Professional Documents
Culture Documents
118 RLE Infection Control PDF
Uploaded by
claire yowsOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
118 RLE Infection Control PDF
Uploaded by
claire yowsCopyright:
Available Formats
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
implementation of the infection
control program in every HC
HISTORY
facility
− By the 1960s, HAIs (Hospital
Acquired/Based Infections) control INFECTION
efforts have been established in
− Disease or condition of the body that
scattered hospitals throughout the US
occurs when harmful germs get in the
− The number of hospitals with high control
body and grow in number
programs increased substantially in the
− Harmful germs to people include
1970s bacteria, fungi, viruses, and parasites
− High control programs were established
− As HC workers, there lies a huge
in virtually every US hospital by the early
responsibility to protect oneself, one’s
90s
family, and patients from danger
− All due to Dr Ignaz Semmelweis, a 19th
because:
century Hungarian doctor who was
a. Work environment encourages
known as the pioneer of handwashing
infection
• Discovered the wonders of the
b. Patients are susceptible to
now basic hygienic practice as a
diseases (pediatrics, elderly,
way to stop the spread of sickly)
infection in 1847 during an
c. Healthcare is always facing new
experiment in a Vienna hospital’s dangers
maternity ward
− The emergence of life-threatening COLONIZATION, INFECTION, AND DISEASE
infections (SARS) and re-emerging
diseases (e.g plague, TB) have − Colonization: describes microorganisms
highlighted the need for efficient present without host inference or
infection prevention and control in all interaction
healthcare settings and capacity − Infection: indicates host interaction with
building for HC workers so they can the organism
implement them • Example: patient colonized with
• A breach in infection control Staphylococcus aureus may have
practices facilitates transmission staphylococci on skin without any
of infection from patients to HC skin interruption/irritation
workers, other patients, and − Infectious disease: the infected host
attendants displays a decline in wellness caused by
• Important for all HC workers, the infection
patients, their family members,
friends and close contacts to INFECTION CONTROL AND PREVENTION
adhere to the infection control
Guidelines followed by HC settings are based
guidelines strictly
on the ff organizations:
• Responsibility of hospital
administrators to ensure − World Health Organization
MYLES, ELOISA, WELLA 1
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
− Centers for Disease Control and respiratory tract (nose, throat,
Prevention (publications, guidelines, and lungs)
website) • As reservoirs, all humans belong in
• Federal agency responsible for one of three groups:
monitoring endemic and ✓ Infected: have harmful
epidemic disease, germs that are making
recommending strategies to them sick; can infect others
decrease disease incidence, and ✓ Not infected: people who
developing guidelines to reduce are well, and are not being
risk to patients and HC workers used as hiding places for
− Occupational Safety and Health harmful germs
Administration (OSHA) ✓ Carriers: those who are
− Local agencies (such as DOH) carrying harmful germs
− Hospital and facility infection control living in their body but it
specialists and facility policies doesn't make them sick;
doesn’t show symptoms of
infection but can still infect
CHAIN OF INFECTION
others
− Represents how one infection is passed 3. Portal of Exit (Way Out)
on from one living being/host to another • Includes sites such as the blood,
− As long as the links of the chain are skin, and mucous membranes,
joined together, an infection may be respiratory tract, genitourinary
passed on from one to the other tract, GI tract, and transplacental
− There are 6 links involved: • Any way that harmful germs can
1. Infectious agent (The Bug) escape the reservoir where
• Microorganisms include bacteria, they’ve been living
viruses, fungi, and protozoa • Includes the nose and mouth
• Harmful germ that causes where harmful germs can live in
infection mucus droplets or saliva, GI tract
2. Reservoir (Hiding Places) where germs can live in stool or
• The place where microorganisms vomit, or skin as it allows harmful
survive, multiply, and await germs to live through direct
transfer to a susceptible host contact, through blood or passed
• Where harmful germs live, grow, from other liquids from inside the
and increase in number body
• May be a person, animal, dirt, 4. Mode of Transmission (Getting Around)
water, or other places in the • how harmful germs get around
environment from place to place
• When it is a person, reservoir areas • #1 mode of transmission is through
include blood, skin, GI tract the hands
(mouth, stomach, intestines), • May travel through:
MYLES, ELOISA, WELLA 2
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
✓ direct or indirect contact ✓ Not having proper
with body fluids from the vaccinations
infected reservoir (blood, ✓ Open cuts or skin
sputum, pus, wound fluid, breakdown
saliva, urine/stool)
✓ Droplet (large particles
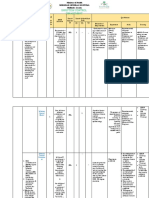
BREAKING THE CHAIN OF INFECTION
released when infected
person sneezes, talks,
- Rapid identification
laughs, or sings)
- Prompt treatment
✓ Airborne (droplets Infectious - Environmental sanitation
suspended in air) agent - Decontamination/
✓ Vehicles (blood, water, disinfection
food, etc) - Hand hygiene
✓ Vector (flies, mosquitos,
- Promotion of good health
fleas, ticks, etc)
- Proper hygiene
5. Portal of Entry (Getting In) - Environmental sanitation
• Any body opening on a person Reservoir
- decontamination/
who doesn’t have an infection disinfection
that allows harmful germs to get in
- Waste management
the body
• Germs can usually get in the same - Wear PPEs
way they get out (portals of entry - Proper hygiene
are the same with portals of exit) - Environmental sanitation
Portal of Exit - decontamination/
• Nose and mouth when the person
Disinfection
breathes in harmful germs, GI
tract when person consumes Waste management
contaminated food/drink, breaks
in skin that allow entry (open sores, - Hand hygiene at all times
cuts, needlestick) - Airflow control
6. Susceptible Host (Next Sick Person) Mode of - Proper food handling
• Person who does not have an Transmission - Isolation precaution
