Professional Documents
Culture Documents
Jurnal 4
Uploaded by
Ahmad Fari Arief LopaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal 4
Uploaded by
Ahmad Fari Arief LopaCopyright:
Available Formats
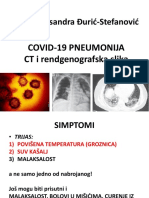
Cardiopulmonar y Imaging • Original Research
Zhou et al.
CT Features of COVID-19 Pneumonia
Cardiopulmonary Imaging
Original Research CT Features of Coronavirus
Disease 2019 (COVID-19)
Pneumonia in 62 Patients in
Downloaded from www.ajronline.org by 125.167.114.159 on 05/24/21 from IP address 125.167.114.159. Copyright ARRS. For personal use only; all rights reserved
Wuhan, China
Shuchang Zhou1 OBJECTIVE. The purpose of this study was to investigate 62 subjects in Wuhan, China,
Yujin Wang with laboratory-confirmed coronavirus disease (COVID-19) pneumonia and describe the CT
Tingting Zhu features of this epidemic disease.
Liming Xia MATERIALS AND METHODS. A retrospective study of 62 consecutive patients with
laboratory-confirmed COVID-19 pneumonia was performed. CT images and clinical data
Zhou S, Wang Y, Zhu T, Xia L were reviewed. Two thoracic radiologists evaluated the distribution and CT signs of the le-
sions and also scored the extent of involvement of the CT signs. The Mann-Whitney U test
was used to compare lesion distribution and CT scores. The chi-square test was used to com-
pare the CT signs of early-phase versus advanced-phase COVID-19 pneumonia.
RESULTS. A total of 62 patients (39 men and 23 women; mean [± SD] age, 52.8 ± 12.2
years; range, 30–77 years) with COVID-19 pneumonia were evaluated. Twenty-four of 30 pa-
tients who underwent routine blood tests (80.0%) had a decreased lymphocyte count. Of 27 pa-
tients who had their erythrocyte sedimentation rate and high-sensitivity C-reactive protein level
assessed, 18 (66.7%) had an increased erythrocyte sedimentation rate, and all 27 (100.0%) had
an elevated high-sensitivity C-reactive protein level. Multiple lesions were seen on the initial CT
scan of 52 of 62 patients (83.9%). Forty-eight of 62 patients (77.4%) had predominantly periph-
eral distribution of lesions. The mean CT score for the upper zone (3.0 ± 3.4) was significantly
lower than that for the middle (4.5 ± 3.8) and lower (4.5 ± 3.7) zones (p = 0.022 and p = 0.020,
respectively), and there was no significant difference in the mean CT score of the middle and
lower zones (p = 1.00). The mean CT score for the anterior area (4.4 ± 4.1) was significantly
lower than that for the posterior area (7.7 ± 6.3) (p = 0.003). CT findings for the patients were
as follows: 25 patients (40.3%) had ground-glass opacities (GGO), 21 (33.9%), consolidation; 39
(62.9%), GGO plus a reticular pattern; 34 (54.8%), vacuolar sign; 28 (45.2%), microvascular di-
lation sign; 35 (56.5%), fibrotic streaks; 21 (33.9%), a subpleural line; and 33 (53.2%), a subpleu-
ral transparent line. With regard to bronchial changes seen on CT, 45 patients (72.6%) had air
bronchogram, and 11 (17.7%) had bronchus distortion. In terms of pleural changes, CT showed
that 30 patients (48.4%) had pleural thickening, 35 (56.5%) had pleural retraction sign, and six
(9.7%) had pleural effusion. Compared with early-phase disease (≤ 7 days after the onset of
symptoms), advanced-phase disease (8–14 days after the onset of symptoms) was characterized
by significantly increased frequencies of GGO plus a reticular pattern, vacuolar sign, fibrotic
streaks, a subpleural line, a subpleural transparent line, air bronchogram, bronchus distortion,
and pleural effusion; however, GGO significantly decreased in advanced-phase disease.
CONCLUSION. CT examination of patients with COVID-19 pneumonia showed a
Keywords: coronavirus disease 2019, COVID-19, CT, mixed and diverse pattern with both lung parenchyma and the interstitium involved. Identi-
pneumonia fication of GGO and a single lesion on the initial CT scan suggested early-phase disease. CT
doi.org/10.2214/AJR.20.22975
signs of aggravation and repair coexisted in advanced-phase disease. Lesions presented with a
characteristic multifocal distribution in the middle and lower lung regions and in the posterior
Received February 16, 2020; accepted without revision lung area. A decreased lymphocyte count and an increased high-sensitivity C-reactive protein
February 19, 2020. level were the most common laboratory findings.
1
All authors: Department of Radiology, Tongji Hospital,
Tongji Medical College, Huazhong University of Science
ince late December of 2019, an ing to the initial investigation, most cases
S
and Technology, 1095 Jiefang Rd, Qiaokou District,
Wuhan, Hubei 430030, China. Address correspondence explosion in the number of cases were thought to originate from the Huanan
to Y. Wang (wangyujin8303@163.com). of a new acute viral respiratory Seafood Wholesale Market in Wuhan [1]. At
disease (coronavirus disease the time of the writing of this article, the vi-
AJR 2020; 214:1287–1294 [COVID-19]) caused by a novel coronavirus rus is rapidly spreading to many other cities
(severe acute respiratory syndrome coronavi- in China and even to other countries around
ISSN-L 0361–803X/20/2146–1287
rus 2 [SARS-CoV-2]) has been reported in the world. Although SARS-CoV-2 is a mem-
© American Roentgen Ray Society the city of Wuhan in central China. Accord- ber of the coronavirus family of viruses, it is
AJR:214, June 2020 1287
Zhou et al.
more distant from SARS coronavirus spectively reviewed the CT images on a PACS nally, bilateral lungs were divided into 12 zones
(SARS-CoV) and Middle East respiratory workstation (Synapses, Fujifilm) with multipla- altogether. The degree of involvement in each lung
syndrome coronavirus, is considered to be a nar reconstruction tools and reached a decision zone was scored as follows [6–8]: a score of 0 de-
new type of betacoronavirus that infects hu- in consensus. The images were viewed in lung noted no involvement; 1, < 25% involvement; 2,
mans [2], and on the basis of the current epi- window settings (width, 1000–1500 HU; level, 25% to less than 50% involvement; 3, 50% to less
demic, is more infectious than SARS-CoV. 700 to −550 HU) and mediastinal window set- than 75% involvement; and 4, ≥ 75% involvement.
Downloaded from www.ajronline.org by 125.167.114.159 on 05/24/21 from IP address 125.167.114.159. Copyright ARRS. For personal use only; all rights reserved
As of 8:00 p.m. on February 17, 2020, a total tings (width, 300–350 HU; level, 30–40 HU). Scores were recorded and summed for each lung
of 68,595 confirmed cases of COVID-19 and The predominant patterns seen on CT imag- zone, with a maximum possible score of 48.
