Professional Documents
Culture Documents
Letters To The Editor: References
Uploaded by
Aji Prasetyo UtomoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Letters To The Editor: References
Uploaded by
Aji Prasetyo UtomoCopyright:
Available Formats
756 Letters to the Editor Journal of Vascular Surgery
August 2020
Within the CEA cohort, 1 patient experienced a tran- REFERENCES
sient ischemic attack (0.9%), and 4 patients developed 1. Rothwell PM, Eliasziw M, Gutnikov SA, et al. Analysis of pooled
a postoperative neck hematoma for which repeat inter- data from the randomised controlled trials of endarterectomy
for symptomatic carotid stenosis. Lancet 2003;361:107-16.
vention was needed (3.6%). During follow-up, 3 patients 2. Orrapin S, Rerkasem K. Carotid endarterectomy for symptomatic
(2.7%) developed symptomatic ipsilateral restenosis of carotid stenosis. Cochrane Database Syst Rev 2017;6:CD00181.
the carotid artery, 2 of which within 90 days of CAS. 3. Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP,
These patients were all successfully treated with CAS. Barnett HJM. Endarterectomy for symptomatic carotid ste-
Complications such as myocardial infarction or cerebral nosis in relation to clinical subgroups and timing of surgery.
Lancet 2004;363:915-24.
hyperperfusion syndrome were not reported in the CAS 4. Bonati LH, Lyrer P, Ederle J, Featherstone R, Brown MM.
and CEA groups. Percutaneous transluminal balloon angioplasty and stenting
With these results, we believe that a temporary CAS first for carotid artery stenosis. Cochrane Database Syst Rev 2012;9:
approach within our center is a safe and reasonable CD000515.
approach. Primary treatment with CAS could reduce
https://doi.org/10.1016/j.jvs.2020.04.476
the burden of care within hospitals and ensure adequate
and timely care for this patient group during a time of
limited capacity.
Risk of peripheral arterial thrombosis in
COVID-19
Joyce Hellegering, MD Since the report of the first COVID-19 cases in Wuhan
Maarten J. van der Laan, MSc, MD, PhD (China) on December 31, 2019, several thrombotic com-
Division of Vascular Surgery plications associated with this disease have been
Department of Surgery described.1,2 These have mainly included venous throm-
University Medical Center Groningen boembolic events3 and myocardial infarction.4 However,
University of Groningen we have noted a rapidly increasing occurrence of a not
Groningen, The Netherlands
previously described vascular complication in critically
ill patients: acute peripheral arterial thrombosis.
Erik-Jan de Heide, MD
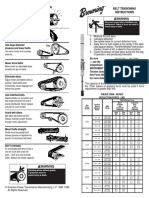
To date, in our institution (Hospital Clinic, Barcelona,
Department of Radiology Spain; a reference center for COVID-19 treatment), we
Medical Imaging Center
have diagnosed acute limb ischemia in four patients
University Medical Center Groningen
University of Groningen infected with COVID-19 that was attributed to the second-
Groningen, The Netherlands ary hypercoagulable state. Of the four patients, three had
presented with infrapopliteal arterial thrombosis of all
Maarten Uyttenboogaart, MD, PhD distal vessels in one or both legs (one and two patients,
Department of Radiology respectively; Fig). The fourth patient had presented with
Medical Imaging Center femoral-popliteal and radial-ulnar arterial thrombosis. All
University Medical Center Groningen four patients had associated distal cutaneous microembo-
University of Groningen lism of the toes or fingers, with progressive distal clinical
Groningen, The Netherlands
onset of symptoms: toe or finger dysesthesia and paresis,
Department of Neurology without muscular infarct. The mean patient age was
University Medical Center Groningen 71 years. The four patients (three men) had had no previous
University of Groningen severe comorbidities or known cardiovascular disease that
Groningen, The Netherlands could have caused the arterial embolisms. Acute ischemia
had appeared on average 15 days after the onset of respira-
Clark J. Zeebregts, MD, PhD tory COVID-19 symptoms. All four patients had previously
Division of Vascular Surgery been admitted to intensive care units because of severe
Department of Surgery respiratory syndrome, with high oxygen and dedicated
University Medical Center Groningen
treatment requirement (lopinavir/ritonavir, hydroxychloro-
University of Groningen
Groningen, The Netherlands quine, corticosteroids, azithromycin, anticoagulation, and,
eventually, tocilizumab or plasma exchange). Only one
Reinoud P. H. Bokkers, MD, PhD case had presented with coexisting venous thromboem-
bolism and splenic infarct. The blood samples revealed an
Department of Radiology
Medical Imaging Center average high D-dimer (>10,000 ng/mL), lactate
University Medical Center Groningen dehydrogenase (823 U/L), and ferritin (2473 ng/mL) levels,
University of Groningen with moderate elevation of C-reactive-protein, platelets,
Groningen, The Netherlands and leukocytosis, and decreased mean coagulation times.