infection now, but is at risk for - decontamination/
disinfection
being the next person to get
infected from the harmful germs
• Body cannot fight off an infection - Aseptic technique
Portal of - Wound care
• Reasons for being unable to fight Entry - Hand hygiene
off infection include:
- Protective equipment
✓ Age
✓ Stress - Treatment of disease
Susceptible - Immunization vaccination
✓ Fatigue
Host - Adequate nutrition and
✓ Poor nutrition
✓ Chronic illness rest
MYLES, ELOISA, WELLA 3
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
Convalescence
Additional ways of breaking the chain of
infection: − Interval when acute symptoms of
infection disappear
− Washing hands frequently
− Length of recovery depends on severity
− Covering coughs and sneezes with tissue of infection and patients host resistance
− Disposing of used tissue in bin
− Recovery may take several weeks to
immediately months
− Practicing social distancing
− Using PPE appropriately
− Cleaning frequently touched surfaces HEALTHCARE ASSOCIATED INFECTIONS (HAIs)
− Patients in HC settings (hospitals and
COURSE OF INFECTION BY STAGE long-term care facilities) have an
increased risk of acquiring infections
Incubation Period − HAIs result from delivery of healthcare
− Interval between entrance of pathogen services in a HC facility
into body and appearance of first − Occurs as a result from invasive
symptoms procedures, antibiotic administration,
− Ex: for chicken pox: 14-16 days after presence of multi-drug resistant
exposure; common colds: 1-2 days after organisms (MDROs), and breaks in
exposure infection prevention and control
Prodromal Stage activities
− Number of HC employees having direct
− Interval from onset of nonspecific signs contact with a patient, type and number
and symptoms (such as low-grade fever of invasive procedures, therapy
or malaise) to more specific symptoms received, and length of hospitalization
− During this time microorganisms grow influence the risk of infection
and multiply − Major sites for HAIs:
− Patient may be capable of spreading • Surgical or traumatic wounds
disease to others • Urinary and respiratory tracts
− Ex: in herpes simplex, it begins with • Bloodstream
tingling and itching at the site before the − If hospital infection control team fails to
lesion appears provide the proper protocols to the HC
Illness Stage team, HC settings can become sources
of infection
− Interval when patient manifests signs and
symptoms specific to type of infection
− Ex: strep throat is manifested by sore NOSOCOMIAL INFECTION
throat, pain and swelling; mumps is
− Result from delivery of health services in
manifested by high fever, parotid and
a healthcare setting, where clients are at
salivary gland swelling
increased risk
MYLES, ELOISA, WELLA 4
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
− HAIs lead to increased HC costs, ORGANISMS OF HEALTH ASSOCIATED INFETIONS
extended hospital stay and prolonged POTENTIAL
recovery time
− Clostridioides difficile
− Most are transmitted by HC workers and
• Most common cause of HAIs
clients as a result of direct contact
− Methicillin-resistant S. aureus (MRSA)
− Infection that occurs more than 48-72
• Healthcare-associated MRSA
hours after admission and within 10 days
• Community-associated MRSA
after discharge are considered
− Vancomycin-resistant enterococcus
nosocomial
(VRE)
− Multidrug-resistant organisms (MDROs)
Clients in a healthcare setting are at risk for
acquiring or developing infections because of
the: PREVENTION OF INFECTION
− Lower resistance to infectious HAI BLOODSTREAM INFECTIONS (CLABSI)
microorganisms
− Bundle approach
− Exposure to an increased number and
1. Hand hygiene
more types of disease-causing organisms
2. Maximal barrier precaution
− Performance of invasive procedures
3. Chlorhexidine skin antisepsis
4. Optimal catheter site selection
FACTORS INFLUENCING INFECTION PREVENTION AND 5. Daily review of line necessity with
CONTROL prompt removal of unnecessary
lines
− Age - an infant has immature defenses
against infection and is incapable of
producing the necessary COMMUNITY-ACQUIRED INFECTIONS
immunoglobulins and WBCs
− Nutritional Status - directly influences − Collaborate effort of CDC, state, and
susceptibility to infection; a reduction in local public health departments
the intake of proteins and other nutrients − Methods
(carbohydrates and fat) reduces the 1. Sanitation techniques
body’s defenses against infection and 2. Regulated health practices
impairs wound healing 3. food preparation
− Stress - body responds to physical or 4. immunization program
emotional stress by the general
adaptation syndrome. BURDENS OF HCAIS
• During the alarm stage - body
metabolic rate increases as the − Need for hospitalization - extra days of
body uses energy stores confinement
− Disease Process - patients with diseases − Income loss
of the immune system are particularly at − Pain and suffering
risk for infection (Leukemia, HIV, etc.) − Disfigurement/disability
− Litigation - Malpractice
MYLES, ELOISA, WELLA 5
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
− Reputation − Staphylococcus aureus
− Death − Viruses (rotavirus)
SOURCES OF AGENTS OF HCAIS “All staff have a responsibility to reduce the risk
for healthcare associated infection.”
− Exogenous - hands, instruments,
catheters, respiratory instruments, “All staff have a responsibility to remind staff
transfusion, IV system, linen and air members of the need to perform hand hygiene
− Endogenous - oropharynx, respiratory, and educate patients and watchers.”
gastrointestinal and skin
“All staff have a responsibility to procure hand
hygiene products in CSR if supplies have run out
Contaminated surfaces increase cross- and need restocking.”
transmission
CDC estimates nearly 2 million patients in the US
Abstract: the risk of hand and glove get an infection in hospitals, 90 of these patients
contamination after contact die as a result of infection.
Resident Flora - normal bacteria; difficult to
remove with a single washing, and rarely causes
MEDICAL ASEPSIS
infection. Infection arises when there is a break
in the skin Aseptic technique refers to the practice or
Examples procedures that help reduce the risk for
infection.
− Coagulate negative staphylococcus
− Staphylococcus epidermidis 2 types: medical and surgical
− Corynebacterium and Ditheroids Basic medical aseptic techniques break the
− Propionibacterium spp. chain of infection.
