Professional Documents
Culture Documents
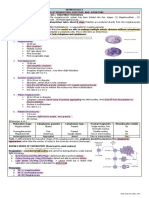
Decreased Hemoglobin Available For Erythrocytes Microcytic, Hypochromic Anemia More Hemoglobin Available For Erythrocytes Macrocytic Anemia
Uploaded by
IB leaksOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Decreased Hemoglobin Available For Erythrocytes Microcytic, Hypochromic Anemia More Hemoglobin Available For Erythrocytes Macrocytic Anemia
Uploaded by
IB leaksCopyright:
Available Formats
insufficient hemoglobin production
→ decreased hemoglobin available Insufficient cell production
for erythrocytes more hemoglobin available for erythrocytes
→ microcytic, hypochromic anemia macrocytic anemia
s
Decreased erythropoiesis
or decreased blood
volume
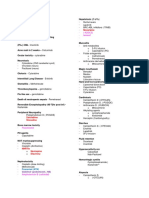
Sideroblastic anemia
Bone marrow failure or
disease
e.g. myeloproliferative
disease;
myelodysplastic syndrome
Microcytic hypochromic anemias MCV < 80 fL
Iron deficiency:
iron due to chronic bleeding (eg, GI loss, menorrhagia), malnutrition, absorption
disorders, GI surgery (eg, gastrectomy);
or demand (eg, pregnancy) final step in heme synthesis.
Labs: iron, TIBC, ferritin, free erythrocyte protoporphyrin, RDW. Microcytosis and
hypochromasia ( central pallor).
Symptoms: fatigue, conjunctival pallor, pica (persistent craving and compulsive eating of
nonfood substances), spoon nails (koilonychia).
May manifest as glossitis, cheilosis, Plummer-Vinson syndrome (triad of iron defciency
anemia, esophageal webs, and dysphagia).
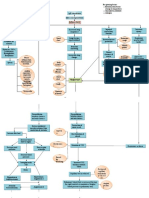
Normocytic normochromic anemia MCV 80-100 fL
Normocytic normochromic anemias are classified as nonhemolytic or hemolytic.
The hemolytic anemias are further classified according to the cause of the hemolysis
(intrinsic vs extrinsic to the RBC) and by the location of the hemolysis (intravascular vs
extravascular).
Hemolysis can lead to increases in LDH, reticulocytes, unconjugated bilirubin, pigmented
gallstones, and urobilinogen in urine.
Aplastic anemia:
- Pancytopenia with bone marrow insufficiency.
- Caused by failure or destruction of hematopoietic stem cells due to:
Idiopathic >50% cases (immune mediated, 1° stem cell defect); may follow acute
hepatitis.
Fanconi anemia (AR; DNA repair defect causing bone marrow failure; also short stature,
50% develop AML or myelodysplastic syndrome, café-au-lait spots, thumb/radial defects
Radiation and drugs (eg, benzene, chloramphenicol, alkylating agents, antimetabolites)
Viral agents (EBV, HIV, hepatitis viruses) – inhibiting hematopoiesis.
Diagnostic:
LAB: pancytopenia, reticulocyte count, EPO.
Bone marrow biopsy (hypocellular fat-filled marrow with normal RBC morphology)
Symptoms: Anemia (pallor, fatigue), Leukopenia (infections), Thrombocytopenia (Petechia,
purpura, gingival bleeding).
