Professional Documents
Culture Documents
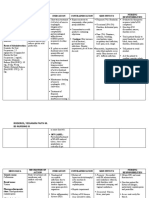
Empirical Antimicrobial Therapy Prescribing Guidance For Adults
Uploaded by
Psychology Today0 ratings0% found this document useful (0 votes)
12 views1 pageThis document provides guidance on empirical antimicrobial therapy for various infections in adults. It emphasizes the importance of obtaining cultures and considering delaying antibiotic therapy unless there is a clear site of infection. It lists recommended first-line oral antibiotic options for lower respiratory tract infections, urinary tract infections, gastrointestinal infections, and skin/soft tissue infections. It notes certain antibiotics should be used with caution in patients at high risk for Clostridium difficile infection.
Original Description:
Original Title
IMG EmpAposter
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides guidance on empirical antimicrobial therapy for various infections in adults. It emphasizes the importance of obtaining cultures and considering delaying antibiotic therapy unless there is a clear site of infection. It lists recommended first-line oral antibiotic options for lower respiratory tract infections, urinary tract infections, gastrointestinal infections, and skin/soft tissue infections. It notes certain antibiotics should be used with caution in patients at high risk for Clostridium difficile infection.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
12 views1 pageEmpirical Antimicrobial Therapy Prescribing Guidance For Adults
Uploaded by
Psychology TodayThis document provides guidance on empirical antimicrobial therapy for various infections in adults. It emphasizes the importance of obtaining cultures and considering delaying antibiotic therapy unless there is a clear site of infection. It lists recommended first-line oral antibiotic options for lower respiratory tract infections, urinary tract infections, gastrointestinal infections, and skin/soft tissue infections. It notes certain antibiotics should be used with caution in patients at high risk for Clostridium difficile infection.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
Guidance for initial hospital therapy in adults.
Specialist units may have separate policies
Empirical Antimicrobial Therapy Prescribing Guidance for Adults
STOP AND THINK BEFORE YOU GIVE ANTIBIOTIC THERAPY! Antibiotics are overused in the elderly (particularly patients with urinary catheters or suspected UTIs) and in patients with viral or non-infective exacerbations
of COPD. Always obtain cultures and consider delay in therapy unless there is a clear anatomical site of infection with high probability of bacterial aetiology, sepsis or clinical deterioration. Check previous microbiology
results. Doses quoted are for patients without renal or hepatic impairment, please adjust if necessary. Consider cautions, contra-indications and drug interactions.
ORAL THERAPY USUALLY RECOMMENDED IMPORTANT NOTES
Lower Respiratory Tract Urinary Tract Gastro-Intestinal Skin/Soft Tissue
REVIEW ANTIBIOTIC THERAPY
GUIDANCE ICONS
Limited soft tissue infection DAILY:
Pneumonia Lower Respiratory Tract Lower UTI/cystitis – female Gastroenteritis
Infection (LRTI) – define Oral Flucloxacillin 1g 6hrly Gentamicin/Vancomycin - see
CURB65 score:
diagnosis (e.g. acute bronchitis,
Antibiotics if symptoms + No antibiotic usually required.
If true penicillin allergy
STOP? ** prescribing guidance on intranet
Confusion (new onset), Urea >7, RR>30, diast BP<60 positive urinalysis. Consider
exacerbation COPD, CAP) and Clostridium difficile Oral Clarithromycin 500mg
or syst BP<90, age >65yrs. delaying antibiotic therapy Aztreonam If eGFR < 30mL/min (CKD>4)
Additional adverse features: hypoxia (SAO2 <92%) or multilobar treat accordingly pending urine culture.
associated diarrhoea 12hrly SIMPLIFY? or known/ suspected AKI consider
consolidation or cavitation on x-ray. Exacerbation of COPD Catheter specimen of urine is Stop/simplify concomitant Duration 7 - 14 days. § aztreonam IV as alternative to gentamicin
antibiotics and gastric acid
Low Severity Community Acquired Pneumonia (CAP) Antibiotics only if purulent
unreliable.
