Professional Documents
Culture Documents
Cardiopulmonary System: Relevant Anatomy & Physiology: Heart
Uploaded by
Julia Salvio0 ratings0% found this document useful (0 votes)
29 views12 pagesCARDIOPULMO PHYSIO
Original Title
11.-Cardiopulmo
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCARDIOPULMO PHYSIO
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
29 views12 pagesCardiopulmonary System: Relevant Anatomy & Physiology: Heart
Uploaded by
Julia SalvioCARDIOPULMO PHYSIO
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 12
CARDIOPULMONARY SYSTEM
o Receives blood supply during diastolic phase
o Left Main Coronary– divides into:
Relevant Anatomy & Physiology: Heart Left Anterior Descending – anterior and apical
surfaces of the LV, portions of the interventricular
Situated in the mediastinum, a mass of tissue that serves a
septum
median partition of the (L) and (R) thoracic cavities
Diagonal
Organs within the mediastinum: heart, pericardium, aorta,
Circumflex – lateral and inferior surfaces of the
trachea, esophagus, thymus gland
LV, portion of the LA
Weighs ~300 grams, roughly the same size as one’s fist, apex
Marginal
points inferiorly and ~45° to the left
o Right Coronary – RA, most of the RV, part of the inferior
Heart is situated in the middle of the chest, apex points
wall of the LV, portions of the interventricular septum,
towards the left
conduction system
o Base - ~between 2nd and 3rd rib
o Posterior Descending – commonly a branch of the RCA
o Apex - ~level of the 5th rib, point of maximal impulse
(right-dominant); posterior heart; left-dominant if it
(PMI)/apical beat, auscultated at (L) 5th intercostal space,
originates from the circumflex artery
9 cm from midsternal line/at the midclavicular line
Cardiac Muscle
o Tricuspid – (R) sternal border of xiphisternal junction at
o Striated, bifurcated ends, with the nucleus in the middle,
the 5th intercostal space
contains gap junctions inside intercalated discs,
o Right Atrium – 2nd intercostal space and angle of Louis
incapable of recruitment
o Aortic valve – (R) sternal border, 2nd intercostal space
o Cell membranes have sodium, potassium, and calcium
o Pulmonic valve – (L) sternal border, 2nd intercostal space
channels
Heart Tissue o Plateau phase prolongs action potential = prolonged
o Pericardium – double-walled sac that surrounds the
absolute refractory period (no response will be elicited),
heart incapable of full tetanic contraction
Fibrous – outermost covering of the heart, o Is not capable of developing significant O2 debt
anchors heart to the surrounding tissues and the
Cardiac Output
central dome of the diaphragm
o Amount of blood that leaves the ventricles/min (L/min),
Serous – contains pericardial fluid between its
reflects the heart’s performance as a pump
two layers; 15 mL, cushions the heart, minimizes
o Frank-Starling’s Law – when venous return ↑ = EDV ↑ =
friction during heart pumping
preload ↑ = SV ↑ = CO ↑
Parietal – connects with the fibrous
o Normal = 5250 mL/min
pericardium
o CO = HR (75 bpm) x SV (70 mL/beat)
Visceral – continuous with the wall of the
o SV = EDV (120 mL) – ESV (50 mL)
heart
o Epicardium – outermost layer of the heart, continuous o Stroke Volume – vol of blood ejected c each myocardial
with the visceral pericardium contraction
o Myocardium – middle and thickest layer, facilitates Preload – amt of blood in ventricle at end of
diastole from the venous return, load the
pumping action of the heart
ventricles must overcome before contraction
o Endocardium – innermost layer, continuous with the
(directly proportional)
tissue of the valves and endothelium of the blood vessel
Contractility – ability of the ventricle to contract
Blood Supply
(directly proportional)
o Provided by the coronary arteries
Afterload (80 mmHg) – force the LV must
o Sinus of Valsalva – where coronary arteries arise,
generate during systole to overcome aortic
located at the origin of the aorta immediately above the pressure and open aortic valve/load against
aortic valve
which the LV contracts during left ventricular Atherosclerosis – affects ages 40-50 in men, ~10 yrs later in
ejection (inversely proportional) women, plaques develop in coronary arteries that result in ↓
Cardiac Conditions blood flow and 02 distribution, body’s chronic compensation is
In the early part of the 20th century, MI tx included 2 mos of development of collateral circulation
bedrest Ischemia – inadequate blood supply of O2 to muscles,
By 40’s-50’s, ambulation began 14 days p an acute episode, completely reversible if transient, but may lead to infarction if
currently the inpatient phase of cardiac rehabilitation prolonged
Primary Prevention – adoption of lifestyle changes to prevent Angina Pectoris
onset of dse Reversible ischemic process, temporary inability to supply
Secondary Prevention – use of techniques to restore, maintain, sufficient O2 to heart muscle
and improve pt’s status p dx of dse Characterized by sudden onset of relatively diffused ant chest
It is the leading cause of death, atherosclerosis is m/c cause of pain, usually squeezing or pressure sensation
CHD; atherosclerosis, altered myocardial mm mechanics, o Stable/Chronic Exertion - Precipitated by exercise/stress,
valvular dysfunction, arrhythmias, HTN substernal chest pain for 5-10 mins; cessation of
activity; rest, lingual nitrates
o Unstable/Crescendo/Pre-infarction – also effort-related,
Stages of HTN but pain occur c ↑ frequency, intensity, duration, may
Stage Systolic Diastoli indicate CAD and ↑ risk of MI; less responsive to
c nitrates, require hospitalization and IV nitrates
Prehyperten 120-130 80-89 o Variant/Prinzmetal/Rest – caused by coronary artery
sion
spasm, pain while at rest frequently early morning/upon
Stage 1 130-140 90-100
rising, usually more intense and of longer duration than
Stage 2 140-160 100-110
stable, frequently leads to MI, more common in women
Stage 3 > 160 > 110
than men; unaffected by exertion, may be relieved by
2017 Guideline by AHA/ACC rest and nitrates
Stages of Systoli Diastoli
o Asymptomatic/Silent - ~70% may be silent, usually
Hypertension c c
Elevated 120- < 80 observed via 24-hr Holter monitor, ischemia at cellular
129 levels documented via ECG
Stage 1 130- 80-89 Dx and Tx:
139 o History
Stage 2 ≥ 140 ≥ 90
o ECG: ST segment elevation c variant, ST segment
depression c unstable
Coronary Artery Disease o Exercise Tolerance Test
Atherosclerotic process, thickening of tunica intima caused by o 24-hr Holter Monitor
accumulation of lipids, insidious onset and process o Beta blockers, nitrates, calcium channel blockers, lipid-
Left Anterior Descending Artery is m/c affected lowering drugs
Manifests as one or more of: Myocardial Infarction
o Sudden cardiac death Necrosis of some portion of cardiac muscle in response to
