Professional Documents
Culture Documents
NCM 118 1.5 Shock and Multisystem Disorders Dean Bautista Balmes Barcelon Belarmino
Uploaded by
Nicko Pazon AranasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCM 118 1.5 Shock and Multisystem Disorders Dean Bautista Balmes Barcelon Belarmino
Uploaded by
Nicko Pazon AranasCopyright:
Available Formats
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
SHOCK o Cardiogenic shock after an MI usually occurs
when 40% or more of the myocardium has been
• It is a life-threatening condition (precisely this is damaged.
under critical care) o The term OBSTRUCTIVE SHOCK is sometimes used
• Potentially lethal, debilitating, and costly (people to include conditions that lead to a sudden
would really spend so much in hospitalization, they obstruction of blood flow e.g., cardiac tamponade,
are not sure if they will survive) tension pneumothorax, pulmonary embolism,
• Defined as failure of the circulatory system to thrombus, embolus
maintain adequate perfusion of vital organs (such us
the lungs, liver, heart, kidney, brain) 3. DISTRIBUTIVE SHOCK/ VASOGENIC
SHOCK
CLASSIFICATION OF SHOCK ⎯ due to changes in blood vessel tone that
1. HYPOVOLEMIC SHOCK increase the vascular space without an
⎯ due to inadequate circulating blood increase in the circulating blood volume.
volume resulting from hemorrhage with
3 TYPES OF DISTRIBUTIVE SHOCK
actual blood loss (shock due to low blood
volume), burns of massive shifts of fluids a. Anaphylactic shock
due to movement of plasma proteins into ⎯ severe hypersensitivity reaction
interstitial spaces, and fluid shifts or resulting in massive systemic
dehydration, with or without loss of fluid vasodilation (sensitivity due to drugs,
volume bee sting, insect bites, allergy to
⎯ develops when the intravascular volume foods).
decreases (due to burns, dehydration) to b. Neurogenic shock
the point where compensatory ⎯ interference with nervous system
mechanisms are unable to maintain control of the blood vessels, can
organ and tissue perfusion. occur with conditions such as spinal
2. CARDIOGENIC SHOCK cord injury (especially cervical spine
⎯ due to inadequate pumping action of the injury, severe spinal injury in
heart (heart attack, MI, CAD). The heart vehicular accident or fall), spinal
muscle can be diseased as a result of anesthesia, or severe vasovagal
primary cardiac muscle dysfunction or reactions caused by pain or psychic
mechanical obstruction of blood flow trauma.
caused by myocardial infarction (MI), c. Septic Shock
valvular insufficiency (due to rheumatic ⎯ caused by the release of vasoactive
heart disease) caused by disease or substances. Current theories suggest
trauma (vehicular accident, gunshot there is a cascade of interactions
wounds, or penetrating wounds), cardiac between immune cells that happens
dysrhythmias (heart blocks), or an rapidly that leads to microcirculatory
obstructive condition such as cardiac alterations.
tamponade (there is water in the
pericardial area) or pulmonary embolus.
The clinical definition of cardiogenic ETIOLOGY
shock is decreased cardiac output and
evidence of tissue hypoxia in the 1. HYPOVOLEMIC SHOCK
presence of adequate intravascular a. Hemorrhage
volume. There is 60 ml of blood per beat ⎯ loss of blood (emergency blood
x 72 beats per minute. Below 60 ml, the transfusion is needed)
tissues can no longer be perfused. ⎯ blood volume deficit of 15% to 25%,
or about 500 to 1500 ml in an adult
HEMODYNAMIC CRITERIA FOR ⎯ wounds of the chest, abdomen
CARDIOGENIC SHOCK (abdominal aorta), and thighs can
lead to hemorrhagic shock.
a. Sustained hypotension (systolic b. Burns
blood pressure <90mmHg for at ⎯ large partial-thickness or full
least 30 min) thickness burns
b. Reduced cardiac index (<2.2 ⎯ caused primarily by a shift of plasma
L/min/m2) from the vascular space into the
interstitial space.
