Professional Documents
Culture Documents
HEMATOLOGY
Uploaded by
MA. ANDREA NICOLE BITOINOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
HEMATOLOGY
Uploaded by
MA. ANDREA NICOLE BITOINCopyright:
Available Formats
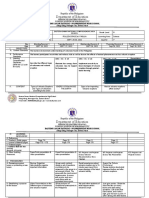
WEEK 8: HEMOGLOBIN METABOLISM
HEMOGLOBIN
→ is one of the most studied proteins in the body
because of the ability to easily isolate it from red
blood cells (RBCs).
→ 95% of cytoplasmic content of RBCs
→ When released into the plasma, it is rapidly
salvaged to preserve its iron and amino acid
components; when salvage capacity is exceeded, it
is excreted by the kidneys GLOBIN BIOSYNTHESIS
→ Concentration: 34 g/dL (normal MCHC) → Six structural genes code for the six globin chains ;
→ Molecular weight: 64,000 Daltons are on the short arms of chromosomes
FUNCTIONS: o Chromosome 16 – alpha and zeta
○ Transport oxygen to the tissues and carbon o Chromosome 11 – beta, delta, gamma, and
dioxide from the tissues to the lungs epsilon
○ Contributes to acid-base balance by binding → Production of globin chains takes place in the
and releasing hydrogen ions (Bohr effect) nucleus and ribosomes of erythroid precursors from
○ Transports nitric oxide → relaxation of the pronormoblast through the circulating
vascular wall smooth muscle and vasodilation polychromatic erythrocyte (reticulocyte), but not in
HEMOGLOBIN STRUCTURE mature erythrocytes
→ Spherical, has four heme groups attached to four → Transcription of the globin genes to messenger
polypeptide chains, and may carry up to four ribonucleic acid (mRNA) occurs in the nucleus, and
molecules of oxygen translation of mRNA to the globin polypeptide chain
→ Conjugated globular protein (TETRAMER) occurs on ribosomes in the cytoplasm
consisting of: → Although transcription of a-globin genes produces
o Globin → two different pairs of polypeptide more mRNA than the b-globin gene, there is less
chains (4 globin chains) efficient translation of the a-globin mRNA;
o Heme → four heme groups, with one heme Therefore, a and b chains are produced in
group imbedded in each of the four approximately equal amounts
polypeptide chains
o 2,3-diphosphoglycerate (2,3-DPG) → After translation is complete, chains are released
- Produced in the anaerobic glycolytic pathway
from the ribosomes in the cytoplasm
(Luebering-Rapoport pathway) HEME STRUCTURE
- Bonded in the center of beta chains
- Inversely related to the hemoglobin-oxygen → Also called as Ferroprotoporphyrin IX
affinity
→ Heme consists of:
o Protoporphyrin IX - ring of carbon,
hydrogen, and nitrogen atom
o Central atom of divalent ferrous iron
(Fe2+) ; reduced iron
→ Each of the four heme groups is positioned
in a pocket of the polypeptide chain near
GLOBIN STRUCTURE the surface ofthe hemoglobin molecule
→ The ferrous iron in each heme molecule
→ The four globin chains comprising each reversibly combines with one oxygen
hemoglobin molecule consist of two identical pairs molecule
of unlike polypeptide chains (Ex. HgbA1🡪 2 alpha → When the ferrous irons are oxidized to the
and 2 beta globin chains) ferric state (Fe 3+), they no longer can bind
→ Variations in amino acid sequences give rise to oxygen( methemoglobin)
different types of polypeptide chains
→ Each chain is designated by a Greek letter HEME BIOSYNTHESIS
→ Heme biosynthesis occurs in the
mitochondria and cytoplasm of bone
marrow erythroid precursors, beginning 4. Hydroxymethylbilane
with the pronormoblast through the
circulating polychromatic erythrocyte 5. Uroporphyrinogen III