o Congestive Heart Failure sustained ischemia
o Angina pectoris Vise-like retrosternal tightening that becomes progressively
o Myocardial infarction intense and unbearable, radiates to jaw, neck, upper back, (L)
Risk factors shoulder, and arm
o Modifiable: smoking, blood lipid levels, obesity, inactivity Accompanied by dyspnea, nausea, vomiting, diaphoresis,
o Non-modifiable: age, sex, family hx generalized weakness, unrelieved by nitrates or rest
Dx Results in ↓ blood flow to tissues and congestion in pulmonary
oHx and symptoms and systemic circulation
oSerum enzymes M/c etiology is ischemic heart disease 2° to CAD, associated c
CK-MB – begins to rise in 2-4 hrs and return to HTN, valvular disease, CHD
normal in 48-72 hrs Changes in myocardial contractility d/t ↓ coronary blood flow,
LDH – LDH1 > LDH2 within 24 hrs, normal in 7-10 causing hypoxia
days Ventricular remodeling – compensatory hypertrophy and
SGOT - ↑ within 24 hrs, normal in 3-4 days dilation of myocardium
Troponin – rise in 4-8 hrs, normal in 7 days Compensatory mechanisms
o ECG changes o ↑ sympathetic nervous system stimulation - ↑ HR and
T wave inversion – ischemia contractility
ST segment elevation – injury o ↑ Na and H2O retention by kidneys
Pathologic Q waves – infarction o Hypertrophy of cardiac muscle fibers – to accommodate
o Cardiac Catheterization – for dx and interventional ↑ volume
purposes, allows visualization of arterial system and Types of Heart Failure
assessment of myocardium o Acute – acute exacerbation of chronic heart failure, rapid
Direct intracoronary antithrombotic therapy failure happens before compensatory mechanisms can
(streptokinase, urokinase, tPA) and percutaneous be effective, symptomatic fall in CO, rapid onset of
transluminal coronary angioplasty (PTCA) symptoms, dyspnea at rest, orthopnea, pulmonary
Goal: rapid reperfusion of ischemic/infarcted area congestion, edema
Complications o Chronic – gradually, associated c compensatory
o Arrhythmias – abnormalities in impulse generation and mechanisms, pulmonary congestion/peripheral edema
conduction usual reason to seek attention, leading cause of
o Heart Failure – abnormality in effective mechanical admission of pts > 65 y/o
performance of heart muscle; inability of heart to o Compensated – maintain adequate CO by compensatory
maintain a CO sufficient to meet O2 demands of tissues mechanisms, at rest appears normal, symptoms appear
o Thrombus formation – stasis embolism when demand ↑
o Heart structural damage o Uncompensated – when a severely damaged heart
cannot regain normal CO though compensatory
mechanisms are at work, fluid retention, gradual heart
Management stretching, diuretics and cardiac glycosides (digitalis)
o Cardiac rehabilitation program o Left-sided – more common than right-sided and
o Vocational counselling frequently leads to right-sided, most frequently seen p
o Education on risk factors MI, retrograde flow d/t ↑ volume builds, into interstitial
o Lifestyle modifications spaces and into alveoli, producing edema, dyspneic,
Sudden Cardiac Death lungs become stiff and less compliant and dyspnea
Sudden cardiac arrest, from cardiac dysfunction, s prior worsens
symptoms or < 6 hrs duration o Right-sided – m/c cause is left ventricular failure and
Leading cause is ventricular tachycardia/fibrillation COPD, ↑ central venous pressure and neck vein
No effective CO, prompt initiation of CPR distention, liver engorgement, ascites, peripheral
Congestive Heart Failure – recurring phenomenon by repeated edema, fatigue, ↓ tolerance of activity, tx towards ↓
exacerbation ↑ in frequency and severity circulatory overload, myocardial workload, and O2
Inability to maintain CO that is adequate to meet demands d/t demand, ↑ myocardial contractility = diuretics, Na
abnormality of function in heart muscle restrictions, cardiac glycosides, O2 therapy
Pericarditis Mediastinal surface is concave, which accommodates the heart
Inflammation of the pericardium, usually caused by bacteria o Cardiac impression is larger and deeper on (L) lung than
Tendency to rub during pumping of the heart (R)
Constant chest pain, friction rubbing upon auscultation o (L) lung is narrower and longer, (R) is larger, shorter,
Can result to abnormal ↑ in production of pericardial fluid wider
called pericardial effusion Pleural cavity – space between 2 layers of pleura, contains
Heavily notched/pointed T waves in adults may indicate serous fluid that reduces friction during ventilation
condition o Parietal pleura – outer
Cardiac Tamponade o Visceral pleura – inner
Pressure is directed towards the heart d/t fluid buildup, Fissures
contraction of the heart is limited o (R) – horizontal/transverse and oblique fissures; 3 lobes,
Complication of pericardial effusion, stab wounds, bleeding into 10 segments
the pericardial space o (L) – oblique fissure; 2 lobes, 8 segments
Cardiomyopathies Conducting Airways
Alterations in the muscular wall of the heart o Upper – nose, mouth, pharynx, larynx
o Dilated – ventricular dilation and altered cardiac muscle Nose – filter, humidify, and warm air before
contractile function; CAD is the primary cause, delivery to pharynx
myocarditis, alcohol abuse Pharynx – divided into nasopharynx (continues to
o Hypertrophic – diastolic dysfunction with ↑ ventricular filter and humidify inspired air), oropharynx, and
mass; chronic HTN and aortic stenosis laryngopharynx (conducts air from oral cavity
o Restrictive – diastolic dysfunction d/t presence of into trachea)
excessively rigid ventricular walls, resulting in ↓ in Epiglottis – leaf-shaped cartilage that covers and
compliance; diabetes protects glottis during swallowing
o Lower
Relevant Anatomy & Physiology: Respiratory System Begins with the trachea, considered the first-
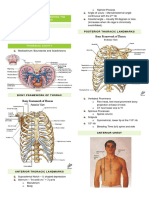
Bony Structures generation ventilatory passageway, originates
Thorax – protects vital organs of the cardiopulmonary system from lower border of cricoid cartilage (C6) and
and upper abdominal viscera, provides skeletal attachment for terminates at level of sternal angle of Louis (T4);
muscles mucous membrane contains both goblet and
Sternum ciliated epithelial cells
Ribs Branches into (L) and (R) main stem bronchi
Thoracic vertebrae which are the second generation of ventilatory
Musculature passageway
Inspiration: principal muscle is the diaphragm, Internal and Bronchi further branch into lobar (third
external intercostals, scalenes, SCM generation), segmental (fourth generation),
subsegmental (fifth generation) bronchi and
Expiration: mainly passive, relaxation of inspiratory muscles
continues for 23 generations until they terminate
Lungs
in the bronchioles
Each lung has an apex, base, costal surface, and mediastinal
Most distal conducting airways are respiratory
surface.
