Professional Documents
Culture Documents
Ana Repro
Uploaded by
FIONA DANE MAURERACopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ana Repro
Uploaded by
FIONA DANE MAURERACopyright:
Available Formats
The Reproductive System Extends from the base of the urinary bladder to the tip of
Gonads – primary sex organs the penis
Testes in males Carries both urine and sperm
Ovaries in females Sperm enters from the ejaculatory duct
Produce gametes (sex cells) and secrete hormones Regions of the urethra
Sperm – male gametes Prostatic urethra – surrounded by prostate
Ova (eggs) – female gametes Membranous urethra – from prostatic urethra to penis
Spongy (penile) urethra – runs the length of the penis
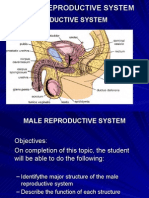
Male Reproductive System Seminal Vesicles
Testes Located at the base of the bladder
Duct system Produces a thick, yellowish secretion (60% of semen)
Epididymis Fructose (sugar)
Ductus deferens Vitamin C
Urethra Prostaglandins
Accessory organs Other substances that nourish and activate sperm
Seminal vesicle
Prostate gland Prostate Gland
Bulbourethral gland or Cowper’s gland Located at the base of the bladder
External genitalia Secretes a milky fluid
Penis Helps to activate sperm
Scrotum
Bulbourethral Glands
Testes Produces a thick, clear mucus
Coverings of the testes Cleanses the urethra of acidic urine
Tunica albuginea – capsule that surrounds each testis Serves as a lubricant during sexual intercourse
Septa – extensions of the capsule that extend into the Secreted into the penile urethra
testis and divide it into lobules
Each lobule contains one to four seminiferous tubules Semen
Function as sperm-forming factories Mixture of sperm and accessory gland secretions
Empty sperm into the rete testis Fructose provides energy for sperm cells
Rete testis to the epididymis or the site of maturation of Neutralizes the acidic environment of vagina
sperm cells Inhibits bacterial multiplication
Interstitial or Leydig’s cells produce androgens such as Enhances sperm motility
testosterone
External Genitalia
Epididymis Scrotum
Comma-shaped, tightly coiled tube Divided sac of skin outside the abdomen
Found on the superior part of the testis and along the Maintains testes at 3°C lower than normal body
posterior lateral side temperature to protect sperm viability
Functions to mature and store sperm cells (20 days) Penis
Expels sperm with the contraction of muscles in the Delivers sperm into the female reproductive tract
epididymis walls to the vas deferens Regions of the penis
o Shaft
Ductus Deferens (Vas Deferens) o Glans penis (enlarged tip)
Carries sperm from the epididymis to the ejaculatory duct o Prepuce (foreskin)
Passes through the inguinal canal and over the bladder Folded cuff of skin around proximal end
Moves sperm by peristalsis Often removed by circumcision
Spermatic cord – ductus deferens, blood vessels, and
nerves in a connective tissue sheath Spermatogenesis
Ends in the ejaculatory duct which unites with the urethra Production of sperm cells
Vasectomy – cutting of the ductus deferens at the level of Begins at puberty and continues throughout life
the testes to prevent transportation of sperm Occurs in the seminiferous tubules
Urethra Processes of Spermatogenesis
Spermatogonia (stem cells) undergo rapid mitosis to Broad ligament – a fold of the peritoneum, encloses
produce more stem cells before puberty suspensory ligament
Follicle stimulating hormone (FSH) modifies
spermatogonia division Uterine (Fallopian) Tubes
One cell produced is a stem cell Receive the ovulated oocyte
The other cell produced becomes a primary Provide a site for fertilization
spermatocyte Attaches to the uterus
Primary spermatocytes undergo meiosis Does not physically attach to the ovary
Haploid spermatids are produced Supported by the broad ligament
Spermiogenesis
Late spermatids are produced with distinct regions Uterine Tube Function
o Head – contains DNA covered by the acrosome Fimbriae – finger-like projections
o Midpiece Cilia inside the uterine tube slowly move the oocyte
o Tail towards the uterus