(reticulocyte
6. Coproporphyrinogen IIII
→ As they lose their ribosomes and
mitochondria, mature erythrocytes can no 7. Protoporphyrinogen IX
longer make hemoglobin
→ Porphyrias - disorders in the heme 8. Protoporphyrinogen IX
biosynthesis pathway
9. Heme
IMPORTANT NOTES:
⮚ Transferrin, a plasma protein, carries iron in the HEMOGLOBIN ASSEMBLY
ferric (Fe3+) form to developing erythroid cells
→ After their release from ribosomes, each globin
⮚ Transferrin binds to transferrin receptors on
chain binds to a heme molecule, then forms a
erythroid precursor cell membranes and the
heterodimer
receptors and transferrin (with bound iron) are
brought into the cell in an endosome → Two heterodimers then combine to form a
tetramer; this completes the hemoglobin molecule
⮚ Acidification of the endosome releases iron from
transferrin → In the native configuration of the hemoglobin
molecule, the four hemes and four polypeptide
⮚ Iron is transported out of the endosome and into
chains are assembled in a very specific spatial
the mitochondria, where it is reduced to the
configuration
ferrous state and is united with protoporphyrin IX
to make heme → Each of the four chains in the molecule coils into
eight helices, forming an egg-shaped molecule
⮚ Heme leaves the mitochondria and is joined to the
with a central cavity
globin chains in the cytoplasm
→ In the process of the binding of the first heme
group to a molecule of oxygen, a change in the
overall configuration of the hemoglobin molecule
occurs
→ This altered configuration of the molecule favors
the additional binding of oxygen to the remaining
heme groups, if sufficient oxygen pressure is
present
Heme Biosynthesis Pathway
1. Succinyl coA + Glycine COMPLETE HEMOGLOBIN MOLECULE
The hemoglobin molecule can be described by its
2. Delta Aminolevunilic Acid (D-ALA)
primary, secondary, tertiary, and quaternary protein
3. Porphobilinogen structures
Primary refers to the amino acid sequence o Are used for fractionation, presumptive
of the polypeptide chains identification, quantification of normal
hemoglobin and hemoglobin variants
Secondary refers to chain arrangements in
helices and non-helices
HEMOGLOBIN OXYGEN DISSOCIATION
CURVE
Tertiary refers to the arrangement of the → The function of hemoglobin is to readily bind
helices into a pretzel-like oxygen molecules in the lungs
configuration o High oxygen affinity to transport
Quaternary also called a tetramer, describes oxygen
the complete hemoglobin o Low oxygen affinity to efficiently
molecule unload oxygen to the tissues
→ During oxygenation, each of the four heme iron
Hb A, is composed of two a- atoms in a hemoglobin molecule can reversibly
globin chains and two b-globin bind one oxygen molecule
chains.; strong a a1-b1 and a2-b2 → Approximately 1.34 mL of oxygen is bound by
bonds hold the dimers in a stable each gram of hemoglobin (3.47 mg of iron)
form → The affinity of hemoglobin for oxygen relates to
the partial pressure of oxygen (PO2), often
The ai-b2 and a2-b1 bonds are defined in terms of the amount of oxygen needed
important for the stability of the to saturate 50% of hemoglobin, called P50 value
quaternary structure in the NORMAL VALUE 27 mm/Hg
oxygenated and deoxygenated
forms SHIFT TO THE <27 mm/Hg
LEFT
NORMAL HEMOGLOBINS SHIFT TO THE >27 mm/Hg
RIGHT
HEMOGLOB MOLECUL STAGE OF NEWB ADULT
IN AR LIFE ORN (%) → The relationship is described by the oxygen
STRUCTUR (%) dissociation curve of hemoglobin, which plots the