− Acinbobacter spp.
− Klebsiella enterobacter group − Never store wet equipment; clean and
dry all equipment after use because this
can only encourage growth of
Transient Flora - skin contaminants, colonized organisms if not dried properly.
superficial layers of the skin, and mostly − All cleaning solutions should be prepared
associated with hospital-acquired infections. fresh, as this may affect the potency or
Acquired through contact with objects and the effectiveness of the solution.
environment, and can be easily removed by General rules:
handwashing
− Start from the highest point and work
Examples towards the lowest point.
− Work from the cleanest to the dirtiest
− Gram negative bacilli (E. coli, Klebsiella &
pseudomonas)
− Salmonella spp.
MYLES, ELOISA, WELLA 6
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
BASIC PRINCIPLES OF ENVIRONMENTAL CLEANING − Wash waste containers regularly
− Equipment used to hold waste should not
− Ensure all equipment is clean and dry
be used for any other purpose
before starting procedure
− Never use hands to compress waste into
− All cleaning solutions should be prepared
the containers
fresh
− Hold plastic bags at the top and keep
− Plan work route and when necessary,
bags from touching or brushing against
remove furniture and equipment
the body
− Wear goggles, mask, and gloves when
− Do proper hand hygiene after removing
preparing cleaning solutions when there
gloves when handling waste
is likelihood of splashing, inhalation of
noxious gas or skin irritating solutions
− Always use clean hazard-warning signs HEALTH AND SAFETY
and position at the start of the task where
− Check pictures, hangings and clocks are
they are most effective, and people will
know that cleaning is in progress. secure
− Do not climb on furniture or overreach
Remove, clean, and return to the
storage area when the task is − Never mix cleaning agents, as poisonous
gases could result
completed, and the floor is dry.
− When cleaning or using cleaning − Careful in manual handling when
moving furniture
equipment, items must be checked for
damage or wear which would impair − Work in small sections to prevent
overstretching
future use or endanger the safety of any
− When mopping a corridor, mop half first,
individual. If damaged, do not use.
Report to supervisor, label as faulty and leaving a clearly identified dry area for
patients/visitors/staff to walk on
remove from use.
− Never mix cleaning agents, as poisonous − Do not over wet the floor
− If mopping stairs, ensure area is
gases could result. Always ventilate any
area where chemicals are used. cordoned-off and warning signs are
displayed
− All equipment should be left clean, dry,
and tidy in the storage area after use. − Cover electric sockets with masking tape
− Avoid splashes of disinfectant on
Never store wet equipment.
furniture, curtains or floor
− Report any damage of surfaces to your
WATER DISPOSAL GUIDELINES supervisor
− All equipment should be left clean, dry,
− Waste should be collected daily or
and tidy in the storage area after use
frequently as needed
− Trash bag should be replaced
immediately of the same type DISINFECTION AND STERILIZATION
− A supply of fresh bags should be readily
available where waste is produced The use of both physical and chemical
processes that disrupt the internal functioning of
− Use PPE when handling waste
microorganisms by destroying cell proteins.
MYLES, ELOISA, WELLA 7
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
Disinfection Rule:
preoperative when using diathermy
preparation of as it can cause
1. Clean first before you disinfect
skin. diathermy burns.
(decontaminate)
2. Make sure you do rule #1
Phenolics 2% (Lysol)
GUIDELINES IN DISINFECTION
Sodium Hypochlorite 1% (Bleach) ANTIBAC Recommended Precautions
Use
Recommended Precautions
Use Only - Protective clothing
environmental should be worn while
disinfection, handling as it can be
Disinfection of - Should be used in well-
mycobacterial absorbed through the
material ventilated areas;
laboratory skin and cause
contaminated causes irritation of the
discard jars. respiratory irritation in
with blood and skin, eyes, and lungs if
higher concentrations
body fluids. used in poorly
- Must not be used in
ventilated areas.
equipment meeting skin
- Protective clothing
and mucous
required while handling
membranes or should
and using when
not be used on food
undiluted.
preparation surfaces.
- Do not mix with strong
acids to avoid release
of chlorine gas.
- Corrosive to metal. Virusolve
Recommended Precautions
Alcohol Use
Recommended Precautions For disinfection - Eye irritant, may cause
Use of hard non-reversible damage
surfaces, if not immediately
medical rinsed off. Avoid
Smooth metal - Flammable, toxic, to be
devices and prolonged contact, use
surface, table used in well-ventilated
instruments gloves and goggles.
top surfaces on area, avoid inhalation,
- Skin irritant, launder
which bleach use for small surface
contaminated clothing
cannot be used. only
before reuse.
In combination - Keep away from heat
- Use in a well-ventilated
with skin source, electrical
area.
emollients can equipment, flames and
be used for hot surfaces.
disinfection of - Allow it to dry
hands, completely, particularly
MYLES, ELOISA, WELLA 8
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
CATEGORIES FOR STERILIZATION, DISINFECTION, AND • Low pressure = air leak = uneven
CLEANING heating (spot dry condition)
− Quality of steam: 100% saturated steam
Items that enter the tissue or vascular and water in the system (Steam
system present a high risk of infection if separator - remove water from steam at
they are contaminated with
required velocity)
CRITICAL
microorganisms. These must be sterile.
• Decreased steam quality =
- Surgical instruments trapped air = wet packs = good
- Cardiac or intravascular catheters bacterial growth for items
- Urinary catheters Monitoring Sterilization Process
- Implants
- External indicator
Items that come in contact with mucous
- Internal indicator
membranes or non-intact skin also
present risks. These items must be free - Biologic indicator
from all microorganisms except Maintenance, Handling and Inspection
SEMI CRITICAL
bacterial spores. Semi-critical items must
be high-level disinfected or sterilized. - Low traffic area
- 30 minutes cooling
- Respiratory and anesthesia - Torn and wet packaging are considered
equipment
contaminated and should be
- Endoscopes
- Endotracheal tubes reprocessed
- GI endoscopes
- Diaphragm fitting rings
STORAGE AND SHELF-LIFE
Items that come in contact with intact
skin, but not mucous membranes must Shelf-life is event-related and depends on
be clean. These must be disinfected. quality of the packaging material, storage
NON-CRITICAL
conditions, and the conditions during transport
- Bedpans and amount of handling.