Treatment:
Cessation of offending agent (Drugs that cause aplastic anemia Can’t Make New
Blood Cells Properly: Carbamazepine; Methimazole; NSAIDs; Benzenes,
Chloramphenicol; Propylthiouracil)
RBC/platelet transfusion
Immunosuppressive regimens (eg, antithymocyte globulin, cyclosporine)
Bone marrow stimulation (eg, GM-CSF)
Hematopoeitic cell transplantation
You might also like
- Hema Part 3 Final PDFDocument188 pagesHema Part 3 Final PDFH.B.ANo ratings yet
- Endomitosis. EndomitosisDocument22 pagesEndomitosis. EndomitosisRUBEN DAMAYO100% (1)
- Hi Stop Hath Ology 2Document22 pagesHi Stop Hath Ology 2vivek govardhanamNo ratings yet
- 1983 Senate Hearing TranscriptDocument1,037 pages1983 Senate Hearing TranscriptStephen LoiaconiNo ratings yet
- Present at 4-12 Months, Development Arrest From Pre-B To BDocument2 pagesPresent at 4-12 Months, Development Arrest From Pre-B To BWaoNo ratings yet
- Auto-Release: David Plaut Beth Friedt & Tammy TaylorDocument51 pagesAuto-Release: David Plaut Beth Friedt & Tammy TaylorasclswisconsinNo ratings yet
- Gene Related DiseaseDocument3 pagesGene Related Diseasevivek govardhanamNo ratings yet
- Genitourinary System: Renal FailureDocument6 pagesGenitourinary System: Renal FailureEn ConejosNo ratings yet
- Cardio Block 3Document62 pagesCardio Block 3Maya LaPradeNo ratings yet
- 'Aliah's Cardiovascular SystemDocument45 pages'Aliah's Cardiovascular SystemLuqman Al-Bashir FauziNo ratings yet
- Product Introduction: Cellavision Dc-1 Loading Capacity: 1 Slide Throughput: 10 Slides/Hr Technical SpecificationsDocument12 pagesProduct Introduction: Cellavision Dc-1 Loading Capacity: 1 Slide Throughput: 10 Slides/Hr Technical SpecificationsElyza L. de GuzmanNo ratings yet
- Do Not Copy Without Permission This Property Is Governed by Republic Act No. 386, Title II, Chapter 1, Article 429 of Property Law of The PhilippinesDocument11 pagesDo Not Copy Without Permission This Property Is Governed by Republic Act No. 386, Title II, Chapter 1, Article 429 of Property Law of The PhilippinesChrissa Mae Tumaliuan CatindoyNo ratings yet
- Subphylum Basidiomycotina - Part 4: Class Holobasidiomycetes Order AgaricalesDocument10 pagesSubphylum Basidiomycotina - Part 4: Class Holobasidiomycetes Order Agaricalessallom1973No ratings yet
- BernaysEdward-Propaganda192879P (1) .Scan TextDocument79 pagesBernaysEdward-Propaganda192879P (1) .Scan TextgwblazerNo ratings yet
- Tumor Immunology: I. Common Tumor MarkersDocument2 pagesTumor Immunology: I. Common Tumor MarkersDivineGloryMalbuyoNo ratings yet
- Staph. Aureus Staph. Epidermidis Staph. SaprophyticusDocument5 pagesStaph. Aureus Staph. Epidermidis Staph. SaprophyticusTom PedersonNo ratings yet
- Salmonela Thyposa: Disease Etiology Unique S&S Brief Patophysiology Diagnostic Treatment / Plan OthersDocument8 pagesSalmonela Thyposa: Disease Etiology Unique S&S Brief Patophysiology Diagnostic Treatment / Plan OthersNatalia_WiryantoNo ratings yet
- c8k Quick Reference Guide en 2.0Document36 pagesc8k Quick Reference Guide en 2.0advanced techNo ratings yet
- Pathogens of The Vagina-Annie Espinosa - This Is The Revised VersionDocument1 pagePathogens of The Vagina-Annie Espinosa - This Is The Revised VersionMicroposterNo ratings yet
- Diseases Link To Chromosomal Abnormalities: Chromoso Me Abnormality DiseaseDocument7 pagesDiseases Link To Chromosomal Abnormalities: Chromoso Me Abnormality Diseasenreena aslamNo ratings yet
- RA MedTech Manila Sept2019 PDFDocument150 pagesRA MedTech Manila Sept2019 PDFPhilBoardResultsNo ratings yet