Journal of Vascular Surgery Letters to the Editor 757
Volume 72, Number 2
REFERENCES
1. Terpos E, Ntanasis-Stathopoulos I, Elalamy I, Kastritis E,
Sergentanis TN, Politou M, et al. Hematological findings and
complications of COVID-19 [published online ahead of print
April 13, 2020]. Am J Hematol doi: 10.1002/ajh.25829.
2. Marietta M, Ageno W, Artoni A, De Candia E, Gresele P,
Marchetti M, et al. COVID-19 and haemostasis: a position
paper from Italian Society on Thrombosis and Haemostasis
(SISET) [published online ahead of print April 8, 2020]. Blood
Transfus doi: 10.2450/2020.0083-20.
3. Wang J, Hajizadeh N, Moore EE, McIntyre RC, Moore PK,
Veress LA, et al. Tissue plasminogen activator (tPA) treatment
for COVID-19 associated acute respiratory distress syndrome
(ARDS): a case series [published online ahead of print April 8,
2020]. J Thromb Haemost doi: 10.1111/jth.14828.
4. Dixon DL, Van Tassell BW, Vecchié A, Bonaventura A, Talasaz
A, Kakavand H, et al. Cardiovascular considerations in treating
patients with coronavirus (COVID-19) [published online ahead
of print April 2, 2020]. J Cardiovasc Pharmacol doi: 10.1097/
FJC.0000000000000836.
https://doi.org/10.1016/j.jvs.2020.04.477
Intra-arterial thrombosis associated with
Fig. Angiography computed tomography three-dimen- COVID-19
sional reconstruction of three cases of infrapopliteal
arterial thrombosis. Severe acute respiratory syndrome coronavirus 2
(SARS-CoV-2) is a global pandemic. The development
of an acquired thrombophilia with activation of the
Of the four cases, two underwent surgery. One patient had coagulation cascade in response to the inflammatory
undergone open bilateral popliteal direct thrombectomy process has been described.1 SARS-CoV-2 appears to
of all distal vessels and one had undergone open femoral- have an affinity for angiotensin-converting enzyme 2
popliteal and radial-ulnar thrombectomy. Both patients receptors that seem to be downregulated, which
recovered immediate patency of all declotted arteries may drive the proinflammatory/prothrombotic
and experienced improved clinical symptoms, despite consequences.2
the finding of segmental distal asymptomatic rethrombo- As this is a novel illness, there has been limited opportu-
sis at 24 hours after surgery (plantar arch or one of the distal nity to understand and to investigate the effect of SARS-
infrapopliteal vessels). The other two patients did not un- CoV-2. In severe disease, there appears to be elevation of
dergo surgery because of their extremely poor respiratory D-dimer levels. Prolongation of prothrombin time and
condition and relatively well-tolerated ischemia; these pa- activated partial thromboplastin time seems to be asso-
tients have continued to receive follow-up. ciated with an increased risk of acute respiratory distress
The vascular community should be aware of this new syndrome and death.3 The development of disseminated
thrombotic complication in critically ill patients with intravascular coagulation appears to be common in
COVID-19. It can be due to the hypercoagulable second- nonsurvivors.4
ary status, and surgery is a valuable treatment option for There appears to be an increased risk of pulmonary
complicated cases, despite the risk of rethrombosis. thromboembolic events in ventilated patients with
SARS-CoV-2, despite the administration of low-
Gaspar Mestres, MD, PhD molecular-weight heparin prophylaxis. In a small se-
Roger Puigmacià, MD ries of minimally invasive autopsies, a significant pro-
Carla Blanco, MD portion of patients were found to have small
Xavier Yugueros, MD, PhD fibrinous thrombi in pulmonary arterioles.1 Similar
Montserrat Esturrica, MD data have been described across Europe with revision
Vincent Riambau, MD, PhD of low-molecular-weight heparin prophylaxis dosing.
