Professional Documents
Culture Documents
Acs Myocardial Infarction
Acs Myocardial Infarction
Uploaded by
ChaturangaNSenerathCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acs Myocardial Infarction
Acs Myocardial Infarction
Uploaded by
ChaturangaNSenerathCopyright:
Available Formats
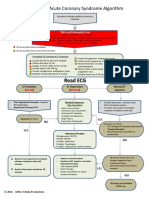
GUIDELINES FOR RISK STRATIFICATION & MANAGEMENT OF ACUTE CORONARY SYNDROMES
(Excluding ST elevation Myocardial Infarction)
MANAGEMENT OF ACUTE CORONARY SYNDROMES
RISK STRATIFICATION (Excluding ST elevation Myocardial Infarction)
HIGH RISK ACUTE CORONARY SYNDROMES
(Excluding STEMI)
1. Prolonged (>20min) or recurrent chest pain not
responding to medical management RISK STRATIFICATION
From history, physical examination, ECG
2. Haemodynamic instability (evidence of heart failure monitoring, blood samples
or hypotension
3. Life threatening arrhythmias (VT or VF)
4. 2mm or more ST segment depression in multiple
HIGH RISK INTERMEDIATE RISK LOW RISK
(≥5) ECG leads
5. Elevated troponin levels
• Aspirin + Clopidogral • Aspirin + Clopidogral • Aspirin + Clopidogral
• LMWH or UFH • LMWH or UFH • Beta blocker
INTERMEDIATE RISK • Nitroglycerin • Nitroglycerin • Statin
• Morphine sulphate • Morphine sulphate • Oral nitrates
• Beta blocker • Beta blocker (if indicated)
1. Prolonged (>20min) or recurrent chest pain • Statin • Statin
• GP IIb/IIIa receptor
responding to medical management blocker
2. Early post infarction angina (if indicated)
3. 2mm or more ST segment depression in < 5 leads
No response to medical
therapy
LOW RISK • ongoing typical angina
Responds to maximum
medical therapy
• haemodynamically
unstable
1. No recurrence of chest pain after admission
2. No elevation of biochemical cardiac markers
3. No ST segment depression
4. Normal ECG TRANSFER TO FULL
FACILITY CARDIAC CENTRE
POST DISCHARGE RISK
STRATIFICATION
After discussion with To assess for inducible
Consultant
You might also like
- Andre Tan's Surgery Notes (Ed 1)Document163 pagesAndre Tan's Surgery Notes (Ed 1)Daniel LimNo ratings yet
- DiltiazemDocument2 pagesDiltiazemE100% (1)
- Opthalmology Visuals New PDF-1Document100 pagesOpthalmology Visuals New PDF-1singh0% (1)
- Acute Coronary Syndrome / Acute Myocardial Infarction AlgorithmDocument37 pagesAcute Coronary Syndrome / Acute Myocardial Infarction AlgorithmHan OWNo ratings yet
- Drug Study - NitroglycerinDocument2 pagesDrug Study - NitroglycerinKian Herrera100% (1)
- Atenolol Drug Study WWW RNpedia ComDocument3 pagesAtenolol Drug Study WWW RNpedia ComYuuki Chitose (tai-kun)No ratings yet
- Metabolic and Endocrine ManagementDocument42 pagesMetabolic and Endocrine ManagementAlyssa MontimorNo ratings yet
- كيفيه التصرف في الحالات المختلفه في الاستقبالDocument91 pagesكيفيه التصرف في الحالات المختلفه في الاستقبالمحمد سعدون موسى عزيزNo ratings yet
- English TestsDocument43 pagesEnglish TestsCoral Srinivasa Ramalu0% (2)
- Chest Pain System - DisorderDocument1 pageChest Pain System - DisorderAA DDNo ratings yet
- Nursing Care Plan Diarrhea Assessment Diagnosis Planning Interventions Rationale EvaluationDocument8 pagesNursing Care Plan Diarrhea Assessment Diagnosis Planning Interventions Rationale EvaluationKrah100% (1)
- Carvedilol - Drug StudyDocument1 pageCarvedilol - Drug StudyAcads useNo ratings yet