Caution with these antibiotics suppressive therapy if possible. Infected bite SWITCH? – see dosing information on intranet
sputum and raised WCC or Human or animal bite
# IffullIVguideline
Co-trimoxazole not available - see
CURB65 score: 0-1 in patients with CKD ≥3 or at Refer to full guidance for list
Oral Amoxicillin 1g 8hrly
CRP. Use 1st line antibiotic
risk of hyperkalaemia. of severity factors.
Oral Co-amoxiclav 625mg DOCUMENT! for advice
unless recent hospitalisation or 8hrly
or Non-severe: oral
recent antibiotic. Trimethoprim 200mg 12hrly Second line or in penicillin
Oral Doxycycline 200mg stat then 100mg daily. Metronidazole 400mg 8hrly
Mild to Moderate Severity
or
Nitrofurantoin 100mg m/r Severe or no improvement
allergy Clostridium difficile infection (CDI) risk.
Duration 5 days – consider extending if symptoms not im- Oral Doxycycline 100mg
proved after 3 days. Oral Amoxicillin 1g 8hrly 12hrly or 50mg i/r 6hrly after 5 days of Metronidazole; 12hrly Use the following antibiotics with caution in high risk patients e.g. frail elderly,
Duration 3 days. oral Vancomycin 125mg +Metronidazole 400mg 8hrly
Moderate Severity CAP If true penicillin allergy 6hrly (add IV Metronidazole immunosupressed, prolonged hospital stay, previous CDI, recent antibiotics.
Doxycyline 200mg stat then Uncomplicated UTI - men Duration 7 days
CURB65 score: = 2 500mg 8hrly if ileus or
100mg daily. As above duration 7 days. hypotension)
High risk antibiotics: clindamycin, ceftriaxone, ceftazidime, ciprofloxacin,
Oral/IV Amoxicillin 1g 8hrly Diabetic Foot Infection
Duration 5 days. levofloxacin, co-amoxiclav, clarithromycin, meropenem.
+ oral Clarithromycin 500mg 12hrly (until atypical excluded) UTI in Pregnancy Total duration 10 days. Refer to protocol on Diabetes
If true penicillin allergy Nitrofurantoin 100mg m/r Recurrent CDI – discuss with Grampian Guidance intranet
microbiology / ID page.
oral Doxycycline monotherapy 100mg 12 hrly Severe Infective
12hrly or 50mg i/r 6hrly URGENT IV THERAPY
or if IV required, treat as per CURB65 >3 (Avoid in 3rd trimester)
Exacerbation of COPD or
Total duration 5-7 days – consider extending if symptoms not Co-trimoxazole 960mg IV# Trimethoprim 200mg 12hrly Intra-abdominal Sepsis Moderate to severe cellulitis
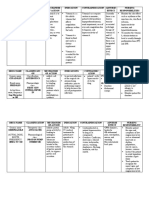
improved after 3 days. Sepsis - Source Unknown CNS Infection Endocarditis
12hrly
Switch to oral
(Avoid in 1st trimester) Gentamicin ** IV
+ Metronidazole 500mg 8hrly
Flucloxacillin 1-2g 6hrly IV
(use 2g if BMI>30)
If 1st line options unsuitable Sepsis - Source Unknown IV therapy to be Possible infective endocarditis
Co-trimoxazole 960mg 12hrly Cefalexin 500mg 12hrly IV
High Severity CAP or Switch to oral administered URGENTLY on
+ Amoxicillin 1g 8hrly IV Flucloxacillin 1g 6hrly Amoxicillin 1g 8hrly IV Seek senior specialist advice.
CURB65 score: ≥3:
No Previous Antibiotic
Doxycycline 200mg stat then
100mg 12 hrly when condition
Duration 7 days.
If true penicillin allergy or If true penicillin allergy or if
+ Gentamicin ** IV
+/- Metronidazole 500mg
arrival at hospital and after
blood cultures. Indolent:
Complicated UTI gentamicin not appropriate MRSA likely Amoxicillin 2g IV 4hrly
IV Amoxicillin 1g 8hrly improves. 8hrly IV (add if anaerobic cover CT scan before LP if seizures,
(renal tract abnormality)
+ Second line
Oral Co-trimoxazole 960mg
Co-trimoxazole 960mg
12hrly IV#
Vancomycin IV
Switch to oral
** required) reduced GCS, papilloedema, + (optional) Gentamicin IV
as per synergistic dosing
Oral Clarithromycin 500mg 12hrly (until atypical excluded) Clarithromycin 500mg 12hrly + Metronidazole 500mg 8hrly In true penicillin allergy or CNS signs or
12hrly Doxycycline 100mg 12hrly immunosuppression. protocol
IV then switch to oral when IV known MRSA
Switch to oral Second line
Doxycycline monotherapy 100mg 12 hrly
condition improves.