bronchioles
Base is concave and rests on diaphragm
Parts of the distal respiratory unit: respiratory
o Dome of (R) hemidiaphragm is slightly higher than the
bronchiole, alveolar ducts, alveolar sacs, alveoli
(L) because of liver Lung Volumes and Capacities
Costal surface is large and convex, conforms to inner contour of
ribcage
Tidal Volume – amount of air inspired and expired during o Irreversible enlargement of airspaces distal to terminal
normal resting ventilation, ~500 mL bronchiole, destruction of their walls s obvious fibrosis
Inspiratory Reserve Volume – additional air that can be further d/t ↓ alpha antitrypsin
inhaled p a tidal breath, ~3000 mL o Clearly associated c smoking, women and African-
Expiratory Reserve Volume – quantity of air that can be Americans more susceptible
potentially exhaled beyond end of tidal exhalation, ~1000 mL o Classified according to anatomic distribution
Residual Volume – volume of air that remains in the lungs p Centriacinar (Centrilobular) – central/proximal
maximal exhalation of ERV, ~1500 mL parts of acini (respiratory bronchioles), distal
Inspiratory Capacity – TV + IRV, 3500 mL; amount of air that alveoli spared; lesions more common and severe
can be expired beginning from a tidal exhalation in upper lobes
Functional Residual Capacity – combined ERV and RV, 2500 mL; Panacinar (Panlobular) – uniformly enlarged
volume of air that remains in the lungs at the end of a tidal respiratory bronchioles to terminal alveoli; occur
exhalation more commonly in lower zones
Vital Capacity – three volumes under volitional control (TV + Distal Acinar (Paraseptal) – proximal part is
IRV + ERV) normal, predominantly involves distal parts;
Total Lung Capacity – TV + IRV + ERV + RV more commonly occurs in upper half of lungs
Forced Expiratory Volume in 1 second (FEV1) – ≥ 70% of total Airspace Enlargement c Fibrosis
FVC; volume of air that can be forcefully exhaled during the (Paracitricial/Irregular) – acinus is irregularly
first second of a forced vital capacity maneuver involved, associated c scarring; asymptomatic
and clinically insignificant
Pulmonary Conditions
o Manifestations do not appear until at least 1/3 of
Pts c COPD benefit from treadmill walking programs (Pierce et
functioning parenchyma is damaged
al., 1964), exercise training and education are major
o First symptom: dyspnea, insidious but steadily
components of rehab
progressive
Obstructive Lung Diseases ♦
o In some, coughing/wheezing is c/c, cough and
o ↑ in resistance to airflow d/t partial/complete
expectoration extremely variable
obstruction at any level, from trachea and larger bronchi
o Barrel-chested and dyspneic, prolonged expiration, sits
to terminal and respiratory bronchioles
forward hunched over, pursed-lip breathing
o ↓ maximal airflow rates during forced expiration, usually
o Dx: Expiratory airflow limitation measured through
measured by FEV1
spirometry
o Only ~10% of pts c COPD are non-smokers, but only a
o May over-ventilate and remain well-oxygenated
minority of smokers develop COPD
o Occur in 2 general conditions: ♦ Chronic Bronchitis (Blue Bloaters)
Chest Wall Disorders - neuromuscular diseases Persistent cough c sputum production for at least 3 mos in 2
such as poliomyelitis, severe obesity, consecutive yrs, common among habitual smokers and
kyphoscoliosis inhabitants of smog-laden activities
Chronic Interstitial and Infiltrative Diseases – Many pts affected also have emphysema, can lead to cor
pneumoconioses and interstitial fibrosis of pulmonale
unknown etiology Earliest feature: hypersecretion of mucus in large airways
Restrictive Lung Diseases ♪ associated c hypertrophy of submucosal glands in trachea and
o ↓ expansion of lung parenchyma and ↓ total lung bronchi
capacity ↑ in goblet cells of small airways excessive mucus
o ↓ total lung capacity, expiratory flow rate is (n) or ↓ production
proportionately Cardinal symptoms: persistent, productive cough
♦ Emphysema (Pink Puffers)
Dyspnea on exertion eventually develops, hypercapnia, Usually affects lower lobes and most severe in more distal
hypoxemia, mild cyanosis bronchi and bronchioles
Emphysema Bronchitis Severe, persistent cough; expectoration of foul-smelling,
Age 50-75 40-45 sometimes bloody sputum, dyspnea and orthopnea in severe
Dyspnea Severe, early Mild, late cases
Cough Late, scanty Early, copious Symptoms often episodic precipitated by URTI or introduction
Infections Occasional Common of new pathogenic agents
Respiratory Terminal Repeated Paroxysms of cough when pt rises in the morning
Insufficiency Clinical Term Site Pathologic Etiology Signs/Sympt
Cor Pulmonale Rare, terminal Common Changes oms
Airway (n), slightly ↑ ↑ Emphysema Acini Airspace Tobacco Dyspnea
Resistance enlargement, smoke
Elastic Recoil Low (n), high wall destruction
Chest Hyperinflation, Prominent vessels, Chronic Bronchi Mucous gland Tobacco Cough,
Radiograph small heart large heart Bronchitis hyperplasia, smoke sputum
hypersecretion production
Appearance Pink Puffer Blue Bloater
Asthma Bronchi Smooth muscle Immunologic Episodic
♦ Asthma hyperplasia, al/Undefined wheezing,
Causes recurrent episodes of wheezing, breathlessness, chest excess mucus, cough,
tightness, cough inflammation dyspnea
Bronchiectas Bronchi Airway dilation, Persistent or Cough,
Widespread, variable bronchoconstriction, partially reversible
is scarring severe purulent
airflow limitation infections sputum, fever
More discouraging and disabling than lethal ♦ Cystic Fibrosis (Mucoviscidosis)
Hallmarks: ↑ airway response to a variety of stimuli, Exocrine gland dysfunction that results in abnormally viscid
inflammation of bronchial walls, ↑ mucus secretions secretions
o Atopic – evidence of allergen sensitization; m/c type, Hereditary disease transmitted as an autosomal-recessive trait
classic example of IgE-mediated hypersensitivity (mutation of CF gene [cystic fibrosis transmembrane
reaction, usually beings in childhood triggered by conductance regulator] in the long arm of chromosome 7)
environmental allergens, skin test c offending antigen Abnormally viscous mucus secreted by tracheobronchial tree
