Professional Documents
Culture Documents
Radio - Musculoskeletal
Uploaded by
Von HippoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Radio - Musculoskeletal
Uploaded by
Von HippoCopyright:
Available Formats
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
LUMBAR SPINE BASICS AND ANATOMY
IMAGING METHODS
refers to the lower back, where the spine curves inward
toward the abdomen. 1. lumbar spine MRI (CHOICE OF MODALITY)
It starts about five or six inches below the shoulder – assess lumbar pain and mass
blades, and connects with the thoracic spine at the top 2. CT-SCAN
and extends downward to the sacral spine. 3. Myelography – inject contrast (can observe
Landmark: on xray, absence of rib (start of L1), then start narrowing/ballooning of SC, like protrusion)
counting... 4. Plain XRAY (standard views)
Compose of 5 (L1-L5) - are the biggest unfused vertebrae Lumbar spine - Standard views
in the spinal column, enabling them to support the weight AP and Lateral *pictures taken from net wala kc s book, so
of the entire torso I included pics for study guide
lumbar spine meets the sacrum at the lumbosacral joint
(L5-S1). This joint allows for considerable rotation L1 follows T12
Intervertebral spaces – in between vertebral bodies T12 –has a rib
Spinal canal – posterior to vertebral body attached to it
On MRI = as white area, with spinal fluid/CSF
Spinal canal
Each lumbar spine segment is comprised of: (see figure above)
1. Vertebral body
2. Joint facet
3. Pedicle
4. Lamina
5. Spinous processes
*Normal spine is LORDOTIC (curved anteriorly)
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 1 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
Lumbar spine systematic approach - Normal AP Dextro-kyphosis: rightward curve (like on the sample image of
kyphosis)
A FRACTURED LUMBAR VERTEBRAL (L1) BODY:
CT-SCAN MRI
NORMAL VS LORDOTIC
DISC PROTRUSION/HERNIATION/BULGING
REMEMBER:
Normal-just at the margin of the vertebral body
Stenosis- beyond the VB; has herniated and
extended/protrusion/bulging porsteriorly-> neural foramina
will be compromised
A bulge encroaching the spinal canal
Pre-fragment – separation from parent disc
THERE IS NO SPINAL CORD AT LUMBAR SPINE
A broad-based disc bulge has been said to be a bulging
annulus fibrosus, and
A focal disc bulge is a herniated nucleus pulposus.
KYPHOSIS
LEVO-KYPHOSIS: leftward curve
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 2 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
*pars articularis – the pillar connecting the vertebral
body to posterior element
*spotty dog sign – if there is a break/fracture in the
pillar or collar of dog, secondary to trauma, tumor
Spotty dog sign
Pars
articularis
T2-weighted image on MRI: spinal canal is white colored, KEY-HOLE DEFORMITY
due to water content Neural foraminal
stenosis
If black-colored= dehydrated or unhealthy disc
SPINAL STENOSIS
encroachment of the bony or soft tissue structures in the
spine on one or more of the neural elements, with
resulting symptoms.
classification of stenosis is on an anatomic basis:
1. central canal
2. neuroforaminal
3. lateral recess
* degenerative disease of the facets with bony hypertrophy (forward slippage of one vertebral body on a lower
most common cause of central canal stenosis that one) occurs from either slippage of two vertebral
encroaches on the central canal. bodies following bilateral spondylolysis or from DJD of
also the most common cause of lateral recess stenosis the facets or pars articularis with slippage of the
Spinal stenosis facets. Resulting to ANGULATION OF SPINAL CORD
*so ang common ng lahat ng stenosis ay: degenerative disease Bilateral spondylolysis can result in a large amount of
of the facets slippage, but facet DJD will usually result in only
*facet: joint either superior or inferior articulation minimal slippage.
If spondylolisthesis is severe, the result can be
central canal stenosis, neuroforaminal stenosis, or
both.
*if you have herniated disc, naturally you have spinal
canal stenosis. So pag may nagbu bulge, there is anterior
impingement of spinal canal, so meron kang spinal
stenosis
SPONDYLOLYSIS & SPONDYLOLISTHEIS
SPONDYLOLYSIS
Defects in the bony pars interarticularis
can be a source of low back pain and instability
*simply problem at articulation
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 3 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
POST-OPERATIVE CHANGES
causes including inadequate surgery (including missed
free disc fragments), postoperative scarring, failure of
bone grafting for fusion, and recurrent disc
protrusion.
1. Marrow Changes
patient with degenerative disc disease
shows fat suppression which represents granulation
tissue
2. Disc Infection
note the high signal in the disc
SKELETAL TRAUMA
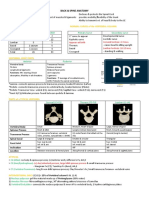
Meyerding grading scale
widely used to describe the degree of be sure to detect fracture or injury to the cervical
spondylolisthesis spine
The more caudal vertebral body is divided into assess neural/spinal canal stenosis
fourths, and the posterior corner of the more
determine spinal stability
cephalad vertebral body is marked at the position
where it has slipped forward. obtain XR: AP and translateral views
Compression Fracture:
Grade 1: If it has slipped forward only into the first Most frequent type of vertebral injury
quarter or 1/4 of the more caudal vertebral body. Burst-fractures
Grade 2: slippage into the second quarter or 50%
Seat-belt fractures
Grade 3: slippage into the third quarter or 75%
Grade 4: slippage into the tip
CERVICAL SPINE
cervical spine is one of the most commonly filmed
parts of the body in a busy emergency department
and can be one of the most difficult examinations to
interpret.
radiologist MUST HAVE the clinical history. If the
patient has been involved in an automobile accident
and has neck pain.
in a trauma victim who has neck pain or neurologic
deficits, obtain a CT scan.
Usually, a cross-table lateral view of the C-spine is
obtained first to avoid unduly moving the
patient who might have a cervical fracture. If the
lateral C-spine appears normal, the remainder of the
C-spine series, including flexion and extension views
(if the patient can cooperate), is obtained.