Ciprofloxacin 500mg oral Switch to oral Total duration 7-14 days. Gentamicin ** IV Seek ID/microbiology advice. Severe sepsis, acute
or
Total duration 7 days. 12hrly Metronidazole 400mg 8hrly Suspected necrotising + Vancomycin ** IV presentation or penicillin allergy:
Amoxicillin 1g 8 hrly Duration 7-14 days.
+
Doxycycline 100-200mg daily
fasciitis or severe or rapidly
progressive infection in an
+/- Metronidazole 500mg
8hrly IV
Meningitis Vancomycin ** IV
Hospital acquired Ceftriaxone 2g 12hrly IV + Gentamicin IV as per
+ Clarithromycin 500mg 12hrly (until atypical excluded) or IVDU Consider aztreonam§ IV as
Pneumonia synergistic dosing protocol
Previous Antibiotics Metronidazole 400mg 8hrly alternative to gentamicin. If true penicillin allergy
Early (≤4 days of admission) Catheter-related UTI EARLY DEBRIDEMENT/
Chloramphenicol 12.5-25mg/
Co-amoxiclav 1.2g 8hrly IV + EXPLORATION IS ESSENTIAL Intra-cardiac prosthesis:
Treat as for CAP Antibiotics are not indicated
+ Clarithromycin 500mg 12hrly Oral/IV (until atypical excluded)
Late (>5 days of admission) unless evidence of systemic
Co-trimoxazole 960mg
12hrly Flucloxacillin 2g 6hrly IV Neutropenic Sepsis kg 6hrly IV
If age >55 to cover Listeria
Vancomycin ** IV
Switch to oral infection e.g. pyrexia, loin + Benzylpenicillin 2.4g 6hrly IV Standard risk patients: + Gentamicin IV as per
Non-severe Total duration 3-5 days. + Amoxicillin 2g 4hrly IV
Doxycycline monotherapy 100mg 12hrly
Amoxicillin oral 1g 8hrly
pain, raised WCC or acute
confusion in elderly. If
+ Gentamicin ** IV
+ Clindamycin IV 600mg-1.2g
Piperacillin/Tazobactam 4.5g
6hrly IV or in penicillin allergy
synergistic dosing protocol
+ Rifampicin 300-600mg
If true penicillin allergy
Co-trimoxazole 960mg 12hrly IV#
If true penicillin allergy systemic infection likely 6-8hrly In mild penicillin allergy
+ Vancomycin IV ** oral / IV 12hrly
Doxycycline oral 100mg treat as complicated UTI or Ceftazidime 2g 8hrly IV Give Dexamethasone IV for
or pyelonephritis depending on Biliary Sepsis Switch to oral
12hrly (In severe penicillin allergy see 4 days
Levofloxacin 500mg 12hrly IV clinical symptoms. Remove/ Flucloxacillin 500mg-1g 6hrly FURTHER ADVICE
or Amoxicillin 1g 8hrly IV below)
+ Amoxicillin 500mg-1g 8hrly Duration 7 days for
Switch to oral
Doxycycline monotherapy 100mg 12hrly
Co-trimoxazole oral 960mg
12hrly
replace catheter following 1st
or 2nd dose of antibiotic.
+ Gentamicin ** IV
+/- Metronidazole 500mg
Clindamycin 600mg 8hrly High risk patients: meningococcal, 14 days for Can be obtained from the
Duty Microbiologist or Clinical
or Total duration 5 days. 8hrly IV In penicillin allergy: Add Gentamicin ** IV to pneumococcal
Pharmacist or the ID Unit
Co-trimoxazole 960mg 12hrly Pyelonephritis / Urosepsis If true penicillin allergy or
Vancomycin IV **
+ Clindamycin 600mg-1.2g
options above Refer to full guidance for further
information.