results in immediate wheal-and-flare and hyperplasia of mucus-secreting glands airway
o Non-atopic – no evidence of allergen sensitization, skin obstruction, recurrent infection, bronchiectasis, hyperinflation
test is usually (-), commonly triggered by respiratory Dx: Sweat test, ↑ levels of NaCl (> 60mEq/L), genotyping for
infections d/t viruses CFTR mutations for pts c borderline sweat chloride results
Chest tightness, dyspnea, wheezing, cough c/s sputum ↓ FEV1, ↑ RV, hypoxemia, hypercapnia
production, ↑ airflow obstruction, difficulty c exhalation,
Pancreatic insufficiency, GI dysfunction meconium ileus at
elevated eosinophils
birth, malabsorption, reproductive problems
Status asthmaticus - most severe form, severe acute paroxysm
♪ Idiopathic Pulmonary Fibrosis
persists for days/weeks, extreme airway obstruction may cause
Cause unknown, begins insidiously c gradually increasing
severe cyanosis/death
dyspnea on exertion and dry cough
♦ Bronchiectasis
Most pts 40-70 yrs old at presentation, mean survival of ≤3 yrs
Permanent dilation of bronchi and bronchioles caused by
Late: hypoxemia, cyanosis, clubbing
destruction of muscle and elastic tissue resulting from or
Progression is unpredictable c gradual deterioration despite
associated c chronic necrotizing infections
medical tx
Develops in association c a variety of conditions (postinfectious
conditions caused by M. Tuberculosis, S. Aureus, H. Influenzae,
♪ Pneumoconioses
congenital conditions such as CF)
Originally non-neoplastic lung reaction to inhalation of mineral Water enters spaces of alveoli
dusts, now includes those induced by organic particulates, Unequal pressures at blood vessels pushes water out of
chemical fumes, vapors capillaries
Air pollution in urban areas, cigarette smoking predisposes to Associated c left-sided heart failure, MI, mitral valve stenosis
accumulation of dust Dyspnea, non-productive cough
o Coal Workers’ Pneumoconiosis (CWP) Pulmonary Embolism
Benign disease, little decrement in lung function Lodging of particles in venous circulation, more on base of the
Some evidence suggests exposure to coal dust ↑ lungs, fatal condition
incidence of chronic bronchitis and emphysema, M/c cause: DVT, can be caused by venous stasis, clotting
independent of smoking disorders, oral contraceptives, air
o Silicosis Sudden acute pain, dyspnea
Slowly progressing, nodular, fibrosing Pleuritis/Pleural Effusion
pneumoconiosis ↑ amounts of pleural fluid, associated c CHF
Inhalation of crystalline silicone dioxide (silica) Causes: CHF, cardiac failure, renal failure, liver cirrhosis
Most prevalent chronic occupational disease in Cardinal sign: Dull/sharp pain
the world
Deep breathing and coughing, doorstop breathing, pleural
Chest radiograph: fine nodularity in upper zones
friction rubbing
of the lung but pulmonary functions are either (n)
Pneumothorax
or moderately affected
Air leaking into pleural space
Late dyspnea, ↑ susceptibility to TB
Forms: Traumatic, iatrogenic, spontaneous
o Asbestosis
Sudden sharp pain, deVere dyspnea, mediastinal shifting, ↓or
Chronic deposition of inhaled fibers from
absent breath sounds
asbestos (crystalline hydrated silicates)
Atelectasis
inflammation and fibrosis
Dyspnea usually first manifestation, provoked by Loss of lung volume expansion
exertion/even at rest, accompanied by Forms:
productive cough o Primary – d/t incomplete inspiration d/t weakness
Appear 10 yrs p exposure, more common p 20 o Secondary – d/t obstruction
yrs or more Cough and sputum production, fever
♪ Pneumonia Severe Acute Respiratory Syndrome
Intra-alveolar infection of lung parenchyma Caused by coronavirus, transmission through direct contact c in
M/c cause: Streptococcal the past 10 days
Can be bacterial, viral, aspiration High-grade fever, hyperthermia, dry cough, myalgia, lethargy,
Chills, fever, chest pain, cough sore throat
♪ Tuberculosis
♪ Bronchogenic Carcinoma
Caused by Mycobacterium Tuberculosis
Tumor arising from bronchial mucosa
Hallmark: Hemoptysis
Types:
Incubation period of 2-10 wks, maximally infectious during first
o Small Cell
2 wks (isolation in (-) pressure room)
o Oat Cell
Long-term medication (6-12 mos)
o Squamous Cell – m/c
Fever, weight loss, cough, lymph nodes enlargement,
hemoptysis Unexplained weight loss, hemoptysis, dyspnea, weakness and
fatigue, hoarseness
Pulmonary Edema Evaluation
Initial contact often happens indirectly, chart review is first o Cheyne-Stokes Respiration – periodic breathing: gradual
point of contact hyperpnea, hypopnea, and apnea; dying, coma,
o Read hx and physical and admission note associated c poor prognosis; usually CNS involvement
o Read last medical note o Kussmaul’s Respiration – hyperventilation (↑ rate and
o Scan remainder of chart depth), underlying cause is metabolic acidosis
o Read reports from medical specialists/consultants o Biot’s Respiration – “irregular irregular” breathing:
o Review pertinent lab tests hyperpnea (or normopnea) and apnea; poor prognosis,
o Review medications neuron damage, TBI
o Review psychosocial information o Ataxic Breathing – sudden change in depth
Anatomical landmarks: American Thoracic Society Dyspnea Scale
o Anterior – midsternal and midclavicular lines Grad Degree Description
o Lateral – Anterior, mid-, and posterior axillary lines e
0 None Not troubled c breathlessness except c
o Posterior – Vertebral and mid-scapular lines
strenuous exercise
Visual Inspection 1 Slight Troubled c SOB when hurrying on level/walking
o Nasal flaring – outward movement of the nares c up a slight hill
inspiration 2 Moderate Walks slower than people of same age on level
o Cyanosis d/t breathlessness/has to stop for breath when
Central – insufficient gas exchange c/in the lungs, walking at own place on level
O2 saturation < 80%; face, lips, tongue 3 Severe Stops for breath p walking about 100 yards/p a
Peripheral – O2 extraction at the periphery is few minutes on level
excessive, associated c low cardiac output 4 Very Too breathless to leave
states; usually occurs in cooler body parts Severe house/dressing/undressing
o Nail clubbing – loss of angle between nail bed and DIP Borg’s Scale - subjective
(Schamroth’s sign) Grade Description