E
percent oxygen saturation of hemoglobin versus
PORTLAND 2 zeta; 2 Embryonic 0% 0% the PO2
gamma
→ The curve is sigmoidal, which indicates low
Gower I 2 zeta; 2 Embryonic 0% 0% hemoglobin affinity for oxygen at low oxygen
epsilon tension and high affinity for oxygen at high
GOWER II 2 alpha; 2 Embryonic 0% 0% oxygen tension
epsilon
SHIFT TO THE LEFT SHIFT TO THE
Fetal 2 alpha; 2 Newborn; 60- 1-2%
gamma adult 90% RIGHT
A1 2 alpha; 2 Newborn; 10- >95% Increased oxygen Decreased oxygen
beta Adult 40%
affinity to hemoglobin affinity to hemoglobin
A2 2 alpha; 2 Newborn; <0.5% 3.5%
delta Adult OXYGEN IS NOT OXYGEN IS
DELIVERED TO THE DELIVERED TO THE
● Embryonic hemoglobin – present up to the 3 rd TISSUES TISSUES
month of fetal life
● Fetal hemoglobin – predominant during second
and third trimester of fetal life and at birth (up to
6 month)
● Adult hemoglobin (HgbA1) – predominant by 6
months of age until adulthood with small amounts
of HgbA2
● Hemoglobin variants – genetic abnormalities in
the hemoglobin molecule (350 hemoglobin
variants)
● Hemoglobin electrophoresis and HPLC
FACTORS AFFECTING THE HGB-O2 → Abnormal hemoglobin variants - causes left
DISSOCIATION CURVE shift
→ 2, 3-DPG
→ Body Temperature
→ Blood pH - Bohr effect
→ Carbon dioxide - Haldane effect
→ Fetal hemoglobin - Causes left shift
FACTORS SHIFT TO THE LEFT (Low except SHIFT TO THE RIGHT
AFFECTING pH) (Rise except pH)
PH INCREASED (BASIC) DECREASED (ACIDIC)
Temperature Decreased Increased
Carbon dioxide Decreased (tissues) Increased (Lungs)
2,3-DPG Decreased Increased
→ Lowered Body temperature → High Body temperature
→ Alkalosis → Acidosis
ASSOCIATED
→ Blood transfusions → Conditions that produce
CONDITIONS
→ Increased carboxyhemoglobin → hypoxia (high altitude,
→ Methemoglobinemia pulmonary insufficiency,
→ Presence of Hgb F congestive heart failure,
severe anemia)
→ Some Hb variants with high affinity
→ Some Hb variants with low
for oxygen
affinity for oxygen
THE ROLE OF 2,3-DPG
DYSHEMOGLOBINS
→ OXYHEMOGLOBIN
○ Oxygenated or Relaxed state → Dysfunctional hemoglobin that are unable to
- As hemoglobin binds oxygen molecules, change transport oxygen
in conformation of the hemoglobin tetramer occurs → Form and may accumulate to toxic levels, after
with a change in hydrophobic interactions at the
a1b1 contact point, a disruption of the salt bridges, exposure to certain drugs or environmental
and release of 2,3 -BPG chemicals or gasses., the offending agent modifies
- A 15-degree rotation of the a1b1 dimer, relative to the structure of the hemoglobin molecule,
the a2b2 dimer, occurs along the a1b2 contact preventing it from binding oxygen
point → EXAMPLES:
- OXYGEN IS NOT RELEASED TO THE
TISSUES - METHEMOGLOBIN
- SULFHEMOGLOBIN
→ DEOXYHEMOGLOBIN
Deoxygenated or Tense state - CARBOXYHEMOGLOBIN
- Binding of 2,3-BPG between the beta-globin METHEMOGLOBIN (MetHb) or Hi
chains; the formation of salt bridges between
the phosphates of 2,3-BPG and positively → Is formed by the reversible oxidation of heme
charged groups on the globin chains further iron to the ferric state (Fe3+)
stabilizes the tetramer in the T conformation → A small amount of methemoglobin is
- The binding of 2,3-BPG shifts the oxygen continuously formed by oxidation of iron during
dissociation curve to the right, OXYGEN IS normal oxygenation and deoxygenation of
RELEASED TO THE TISSUES hemoglobin (1% of total hemoglobin)
→ COLOR OF BLOOD:CHOCOLATE BROWN
→ Cannot carry oxygen because oxidized ferric