- Kegawatan Jantung - MeDocument41 pagesKegawatan Jantung - MeNam Min BinNo ratings yet
- Abdominal Compartment SyndromeDocument22 pagesAbdominal Compartment SyndromeHalbana Al MaududyNo ratings yet
- Soscg - 3RD EditionDocument168 pagesSoscg - 3RD Editionsamantha80% (5)
- Dr. Rony M Santoso - ACS From Diagnosis To Long Term Treatment - Focus On Oral AntiplateletDocument25 pagesDr. Rony M Santoso - ACS From Diagnosis To Long Term Treatment - Focus On Oral AntiplateletluckyariadneeNo ratings yet
- ACLS ACS Algorithm NewDocument3 pagesACLS ACS Algorithm Newsambo100% (1)
- Slide Deck ACS Referral Forum - DR Adhitia MIni Simposium ACSDocument20 pagesSlide Deck ACS Referral Forum - DR Adhitia MIni Simposium ACSsyahrial fazaNo ratings yet
- Acute Coronary Syndrome - YMDocument64 pagesAcute Coronary Syndrome - YMNirwanaNo ratings yet
- NTSEMI and Unstable Angina ANdreaDocument17 pagesNTSEMI and Unstable Angina ANdreaandreaNo ratings yet
- DR Fadillah Maricar, SPJP Angina Pectoris Dan Infark MiokardDocument50 pagesDR Fadillah Maricar, SPJP Angina Pectoris Dan Infark MiokardMuhaswadNo ratings yet
- Ds Week 6 Nrg301 ValenzonaDocument2 pagesDs Week 6 Nrg301 ValenzonaJoshennaNo ratings yet
- Myocardial InfarctionDocument17 pagesMyocardial InfarctionCher HorowitzNo ratings yet
- Dx. StudyDocument3 pagesDx. Studymayumitanaka8042No ratings yet
- ACS Management in Pandemic EraDocument56 pagesACS Management in Pandemic EraFatmawati nersNo ratings yet
- Algorithm 1: Initial Evaluation and Management: Symptoms of Possible ACSDocument6 pagesAlgorithm 1: Initial Evaluation and Management: Symptoms of Possible ACSNenyNo ratings yet
- Acute Coronary Syndrome / Acute Myocardial Infarction AlgorithmDocument37 pagesAcute Coronary Syndrome / Acute Myocardial Infarction Algorithmjitendra magarNo ratings yet
- Acs CCS 2021 KLDocument52 pagesAcs CCS 2021 KLPitchya WangmeesriNo ratings yet
- Medication: Expected Pharmacological Action Therapeutic UseDocument1 pageMedication: Expected Pharmacological Action Therapeutic UseMike EveretteNo ratings yet
- Acca-Toolkit - 2018-Chapter 3-Secondary Prevention After AcsDocument14 pagesAcca-Toolkit - 2018-Chapter 3-Secondary Prevention After AcstrimardiyanaisyanNo ratings yet
- Atrial FibrillationDocument3 pagesAtrial FibrillationececasselNo ratings yet
- K31a - Electrophysiology and Cardiac Arrhytmia EmergencyDocument46 pagesK31a - Electrophysiology and Cardiac Arrhytmia EmergencyXeniel AlastairNo ratings yet
- Acute Coronary Syndrome: An Essential & Practical ApproachDocument35 pagesAcute Coronary Syndrome: An Essential & Practical ApproachGinawidiyastutiNo ratings yet
- Dr. Satyam Rajvanshi Dr. Ram Manohar Lohia Hospital, New DelhiDocument124 pagesDr. Satyam Rajvanshi Dr. Ram Manohar Lohia Hospital, New DelhiazizhaNo ratings yet
- Nursing CS Treatment-Of-Atrial-Dysrhythmias 02Document1 pageNursing CS Treatment-Of-Atrial-Dysrhythmias 02frankshro156No ratings yet
- Algorithms of Care (Myocardial Infarction)Document3 pagesAlgorithms of Care (Myocardial Infarction)Julius Delos SantosNo ratings yet
- Unit Farmasi Klinikal (Ufk), Husm.: Atrial Fibrillation in Critical Care - Amiodarone or Digoxin ?Document41 pagesUnit Farmasi Klinikal (Ufk), Husm.: Atrial Fibrillation in Critical Care - Amiodarone or Digoxin ?Ichwan Zuanto SjamanNo ratings yet