1667 deaths were reported. In the present es were classified into three major categories:
study, we identified 62 patients in Wuhan, lung, bronchial, and pleural changes. Each major Statistical Analysis
China, who had laboratory-confirmed category was divided into subcategories. Lung Data were recorded using spreadsheet soft-
COVID-19 pneumonia and described the CT changes were classified into the following eight ware (Excel 2010, Microsoft) and were analyzed
features of this pneumonia. subcategories: ground-glass opacities (GGO; in- using statistical software (SPSS, version 22.0,
creased attenuation without obscuration of the IBM). Continuous variables were expressed as
Materials and Methods underlying lung vessels) [3], consolidation (ho- mean (± SD) values. The Kolmogorov-Smirnov
The ethics committee at Huazhong University mogeneous increased intensity of lung parenchy- test was used for the normal distribution test,
of Science and Technology waived the need for in- ma with obscuration of the underlying vessels), and continuous variables were compared using
formed consent for this retrospective study. GGO plus a reticular pattern (a reticular shad- the Mann-Whitney U test. The frequency of CT
We retrospectively reviewed 118 patients seen ow on the background of GGO and thickening of signs was expressed as the number (percentage)
with suspected COVID-19 pneumonia from Janu- the interlobular septum and interlobular septum, of occurrences and was compared for cases of
ary 16 to January 30, 2020. All patients had ab- showing paving stone sign) [4], vacuolar sign (a early- versus advanced-phase disease using the
normal CT findings that suggested pneumonia as vacuole-like transparent shadow of < 5 mm in chi-square test or the Fisher exact test. Differenc-
the diagnosis. A patient with suspected COVID-19 length observed in the lesion), microvascular di- es for which p < 0.05 were considered statistical-
pneumonia was defined as a patient with pneumo- lation sign (dilated small vessels in the lesion), fi- ly significant.
nia who met at least three of the following five cri- brotic streaks (an irregular strip shadow), a sub-
teria: fever, a low or normal WBC count or low pleural line (an arc-shaped linear shadow 2–5 cm Results
lymphocyte count, exclusion of other respiratory in length appearing parallel to the chest wall), or Clinical Characteristics
virus species on the basis of laboratory findings, a subpleural transparent line (a thin and transpar- A total of 62 patients (mean age, 52.8 ±
no relief in symptoms noted after receipt of empir- ent line lying between the lesions and the viscer- 12.2 years; range, 30–77 years) with COV-
ical antimicrobial or antiinfluenza treatment for 3 al layer of pleura). Bronchial changes were classi- ID-19 pneumonia were included in the study.
days, and in particular, an epidemiologic link to fied into two subcategories: air bronchogram (an Thirty-nine of the 62 patients (62.9%) were
the Huanan Seafood Wholesale Market or a his- air-filled image of bronchus in lung lesions) and men (mean age, 54.1 ± 11.8 years; range,
tory of contact with other patients with COVID-19 bronchus distortion. Pleural changes were clas- 30–77 years), and 23 (37.1%) were women
pneumonia. A total of 62 patients were confirmed sified into three subcategories: thickening of the (mean age, 50.7 ± 12.8 years; range, 30–73
to have COVID-19 nucleic acid on the basis of pleura, pleural retraction sign (lesions present years). All patients had symptoms at onset of
positive findings for respiratory samples tested close to the visceral pleura and pull pleura), or the disease, with fever noted in 54 patients
using real-time reverse-transcription–polymerase pleural effusion. Distribution of the lung lesions (87.1%), coughing and sputum in 28 patients
chain reaction. Two of the researchers recorded was classified as predominantly peripheral (in- (45.2%), fatigue in 14 patients (22.6%), short-
clinical data, including symptoms, date of onset volving mainly the peripheral region comprising ness of breath in 15 patients (24.2%), mus-
of symptoms, laboratory examination results, and one-third of the lung), central (involving mainly cle pain in 20 patients (32.3%), and gastro-
information regarding other accompanying condi- the central region comprising two-thirds of the intestinal symptoms, including abdominal
tions or diseases. lung), or peripheral plus central (involving both pain and diarrhea, in nine patients (14.5%).
the peripheral and central regions) [5]. Because Routine blood tests were performed for 30
CT Scanning Protocol no cases of lymphadenopathy and pneumothorax patients. Six patients (20.0%) had leukope-
MDCT was performed using either of the follow- were found, those two signs will not be described nia, 24 (80.0%) had a decreased lympho-
ing CT scanners: the 16-MDCT LightSpeed scan- in the present study. cyte count, and 15 (50.0%) had a decreased
ner (GE Healthcare) or the uCT 760 scanner (Unit- The extent of involvement on thin-section CT percentage of lymphocytes. The erythrocyte
ed Imaging). The parameters used for the scanning images was also assessed by the two radiologists. sedimentation rate and high-sensitivity C-re-
protocol were as follows: patient in the supine po- Each side of the lung was divided (from top to bot- active protein (hs-CRP) level were evaluated
sition; end inspiratory acquisition; tube voltage, tom) into three zones: the upper zone (above the in 27 patients. Of these patients, 18 (66.7%)
100–120 kV; tube current–exposure time product, carina), the middle zone (from the carina to the had an increased erythrocyte sedimenta-
200–300 mAs; pitch, 1.375 and 0.9125; and sec- inferior pulmonary vein), and the lower zone (be- tion rate, and all 27 (100.0%) had an elevat-
tion thickness after reconstruction, 1.25 mm. Un- low the inferior pulmonary vein). Each zone was ed hs-CRP level. Four patients had a history
enhanced CT scans were obtained for all patients. then divided into two areas: the anterior area (the of hypertension, four had diabetes, one had
area before the vertical line of the midpoint of the cerebral infarction, one had chronic kidney
Image Viewing and Evaluation diaphragm in the sagittal position) and the poste- disease, and two were pregnant. Table 1 sum-
Two experienced radiologists with 13 and 9 rior area (the area after the vertical line of the mid- marizes the demographic and clinical char-
years of experience in thoracic radiology retro- point of the diaphragm in the sagittal position). Fi- acteristics of the patients.
1288 AJR:214, June 2020
CT Features of COVID-19 Pneumonia
TABLE 1: Demographic and Clinical TABLE 2: Distribution and CT Score for Parenchymal Abnormalities in 62
Characteristics of Patients Patients With Coronavirus Disease 2019 Pneumonia
With Coronavirus Disease
2019 Pneumonia Category and Subcategory No. (%) of Patients CT Score, Mean ± SD p
Lesion distribution 0.008a
Characteristic Value
Peripheral 48 (77.4)
Downloaded from www.ajronline.org by 125.167.114.159 on 05/24/21 from IP address 125.167.114.159. Copyright ARRS. For personal use only; all rights reserved
Sex, no. of patients/total patients
Peripheral and central 14 (22.6)
Male 39/62
Lung
Female 23/62
Left 5.9 ± 5.1 0.750
Symptom, no. of patients/total patients
Right 6.2 ± 5.3
Fever 54/62
Lung zone
Coughing and sputum 28/62
Upper 3.0 ± 3.4 0.024a
Fatigue 14/62
Middle 4.5 ± 3.8
Shortness of breath 15/62
Lower 4.5 ± 3.7
Muscle pain 20/62
Lung area
Abdominal pain or diarrhea 9/62
Anterior 4.4 ± 4.1 0.003a
Laboratory test finding, no. of patients/
total patients Posterior 7.7 ± 6.3
aStatistically significant difference.
