Professional Documents
Culture Documents
NRS210 Clinical Assignment Packet
Uploaded by
Sally GigelioOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NRS210 Clinical Assignment Packet
Uploaded by
Sally GigelioCopyright:
Available Formats
1
OB Clinical
Assignment Packet
NRS 210/210C:
Nursing Concepts for the Multigenerational Childbearing Family
Revised 3/12/2020 KSM
2
Preparation for OB Clinical:
The OB Preparation Packet (which will require viewing the OB SIM video to
complete it) must be completed by the end of week 1.
Will be available to view/download within mydsn.net (NRS210) and the
Simulation Google Classroom as of Monday Week 11, and on Blackboard on
Day 1/ Week 1 of the quarter.
Students will need to arrive at clinical with:
1. OB Clinical Packet
2. OB Preparation Packet (completed)
3. OB Assignment Packet (not completed, since it will be completed during
the clinical)
4. Completed set of Med Cards (can convert the med log from the OB
Preparation Packet into 3x5 cards); placing a ring through the cards makes
them easier to use, if possible.
Instructors will check students off for these items when they arrive at clinical on
Day 1; lack of completion of the OB Preparation Packet will warrant a fail.
During clinical, complete the OB Care Plan and Newborn Assessment:
Students must complete the OB Assignment Packet, which includes a
comprehensive OB Nursing Care Plan and a hands-on Newborn Assessment. A
grade of 78% or higher is required on each to pass the course. The care plan is
written on one patient (mom or newborn) and includes three nursing diagnoses,
as well as goals, interventions and rationales describing how the interventions
support the goals. The OB care plan will be written for a patient cared for in the
clinical setting and graded by the DCN Clinical Instructor. The newborn
assessment will also be graded by the DCN Clinical Instructor. If your clinical
rotation has a preceptor or clinical scholar (hospital employee), the assignments
will be graded by the OB Didactic Professor.
*Once your assignments are graded please upload the assignments and the
rubrics to Blackboard in a timely fashion.*
Revised 2/27/2020 KSM
3
OB Nursing Care Plan
Student name_______________________________________________________ Cohort _______
Patient identifier (initials), age, G/P ________________________________________________________
Relevant Antepartum/Intrapartum History (comprehensive) ____________________________________
_____________________________________________________________________________________
Current Labor/PP/NB Status (provide brief write-up of status) __________________________________
_____________________________________________________________________________________
Assessment data Nursing Dx #1 (PES)
(relevant per
nursing diagnosis)
SMART Goal (Pt Interventions (RN Rationale (how do Evaluation (met/not
will…) will…) interventions met AEB,
promote goal?) continuation plan)
1. 1.
2. 2.
3. 3.
Nursing Dx #2 (PES)
SMART Goal Interventions Rationale Evaluation
1. 1.
2. 2.
3. 3.
Nursing Dx #3 (PES)
Revised 2/27/2020 KSM
4
SMART Goal Interventions Rationale Evaluation
1. 1.
2. 2.
3. 3.
Rubric for OB Nursing Care Plans
Student Name: Cohort: Grade Awarded for Assignment:
*Please use this rubric as a guide when formulating your care plan. Use information from the patient,
the chart, and your hands-on assessment to create a personalized care plan for each patient. Listed
below are the criteria that will be used to grade your care plans.* MUST BE TYPE-WRITTEN
4 3 2 1 0
Criteria Excellent Very Good Fair Not
Good Acceptable
>90%of 80- 70- 60- < 60% met
criteria 90% 80% 70%
met met met met
Patient Information
Patient identifier, age and G/P is included
Comprehensive antepartum/ intrapartum
information, including complications, is
included
Current Labor/ PP/ NB status (brief write-
up) is provided
Assessment Data:
Should include data such as vital signs, lab
values, physical exam findings, assessment
of attachment and bonding, breastfeeding,
Revised 2/27/2020 KSM
5
etc.