*avoid much movement of neck post-trauma upon obtaining
xray
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 4 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
in their size and appearance, although C7 is consistently
the largest. A fracture of one of the spinous processes, by
itself, is not a serious injury, but it occasionally heralds
other, more serious injuries.
additional info from the book:
five parallel (more or less) lines evaluation for step-
offs or discontinuity as follows EXAMPLES OF FRACTURES, DISLOCATIONS, AND OTHER
Line 1 - is the prevertebral soft tissue and extends down the ABNORMALITIES
posterior aspect of the airway; it should be several
millimeters from the first three or four vertebral bodies JEFFERSON FRACTURE
and then moves further away at the laryngeal cartilage. It
should be less than one vertebral body width from the A blow to the top of the head, such as when an object
anterior vertebral bodies from C3 or C4 to C7, and it falls directly on the apex of the skull, can cause the
should be smooth in its contour. lateral masses of C1 to slide apart, splitting the bony
Line 2 - follows the anterior vertebral bodies and should be ring of C1.
smooth and uninterrupted. Anterior osteophytes can DISPLACEMENT OF C1 laterally causing neck pain
encroach on this line and extend beyond it and should
therefore be ignored in drawing this line. Interruption of
the anterior vertebral body line is a sign of a serious
injury.
Line 3 - is similar to the anterior vertebral body line (line 2)
except that it connects the posterior vertebral bodies.
Like line 2, it should be smooth and uninterrupted, and
any disruption signifies a serious injury.
Line 4 - connects the posterior junction of the lamina with the
spinous processes and is called the spinolaminar line.
The spinal cord lies between lines 3 and 4; therefore, any
offset of either of these lines could mean a bony
structure is impinging the cord. It takes very little force
against the cord to cause severe neurologic deficits, and
any bony structure lying on the cord must be recognized
as soon as possible.
Line 5 - is not really a line so much as a collection of points—
the tips of the spinous processes. They are quite variable
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 5 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
CLAY-SHOVELER FRACTURE FLEXION TEARDROP FRACTURE
a fracture of the C6 or C7 spinous process
causing the ligaments attached to the spinous Severe flexion of the cervical spine can cause a
processes (supraspinous ligaments) to undergo a disruption of the Posterior ligaments with anterior
tremendous force, pulling on the spinous process and compression of a vertebral body.
avulsing it. usually associated with spinal cord injury, often from
This can occur at any of the lower cervical spinous the posterior portion of the vertebral body being
processes displaced into the central canal.
HANGMAN FRACTURE UNILATERAL LOCKED FACETS
Severe flexion associated with some rotation, result
is an unstable, serious fracture of the upper cervical in rupture of the apophyseal joint ligaments and facet
spine that is caused by hyperextension anD joint dislocation.
distraction (such as hitting one’s head on a This can result in locking of the facets in an overriding
dashboard). WHIPLASH INJURY position that, in effect, causes some stabilization to
This is a fracture of the posterior elements of C2 and, protect against further injury.
usually, displacement of the C2 body anterior to C3.
often escape neurologic impairment
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 6 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
SEATBELT INJURY
is seen secondary to hyperflexion at the waist (as
occurs in an automobile accident while restrained by
a lap belt).
This causes distraction of the posterior elements and
ligaments and anterior compression of the vertebral
body.
It usually involves the T12, Ll, or L2
Several variations of this injury can occur:
1. a fracture of the posterior body is called a Smith MALLET FINGER OR BASEBALL FINGER
fracture and
2. a fracture through the spinous process is called a is an avulsion injury at the base of the distal phalanx
Chance fracture. where the extensor digitorum tendon inserts.
GAMEKEEPER’S THUMB
is an avulsion on the ulnar aspect of the first
metacarpophalangeal joint; this is where the ulnar
collateral ligament of the thumb inserts.
HAND AND WRIST
BENNETT FRACTURE
A small corner fracture of the base of the thumb, into
the carpometacarpal joint
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 7 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
ROLANDO FRACTURE
is a more serious type of Bennett fracture
A comminuted fracture of the base of the thumb that
extends into the articular surface
LUNATE/PERILUNATE DISLOCATION
Occurs when the ligaments between the capitate and
the lunate are disrupted, allowing the capitate to
dislocate from the cup-shaped articulation of the
lunate. AVASCULAR NECROSIS OF NAVICULAR
This is best seen on lateral views.
it is the proximal fragment that undergoes necrosis
diagnosed by noting increased density of the proximal
pole of the navicular
NAVICULAR FRACTURE
ARMS
MC fracture of the carpals
is a potentially serious injury because of the high rate
Colle’s Fracture
of avascular necrosis When avascular
Smith Fracture
usually requires surgical intervention with a metallic
Monteggia’s Fracture
screw and bone grafting to obtain healing.
Galeazzi’s Fracture
Shoulder dislocation
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 8 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
COLLE’S FRACTURE deformity of the forearm and is often treated by breaking
the bones with the patient under anesthesia and resetting
Fracture of distal radius with dorsal angulation of the distal them. Left untreated, a plastic bowing deformity can result
in reduced supination and pronation.
fragment; most common fx in the wrist
MONTEGGIA’S FRACTURE
fx of the proximal ulna, associated with dislocation of
the proximal radius at the elbow joint
Distal radius nafracture , with dorsal angulation, may lateral
view nag dorsally plate ang distal fragment
One of the most common fractures of the forearm is a
fracture of the distal radius and ulna after a fall on an
outstretched arm. How could you say this ulna and this is radius?
This results in a dorsal angulation of the distal forearm and Olecranon process in the elbow joint – ulna
wrist and is called a Colles fracture
In the forearm, a fracture of one bone should be
accompanied by a fracture of the other. If the second
SMITH FRACTURE (REVERSE COLLE’S) fracture is not present, a dislocation of the non fractured
bone usually occurs
Fracture of distal radius with palmar/ventral Most common example of this is a fracture of the ulna with
displacement a dislocation of the proximal radius
The dislocated radial head can be missed clinically and
develop into avascular necrosis with subsequent elbow
dysfunction.
Whenever the forearm is fractured, the elbow must be
examined to exclude a dislocation.
GALEAZZI’S FRACTURE
fx radial shaft with dislocation of inferior radioulnar
joint proximally at the area of the wrist
o cause by direct blow or fall on
outstretched hand with pronation
of forearm
When the fracture angulates volarly, it is called a
Smith fracture
Sometimes the radius and ulna suffer a traumatic insult,
and the force on the bones causes bending instead of a
frank fracture. This has been termed a plastic bowing
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 9 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
Anterior dislocation occurs when the arm is forcibly
externally rotated and abducted.