OTHER MANIFESTATIONS OF TISSUE ⎯ client may have cardiac dysfunction
HYPOPERFUSION that is due to the presence of
• oliguria (<30ml/hr) myocardial depressant factor (MDF)
Normal urine is 1 ml/minute. There ⎯ Fluid shifts similar to those in burns
should be 60 ml of urine per hour. include nephrotic syndrome (people
• cool extremities with nephrotic syndrome have
Due to lack of blood supply generalized edema known as
• altered mentation anasarca), severe crush injuries
altered state of consciousness (vehicular accident), starvation,
BAUTISTA, BALMES, BELARMINO, BARCELON 1
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
surgery and conditions causing compresses the heart and great
plasma fluids to accumulate in the vessels, thus interfering with
abdominal cavity (e.g. cirrhosis of venous return to the heart.
the liver, pancreatitis, bowel When you want to belch, the air
obstruction) compresses the heart, then
c. Dehydration chest pain occurs.
⎯ reduced oral fluid intake from
significant fluid losses (e.g. rigorous OTHER CAUSES OF CARDIOGENIC SHOCK
exercise causing fluid loss from
sweating and insensible fluid loss 1. Cardiac Valvular insufficiency from
through the respiratory tract and in trauma or disease (in rheumatic heart
hot environment) disease wherein the valve flaps are
⎯ excessive urine output (Diabetes involved)
insipidus) or prolonged vomiting or 2. Myocardial aneurysms (aneurysm in the
diarrhea, leading to dehydration- coronary arteries)
induced hypovolemic shock 3. Rupture of a valvular papillary muscle
(Dysentery, Cholera – dies due to (rupture of the valves such as tricuspid
dehydration) valve, mitral valve, pulmonic valve, aortic
⎯ an inability to obtain fluids, valve. Usually mitral is involved)
inadequate maintenance of chronic 4. Ventricular rupture (if there is left
conditions (e.g. increased blood ventricular hypertrophy. Left ventricle
glucose levels with diabetes) dilates due to prolonged high blood
⎯ Inadequate monitoring of pressure. Excessive dilation or
therapeutic regimens (e.g. diuretic- hypertrophy would cause rupture -
induced dehydration) ventricular rupture)
2. CARDIOGENIC SHOCK 5. Aortic stenosis (the aortic valve leading
a. Myocardial infarction to the aorta, blood from the left ventricle
⎯ impaired heart muscle action is most going to the aorta. Sometimes in aortic
often caused by MI (obstruction in valve, there is stenosis, this may be due
the coronary arteries, so the muscles to inflammatory conditions such as
in the heart are not perfused with rheumatic fever, or it could be
blood. Remaining muscles die) congenital)
⎯ the area of dead or dying tissue that 6. Mitral regurgitation (mitral valve
occurs with infarction impairs connecting the left ventricle and left atria
contractility (due to necrosis) of the is defective due to rheumatic heart
myocardium and cardiac output (15- disease, rheumatic fever, or congenital.