Department of Vascular Surgery As well as the described pulmonary thrombotic com-
Cardiovascular Institute plications, a series of early circuit occlusions has been
Hospital Clinic Barcelona encountered in patients on hemofiltration as a conse-
University of Barcelona quence of multiple organ dysfunction syndrome from
Barcelona, Spain
SARS-CoV-2.
You might also like
- (RCT) Cardiovascular Injuries After Covid-19 InfectionDocument7 pages(RCT) Cardiovascular Injuries After Covid-19 InfectionPatrick NunsioNo ratings yet
- Fibrinolysis shutdown on TEG predicts thrombotic risks in severe COVID-19Document12 pagesFibrinolysis shutdown on TEG predicts thrombotic risks in severe COVID-19Ria GandaNo ratings yet
- ECMO For COVID-19 Patients in Europe and Israel: LetterDocument5 pagesECMO For COVID-19 Patients in Europe and Israel: LetterJackson ErasmoNo ratings yet
- Thrombosis Research: A B C D e F G A e A A 1 F 1Document3 pagesThrombosis Research: A B C D e F G A e A A 1 F 1Natasya IntanNo ratings yet
- A Rare Vascular Complication in A COVID 19 Patient A Case Report of Free Floating Carotid ThrombusDocument6 pagesA Rare Vascular Complication in A COVID 19 Patient A Case Report of Free Floating Carotid ThrombusAthenaeum Scientific PublishersNo ratings yet
- Ijhbr January 2018 23-30Document8 pagesIjhbr January 2018 23-30farhanomeNo ratings yet
- St-Elevation Myocardialinfarction Inpatients With Covid-19 (About A Case Report and Review of The Litterature)Document5 pagesSt-Elevation Myocardialinfarction Inpatients With Covid-19 (About A Case Report and Review of The Litterature)IJAR JOURNALNo ratings yet
- Cardiac Pathology 6 Months After Hospitalization For COVID-19 and Association With The Acute Disease SeverityDocument11 pagesCardiac Pathology 6 Months After Hospitalization For COVID-19 and Association With The Acute Disease SeverityArdhia Kusuma PutriNo ratings yet
- Thrombosis Research: Full Length ArticleDocument6 pagesThrombosis Research: Full Length ArticleCarol GomezNo ratings yet
- Dutta 2017Document3 pagesDutta 2017Kartik DuttaNo ratings yet
- 2021 Thrombocytopenia and Intracranial Venous Sinus Thrombosis AfterDocument10 pages2021 Thrombocytopenia and Intracranial Venous Sinus Thrombosis AfterBeatriz VásquezNo ratings yet
- Ehac 515Document18 pagesEhac 515Phuoc NguyenNo ratings yet
- Salim 2009Document6 pagesSalim 2009raden chandrajaya listiandokoNo ratings yet
- HSHDDocument193 pagesHSHDRianda AkmalNo ratings yet
- Successful Surgical Management of Large Pulmonary Artery 2024 InternationalDocument5 pagesSuccessful Surgical Management of Large Pulmonary Artery 2024 InternationalRonald QuezadaNo ratings yet
- s40560-017-0223-2Document10 pagess40560-017-0223-2ERICK KUMAR BAUTISTA GOMEZNo ratings yet
- J Thromres 2012 05 016Document6 pagesJ Thromres 2012 05 016Alexandra RosaNo ratings yet
- J Jacc 2022 01 022Document16 pagesJ Jacc 2022 01 022hkNo ratings yet
- D-Dimer Cut-Off LevelsDocument2 pagesD-Dimer Cut-Off LevelsSoraya RezekiNo ratings yet
- Pathological Evidence of Pulmonary Thrombotic Phenomena in Severe COVID 19Document5 pagesPathological Evidence of Pulmonary Thrombotic Phenomena in Severe COVID 19Victor AugustoNo ratings yet