This is commonly seen when football players “arm tackle,”
when kayakers “brace” with the paddle above their heads
and allow their arms to get too far posterior, when skiers
GLENOHUMERAL JOINT DISLOCATION plant their uphill pole and get it stuck, and from other
similar athletic positions.
Radiographically, the diagnosis is easily made on an AP
Anterior dislocation – most common (99%) shoulder film: the humeral head is seen to lie inferiorly and
o subcoracoid medial to the glenoid
o subglenoid
Posterior dislocation can also be seen but rarely
Posterior dislocation can be a difficult diagnosis to make,
both clinically and radiographically.
An AP view may look completely normal, or nearly so. On
the AP view of a normal shoulder, the humeral head should
slightly overlap the glenoid forming what has been called a
“crescent sign.”
In a patient with a posterior dislocation, this crescent of
bony overlap is usually absent and a small space is seen
between the glenoid and the humeral head
The best way to unequivocally diagnose a dislocated
shoulder is to obtain a transscapular view.
The transscapular view is obtained by angling the x-ray
beam across the shoulder in the same plane as the blade of
the scapula. This gives an en face view of the glenoid, and
the humeral head can easily be related to it as either
normal, anterior, or posterior.
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 10 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
NORMAL ANATOMY OF THE SHOULDER JOINT humeral head often impacts on the inferior lip of the
glenoid causing an indentation on theposterosuperior
portion of the humeral head;
greater likelihood of recurrent dislocation, and some
surgeons use it as an indicator to intervene surgically to
prevent a recurrence
Bankart deformity
The humerus should be in the glenoid fossa. Once it
deviates from there, it is anteriorly located, it is
anterior / inferior dislocation of the shoulder joint
ANTERIOR DISLOCATION
Hill Sach’s deformity
deformity seen in the glenoid labrum on the inferior aspect
because of the dislocation
Post reduction, there is a defect or deformity on the glenoid
labrum
bony irregularity or fragment off the inferior glenoid, which
occurs from the same mechanism as the Hill–Sachs
deformity
inferior displacement of the humerus in relation to
the glenohumeral joint but the deformity seen like an
invagination of the area of the humeral head
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 11 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
someone visits on Xray, therefore you have to subject your
patient into nuclear imaging.
So, dun mo makikita yung HONDA SIGN, letter H sa sacrum.
PELVIS That is stress fracture on bone scan.
Said to occur in half the cases that have pelvic fractures.
They can be difficult to see on even the best of films
FRACTURE OF THE PELVIS because the sacrum is often hidden by bowel gas. In looking
for sacral fractures, one should examine the arcuate lines of
the sacrum bilaterally to see whether they are intact.
Fractures often interrupt these lines and, because of the
side-to-side asymmetry, can therefore be easily identified
SACRAL STRESS FRACTURES
Fracture of the pelvic bone, you have your iliac bone,
ischium and the pubic area. You have the femoral head in
the acetabulum both side. There should be symmetrical
obturator foramen,superior pubic ramus, inferior pubic
ramus right and left side
POLYFRACTURES
maybe simple or complex, maybe correlated with sacroiliac
joint dislocation. Very complex because of fracture in the
iliac bone, fracture of superior pubic ramus, dislocation of
symphysis pubis, that will be on Xray ha. Pag na CT scan,
there would be more findings like urinary bladder
pathology, iliac bone, dense spaces of symphysis pubis
CT scanning should be considered in almost all acetabular
fractures because of the possibility of free fragments and
subtle fractures that plain films do not show
in patients who are osteoporotic or who have undergone
SACRAL FRACTURES radiation therapy
we may see them on Xray we may also need them can present as patchy or linear sclerosis on the sacral ala
sometimes. that may or may not show cortical disruption on plain films
CT scan – fracture of the sacrum, with angulation of the These should be differentiated from metastatic disease
fragments, sequel of insufficiency fracture because more on because of their characteristic location, appearance, and
the heavy side there is stress fracture in the sacrum and if history of prior radiation and by seeing a cortical break.
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 12 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
CT will usually, but not always, demonstrate cortical
disruption
These fractures have a characteristic appearance on
radionuclide bone scans, which is termed the Honda sign
because of its appearance to the logo of the car. The Honda
sign is seen only with bilateral stress fractures; unilateral
fractures will have increased radionuclide uptake
throughout one sacral ala.
MR will demonstrate an area of diffuse low signal on T1WIs
corresponding to the area of involvement
Sacral stress fractures have also been termed insufficiency
fractures, indicating that the underlying bone is abnormal,
similar to a pathologic fracture.
HIP FRACTURE
Hip fractures in the elderly population can be very
LEGS Difficult to detect, and a high index of suspicion should be
maintained.
A negative plain film in an elderly patient with hip pain after
STRESS FRACTURES trauma (even relatively mild trauma) does not exclude a
The most serious stress fracture, and fortunately, one of the femoral neck fracture.
rarest, is the femoral neck stress fracture MR has been shown to be very useful in demonstrating
Rarely, these progress to complete fractures that, with femoral neck fractures that are occult
continued weight bearing, can displace; these are very
serious lesions occur in the distal diaphysis of the femur and TIBIAL PLATEAU FRACTURE
in the proximal, middle, and distal thirds of the tibia.
All of these stress fractures need to be treated with the
utmost caution because complete fractures are not
uncommon with continued stress.
Sclerosis in a weight-bearing bone that has a horizontal or
oblique linear pattern should be considered a stress
fracture until proved otherwise.
A history of repetitive stress is not always obtained, and
therefore, the diagnosis should not depend solely on the
history.
A stress fracture occasionally will appear somewhat
aggressive, with aggressive periostitis and no definite
linearity to the sclerosis If this is mistaken for a tumor and
undergoes biopsy, it
can be confused with a malignancy, with subsequent radical
therapy. Cross-table lateral plain film should be obtained in cases of
These should, therefore, not undergo biopsy under any knee trauma to look for a fat-fluid level; this indicates a
circumstance. If the clinical presentation is unusual for a fracture that allows fatty marrow to leak into the knee joint.
stress fracture and In the appropriate clinical setting, MRI or CT may be
necessary to make the diagnosis.
The plain films are not diagnostic, take additional films 1 or
2 weeks later.
CT and MR sometimes will better delineate the lesion.
Stress fractures can be difficult to diagnose radiologically
early on but should be straightforward after several weeks.