iron cannot bind it; an increase in
methemoglobin level results in decreased
delivery of oxygen to the tissues
→ TOXIC LEVELS:
o <25% - asymptomatic → Ineffective for oxygen transport, and patients with
o >30% - cyanosis and symptoms of elevated levels present with cyanosis
hypoxia → Cannot be converted to normal Hb A; it persists for
o >50% - coma or death the life of the cell
→ is assayed by spectral absorption analysis → Treatment consists of prevention by avoidance of
instruments such as the CO-oximeter (absorption the offending agent
peak/wavelength at 630 nm)
CARBOXYHEMOGLOBINS (HgBCO)
METHEMOGLOBIN (Hi)
→ Results from the combination of carbon monoxide
→ METHEMOGLOBINEMIA (CO) with heme iron
o Increased in methemoglobin ; can be acquired or → Carbon monoxide has 210-240 times more affinity
hereditary for hemoglobin com
o Acquired → CO shifts the hemoglobin-oxygen dissociation
▪ Aka toxic methemoglobinemia ; occurs in curve to the left (shift to the left) further increasing
normal individuals after exposure to its affinity and severely impairing release of oxygen
anexogenous oxidant, such as nitrites, to the tissues
primaquine, dapsone, or benzocaine → Some carboxyhemoglobin is produced
▪ Treatment - removal of offending oxidant ; endogenously, but it normally comprises less than
>30% is treated with methylene blue or 2% of total hemoglobin
exchange transfusion → Has been termed the silent killer because it is an
o Hereditary odorless and colorless gas, and victims may quickly
o Mutations in the gene (CYB5R3) required become hypoxic
for NADH-cytochrome b5 reductase 3 → May be detected by spectral absorption instruments
▪ Autosomal dominant at 540 nm
▪ Hemoglobin is called as Hemoglobin M → COLOR OF BLOOD: CHERRY RED
30-50% of total hemoglobin → TOXIC LEVELS
▪ No effective treatment o 20-30% - headache, dizziness,
o Cytochrome b5 reductase deficiency disorientation
▪ Autosomal recessive o >40% - coma, seizure, hypotension, cardiac
▪ <50% of total hemoglobin arrhythmias, pulmonary edema, and death
→ CAUSES:
SULFHEMOGLOBIN (HgbS)
o Exhaust of automobiles
→ Formed by the addition of a sulfur atom to the o Tobacco smoke – in smokers,
pyrrole ring of heme; In vitro and in the presence of carboxyhemoglobin levels may be as high
oxygen, hemoglobin reacts with hydrogen sulfide as 15% (higher hematocrit and
→ Produces an IRREVERSIBLE CHANGE in the polycythemia to compensate for hypoxia)
polypeptide chains of the hemoglobin molecule due o Industrial pollutants (coal, coal gas,
to oxidant stress, and further change can result in charcoal burning)
denaturation and the precipitation of hemoglobin as → Diagnosis of carbon monoxide poisoning is made if
Heinz bodies the level is >3% in nonsmokers and >10% in
→ Can combine with carbon monoxide to form smokers
carboxysulfhemoglobin → Treatment:
→ Sulfhemoglobin has a similar peak (630 nm) to o Removing the carbon monoxide source and
methemoglobin on a spectral absorption administration of 100% oxygen
instrument ; cannot be converted to o Use of hyperbaric oxygen therapy is
cyanmethemoglobin controversial; it is primarily used to prevent
→ COLOR OF BLOOD: GREENISH PIGMENT neurologic and cognitive impairment after
(MAUVE-LAVENDER in sulfhemoglobinemia) acute carbon monoxide exposure in patients
→ CAUSES whose level exceeds 25%
- Drugs (such as sulfanilamides, phenacetin,
nitrites, and phenylhydrazine)
- Exposure to sulfur chemicals in industrial or
environmental settings
Patients with severe constipation, in cases of