- BP cuffs & stethoscopes
- Bed rails − Sterility maintenance covers
- Linens − Close or cover cabinets
- Bedside trays and patient furniture
− Open shelving
- Food utensils
• 2” from outside walls
• 8” to 10” from floor
STERILIZATION • 18” from ceiling
• No bent, crunched, compressed
This is the basic requirement of quality patient punctures or near location that
care today. could become wet
− Protective environment
Efficacy of Autoclaving
− Design and traffic pattern: 3-Zone
− Air tightness of the sterilizer Concept
− Atmospheric pressure − Ventilation, filtered air, temperature and
humidity
MYLES, ELOISA, WELLA 9
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
• Positive pressure system Surfaces
• contaminated with
• Filter air 20 changes/hour patient specimen should be
• Temp. 18-24 degrees centigrade carefully cleaned and disinfected
• Humidity 50-55% • Sink must be scrubbed daily
• Ideally 1-degree centigrade • Walls, windows, shelves, etc.
cooler than the outer area. should be cleaned periodically
− Double gloving − Basic infection Control Personnel
− Environmental cleaning Education
− Environmental sampling
− Principles of Draping must be observed
CDC PRECAUTIONS TO PREVENT TRANSMISSION OF
in all areas
INFECTIOUS AGENTS
OPERATING ROOM/DELIVERY ROOM INFECTION
Two tiers:
PREVENTION
a. Standard precautions
Surgical Site Infection and Bundling Prevention
b. Transmission-based precautions
− Classification of Wound and Risk
Infection
• Clean < 2% Standard Precautions:
• Clean-contaminated < 10% − Which applies to all clients and patients
• Contaminated ~ 20% in all health care settings regardless of
• Dirty ~ 40% the suspected or confirmed presence of
− Bundles of Care in SSI infectious agents
• Clippers, no razors − Guidelines include:
• Prophylactic antibiotics • Consider every person as
• Normothermia potentially infectious and
• Glucose control susceptible
• Oxygen control • Handwashing as most important
procedure
NICU/NURSERY INFECTION PREVENTION • Wear gloves before touching any
wet or performing invasive
− Physical Area maintained clean procedures
− Administrative Arrangements • Use antiseptic for cleansing skin
• Staff health and mucous membranes
• Dress code • Use safe work practices
− General housekeeping − Standard precautions apply to:
• Dust should not be dispensed in • Blood
the air • All body fluids, secretions and
• Cabinets and work surfaces must excretions except sweat,
be cleaned daily regardless of whether they
• Friction cleaning contain visible blood
• Non-intact skin
MYLES, ELOISA, WELLA 10
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
• Mucous membranes • Clean reusable equipment prior
to reuse
− Environmental Cleaning
STANDARD PRECAUTION: KEY COMPONENTS
• Routinely care, clean, and
− Handwashing disinfect equipment and
• After touching blood, body fluids, furnishings in patient care areas
excretion, and contaminated • Make sure to use appropriate PPE
items − Sharps
• Immediately after removing • Should be properly dispose din
gloves punctured proof containers with
• Between patient contact antibac 1000ppm (ward) and 500
− Gloves ppm (special areas/infectious)
• For contact with blood, body • Should never use hand to pick-up
fluids, secretions, and sharps
contaminated items − Patient placement
• For contact with mucous • Place patients who contaminate
membranes and non-intact skin the environment or cannot
− Mask, goggles, face masks maintain appropriate hygiene in
• When contact with of private rooms
membranes of eyes, nose, and
mouth when contact with blood
PERSONAL PROTECTIVE EQUIPMENT
and body fluids is likely
− Gowns
• Protect skin from blood or body
fluid contact
• Prevent soil in of clothing during
procedures that may involve
contact with blood or body fluids
− Linens
• Handle in a manner that prevents
transfer of microorganisms to
others and to the environment PPE GUIDELINES AND SAFE PRACTICE
• Wear gloves if visibly − PPE is used in addition to normal uniforms.
contaminated Uniforms are not considered personal
• Placing infectious soiled linens in a protective equipment.
yellow cellophane − PPE will not protect against sharp injuries,
− Patient Care Equipment avoidance or caution in the use of sharps
• Handle soiled equipment in a
where possible.
manner to prevent contact with − PPE is identified as single use and must
skin or mucous membranes and to
not be kept for reuse.
prevent contamination of
clothing or the environment
MYLES, ELOISA, WELLA 11
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
− The need for protective equipment shall − Take gloves off carefully and do not
be task related approach, not disease touch your skin or clothes with the dirty
specific. sides of the gloves
− Selection of protective equipment − Do not touch anything with your dirty
should be selected on the basis of an gloves that anyone may touch without
assessment of the risks of transmissions of gloves, like a doorknob
microorganisms to the patient and the − The fit should be comfortable - not to
risk of contamination of health care loose or not too tight
practitioners clothing and skin by the − Important: the use of gloves does not
patient’s blood, body fluids, secretions preclude the need for hand washing
and excretions.
− PPE protects intact skin. Cuts, abrasions,
exposed fresh unhealed body piercings Respiratory hygiene/cough etiquette: Instruct
symptomatic persons and healthcare workers
must be covered with waterproof plaster
or other suitable dressing in addition to to cover their mouths and noses when
coughing or sneezing, use and dispose of
PPE.
− Keep hands away from face and never tissues, perform hand hygiene after hands have
been in contact with the respiratory secretions,
adjust PPE with contaminated gloves.