Leukopenia 6/30
Decreased lymphocyte count 24/30
one (10.0%) had a lesion in the lingual seg- ilar to those of a previous study [8]. Other
Decreased percentage of lymphocytes 15/30 ment of the upper lobe of the left lung. lung changes that were observed on CT were
Increased ESR 18/27 In terms of lesion distribution, distribution as follows: 39 patients (62.9%) had GGO
Increased hs-CRP level 27/27 was predominantly peripheral in 48 of 62 pa- plus a reticular pattern; 34 (54.8%), vacuo-
tients (77.4%), peripheral plus central in 14 lar sign; 28 (45.2%), microvascular dilation
Accompanying condition or disease,
no. of patients
patients (22.6%) cases, and central in none sign; 35 (56.5%), fibrotic streaks; 21 (33.9%),
of the patients. When the CT score was used a subpleural line; and 33 (53.2%), a subpleu-
Hypertension 4 to determine the extent of involvement, we ral transparent line. In terms of bronchial
Diabetes 4 compared involvement of the left and right changes, 45 patients (72.6%) had air bron-
Cerebral infarction 1 lungs; the upper, middle, and lower zones; chogram on CT, and 11 (17.7%) had bronchus
and the anterior and posterior areas. No distortion. With regard to pleural changes
Chronic kidney disease 1
significant difference was observed between seen on CT, 30 patients (48.4%) had thicken-
Pregnancy 2 the mean CT scores for the left lung (5.9 ± ing of pleura, 35 (56.5%) had pleural retrac-
Note—ESR = erythrocyte sedimentation rate, 5.1) and right lung (6.2 ± 5.3) (p = 0.75). The tion sign, and six (9.7%) had pleural effusion
hs-CRP = high-sensitivity C-reactive protein. mean CT score for the upper zone (3.0 ± 3.4) (Table 2 and Figs. 2–4).
was significantly lower than that for the mid- When the course of disease was divided
CT Findings of Coronavirus Disease dle (4.5 ± 3.8) and lower (4.5 ± 3.7) zones into an early phase (≤ 7 days after the on-
2019 Pneumonia (p = 0.022 and p = 0.020, respectively), and set of symptoms) (n = 40) and an advanced
In 10 of 62 patients (16.1%), COVID-19 no significant difference was observed be- phase (8–14 days after the onset of symp-
pneumonia was seen as a single lesion on the tween those of the middle and lower zones toms) (n = 22), we found that the frequency of
first CT scan obtained, with CT performed (p = 1.00). The mean CT score for the an- GGO was significantly higher in early-phase
1–7 days (mean, 2.2 ± 1.8 days) after the on- terior area (4.4 ± 4.1) was significantly low- disease than in advanced-phase disease. The
set of symptoms. In the remaining 52 patients er than that for the posterior area (7.7 ± 6.3) frequencies of GGO plus a reticular pattern,
(83.9%), COVID-19 pneumonia was seen (p = 0.003) (Fig. 1 and Table 2). vacuolar sign, fibrotic streaks, a subpleural
as multiple lesions on the first CT scan ob- The CT features of COVID-19 pneumonia line, a subpleural transparent line, air bron-
tained, with CT performed 1–14 days (mean, included lung changes (GGO, consolidation, chogram, bronchus distortion, and pleu-
6.6 ± 4.0 days) after the onset of symptoms, GGO plus a reticular pattern, vacuolar sign, ral effusion were also significantly lower in
a significantly longer interval than that noted microvascular dilation sign, fibrotic streaks, patients with early-phase disease compared
for patients with a single lesion (p < 0.05). a subpleural line, and a subpleural transpar- with those with advanced-phase disease (Ta-
Of the 10 patients with a single lesion, sev- ent line), bronchial changes (air broncho- bles 3 and 4).
en (70.0%) had lesions that were initially lo- gram and bronchus distortion) and pleural
cated in the inferior lobe of the right lung; changes (pleural thickening, pleural retrac- Discussion
of the three remaining patients in this group, tion sign, and pleural effusion). In terms of COVID-19 pneumonia is a new, highly
one (10.0%) had a lesion located in the mid- lung changes, CT showed that 25 patients contagious viral pneumonia caused by a nov-
dle lobe of the right lung, one (10.0%) had a (40.3%) had GGO and 21 (33.9%) had con- el coronavirus (SARS-CoV-2) of unclear ori-
lesion in the upper lobe of the right lung, and solidation; these findings are somewhat sim- gin. In this study, we investigated 62 patients
AJR:214, June 2020 1289
Zhou et al.
TABLE 3: CT Features of C
oronavirus TABLE 4: CT Features of Coronavirus Disease 2019 Pneumonia in Patients
Disease 2019 Pneumonia With Early- and Advanced-Phase Disease
No. (%) of Early-Phase Advanced-Phase Chi-Square Test
Patients CT Feature Disease (n = 40) Disease (n = 22) Statistic p
CT Feature (n = 62)
Lung change
Downloaded from www.ajronline.org by 125.167.114.159 on 05/24/21 from IP address 125.167.114.159. Copyright ARRS. For personal use only; all rights reserved
Lesion presentation on initial scan
GGO 19 (47.5) 6 (27.3) 2.413 0.012a
Single lesion 10 (16.1)
Consolidation 15 (37.5) 6 (27.3) 0.663 0.416
Multiple lesions 52 (83.9)
GGO and reticular pattern 20 (50.0) 19 (86.4) 8.043 0.005a
Lesion distribution
Vacuolar sign 16 (40.0) 18 (81.8) 10.022 0.002a
Peripheral 48 (77.4)
Microvascular dilation sign 19 (47.5) 9 (40.9) 0.249 0.618
Peripheral and central 14 (22.6)
Fibrotic streaks 17 (42.5) 18 (81.8) 8.925 0.003a
CT sign
Subpleural line 10 (25.0) 11 (50.0) 3.961 0.047a
Lung change
Subpleural transparent line 17 (42.5) 16 (72.7) 5.209 0.022a
GGO 25 (40.3)
Bronchial change
Consolidation 21 (33.9)
Air bronchogram 25 (62.5) 20 (90.9) 5.756 0.016a
GGO and reticular pattern 39 (62.9)
Bronchus distortion 4 (10.0) 7 (31.8) 4.630 0.031a
Vacuolar sign 34 (54.8)
Pleural change
Microvascular dilation sign 28 (45.2)
Thickening of pleura 17 (42.5) 13 (59.1) 1.564 0.211
Fibrotic streaks 35 (56.5)
Pleural retraction sign 23 (57.5) 12 (54.5) 0.050 0.822
Subpleural line 21 (33.9)
Pleural effusion 1 (2.5) 5 (22.7) 6.644 0.010a
Subpleural transparent line 33 (53.2)
Note—Except where otherwise indicated, data are number (%) of patients. All comparisons were performed
Bronchial change using the chi-square test. GGO = ground-glass opacities.
aStatistically significant difference.
