristen TanNo ratings yet
- Biochemistry JD 2Document6 pagesBiochemistry JD 2failinNo ratings yet
- 1.1. Company BackgroundDocument32 pages1.1. Company BackgroundZahid GondalNo ratings yet
- Chapter - 13 - Cardiovascular - Responses - Exercise Physiology For Health Fitness and PerformanceDocument32 pagesChapter - 13 - Cardiovascular - Responses - Exercise Physiology For Health Fitness and Performanceec16043No ratings yet
- Collagen Synthesis ProcessDocument5 pagesCollagen Synthesis ProcessEusebio LeeNo ratings yet
- Anticancer Drugs PharmacologyDocument120 pagesAnticancer Drugs PharmacologyCARSON 539100% (1)
- Title of Qualification Awarded Diploma in Computerize Accounting & FinanceDocument2 pagesTitle of Qualification Awarded Diploma in Computerize Accounting & FinanceAtif Raza0% (2)
- Industrial MarketingDocument11 pagesIndustrial Marketingmyraa_nasirrNo ratings yet
- Enzymology: Discuss About Regulation of Enzyme ActivityDocument4 pagesEnzymology: Discuss About Regulation of Enzyme ActivityNorrifhan Akmal IsmailNo ratings yet
- Uv U+v: Focal Length of Convex Lens AimDocument10 pagesUv U+v: Focal Length of Convex Lens AimMoghanNo ratings yet
- 7 VisionDocument4 pages7 VisionZei RuhanoNo ratings yet
- Letter BusinessDocument9 pagesLetter BusinessDhony Agung PrandaniNo ratings yet
- 3D Cloud Computing Presentation.Document22 pages3D Cloud Computing Presentation.Rajnish BaranwalNo ratings yet
- Patients Beyond Borders Turkey Edition: Everybody's Guide to Affordable, World-Class Medical TourismFrom EverandPatients Beyond Borders Turkey Edition: Everybody's Guide to Affordable, World-Class Medical TourismNo ratings yet
- Community MedicineDocument2 pagesCommunity MedicinePreethiHonavar100% (1)
- BloodDocument38 pagesBloodchukwukerechimezirimNo ratings yet
- Gross Anatomy of Posterior Thigh CompartmentDocument20 pagesGross Anatomy of Posterior Thigh CompartmentOnah ArinzeNo ratings yet
- Differential White Blood Cell CountDocument20 pagesDifferential White Blood Cell CountNada hasan100% (2)
- Embryology of the Integumentary System DevelopmentDocument3 pagesEmbryology of the Integumentary System DevelopmentJonathan PaghubasanNo ratings yet
- Drugs: Assalamualaikum Wr. WBDocument4 pagesDrugs: Assalamualaikum Wr. WBMadiNo ratings yet
- 3 Shoulder Joint - Chapter Summary - Anatomy of The Shoulder Joint by Snell Medicine LectureDocument76 pages3 Shoulder Joint - Chapter Summary - Anatomy of The Shoulder Joint by Snell Medicine LectureRobin TolentinoNo ratings yet
- Electron Transport ChainDocument19 pagesElectron Transport Chaingaurav saxenaNo ratings yet
- 200L Excitable Tissues & Ans PhysiologyDocument65 pages200L Excitable Tissues & Ans PhysiologyAdedolapo bello100% (1)
- Red Blood Cells, Anemia, and PolycythemiaDocument7 pagesRed Blood Cells, Anemia, and PolycythemiaShi no Me100% (1)
- PATHOLOGY AND PATHOGENESIS OF TUBERCULOSISDocument46 pagesPATHOLOGY AND PATHOGENESIS OF TUBERCULOSISJaya Semara PutraNo ratings yet
- Fatty Acid MetabolismDocument40 pagesFatty Acid MetabolismMichelle Arredondo100% (1)
- Biochemistry of Blood Elements: The Figure Is Found at (March 2007)Document37 pagesBiochemistry of Blood Elements: The Figure Is Found at (March 2007)Sadam_fasterNo ratings yet
- CH 19 Integration of MetabolismDocument63 pagesCH 19 Integration of Metabolismshee140802100% (1)
- Hip JointDocument25 pagesHip JointHashim OmarNo ratings yet
- Biomecanis of Sitting and LyingDocument45 pagesBiomecanis of Sitting and Lyingsajjad50% (2)
- Individual Drug ResponseDocument18 pagesIndividual Drug ResponseIlham rianda100% (1)
- Retina: Zarieh Dawn L. Novela Medicine 2Document50 pagesRetina: Zarieh Dawn L. Novela Medicine 2Zari NovelaNo ratings yet
- Short Textbook of Surgery Himansu Roy PDFDocument723 pagesShort Textbook of Surgery Himansu Roy PDFUmer KhanNo ratings yet
- Tuberculosis DrugsDocument136 pagesTuberculosis DrugsSyed Gulshan NaqviNo ratings yet
- 04 EnzymologyDocument39 pages04 EnzymologyFrances FranciscoNo ratings yet
- CellDocument47 pagesCellAnami NizamNo ratings yet
- Muscular SystemDocument36 pagesMuscular SystemDeepak KdNo ratings yet
- The Pelvic Girdle: By/Dr - Abdisamad Omar AliDocument30 pagesThe Pelvic Girdle: By/Dr - Abdisamad Omar AliSAKARIYE MAXAMEDNo ratings yet