Chosen assessment data shows an
understanding of what to include as it
pertains to the nursing diagnosis
Assessment (comprehensively, in the
entire care plan) reflects physiological,
psychological, sociocultural, spiritual, and
economic data, as well as other lifestyle
factors
Criteria 4 3 2 1 0
Excellent Very Good Fair Not
Good Acceptable
Nursing Diagnosis Statements
Three [3] Nursing Diagnoses are
presented; two medical/ physical and one
psychosocial
NANDA approved diagnoses are used
Written in proper format (PES)
Relevant to assigned patient per
assessment
Listed from highest to lowest priority and
actual problems are listed before “risk for”
problems
Plan: Goal Statements
One goal is written for each nursing
diagnosis
Goals are patient-centered [PC] (Pt. will...)
Goals are Specific, Measurable, Attainable,
Realistic, Time-specific [SMART]
Nursing Interventions
Three interventions are presented per
goal, stated as instructions (“RN will”)
Are specific (what/ when/ how often/ how
Revised 2/27/2020 KSM
6
much)
Are related to goals
Are prioritized, reasonable, and achievable
Rationale for each intervention cited, using
APA format
Criteria 4 3 2 1 0
Excellent Very Good Fair Not
Good Acceptable
Evaluation and Revision of Plan
Evaluation statements (one per goal) state
whether goal was met/ partially met/ not
met
Evaluations directly reflect goal
statements
A continuation of care plan is included
(e.g. ongoing monitoring, education at the
time of discharge, etc.)
General
Care plan is readable, makes sense, is
practical and realistic; must be typed!
Spelling and grammar are correct
Rubric is attached to care plan
Score: ____________/100 (Maximum Score= 100 points) = _________%
Clinical Instructor/RN Signature Date
______________________________________________ _________________
*Students: Please attach this rubric to your OB Nursing Care Plan when you submit it for grading*
Newborn Assessment
Student name _____________________________________________ Cohort_________________
Newborn Time of delivery: APGAR 1/5/10 Birth weight _______grams
Identifier and
Birthdate:
Revised 2/27/2020 KSM
7
Current weight _____grams
Length: Head circumference: Chest Gestational (Circle one)
circumference: age:
_______cm ______cm
_________ cm
AGA SGA LGA
Maternal age ____________ G___/ P________ Blood Type _______ GBS Status ______________
Labor Hx: Onset/ total hrs of labor _______________________________________________________
AROM/ SROM time___________ Meconium stained fluid or terminal meconium? ______________
Maternal medications/ analgesia _________________________________________________________
Antepartum/ Intrapartum complications ___________________________________________________
Delivery: NSVD/ time __________________ Vacuum/forceps _______________________________
C/S: Planned/ Urgent/ Emergent Reason _____________________________________
Cord clamped at __________min. Skin-to-skin _______________min
Newborn resuscitation required? _________________________________________________________
Newborn blood sugar (in preterm, postterm SGA, LGA, maternal diabetic, other), give level __________
Bilirubin (TcB or TSB) ___________ CCHD result ____________ Hearing screen result ____________
First feeding @ ____________ min/ hr of life Type of feeding (breast/ bottle) __________________
Complete the following by circling or highlighting exam findings, include any deviations from normal.
CATEGORY OBSERVATIONS COMMENTS (include
abnormal findings)
General Color: pink/ pale/ acrocyanosis/ jaundiced
Appearance
Cry: strong/ weak/ high-pitched
Tone: normal (flexed)/ hypotonic/ hypertonic
Revised 2/27/2020 KSM
8
Skin Peeling/ rash/ bruising/ vernix/ petechiae/
mongolian spots
Head Molding/ caput/ open flat fontanels/ cephalhematoma
Eyes Clear/ discharge/ jaundice/ hemorrhage
ENT Intact palate/ normal ear setting/ patent nares/ nasal
flaring
Airway patent? Upper airway congestion?
Chest Symmetrical/ clavicle (intact)/ fractured (L R)
Nipple placement/ breast tissue
Chest movement symmetrical/ ribs symmetrical
Respiratory RR ____
Clear/ equal bilaterally/ retractions/ grunting/ coarse
breath sounds (eg, crackles)/ apneic episodes
Heart HR _______
Regular rate/ peripheral pulses bilaterally (femoral)/
murmur/ PMI
Abdomen Soft/ distended/ bowel sounds (present, diminished,
absent), umbilical vessels ____, cord clamp
Genitalia Male/ female/ ambiguous
Testes descended (R, L), undescended
Female: pseudomenstruation/ discharge/ appearance
Anus Placement normal/ meconium (present/absent)
Anal wink?