- Atm 08 23 1626Document12 pagesAtm 08 23 1626Susana MalleaNo ratings yet
- Gangi Et Al 2021 Imaging and Hematologic Findings in Thrombosis and Thrombocytopenia After Chadox1 Ncov 19Document8 pagesGangi Et Al 2021 Imaging and Hematologic Findings in Thrombosis and Thrombocytopenia After Chadox1 Ncov 19Valentina EnacheNo ratings yet
- 1 s2.0 S0140673620326581 MainDocument14 pages1 s2.0 S0140673620326581 MainSol LakosNo ratings yet
- Venous and Arterial Thromboembolic Complications in COVID-19 PatientsDocument6 pagesVenous and Arterial Thromboembolic Complications in COVID-19 PatientsWilliam MilesNo ratings yet
- TVP y Covid19Document28 pagesTVP y Covid19Nestor Alonso Lopez RubioNo ratings yet
- Endocarditis in The Elderly: Clinical, Echocardiographic, and Prognostic FeaturesDocument8 pagesEndocarditis in The Elderly: Clinical, Echocardiographic, and Prognostic FeaturesMehdi285858No ratings yet
- 1882-Article Text-7722-1-10-20200608 PDFDocument6 pages1882-Article Text-7722-1-10-20200608 PDFRyanNo ratings yet
- A 40 YearsDocument9 pagesA 40 YearsDra Mariana Huerta CampaNo ratings yet
- Gambar MappingDocument9 pagesGambar Mappingyana kristinaNo ratings yet
- 4Document16 pages4Ihsanul Ma'arifNo ratings yet
- 0102 7638 RBCCV 37 06 0829Document7 pages0102 7638 RBCCV 37 06 0829dr.baristimurNo ratings yet
- Journal Pre-Proof: ChestDocument33 pagesJournal Pre-Proof: ChestJunca VictorNo ratings yet
- Pulmonary Hypertension Mediastinal FibrosisDocument10 pagesPulmonary Hypertension Mediastinal FibrosisAndreiSefNo ratings yet
- Contegra Study 2012Document11 pagesContegra Study 2012AkilaNo ratings yet
- A Case Series of Intracardiac Thrombosis Revealing Behcets Disease in Moroccan PatientsDocument4 pagesA Case Series of Intracardiac Thrombosis Revealing Behcets Disease in Moroccan PatientsIJAR JOURNALNo ratings yet
- MAnaagement Koagulapati Dan Thrombolis Pada Pasien CovDocument13 pagesMAnaagement Koagulapati Dan Thrombolis Pada Pasien CovJuwita Rashi LumbantoruanNo ratings yet
- DIABtunismedv100i2-143-148 18Document6 pagesDIABtunismedv100i2-143-148 18marsim92No ratings yet
- 2022 Acute Coronary SyndromesDocument13 pages2022 Acute Coronary SyndromesOmar Alejandro Agudelo ZuluagaNo ratings yet
- Comparative Clinical Characteristics of Rheumatic Heart Disease Patients Undergoing Surgical Valve ReplacementDocument13 pagesComparative Clinical Characteristics of Rheumatic Heart Disease Patients Undergoing Surgical Valve ReplacementElvira AnitaNo ratings yet
- Venous Thromboembolism in The ICU: Main Characteristics, Diagnosis and ThromboprophylaxisDocument9 pagesVenous Thromboembolism in The ICU: Main Characteristics, Diagnosis and ThromboprophylaxisCourtneykdNo ratings yet
- Eci 12222Document9 pagesEci 12222Andikaputra Brahma WidiantoroNo ratings yet
- Tromboembolismo en Covid19Document7 pagesTromboembolismo en Covid19Nestor Alonso Lopez RubioNo ratings yet
- Tonino 2009Document12 pagesTonino 2009Paul CalbureanNo ratings yet
- Pericardiectomy For Tuberculous Effusive-Constrictive PericarditisDocument5 pagesPericardiectomy For Tuberculous Effusive-Constrictive PericarditisIJAR JOURNALNo ratings yet