Aberdeen Royal Infirmary.
Severe Septic shock or severe Infection Control advice may be
Total duration (IV plus oral) 7-10 days Co-amoxiclav IV 1.2g 8hrly Gentamicin ** IV (NB: if gentamicin not appropriate
Co-trimoxazole 960mg
IV 6-8hrly penicillin allergy in Standard / given by the duty microbiologist.
+ Gentamicin ** IV if life reduced or unstable renal
function give single dose 12hrly IV#
+ Gentamicin ** IV
Switch to oral options
High risk patients Encephalitis
Aciclovir 10mg/kg 8hrly IV The full antibiotic guidelines and
threatening. +/- Metronidazole 500mg Meropenem 1g 8hrly IV
Aspiration Pneumonia Switch to oral Co-amoxiclav only then review with ID or depending on sensitivities. policies can be found on the
microbiology) 8hrly IV Consider aztreonam§ IV as Duration 14 - 21 days intranet at:
If oral antibiotics appropriate, 625mg 8 hrly. Duration: micro/ID advice alternative to gentamicin. (if confirmed).
+ Amoxicillin 1g IV 8hrly Switch to oral www.nhsgrampian.org/gjf -
Oral Amoxicillin 1g 8hrly If true penicillin allergy Switch to oral option guided Doxycycline 100-200mg daily Chapter 5 Infections.
+ Oral Metronidazole 400mg 8hrly Levofloxacin 500mg (IV or by microbiology sensitivities. +/- Metronidazole 400mg
oral) 12hrly Post-operative infection – “Clean sites” Post-operative infection – “Dirty sites” e.g.
If IV required, 8hrly Abdominal, Female genital tract, Head/Neck Produced by the NHS Grampian
In penicillin allergy Flucloxacillin 500mg-1g 6hrly IV or oral Antimicrobial Management Team
IV Amoxicillin 1g 8hrly Total duration 7-10 days. Ciprofloxacin 500mg oral (or or
In penicillin allergy Co-trimoxazole 960mg IV# 12hrly
+ IV Metronidazole 500mg 8hrly If MRSA likely add 400mg IV) 12hrly. Co-trimoxazole 960mg November 2018.
+/- Metronidazole 500mg IV 8hrly
If true penicillin allergy Vancomycin ** IV as per Total duration 7 days (if
12hrly Vancomycin IV ** as per protocol
Switch to oral
Review November 2021.
Clarithromycin 500mg 12hrly (oral or IV) protocol. +/- Metronidazole 400mg Switch to oral
urinary tract abnormality 8hrly Co-trimoxazole 960mg 12hrly
+ Metronidazole 8hrly (oral 400mg or IV 500mg) consider 10-14 days). Co-trimoxazole 960mg 12hrly
Total duration 10-14 days +/- Metronidazole 400mg 8hrly
Total duration 7 days.
Total duration 7 days. Total duration 10-14 days Version 6
ZA03441 CGD180364
You might also like
- IMG EmpAposterDocument1 pageIMG EmpAposterChiu LeoNo ratings yet
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- OB Drug StudyDocument5 pagesOB Drug Studyvanni213No ratings yet
- Drug Study MetoclopramideDocument2 pagesDrug Study Metoclopramiderica sebabillones100% (1)
- Drug Study: Nursing DepartmentDocument2 pagesDrug Study: Nursing Departmentrica sebabillones100% (1)
- Drug Study: Nerviol, JanaicaDocument2 pagesDrug Study: Nerviol, JanaicaCherry Dianopra VillaruelNo ratings yet
- Empirical Prescribing Chart GlasgowDocument1 pageEmpirical Prescribing Chart GlasgowHariharan Narendran75% (4)
- Tetanus toxoid side effects and nursing responsibilitiesDocument10 pagesTetanus toxoid side effects and nursing responsibilitiesElle RosalesNo ratings yet
- Case Scenario Typhoid FeverDocument5 pagesCase Scenario Typhoid FeverMae Arra Lecobu-anNo ratings yet
- CandidiasisDocument5 pagesCandidiasisGallel PanumNo ratings yet
- Ketorolac DRUG STUDYDocument3 pagesKetorolac DRUG STUDYA.No ratings yet