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 13 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
LISFRANC FRACTURE intertrochanteric - in between the greater and lesser
Named after a surgeon in Napoleon’s army who would do trochanter
forefoot amputations in patients with gangrenous toes as a subtrochanteric – below the trochanters
result of frostbite.
A fracture-dislocation of the tarsometatarsals.
If the dislocation is slight, it can be easily overlooked.
A key to normal alignment is that the medial border of the
second metatarsal should always line up with the medial
border of the second cuneiform.
If it does not, a Lisfranc fracture-dislocation should be
suspected.
This fracture is seen most commonly in patients who catch
the forefoot in something such as a hole in the ground or a
horseback rider falling and hanging by the forefoot in the
stirrups.
It is commonly seen as a neurotrophic or Charcot joint in
diabetics.
FRACTURE OF THE CALCANEUS
It matters for the orthopaedic surgeon we will be advising
the patient whether they put a different ways or unless a
rod there
Can be difficult to appreciate on routine radiographs. perisymmetrical dapat yan, kung ano makikita mo sa right,
Böhler angle is a normal anatomic landmark that should be makikita mo din sa left. Tingnan ang left and right hindi sila
looked for in every foot film when trauma has occurred
pantay.
If this angle is narrower than 20°, it indicates a compression
of the calcaneus, as seen in jumping injuries There is an angulation of the femoral head in relation to
shaft of the femur. That is basicervical fracture. The greater
and lesser trochanter but the fracture is not there, superior
FRACTURES OF THE FEMUR to that, which is basicervical area.
Different types:
subcapital – below the humeral head
transcervical – neck part
basicervical – below the neck part
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 14 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
With prosthesis
KNEE
Comprises of femur, tibia, fibula, patella, superimposing the most common dislocation of the foot
patellar fossa A serious fracture in the foot that can be missed
Leg – tibia, medially located the right tibia, left tibia, fibula radiographically when little or no displacement occurs is the
on lateral aspect Lisfranc fracture.
You see the tarsal bones, metatarsals and proximal, mid and It is named after a surgeon in Napoleon’s army who would
do forefoot amputations in patients with gangrenous toes
distal.
as a result of frostbite.
The Lisfranc fracture is a fracture-dislocation of the
SPECIAL TYPES OF FRACTURES
tarsometatarsals. If the dislocation is slight, it can be easily
STRESS FRACTURES - will occur in normal bone or abnormal
overlooked. A key to normal alignment is that the medial
bones subjected to repeated cyclic loading border of the second metatarsal should always line up with
the medial border of the second cuneiform.
FATIGUE FRACTURE – if there is application of abnormal If it does not, a Lisfranc fracture-dislocation should be
stress bone with normal elastic resistance (constantly suspected.
marching, training as military recruits) This fracture is seen most commonly in patients who catch
the forefoot in something such as a hole in the ground or a
INSUFFICIENCY FRACTURE – application of normal stress
horseback rider falling and hanging by the forefoot in the
kahit gaano kagaan yung load but then if the bone is stirrups. It is commonly seen as a neurotrophic or Charcot
pathologic, or deficient in elastic resistance then joint in diabetics.
LISFRANC FRACTURE DISLOCATION – dorsal dislocation of SKELETAL “DO NOT TOUCH” LESIONS
the tarsometatarsal joint
Post traumatic lesions
Normal variants
Obviously benign lesions
Be careful on reporting them because they are not
suppose to be biopsy or not suppose to be touch.
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 15 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
POST TRAUMATIC LESIONS AVULSION INJURY
Myositis ossificans
Avulsion injuries
Cortical desmoid
Trauma
Discogenic vertebral sclerosis
Fractures
Pseudoislocation of the humerus
MYOSITIS OSSIFICANS
If you have avulsion injury in the iliac bone, you don’t do
anything on it. Might give patient some analgesics
These injuries can have an aggressive radiographic
appearance, but because of their characteristic location at
ligament and tendon insertion sites (e.g., anterior-inferior
iliac spine or ischial tuberosity), they should be recognized
as benign .
As with myositis ossificans, delayed films of several weeks
will usually allow the problem case to become more
radiographically clear.
Circumferential classification with lucent center. By clinical Biopsy can lead to the mistaken diagnosis of a sarcoma and
alone, you will see calcification (black area) that will be a should therefore be avoided
benign tumor, no touchy lesion because it does not
CORTICAL DESMOIDS
necessitate biopsy
an example of a lesion that should not undergo biopsy
because its aggressive histologic appearance can often
mimic a sarcoma
The typical radiologic appearance of myositis ossificans is
circumferentialcalcification with a lucent center
best appreciated on a computed tomographic scan.
Occasionally, the peripheral calcification of myositis
ossificans can be too faint to appreciate; in these cases, a
computed tomographic scan should help, or delayed films 1
or 2 weeks later are recommended.
Thickening on the posterior aspect of femur. Result to
avulsion of adductor magnus muscle if there is unusual
thickening that is cortical desmoids
is a process on the medial supracondylar ridge of the distal
femur that is considered by many to be the result of an
avulsion of the adductor magnus muscle.
It occasionally simulates an aggressive lesion
radiographically, and, histologically, it can look malignant.
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 16 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
In many instances, biopsy has led to amputation for this May create worry to the attending physician but if there is
benign, radiographically characteristic lesion. sclerosis of the adjoining endplates, narrowing that must be
Cortical desmoids occur only on the posteromedial condyle discogenic vertebral sclerosis
of the femur. Most often is sclerotic and focal. It is always adjacent to the
They might or might not be associated with pain and can endplate, and the associated disc space should be narrow.
have increased radionuclide uptake on a bone scan. Osteophytosis is invariably present. It really is a variant of a
They might or might not exhibit periosteal new bone and Schmorl node and should not be confused with a
usually occur in young people. metastatic focus.
Biopsy should be avoided in all cases. On occasion, it can be lytic or even mixed lytic-sclerotic.
Painful cortical desmoids should become asymptomatic The typical clinical setting is a middle-aged woman with
with rest. chronic low back pain.