- Mitral Valve Endocarditis in Hypertrophic Cardiomyopathy: Case Report and Literature ReviewDocument3 pagesMitral Valve Endocarditis in Hypertrophic Cardiomyopathy: Case Report and Literature ReviewChristabella Natalia WijayaNo ratings yet
- Jurnal Analitik YudhityaazraDocument13 pagesJurnal Analitik YudhityaazraYosa DhikaNo ratings yet
- Tto VasoespasmoDocument6 pagesTto VasoespasmoHernando CastrillónNo ratings yet
- Critical Care for Potential Liver Transplant CandidatesFrom EverandCritical Care for Potential Liver Transplant CandidatesDmitri BezinoverNo ratings yet
- Troponina Guided Coronary ComputedDocument11 pagesTroponina Guided Coronary ComputedafFNo ratings yet
- +american J Transplantation - 2018 - Peters Sengers - DCD Donor Hemodynamics As Predictor of Outcome After KidneyDocument12 pages+american J Transplantation - 2018 - Peters Sengers - DCD Donor Hemodynamics As Predictor of Outcome After KidneyChavalit ChotruangnapaNo ratings yet
- Fibrinolysis in COVID-19 Patients With Hemodynamic UnstableDocument2 pagesFibrinolysis in COVID-19 Patients With Hemodynamic UnstableTuan HaiNo ratings yet
- COVID-19 y Parametros de CoagulacionDocument4 pagesCOVID-19 y Parametros de CoagulacionSMIBA MedicinaNo ratings yet
- Management of Penetrating Wounds of The HeartDocument2 pagesManagement of Penetrating Wounds of The HeartInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Clinical Risk Factors of Asymptomatic Deep VenousDocument7 pagesClinical Risk Factors of Asymptomatic Deep VenoussenkonenNo ratings yet
- Ijmsv 14 P 1241Document10 pagesIjmsv 14 P 1241Milan PetrikNo ratings yet
- MainDocument14 pagesMainDoménica SánchezNo ratings yet
- Amin 2018Document22 pagesAmin 2018Han's OfficialNo ratings yet
- International Journal of Scientific Research: General MedicineDocument4 pagesInternational Journal of Scientific Research: General MedicineTriple ANo ratings yet
- MA-DENGUE-D.C.LYE-EDocument4 pagesMA-DENGUE-D.C.LYE-EJazmin ZantiNo ratings yet
- JURNAL LASER NAEVI (NXPowerLite Copy)Document20 pagesJURNAL LASER NAEVI (NXPowerLite Copy)Aji Prasetyo UtomoNo ratings yet
- Systemic Lupus Erythematosus (SLE): Causes, Symptoms and TreatmentDocument21 pagesSystemic Lupus Erythematosus (SLE): Causes, Symptoms and TreatmentAji Prasetyo UtomoNo ratings yet
- 05 2 Wound HealingDocument158 pages05 2 Wound HealingRidhofar AkbarNo ratings yet
- Animal Bite WoundDocument54 pagesAnimal Bite WoundAji Prasetyo UtomoNo ratings yet
- Wound IARW2013 YevaDocument36 pagesWound IARW2013 YevaAji Prasetyo UtomoNo ratings yet
- Patogenesis Dan Biologi NeoplasmaDocument61 pagesPatogenesis Dan Biologi NeoplasmaAji Prasetyo UtomoNo ratings yet
- 221-Article Manuscript-403-1-10-20171006Document6 pages221-Article Manuscript-403-1-10-20171006Aji Prasetyo UtomoNo ratings yet
- Profil Palatoskisis Di Bagian Ilmu Bedah Plastik Blu Rsup Prof. Dr. R.D. Kandou Manado Periode Januari-Desember 2011Document5 pagesProfil Palatoskisis Di Bagian Ilmu Bedah Plastik Blu Rsup Prof. Dr. R.D. Kandou Manado Periode Januari-Desember 2011Putri WulandariNo ratings yet