- 1 Ge Stimulations Mast Cell Degeneration Asthma AttackDocument4 pages1 Ge Stimulations Mast Cell Degeneration Asthma Attacknebbie06No ratings yet
- Myeloproliferative Disorders (MPD) : Pathogenesis Clinical Laboratory FindingsDocument2 pagesMyeloproliferative Disorders (MPD) : Pathogenesis Clinical Laboratory FindingskakuNo ratings yet
- WritemepleasetodayDocument40 pagesWritemepleasetodayMariel AbatayoNo ratings yet
- Haemopoiesis: Composition of Whole Blood & Its ComponentsDocument8 pagesHaemopoiesis: Composition of Whole Blood & Its ComponentsSafiya JamesNo ratings yet
- Rodaks 6th Ed. Hema Lab Midterm ReviewerDocument30 pagesRodaks 6th Ed. Hema Lab Midterm ReviewerGerald SorianoNo ratings yet
- What Is NEW Atheism ?Document9 pagesWhat Is NEW Atheism ?Nicholas LombardiNo ratings yet
- Low BP - Decreased Cardiac Output - Improved Renal Blood FlowDocument2 pagesLow BP - Decreased Cardiac Output - Improved Renal Blood Flowtantalizin marieNo ratings yet
- Finals Trans (Hema)Document16 pagesFinals Trans (Hema)Ayesha CaragNo ratings yet
- Clinical Medicine CVS Tabulated 2019Document5 pagesClinical Medicine CVS Tabulated 2019Justin TayabanNo ratings yet
- RBC MorphologyDocument9 pagesRBC MorphologybiancsNo ratings yet
- Handouts Integumentary Sys Sp11 B201Document7 pagesHandouts Integumentary Sys Sp11 B201Kelly TrainorNo ratings yet
- Histology and HistopathologyDocument42 pagesHistology and HistopathologyDreyden HaloNo ratings yet
- Tumor Markers: Blood Group AntigenDocument5 pagesTumor Markers: Blood Group AntigenAngela ReyesNo ratings yet
- Mechanisms of Cell Death NotesDocument30 pagesMechanisms of Cell Death NotesPatel AnkurNo ratings yet
- Clin Path Trans 3.05 Urinalysis (2b)Document6 pagesClin Path Trans 3.05 Urinalysis (2b)Reymart FernandezNo ratings yet
- Anemia Flow ChartDocument1 pageAnemia Flow ChartCynthiaNo ratings yet
- Cell Inclusions: John SantangeloDocument45 pagesCell Inclusions: John Santangelosaint5470No ratings yet
- Ready To Upgrade? Get The Full PSO-VR Here: IndexDocument22 pagesReady To Upgrade? Get The Full PSO-VR Here: IndexPepe PeprNo ratings yet
- Differential Diagnosis of Genital Ulcer Differential Diagnosis of Genital UlcersDocument3 pagesDifferential Diagnosis of Genital Ulcer Differential Diagnosis of Genital UlcersNurhayati HasanahNo ratings yet
- Flash Notes Billie-GeneticsDocument29 pagesFlash Notes Billie-GeneticsschxzerrydawnNo ratings yet
- GI + Renal OSCE: AMSA Edinburgh X IMU Y4Document41 pagesGI + Renal OSCE: AMSA Edinburgh X IMU Y4Abby LiewNo ratings yet
- Antibiotics Chart For MicrobiologyDocument5 pagesAntibiotics Chart For MicrobiologyTrevorNo ratings yet
- Essential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsDocument5 pagesEssential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsRika Ariyanti SaputriNo ratings yet
- Neuro Written III TablesDocument5 pagesNeuro Written III TablesSolomon Seth SallforsNo ratings yet
- Test LFTsDocument2 pagesTest LFTsostarburstoNo ratings yet
- Microscopic ExaminationDocument9 pagesMicroscopic ExaminationMariella DingleNo ratings yet
- Chart - WBC DisordersDocument1 pageChart - WBC DisordersSamuel RothschildNo ratings yet
- Kidney Physiology (Q & A)Document28 pagesKidney Physiology (Q & A)ramadan100% (1)
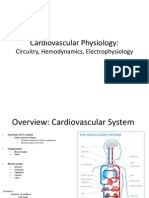
- Cardiovascular Physiology:: Circuitry, Hemodynamics, ElectrophysiologyDocument27 pagesCardiovascular Physiology:: Circuitry, Hemodynamics, Electrophysiologyrsmoney3No ratings yet