Air bronchogram 45 (72.6)
Bronchiectasis 20 (32.2) patients had a decreased percentage of lym- to invade the branches of the right inferior lo-
Bronchus distortion 11 (17.7) phocytes. Of 27 patients who underwent eval- bar bronchus and cause infection. Consider-
uation of the erythrocyte sedimentation rate ing the range of involvement, we found that
Pleural change
and hs-CRP level, 66.7% had an increased lesions showed a predominantly peripheral
Thickening of pleura 30 (48.4) erythrocyte sedimentation rate, and 100.0% distribution (75.8%). The middle and lower
Pleural retraction sign 35 (56.5) had an elevated hs-CRP level. Therefore, a de- zones and the posterior area of both lungs
Pleural effusion 6 (9.7) creased lymphocyte count and an elevated hs- were significantly more involved.
CRP level were the most sensitive parameters. We found diversified CT patterns of
Note—GGO = ground-glass opacities.
In reviewing and analyzing the CT fea- COVID-19 pneumonia, including lung chang-
tures of 62 cases of COVID-19 pneumonia, es (GGO [40.3%], consolidation [33.9%],
with confirmed COVID-19 pneumonia. Most we found that cases were most often seen GGO plus a reticular pattern [62.9%], vacu-
(62.9%) of the infected patients were men. In to manifest as multiple lesions on the ini- olar sign [54.8%], microvascular dilation sign
terms of symptoms, fever occurred in 87.1% tial CT scan (83.9%); however, 16.1% of cas- [45.2%], fibrotic streaks [56.5%], subpleu-
of patients; coughing and sputum, in 45.2%; es manifested as single lesion, and of these ral line [33.9%], subpleural transparent line
muscle pain, 32.3%; shortness of breath, cases, 70.0% occurred in the inferior lobe [53.2%]), bronchial changes (air bronchogram
24.2%; fatigue, 22.6%; and gastrointestinal of the right lung. When patients with sin- [72.6%] and bronchus distortion [17.7%]), and
symptoms such as abdominal pain and diar- gle and multiple lesions were compared, pleural changes (thickening of pleura [48.4%],
rhea, 14.5%. In addition to respiratory and multiple lesions were identified on imaging pleural retraction sign [56.5%], and pleu-
systemic symptoms of viral infection, some performed at a mean of 6.6 ± 4.0 days af- ral effusion [9.7%]). On CT, the COVID-19
patients with COVID-19 pneumonia present- ter onset of symptoms, whereas single le- pneumonia was seen to have a rather mixed
ed with a gastrointestinal symptom as the ini- sions were identified on imaging performed pattern involving both lung parenchyma and
tial symptom; this finding suggests that gas- at a significantly earlier phase of the disease lung interstitium [12]. The virus first invaded
trointestinal symptoms may be associated (2.2 ± 1.8 days). This may be because of the the pulmonary interstitium, which was char-
with the pathogenesis of C OVID-19 pneu- innate anatomic features of the right inferi- acterized by edema and thickening of the in-
monia as a result of the virus binding to hu- or lobar bronchus. The bronchus of the right terlobular septum, interlobular interstitium,
man receptor angiotensin-converting enzyme lower lobe of the lung is straighter and steep- subpleural interstitium, interlobular central
2 [9], which also shows high expression in the er than other bronchial branches, and the an- interstitium, and peribronchovascular inter-
gastrointestinal tract [10]. In terms of labo- gle between the right lower lobe and the long stitium, manifesting as GGO. Consolidation
ratory findings, 80.0% of patients had a de- axis of the trachea is smaller, so in the early might represent further infiltration of the pa-
creased lymphocyte count [11], and 50.0% of phase of the disease, the virus is more likely renchyma. The vacuole sign could be caused
1290 AJR:214, June 2020
CT Features of COVID-19 Pneumonia
by an incompletely filled alveolar cluster in was accompanied by repair changes. There tion and epidemiology of 2019 novel coronavirus:
the exudative lung parenchyma. The micro- was no significant difference between early- implications for virus origins and receptor bind-
vascular dilation sign probably indicated in- phase disease versus advanced-phase disease ing. Lancet 2020; 395:565–574
creased blood supply to the inflammatory in terms of consolidation, the microvascular 3. Joynt GM, Antonio GE, Lam P, et al. Late-stage
area. Air bronchogram was formed by bron- dilation sign, thickening of pleura, and the adult respiratory distress syndrome caused by se-
chus containing air in consolidation. GGO pleural retraction sign. vere acute respiratory syndrome: abnormal findings
Downloaded from www.ajronline.org by 125.167.114.159 on 05/24/21 from IP address 125.167.114.159. Copyright ARRS. For personal use only; all rights reserved
plus a reticular pattern represented thicken- The present study has two limitations. First, at thin-section CT. Radiology 2004; 230:339–346
ing of the interlobular septum resulting from because the course of COVID-19 pneumonia 4. Wong KT, Antonio GE, Hui DS, et al. Thin-sec-
the GGO, which ultimately evolved into the is short, changes seen on CT over its entire tion CT of severe acute respiratory syndrome:
subpleural line. Fibrotic streaks indicated lo- course have not been completely tracked and evaluation of 73 patients exposed to or with the
cal inflammatory absorption and residual fi- described for all patients. Second, there is not disease. Radiology 2003; 228:395–400
brosis, and bronchus distortion suggested that enough pathologic data on these patients for a 5. Ajlan AM, Ahyad RA, Jamjoom LG, Alharthy A,
the local inflammation absorbed and retract- comparative study to be performed. Madani TA. Middle East respiratory syndrome
ed the bronchus inside or surrounded it. The In conclusion, CT findings for patients coronavirus (MERS-CoV) infection: chest CT
pleura were often involved and were charac- with COVID-19 pneumonia showed that the findings. AJR 2014; 203:782–787
terized by thickening and retraction resulting disease has a mixed and diverse pattern, with 6. Ooi GC, Khong PL, Müller NL, et al. Severe acute
from the inflammatory reaction. both lung parenchyma and interstitium in- respiratory syndrome: temporal lung changes at
In early-phase COVID-19 pneumonia (≤ 7 volved. The presence of GGO and a single thin-section CT in 30 patients. Radiology 2004;
days after the onset of symptoms), bron- lesion at the onset of COVID-19 pneumonia 230:836–844
chus distortion (10.0%) and pleural effu- suggested that the disease was in its early 7. Chang YC, Yu CJ, Chang SC, et al. Pulmonary
sion (2.5%) were relatively rare compared phase. CT signs of aggravation and repair co- sequelae in convalescent patients after severe
with other signs (frequency, 27.5–62.5%). existed in examinations of patients with ad- acute respiratory syndrome: evaluation with thin-
In advanced-phase disease (8–14 days after vanced-phase disease. Pleural effusion might section CT. Radiology 2005; 236:1067–1075
the onset of symptoms), GGO plus a retic- occur in the advanced phase. Multifocality 8. Chung M, Bernheim A, Mei X, et al. CT imaging
ular pattern (86.4%), vacuolar sign (81.8%), as well as primary distribution of lesions in features of 2019 novel coronavirus (2019-nCoV).