25%) decreases Blood in the left atrium cannot flow. Not
⎯ impaired myocardial contractility all of the blood will enter the left
(heart cannot contract that is why ventricle, some will come back to the left
there is 15-25% blood deficit) may atrium because the mitral valve cannot
also occur with blunt cardiac trauma close. Normally, when the heart
(vehicular accident, gunshot wound), contracts, the valves close)
cardiomyopathy, and heart failure 7. Cardiac dysrhythmias (heart block. There
b. Obstructive Conditions is lack of connection between the SA
• Large Pulmonary Embolism node and AV node because of the
⎯ an embolus is usually the result problem in electrical activity, there is no
of a blood clot that breaks loose rhythm)
in a person with deep vein 8. Infectious and inflammatory processes
thrombosis (DVT) such as myocarditis and endocarditis
A thrombus that travels becomes 9. Pulmonary hypertension (due to left
an embolus ventricular hypertrophy, patent ductus
⎯ this embolus travels through the arteriosus, right-sided heart failure)
venous system to the right side 10. Toxic drugs
of the heart and into the
pulmonary artery 3. DISTRIBUTIVE (VASOGENIC) SHOCK
• Pericardial Tamponade ⎯ size of the vascular space
⎯ accumulation of blood or fluid in increases dramatically because of massive
the pericardial space (outer vasodilation
layer of the heart) that ⎯ result is maldistribution of the blood
compresses the myocardium because of decreased blood pressure
and interferes with the ability of (BP)/hypotension and lack of blood
the myocardium to expand or returning to the heart
contract. ⎯ it is often referred to as “relative”
• A Tension Pneumothorax hypovolemia
⎯ significant amount of air ⎯ volume of blood remains constant, but the
in the pleural space that blood has pooled because of increased
BAUTISTA, BALMES, BELARMINO, BARCELON 2
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
capacity of the vascular system of hypoperfusion
- Septic shock is defined as sepsis with
a. Acute Allergic Reaction persistent hypotension despite fluid
(Anaphylactic Shock) resuscitation and resulting tissue
⎯ common sensitizing agents are hypoperfusion.
Penicillin, Penicillin derivatives, bee - Bacteremia is the presence of viable
stings, chemotherapy, latex, bacteria in the blood. Bacteremia may be
chocolate, strawberries, peanuts, primary (without an identifiable focus of
snake venom, iodine-based infection)
contrast for X-ray studies, seafood
and nonsteroidal anti- Pathophysiology
inflammatory drugs (NSAIDS), - Shock occurs when there is not adequate
food, vaccination circulating volume to maintain aerobic
⎯ re-exposure to the foreign metabolism in the cells.
substance results in the offending - Adequate circulating volume is dependent on
antigen binding to previously three interrelated components of the
synthesized immunoglobulins (e.g. cardiovascular system:
IgE) on the mast cell ⮚ The heart
⎯ this binding causes the release of ⮚ Vascular tone
histamine
⮚ Blood volume
MANIFESTATIONS - If the heart muscle cannot pump effectively,
o Massive vasodilation cardiac output falls.
o Urticaria (hives) - Vascular tone refers to degree of constriction
o Laryngeal edema (cannot by the smooth muscle in the arteriole.
breathe due to edema in the - If one of the three components of circulation
larynx, this leads to death) falls, other parts of the system initiate
o Bronchial constriction compensatory mechanisms. For example,
vasoconstriction and increased cardiac
b. Spinal Cord Injury (Neurogenic output to compensate for decreased volume.
Shock)
⎯ injuries around the T6 level Cardiogenic shock:
⎯ below the level of injury there is - Is failure of the left ventricle to pump
blocking of sympathetic nervous adequate blood volume
stimulation - When cardiac output falls, the body
⎯ the parasympathetic system acts compensates by releasing catecholamines
unopposed (epinephrine and norepinephrine) to increase
⎯ this unopposed stimulation heart rate and systemic vascular resistance to
causes vasodilation, decreased increase venous return.
cardiac output and decreased - The diseased heart cannot maintain its own
tissue perfusion myocardial tissue oxygenation, which results
⎯ neurogenic shock is manifested in a spiral of decreased cardiac output,
by the triad of hypotension, hypotension and further myocardial ischemia
bradycardia, and hypothermia
⎯ after injury, protect the client’s Anaphylactic shock:
spine, maintain the airway and - When a sensitized client comes in contact
breathing (oxygen), provide with an antigen, IgE is stimulated and the
circulatory support (plasma, blood mast cells and basophils release large
transfusion) and provide for amounts of histamine. Histamine leads to
thermoregulation (blanket) vasodilation, bronchial constriction,
c. Infection (Septic Shock) bronchorrhea, pruritus, laryngeal edema and
⎯ Sepsis is the presence of infection angioedema.