bacteremia due to Clostridium perfringens and
Clostridium welchii, and in a condition known
enterogenous cyanosis
You might also like
- Abnormal Psychology (Chapter 2)Document8 pagesAbnormal Psychology (Chapter 2)Mavy QueenNo ratings yet
- Trans Savi Oto Lec 01 Head and Neck History and PE 1st SemesterDocument12 pagesTrans Savi Oto Lec 01 Head and Neck History and PE 1st SemesterJoherNo ratings yet
- Biochemistry Lab Module 2 Case 2 #1,2Document3 pagesBiochemistry Lab Module 2 Case 2 #1,2theodore_estradaNo ratings yet
- Anatomy and PhysiologyDocument86 pagesAnatomy and PhysiologyAshinoyaaa JaehyungkookNo ratings yet
- Neuroanatomy TractsDocument7 pagesNeuroanatomy TractsLola PNo ratings yet
- General Biology 1 DraftDocument136 pagesGeneral Biology 1 DraftReiggie Resurreccion100% (1)
- Lecture 2. Cells and TissuesDocument15 pagesLecture 2. Cells and TissuesAANo ratings yet
- II-Pharmacology of The Autonomic Autonomic Ne Nervous Rvous Sys System TEMDocument88 pagesII-Pharmacology of The Autonomic Autonomic Ne Nervous Rvous Sys System TEMks asNo ratings yet
- NeurophysiologyDocument21 pagesNeurophysiologyKeya PatelNo ratings yet
- Table On Chromosomal AbnormalitiesDocument2 pagesTable On Chromosomal AbnormalitiesJoanne Mary RomoNo ratings yet
- ChordatesDocument43 pagesChordatesafiqah fatina zahraNo ratings yet
- Occupational Therapists 06-2023Document6 pagesOccupational Therapists 06-2023PRC BaguioNo ratings yet
- Gecart ReviewerDocument22 pagesGecart ReviewerAhnNo ratings yet
- Cytology and Chemicals of LifeDocument53 pagesCytology and Chemicals of LifeIVAN HUNCHONo ratings yet
- Panoramic Radiographs: Technique & Anatomy Review: Continuing EducationDocument20 pagesPanoramic Radiographs: Technique & Anatomy Review: Continuing EducationRay AustraliaNo ratings yet
- CHAPTER 18 CARBOHYDRATES ReviewerDocument12 pagesCHAPTER 18 CARBOHYDRATES ReviewerMel MasculinoNo ratings yet
- Physiology U-1 IntroductionDocument139 pagesPhysiology U-1 Introductionsinte beyuNo ratings yet
- Presentation Part IDocument24 pagesPresentation Part IHIEL MAALIHANNo ratings yet
- Gen Bio Cell TypesDocument27 pagesGen Bio Cell TypesJonaya AmpasoNo ratings yet
- BIOENERGETICSDocument8 pagesBIOENERGETICSSarah CalventasNo ratings yet
- 1st QRTR Gr9 DLL Wk5Document6 pages1st QRTR Gr9 DLL Wk5rollen grace fabulaNo ratings yet
- Fixation ImpregnationDocument18 pagesFixation ImpregnationKarla Mae Tolelis - BurlatNo ratings yet
- Module 10 - The Nervous SystemDocument8 pagesModule 10 - The Nervous SystemAngela FelixNo ratings yet
- (HST) Lab Le 2 SamplexDocument12 pages(HST) Lab Le 2 SamplexFrances Dei100% (1)
- Chapter 4 TissuesDocument10 pagesChapter 4 TissuesAl-Shuaib Astami Son100% (1)
- Upper and LowerDocument268 pagesUpper and LowerFerjie Angelica DalandaoNo ratings yet
- Neurology 4 PDF-mergedDocument358 pagesNeurology 4 PDF-mergedAnuraag YadavNo ratings yet
- Anaphy Midterm ReviewerDocument14 pagesAnaphy Midterm ReviewerCarmela Jane SonzaNo ratings yet
- Module 3.1 - AlkanesDocument10 pagesModule 3.1 - AlkanesNigel HopeNo ratings yet
- AA GeneticsDocument81 pagesAA GeneticsMenalqueNo ratings yet
- PortfolioDocument27 pagesPortfolioNathalieNo ratings yet
- Funda Sample Test PDFDocument6 pagesFunda Sample Test PDFKyle GonzalesNo ratings yet
- Physio Lab PBLDocument4 pagesPhysio Lab PBLtheodore_estradaNo ratings yet
- Membranes Part 2 StudentDocument55 pagesMembranes Part 2 StudentBrownyNo ratings yet
- Integumentary System PPTDocument34 pagesIntegumentary System PPTInsatiable CleeNo ratings yet