Spine Gluteal folds (equal/ unequal)/ pilonidal dimple
Spine straight/ curved
Extremities Symmetrical movement/ polydactyly/ syndactyly
Flexion (range of motion)/ muscle tone
Revised 2/27/2020 KSM
9
Reflexes noted Moro/ grasp/ suck/ rooting/ swallow/ babinski/ tonic
neck/ trunk incurvation/ step
State Quiet awake/ alert/ active/ sleeping/ crying
Note other relevant care data, including maternal/infant interactions:
_____________________________________________________________________________________
Complete the following newborn pain assessment by circling or highlighting findings.
Revised 2/27/2020 KSM
10
Revised 2/27/2020 KSM
11
Revised 2/27/2020 KSM
12
Rubric for Newborn Assessment
Student Name: Cohort: Grade Awarded for Assignment:
10 9 8 7 6 5
Criteria Excellent Very Good Fair Poor Not
Good Acceptable
>90% of 70- 60- < 60%
criteria 80- 80% 70% met < 50% met
met 90% met met
met
1. Apgar score noted/ measurements
and gestational age accurately noted
2. Newborn testing accurately noted
(blood sugar, TcB/ TSB, CCHD, hearing)
3. Maternal data recorded accurately
4. Data relevant to delivery and
associated events or any
antepartum/intrapartum
complications
5. Labor history, including duration ROM
and mode of delivery noted
6. Medications in labor noted
7. Feeding information recorded
8. Head-to-toe assessment accurately
documented
9. NIPS score accurately documented
10. Student observed performing exam
and recording data
Clinical Instructor verifies observation of Newborn exam: Date
___________________________________________________ ____________________
Score: ________/100 (Maximum Score= 100 points) = ___________%
Revised 2/27/2020 KSM
13
*Students: Please attach this rubric to your Newborn Assessment when you submit it for grading*
Brief Head-to-Toe Assessment
This Brief Head-to-Toe assessment guide is a summary of the most common assessments done by
nurses in the acute care setting. Nursing students need to practice these often to develop their own
style of a thorough yet quick assessment of the patient’s status. Once the BHT is completed, if findings
are abnormal, nurses must decide and prioritize their next course of action through following the
remaining steps of the nursing process. **All palpation and auscultation must be done directly on the
skin** Please remember this assessment is only for reflection and is not to substitute a full head to toe
as appropriate for your patient. Pregnant women have additional assessment needs.
As you enter the patient’s room:
SWIPE – See Universal Safety Protocol
Observe patient & their response as you perform SWIPE as this initial communication will help you
assess the patient’s neuro status, thought processes, speech, etc.
Vital Signs:
T: __________ P: __________ R: __________ BP: __________ (manual) SpO2: ______ O2 delivery: ____
Pain: (OPQRSTU) ____________________________________________________________________
General Survey:
Neuro: appearance, behavior, hygiene, affect, mood, eye contact
Overall skin color; Breathing effort (rhythm & depth)
Head:
Level of Consciousness: Alertness and Orientation to person, place, time, situation; If altered, use
GCS
HEENT: symmetry/movement, deformities, skin integrity; PERRLA
(Perform associated Cranial Nerve assessments as indicated)
Thorax:
Respiratory: inspect chest for shape and respiratory effort; auscultate anterior/posterior lung
sounds