- Meninges, Ventricles - CSF - Study GuideDocument3 pagesMeninges, Ventricles - CSF - Study Guideshivani patelNo ratings yet
- DI-60 Integrated Slide Processing System BrochureMKT-10-1196 - Rev4Document12 pagesDI-60 Integrated Slide Processing System BrochureMKT-10-1196 - Rev4Hw XuNo ratings yet
- A Bunch of Pharm ShitDocument2 pagesA Bunch of Pharm ShitkatNo ratings yet
- Flash Notes Tumor MarkersDocument22 pagesFlash Notes Tumor MarkersschxzerrydawnNo ratings yet
- Hematology Basics NewDocument32 pagesHematology Basics Newkimbo23No ratings yet
- ECG Demographics Rate: 300/# Large Box in RR IntervalDocument11 pagesECG Demographics Rate: 300/# Large Box in RR IntervalJonathan DavisNo ratings yet
- Most Common Complication: Sabay SilaDocument6 pagesMost Common Complication: Sabay SilaSheryl Layne Lao-SebrioNo ratings yet
- Acute Myeloproliferative Acute Lymphoproliferative Chronic Myeloproliferative Chronic Lymphoproliferative Plasma Cell NeoplasmDocument1 pageAcute Myeloproliferative Acute Lymphoproliferative Chronic Myeloproliferative Chronic Lymphoproliferative Plasma Cell NeoplasmAudreySlitNo ratings yet
- Kuliah AnemiaaDocument44 pagesKuliah AnemiaaAhmad Umar AfNo ratings yet
- SBRC HematologyOncology 1Document80 pagesSBRC HematologyOncology 1dalia khamoNo ratings yet
- Madni 2018Document8 pagesMadni 2018IB leaksNo ratings yet
- Surgery q.1 10 State AngDocument98 pagesSurgery q.1 10 State AngIB leaksNo ratings yet
- HyperkalemiaDocument2 pagesHyperkalemiaIB leaksNo ratings yet
- Dividend Payment Record Common Stock 2132020Document5 pagesDividend Payment Record Common Stock 2132020IB leaksNo ratings yet
- C - SpineDocument10 pagesC - SpineCharly MontielNo ratings yet
- Dividend Radar 2021-01-15Document325 pagesDividend Radar 2021-01-15IB leaksNo ratings yet
- C - SpineDocument10 pagesC - SpineCharly MontielNo ratings yet
- AIT Art 37979-10Document9 pagesAIT Art 37979-10IB leaksNo ratings yet
- Atls® Written Pretest 10th Edition: 684 Section 4 Student Course ResourcesDocument9 pagesAtls® Written Pretest 10th Edition: 684 Section 4 Student Course ResourcesIB leaksNo ratings yet
- Example 6.2: Calculating Sample Size When Using The Chi-Squared TestDocument1 pageExample 6.2: Calculating Sample Size When Using The Chi-Squared TestIB leaksNo ratings yet
- ATLS Practice Test 2Document10 pagesATLS Practice Test 2Ken Evans100% (12)
- ATLS PretestDocument3 pagesATLS PretestDavid Reznick100% (5)
- ATLSPracticeTest3 PDFDocument10 pagesATLSPracticeTest3 PDFRodrigo Sanjines75% (4)
- ATLS Practice Test 1 Answers & ExplanationsDocument10 pagesATLS Practice Test 1 Answers & ExplanationsYou Wei Lin88% (16)
- Renal Function: Nephrology 1. Renal Function. Methods To Detect The Main Parameter of Renal FunctionDocument3 pagesRenal Function: Nephrology 1. Renal Function. Methods To Detect The Main Parameter of Renal FunctionIB leaksNo ratings yet
- Decreased Hemoglobin Available For Erythrocytes Microcytic, Hypochromic Anemia More Hemoglobin Available For Erythrocytes Macrocytic AnemiaDocument2 pagesDecreased Hemoglobin Available For Erythrocytes Microcytic, Hypochromic Anemia More Hemoglobin Available For Erythrocytes Macrocytic AnemiaIB leaksNo ratings yet
- ATLS Practice Test 1: Other ThanDocument11 pagesATLS Practice Test 1: Other ThanGarcia Rosa75% (8)
- PONR - Comprehensive Nursing Health History and Physical ExaminationDocument21 pagesPONR - Comprehensive Nursing Health History and Physical ExaminationDRJC100% (1)