- 109890management StrokeDocument33 pages109890management StrokeAndleeb GanaieNo ratings yet
- Laporan Learning Objective Skenario 2 Blok Emergency: Sabrina Fazriesa 1418011194Document22 pagesLaporan Learning Objective Skenario 2 Blok Emergency: Sabrina Fazriesa 1418011194Sabrina FazriesaNo ratings yet
- Acute Coronary Syndrome EditedDocument38 pagesAcute Coronary Syndrome EditedSurgicalgownNo ratings yet
- Atrial Arrthymia WithoutDocument16 pagesAtrial Arrthymia Withoutapi-716714980No ratings yet
- Generic Name T Rade Name Classification Minitran Anti Angina NitroglycerinDocument1 pageGeneric Name T Rade Name Classification Minitran Anti Angina NitroglycerinChristopher LeeNo ratings yet
- Obat Obat EmergencyDocument34 pagesObat Obat EmergencymatkwokNo ratings yet
- LidocaineDocument2 pagesLidocaineRomwella May AlgoNo ratings yet
- Acute Heart Failure in Acute Coronary Syndrome: Buying Time To RevascularizationDocument43 pagesAcute Heart Failure in Acute Coronary Syndrome: Buying Time To RevascularizationMunasir BahriNo ratings yet
- Atrial Fibrillation - Student ResidencyDocument6 pagesAtrial Fibrillation - Student Residencyapi-404356063No ratings yet
- Acute Coronary Syndromes Algorithm: Patient Has Signs Suggestive of Ischemia or InfarctionDocument1 pageAcute Coronary Syndromes Algorithm: Patient Has Signs Suggestive of Ischemia or Infarctionjohndoe1995No ratings yet
- ACS Algorithm 2016 PDFDocument1 pageACS Algorithm 2016 PDFrabin1994No ratings yet
- PericarditisDocument3 pagesPericarditisececasselNo ratings yet
- AlgorithmACLStachycardiawithapulse PDFDocument1 pageAlgorithmACLStachycardiawithapulse PDFDendy Frannuzul RamadhanNo ratings yet
- Tachycardia With A Pulse Algorithm: Assess Appropriateness For Clinical ConditionDocument1 pageTachycardia With A Pulse Algorithm: Assess Appropriateness For Clinical ConditionDendy Frannuzul RamadhanNo ratings yet
- 3,4 - Anti-Arrhythmic Drugs (Summary, SAQ and MCQS)Document10 pages3,4 - Anti-Arrhythmic Drugs (Summary, SAQ and MCQS)Mengot Ashu RoseNo ratings yet
- NON Malig HaemDocument49 pagesNON Malig HaemNisini ImanyaNo ratings yet
- Acs With New Stemi GuidelineDocument35 pagesAcs With New Stemi Guidelinematmin07No ratings yet
- ACS Final DraftDocument33 pagesACS Final Draftomcm17006No ratings yet
- Trial of Routine Angioplasty and Stenting After Fibrinolysis To Enhance Reperfusion in Acute Myocardial Infarction The Transfer-Ami TrialDocument18 pagesTrial of Routine Angioplasty and Stenting After Fibrinolysis To Enhance Reperfusion in Acute Myocardial Infarction The Transfer-Ami TrialAji WiyasaNo ratings yet
- Angina Medication TableDocument3 pagesAngina Medication TableVictoria NieNo ratings yet
- Angiotensin-Converting Enzyme (ACE)Document5 pagesAngiotensin-Converting Enzyme (ACE)Isabella SamsonNo ratings yet
- Acute Coronary SyndromeDocument52 pagesAcute Coronary Syndromeindra muhammadNo ratings yet
- Penyakit Jantung Iskemik: Dr. Abraham Avicenna, SPJPDocument31 pagesPenyakit Jantung Iskemik: Dr. Abraham Avicenna, SPJPradian diptaNo ratings yet
- Anti Arrhythmic DrugsDocument12 pagesAnti Arrhythmic DrugsMunazza QuraishiNo ratings yet
- Controlling Heart Rate And/or RhythmDocument3 pagesControlling Heart Rate And/or RhythmDaia DaiaNo ratings yet