Cardiac: auscultate APEtoMan (S3/S4 sounds? murmurs?); auscultate apical HR for 1 minute
Gastrointestinal: inspect abdominal contour; auscultate bowel sounds in all 4 quads; light palpation,
last BM
Genitourinary: consider ability to void, incontinence, indwelling catheter placement and condition
Upper Extremities: (anterior/posterior)
Skin: Inspect for overall skin color and intactness; IV lines (peripheral); fingernail shape/condition
Cardiac: Inspect color, Palpate for temperature, edema, radial pulses & capillary refill on fingers
Musculoskeletal/Neuro: Inspect for deformities; Assess shoulder shrug, arm & grip strength and
sensation bilaterally
Lower extremities: (anterior/posterior)
Skin: Inspect for overall skin color and intactness
Cardiac: Inspect color, Palpate for temperature, edema, pedal pulses & capillary refill on toes
Musculoskeletal/Neuro: Inspect for deformities, check foot pushes, leg lifts, and sensation
bilaterally; May assess gait with the Get Up and Go test
Revised 2/27/2020 KSM
14
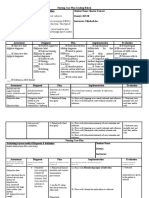
Medication Preparation Log
Student Name: _________________________________________________________________ Cohort _________________________
Clinical Rotation Date: _________________________
Patient Identifier: Diagnosis:
Code Status:
Allergies: Relevant Medical/Surgical History:
Pt. Dose/ Reason pt. Nrsg Implications/ MUST
Drug (Generic/Trade) Normal Range Route Frequency Classification receiving RX Top 4 Side Effects KNOW
Revised 3/12/2020 KSM
15
Pt. Dose/ Reason pt. Nrsg Implications/ MUST
Drug (Generic/Trade) Normal Range Route Frequency Classification receiving RX Top 4 Side Effects KNOW
Revised 2/27/2020 KSM
16
DCN Universal Safety Protocol
SWIPE In
State your name & title/ Scan environment
Wash hands
Identify patient (name/DOB)
Provide privacy
Explain procedure/Ask Permission
BRowN COW Out
Bed low
Rails up (cannot restrain)
Needed items in reach
Call light in reach
Open privacy curtain
Wash hands
Revised 3/12/2020 KSM
You might also like
- PN Day2Document10 pagesPN Day2Doneva Lyn MedinaNo ratings yet
- Must Use Forms Provided Must Be TypedDocument8 pagesMust Use Forms Provided Must Be TypedVincent Karimi GichimuNo ratings yet
- Nursing Care Plan (Compartment Sydnrome)Document6 pagesNursing Care Plan (Compartment Sydnrome)Zyiv BalogalNo ratings yet
- NR 465 Care of Childbearing Families and Reproductive HealthDocument5 pagesNR 465 Care of Childbearing Families and Reproductive HealthSam DanaNo ratings yet
- NUR 238 Fall 2019 Clinical Packet 6-7-19Document26 pagesNUR 238 Fall 2019 Clinical Packet 6-7-19Frank Loria100% (2)
- Nursing Care Plan Template and Grading RubricDocument4 pagesNursing Care Plan Template and Grading RubricSharon TanveerNo ratings yet
- Nursing Care Plan: Name of The StudentDocument7 pagesNursing Care Plan: Name of The Studentjmzm650No ratings yet
- Maharashtra State Board Nursing FormsDocument26 pagesMaharashtra State Board Nursing FormsSwarnima Robinson100% (1)
- Session 22Document6 pagesSession 22nicoleangela ubasroselloNo ratings yet
- A Brief Introduction to the Multi-Specialty Recruitment Assessment (MSRA)From EverandA Brief Introduction to the Multi-Specialty Recruitment Assessment (MSRA)Rating: 5 out of 5 stars5/5 (1)
- PN CJM AssignmentDocument7 pagesPN CJM Assignmenttcarmen49No ratings yet
- Electrolyte ImbalanceDocument4 pagesElectrolyte ImbalanceDoneva Lyn MedinaNo ratings yet