Sperm cells result after maturing of spermatids Fertilization occurs inside the uterine tube
Spermatogenesis takes 64 to 72 days
Uterus
Located between the urinary bladder and rectum
Anatomy of a Mature Sperm Cell Hollow organ
The only human flagellated cell Functions of the uterus
DNA is found in the head Receives a fertilized egg
Retains the fertilized egg
Testosterone Production Nourishes the fertilized egg
The most important hormone of the testes
Produced in interstitial cells Support for the Uterus
Functions of testosterone Broad ligament – attached to the pelvis
Stimulates reproductive organ development Round ligament – anchored interiorly
Underlies sex drive Uterosacral ligaments – anchored posteriorly
Causes secondary sex characteristics
Deepening of voice Regions of the Uterus
Increased hair growth Body – main portion
Enlargement of skeletal muscles Fundus – area where uterine tube enters
Thickening of bones Cervix – narrow outlet that protrudes into the vagina
Regulation of Male Androgens (Sex Hormones) Walls of the Uterus
FSH – sperm production Endometrium
LH – testosterone production Inner layer
Allows for implantation of a fertilized egg
Female Reproductive System Sloughs off if no pregnancy occurs (menses)
Ovaries Myometrium – middle layer of smooth muscle
Duct System Serous layer – outer visceral peritoneum
Uterine tubes (fallopian tubes)
Uterus Vagina
Vagina Extends from cervix to exterior of body
External genitalia Behind bladder and in front of rectum
Serves as the birth canal
Ovaries Receives the penis during sexual intercourse
Composed of ovarian follicles (sac-like structures) Hymen – partially closes the vagina until it is ruptured
Oocyte
Follicular cells External Genitalia (Vulva)
Mons pubis
Support for Ovaries Fatty area overlying the pubic symphysis
Suspensory ligaments – secure ovary to lateral walls of Covered with pubic hair after puberty
the pelvis Labia – skin folds
Ovarian ligaments – attach to uterus Labia majora
Labia minora
Vestibule
Enclosed by labia majora
Contains opening of the urethra and the greater
vestibular glands (produce mucus)
Clitoris
Contains erectile tissue
Corresponds to the male penis
Perineum – diamond
Oogenesis
The total supply of eggs are present at birth
Ability to release eggs begins at puberty
Reproductive ability ends at menopause
Oocytes are matured in developing ovarian follicles
Primary oocytes are inactive until puberty
Follicle stimulating hormone (FSH) causes some primary
follicles to mature
Meiosis starts inside maturing follicle
o Produces a secondary oocyte and the first polar
body
Meiosis is completed after ovulation only if sperm
penetrates
o Two additional polar bodies are produced
Menstrual (Uterine) Cycle
Cyclic changes of the endometrium
Regulated by cyclic production of estrogens and
progesterone Hormone Production by the Ovaries
Menses – functional layer of the endometrium is Estrogens
sloughed Produced by follicle cells
Proliferative stage – regeneration of functional layer Cause secondary sex characteristics
Secretory stage – endometrium increases in size and Enlargement of accessory organs
readies for implantation Development of breasts
Appearance of pubic hair
Increase in fat beneath the skin
Widening and lightening of the pelvis
Onset of menses
Progesterone
Produced by the corpus luteum
Production continues until LH diminishes in the
blood
Helps maintain pregnancy
Mammary Glands
Present in both sexes, but only function in females
Hormonal Control of the Ovarian and Uterine Cycles
Modified sweat glands
Function is to produce milk
Stimulated by sex hormones (mostly estrogens) to
increase in size
Anatomy of Mammary Glands
Areola – central pigmented area
Nipple – protruding central area of areola
Lobes – internal structures that radiate around nipple
Alveolar glands – clusters of milk producing glands
within lobules
Lactiferous ducts – connect alveolar glands to nipple
Stages of Pregnancy and Development
Fertilization
Embryonic development
Fetal development
Childbirth
Fertilization
The oocyte is viable for 12 to 24 hours after ovulation