air bronchogram (81.8%), fibrotic streaks the middle and lower zones and the posteri- Radiology 2020 Feb 24 [Epub ahead of print]
(90.9%), and the subpleural transparent or area of the lungs were rather characteris- 9. Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor
line (72.7%) were relatively more common tic manifestations. A decreased lymphocyte recognition by novel coronavirus from Wuhan: an
than other signs (frequency, 22.7–59.1%). count and an elevated hs-CRP level were the analysis based on decade-long structural studies of
Compared with early-phase disease, ad- most common laboratory findings. SARS. J Virol 2020 Jan 29 [Epub ahead of print]]
vanced-phase disease was associated with 10. Harmer D, Gilbert M, Borman R, Clark KL.
a significantly increased frequency of GGO Acknowledgment Quantitative mRNA expression profiling of ACE
plus a reticular pattern, vacuolar sign, fibrot- We thank Zujun Hou for assistance in re- 2, a novel homologue of angiotensin converting
ic streaks, air bronchogram, bronchus distor- vising this manuscript. enzyme. FEBS Lett 2002; 532:107–110
tion, a subpleural line, a subpleural transpar- 11. Chen N, Zhou M, Dong X, et al. Epidemiological
ent line, and pleural effusion, but GGO was References and clinical characteristics of 99 cases of 2019
significantly decreased. These changes sug- 1. Huang C, Wang Y, Li X, et al. Clinical features of novel coronavirus pneumonia in Wuhan, China: a
gested that GGO was a relatively early sign patients infected with 2019 novel coronavirus in descriptive study. Lancet 2020; 395:507–513
in the course of the disease and that in the ad- Wuhan, China. Lancet 2020; 395:497–506 [Erra- 12. Koo HJ, Lim S, Choe J, Choi SH, Sung H, Do KH.
vanced phase, the involvement of lung paren- tum in Lancet 2020; 395:496]. Radiographic and CT features of viral pneumo-
chyma and interstitium was aggravated but 2. Lu R, Zhao X, Li J, et al. Genomic characterisa- nia. RadioGraphics 2018; 38:719–739
(Figures start on next page)
AJR:214, June 2020 1291
Zhou et al.
Downloaded from www.ajronline.org by 125.167.114.159 on 05/24/21 from IP address 125.167.114.159. Copyright ARRS. For personal use only; all rights reserved
A B
C D E
Fig. 1—Distribution of lesions in five patients with coronavirus disease 2019 pneumonia.
A, 30-year-old man. CT image obtained on day 2 after onset of symptoms shows single lesion that developed in inferior lobe of right lung.
B, 49-year-old man. CT image obtained on day 7 after onset of symptoms shows multiple lesions involving multiple lobes of bilateral lungs.
C, 38-year-old man. CT image obtained on day 5 after onset of symptoms shows peripheral distribution of patchy ground-glass opacities plus reticular pattern with
vacuole inside.
D, 46-year-old woman. CT image obtained on day 9 after onset of symptoms shows peripheral plus central distribution of ground-glass opacities, partial consolidation,
and fibrosis streak.
E, 38-year-old woman. CT image obtained on day 7 after onset of symptoms shows posterior area with more serious involvement than anterior area.
A B C
Fig. 2—CT features indicating changes in lungs caused by coronavirus disease 2019 pneumonia in eight patients.
A, 52-year-old woman. CT image obtained on day 4 after onset of symptoms shows multiple ground-glass opacities (box) in inferior lobe of left lung.
B, 55-year-old man. CT image obtained on day 8 after onset of symptoms shows area of consolidation (box) with ground-glass opacities surrounded (arrow) in lingual
segment of upper lobe of left lung. Air bronchogram can be seen inside consolidation.
C, 32-year-old woman. CT image obtained on day 5 after onset of symptoms shows ground-glass opacities plus reticular pattern (box) in peripheral area of inferior lobe of
right lung.
(Fig. 2 continues on next page)
1292 AJR:214, June 2020
CT Features of COVID-19 Pneumonia
Downloaded from www.ajronline.org by 125.167.114.159 on 05/24/21 from IP address 125.167.114.159. Copyright ARRS. For personal use only; all rights reserved
D E F
Fig. 2 (continued)—CT features indicating changes in
lungs caused by coronavirus disease 2019 pneumonia
in eight patients.
D, 57-year-old woman. CT image obtained on day 7
after onset of symptoms shows vacuolar sign (arrow).
E, 55-year-old man. CT image obtained on day 7 after
onset of symptoms shows microvascular dilation sign
(arrow) in ground-glass opacities.
F, 57-year-old woman. CT image obtained on day 10
after onset of symptoms shows fibrotic streaks (box)
in inferior lobe of left lung.
G, 39-year-old man. CT image obtained on day 14
after onset of symptoms shows subpleural line
(arrow) in right lung.
H, 45-year-old man. CT image obtained on day 12 after
onset of symptoms shows subpleural transparent line
(arrows) below left pleura.
G H
AJR:214, June 2020 1293
Zhou et al.
Downloaded from www.ajronline.org by 125.167.114.159 on 05/24/21 from IP address 125.167.114.159. Copyright ARRS. For personal use only; all rights reserved
A B C
Fig. 3—CT features indicating bronchial changes caused by coronavirus disease 2019 pneumonia.
A, 41-year-old man. CT image obtained on day 7 after onset of symptoms shows air bronchogram (arrow) in patchy ground-glass opacities with partial consolidation in
inferior lobe of right lung.
B, 55-year-old man. CT image obtained on day 16 after onset of symptoms shows air bronchogram (arrow) in consolidation in lingual segment of upper lobe of left lung.
C, 57-year-old woman. CT image obtained on day 16 after onset of symptoms shows bronchus distortion (arrow) in ground-glass opacities.
Fig. 4—CT features indicating pleural changes
caused by coronavirus disease 2019 pneumonia. Top
images were obtained with lung window settings;
bottom images were obtained with mediastinal
window settings.
A, 36-year-old man. CT images obtained on day 10
after onset of symptoms show mixed ground-glass
opacities in inferior lobe of left lung and adjacent
pleural thickening (arrow).
B, 33-year-old woman. CT images obtained on
day 4 after onset of symptoms show patchy area
of consolidation with ground-glass opacities
surrounded in inferior lobe of right lung and adjacent
pleural retraction (arrows) and thickening.