- Community Health Nursing Case Study: 2-Year-Old Boy with Fever and RashDocument5 pagesCommunity Health Nursing Case Study: 2-Year-Old Boy with Fever and RashIsaiah RabangNo ratings yet
- ANC EvaluationDocument2 pagesANC EvaluationKelbriline SaamoiNo ratings yet
- Orientation Plan and Evaluation ToolDocument10 pagesOrientation Plan and Evaluation Toolapi-259047759100% (2)
- 先天性斜颈2018循证临床实践指南Document8 pages先天性斜颈2018循证临床实践指南施凯No ratings yet
- Nrs 110 Lecture 1 Care Plan WorkshopDocument45 pagesNrs 110 Lecture 1 Care Plan Workshopalphabennydelta4468100% (2)
- NCMH Perfomance Eval Tool (1) .Xls PERF. CHECKLIST (PI)Document4 pagesNCMH Perfomance Eval Tool (1) .Xls PERF. CHECKLIST (PI)JAN MARIELLE GALLARDENo ratings yet
- VN - Med Surg I Clinical Perf EvaluationDocument4 pagesVN - Med Surg I Clinical Perf EvaluationvineelainjetyNo ratings yet
- Nursing Care Plan (NCP) Rubric Name of Student: Date: Student Number: Score: /4Document1 pageNursing Care Plan (NCP) Rubric Name of Student: Date: Student Number: Score: /4ameeralahmadi075No ratings yet
- Background of StudyDocument9 pagesBackground of StudySchuberg AliceNo ratings yet
- Log Book for Musculoskeletal AssessmentsDocument11 pagesLog Book for Musculoskeletal AssessmentsHarram SajjadNo ratings yet
- CHCDIS002 Follow Established Person-Centred Behaviour Supports SAB V3.4 1Document33 pagesCHCDIS002 Follow Established Person-Centred Behaviour Supports SAB V3.4 1sudipNo ratings yet
- 2018 5-4 Care PlanningDocument4 pages2018 5-4 Care PlanningEd SchnurnbergerNo ratings yet
- NCP Nursing Care PlanDocument7 pagesNCP Nursing Care Planalmayasa2002No ratings yet
- Nursing EvaluationDocument9 pagesNursing Evaluationnayla.vtcNo ratings yet
- HLTAAP001 Student Assessment Booklet (ID 96973)Document72 pagesHLTAAP001 Student Assessment Booklet (ID 96973)Show Ssti0% (5)
- PSDQ-Short Version Sample Report - PsyPackDocument11 pagesPSDQ-Short Version Sample Report - PsyPackNaina SinghNo ratings yet
- Eval d704 2016Document14 pagesEval d704 2016api-317443453No ratings yet
- Assignment - Spiritual DistresssDocument4 pagesAssignment - Spiritual DistresssRuth RallosNo ratings yet
- HS3214 - Final - Case Presentation RubricDocument5 pagesHS3214 - Final - Case Presentation RubricSelina LeowNo ratings yet
- He Sas 23Document10 pagesHe Sas 23Hoorise NShineNo ratings yet
- Pediatric Patient Teaching PlanDocument4 pagesPediatric Patient Teaching Planسُندس الحاجيNo ratings yet
- Nursing Care Plan - PPT HandoutDocument43 pagesNursing Care Plan - PPT HandoutCharlie Abagon100% (2)
- Formal Assignment: Nursing Care Plan: Basic Conditioning Factors (Document11 pagesFormal Assignment: Nursing Care Plan: Basic Conditioning Factors (Suraj ChavanNo ratings yet
- HLTAAP001 Recognise Healthy Body System SAB v3.0 - THEORYDocument41 pagesHLTAAP001 Recognise Healthy Body System SAB v3.0 - THEORYSujan AdhikariNo ratings yet
- Slide 7 - Patient - Nursing Care Plan (NCP)Document27 pagesSlide 7 - Patient - Nursing Care Plan (NCP)Gilang Cahyo Kumolo100% (2)
- BASIC STATISTICS CONCEPTS AND DATA COLLECTIONDocument47 pagesBASIC STATISTICS CONCEPTS AND DATA COLLECTIONkolNo ratings yet
- Mini-CEX and CbD Evaluation FormsDocument3 pagesMini-CEX and CbD Evaluation FormsEksa RachmadiansyahNo ratings yet
- Criteria and Rubric For Marking The Care PlanDocument3 pagesCriteria and Rubric For Marking The Care PlanHaitham ZraigatNo ratings yet