- Deep Sternal Wound Infection After Cardiac SurgeryDocument6 pagesDeep Sternal Wound Infection After Cardiac SurgeryAji Prasetyo UtomoNo ratings yet
- Early Vascular Surgery Response To The COVID-19 Pandemic: Results of A Nationwide SurveyDocument9 pagesEarly Vascular Surgery Response To The COVID-19 Pandemic: Results of A Nationwide SurveyAji Prasetyo UtomoNo ratings yet
- Improvement of A Clinical Score ForDocument13 pagesImprovement of A Clinical Score ForAji Prasetyo UtomoNo ratings yet
- 2019 Genetika - Molekuler NeoplasmaDocument38 pages2019 Genetika - Molekuler NeoplasmaAji Prasetyo UtomoNo ratings yet
- Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19Document9 pagesPulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19anablllNo ratings yet
- Prevalensi Labioschisis Di Rsup. Prof. Dr. R. D. Kandou Manado Periode Januari 2011 - Oktober 2012Document6 pagesPrevalensi Labioschisis Di Rsup. Prof. Dr. R. D. Kandou Manado Periode Januari 2011 - Oktober 2012Aji Prasetyo UtomoNo ratings yet
- Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19Document9 pagesPulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19anablllNo ratings yet
- Letters To The Editor: AppendixDocument3 pagesLetters To The Editor: AppendixAji Prasetyo UtomoNo ratings yet
- Preparing for Post-COVID Vascular SurgeryDocument2 pagesPreparing for Post-COVID Vascular SurgeryAji Prasetyo UtomoNo ratings yet
- 05 2 Wound HealingDocument158 pages05 2 Wound HealingRidhofar AkbarNo ratings yet
- COVID-19-Induced Neurovascular Injury: A Case Series With Emphasis On Pathophysiological MechanismsDocument17 pagesCOVID-19-Induced Neurovascular Injury: A Case Series With Emphasis On Pathophysiological MechanismsAji Prasetyo UtomoNo ratings yet
- PIIS0890509620307950Document8 pagesPIIS0890509620307950Aji Prasetyo UtomoNo ratings yet
- Molecular Basis of Cardiac and Vascular Injuries Associated With COVID-19Document15 pagesMolecular Basis of Cardiac and Vascular Injuries Associated With COVID-19Aji Prasetyo UtomoNo ratings yet
- Journal Reading BurnsDocument14 pagesJournal Reading BurnsAji Prasetyo UtomoNo ratings yet
- MainDocument3 pagesMainAji Prasetyo UtomoNo ratings yet
- 05 2 Wound HealingDocument158 pages05 2 Wound HealingRidhofar AkbarNo ratings yet
- Journal Reading BurnsDocument14 pagesJournal Reading BurnsAji Prasetyo UtomoNo ratings yet
- Deep Sternal Wound Infection After Cardiac SurgeryDocument6 pagesDeep Sternal Wound Infection After Cardiac SurgeryAji Prasetyo UtomoNo ratings yet
- Deep Sternal Wound Infection After Cardiac SurgeryDocument6 pagesDeep Sternal Wound Infection After Cardiac SurgeryAji Prasetyo UtomoNo ratings yet
- Infeksi Jaringan Lunak (NXPowerLite Copy)Document35 pagesInfeksi Jaringan Lunak (NXPowerLite Copy)Aji Prasetyo UtomoNo ratings yet
- Wound HealingDocument756 pagesWound HealingKerin Ardy100% (2)
- ISO 14000 - WikipediaDocument5 pagesISO 14000 - WikipediaalexokorieNo ratings yet
- SampleDocument8 pagesSampleAntônioNo ratings yet
- The Practical Welding EngineerDocument154 pagesThe Practical Welding EngineerMohamed Atef0% (1)