Chest Wall Configuration 0 Nothing at all
o AP to lateral diameter is 1:2 or 5:7, angle of ribs > 90° 0.5 Very, very slight
o Barrel chest - ↑ AP diameter as ribs become more (just noticeable)
1 Very slight
horizontal; most commonly observed in pt c COPD
2 Slight
o Pectus excavatum – funnel chest; depressed lower
3 Moderate
sternum, can result into restrictive lung disease
o Pectus carinatum – pigeon chest; prominent upper 4 Somewhat severe
sternum 5 Severe
o Flail chest – chest wall moves inward c inspiration 7 Very severe
9 Very, very severe (almost
Breathing Pattern – normally between 12-20 bpm; normal ratio
maximal)
of inspiratory to expiratory time is 1:2
10 Maximal
o Eupnea – normal breathing cycle
Auscultation – art of listening to the sounds produced by the
o Apnea – temporary halt in breathing
body
o Tachypnea – rapid, shallow breathing pattern, > 20 bpm
o Breath sounds
o Bradypnea – slowed breathing, < 12 bpm
Normal
o Orthopnea – difficulty breathing when lying flat;
Bronchial (tracheal) – high-pitched,
pulmonary edema, CHF
hollowed; heard in both inspiration and
o Dyspnea – shortness of breath
expiration, louder on expiration with
pause between phases; over manubrium
Bronchovesicular – high-pitched c equal Whispered pectoriloquy – whispered
inspiratory and expiratory cycles but s sounds become distinct and clear, can be
pause; superior to clavicles, present when bronchophony and
suprascapular, parasternal, interscapular; egophony are absent; identifying smaller
over main stem bronchi: 1st and 2nd ICS or patchy areas of lung consolidation
anteriorly and between scapulae o Extrapulmonary sounds
posteriorly Friction rub – rubbing or leathery sounds during
Vesicular – soft, low-pitched; over both inspiration and expiration; rubbing of
remaining peripheral lung fields; mainly parietal and visceral pleura such as inflammation
inspiration c initial 1/3 of expiration or neoplasm, usually associated c pain
audible s pause between phases o Heart sounds
Abnormal Pt position: supine and sitting – all areas, side-
Bronchial (tubular) – consolidation lying – apex using bell
pneumonia, compression of lung tissue; S1 – “Lubb,” closing of AV valves, duration: 1.10
when peripheral lung tissue becomes s, loudest at apex, systolic phase:
airless; louder expiration Isometric/isovolumic contraction –
Decreased – hyperinflation d/t ventricles contract s movement, all 4
emphysema, depth of valves are closed
respiration/thickness of chest wall Ejection – specific phase when S1 is
Absent – loss of lung compliance d/t heard; closed AV valves, open semilunar
fibrosis (can lead to decrease or absence) valves
Adventitious – extraneous noises over S2 – “Dupp,” closing of semilunar valves and end
bronchopulmonary tree of ventricular systole
Crackles – discontinuous, low-pitched Isometric/isovolumic relaxation – specific
primarily during inspiration; peripheral phase when S2 is heard; all 4 valves are
airway process closed
Rhonchi – low-pitched but continuous Ventricular filling – open AV valves, closed
sounds in both inspiration and expiration; semilunar valves
snoring quality; obstructive process in the S3 – faint, low-frequency sound, reflects early
larger, more central airways ventricular filling p AV valves open; abnormal in
Wheezes – continuous, high-pitched; pt > 40 y/o; ideal position is (L) side-lying;
hissing or whistling primarily during ventricular failure, tachycardia, mitral
expiration; bronchospasms. Movement of regurgitation
air through secretions S4 – dull-sounding, rapid ventricular filling p atrial
Voice sounds – low-pitched, muffled or mumbled contraction; may be heard c left ventricular
Bronchophony - ↑ vocal transmission, hypertrophy; systemic HPN, cardiomyopathies,
louder and clearer; ↑ lung density e.g. coarctation of the aorta
consolidation Murmurs – vibrations from turbulent blood flow,
Egophony - ↑ transmission of vocal swishing sound
vibrations, “eee” is distorted as “aaa”, Systolic – AV valve insufficiency,
coexists c bronchophony semilunar valve stenosis
Whispered – low-pitched vibrations Diastolic – AV valve stenosis, semilunar
muffled by normal lung parenchyma valve insufficiency
Continuous – starts in S1 and lasts
through portion or all of S2
Gra SA Node – upper part of the RA; heart’s primary
de pacemaker, makes the atria contract; highest
I Faint Requires concentrated effort to rate of rhythmicity, greatest frequency of
hear firing/min = 60-100 impulses/min
II Faint Audible immediately AV Node – lower part of the RA; fires 40-60
III Louder than II Intermediate intensity impulses/min
IV Loud Intermediate intensity;
Bundle of His – transmits impulses from AV node
associated c palpable vibration
to the ventricles
(thrill)
V Very loud Thrill present (L) & (R) Bundle Fibers
VI Audible s Purkinje Fibers – located in the inner ventricular
stethoscope walls in a space called the subendocardium,
* Grade III+ usually associated c cardiac pathology makes the ventricles contract; fires 20-40
Mediate Percussion – assess density of underlying organs impulses/min
o Resonant – loud/high amplitude, low-pitched, longer o Normal ECG
duration, heard over air-filled organs e.g. lungs P wave – sinus node and atrial depolarization
o Dull – low amplitude, med to high-pitched, short PR/PQ segment – AV node conduction
duration, heard over solid organs e.g. liver QRS complex – atrial repolarization/ventricular
o Flat – high-pitched, short duration, heard over muscle depolarization
mass e.g. thigh ST segment – initiation of ventricular
o Tympanic – high-pitched, medium duration, heard over repolarization
hollow structures e.g. stomach T wave – completion of ventricular repolarization
o Hyper-resonant – very low-pitched, prolonged duration, U wave – ventricular relaxation
heard over tissue c ↓ density (↑ air: tissue ratio);
abnormal in adults; lungs c emphysema
o Diaphragmatic Excursion – 3-5 cm, difference between
lowest level of diaphragm on max inspiration and lowest
area of resonance p expiration; ↓ in pt c COPD
Chest Wall Excursion (Chest Expansion Symmetry) – 3.25 in
(8.5 cm) in young adults between 20-30 y/o
Count-off Method – only applicable when rhythm is normal