- Appendix: Flow Charts and Treatment TablesDocument20 pagesAppendix: Flow Charts and Treatment TablesLeon LellaNo ratings yet
- Agust 2020Document29 pagesAgust 2020Danny YanuarNo ratings yet
- Department of Obstetrics and Gynecology FinalDocument42 pagesDepartment of Obstetrics and Gynecology Finalkremlin23455No ratings yet
- Definitive Guide To Red Light Therapy PhotobiomodulationDocument10 pagesDefinitive Guide To Red Light Therapy PhotobiomodulationDavid Jenkins0% (2)
- Using Sugar To Treat Those Nasty Wounds: American Farriers Journal Special Management Report #1..Document3 pagesUsing Sugar To Treat Those Nasty Wounds: American Farriers Journal Special Management Report #1..alfirafresdiNo ratings yet
- V1.0-Emergency Plan For Prevention and Control of New Coronavirus - Disease-CPPESEA PDFDocument12 pagesV1.0-Emergency Plan For Prevention and Control of New Coronavirus - Disease-CPPESEA PDFNutthakarn WisatsiriNo ratings yet
- Implanted Venous Access Device (IVAD) - "Dome" or "Port"Document12 pagesImplanted Venous Access Device (IVAD) - "Dome" or "Port"JunkNo ratings yet
- Diabetis 2Document33 pagesDiabetis 2Fercho MedNo ratings yet
- Option Com - Content&view Section&layout Blog&id 3 &itemid 60 FaqsDocument7 pagesOption Com - Content&view Section&layout Blog&id 3 &itemid 60 FaqsJig GamoloNo ratings yet
- THC AspergerDocument168 pagesTHC AspergerMICHAELNo ratings yet
- De Quervains TendonitisDocument2 pagesDe Quervains TendonitisisnainiNo ratings yet
- Sexually Transmitted DiseaseDocument38 pagesSexually Transmitted Diseaserana arslanNo ratings yet
- ASCITES (Water Belly)Document5 pagesASCITES (Water Belly)Santosh BhandariNo ratings yet
- Aches and Pains in The ElderlyDocument34 pagesAches and Pains in The ElderlyAna CampeanuNo ratings yet
- NCM 104 RLE Module 3 FinalsDocument22 pagesNCM 104 RLE Module 3 FinalsAlexander DontonNo ratings yet
- Psychiatric ScreeningDocument1 pagePsychiatric ScreeningCatalina BorquezNo ratings yet
- Nursing Care Plan Placenta PreviaDocument2 pagesNursing Care Plan Placenta PreviaApril Ann HortilanoNo ratings yet
- Chikungunya Virus Disease: Ii. Clinical InformationDocument2 pagesChikungunya Virus Disease: Ii. Clinical Informationkbl27No ratings yet
- Benign Breast Diseases29.7Document65 pagesBenign Breast Diseases29.7api-3701915No ratings yet
- EVC2019 Final Program PDFDocument29 pagesEVC2019 Final Program PDFFathiBestNo ratings yet
- NCP (Diarrhea)Document2 pagesNCP (Diarrhea)Rodj Bilang Jr.83% (30)
- ICMR GuidelinesType2diabetes2018 0Document82 pagesICMR GuidelinesType2diabetes2018 0VISHWANATH MARSHIVANIKARNo ratings yet
- Clinical Learning Log 3 Go Solo - Docx-1Document11 pagesClinical Learning Log 3 Go Solo - Docx-1JezraleFame AntoyNo ratings yet
- Pathogenesis of Bacterial InfectionDocument35 pagesPathogenesis of Bacterial InfectionDiyantoro NyoNo ratings yet
- Case 4-2021: A 70-Year-Old Woman With Dyspnea On Exertion and Abnormal Findings On Chest ImagingDocument12 pagesCase 4-2021: A 70-Year-Old Woman With Dyspnea On Exertion and Abnormal Findings On Chest ImagingBruno ConteNo ratings yet
- Vaginal Prolapse: by DR MutevheDocument32 pagesVaginal Prolapse: by DR MutevhedanielNo ratings yet
- Pass The MRCS HistoryDocument115 pagesPass The MRCS HistoryMariajanNo ratings yet
- Health Teaching Plan Mars and LainDocument7 pagesHealth Teaching Plan Mars and LainMarissa AsimNo ratings yet
- Concomitant SquintDocument21 pagesConcomitant SquintShivani NairNo ratings yet