− Limit surfaces touched. Do not touch and wear surgical mask if tolerated or maintain
spatial separation, more than three feet is
environmental surfaces except as
possible.
necessary during patient care.
− Change gloves when torn or heavily
contaminated
− All hospital personnel shall wear TO HELP STOP THE SPREAD OF GERMS
enclosed footwear, preferably resistant
− Cover your mouth and nose with a tissue
to spills of hazardous substances
when you cough or sneeze
− Put your used tissue in the waste basket
RULES IN WEARING GLOVES − If you don't have a tissue, cough or
sneeze into your upper sleeve or elbow,
− Gloves should be worn once and then not your hands
thrown away − You may be asked to put on a face mask
− When you wear gloves, always work from to protect others
(or touch) a clean area before you − Wash your hands often with soap and
touch the contaminated area water for 20 seconds
− Change gloves if your hands are going
to move from a body part that is
contaminated, to a body part that is not ELEMENTS OF RESPIRATORY HYGIENE/COUGH
contaminated ETIQUETTE
− Change gloves to right away if they get
− Healthcare personnel are advised to
dirty or tear
observe droplet precautions and hand
hygiene when examining and caring for
MYLES, ELOISA, WELLA 12
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
patients with signs and symptoms of − For the droplet (green) precaution,
respiratory infection we do hand hygiene, we wear masks
− Healthcare personnel with respiratory with goggles or face shield if
infection are advised to avoid patient necessary, so that is case-to-case
contact when they are actively basis.
coughing and producing respiratory − For the airborne (blue) precaution,
secretions we wear our mask, then after, we
need to make sure that we close the
door to avoid spreading of
BLOOD AND BODY FLUID RISK ASSESSMENT
microorganisms.
A. HIGH RISK
- Blood, all body fluids
DISEASE SPECIFIC ISOLATION PRECAUTIONS
contaminated with blood,
cerebrospinal, peritoneal, a. Contact precaution
pericardial, synovial, amniotic • MRSA
fluids, breast milk, semen, vagina • VRE
secretions, and all unfixed tissues • Adenovirus
organs and parts of the body • Diarrhea
B. MINIMAL RISK • C. Difficile
- Urine, feces, saliva, sputum, tears, • Rotavirus
sweat, and vomit • E Coli 0157
• Enterovirus
• Salmonella
TRANSMISSION BASED PRECAUTION
• Shigella
a. Yellow - Contact • Hepatitis A
b. Green - Droplet • Herpes Zoster (shingles, localized)
c. Blue - Airborne • Herpes simplex, Parainfluenza
(mask if coughing)
• RSV (mask if productive cough)
• Lice
• Scabies
• Chicken pox (symptomatic, until
all lesions crusted and dried)
− For every precaution, we must first do b. Droplet precaution
the hand hygiene. • Pertussis
− For the contact precaution, after • Influenza A or B
doing the hand hygiene, we wear • MRSA (respiratory infection)
gloves and wear a gown if necessary, • Neissera meningitides (suspected
and we just do after care to all or confirmed)
equipment touched to the patient. • Coxsackle
MYLES, ELOISA, WELLA 13
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
• Bacterial meningitis (for 24 hours PRIORITY: protect self and patients from
after effective antibiotic therapy) cross contamination. Use antibac 5000
• RSV (droplet and contact) ppm and disinfectants when cleaning.
• Mumps Make sure to include aircon in deep
• Rubella cleaning.
c. Airborne precaution DISCHARGE OR TRANSFER TO REGULAR ROOM
• Chicken pox
− All equipment used to be disinfected
• Disseminated herpes zoster
with disinfectants, sprayed, and air-dried
• Measles
− BP cuffs - Return to nurses station for
• N95 mask:
cleaning
✓ TB
− You will be notified by NOD if patient is
✓ SARS
for transfer and discharge for timely
✓ Avian influenza
decontamination, cleaning, and
disinfection
ISOLATION PRECAUTION − Aircon maintenance should be notified
for them to facilitate aircon cleaning
Cases that require private room isolation:
− PTB CASES THAT REQUIRE REVERSE ISOLATION
− Mumps
− Rubella − Cancer patients who will undergo
− Chicken pox chemotherapy
− Measles − Preterm, neonates, newborn, or children
− Pertussis below 1 year old
− 2nd and 3rd degree burn patients
Strict isolation: − Leukemia, aplastic anemia, similarly
severe prolonged neutropenia
− Meningococcemia, tetanus, rabies, − All patients confined in ICU and NICU
AH1N1 or SARS, leprosy, active PTB
MANAGING PATIENTS ON REVERSE ISOLATION
ISOLATION ROOM OCCUPANCY
− All must wear mask before entering
− Soiled linens - Place inside a yellow − Wash hands
cellophane prior to dispensing to linen − Limit visitors
department − Close the door and never leave the door
− Body fluid spillage - Soak in paper towel open
or absorbent material and placed in − When leaving, remove PPE outside and
yellow trash can then spray with antibac discard in yellow trash
solution and air dry
− Use appropriate personal protective
equipment before going inside the room.