o Upper Lobe – suprasternal notch
1 small square – 0.04 secs (40 ms)
o Middle Lobe – xiphoid process
1 large square – 0.2 secs (200 ms)
o Lower lobe – back
5 large squares – 1 sec
Tactile fremitus – transmitted vibrations from spoken R-R interval - Heart Rate Relationship
words/vocalization (↑ = less air, ↓ = more air) R-R Interval Heart Rate
Tracheal Deviation – index finger in medial aspect of (bpm)
suprasternal notch 1 300
Contralateral – pneumothorax, pleural effusion, 2 150
tumor 3 100
Ipsilateral – atelectasis
4 75
ECG Interpretation – Dr. Willem Einthoven
5 60
o Main function is to monitor electrical activity of the heart
o P wave
o Pacemaker/Nodal cells – can generate their own action
Conduction of electrical impulse through atria
potential, found in the heart’s intrinsic conduction
Precedes QRS complex
system:
2-3 mm high
0.06-0.12 secs Depression – 0.5 mm below baseline; may
Usually rounded and upright indicate myocardial ischemia &
o QRS Complex unstable angina
Follows PR interval o Leads
5-30 mm high, differs for each lead used Precordial leads – unipolar; back-front and right-
0.06-0.10 secs/half of PR interval left
Beginning of Q wave to end of S wave/beginning V1 – RSB, 4th ICS
of R wave if Q wave is absent V2 – LSB, 4th ICS
Q wave – first negative deflection p the P wave V3 – between V2 and V4
R wave – first positive deflection p P or Q wave V4 – 5th ICS, (L) MCL
S wave – first negative deflection p R wave V5 – between V4 and V6
Variety – qRs, rS, QS, Rs, rsR, qR, Qr
V6 – 5th ICS, (L) MAL
o T wave
Limb leads – bipolar; up-down and right-left
Ventricular recovery/repolarization, peak
aVF – (L) foot
represents relative refractory period of
aVL – (L) arm
ventricular repol
aVR – (R) arm
Follows S wave
Leads II, III, and aVF signify activity of the inferior
0.5 mm in leads I, II, III, up to 10 mm in
wall of the heart
precordial leads
o Abnormalities
Usually round and smooth
Usually upright in leads I, II, and V3-V6, inverted Dysrhythmia – abnormal rhythm
in lead aVR, variable in others Arrhythmia – absence of a rhythm
o PQ/PR Interval – 0.12 – 0.20 secs T wave inversion – abnormality in the ventricles
(myocardium); may indicate myocardial
Length of SA – AV conduction
infarction
Prolongation causes ↓ HR
Bundle Branch Block (either left or right) - QRS
M/c cause of prolongation is AV node block
complex looks like a bishop’s miter/double
Represents electrical events that take place in
peak/bigeminal and prolonged (>0.12 ms)
the atria
AV Node Block – m/c cause of PR interval
o QT Interval – electrical depolarization and repolarization
prolongation
of the ventricles; conduction from AV node to Purkinje
1st Degree – mildest form, delayed but all
fibers
impulses still reach Purkinje fibers
Represents electrical events that take place in
the ventricles 2nd Degree – partially damaged AV node,
o ST Segment – found within the QT interval, flatline some impulses do not reach Purkinje;
causes dropped wave, wherein QRS
between S and T waves; latency period between
occurs p 2 P waves
ventricular depolarization and repolarization
Prolongation means that ventricular 3rd Degree – complete heart block; QRS
repolarization is delayed occurs p 3 P waves
ST displacement – not all are significant, only Atrial Fibrillation
those measuring ≥ 2 mm (1 small box = 1 mm) No distinguishable P wave, only QRS
Elevation – above baseline, immediately complex
after R wave; may indicate myocardial Caused by firing of individual myocardial
infarction & variant angina cells
Leads to stasis, which can lead to
thrombus formation
Flutter – more severe form of fibrillation
o IN SUMMARY:
1. Determine the rhythm. P-P and R-R intervals
2. Determine the rate. Count-off method.
3. Evaluate the P wave.
4. Determine the duration of the PR interval.
5. Determine the duration of the QRS complex.
6. Evaluate the T waves.
7. Determine the duration of the QT interval.
8. Evaluate any other components.
Arterial Blood Gas Analysis
o PaO2 – >75 mmHg, partial pressure of O2 in arterial blood
o M/c site of extraction is the radial artery
o pH – 7.35-7.45, “per hydrogen”
Signifies acidity/alkalinity of blood, expressed in
negative logarithm of H+
↑ means less hydrogen, alkalosis
↓ means more hydrogen, acidic
o PaCO2 – 35-45 mmHg, partial pressure of CO2 in arterial
blood
Neutralizes effects of excessive alkalinity
o Bicarbonate (HCO3) – 22-26 mmol/L = mmol L-1 = mEq/L
buffer, neutralizes effects of excess acid
o Buffering Systems
Respiratory – regulates PaCO2
Metabolic – regulates HCO3
o How is the pt?
o Assess oxygenation
o Determine pH
o Determine respiratory component
o Determine metabolic component
You might also like
- Cardio Pulmo NotesDocument12 pagesCardio Pulmo NotesCherrie MaeNo ratings yet
- Cardiopulmo Notes 2ndDocument12 pagesCardiopulmo Notes 2ndCherrie MaeNo ratings yet
- ANPH Wk12 - Cardiovascular SystemDocument17 pagesANPH Wk12 - Cardiovascular SystemSin I GangNo ratings yet
- Cardiovascular System and BloodDocument21 pagesCardiovascular System and BloodFRANCINE JANE PATI�ONo ratings yet
- Anatomy of The Heart & Its ValvesDocument9 pagesAnatomy of The Heart & Its ValvesJustine CastilloNo ratings yet
- Cardiovascular SystemDocument9 pagesCardiovascular SystemCrazy StrangerNo ratings yet
- Cardiovascular System Heart ReviewerDocument8 pagesCardiovascular System Heart ReviewerImmanuel Cris PalasigueNo ratings yet
- CARDIODocument17 pagesCARDIORayana Ubas100% (1)
- Basic Anatomy & Physiology: Cardiovascular Heart AnatomyDocument16 pagesBasic Anatomy & Physiology: Cardiovascular Heart AnatomyLalu Ahmad AsmayadiNo ratings yet
- Med 1 Block 2 - Wet Lab NotesDocument36 pagesMed 1 Block 2 - Wet Lab NotesluckyNo ratings yet
- FA 2019 CardiovascularDocument44 pagesFA 2019 CardiovascularLexNo ratings yet
- HEARTDocument5 pagesHEARTCUESCANO, CRISTEL G. BSMT 2-ANo ratings yet
- Whitaker 2010Document3 pagesWhitaker 2010Gabriel Jose CarvajalNo ratings yet
- 1 Cardiovascular System (FINAL) PDFDocument11 pages1 Cardiovascular System (FINAL) PDFJohn Juan TwanNo ratings yet
- Assessing Heart and Neck Vessel Heart Heart Chambers: (Tricuspid & Bicuspid)Document7 pagesAssessing Heart and Neck Vessel Heart Heart Chambers: (Tricuspid & Bicuspid)Dan Floyd FernandezNo ratings yet