A B
1294 AJR:214, June 2020
You might also like
- NACH Greater NGH Chapter Newsletter Highlights Hypno-KinesiologyDocument10 pagesNACH Greater NGH Chapter Newsletter Highlights Hypno-Kinesiologymoumona100% (1)
- Cure For The CureDocument330 pagesCure For The Curescribd_tm100% (1)
- Student Nurse QuizzesDocument10 pagesStudent Nurse QuizzesElesis samaNo ratings yet
- Case Study On Chronic Kidney DiseaseDocument9 pagesCase Study On Chronic Kidney DiseaseHalles Beverlyn Crisostomo GeraldeNo ratings yet
- General Practitioner - Neurology MCQsDocument20 pagesGeneral Practitioner - Neurology MCQsAsif Newaz100% (3)
- Anthropology of The Body SyllabusDocument7 pagesAnthropology of The Body SyllabusAndrei MihailNo ratings yet
- Jurnal 2-DikonversiDocument11 pagesJurnal 2-DikonversiRidhya SilmiNo ratings yet
- CT Features of COVID 19 in 30 Pediatric PatiensDocument9 pagesCT Features of COVID 19 in 30 Pediatric PatiensNur aini noviyantiNo ratings yet
- Ajr 20 22954Document7 pagesAjr 20 22954Tsega HagosNo ratings yet
- 10 2214@ajr 20 22975Document8 pages10 2214@ajr 20 22975yandraNo ratings yet
- Pregnancy and Perinatal Outcomes of Women With Coronavirus Disease (COVID-19) Pneumonia: A Preliminary AnalysisDocument6 pagesPregnancy and Perinatal Outcomes of Women With Coronavirus Disease (COVID-19) Pneumonia: A Preliminary AnalysisIvana SilvanyNo ratings yet
- Imagen TacDocument5 pagesImagen TacEliana TorresNo ratings yet
- Imaging Profile of The COVID-19 Infection: Radiologic Findings and Literature ReviewDocument9 pagesImaging Profile of The COVID-19 Infection: Radiologic Findings and Literature ReviewHielmy Auliya HasyimNo ratings yet
- CT Scan Vs PCR2Document6 pagesCT Scan Vs PCR2risanataliasiburianNo ratings yet
- LC PDFDocument10 pagesLC PDFJorge Andres Balza GranadosNo ratings yet
- CT Manifestations of Coronavirus Disease 2019 A RDocument5 pagesCT Manifestations of Coronavirus Disease 2019 A ReugeniaNo ratings yet
- UyutdgfDocument5 pagesUyutdgfswabrijNo ratings yet
- Engineering: Research Coronavirus Disease 2019-ArticleDocument8 pagesEngineering: Research Coronavirus Disease 2019-ArticleJackyNo ratings yet
- Radiological Evaluation and Correlation of CT Chest With Progress of Disease in Covid 19 PatientsDocument14 pagesRadiological Evaluation and Correlation of CT Chest With Progress of Disease in Covid 19 PatientsIJAR JOURNALNo ratings yet
- 2002 09334 PDFDocument29 pages2002 09334 PDFGaurav GuptaNo ratings yet
- CT Imaging Features of 2019 Novel Coronavirus (2019-Ncov) : Materials and MethodsDocument6 pagesCT Imaging Features of 2019 Novel Coronavirus (2019-Ncov) : Materials and MethodsALEJANDRANo ratings yet
- Wu2020 Article InterpretationOfCTSignsOf2019NDocument8 pagesWu2020 Article InterpretationOfCTSignsOf2019NBruce WilliamNo ratings yet
- Us Chest CT Findings in Coronavirus Disease PDFDocument7 pagesUs Chest CT Findings in Coronavirus Disease PDFRomit JainNo ratings yet
- Iaa CovisDocument8 pagesIaa Covissanya eusebia lupaca lupacaNo ratings yet
- Calon Jurnal Radio 4Document7 pagesCalon Jurnal Radio 4harryNo ratings yet
- Cryptogenic Organizing Pneumonia: Serial High-Resolution CT Findings in 22 PatientsDocument7 pagesCryptogenic Organizing Pneumonia: Serial High-Resolution CT Findings in 22 Patientsdicky wahyudiNo ratings yet
- Evaluation of Covid-19 Pneumonia by Conventional Radiographyat Agmc & GBP HospitalDocument8 pagesEvaluation of Covid-19 Pneumonia by Conventional Radiographyat Agmc & GBP HospitalIJAR JOURNALNo ratings yet
- Acute Pulmonary Embolism Associated With COVID-19 Pneumonia Detected With Pulmonary CT AngiographyDocument3 pagesAcute Pulmonary Embolism Associated With COVID-19 Pneumonia Detected With Pulmonary CT AngiographyAdriano OliveiraNo ratings yet
- European Journal of Radiology: A B 1 B C 1 D 1 e 1 F B C B G G B C H eDocument9 pagesEuropean Journal of Radiology: A B 1 B C 1 D 1 e 1 F B C B G G B C H eLia NadaNo ratings yet
- Trombositopenia Covid PDFDocument16 pagesTrombositopenia Covid PDFYenni PramithaNo ratings yet
- Computers in Biology and MedicineDocument9 pagesComputers in Biology and MedicinePraneethaNo ratings yet
- Covid-19 Pneumonija Radioloska SlikaDocument11 pagesCovid-19 Pneumonija Radioloska SlikaStefan BaumanNo ratings yet
- The Pulmonary Sequalae in Discharged Patients With COVID-19: A Short-Term Observational StudyDocument7 pagesThe Pulmonary Sequalae in Discharged Patients With COVID-19: A Short-Term Observational StudyCloud NeilalungNo ratings yet
- Evaluation of Corona Virus Related Respiratory Illness by Chest Radiography at Tertiary Care Hospital, Agartala A Descriptive StudyDocument5 pagesEvaluation of Corona Virus Related Respiratory Illness by Chest Radiography at Tertiary Care Hospital, Agartala A Descriptive StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Imaging and Clinical Features of Patients With 2019 Novel Coronavirus Sars-Cov-2Document6 pagesImaging and Clinical Features of Patients With 2019 Novel Coronavirus Sars-Cov-2NadanNadhifahNo ratings yet
- Clinico Radiological Evaluation and Correlation of CTDocument1 pageClinico Radiological Evaluation and Correlation of CTRevaNo ratings yet
- Radiologi 3Document5 pagesRadiologi 3Sarah watiNo ratings yet
- Biomedical Signal Processing and Control: Prasad Kalane, Sarika Patil, B.P. Patil, Davinder Pal SharmaDocument9 pagesBiomedical Signal Processing and Control: Prasad Kalane, Sarika Patil, B.P. Patil, Davinder Pal SharmaShivam Mani Tripathi x-c 11No ratings yet
- Chest CT CovidDocument6 pagesChest CT CovidShinta FrennandaNo ratings yet