MYLES, ELOISA, WELLA 14
LECTURER: SIR DAÑOS
BSN 4 | FIRST SEM | BATCH 2022 | TOPIC: 4: INFECTION CONTROL & PREVENTION
NEEDLE STICK INJURY
− Encourage bleeding under running
water
− Do not suck blood from wound
− Thoroughly wash wound with soap and
water followed by a 70% alcohol
− Do not scrub
− Dry and apply waterproof dressing
− Report incident to the supervisor on duty
and infection control nurse
− Fill out a needle stick or sharps injury
report form
− Consult with the ICC chairperson and
work out an appropriate action in
accordance to the hospital infection
control plan on needle stick injuries
HOME-BASED CARE OF INFECTIOUS DISEASE
− Reduction of risk to patients
• Care of equipment
• Patient education
− Reduction of risk to household members
• Prevention of transmission
• Education
• Fever and comfort
− Healthcare workers should follow
standard precautions in the home setting
− Patient and family education
• Establish an environment that
facilitates hand hygiene and
aseptic technique
• Family caregivers should receive
annual influenza vaccine
• Equipment care
• Common sense cleanliness
• Food preparation and personal
hygiene
• Establishment of reasonable
barriers to protect family members
MYLES, ELOISA, WELLA 15
You might also like
- Complications in Treatment of LYMEDocument131 pagesComplications in Treatment of LYMECharles Mitchell100% (1)
- Peri - Operative Nursing: Learning Manual DescriptionDocument41 pagesPeri - Operative Nursing: Learning Manual DescriptionCezanne Cruz100% (4)
- Theaters of The BodyDocument200 pagesTheaters of The BodyRenata Schaun100% (6)
- Zang-Fu Syndrome Differentiation - UERMDocument113 pagesZang-Fu Syndrome Differentiation - UERMNathaniel P. Peralta0% (1)
- Functioning of Infection Control CommitteeDocument3 pagesFunctioning of Infection Control Committeetummalapalli venkateswara raoNo ratings yet
- Infection Control LectureDocument21 pagesInfection Control LectureJessica Medina100% (1)
- Motivating Climate PLPDocument29 pagesMotivating Climate PLPclaire yowsNo ratings yet
- QRS 4-2Document1,057 pagesQRS 4-2Sree Harsha Gunneri100% (1)
- CCN Lecture NotesDocument56 pagesCCN Lecture NotesDarwin AndalNo ratings yet
- Infection Control Guidelines CDC 2003Document108 pagesInfection Control Guidelines CDC 2003Wan NoorinaNo ratings yet
- Hospital Acquired Infections-IIDocument52 pagesHospital Acquired Infections-IIFATHIMA ANo ratings yet
- Communicable DiseasesDocument22 pagesCommunicable DiseaseskaramnNo ratings yet
- Universal Precaution by FithriDocument62 pagesUniversal Precaution by FithriFithriKurniatiNo ratings yet
- Surveillance Prevention and Control of Infection PlanDocument11 pagesSurveillance Prevention and Control of Infection Plansony kurniawanNo ratings yet
- Group 3 RESEARCH PROPOSALDocument41 pagesGroup 3 RESEARCH PROPOSALCindy Mae Macamay100% (5)
- 118 RLE Mechanical Ventilation PDFDocument5 pages118 RLE Mechanical Ventilation PDFclaire yowsNo ratings yet
- Hospital Infection Control: Cecilia S. Montalban, MD, MSCCTMDocument51 pagesHospital Infection Control: Cecilia S. Montalban, MD, MSCCTMDelantar Percivic100% (1)
- Infection Control Questions For StaffDocument3 pagesInfection Control Questions For StaffManisha maharaNo ratings yet
- Osteopathy in The Cranial FieldDocument110 pagesOsteopathy in The Cranial FieldRukaphuongNo ratings yet
- Infection and Prevention Control-2Document14 pagesInfection and Prevention Control-2NIKHIL RAJNo ratings yet
- Respiratory Medicine Curriculum in UKDocument81 pagesRespiratory Medicine Curriculum in UKfflintNo ratings yet
- Module 12: Infection Control in Health Care Settings: Image Courtesy Of: World Lung FoundationDocument37 pagesModule 12: Infection Control in Health Care Settings: Image Courtesy Of: World Lung FoundationAniruddhaNo ratings yet
- Infection Prevention and Control: DR Rahul KambleDocument61 pagesInfection Prevention and Control: DR Rahul KambleDrRahul KambleNo ratings yet
- CPG Management of Post-Operative Infectious EndophthalmitisDocument41 pagesCPG Management of Post-Operative Infectious EndophthalmitisnrajentranNo ratings yet
- Infc ContrlDocument36 pagesInfc ContrlgopscharanNo ratings yet
- Recovery High Schools in Massachusetts: A Promising, Comprehensive Model For Adolescent Substance Abuse and DependenceDocument44 pagesRecovery High Schools in Massachusetts: A Promising, Comprehensive Model For Adolescent Substance Abuse and DependenceThe Stacie Mathewson FoundationNo ratings yet
- Image Courtesy Of: World Lung FoundationDocument37 pagesImage Courtesy Of: World Lung Foundationines syadzaNo ratings yet
- Infection ControlDocument20 pagesInfection ControlNorj BaraniNo ratings yet
- What Is The Role of An Infection Control NurseDocument7 pagesWhat Is The Role of An Infection Control NurseDENNIS N. MUÑOZNo ratings yet
- Infection Control: Evangeline H, SKPDocument49 pagesInfection Control: Evangeline H, SKPEvangeline HutabaratNo ratings yet
- Outbreak Control POLICYDocument11 pagesOutbreak Control POLICYAdrian SavastitaNo ratings yet
- Concept of HealthDocument20 pagesConcept of HealthMOZAIDNo ratings yet