- A&P - 1. Heart Anatomy (9p)Document9 pagesA&P - 1. Heart Anatomy (9p)mr. fakeNo ratings yet
- Cardiovascular Notes - All in One FileDocument299 pagesCardiovascular Notes - All in One FileHasan DiabNo ratings yet
- CVS Block..anatomy Word 2022Document25 pagesCVS Block..anatomy Word 2022Kero amgedNo ratings yet
- Chapter 12: Heart: Functions of The HeartDocument12 pagesChapter 12: Heart: Functions of The Heartchristian anchetaNo ratings yet
- Cardiovascular SystemDocument30 pagesCardiovascular SystemJuan Miguel TevesNo ratings yet
- LVH - Lateral To The Midclavicular Line: Right and Left 2 ICS Next To The SternumDocument15 pagesLVH - Lateral To The Midclavicular Line: Right and Left 2 ICS Next To The SternumRobin Abraham-BalisiNo ratings yet
- HPP Lec Cvs2Document4 pagesHPP Lec Cvs2carlo baculiNo ratings yet
- Anatomy of The HeartDocument3 pagesAnatomy of The HeartCanan YilmazNo ratings yet
- Pathophysiology of Heart Disease - A Collaborative Project of Medical Students and Faculty (PDFDrive) - 12-19Document8 pagesPathophysiology of Heart Disease - A Collaborative Project of Medical Students and Faculty (PDFDrive) - 12-19nurul hidayatiNo ratings yet
- EXTERNALFEATURESOFTHEHEART - ppt1Document28 pagesEXTERNALFEATURESOFTHEHEART - ppt1Mridula SaranNo ratings yet
- 1-Anatomy of The HeartDocument30 pages1-Anatomy of The Hearta730482776No ratings yet
- ANATOMY Final pt.1Document26 pagesANATOMY Final pt.1Gladys Mae S. BañesNo ratings yet
- CVP Review of Relevant Anatomy Physiology SarioDocument15 pagesCVP Review of Relevant Anatomy Physiology SariorkNo ratings yet
- PEDIA - Cardio (Esguerra) PDFDocument9 pagesPEDIA - Cardio (Esguerra) PDFMedisina101No ratings yet
- Reviewer 2 Health AssessmentDocument13 pagesReviewer 2 Health AssessmentchristinejeancenabreNo ratings yet
- Sample Transes 2Document11 pagesSample Transes 2Sophia SalamatNo ratings yet
- HeartDocument11 pagesHeartKei GauranoNo ratings yet
- Thoracic Cavity (Chapter 3)Document13 pagesThoracic Cavity (Chapter 3)Alenna BenitezNo ratings yet
- Cardiovascular System - The HeartDocument37 pagesCardiovascular System - The HeartCecil AlbaNo ratings yet
- Regional Anatomy of The Thorax: DR John Yuen, Associate Professor School of NursingDocument25 pagesRegional Anatomy of The Thorax: DR John Yuen, Associate Professor School of NursingEngineers go fishing JustkiddingNo ratings yet
- Cardiovascular System WordDocument18 pagesCardiovascular System WordLapitan Jared Anne S.No ratings yet
- Dr. Alurkur's Book On Cardiology - 2Document85 pagesDr. Alurkur's Book On Cardiology - 2Bhattarai ShrinkhalaNo ratings yet
- CARDIOLOGYDocument15 pagesCARDIOLOGYPatty RomeroNo ratings yet
- The Emotion That Breaks Your Heart Is Sometimes The Very One That Heals It!Document4 pagesThe Emotion That Breaks Your Heart Is Sometimes The Very One That Heals It!A-Naeem To'mah Al-sawaieNo ratings yet
- ANPH111 Cardiovascular System OverviewDocument7 pagesANPH111 Cardiovascular System OverviewUwen NalpNo ratings yet
- Cardio TransDocument7 pagesCardio TransweissNo ratings yet
- Respiratory System. Assessing The Thorax and LungsDocument27 pagesRespiratory System. Assessing The Thorax and LungsLorenz Jude CańeteNo ratings yet
- 01 HeartDocument39 pages01 HeartFahvy tvNo ratings yet
- HEART FINALS REVIEWERDocument7 pagesHEART FINALS REVIEWERshannenmaehfajanilanNo ratings yet
- Heart Valves & CirculationDocument4 pagesHeart Valves & Circulationyoonie catNo ratings yet
- Care of Clients With Problems in OxygenationDocument5 pagesCare of Clients With Problems in OxygenationSkyla FiestaNo ratings yet
- #3 Cardiovascular SystemDocument18 pages#3 Cardiovascular SystemLapitan Jared Anne S.No ratings yet
- Heart Structure and CirculationDocument13 pagesHeart Structure and CirculationKyle LumingkitNo ratings yet
- Anaphy HeartDocument6 pagesAnaphy HeartAngellene GraceNo ratings yet
- Diaphragm + Abdominal Aorta + IVC + LiverDocument2 pagesDiaphragm + Abdominal Aorta + IVC + LiverannaNo ratings yet
- Cardiac Anatomy and Phvsiologv A Review - Aorn800Document16 pagesCardiac Anatomy and Phvsiologv A Review - Aorn800Citra Ayu ApriliaNo ratings yet
- WEEK 1 MEDSURG AsynchDocument12 pagesWEEK 1 MEDSURG AsynchLeigh Angelika Dela CruzNo ratings yet
- Anaphy CardioDocument6 pagesAnaphy CardioDianne DimaanoNo ratings yet
- HEARTDocument8 pagesHEARTSJane FeriaNo ratings yet
- Heart Anatomy & Development in the Middle MediastinumDocument42 pagesHeart Anatomy & Development in the Middle MediastinumVidya BalaNo ratings yet
- Heart External AnatomyDocument6 pagesHeart External AnatomyKrissia BaasisNo ratings yet
- HeartDocument7 pagesHeartlilac.poppy.48No ratings yet
- Circulation Lec 2 Part-2Document21 pagesCirculation Lec 2 Part-2Rudrapalash ChakrabartiNo ratings yet
- CARDIOVASDocument3 pagesCARDIOVASFrama Intan MiguelNo ratings yet
- Gait Deviations in Orthotics & ProstheticsDocument10 pagesGait Deviations in Orthotics & ProstheticsJulia SalvioNo ratings yet
- Ultraviolet Radiation (Uvr)Document34 pagesUltraviolet Radiation (Uvr)Julia SalvioNo ratings yet
- Ultraviolet Radiation (Uvr) : ApplicationDocument28 pagesUltraviolet Radiation (Uvr) : ApplicationJulia Salvio100% (1)
- UltrasoundDocument24 pagesUltrasoundJulia SalvioNo ratings yet
- UE Prosthesis Components GuideDocument23 pagesUE Prosthesis Components GuideJulia SalvioNo ratings yet
- GSC - DDH LCPD SCFE and OthersDocument3 pagesGSC - DDH LCPD SCFE and OthersJulia SalvioNo ratings yet
- Low Back Pain ExcercisesDocument55 pagesLow Back Pain ExcercisesJulia SalvioNo ratings yet
- Fracture Treatment RehabDocument30 pagesFracture Treatment RehabJulia SalvioNo ratings yet
- Interferential Therapy: An Effective Electrotherapy ModalitDocument22 pagesInterferential Therapy: An Effective Electrotherapy ModalitJulia SalvioNo ratings yet
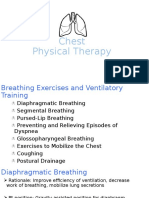
- Chest Physical Therapy Breathing ExercisesDocument28 pagesChest Physical Therapy Breathing ExercisesJulia SalvioNo ratings yet
- Functional Electrical Nerve StimulatorDocument15 pagesFunctional Electrical Nerve StimulatorJulia SalvioNo ratings yet