- Covid - Mtnet: Covid-19 Detection With Multi-Task Deep Learning ApproachesDocument11 pagesCovid - Mtnet: Covid-19 Detection With Multi-Task Deep Learning ApproachesEbrahim Abd El HadyNo ratings yet
- Big Data ApplicationsDocument9 pagesBig Data ApplicationsAndy BaiNo ratings yet
- Diagnostic Accuracy of CT-Guided Transthoracic Needle Biopsy For Solitary Pulmonary NodulesDocument9 pagesDiagnostic Accuracy of CT-Guided Transthoracic Needle Biopsy For Solitary Pulmonary NodulesDesiree MejicaNo ratings yet
- International Journal of Infectious DiseasesDocument3 pagesInternational Journal of Infectious DiseasesDetti FahmiasyariNo ratings yet
- Covid 19Document9 pagesCovid 19MonicaNo ratings yet
- Clinical Microbiology and Infection: Research NoteDocument4 pagesClinical Microbiology and Infection: Research NoteNoorNo ratings yet
- International Journal of Infectious DiseasesDocument7 pagesInternational Journal of Infectious Diseaseshardilas kaur behalNo ratings yet
- Radiology Indispensable For Tracking COVID-19Document7 pagesRadiology Indispensable For Tracking COVID-19Leonard AcsinteNo ratings yet
- JCS: An Explainable COVID-19 Diagnosis System via Joint Classification and SegmentationDocument11 pagesJCS: An Explainable COVID-19 Diagnosis System via Joint Classification and Segmentationzj xiaoNo ratings yet
- Covid - Mtnet: Covid-19 Detection With Multi-Task Deep Learning ApproachesDocument12 pagesCovid - Mtnet: Covid-19 Detection With Multi-Task Deep Learning ApproachesFidel Huanco RamosNo ratings yet
- Clinical Characteristics of CoronavirusDocument13 pagesClinical Characteristics of Coronavirusleonardo almeidaNo ratings yet
- The Value of HRCT Chest in Diagnosis of COVID 19 and Its Correlation With RT-PCRDocument5 pagesThe Value of HRCT Chest in Diagnosis of COVID 19 and Its Correlation With RT-PCREditor IJETBSNo ratings yet
- The Role of Chest CT Quantitative Pulmonary Inflammatory Index in The Evaluation of The Course and Treatment Outcome of COVID 19 PneumoniaDocument10 pagesThe Role of Chest CT Quantitative Pulmonary Inflammatory Index in The Evaluation of The Course and Treatment Outcome of COVID 19 PneumoniaEka BagaskaraNo ratings yet
- Nejmoa 2002032Document13 pagesNejmoa 2002032Juan Antonio LópezNo ratings yet
- BJR 20200219Document9 pagesBJR 20200219WilsonR.CorzoNiñoNo ratings yet
- Effect of respiratory rehabilitation on quality of life in pneumoconiosis patientsDocument4 pagesEffect of respiratory rehabilitation on quality of life in pneumoconiosis patientssukiyantoNo ratings yet
- Positive Chest CT Features in Patients With COVID-19 Pneumonia and Negative Real-Time Polymerase Chain Reaction TestDocument16 pagesPositive Chest CT Features in Patients With COVID-19 Pneumonia and Negative Real-Time Polymerase Chain Reaction TestHector MarrufoNo ratings yet
- XmdffaDocument5 pagesXmdffaIndira LarasatiNo ratings yet
- AI analysis of COVID-19 CT features by clinical typeDocument9 pagesAI analysis of COVID-19 CT features by clinical typeWilsonR.CorzoNiñoNo ratings yet
- Clinical Characteristics of Coronavirus Disease 2019 in ChinaDocument13 pagesClinical Characteristics of Coronavirus Disease 2019 in ChinaprimaNo ratings yet
- Novel Coronavirus PneumoniaDocument2 pagesNovel Coronavirus PneumoniaTeo LazzariNo ratings yet
- Diagnostik Dasar Radiologis COVID-19Document42 pagesDiagnostik Dasar Radiologis COVID-19tenty isniNo ratings yet
- CT UrethrographyDocument7 pagesCT UrethrographyhopephaseNo ratings yet
- (IJCST-V8I3P13) :pranali Manapure, Kiran Likhar, Hemlata KosareDocument5 pages(IJCST-V8I3P13) :pranali Manapure, Kiran Likhar, Hemlata KosareEighthSenseGroupNo ratings yet
- Histopathologic Analysis of Ct-Guided Core Needle Biopsy in Radiologically Detected Suspicious Mediastinal and Lung Mass: Two Years' Study in Tertiary HospitalDocument4 pagesHistopathologic Analysis of Ct-Guided Core Needle Biopsy in Radiologically Detected Suspicious Mediastinal and Lung Mass: Two Years' Study in Tertiary HospitalDesiree MejicaNo ratings yet
- Upper Respiratory Viral Load in Asymptomatic Individuals and Mildly Symptomatic Patients With Sars-Cov-2 InfectionDocument4 pagesUpper Respiratory Viral Load in Asymptomatic Individuals and Mildly Symptomatic Patients With Sars-Cov-2 InfectionVenkatapathi RajuNo ratings yet
- Diagnostic Imaging of Novel Coronavirus PneumoniaFrom EverandDiagnostic Imaging of Novel Coronavirus PneumoniaMinming ZhangNo ratings yet
- Long-Term Control of Macular Edema With Adalimumab After Cataract Surgery in A Japanese Child With Juvenile Idiopathic Arthritis: Case Report and Review of 26 Japanese PatientsDocument10 pagesLong-Term Control of Macular Edema With Adalimumab After Cataract Surgery in A Japanese Child With Juvenile Idiopathic Arthritis: Case Report and Review of 26 Japanese PatientsAhmad Fari Arief LopaNo ratings yet
- 2019 Article 1273Document17 pages2019 Article 1273Ahmad Fari Arief LopaNo ratings yet
- 2019 Article 1273Document17 pages2019 Article 1273Ahmad Fari Arief LopaNo ratings yet
- Image Quality of Prospectively ECG-Triggered Coronary CT Angiography in Heart Transplant RecipientsDocument6 pagesImage Quality of Prospectively ECG-Triggered Coronary CT Angiography in Heart Transplant RecipientsAhmad Fari Arief LopaNo ratings yet
- CT Findings of Pneumonia After Lung TransplantationDocument8 pagesCT Findings of Pneumonia After Lung TransplantationAhmad Fari Arief LopaNo ratings yet
- Jurnal 20Document5 pagesJurnal 20Ahmad Fari Arief LopaNo ratings yet
- Image Quality of Prospectively ECG-Triggered Coronary CT Angiography in Heart Transplant RecipientsDocument6 pagesImage Quality of Prospectively ECG-Triggered Coronary CT Angiography in Heart Transplant RecipientsAhmad Fari Arief LopaNo ratings yet