- Module 4 NRG 203 Intrapartum - 2023 2024Document20 pagesModule 4 NRG 203 Intrapartum - 2023 2024alliahjaneadlawanNo ratings yet
- Phases: Nursing CareDocument3 pagesPhases: Nursing CareKathryn LauditNo ratings yet
- Cardiovascular Module2Document27 pagesCardiovascular Module2Gracia MayaNo ratings yet
- 002n SOAPIEDocument3 pages002n SOAPIEKyles JumaritoNo ratings yet
- Gha Program StatementDocument1 pageGha Program StatementGlobal Health AffairsNo ratings yet
- Care PlanDocument2 pagesCare Planyousif AlblooshiNo ratings yet
- CR Excerpt Student Manual 2017Document2 pagesCR Excerpt Student Manual 2017Khang LuNo ratings yet
- CSSPT-406-2303-Fitness Testing Task 1 D2-2Document3 pagesCSSPT-406-2303-Fitness Testing Task 1 D2-2aidantabone0212No ratings yet
- Nursing Diagnosis To EvaluationDocument49 pagesNursing Diagnosis To Evaluation21912664No ratings yet
- Graduate Nurse PolicyDocument2 pagesGraduate Nurse PolicyclarengirausuiNo ratings yet
- Nursing Process EvaluationDocument3 pagesNursing Process EvaluationKyle VargasNo ratings yet
- Clinical Judgement 360 Concept MapDocument7 pagesClinical Judgement 360 Concept Mapapi-316178186No ratings yet
- Performance Appraisal of Intensive Care Unit NursesDocument5 pagesPerformance Appraisal of Intensive Care Unit NursesJoyce Albaladejo100% (1)
- Level 3 Self Assessment - Cardiovascular NursingDocument20 pagesLevel 3 Self Assessment - Cardiovascular NursingkkenNo ratings yet
- National Immunization Program: Manual of Procedures Booklet 9Document24 pagesNational Immunization Program: Manual of Procedures Booklet 9Blue PielagoNo ratings yet
- College of Nursing Evaluation Tool General Ward: Uc-Vpaa-Con-Form-13 Page 1of 2 June 2012 Rev 00Document2 pagesCollege of Nursing Evaluation Tool General Ward: Uc-Vpaa-Con-Form-13 Page 1of 2 June 2012 Rev 00clarheenaNo ratings yet
- Competency ChecklistDocument3 pagesCompetency ChecklistJon Bandola100% (1)
- LeeelectroncompDocument2 pagesLeeelectroncompapi-247490129No ratings yet
- Brookeperrycet 2Document7 pagesBrookeperrycet 2api-309581156No ratings yet
- Assessment Instructions and Coversheet Task 3-1Document4 pagesAssessment Instructions and Coversheet Task 3-1harryNo ratings yet
- Student Clinical Report SheetDocument2 pagesStudent Clinical Report SheetMike100% (4)
- Labour and Delivery Soap Note Free Word DownloadDocument6 pagesLabour and Delivery Soap Note Free Word DownloadSally GigelioNo ratings yet
- PT Assessment ToolDocument2 pagesPT Assessment ToolSally GigelioNo ratings yet
- Mentor and LD ChecklistDocument6 pagesMentor and LD ChecklistSally GigelioNo ratings yet
- ApplyingRestraints DocumentationDocument1 pageApplyingRestraints DocumentationSally GigelioNo ratings yet
- NRS210 Clinical Assignment PacketDocument16 pagesNRS210 Clinical Assignment PacketSally GigelioNo ratings yet
- ATI Skills Modules Checklist For Intravenous Therapy: Verify OrderDocument7 pagesATI Skills Modules Checklist For Intravenous Therapy: Verify OrderSally GigelioNo ratings yet
- Labour and Delivery Soap Note Free Word DownloadDocument6 pagesLabour and Delivery Soap Note Free Word DownloadSally GigelioNo ratings yet
- Schizophrenia: Biopsikologi James J W Kalat Siti Muthia Dinni, M. Psi., PsikologDocument17 pagesSchizophrenia: Biopsikologi James J W Kalat Siti Muthia Dinni, M. Psi., PsikologSalsabilaNo ratings yet
- Position SoughtDocument1 pagePosition Soughtapi-301736694No ratings yet
- Rcdso Ipac Selfaudit FormDocument15 pagesRcdso Ipac Selfaudit FormdoctorlupuNo ratings yet