- Course 2: Origin, Destination and Structure of Cells and Tissues of The Immune SystemDocument29 pagesCourse 2: Origin, Destination and Structure of Cells and Tissues of The Immune SystemCristinaGheorgheNo ratings yet
- RespirationDocument29 pagesRespirationbemina jaNo ratings yet
- The Fate of Metabolism Andmabolic PathwaysDocument25 pagesThe Fate of Metabolism Andmabolic PathwaysXuân Vi100% (1)
- Physiology of Skin ReceptorsDocument16 pagesPhysiology of Skin ReceptorsJaynier Jayson JayaNo ratings yet
- Introduction To CNS PharmacologyDocument49 pagesIntroduction To CNS Pharmacologymatchees-gone rogueNo ratings yet
- Lipoprotein MetabolismDocument23 pagesLipoprotein MetabolismDarien LiewNo ratings yet
- Exam 1 NotesDocument54 pagesExam 1 NotesAnonymous If9p21kwZKNo ratings yet
- And The Band Played OnDocument3 pagesAnd The Band Played Onapi-302562798100% (1)
- Health Assessment ChecklistDocument10 pagesHealth Assessment ChecklistRuby Ann NarvasaNo ratings yet
- Hawkmoon - Mongoose CorebookDocument165 pagesHawkmoon - Mongoose CorebookArnaud Kirschvinck100% (1)
- Subject Verb AgreementDocument78 pagesSubject Verb Agreementanniedream80% (5)
- Complete DentureDocument33 pagesComplete DentureMohsin HabibNo ratings yet
- White Spot On Dobermans Chest Doberman Forum Doberman Breed Dog ForumsDocument1 pageWhite Spot On Dobermans Chest Doberman Forum Doberman Breed Dog Forums5wzqfx2jq8No ratings yet
- Monika Sukoco, Asih Budiastuti, Paulus YogyartonoDocument7 pagesMonika Sukoco, Asih Budiastuti, Paulus YogyartonoNur CameliaNo ratings yet
- Fever With Rash in A Child in IndiaDocument13 pagesFever With Rash in A Child in Indiamicheal1960No ratings yet
- Lab 03 Reflexes Referred PainDocument14 pagesLab 03 Reflexes Referred PainViraj TatikondaNo ratings yet
- Devendra (Division Agriculture, Nutrition Sciences International Development Research Centre Tanglin SingaporeDocument34 pagesDevendra (Division Agriculture, Nutrition Sciences International Development Research Centre Tanglin SingaporeMarisa PaysaNo ratings yet
- 054 Physiology MCQ ACEM Primary RenalDocument1 page054 Physiology MCQ ACEM Primary RenalYasif AbbasNo ratings yet
- Secrets Your Dentist Won't TellDocument8 pagesSecrets Your Dentist Won't TellKathryn89% (9)
- June 2015 (IAL) QP - Unit 3 Edexcel Biology A-LevelDocument16 pagesJune 2015 (IAL) QP - Unit 3 Edexcel Biology A-LevelConnor O'HanlonNo ratings yet
- .mp3 Otter - AiDocument2 pages.mp3 Otter - AiomarNo ratings yet
- 3 FertilizationDocument24 pages3 FertilizationSilmy AuliaNo ratings yet
- Fowl Typhoid and Pullorum Disease: H I - ShivaprasadDocument20 pagesFowl Typhoid and Pullorum Disease: H I - Shivaprasadrana harisNo ratings yet
- Dengue (DHF) CotDocument48 pagesDengue (DHF) CoteleonoraNo ratings yet
- Artificial Insemination Emerging Agribusiness TechnologyDocument5 pagesArtificial Insemination Emerging Agribusiness TechnologyRosel Gonzalo-Aquino100% (1)
- Neural Regulation of RespirationDocument19 pagesNeural Regulation of RespirationAbeer SallamNo ratings yet
- IAF Medical Standards for PilotsDocument43 pagesIAF Medical Standards for PilotsBIJAY KUMAR ROUTNo ratings yet
- Sex Advice For MenDocument38 pagesSex Advice For MenPerfectKey21No ratings yet
- Notes IV Polygraph InstrumnetDocument4 pagesNotes IV Polygraph InstrumnetKristine Ann QuiñonesNo ratings yet
- Planes Systems OrganizationDocument36 pagesPlanes Systems OrganizationR. EssoNo ratings yet
- 16-Pediatric Infections - Volume 1 - VaricellaDocument24 pages16-Pediatric Infections - Volume 1 - VaricellaFernando FernándezNo ratings yet
- 28 DiscusDocument2 pages28 DiscusGeorgeGabrielNo ratings yet
- Cap. 08 - RabbitsDocument23 pagesCap. 08 - RabbitsNailson JúniorNo ratings yet
- Count Able UncountableDocument6 pagesCount Able UncountableGosia MrówkaNo ratings yet
- Skin and Its AppendagesDocument28 pagesSkin and Its AppendagesTK Balbin Liquit100% (1)
- Contraceptive methods guide under 40 charactersDocument13 pagesContraceptive methods guide under 40 charactersJasper Padilla CaranyaganNo ratings yet
- Hypersensitivity Rev BWDocument34 pagesHypersensitivity Rev BWGuhanNo ratings yet