- Controlling Heart Rate And/or RhythmDocument3 pagesControlling Heart Rate And/or RhythmDaia DaiaNo ratings yet
- TachycardiaDocument12 pagesTachycardiaPuskesmas Pinang JayaNo ratings yet
- CVS1 - K25 - Cardiac EmergencyDocument34 pagesCVS1 - K25 - Cardiac EmergencyAdmin neuro-usu.idNo ratings yet
- Basic Cardio 3Document6 pagesBasic Cardio 3Malek ZanNo ratings yet
- Prescribing in Chest PainDocument4 pagesPrescribing in Chest PainYY_1992No ratings yet
- Hepatitis: Charles Manoj Chauhan Vedprakash Thakur AlokDocument29 pagesHepatitis: Charles Manoj Chauhan Vedprakash Thakur AlokCk LamaNo ratings yet
- CS NURS 529 Clinical Infectious DiseasesDocument9 pagesCS NURS 529 Clinical Infectious DiseasesAhmad Khalil Ahmad Al-SadiNo ratings yet
- Serious Diseases - One Stop Clil PDFDocument8 pagesSerious Diseases - One Stop Clil PDFKarydawson.APNo ratings yet
- Upper Gastrointestinal Bleeding Ugb Causes and Treatment 2475 3181 1000153Document3 pagesUpper Gastrointestinal Bleeding Ugb Causes and Treatment 2475 3181 1000153Envhy AmaliaNo ratings yet
- Alcohol AbuseDocument13 pagesAlcohol AbuseSandy SandyNo ratings yet
- Broiler Breeder ProductionDocument7 pagesBroiler Breeder ProductionCamille CarengNo ratings yet
- List of Autoimmune DiseasesDocument11 pagesList of Autoimmune DiseasesDuwa AhmadNo ratings yet
- Natural History and Risk Factors of Infantile Atopic Dermatitis: A Case Report and Literature ReviewDocument7 pagesNatural History and Risk Factors of Infantile Atopic Dermatitis: A Case Report and Literature ReviewZany BrilliantNo ratings yet
- Negative AutopsyDocument2 pagesNegative AutopsyJaweria SikanderNo ratings yet
- Kuliah CviDocument33 pagesKuliah CviAliffiaNo ratings yet
- 3 MODULE 5 - Topic 3 HIRSUTISM AND VIRILIZATIONDocument2 pages3 MODULE 5 - Topic 3 HIRSUTISM AND VIRILIZATIONJc Mae CuadrilleroNo ratings yet
- Adc 2001 RelesedDocument5 pagesAdc 2001 Relesedsweety49No ratings yet
- CVP Plus Rituximab (R-CVP) For Lymphoma: Page 1 of 2Document2 pagesCVP Plus Rituximab (R-CVP) For Lymphoma: Page 1 of 2Andreea NeculceaNo ratings yet
- Thomas Bogale TDocument64 pagesThomas Bogale TAlemayehu KebedeNo ratings yet
- Question Pre Final NursingDocument3 pagesQuestion Pre Final Nursingudaymarch03No ratings yet
- Medical Emergency Preparedness / First Aid in Trauma SituationsDocument66 pagesMedical Emergency Preparedness / First Aid in Trauma Situations1pallabNo ratings yet
- 20 - Neonatal InfectionsDocument4 pages20 - Neonatal InfectionsYassboy MsdNo ratings yet
- Seronegative Antiphospholipid Syndrome: Refining The Value of "Non-Criteria" Antibodies For Diagnosis and Clinical ManagementDocument11 pagesSeronegative Antiphospholipid Syndrome: Refining The Value of "Non-Criteria" Antibodies For Diagnosis and Clinical ManagementMike KrikNo ratings yet
- HSE705 Cardiopulmonary Weekly Schedule 2015 1Document4 pagesHSE705 Cardiopulmonary Weekly Schedule 2015 1Ayden ShawNo ratings yet
- Epicondylitis, Lateral: (Tennis Elbow)Document6 pagesEpicondylitis, Lateral: (Tennis Elbow)ArieZta Kautsar RahmanNo ratings yet
- Suicide PreventionDocument11 pagesSuicide PreventionYannah ZeuhNo ratings yet
- SWAMEDIKASI Inggris RevisiDocument3 pagesSWAMEDIKASI Inggris RevisiMirzania Mahya FathiaNo ratings yet