and activation of the inflammatory
cascade (tooth decay, liver Septic shock:
inflammation, inflammation of uterus - About 50% of clients with septic shock have
can cause septic shock) bacteremia, with gram-negative rods and
⎯ Systemic inflammatory response gram-positive organism being the most
syndrome (SIRS) exists in two of the common agents.
following four clinical parameters: - Endotoxins (also called lipopolysaccharides)
o Body temperature are produced by gram-negative organisms.
o Heart rate - Gram-positive cocci also produce exotoxins.
o Respiratory rate - Host resitance and organism virulence are
o Peripheral leukocyte count both factors that determine the body’s
- Sepsis is defined as the presence of SIRS in response. Gram-negative (endotoxins) and
the setting of infection. gram-positive (exotoxins)
- Severe sepsis is defined as sepsis with - Initially, there is an overwhelming
evidence of end-organ dysfunction as a result inflammatory response to the microbes that
BAUTISTA, BALMES, BELARMINO, BARCELON 3
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
is regulated by tumor necrosis factor (TNF), cycle of inadequate tissue perfusion is not
interferon, and the interleukins. interrupted.
- Mediators with vasodilatory and endotoxic - The shock becomes progressively more
properties are released systemically, severe, even though the initial cause of the
including prostaglandins, thromboxane A2 shock is not itself becoming more severe.
and nitric oxide. Cellular ischemia and necrosis lead to organ
- Results in vasodilation and endothelial failure and death. Cellular ischemia kay
damage, which leads to hypoperfusion and waray na blood supply, lead to cellular
capillary leakage. necrosis then eventually cellular death.
- Cytokines activate the coagulation pathway,
resulting in the capillary microthrombi and SYSTEMIC EFFECTS OF SHOCK
end-organ ischemia.
1. Respiratory system
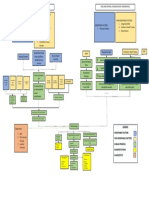
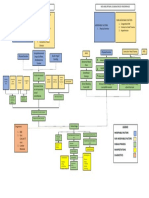
STAGES OF SHOCK - Circulatory deprivation results in tissue
hypoxia and anoxia.
1. Nonprogressive Stage - Respiratory failure continues to be a major
- Cardiac output is slightly decreased because cause of death in shock.
of the loss of actual or relative blood volume - Aspiration and loss of neurologic control of
- Body’s compensatory mechanism can breathing.
maintain BP within a normal to low-normal 2. Acid-Base Balance
range and can maintain perfusion to the vital - Oxygen and nutrients are essential to life
organs. because they synthesize adenosine
- During the compensatory phase, the triphosphate (ATP). ATP is the ultimate
systemic circulation and microcirculation source of energy for life processes. When
work together in a hyperdynamic state. oxygen is not present, ATP is produced
- This hyperdynamic state leads to an increase through anaerobic metabolism.
in lactic acid levels. - Anaerobic metabolism produces anaerobic
metabolites, such as lactic acid (which causes
2. Progressive Stage intracellular acidity with consequent cellular
- If shock and the compensatory damage) and substrates of the adenylic acid
vasoconstriction persist, the body begins to system (which depress the heart)
decompensate and the systemic circulation - In response to the chemoreceptors sensing
and microcirculation no longer work in decreased pH, the rate and depth of
unison. respirations are increased to “blow-off”
- As vasoconstriction continues, the supply of (exhale ) Co2 to compensate for the
oxygenated blood to the tissues is reduced. metabolic acidosis. This results to respiratory
- This results in anaerobic metabolism and alkalosis.
further lactic acidosis. - Because lactic acid is not exhaled, it
- Acidosis and the increasing PaCo2 cause the accumulates in tissue fluids, which become
microcirculation to dilate. increasingly acidic. Metabolic acidosis is
- This dilation causes decreased in venous eventually produced.
return and decreased circulation of - Acidotic reaction resulting from metabolic
reoxygenated blood. acidosis ultimately kills the cells. The buildup
- Increased vascular capacity, decreased blood of lactic acid causes such a severe local
volume, or decreased heart action reduces acidosis that cellular enzymes are inactivated.
the mean arterial pressure (MAP) Cells soon die.