They are often seen as an incidental finding on MRI of the Old films often confirm the benign nature of this process.
knee and have a characteristic appearance In the setting of disc space narrowing and osteophytosis,
focal sclerosis adjacent to an endplate should not undergo
TRAUMA biopsy
Can lead to large, cystic geodes or subchondral cysts near
joints and can be mistaken for other lesions, resulting in a FRACTURES
biopsy being ordered. Although the biopsy specimen is not Will be the cause of extensive osteosclerosis and periostitis,
likely to mimica malignant process, it is nevertheless
which can mimic a primary bone tumor.
avoidable.
Lack of immobilization can result in exuberant callus, which
Because geodes from degenerative disease almost always
can be misinterpreted as aggressive periostitis or even new
are associated with additional findings such as joint space
tumor bone.
narrowing, sclerosis, and osteophytes, a diagnosis should be
made radiographically Results of a biopsy in such a case might resemble a
malignant lesion; therefore, any case associated with
DISCOGENIC VERTEBRAL STENOSIS trauma should be carefully reviewed for a fracture.
PSEUDODISLOCATION OF THE HUMERUS
Sclerotic and focal adjacent to the endplate, narrowed disc results from a fracture with hemarthrosis, which causes
space and osteophytes. Often confused for metastatic distension of the joint and migration of the humeral head
disease (gosh, nag RAP siya dito) inferiorly.
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 17 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
An axial or transscapular view shows it is not anteriorly or PSEUDOCYST OF THE HUMERUS
posteriorly dislocated (the usual forms of shoulder
dislocation) but merely inferiorly subluxated.
On an anteroposterior view, it can mimic a posterior Another entity often confused for a lytic pathologic lesion is
dislocation in that the normal superimposition of the a pseudocyst of the humerus
humeral head and the glenoid is missing. This is merely an anatomic variant caused by the increased
Often, attempts are made to “relocate” the humeral ancellous bone in the region of the greater tuberosity of the
head, which, of course, are both fruitless (because it is not humerus that gives this region a more lucent appearance on
dislocated) and painful. radiographs
A fracture is invariably present, and if not seen on the With hyperemia and disuse caused by rotator cuff
initial films, it should be sought after with additional views. problems or any other shoulder disorder, this area of
lucency may appear strikingly more lucent and mimic a lytic
The transscapular or the axial view is the key to making the
lesion.
diagnosis of a pseudodislocation.
If necessary, the joint can be aspirated to confirm the
OS ODOINTODEUM
presence of a bloody effusion and to show the normal
position of the humeral head when fluid has been removed
from the joint
NORMAL VARIANTS
DORSAL DEFECT OF THE PATELLA
There is a defect in patella, dorsal defect in patella there
should be thicken of the fracture. To another view, AP view
then correlate. If there is no trauma and incidentally, no
defect there, therefore must be due to dorsal defect of
patella. This may be mistaken as metastatic disease but if
you follow up the patient and does not show any increase in
size, changes in the character then it must be a benign
finding.
A normal variant that has been described in the patella that
can be mistaken for a pathologic process is a lytic defect in
the upper, outer quadrant called a dorsal defect of the
patella The dens maybe separated but in normal variant, what you
It can mimic a focus of infection or osteochondritis called as os odointodeum, yung unfused dens, mimics
dissecans. fractured dens. Kapag nakakiyta kayo ng ganyan tapos wala
It is a normal developmental anomaly, however, and naman trauma, likely anatomic variants yan.
because of its characteristic location, it should not undergo A normal variant of the cervical spine that may, in fact, be
biopsy. posttraumatic.
On MR, it will have an appearance similar to many other It is an unfused dens that may move anterior to the C2 body
bony lesions, that is, low signal on T1-weighted images and with flexion and can mimic a fractured dens. Many of these
high signal on T2-weighted images require surgical fixation; some surgeons fuse every case,
believing that they are all unstable.
Radiologists should recognize that this process is not acute
and, thus, save the patient halo fixation and possible
immediate surgical intervention.
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 18 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
Most of these cases are seen after trauma, and if no
neurologic deficits are present, these patients can be seen BONE ISLANDS
electively and spared the morbidity associated with
treatment of the acutely fractured cervical spine.
The radiologic signs for recognizing an os odontoideum are
the smooth, often well-corticated, inferior border of the
dens and the hypertrophied, densely corticated anterior
arch of C1
OBVIOUSLY BENIGN LESIONS
Nonossifying fibroma
Bone islands
Early bone infarction
NON OSSIFYING FIBROMA
usually oblong, usually assumes the coarse or long axis of
the bone, elongated, following the trabecula of the bone
and doesn’t show any changes
Not a radiographic dilemma when they are 1 cm or less in
size.
Occasionally, however, they grow to golf ball size or larger
and mimic sclerotic metastases (Fig.
They are always asymptomatic.
Radiographically, two signs can be found to help distinguish
giant bone islands from metastases:
First, bone islands usually are oblong, with their long axis in
the axis of stress on the bone, for example, in a long bone
they align themselves along the axis of the diaphysis.
Second, the margins of a bone island, if examined closely,
usually reserved for defects larger than 2 cm. will show bony trabeculae extending from the lesion into
They are, classically, lytic lesions located in the cortex of the the normal bone in a spiculated fashion
metaphysis of a long bone and have a well-defined, often
sclerotic, scalloped border with slight cortical expansion UNICAMERAL BONE CYST
They are almost exclusively found in patients younger than
the age of 30 years; hence, the natural history of the lesion
is involution.
As they involute, they fill in with newbone, giving it a
sclerotic appearance; thus, they can have some increased
radionuclide activity on bone scans.
They are most often mistaken for an area of infection,
eosinophilic granuloma, fibrous dysplasia, or aneurysmal
bone cyst.
They are asymptomatic and have never been reported to
be associated with malignant degeneration.
On occasion, a pathologic fracture can occur through these
lesions, but most surgeons do not advocate prophylactic
curettage to prevent fracture, as with unicameral bone
cysts.
Nonossifying fibromas can be quite large but invariably
have a benign appearance and biopsy should be avoided.
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 19 of 20
adiuvante Dei gratia doctorum factionis 2014-2015
SUBJECT: MUSCULOSKELETAL DRA. MARIE
NELL RAGUNJAN
RADIOLOGY PART 2
are often prophylactically curettaged and packed so as to
prevent fracture with subsequent deformity.
When these cysts occur in the calcaneus, however, they
should be left alone.
They always occur in the anterior-inferior portion of the
calcaneus, an area that does not receive undue stress.