- Ketorolac, Pregabalin, Metoprolol nursing considerationsDocument4 pagesKetorolac, Pregabalin, Metoprolol nursing considerationsgayeng04No ratings yet
- Viii. Pharmacologic Intervention (Drug Study)Document10 pagesViii. Pharmacologic Intervention (Drug Study)Cyril Jane Caanyagan AcutNo ratings yet
- Generic Name Indication Classification Pharmacokinetics Nursing ConsiderationDocument5 pagesGeneric Name Indication Classification Pharmacokinetics Nursing Considerationjoy rachel tabernillaNo ratings yet
- Drug Study - CoAmoxiclavDocument2 pagesDrug Study - CoAmoxiclavLegendX100% (6)
- Clindamycin and Balsalazide Drug SheetDocument5 pagesClindamycin and Balsalazide Drug SheetLouwella RamosNo ratings yet
- AmikinDocument2 pagesAmikinLIEZEL GRACE VELAYONo ratings yet
- Drug Study EntecavirDocument4 pagesDrug Study EntecavirClarimae AwingNo ratings yet
- Bagong DrugsDocument7 pagesBagong DrugsmcensoredNo ratings yet
- 4 DrugsuDocument8 pages4 Drugsuahmad ryanNo ratings yet
- Cefuroxomine Drug StudyDocument3 pagesCefuroxomine Drug StudyNiziu BearsNo ratings yet
- Drug StudyDocument25 pagesDrug StudyRoland YusteNo ratings yet
- Medication Mechanism of Action Indications Contraindications Side Effects Nursing ResponsibilitiesDocument1 pageMedication Mechanism of Action Indications Contraindications Side Effects Nursing Responsibilitiesjoan bagnateNo ratings yet
- Classification: Gastrointestinal Drugs-Laxatives Generic Name Precaution/ Consideration Nursing Contraindication AdverseDocument12 pagesClassification: Gastrointestinal Drugs-Laxatives Generic Name Precaution/ Consideration Nursing Contraindication AdverseLenjunNo ratings yet
- H2 Receptor Antagonists and LidocaineDocument14 pagesH2 Receptor Antagonists and LidocaineJoharaNo ratings yet
- Clarithromycin (Biaxin)Document1 pageClarithromycin (Biaxin)Jocelyn Rivera100% (1)
- Drug StudyDocument3 pagesDrug StudyJaNo ratings yet
- Final AcetylcysteineDocument2 pagesFinal AcetylcysteineGwyn RosalesNo ratings yet
- Nameof DrugDocument16 pagesNameof DrugshiNo ratings yet
- 2021 Infection Management PosterDocument1 page2021 Infection Management PosterBosco WoodsNo ratings yet
- Drugstudy 3Document1 pageDrugstudy 3Lorlyn OrehuelaNo ratings yet
- Drug Name Classification Mechanism of Action Indication ContraindicationsDocument4 pagesDrug Name Classification Mechanism of Action Indication ContraindicationsAthena SaturdayNo ratings yet
- Orthopaedic Infection in Adults UHL GuidelineDocument10 pagesOrthopaedic Infection in Adults UHL GuidelineFadlu ManafNo ratings yet
- Brand Name: Generic Name: Drug ClassificationDocument2 pagesBrand Name: Generic Name: Drug ClassificationChristine Pialan SalimbagatNo ratings yet
- Dosage and effects of ampicillinDocument1 pageDosage and effects of ampicillinkimglaidyl bontuyanNo ratings yet
- ErythromycinDocument2 pagesErythromycinBtob meloNo ratings yet
- Bronchospasm Child: PO 2-6 Y, 0.1-: 0.2 MG/KG T.I.D. (Max: 4 Mg/dose) 6-12 Y, 2 MG 3-4 Times/dDocument2 pagesBronchospasm Child: PO 2-6 Y, 0.1-: 0.2 MG/KG T.I.D. (Max: 4 Mg/dose) 6-12 Y, 2 MG 3-4 Times/dArnold De Guzman Jr.No ratings yet
- NALAM 106 Ass. AntibioticsDocument6 pagesNALAM 106 Ass. AntibioticsBeth100% (1)
- Drug Study: Phinma - University of Iloilo College of Allied Health SciencesDocument3 pagesDrug Study: Phinma - University of Iloilo College of Allied Health Scienceslhie cabanlitNo ratings yet