- Night School by Richard WisemanDocument11 pagesNight School by Richard WisemansimasNo ratings yet
- GUIDE TO CLINICAL USES OF SPACE MAINTAINERSDocument6 pagesGUIDE TO CLINICAL USES OF SPACE MAINTAINERSKhalid AhmedNo ratings yet
- CASE IH MAXXUM 125 Multicontroller TRACTOR Service Repair Manual PDFDocument120 pagesCASE IH MAXXUM 125 Multicontroller TRACTOR Service Repair Manual PDFjfjksekdmeik100% (3)
- Budd-Chiari Syndrome As An Initial Presentation of Systemic LupusDocument5 pagesBudd-Chiari Syndrome As An Initial Presentation of Systemic LupusNatnael GetahunNo ratings yet
- Excerpts From Dr. Plotkin Deposition - January 2018Document137 pagesExcerpts From Dr. Plotkin Deposition - January 2018Elena ConstantinNo ratings yet
- Top 100 Biology GK Questions For SSC Exams (WWW - Thegkadda.com) PDFDocument3 pagesTop 100 Biology GK Questions For SSC Exams (WWW - Thegkadda.com) PDFMi MolNo ratings yet
- Ebook MriDocument26 pagesEbook MrikadekNo ratings yet
- Nur Jamal SKDocument54 pagesNur Jamal SKshjzjxhxnajsjdNo ratings yet
- 2008, Editrice Kurtis: Square-Stepping Exercise Versus Strength and Balance Training For Fall Risk FactorsDocument6 pages2008, Editrice Kurtis: Square-Stepping Exercise Versus Strength and Balance Training For Fall Risk Factorsnandhini raguNo ratings yet
- Abortion & ReligionDocument21 pagesAbortion & ReligionCeola WadeNo ratings yet
- T Cells & Autoimmunity, s3Document21 pagesT Cells & Autoimmunity, s3LiaAriestaNo ratings yet
- Ocular Exam GuideDocument2 pagesOcular Exam GuideMuhammad HaziqNo ratings yet
- Dentalconsent-Vizilite 0001Document4 pagesDentalconsent-Vizilite 0001Orlando GesualdoNo ratings yet
- Group 6Document37 pagesGroup 6LohithNo ratings yet
- Mauritius Government GazetteDocument2 pagesMauritius Government GazetteAmrit ChutoorgoonNo ratings yet
- Atrial Septal DefectDocument7 pagesAtrial Septal DefectRis Amy AyaNo ratings yet
- Body Revolution Syllabus DraftDocument4 pagesBody Revolution Syllabus Draftapi-508557357No ratings yet
- Technologies Diseases: Related To The Circulatory SystemDocument5 pagesTechnologies Diseases: Related To The Circulatory SystemHannahNo ratings yet
- Specimen Collection: Clini CalDocument81 pagesSpecimen Collection: Clini CalNoreen B. Bañagado100% (3)
- Safety Data Sheet for LOCTITE PC 5070 TAPEDocument13 pagesSafety Data Sheet for LOCTITE PC 5070 TAPEangga alvianNo ratings yet
- Activity-Accomplishment Report On 44th Anniversary CelebrationDocument3 pagesActivity-Accomplishment Report On 44th Anniversary CelebrationjohnNo ratings yet
- PCTH 400 - T2 SyllabusDocument2 pagesPCTH 400 - T2 SyllabusAliseyNo ratings yet
- Mahajan 2018Document14 pagesMahajan 2018nguyenvinh daoNo ratings yet
- Association Between Maternal Characteristics and The Risk of Isolated Maternal HypothyroxinemiaDocument7 pagesAssociation Between Maternal Characteristics and The Risk of Isolated Maternal HypothyroxinemiaAndres GallegosNo ratings yet
- Ultimate Aluminum Protectant: Section 1: IdentificationDocument6 pagesUltimate Aluminum Protectant: Section 1: IdentificationwoodywheelNo ratings yet
- Mapeh - Health 6: First Quarter-Module 1 Personal Health Issues and ConcernDocument10 pagesMapeh - Health 6: First Quarter-Module 1 Personal Health Issues and ConcernNICOLE ALANANo ratings yet
- Pelvic Anatomy Slides FINALDocument36 pagesPelvic Anatomy Slides FINALRajashekharNo ratings yet