- Prevention and Control of InfectionsDocument21 pagesPrevention and Control of InfectionsSunil ThomasNo ratings yet
- Healthpromotlectamany 150627111718 Lva1 App6892Document56 pagesHealthpromotlectamany 150627111718 Lva1 App6892B 70 Mohit KumarNo ratings yet
- Lecture-1: University of Kufa Faculty of Nursing, Community Health Nursing BranchDocument27 pagesLecture-1: University of Kufa Faculty of Nursing, Community Health Nursing Branchآمنة محمد كاظمNo ratings yet
- Infection ControlDocument1 pageInfection Controlskmc002No ratings yet
- Annual Plan: Infection Prevention & Control DepartmentDocument3 pagesAnnual Plan: Infection Prevention & Control DepartmentSherina Edding0% (1)
- Global and Philippine Health SituationDocument6 pagesGlobal and Philippine Health SituationMonsour Salazar100% (1)
- Infection Control in NurseryDocument5 pagesInfection Control in Nurserysandeepv08No ratings yet
- Sop IsolationDocument10 pagesSop IsolationROHI SINGHNo ratings yet
- Infection ControlDocument235 pagesInfection Controldisaster6993No ratings yet
- Role of Nursing Staff in Patient Centric Care, Patient Safety and Hospital Infection ControlDocument31 pagesRole of Nursing Staff in Patient Centric Care, Patient Safety and Hospital Infection ControlVincy MacwanNo ratings yet
- Communication DiseasesDocument9 pagesCommunication DiseasesMonika MathurNo ratings yet
- Autonomy of Nurse PDFDocument8 pagesAutonomy of Nurse PDFDennis CobbNo ratings yet
- AEFI Surveillance and management-RVVDocument19 pagesAEFI Surveillance and management-RVVadi100% (1)
- Biosafety and Regulations Presentation On BioterrorismDocument32 pagesBiosafety and Regulations Presentation On BioterrorismGagan KhuranaNo ratings yet
- Nursing ProcessDocument68 pagesNursing ProcessSareno PJhēaNo ratings yet
- Developing and Implementing Training Materials For Integrated Community Case Management in South SudanDocument28 pagesDeveloping and Implementing Training Materials For Integrated Community Case Management in South Sudanmalaria_consortiumNo ratings yet
- Disaster Associated Health IssuesDocument29 pagesDisaster Associated Health Issuesmeshack mbalaNo ratings yet
- Mask19Document8 pagesMask19steven saputraNo ratings yet
- Bundle Care 2022Document10 pagesBundle Care 2022Kalla Daniel SharonNo ratings yet
- GSK Sotrovimab Fact Sheet For HCP 12222021Document34 pagesGSK Sotrovimab Fact Sheet For HCP 12222021Jillian SmithNo ratings yet
- Infections in ICUDocument7 pagesInfections in ICUNikolay ToméNo ratings yet
- Pharma Notes MidsDocument17 pagesPharma Notes MidsMa. Rita Concepcion TungulNo ratings yet
- Duties and Responsibilities of Staff Nurse - A StudyDocument7 pagesDuties and Responsibilities of Staff Nurse - A StudyIJRASETPublicationsNo ratings yet
- Dsunzh Ekè Fed F'K (KK CKKSMZ: F'K (KK Lnu) 17) Bulfvv W'Kuy (Ks K) JKMT, Osu Q) Fnyyh&110002Document8 pagesDsunzh Ekè Fed F'K (KK CKKSMZ: F'K (KK Lnu) 17) Bulfvv W'Kuy (Ks K) JKMT, Osu Q) Fnyyh&110002Tanvi Tanya100% (1)
- NCM 112 Prefinal LectureDocument10 pagesNCM 112 Prefinal LectureFatima-Ridziana AbdurahmanNo ratings yet
- 5.infection Control & Standard PrecautionsDocument33 pages5.infection Control & Standard PrecautionsGilbert JohnNo ratings yet
- Infection Control DepartmentDocument3 pagesInfection Control DepartmentSherina EddingNo ratings yet
- Total Quality ManagementDocument29 pagesTotal Quality ManagementReia Anghel100% (1)
- CHN 1 Topic 1 HandoutsDocument26 pagesCHN 1 Topic 1 Handoutsfleur harrisonNo ratings yet
- Illicit Use of Drugs Among The Youth and Adults in The Frances Baard Region Northern Cape, South AfricaDocument10 pagesIllicit Use of Drugs Among The Youth and Adults in The Frances Baard Region Northern Cape, South AfricaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Handling of The H1N1 Pandemic: More Transparency NeededDocument18 pagesThe Handling of The H1N1 Pandemic: More Transparency Neededmarc_vg100% (1)
- Api Q0315Document68 pagesApi Q0315Abidi HichemNo ratings yet
- Philippine Infectious Control Nurse AssociationDocument3 pagesPhilippine Infectious Control Nurse AssociationFerdinand Natividad0% (1)
- Japanese Encephalitis by RobelDocument2 pagesJapanese Encephalitis by RobelRobel_Saoi_2309No ratings yet
- Care of The Unconscious PatientDocument33 pagesCare of The Unconscious Patientta CNo ratings yet
- A Study To Assess The Knowledge and Practices On Control Mesaures of Hypertension Among The Adults in Selected Areas of Gwalior in A View To Develop A Self Instructional ModuleDocument8 pagesA Study To Assess The Knowledge and Practices On Control Mesaures of Hypertension Among The Adults in Selected Areas of Gwalior in A View To Develop A Self Instructional ModuleEditor IJTSRDNo ratings yet
- IAS53 - Outbreak - Infectious DiseaseDocument57 pagesIAS53 - Outbreak - Infectious DiseaseJinyoungNo ratings yet
- Lesson 1.1 Historical Perspectives of NiDocument24 pagesLesson 1.1 Historical Perspectives of Niclaire yowsNo ratings yet
- 0 Week 8 Hypothesis PDFDocument3 pages0 Week 8 Hypothesis PDFclaire yowsNo ratings yet
- Mod1 Lecture 1.3 - InterstateDocument7 pagesMod1 Lecture 1.3 - Interstateclaire yowsNo ratings yet