In fact, a pseudotumor of the calcaneus is seen in the
identical position because of the absence of stress and the
resulting atrophy of bony trabeculae
These lesions are asymptomatic, only rarely fracture, and
should not suffer the same fate as their counterparts in long
bones, that is, surgical removal.
BONE INFRACTION
Early in the course of its development, a bone infarct can
have a patchy or a mixed lytic-sclerotic pattern or even
resemble a permeative process.
In a patient with bone pain and a permeative bone lesion,
many aggressive disorders head the differential list and a
biopsy soon ensues.
If this process can be noted to be multiple and in the
diametaphyseal region of a long bone, especially if the
patient has an underlying disorder such as sickle cell anemia
or systemic lupus erythematosus, areas of early bone
infarction should be considered.
In some cases, the characteristic MR appearance of an
infarct may save a patient from biopsy when the plain films
are equivocal
"YOU ARE GROOT! Repeat to self. YOU ARE GROOT!.":p
CINDZ AND COOKIE
Page 20 of 20
You might also like
- Medicine AnswersDocument6 pagesMedicine AnswersHarsha Vipin100% (5)
- Spine PDFDocument7 pagesSpine PDFDRAHMEDFAHMYORTHOCLINIC100% (1)
- Case Report ScoliosisDocument67 pagesCase Report ScoliosisNurul Husna RashidNo ratings yet
- Evaluation of Lumbar Spine MRIDocument20 pagesEvaluation of Lumbar Spine MRIDharam Pandey100% (2)
- Bone PDFDocument14 pagesBone PDFVon HippoNo ratings yet
- Degenerative DiseasesDocument8 pagesDegenerative Diseasesadrian kristopher dela cruz100% (1)
- Radiography of The SpineDocument4 pagesRadiography of The SpineJorge VergaraNo ratings yet
- Cervical SpineDocument19 pagesCervical Spineمحمد الريسNo ratings yet
- Cranial Nerves: Afferents and EfferentsDocument4 pagesCranial Nerves: Afferents and Efferentsmay_74846422No ratings yet
- PM&R in Degenearative Joint DiseaseDocument66 pagesPM&R in Degenearative Joint DiseaseLorenz SmallNo ratings yet
- HA L2 Assessing Head, Neck, Breasts, and Lymphatic SystemDocument3 pagesHA L2 Assessing Head, Neck, Breasts, and Lymphatic SystemljtorreslriejyNo ratings yet
- Interpretation of MriDocument12 pagesInterpretation of Mrijimitkapadia100% (1)
- Referensi: Wisnu Prasetyo Adhi, Sst. FTRDocument19 pagesReferensi: Wisnu Prasetyo Adhi, Sst. FTRWisnu Prasetyo AdhiNo ratings yet
- OSCE Cerebellar Examination PDFDocument6 pagesOSCE Cerebellar Examination PDFriczen vilaNo ratings yet
- Spinal Cord and Its Lesions - Dr. Mattheus (2023)Document8 pagesSpinal Cord and Its Lesions - Dr. Mattheus (2023)Noreen Hannah GabrielNo ratings yet
- THE SPINE-b-1Document37 pagesTHE SPINE-b-1Justine NyangaresiNo ratings yet
- Paralysis in Dogs and CatsDocument56 pagesParalysis in Dogs and Catscat clinic pdhbNo ratings yet
- Cervical SpineDocument3 pagesCervical SpineCherrie MaeNo ratings yet
- SPINEDocument8 pagesSPINEadrian kristopher dela cruzNo ratings yet
- Neurologic Conditions 1 SciDocument5 pagesNeurologic Conditions 1 SciEdward De LeonNo ratings yet
- 5-Thoacolumbar SpineDocument20 pages5-Thoacolumbar SpineJULIONo ratings yet
- X Ray Spine JihanDocument25 pagesX Ray Spine JihanJihan AnisaNo ratings yet
- Spinal Cord Anatomy, Localization, and Overview of Spinal Cord SyndromesDocument25 pagesSpinal Cord Anatomy, Localization, and Overview of Spinal Cord SyndromesValentina Pimentel PatiñoNo ratings yet
- Vertebral Column of DogDocument3 pagesVertebral Column of DogEmit Rosary PenetranteNo ratings yet
- The Abdomen: E Sther Sunday C. Faller, RMT, MDDocument7 pagesThe Abdomen: E Sther Sunday C. Faller, RMT, MDMarimiel PagulayanNo ratings yet
- Modern CircuitDocument28 pagesModern Circuitمركز ريلاكس للعلاج الطبيعيNo ratings yet
- Vertebral Column and Contents of The Vertebral CanalDocument6 pagesVertebral Column and Contents of The Vertebral CanalCay KaiNo ratings yet
- Neurosurg Le1 TransDocument30 pagesNeurosurg Le1 Transd99452727No ratings yet
- GFHDocument34 pagesGFHaisa mutiaraNo ratings yet
- SPINEDocument8 pagesSPINEadrian kristopher dela cruzNo ratings yet
- Telaah 1Document3 pagesTelaah 1anri albarruNo ratings yet
- Spondylitis TBDocument47 pagesSpondylitis TBSadam_fasterNo ratings yet
- W3 MHSB LEC2 Ascending Fiber Tract in The Spinal Cord For GSS Impulses From The Head Trunk ExtremitiesDocument4 pagesW3 MHSB LEC2 Ascending Fiber Tract in The Spinal Cord For GSS Impulses From The Head Trunk ExtremitiesjoydalanonNo ratings yet
- DiagnosticsDocument16 pagesDiagnosticsSalwa ZeinNo ratings yet
- Radiology SignDocument25 pagesRadiology Signمركز ريلاكس للعلاج الطبيعيNo ratings yet
- Isolated Abducens Nerve Palsy: Update On Evaluation and DiagnosisDocument1 pageIsolated Abducens Nerve Palsy: Update On Evaluation and DiagnosisalecsaNo ratings yet
- Neuroana Topic 3 LectureDocument6 pagesNeuroana Topic 3 LecturexoNo ratings yet
- Current Diagnosis and Management of Cervical Spondylotic MyelopathyDocument20 pagesCurrent Diagnosis and Management of Cervical Spondylotic MyelopathyaisyahNo ratings yet