- BTUH Antibiotics Pocket Guidelines For Prescribing in Adults 2017 2018Document2 pagesBTUH Antibiotics Pocket Guidelines For Prescribing in Adults 2017 2018Corry ApriliaNo ratings yet
- Name of Drug Mechanism of Action Indication/ Contraindicatio N Side Effects Nursing Responsibiliti EsDocument12 pagesName of Drug Mechanism of Action Indication/ Contraindicatio N Side Effects Nursing Responsibiliti EsdeliejoyceNo ratings yet
- Metoclopramide for Nausea, GERD and GastroparesisDocument2 pagesMetoclopramide for Nausea, GERD and GastroparesisBeatrizz P GellaNo ratings yet
- Drug Study: Cefuroxime, Ranitidine, Metoclopramide, ParacetamolDocument7 pagesDrug Study: Cefuroxime, Ranitidine, Metoclopramide, ParacetamolKceey CruzNo ratings yet
- Treating Febrile NeutropeniaDocument2 pagesTreating Febrile NeutropeniaAlvy SyukrieNo ratings yet
- Drug Study (Covid Case)Document5 pagesDrug Study (Covid Case)YessaminNo ratings yet
- Generic Name: BudesonideDocument8 pagesGeneric Name: BudesonidemeangelmeNo ratings yet
- Pediatric Guidelines: Head and Neck Infections - MastoiditisDocument3 pagesPediatric Guidelines: Head and Neck Infections - MastoiditisJr SparkNo ratings yet
- Davao Doctor Drug Study Program CriteriaDocument3 pagesDavao Doctor Drug Study Program Criteriakkd nyleNo ratings yet
- Drug Tabulation of Ampicillin SulbactamDocument1 pageDrug Tabulation of Ampicillin SulbactamJobie CasipongNo ratings yet
- Drug Study: Phinma University of PangasinanDocument1 pageDrug Study: Phinma University of Pangasinangiselle chloeNo ratings yet
- Nursing considerations for gentamycin drug studyDocument1 pageNursing considerations for gentamycin drug studygiselle chloeNo ratings yet
- Algorithm Hypertension Sci PDFDocument1 pageAlgorithm Hypertension Sci PDFGustavo CabanasNo ratings yet
- Penicillin G Drug StudyDocument1 pagePenicillin G Drug Studyjean therese100% (1)
- Drug StudyDocument7 pagesDrug StudyLA GomezNo ratings yet
- Drug Study - AmpicillinDocument1 pageDrug Study - AmpicillinJet BautistaNo ratings yet
- Antibiotic (Bacteriostatic) DrugsDocument15 pagesAntibiotic (Bacteriostatic) DrugsVictor LeeNo ratings yet
- Viii. Medications: Generic Name: Actions: AssessmentDocument4 pagesViii. Medications: Generic Name: Actions: AssessmentJohn Alex Maramba MelencioNo ratings yet
- Drug Study SummaryDocument2 pagesDrug Study SummaryLouisse Angeli AbucejoNo ratings yet
- CefuroximeDocument2 pagesCefuroximeJon Corpuz AggasidNo ratings yet
- Medical Certificate To Be Filled by DoctorDocument3 pagesMedical Certificate To Be Filled by DoctorPsychology TodayNo ratings yet
- Authorization To Release Medical CertificateDocument1 pageAuthorization To Release Medical CertificatePsychology TodayNo ratings yet
- PDF FileDocument1 pagePDF FilePsychology TodayNo ratings yet
- Sample Emergency Medicine Questions & Critiques: Question #1Document16 pagesSample Emergency Medicine Questions & Critiques: Question #1Psychology TodayNo ratings yet
- IELTS Notice To CandidatesDocument1 pageIELTS Notice To CandidatesMinh AnhNo ratings yet
- Restraint Prevalence and Perceived Coercion Among Psychiatric Inpatientsfrom South IndiaDocument7 pagesRestraint Prevalence and Perceived Coercion Among Psychiatric Inpatientsfrom South IndiaEdson HilárioNo ratings yet