- Pressure gradient for the venous return of 3. Respiratory Alkalosis or Respiratory Acidosis
blood decreases. - Perfusion and oxygen delivery to the tissue
- This also contributes to venous pooling of decrease, cellular energy production
blood, decreased venous return to the heart, decreases. To compensate, cells increase
decreased cardiac output. Kon low an anaerobic metabolism, which results in the
cardiac output, low blood an nakadto ha build-up of lactic acid in the cell.
systemic circulation , there is low tissue - As the pH of the cells decrease, lysosomes
perfusion leading to tissue death or necrosis. within the cell explode, releasing the
- The result is a low central venous pressure powerful, destructive enzymes.
(CVP) and inadequate venous return to the - The enzymes destroy the cellular membrane
right side of the heart, with further decrease and digest the cell contents.
in cardiac output. 4. Lysosomal Enzymes
- This resultant decrease in circulating volume - Lysosomal enzymes are released from dead
and capillary flow does not allow adequate cells undergoing autolysis.
perfusion and oxygenation of vital organs. - During shock, however, the accompanying
- With the prolonged decrease in capillary metabolic acidosis accelerates the activation
blood flow, the tissues become hypoxic. of lysosomal hydrolases within the cells and
their release into the circulation markedly
3. Irreversible Stage exacerbate the tissue injury that occurs
- The irreversible stage of shock occurs if the during shock.
BAUTISTA, BALMES, BELARMINO, BARCELON 4
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
- The release of active lysosomal proteases - Their general effects are to increase blood
and other enzymes from damaged tissue into flow to the brain, heart, and striated
the bloodstream and their action on (skeletal) muscle and to decrease blood flow
extracellular and intracellular structures to the skin, kidneys and splanchnic bed.
probably contribute to the progression of - Sustained vasoconstriction to stagnant
injury from cell to cell. hypoxia and cellular death.
5. Myocardial Deterioration 10. Vasoactive Polypeptides
- MDF, a polypeptide with vasoactive a. Histamine- causes vasodilation,
properties, released in response to ischemia increased capillary permeability,
of the gastrointestinal (GI) tract. It causes bronchoconstriction, coronary
significant reduction in cardiac output. vasodilation and cutaneous reactions
- Myocardial zonal lesions, which appear in the (flares, wheals)
myocardium after ischemia or infarction. b. Bradykinin- a kinin peptide, bradykinin
- Cells in these areas do not fully repolarize and produces vasodilation, increased
thus interfere with the usual efficient capillary permeability, smooth muscle
electrical conduction in the heart, which relaxation, pain, and infiltration of an
results in impaired contraction and possibly area with leukocytes.
cardiac failure. c. Angiotensin- results from the action of
6. Disseminated Intravascular Coagulation renal renin on angiotensinogen which
- Anaerobic metabolism increases the causes vasoconstriction and increased
production of lactic acid. vascular resistance.
- The slow-moving acidic blood is d. MDF – is a vasoactive polypeptide that
hypercoagulable. contributes to cardiac failure in clients in
- Hemolysis (destruction of red blood cells with shock by depressing cardiac muscle
the liberation of hemoglobin) accompanies contraction.
trauma, especially when massive crushing 11. General adaptation Syndrome Response
injury occurs. - Neuroendocrine responses during shock are
- DIC is associated with multiple thrombi or defensive reactions that occur during the
emboli that are deposited in the body’s stage of resistance in the general
microvascular circulation, with resultant Adaptation Syndrome (GAS).