- Workbook Answers PDFDocument36 pagesWorkbook Answers PDFPeriperi PeriperiNo ratings yet
- Anaphy Chap 1-12Document103 pagesAnaphy Chap 1-12Margaret Isabel LacdaoNo ratings yet
- (MT 57) PARA - Specimen CollectionDocument10 pages(MT 57) PARA - Specimen CollectionLiana JeonNo ratings yet
- Chapter 2 UNIT 1Document19 pagesChapter 2 UNIT 1Ayen LatosaNo ratings yet
- 7 MSCI ModuleDocument45 pages7 MSCI ModuleCoffee MorningsNo ratings yet
- Trigeminal NerveDocument23 pagesTrigeminal NerveLilly PaulNo ratings yet
- Visual ImpairmentDocument57 pagesVisual ImpairmentNavami KrishnaNo ratings yet
- Female Reproductive System-1Document43 pagesFemale Reproductive System-1Je Lan NieNo ratings yet
- PEDIA Review TransesDocument12 pagesPEDIA Review TransesJennie KimNo ratings yet
- Zoology 232 NotesDocument36 pagesZoology 232 NotesKevinNo ratings yet
- Animal Reproduction and DevelopmentDocument21 pagesAnimal Reproduction and DevelopmentEmerald SugotNo ratings yet
- MATLAB Practical File (Codes) by Priyanshu SinhaDocument35 pagesMATLAB Practical File (Codes) by Priyanshu SinhaPriyanshu SinhaNo ratings yet
- Module Template 9 10 1Document17 pagesModule Template 9 10 1Keesha Mae Urgelles TimogNo ratings yet
- Abpsy Lecture Chapter 1.1 - 2Document4 pagesAbpsy Lecture Chapter 1.1 - 2Tracey GoldNo ratings yet
- Macronutrients Protein and Amino AcidsDocument2 pagesMacronutrients Protein and Amino AcidsJilliary AlexandraNo ratings yet
- Cells 1Document6 pagesCells 1amethys manuelNo ratings yet
- Integumentary System Lab ExerciseDocument12 pagesIntegumentary System Lab Exercisekams sardinesNo ratings yet
- Strasinger AUBFDocument44 pagesStrasinger AUBFangela tanteoNo ratings yet
- Biology Group 2 NotesDocument116 pagesBiology Group 2 NotesAllacheruvu Venkata sai kumarNo ratings yet
- AMPARO IO PSYCH ANSWER SHEET 2023 (AutoRecovered)Document7 pagesAMPARO IO PSYCH ANSWER SHEET 2023 (AutoRecovered)Ferchie AmparoNo ratings yet
- Amparo Dev Psych Answer Sheet 2023Document21 pagesAmparo Dev Psych Answer Sheet 2023Ferchie AmparoNo ratings yet
- GENERAL PSYCHOLOGY Prelim ModuleDocument15 pagesGENERAL PSYCHOLOGY Prelim ModuleChristal Vail DalusonNo ratings yet
- Human Body Orientation, Terms and Organization: NursingDocument7 pagesHuman Body Orientation, Terms and Organization: NursingWai KikiNo ratings yet
- Unit 3 The Cellular Basis of LifeDocument41 pagesUnit 3 The Cellular Basis of LifeEbenezer AbrahamNo ratings yet
- Hemoglobin MetabolismDocument7 pagesHemoglobin MetabolismMicael MendozaNo ratings yet
- HEMATOLOGYDocument5 pagesHEMATOLOGYMA. ANDREA NICOLE BITOINNo ratings yet
- HEMATOLOGYDocument17 pagesHEMATOLOGYMA. ANDREA NICOLE BITOINNo ratings yet
- HEMATOLOGYDocument11 pagesHEMATOLOGYMA. ANDREA NICOLE BITOINNo ratings yet
- HEMATOLOGYDocument36 pagesHEMATOLOGYMA. ANDREA NICOLE BITOINNo ratings yet
- A Genetic Algorithm TutorialDocument42 pagesA Genetic Algorithm TutorialMárcio RamosNo ratings yet
- MutationDocument11 pagesMutationNewsonNo ratings yet
- Las 6 Bio2 PDFDocument10 pagesLas 6 Bio2 PDFPeanut BlobNo ratings yet
- Molecular Biophysics and BiochemistryDocument3 pagesMolecular Biophysics and BiochemistryukrikeNo ratings yet
- NIH Public Access: Author ManuscriptDocument41 pagesNIH Public Access: Author Manuscriptmarej312No ratings yet
- First and Second Week of DevelopmentDocument18 pagesFirst and Second Week of Developmentapi-249972919No ratings yet
- Dotter ManualDocument17 pagesDotter ManualVlad - Stefan BogdanNo ratings yet