- Rare Fungal Infection Linked To A Case of Juvenile ArthritisDocument9 pagesRare Fungal Infection Linked To A Case of Juvenile ArthritisAhmad Fari Arief LopaNo ratings yet
- Jurnal 2Document9 pagesJurnal 2Ahmad Fari Arief LopaNo ratings yet
- RG 2018170048 PDFDocument21 pagesRG 2018170048 PDFDiana CaballeroNo ratings yet
- COVID-19 Pneumonia: A Pictorial Review of CT Findings and Differential DiagnosisDocument8 pagesCOVID-19 Pneumonia: A Pictorial Review of CT Findings and Differential DiagnosisAhmad Fari Arief LopaNo ratings yet
- Adenovirus Pneumonia in Adults: Radiographic and High-Resolution CT Findings in Five PatientsDocument6 pagesAdenovirus Pneumonia in Adults: Radiographic and High-Resolution CT Findings in Five PatientsAhmad Fari Arief LopaNo ratings yet
- Imaging of COVID-19 Pneumonia: Patterns, Pathogenesis, and AdvancesDocument12 pagesImaging of COVID-19 Pneumonia: Patterns, Pathogenesis, and AdvancesFafan UpinNo ratings yet
- Jurnal 20Document5 pagesJurnal 20Ahmad Fari Arief LopaNo ratings yet
- Jurnal 7Document8 pagesJurnal 7Ahmad Fari Arief LopaNo ratings yet
- Jurnal 2Document9 pagesJurnal 2Ahmad Fari Arief LopaNo ratings yet
- Jurnal 1Document6 pagesJurnal 1Ahmad Fari Arief LopaNo ratings yet
- Jurnal 1Document6 pagesJurnal 1Ahmad Fari Arief LopaNo ratings yet
- Jurnal 4Document8 pagesJurnal 4Ahmad Fari Arief LopaNo ratings yet
- Adenovirus Pneumonia in Adults: Radiographic and High-Resolution CT Findings in Five PatientsDocument6 pagesAdenovirus Pneumonia in Adults: Radiographic and High-Resolution CT Findings in Five PatientsAhmad Fari Arief LopaNo ratings yet
- 1 SMDocument9 pages1 SMSiti Lailatun NikmahNo ratings yet
- Referat Kandidosis Kutis - Dhira Dan A. Fari-70700120034 Dan 038Document14 pagesReferat Kandidosis Kutis - Dhira Dan A. Fari-70700120034 Dan 038Ahmad Fari Arief LopaNo ratings yet
- Early Clinical and CT Manifestations of Coronavirus Disease 2019 (COVID-19) PneumoniaDocument6 pagesEarly Clinical and CT Manifestations of Coronavirus Disease 2019 (COVID-19) PneumoniaAhmad Fari Arief LopaNo ratings yet
- Early Clinical and CT Manifestations of Coronavirus Disease 2019 (COVID-19) PneumoniaDocument6 pagesEarly Clinical and CT Manifestations of Coronavirus Disease 2019 (COVID-19) PneumoniaAhmad Fari Arief LopaNo ratings yet
- Journal Reading BartholinithisDocument21 pagesJournal Reading BartholinithisAhmad Fari Arief LopaNo ratings yet
- Journal Reading BartholinithisDocument21 pagesJournal Reading BartholinithisAhmad Fari Arief LopaNo ratings yet
- Elastic Bandage and Triangular Bandage UsesDocument1 pageElastic Bandage and Triangular Bandage UsesAllyssa ThalliaNo ratings yet
- VI. Week6-CM - HIV AWARENESSDocument14 pagesVI. Week6-CM - HIV AWARENESSMarianne Jade HonorarioNo ratings yet
- Chapter 1 Introduction To Emergency Medical CareDocument19 pagesChapter 1 Introduction To Emergency Medical Carejmmos207064100% (1)
- ALF 418RLE Group1Document22 pagesALF 418RLE Group1PAOLA LUZ CRUZNo ratings yet
- Brain-Attack or Stroke or Cerebrovascular-AccidentDocument29 pagesBrain-Attack or Stroke or Cerebrovascular-AccidentMission JupiterNo ratings yet
- Urethral Stricture Diagnosis and TreatmentDocument9 pagesUrethral Stricture Diagnosis and TreatmentNadila Ayu PutriNo ratings yet
- 4 Accidents and EmergenciesDocument4 pages4 Accidents and EmergenciesViska Ayu NiraniNo ratings yet
- Online CatalogueDocument21 pagesOnline CatalogueAsishmukundan AsishNo ratings yet
- HIV Prevention Module StrategiesDocument12 pagesHIV Prevention Module StrategieslebogangNo ratings yet
- Diets Based On Ayurvedic Constitution - Potential For Weight ManagementDocument89 pagesDiets Based On Ayurvedic Constitution - Potential For Weight ManagementHema NarulaNo ratings yet
- S.K. Yee Medical Foundation: Application Form For Funding of ProjectDocument12 pagesS.K. Yee Medical Foundation: Application Form For Funding of ProjectLawrence ChanNo ratings yet
- Drop Foot, An Unexpected Complication of Vaginal HysterectomyDocument4 pagesDrop Foot, An Unexpected Complication of Vaginal HysterectomySandraSaracNo ratings yet
- Systematic Approach in Anemia Evaluation and Review of Peripheral SmearsDocument72 pagesSystematic Approach in Anemia Evaluation and Review of Peripheral SmearsSukma Eka PratiwiNo ratings yet
- Course: Medical Astrology: Basic To Advanced Course ConductorDocument2 pagesCourse: Medical Astrology: Basic To Advanced Course ConductorAshok ShettigarNo ratings yet
- Dr. Tariq Mahmood Sheikh GP-Diploma MRT (ONCOLOGY)Document3 pagesDr. Tariq Mahmood Sheikh GP-Diploma MRT (ONCOLOGY)cdeekyNo ratings yet
- 1 Choosing An Org Worksheet 2Document4 pages1 Choosing An Org Worksheet 2api-562131193No ratings yet
- Dosage Form ExamDocument9 pagesDosage Form ExamsongaNo ratings yet
- Dry CoughDocument3 pagesDry Coughnevismn3498No ratings yet
- Heartsaver SlidesDocument21 pagesHeartsaver SlidesBelLa EakoiNo ratings yet
- EuthanasiaDocument4 pagesEuthanasiaAlessandra CruzNo ratings yet
- Forand Et Al. (2019) Guided Internet CBT Versus "Gold Standard" Depression Treatments - An Individual Patient AnalysisDocument14 pagesForand Et Al. (2019) Guided Internet CBT Versus "Gold Standard" Depression Treatments - An Individual Patient AnalysisPhilip BeardNo ratings yet
- ANTENATAL CARE Translate GooglingDocument26 pagesANTENATAL CARE Translate GooglingLutfi ari206100% (2)
- Early Theories about Cancer CausesDocument13 pagesEarly Theories about Cancer CausesBernadetteGaleraNo ratings yet
- Pathology and Physiology Nums McqsDocument68 pagesPathology and Physiology Nums McqsZara100% (1)