- 8.thoracic BlocksDocument39 pages8.thoracic BlocksMiguel AradaNo ratings yet
- Canal Stenosis Related To Degenerative DiskDocument38 pagesCanal Stenosis Related To Degenerative DiskNugroho SigitNo ratings yet
- Ultrasound-Guided Lumbar Central Neuraxial Block 2016Document8 pagesUltrasound-Guided Lumbar Central Neuraxial Block 2016drkis20100% (1)
- Anatomic Localization in Clinical Neurology: GeneralitiesDocument11 pagesAnatomic Localization in Clinical Neurology: GeneralitiesChennieWong100% (1)
- Presented By: Directed By:: Department of Tashreeh-UL-Badan (Anatomy)Document38 pagesPresented By: Directed By:: Department of Tashreeh-UL-Badan (Anatomy)QC quadcoreNo ratings yet
- Spine Injury Slide DR ML Final EditionDocument63 pagesSpine Injury Slide DR ML Final Editionerica luisNo ratings yet
- ISMT 12 - Day 383 - Vito - Lumbopelvic Fixation TechniquesDocument18 pagesISMT 12 - Day 383 - Vito - Lumbopelvic Fixation TechniquesVito MasagusNo ratings yet
- Static Palpation of The Spine FINALDocument13 pagesStatic Palpation of The Spine FINALPrathap KumarNo ratings yet
- Lumbar Spinal StenosisDocument13 pagesLumbar Spinal Stenosis7w7dzjhgbqNo ratings yet
- Radial Nerve Compression RaDocument28 pagesRadial Nerve Compression RaIndra RanteNo ratings yet
- OSULLIVAN y GLASS 2017 Cip Physitis A Fracture-In-An-English-BulldogDocument4 pagesOSULLIVAN y GLASS 2017 Cip Physitis A Fracture-In-An-English-BulldogWendy Gabriela Mayén AriasNo ratings yet
- Special Review On Knee Joint and Related Structures Part 1Document2 pagesSpecial Review On Knee Joint and Related Structures Part 1Jeffrey RamosNo ratings yet
- Anatomia Da ColunaDocument59 pagesAnatomia Da ColunaPaula Duarte MarquesNo ratings yet
- Applied Epidural Anatomy CEACCP 2005Document3 pagesApplied Epidural Anatomy CEACCP 2005eryxspNo ratings yet
- Back Spine AnatomyDocument3 pagesBack Spine AnatomyNinjaNo ratings yet
- Bone CongenitalDocument33 pagesBone CongenitalRadio ResidentNo ratings yet
- Evaluation of Low Back Pain (Ray)Document81 pagesEvaluation of Low Back Pain (Ray)Naeem AminNo ratings yet
- The Sciatic Nerve Block: S. Shevlin, D. Johnston and L. TurbittDocument9 pagesThe Sciatic Nerve Block: S. Shevlin, D. Johnston and L. TurbittLucille IlaganNo ratings yet
- Neuroanatomy Notes 2010Document33 pagesNeuroanatomy Notes 2010Jennifer David InauenNo ratings yet
- Aging Spine: A Degenerative Cascade: TH STDocument4 pagesAging Spine: A Degenerative Cascade: TH STChristi EspinosaNo ratings yet
- Dr. Andi Dhedie P. Sam, M.Kes, SP - OTDocument31 pagesDr. Andi Dhedie P. Sam, M.Kes, SP - OTFebriyantiNo ratings yet
- LR Vor VSRDocument53 pagesLR Vor VSRAlfira UlfaNo ratings yet
- Gyne 2.6 - Benign and Malignant Tumors of The Ovaries and Fallopian TubesDocument8 pagesGyne 2.6 - Benign and Malignant Tumors of The Ovaries and Fallopian TubesVon HippoNo ratings yet
- Diagnostic Performance of International Ovarian Tumor Analysis IotaDocument7 pagesDiagnostic Performance of International Ovarian Tumor Analysis IotaVon HippoNo ratings yet
- Joint and Connective Tissue Disorders: QuestionsDocument11 pagesJoint and Connective Tissue Disorders: QuestionsVon HippoNo ratings yet
- Psychiatric 3: Substance Abuse (DR Rosales) : Substance Use Related DisordersDocument11 pagesPsychiatric 3: Substance Abuse (DR Rosales) : Substance Use Related DisordersVon HippoNo ratings yet
- Psychiatric 3: Suicide (DR Rosales) June 8, 2011Document4 pagesPsychiatric 3: Suicide (DR Rosales) June 8, 2011Von HippoNo ratings yet
- Urinary Tract Infection (Book) : NephrologyDocument4 pagesUrinary Tract Infection (Book) : NephrologyVon HippoNo ratings yet
- KissPrep-Anatomy Physiology PDFDocument1 pageKissPrep-Anatomy Physiology PDFVon HippoNo ratings yet
- CLINPATH Finals ReviewerDocument28 pagesCLINPATH Finals ReviewerVon HippoNo ratings yet
- Psychopharmacology-Mood StabilizerDocument5 pagesPsychopharmacology-Mood StabilizerVon Hippo100% (1)
- PEDIA2 2.01b Fluids Electrolytes Summary TablesDocument4 pagesPEDIA2 2.01b Fluids Electrolytes Summary TablesVon HippoNo ratings yet
- Recalls: 2nd Shifting ExamDocument13 pagesRecalls: 2nd Shifting ExamVon HippoNo ratings yet
- Adult Emergency PDFDocument2 pagesAdult Emergency PDFVon HippoNo ratings yet
- Psychiatric EmergencyDocument3 pagesPsychiatric EmergencyVon HippoNo ratings yet
- Child PsychiatryDocument6 pagesChild PsychiatryVon HippoNo ratings yet
- Brainstem Lesions Trans 2019 PDFDocument8 pagesBrainstem Lesions Trans 2019 PDFVon HippoNo ratings yet
- Abdominal: Al HerniaDocument3 pagesAbdominal: Al HerniaVon Hippo100% (1)
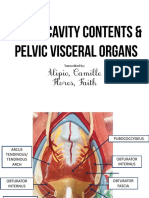
- Alipio, Camille Flores, Faith: Transcribed byDocument7 pagesAlipio, Camille Flores, Faith: Transcribed byVon HippoNo ratings yet
- Motor System: Three Types of Movement Generated by Motor SystemDocument10 pagesMotor System: Three Types of Movement Generated by Motor SystemVon Hippo100% (1)
- Clinical Scenario: CPT Case 9 Neonatal SepsisDocument15 pagesClinical Scenario: CPT Case 9 Neonatal SepsisVon HippoNo ratings yet