Sperm are viable for 12 to 48 hours after ejaculation
Sperm cells must make their way to the uterine tube for
fertilization to be possible
Mechanisms of Fertilization
Membrane receptors on an oocyte pulls in the head of the
first sperm cell to make contact
The membrane of the oocyte does not permit a second
sperm head to enter
The oocyte then undergoes its second meiotic division
Fertilization occurs when the genetic material of a sperm
combines with that of an oocyte to form a zygote
The Zygote
First cell of a new individual
The result of the fusion of DNA from sperm and egg
The zygote begins rapid mitotic cell divisions
The zygote stage is in the uterine tube, moving toward the
uterus
The Embryo
Developmental stage from the start of cleavage until the
ninth week
The embryo first undergoes division without growth
The embryo enters the uterus at the 16-cell state
The embryo floats free in the uterus temporarily
Uterine secretions are used for nourishment
The Blastocyst
Ball-like circle of cells
Begins at about the 100 cell stage
Secretes human chorionic gonadotropin (hCG) to produce
the corpus luteum to continue producing hormones
Functional areas of the blastocyst
Trophoblast – large fluid-filled sphere
Inner cell mass
Primary germ layers are eventually formed
Ectoderm – outside layer
Mesoderm – middle layer
Endoderm – inside layer
The late blastocyst implants in the wall of the uterus (by
day 14)
You might also like
- Reproductive System ModuleDocument17 pagesReproductive System ModulePATRICIA KAYE RIONo ratings yet
- File 0441Document149 pagesFile 0441Kellie ManganNo ratings yet
- Reproductive SystemDocument5 pagesReproductive SystemkhakimagdalenaNo ratings yet
- Cmca 1Document5 pagesCmca 1Erika Mae Sta. MariaNo ratings yet
- MATERNAL-AND-CHILD-NURSING Notes For BoardsDocument10 pagesMATERNAL-AND-CHILD-NURSING Notes For BoardsJill Margarett BongatoNo ratings yet
- BIO 282 Male Reproductive SystemDocument46 pagesBIO 282 Male Reproductive SystemLira Pagara100% (1)
- The Reproductive System: Alyssa Ashley R. DiegoDocument46 pagesThe Reproductive System: Alyssa Ashley R. DiegoteacherashleyNo ratings yet
- Y11 Hum - Rep1 20 3 17Document8 pagesY11 Hum - Rep1 20 3 17Rabia RafiqueNo ratings yet
- Human ReproductionDocument41 pagesHuman ReproductionMmabatho VilakaziNo ratings yet
- Physics Class 10 ICSEDocument5 pagesPhysics Class 10 ICSEmohammedumar7864521No ratings yet
- The Reproductive SystemDocument68 pagesThe Reproductive SystemStef FieNo ratings yet
- Female and Male Reproductive OrgansDocument2 pagesFemale and Male Reproductive OrgansPink EaintNo ratings yet
- Reproductive SystemDocument7 pagesReproductive SystemAngelica JovenNo ratings yet
- Lecture Notes Introduction To Reproductive SystemDocument8 pagesLecture Notes Introduction To Reproductive SystemKirstie Goc-ongNo ratings yet
- Reproductive System Notes - 2014-15 DraftDocument62 pagesReproductive System Notes - 2014-15 DraftMiguel MenendezNo ratings yet
- (Week 17) Reproductive SystemDocument3 pages(Week 17) Reproductive SystemDiana Leen Dela CruzNo ratings yet
- Science 10 Reviewer 3RDDocument12 pagesScience 10 Reviewer 3RDaltheaburgas9No ratings yet
- Sexual Reproduction: Male Reproductive SystemDocument10 pagesSexual Reproduction: Male Reproductive SystemcyprianNo ratings yet
- SXSXDocument27 pagesSXSXJoevany E. BigorniaNo ratings yet
- Male Reproductive SystemDocument71 pagesMale Reproductive Systemאילן גרינולדNo ratings yet
- Topic 17: ReproductionDocument29 pagesTopic 17: ReproductionEva SidhaniNo ratings yet
- The Reproductive SystemDocument9 pagesThe Reproductive SystemRichard Castada Guanzon Jr.No ratings yet
- 19 Reproductive SystemDocument6 pages19 Reproductive SystemEugene HerreraNo ratings yet
- Reproductive SystemDocument11 pagesReproductive SystemCHESKA LYKA ASILONo ratings yet
- Human ReproductionDocument19 pagesHuman ReproductionSantosh JoshiNo ratings yet
- Reproduction NotesDocument2 pagesReproduction NotesNerminNo ratings yet
- Reproductive SystemDocument75 pagesReproductive SystemErnie SyarinaNo ratings yet