- Quest The Last RemnantDocument67 pagesQuest The Last Remnantding suheNo ratings yet
- MayankDocument38 pagesMayankmayank13430No ratings yet
- The Following Functional Health Pattern Assessment Is Based On A 65 Year Old Scottish Woman Who Lives Independently With Her Husband in Their Home at Happy ValleyDocument9 pagesThe Following Functional Health Pattern Assessment Is Based On A 65 Year Old Scottish Woman Who Lives Independently With Her Husband in Their Home at Happy ValleyJajangNo ratings yet
- Magellans of The Sky - Prologue - Summer 2010Document12 pagesMagellans of The Sky - Prologue - Summer 2010Prologue MagazineNo ratings yet
- Hyundai-25 30 33L 35LN-9A19.01Rev.6 Eng-D4 PDFDocument20 pagesHyundai-25 30 33L 35LN-9A19.01Rev.6 Eng-D4 PDFVicente Antonio GonzalezNo ratings yet
- Aircraft Control Systems, Basic Construction, Wing and Fuselage ConstructionDocument146 pagesAircraft Control Systems, Basic Construction, Wing and Fuselage ConstructionTAMILSELVAM NALLUSAMYNo ratings yet
- Orac Charts - BuenisimoDocument92 pagesOrac Charts - BuenisimosanthigiNo ratings yet
- Biologic License ApplicationDocument16 pagesBiologic License ApplicationJean Sandra PintoNo ratings yet
- Kant On Religion and ScienceDocument21 pagesKant On Religion and ScienceEduardo CharpenelNo ratings yet
- Chapter 1 and 2Document67 pagesChapter 1 and 2Tle SupawidNo ratings yet
- Alaina W - Food Project ReflectionDocument1 pageAlaina W - Food Project Reflectionapi-438601399No ratings yet
- Blackmer Pump Parts ListDocument2 pagesBlackmer Pump Parts ListFelipe Ignacio PaillavilNo ratings yet
- DST Sketch S.E Alhamd 2Document3 pagesDST Sketch S.E Alhamd 2GPCNo ratings yet
- Mini ProjectDocument6 pagesMini Projectirene0% (1)
- Essay Writing-PTEDocument13 pagesEssay Writing-PTEAnita GajjarNo ratings yet
- Capacitores Electroliticos SMDDocument8 pagesCapacitores Electroliticos SMDalvaro marrugoNo ratings yet
- Column FootingDocument57 pagesColumn Footingnuwan01100% (7)
- Fiber Crops - FlaxDocument33 pagesFiber Crops - Flaxmalath bashNo ratings yet
- Browning Belt Tension GaugeDocument2 pagesBrowning Belt Tension GaugeJasperken2xNo ratings yet
- Tcgbutopia G8Document216 pagesTcgbutopia G8faffsNo ratings yet
- Theoretical Development of The Brooks-Corey CapillDocument7 pagesTheoretical Development of The Brooks-Corey CapillDiana Vanessa PedrazaNo ratings yet
- Ahmed Ali Alshehri Mobile 00966-508-217284 Address: P.O.Box 70132 Zipcode:31952 Riyadh Street, Al-Khobar, Saudi ArabiaDocument9 pagesAhmed Ali Alshehri Mobile 00966-508-217284 Address: P.O.Box 70132 Zipcode:31952 Riyadh Street, Al-Khobar, Saudi ArabiaShah KhalidNo ratings yet
- GTA San Andreas CheatDocument9 pagesGTA San Andreas CheatHatta YanuarNo ratings yet
- Fesh S A0001171549 1Document7 pagesFesh S A0001171549 1ismuNo ratings yet
- English HL Grade 8 Language Exam Nov 2017 MEMODocument12 pagesEnglish HL Grade 8 Language Exam Nov 2017 MEMOThegn's PicklesNo ratings yet
- BMK PDFDocument8 pagesBMK PDFHuỳnh Minh SángNo ratings yet
- TheologicalDiscipleship English 2011-1Document144 pagesTheologicalDiscipleship English 2011-1bilnyangnatNo ratings yet