- 1) Any Medical Student or GraduateDocument27 pages1) Any Medical Student or GraduateVon HippoNo ratings yet
- Internal Medicine - Nephrology: Topic: Cystic Kidney Diseases Lecturer: Dra. Myrna NgoDocument3 pagesInternal Medicine - Nephrology: Topic: Cystic Kidney Diseases Lecturer: Dra. Myrna NgoVon HippoNo ratings yet
- Book: - RecordingDocument8 pagesBook: - RecordingVon HippoNo ratings yet
- Renal Cell CarcinomaDocument3 pagesRenal Cell CarcinomaVon HippoNo ratings yet
- Compilation of Platings in MicrobiologyDocument6 pagesCompilation of Platings in MicrobiologyVon HippoNo ratings yet
- Biochem: Gene Expression Part 2: Recap of Transcription (Part 1 of Lecture)Document14 pagesBiochem: Gene Expression Part 2: Recap of Transcription (Part 1 of Lecture)Von HippoNo ratings yet
- 2013 Compiled para Exams and Shiftings PDFDocument27 pages2013 Compiled para Exams and Shiftings PDFVon HippoNo ratings yet
- Fluid and Electrolytes YMDocument8 pagesFluid and Electrolytes YMVon HippoNo ratings yet
- NEPHRO - Renal Stones PDFDocument3 pagesNEPHRO - Renal Stones PDFVon HippoNo ratings yet
- Hemodialysis: Navigation SearchDocument14 pagesHemodialysis: Navigation SearchepingNo ratings yet
- Consulta. Roux-En-Y Gastric Bypass Surgery For Morbid ObesityDocument9 pagesConsulta. Roux-En-Y Gastric Bypass Surgery For Morbid ObesityAle LizárragaNo ratings yet
- Jamaophthalmology Biswas 2016 Oi 160055Document8 pagesJamaophthalmology Biswas 2016 Oi 160055Ghalia HayetNo ratings yet
- ANTIBIOTIKDocument20 pagesANTIBIOTIKGudang FarmasiNo ratings yet
- Techniques On Vertical Ridge Augmentation: Indications and EffectivenessDocument30 pagesTechniques On Vertical Ridge Augmentation: Indications and Effectivenessrmartins76No ratings yet
- Journal Club I: Methods To Check Occlusal Clearance During Tooth PreparationDocument16 pagesJournal Club I: Methods To Check Occlusal Clearance During Tooth Preparationshaikhhumaira08No ratings yet
- CD HORIZON® LONGITUDE® II Surgical TechniqueDocument56 pagesCD HORIZON® LONGITUDE® II Surgical Techniquelavern antalanNo ratings yet
- Step by Step Anaesthesia in Dentistry Local and GeneralDocument208 pagesStep by Step Anaesthesia in Dentistry Local and Generaldrnadeemulla khanNo ratings yet
- Prosthesis: Uganeswary VenugopalDocument14 pagesProsthesis: Uganeswary VenugopalUganeswary VenugopalNo ratings yet
- Types of AnesthesiaDocument27 pagesTypes of Anesthesiasncmanguiat.2202276.chasnNo ratings yet
- List of Videos To Watch On Wise MDDocument1 pageList of Videos To Watch On Wise MDalthrasherNo ratings yet
- Fracture RehabilitationDocument43 pagesFracture Rehabilitationnanahossam12345No ratings yet
- Immediate Restoration and Loading of Dental Implants: Clinical Considerations and ProtocolsDocument6 pagesImmediate Restoration and Loading of Dental Implants: Clinical Considerations and ProtocolsArlette MegNo ratings yet
- Private Tariff Schedule 2016Document24 pagesPrivate Tariff Schedule 2016Sirkd ShumbaNo ratings yet
- En SCD600Document2 pagesEn SCD600Surta DevianaNo ratings yet
- Aaron 800 - Eu AARON 900Document60 pagesAaron 800 - Eu AARON 900Carlos Equipamiento M-h M-vNo ratings yet
- Caustic Skin Burn Caused by Sodium Hydroxide: Images inDocument2 pagesCaustic Skin Burn Caused by Sodium Hydroxide: Images inJ. Antonio Mestas R.No ratings yet
- SBRT Vs SurgeryDocument7 pagesSBRT Vs SurgerySandra SkaržinskaitėNo ratings yet
- Midterm Exam 1Document6 pagesMidterm Exam 1Joanne Bernadette AguilarNo ratings yet
- KingMark ProductSheet 2015Document1 pageKingMark ProductSheet 2015Francisco GonzalezNo ratings yet
- Pre and Post Operative Management Required For Hip Replacement Including Investigation and Education - EditedDocument8 pagesPre and Post Operative Management Required For Hip Replacement Including Investigation and Education - EditedMarvin CJNo ratings yet
- Estimasi Biaya Bedah DigestifDocument2 pagesEstimasi Biaya Bedah DigestifDei RahayuNo ratings yet
- Apollo Hospitals: Towards Touching A ..Billion LivesDocument22 pagesApollo Hospitals: Towards Touching A ..Billion LivesAtyukti PachauriNo ratings yet
- Cosmetic Surgery An Interdisciplinary ApproachDocument1,004 pagesCosmetic Surgery An Interdisciplinary ApproachDaniel FilizzolaNo ratings yet
- Test Bank For Lets Code It 1st Edition by SafianDocument8 pagesTest Bank For Lets Code It 1st Edition by SafianRonald Sturgeon100% (32)
- Section 4: Medical Suppliers Section 4: Medical Suppliers: Albert Massaad S.A.R.LDocument7 pagesSection 4: Medical Suppliers Section 4: Medical Suppliers: Albert Massaad S.A.R.LTannousNo ratings yet
- Free Gingival Graft Vs Pedicle GraftDocument2 pagesFree Gingival Graft Vs Pedicle GraftSharannia Kumara VelooNo ratings yet
- Batiquin Vs Court of AppealDocument2 pagesBatiquin Vs Court of AppealFer Grace AniñonAcabalcuid CatayloNo ratings yet
- Archivetemp2018 TransCode Mock Test 4-AnswersDocument17 pagesArchivetemp2018 TransCode Mock Test 4-AnswersSathya Kishore100% (1)