- MEM Micro-ProjectDocument16 pagesMEM Micro-ProjectGanesh GoreNo ratings yet
- Glycerol PDFDocument3 pagesGlycerol PDFTushar GaikarNo ratings yet
- SOP - APS - PUR - 02A - Flow Chart For PurchaseDocument2 pagesSOP - APS - PUR - 02A - Flow Chart For Purchaseprakash patelNo ratings yet
- Harvia Sauna: Glass, light and beautiful contrast – read more about the new Harvia Claro sauna on page 11Document36 pagesHarvia Sauna: Glass, light and beautiful contrast – read more about the new Harvia Claro sauna on page 11Kadiri Olanrewaju100% (1)
- ProVent - MANN + HUMMEL ProVent - Oil Separator For Open and Closed Crankcase Ventilation SystemsDocument29 pagesProVent - MANN + HUMMEL ProVent - Oil Separator For Open and Closed Crankcase Ventilation SystemsJosephNo ratings yet
- End Time ProphecyDocument16 pagesEnd Time ProphecyMarven JabianNo ratings yet
- Welfare Schemes in TelanganaDocument46 pagesWelfare Schemes in TelanganaNare ChallagondlaNo ratings yet
- Pipe Material & Dimension Standard MatrixDocument2 pagesPipe Material & Dimension Standard MatrixHemantNo ratings yet
- EVBAT00100 Batterij ModuleDocument1 pageEVBAT00100 Batterij ModuleSaptCahbaguzNo ratings yet
- Antibiotic Susceptibility TestDocument5 pagesAntibiotic Susceptibility Testfarhanna8100% (3)
- Veena Singh-176-189 - Findings, Implications and ConclusionsDocument14 pagesVeena Singh-176-189 - Findings, Implications and ConclusionsValerine SNo ratings yet
- Five Brothers and Their Mother's LoveDocument4 pagesFive Brothers and Their Mother's Lovevelo67% (3)
- Camco D Series Running ToolsDocument2 pagesCamco D Series Running Toolshosam aliNo ratings yet
- Grundfosliterature 743129Document7 pagesGrundfosliterature 743129Ted Andrew AbalosNo ratings yet
- Pharm.D 2nd Year SyllabusDocument21 pagesPharm.D 2nd Year Syllabus12 E 36 Yatri PatelNo ratings yet
- KJ's Take Out MenuDocument1 pageKJ's Take Out MenuintegiegirlNo ratings yet
- Biosample Urine Sample Collection Protocol Infant v2Document2 pagesBiosample Urine Sample Collection Protocol Infant v2api-531349549No ratings yet
- Gulayan Project ProposalDocument2 pagesGulayan Project ProposalMarvin LagunillaNo ratings yet
- Previews 2013360 PreDocument13 pagesPreviews 2013360 PreEko Setyo BudiNo ratings yet
- 01 Itp-380kv Gis - PlanDocument9 pages01 Itp-380kv Gis - PlanYahya SamaraNo ratings yet
- Using Roger's Diffusion of Innovation Theory To Implement The Healthy Schools National AccreditationDocument6 pagesUsing Roger's Diffusion of Innovation Theory To Implement The Healthy Schools National AccreditationputriNo ratings yet
- Specification for Child MUAC Tape Quality ChecksDocument4 pagesSpecification for Child MUAC Tape Quality ChecksM HussainNo ratings yet
- Spelling Bee WordsDocument3 pagesSpelling Bee WordsDana GomezNo ratings yet
- Aos Ce 15400Document4 pagesAos Ce 15400Jovenal TuplanoNo ratings yet
- S35MC Engine Layout and Load DiagramsDocument17 pagesS35MC Engine Layout and Load DiagramsMuhammad AlfaniNo ratings yet
- Self Esteem and The Real Body ImageDocument12 pagesSelf Esteem and The Real Body ImageChy Alcarde50% (2)
- Transformer Protection Techniques for Fault DetectionDocument32 pagesTransformer Protection Techniques for Fault DetectionshashankaumNo ratings yet
- Thermo Fluids LabDocument23 pagesThermo Fluids LabMuket AgmasNo ratings yet
- Sect 5Document25 pagesSect 5PuneetNo ratings yet