- Congenital Deformities ExplainedDocument46 pagesCongenital Deformities ExplainedJulia SalvioNo ratings yet
- CVA Ken Presentation FINALDocument110 pagesCVA Ken Presentation FINALJulia Salvio100% (1)
- Donatelli Chapter 2 Shoulder 2018Document16 pagesDonatelli Chapter 2 Shoulder 2018Julia SalvioNo ratings yet
- Electro NotesDocument9 pagesElectro NotesJulia SalvioNo ratings yet
- Culturally Effective Healthcare: Understanding Cultural Diversity in Medical PracticeDocument17 pagesCulturally Effective Healthcare: Understanding Cultural Diversity in Medical PracticeJulia SalvioNo ratings yet
- Cardiac RehabilitationDocument117 pagesCardiac RehabilitationJulia SalvioNo ratings yet
- Etiology: Molecular Mimicry - Myelin-ReactiveDocument2 pagesEtiology: Molecular Mimicry - Myelin-ReactiveJulia SalvioNo ratings yet
- Cerebrovascular Accident: Causes, Risks & TreatmentDocument53 pagesCerebrovascular Accident: Causes, Risks & TreatmentJulia Salvio50% (2)
- Amputation Lower ExtremityDocument5 pagesAmputation Lower ExtremityJulia SalvioNo ratings yet
- Bobath Approach: Concepts and PrinciplesDocument30 pagesBobath Approach: Concepts and PrinciplesJulia SalvioNo ratings yet
- Shortwave and Microwave Diathermy: A Guide to Applications and EquipmentDocument31 pagesShortwave and Microwave Diathermy: A Guide to Applications and EquipmentJulia SalvioNo ratings yet
- 22 - ParkinsonsDocument2 pages22 - ParkinsonsJulia SalvioNo ratings yet
- Myasthenia GravisDocument2 pagesMyasthenia GravisJulia SalvioNo ratings yet
- 23 - DysraphismDocument2 pages23 - DysraphismJulia SalvioNo ratings yet
- Guillain-Barré Syndrome Causes, Symptoms, TreatmentDocument1 pageGuillain-Barré Syndrome Causes, Symptoms, TreatmentJulia SalvioNo ratings yet
- 24 - MyopathiesDocument1 page24 - MyopathiesJulia Salvio100% (1)
- 20 - PolioDocument1 page20 - PolioJulia SalvioNo ratings yet
- Amyotrophic Lateral Sclerosis: PathophysiologyDocument4 pagesAmyotrophic Lateral Sclerosis: PathophysiologyJulia SalvioNo ratings yet
- Pott's Disease Treatment and ManagementDocument1 pagePott's Disease Treatment and ManagementJulia SalvioNo ratings yet
- ChromosomesDocument24 pagesChromosomesapi-249102379No ratings yet
- Boala Cronica Obstructive: BpocDocument21 pagesBoala Cronica Obstructive: BpocNicoleta IliescuNo ratings yet
- GD&T WIZ Tutor Covers The Vast Breadth of Geometric Dimensioning and Tolerancing Without Compromising On The Depth. The Topics Covered AreDocument1 pageGD&T WIZ Tutor Covers The Vast Breadth of Geometric Dimensioning and Tolerancing Without Compromising On The Depth. The Topics Covered AreVinay ManjuNo ratings yet
- Ringkasan LaguDocument4 pagesRingkasan LaguJoe PyNo ratings yet
- Akhmatova, Anna - 45 Poems With Requiem PDFDocument79 pagesAkhmatova, Anna - 45 Poems With Requiem PDFAnonymous 6N5Ew3No ratings yet
- District Wise List of Colleges Under The Juridiction of MRSPTU BathindaDocument13 pagesDistrict Wise List of Colleges Under The Juridiction of MRSPTU BathindaGurpreet SandhuNo ratings yet
- Ketchikan Shipyard Improvements Plan CompleteDocument230 pagesKetchikan Shipyard Improvements Plan CompleteOpó Ishak Bawias Adare100% (1)
- CHEMICAL ANALYSIS OF WATER SAMPLEDocument5 pagesCHEMICAL ANALYSIS OF WATER SAMPLEAiron Fuentes EresNo ratings yet
- Types of Speech StylesDocument31 pagesTypes of Speech StylesRomnick BistayanNo ratings yet
- 2 5 Marking ScheduleDocument6 pages2 5 Marking Scheduleapi-218511741No ratings yet
- Class Opening Preparations Status ReportDocument3 pagesClass Opening Preparations Status ReportMaria Theresa Buscato86% (7)
- Geometric Sculpture From 72 PencilsDocument5 pagesGeometric Sculpture From 72 PencilsHugo Iván Gonzalez CruzNo ratings yet
- 1 PBDocument11 pages1 PBAnggita Wulan RezkyanaNo ratings yet
- Hydrocarbon: Understanding HydrocarbonsDocument9 pagesHydrocarbon: Understanding HydrocarbonsBari ArouaNo ratings yet
- Lateral capacity of pile in clayDocument10 pagesLateral capacity of pile in clayGeetha MaNo ratings yet
- Common Pesticides in AgricultureDocument6 pagesCommon Pesticides in AgricultureBMohdIshaqNo ratings yet
- Translation of Japanese Onomatopoeia Into Swedish (With Focus On Lexicalization)Document20 pagesTranslation of Japanese Onomatopoeia Into Swedish (With Focus On Lexicalization)Aldandy OckadeyaNo ratings yet
- 3.1 C 4.5 Algorithm-19Document10 pages3.1 C 4.5 Algorithm-19nayan jainNo ratings yet
- Oral Medication PharmacologyDocument4 pagesOral Medication PharmacologyElaisa Mae Delos SantosNo ratings yet
- MATHEMATICAL ECONOMICSDocument54 pagesMATHEMATICAL ECONOMICSCities Normah0% (1)
- The Interview: P F T IDocument14 pagesThe Interview: P F T IkkkkccccNo ratings yet
- Strategic Flexibility: The Evolving Paradigm of Strategic ManagementDocument3 pagesStrategic Flexibility: The Evolving Paradigm of Strategic Managementnanthini kanasanNo ratings yet
- Digital Water Monitoring and Turbidity Quality System Using MicrocontrollerDocument8 pagesDigital Water Monitoring and Turbidity Quality System Using MicrocontrollerIrin DwiNo ratings yet
- Best Home Oxygen Concentrators-Lowest Prices & Fast Shipping (Oxygen Machines) - 2021 - YuwellDocument1 pageBest Home Oxygen Concentrators-Lowest Prices & Fast Shipping (Oxygen Machines) - 2021 - YuwellPelayanan ResusitasiNo ratings yet
- Document-SAP EWM For Fashion 1.0: 1.general IntroductionDocument3 pagesDocument-SAP EWM For Fashion 1.0: 1.general IntroductionAnonymous u3PhTjWZRNo ratings yet
- 2 Druid StreetDocument4 pages2 Druid StreetthamestunnelNo ratings yet
- Administracion Una Perspectiva Global Y Empresarial Resumen Por CapitulosDocument7 pagesAdministracion Una Perspectiva Global Y Empresarial Resumen Por Capitulosafmqqaepfaqbah100% (1)
- Lesson Plan 2 Revised - Morgan LegrandDocument19 pagesLesson Plan 2 Revised - Morgan Legrandapi-540805523No ratings yet
- Business StrategiesDocument2 pagesBusiness Strategiesthristanlexter694No ratings yet
- Second Quarterly Examination Math 9Document2 pagesSecond Quarterly Examination Math 9Mark Kiven Martinez94% (16)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (14)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)