- BE Beneficence and NonmaleficenceDocument6 pagesBE Beneficence and Nonmaleficenceclaire yowsNo ratings yet
- Infection Control MeasuresDocument33 pagesInfection Control Measuresclaire yowsNo ratings yet
- 118 Rle Abg PDFDocument6 pages118 Rle Abg PDFclaire yowsNo ratings yet
- 118 Rle Ecg PDFDocument5 pages118 Rle Ecg PDFclaire yowsNo ratings yet
- 118 Rle Ecg 2 PDFDocument3 pages118 Rle Ecg 2 PDFclaire yowsNo ratings yet
- BE AutonomyDocument6 pagesBE Autonomyclaire yowsNo ratings yet
- 118 RLE Suction PDFDocument4 pages118 RLE Suction PDFclaire yowsNo ratings yet
- Mechanical VentilationDocument16 pagesMechanical Ventilationclaire yowsNo ratings yet
- 118 RLE Glasgow Coma Scale GCS PDFDocument4 pages118 RLE Glasgow Coma Scale GCS PDFclaire yowsNo ratings yet
- Ecg MonitoringDocument26 pagesEcg Monitoringclaire yowsNo ratings yet
- Continuation Controlling - PLPDocument7 pagesContinuation Controlling - PLPclaire yowsNo ratings yet
- HGT MonitoringDocument9 pagesHGT Monitoringclaire yowsNo ratings yet
- Controlling PLPDocument17 pagesControlling PLPclaire yowsNo ratings yet
- Ethical Leadership in Nursing - PLP1Document21 pagesEthical Leadership in Nursing - PLP1claire yowsNo ratings yet
- Conflict Management PLPDocument27 pagesConflict Management PLPclaire yowsNo ratings yet
- Delegation PLPDocument22 pagesDelegation PLPclaire yowsNo ratings yet
- Overview To DEFINITION OF TERMS - PLP1Document16 pagesOverview To DEFINITION OF TERMS - PLP1claire yowsNo ratings yet
- Pronunciation GuideDocument7 pagesPronunciation Guideclaire yowsNo ratings yet
- Frameworks For Ethical Decision-Making - PLP1Document23 pagesFrameworks For Ethical Decision-Making - PLP1claire yowsNo ratings yet
- PK Reflection Paper PDFDocument3 pagesPK Reflection Paper PDFclaire yowsNo ratings yet
- Monist 197054217Document3 pagesMonist 197054217claire yowsNo ratings yet
- AUTOCRATICDocument2 pagesAUTOCRATICclaire yowsNo ratings yet
- WEEK 3 119 LEC 2 - Leadership - and - Management PDFDocument8 pagesWEEK 3 119 LEC 2 - Leadership - and - Management PDFclaire yowsNo ratings yet
- Ontological EssayDocument8 pagesOntological Essayclaire yowsNo ratings yet
- WEEK 3 119 LEC 1 - Requisites - For - Successful - L - M PDFDocument4 pagesWEEK 3 119 LEC 1 - Requisites - For - Successful - L - M PDFclaire yowsNo ratings yet
- Kaposi SarcomaDocument14 pagesKaposi Sarcomaedgar mandengNo ratings yet
- Sierra de Cinta Bauer ManualDocument16 pagesSierra de Cinta Bauer Manualluis daniel aguirreNo ratings yet
- Ceii205 PhysiotherapyDocument49 pagesCeii205 PhysiotherapyWaltas KariukiNo ratings yet
- Abstract, Introduction and Statement of The Problem 1.1 AbstractDocument39 pagesAbstract, Introduction and Statement of The Problem 1.1 AbstractIrish Mae JovitaNo ratings yet
- DOH PowerpointDocument232 pagesDOH PowerpointEmmanuel ApuliNo ratings yet
- Suppositories: Abenol (CAN)Document2 pagesSuppositories: Abenol (CAN)Mikko McDonie VeloriaNo ratings yet
- Week 6 Bone Case StudyDocument7 pagesWeek 6 Bone Case StudyAndriNo ratings yet
- Cough: - Atheer AljthalinDocument15 pagesCough: - Atheer AljthalinAmira AlmutairiNo ratings yet
- Algorithm-ACLS CA 200731Document1 pageAlgorithm-ACLS CA 200731Hyunsoo EllisNo ratings yet
- Anaesthesia For Tonsillectomy TOTW 051 2007 230316 022350Document10 pagesAnaesthesia For Tonsillectomy TOTW 051 2007 230316 022350Srihari JanakiNo ratings yet
- Disturbed Body ImageDocument3 pagesDisturbed Body ImageShenaNo ratings yet
- Insecticidal Activity of Tomato (Solanum Lycopersicum) Extract On American Cockroach (Periplenata Americana)Document7 pagesInsecticidal Activity of Tomato (Solanum Lycopersicum) Extract On American Cockroach (Periplenata Americana)heheeheheNo ratings yet
- Definition: Anemic Syndrome:: Semiotics of Basic Diseases of The Blood SystemDocument4 pagesDefinition: Anemic Syndrome:: Semiotics of Basic Diseases of The Blood SystemSagar KhairwalNo ratings yet
- Health 8: Learning Activity Sheet Communicable DiseaseDocument5 pagesHealth 8: Learning Activity Sheet Communicable DiseaseJoeffrie G. CostalesNo ratings yet
- Community Health Nursing 1Document76 pagesCommunity Health Nursing 1Nerlyne Mae PonaseNo ratings yet
- Medsurg Clinical Cheat SheetDocument1 pageMedsurg Clinical Cheat Sheetj.siemens1dNo ratings yet
- Sample ReportDocument3 pagesSample ReportRobeants Charles PierreNo ratings yet
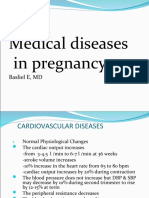
- Medical Diseases in PregnancyDocument37 pagesMedical Diseases in PregnancyAsteway MesfinNo ratings yet
- KSSM Science Form 4 Chapter 10Document16 pagesKSSM Science Form 4 Chapter 10Tang Lilee100% (1)
- The Mechanism Isorhythmic: of Synchronization A-VDocument11 pagesThe Mechanism Isorhythmic: of Synchronization A-VSheila AdiwinataNo ratings yet
- Fracture Healing PDFDocument2 pagesFracture Healing PDFAhmed SalmanNo ratings yet
- Care Plan: Degree Programme in Nursing School of Health and Social StudieDocument14 pagesCare Plan: Degree Programme in Nursing School of Health and Social Studiepevala8648No ratings yet
- Assessing The Thorax and Lung PDFDocument9 pagesAssessing The Thorax and Lung PDFYudi TrigunaNo ratings yet