- Project - 4e - TB1 - CZ JóóóóDocument127 pagesProject - 4e - TB1 - CZ JóóóóAnikó Szerencsiné Pataki75% (4)
- I. Introduction To Anatomical Terms and Organization of The Human BodyDocument94 pagesI. Introduction To Anatomical Terms and Organization of The Human BodyAradani Ongchi Frena100% (1)
- Muscular TissuesDocument46 pagesMuscular TissuesDAVE CANALETANo ratings yet
- Full Download Bailey and Scotts Diagnostic Microbiology 13th Edition Tille Test BankDocument36 pagesFull Download Bailey and Scotts Diagnostic Microbiology 13th Edition Tille Test Bankardellazusman100% (34)
- Read The Article - Then, Answer The Question That FollowDocument1 pageRead The Article - Then, Answer The Question That FollowEldrick Neil ReyesNo ratings yet
- Straight Is To Gay As Family Is To No FamilyDocument4 pagesStraight Is To Gay As Family Is To No FamilyPreesha ChoudharyNo ratings yet
- Vesicular Mole: Dr. Mohammed Abdalla Egypt, Domiat G. HospitalDocument32 pagesVesicular Mole: Dr. Mohammed Abdalla Egypt, Domiat G. HospitalPrathibha GuruguriNo ratings yet
- Biology Data: D N A V T N B, BDocument3 pagesBiology Data: D N A V T N B, Bapara_jitNo ratings yet
- David M. Buss, Joshua D. Duntley (Auth.), Todd K. Shackelford, Ranald D. Hansen (Eds.) - The Evolution of Violence-Springer-Verlag New York (2014)Document250 pagesDavid M. Buss, Joshua D. Duntley (Auth.), Todd K. Shackelford, Ranald D. Hansen (Eds.) - The Evolution of Violence-Springer-Verlag New York (2014)supernezNo ratings yet
- New Species of The Genus Curvularia. Fungal Keratitis 2020Document14 pagesNew Species of The Genus Curvularia. Fungal Keratitis 2020Anonymous argZ1ZNo ratings yet
- Rodriguez Canales2016Document22 pagesRodriguez Canales2016Triaprasetya HadiNo ratings yet
- 1 - Histology Lecture - Structure of Cell Membrane and Membranous OrganellesDocument40 pages1 - Histology Lecture - Structure of Cell Membrane and Membranous OrganellesAMIRA HELAYELNo ratings yet
- 〈64〉 PROBIOTIC TESTSDocument4 pages〈64〉 PROBIOTIC TESTSevct1989100% (1)
- Ambiguous GenitaliaDocument11 pagesAmbiguous GenitaliadragondostNo ratings yet
- Diseases of Mites and TicksDocument344 pagesDiseases of Mites and TicksMaria Eduarda Chiaria FurquimNo ratings yet
- NCERT Exemplar For Class 8 Science Chapter 9 Reproduction in AnimalsDocument11 pagesNCERT Exemplar For Class 8 Science Chapter 9 Reproduction in AnimalsVivek KumarNo ratings yet
- Test Bank For Ecology The Economy of Nature 8th Edition Rick Relyea Robert e RicklefsDocument13 pagesTest Bank For Ecology The Economy of Nature 8th Edition Rick Relyea Robert e RicklefsJohn Rigby100% (32)
- Test Bank For Principles of Life 3rd Edition HillisDocument42 pagesTest Bank For Principles of Life 3rd Edition Hillismangcornuntune6o9xNo ratings yet
- "The Evolution of The Banana, Star of The Western Fruit Bowl" by Rosie MestelDocument2 pages"The Evolution of The Banana, Star of The Western Fruit Bowl" by Rosie MestelPedroNo ratings yet
- Advances in Animal in Vitro FertilizationDocument33 pagesAdvances in Animal in Vitro FertilizationTaha TottiNo ratings yet
- 7396 26182 1 PBDocument17 pages7396 26182 1 PBdavideNo ratings yet
- Newsletter: Plant Mutation BreedingDocument3 pagesNewsletter: Plant Mutation BreedingGabbyNo ratings yet
- Profitability, Productivity, and Sustainability: Organizational Behavior and Strategic AlignmentDocument345 pagesProfitability, Productivity, and Sustainability: Organizational Behavior and Strategic Alignmentshahrooz.admkNo ratings yet