- Reproductive System ReproductionDocument9 pagesReproductive System ReproductionDaBestMusicNo ratings yet
- Biology 12 Worksheet Male Reproductive SystemDocument4 pagesBiology 12 Worksheet Male Reproductive SystemMJ VergaraNo ratings yet
- Human Male and Female Reproductive System (Reviewer)Document8 pagesHuman Male and Female Reproductive System (Reviewer)Justine Yuan DoradoNo ratings yet
- Reproductive System - Male and FemaleDocument27 pagesReproductive System - Male and FemaleJerome CameroNo ratings yet
- 2 The Reproductive SystemDocument122 pages2 The Reproductive SystemBryan Lloyd Ballestar RayatNo ratings yet
- Science Reviewer 3RD QuarterDocument13 pagesScience Reviewer 3RD QuarterKurt John DecenaNo ratings yet
- Kuliah Sem4 2008-2Document16 pagesKuliah Sem4 2008-2cathencloxNo ratings yet
- Science 5 DLP 1 Human Reproductive SystemDocument12 pagesScience 5 DLP 1 Human Reproductive SystemDyaan TrajicoNo ratings yet
- PSGUNP279020221123075249578Unit 2 - Lesson 3 - Human Reproductive System - OrgansDocument11 pagesPSGUNP279020221123075249578Unit 2 - Lesson 3 - Human Reproductive System - OrgansAshneel ChakravortyNo ratings yet
- Male Reproductive System Female Reproductive SystemDocument1 pageMale Reproductive System Female Reproductive SystemEunimae VillanuevaNo ratings yet
- Week 2 Supplementary Activity 1 - Parts and Function Reproductive SystemDocument4 pagesWeek 2 Supplementary Activity 1 - Parts and Function Reproductive SystemBernadette Vidon-PangilinanNo ratings yet
- G.R. Pitts, J.R. Schiller, and James F. Thompson, PH.DDocument91 pagesG.R. Pitts, J.R. Schiller, and James F. Thompson, PH.DrerenNo ratings yet
- Reproduction in Humans: SMPK 6 PenaburDocument24 pagesReproduction in Humans: SMPK 6 PenaburOKTAVIANI HAPSARINo ratings yet
- Reproductive SystemDocument5 pagesReproductive Systemmuli.michaelNo ratings yet
- MCN LEC (Prelims)Document19 pagesMCN LEC (Prelims)BIANCA ANGELICA GERARDONo ratings yet
- Human Reproductive SystemDocument26 pagesHuman Reproductive SystemAlmario DacalcapNo ratings yet
- 07 05 Reproductive SystemDocument6 pages07 05 Reproductive SystemOkoye ClappinNo ratings yet
- S10 Q3 WEEK1 Reproductive System LECTUREDocument35 pagesS10 Q3 WEEK1 Reproductive System LECTUREREGLOS, Marie Nhelle K.No ratings yet
- Group3 ReproductivesystemDocument19 pagesGroup3 ReproductivesystemLeonie OngNo ratings yet
- The Reproductive SystemDocument42 pagesThe Reproductive SystemAries BautistaNo ratings yet
- Male Reproductive SystemDocument13 pagesMale Reproductive SystemMono CerosNo ratings yet
- Reproductive System Power Point AckroydDocument19 pagesReproductive System Power Point AckroydTrung Ngô Lê BảoNo ratings yet
- 4 Male and Female Reproductive Organs PPTDocument71 pages4 Male and Female Reproductive Organs PPTDanica Marie Sibay100% (2)
- Presentation 2Document21 pagesPresentation 2ericasinamagNo ratings yet
- The Male Reproductive SystemDocument10 pagesThe Male Reproductive SystemJrp AneworNo ratings yet
- Summary QuestionDocument4 pagesSummary QuestionwagkangtangaNo ratings yet
- Male Reproductive System:: Summary QuestionDocument4 pagesMale Reproductive System:: Summary QuestionwagkangtangaNo ratings yet
- Reproductive SystemDocument8 pagesReproductive SystemaynNo ratings yet
- Male and Female Reproductive OrganDocument4 pagesMale and Female Reproductive OrganLawren Ira LanonNo ratings yet
- G.R. Pitts, J.R. Schiller, and James F. Thompson, PH.DDocument92 pagesG.R. Pitts, J.R. Schiller, and James F. Thompson, PH.DJonalynCollodChewacheoNo ratings yet
- 4 Male and Female Reproductive Organs PPTDocument71 pages4 Male and Female Reproductive Organs PPTDanica Marie Sibay100% (1)
- Testes OvariesDocument7 pagesTestes OvariesLoraine Joy RomeroNo ratings yet
- Ana EndoDocument2 pagesAna EndoFIONA DANE MAURERANo ratings yet
- Ana CardioDocument3 pagesAna CardioFIONA DANE MAURERANo ratings yet
- Ana DigesDocument3 pagesAna DigesFIONA DANE MAURERANo ratings yet
- Ana BloodDocument2 pagesAna BloodFIONA DANE MAURERANo ratings yet
- Lab ParticularsDocument57 pagesLab ParticularssaranyaNo ratings yet
- Resource UnitDocument5 pagesResource UnitRyan Robert V. VentoleroNo ratings yet
- Maternal and Child Health MCQ Quiz Questions and Answers - ProProfs QuizDocument5 pagesMaternal and Child Health MCQ Quiz Questions and Answers - ProProfs QuizMuhammad AliNo ratings yet
- Brand Plan For Dienogest by Saqib AltafDocument13 pagesBrand Plan For Dienogest by Saqib AltafSakib ZabooNo ratings yet
- Obstetrics Case StudiesDocument5 pagesObstetrics Case StudiesDiane AlvaradoNo ratings yet
- University of Cambridge International Examinations International General Certificate of Secondary EducationDocument20 pagesUniversity of Cambridge International Examinations International General Certificate of Secondary EducationAli AshrafNo ratings yet
- Group 2: Abdulmalik, Arroyo, Cader, Dapanas, Langilao, Mejia, Madelo, Obinay, Sabac, TomambilingDocument37 pagesGroup 2: Abdulmalik, Arroyo, Cader, Dapanas, Langilao, Mejia, Madelo, Obinay, Sabac, TomambilingEvelyn MedinaNo ratings yet
- Accoppiamenti D&D 5eDocument34 pagesAccoppiamenti D&D 5eErnangelo CarracchiaNo ratings yet
- Fetal Brain Ultrasound Image Classification Using Deep LearningDocument5 pagesFetal Brain Ultrasound Image Classification Using Deep LearningInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Gee2 ActivitiesDocument7 pagesGee2 ActivitiesNiña Edrienne JuntillaNo ratings yet
- Astraia Manual 1.26 EnglishDocument264 pagesAstraia Manual 1.26 Englishمسلم البرغوثيNo ratings yet
- New England Journal Medicine: The ofDocument10 pagesNew England Journal Medicine: The ofSuwandi ChangNo ratings yet
- Gestational Diabetes MellitusDocument3 pagesGestational Diabetes MellitusJustine DumaguinNo ratings yet
- Endometriosis and Adenomycosis - CaramelMacchiatoDocument6 pagesEndometriosis and Adenomycosis - CaramelMacchiatoJanelle MatamorosaNo ratings yet
- MiscarriageDocument38 pagesMiscarriagezianab aliNo ratings yet
- Serum IGF-1 and IGFBP-3 Levels in Healthy Children Between 0 and 6 Years of AgeDocument6 pagesSerum IGF-1 and IGFBP-3 Levels in Healthy Children Between 0 and 6 Years of Ageyulia fatma nstNo ratings yet
- Cardiovascular Complications of Down Syndrome Scoping Review and Expert Consensus PDFDocument17 pagesCardiovascular Complications of Down Syndrome Scoping Review and Expert Consensus PDFDaniela Peinado RiosNo ratings yet
- Antenatal and Postnatal PPT PDFDocument15 pagesAntenatal and Postnatal PPT PDFNikita -0251 ENo ratings yet
- Deepika.R:::: Patient Age / Sex 26 Y / Female BranchDocument2 pagesDeepika.R:::: Patient Age / Sex 26 Y / Female BranchkannanNo ratings yet
- Jurnal Profesi Medika: Jurnal Kedokteran Dan ISSN 0216-3438 (Print) - ISSN 2621-1122 (Online) KesehatanDocument8 pagesJurnal Profesi Medika: Jurnal Kedokteran Dan ISSN 0216-3438 (Print) - ISSN 2621-1122 (Online) KesehatanNasriNo ratings yet
- Population and Related IssuesDocument57 pagesPopulation and Related IssuesFrancis Hassel Pedido100% (3)
- Tragic Romance DramaDocument1 pageTragic Romance Dramakristine camachoNo ratings yet
- FSRH Guideline Intrauterine Contraception Sep 2019Document59 pagesFSRH Guideline Intrauterine Contraception Sep 2019aarfeen shumailNo ratings yet
- Adolescent Reproductive HealthDocument2 pagesAdolescent Reproductive HealthLabista SmithNo ratings yet
- Physiologic Changes of The Postpartal PeriodDocument13 pagesPhysiologic Changes of The Postpartal PeriodKrishna Faith P. DelaraNo ratings yet
- Editorial: Breastmilk: It's Not Just For Breakfast Anymore!Document1 pageEditorial: Breastmilk: It's Not Just For Breakfast Anymore!lila bNo ratings yet
- Case # 1 Our Lady of Lourdes Hospital, Petitioner Spouses Romeo and Regina Capanzana, RespondentsDocument2 pagesCase # 1 Our Lady of Lourdes Hospital, Petitioner Spouses Romeo and Regina Capanzana, RespondentsjohnricNo ratings yet
- Proceeding 4th Aceh Surgery UpdateDocument83 pagesProceeding 4th Aceh Surgery UpdateUNS KAMERA BELAKANGNo ratings yet
- Call For Legalization of Surrogacy6188 PDFDocument18 pagesCall For Legalization of Surrogacy6188 PDFsamiaNo ratings yet
- Respiratory Physiology & NeurobiologyDocument14 pagesRespiratory Physiology & NeurobiologyRaul DoctoNo ratings yet