organ obstruction and increased tissue 12. Adrenal Response
ischemia. - The release of epinephrine and
- Because of the inappropriate clotting that norepinephrine from the adrenal medulla
occurs with DIC, the body attempts to (which results in increased respiratory and
reverse the process by breaking down clots. heart rates , increased BP, increased blood
- This results in bleeding in areas previously flow to organs, decreased blood flow to
sealed by clots (e.g. venipuncture sites, peripheral tissues).
vascular leaks in the brain) - Release of mineralocorticoids (which control
- As DIC progresses, clotting factors are fluid and electrolyte balance) and
depleted, causing an inability to form normal glucocorticoids (which increase blood glucose
clots in the presence of bleeding. levels and reduce pain) from the adrenal
7. Vasoconstriction cortex.
- Increased levels of CO2 dilate arterioles - The main mineralocorticoids-aldosterone
located in active tissues and constrict those deoxycorticosterone-help increase
in nonactive tissues. intravascular fluid volume by stimulating the
- Because of the heart’s increased activity, kidneys to retain sodium and water.
excessive CO2 is produced in the - Aldosterone is essential to the conservation
myocardium. of sodium. Because water is retained in the
- Increased concentration of CO2 directly body along with sodium, urine excretion is
dilates the coronary arteries leading to the diminished during shock. This fluid is retained
myocardium, which allows myocardium to in the bloodstream to increase blood volume.
receive more arterial blood. Increasing the blood.
- Co2 is also a powerful stimulant of the 13. Pituitary Response
vasoconstrictor center in the sympathetic - ADH is produced by the posterior pituitary
nervous system. gland.
8. Vasoactive Substances - The osmolality (osmotic concentration) of the
- The influence they exert may be altered by blood increases with dehydration. That
factors such as pH, the specific tissue (e.g. stimulates osmoreceptors in the
heart, lung), the presence of drugs or other hypothalamus to release ADH from the
substances, serum electrolyte levels and posterior pituitary gland. ADH is carried via
sensitivity of the end organ. the blood to the kidneys, where it causes the
9. Catecholamines body to retain water.
- Catecholamines, such as epinephrine and 14. Metabolic Response
norepinephrine, are present early in shock - These fuels (e.g. amino acids, fatty acids,
and are related to the fight-or-flight glucose) are produced by the breakdown of
response. food. These substances are then chemically
BAUTISTA, BALMES, BELARMINO, BARCELON 5
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
converted into energy, resulting in the restored to normal levels.
formation of ATP. 20. Renal Ischemia
- The glucocorticoids particularly - During shock, the kidneys, may experience
hydrocortisone, mobilize energy stores. renal ischemia.
- Protein catabolism and negative nitrogen - When injury to the kidneys is extensive and
balance occur as part of the metabolic renal failure ensures, acute tubular necrosis
response because of glucogenesis (resulting (ATN) occurs.
from glucocorticoid action) and salivation.
15. Neurologic response CLINICAL MANIFESTATIONS
- With shock, cerebral blood flow and cerebral Systemic Manifestation of Shock:
metabolism may become insufficient to 1. Respiratory System
maintain normal mental level of - Rapid, shallow respirations (tachypnea)
consciousness. Because the brain is totally because of decreased tissue perfusion.
dependent on oxygen and glucose and to - Respiratory rate increase as the oxygen-
fluid imbalances. When the brain becomes carrying capacity of the blood decreases.
hypoxic, the cerebral vessels dilate to restore These changes may signal development of
blood flow. hypoxemia and respiratory alkalosis.
16. Immune System 2. Cardiovascular System
- All forms of shock severely depress − Tachycardia. Increased heart rate is the
macrophages, which are located in both the result of increased sympathetic stimulation.
blood and the tissues. The capacity of It is an attempt to maintain adequate cardiac
macrophages to remove bacteria is greatly output and MAP when the blood’s circulating
reduced. volume declines.
- Alterations in the blood itself are partially due − The pulse rate may become extremely slow
to tissue hypoxia and impairment of in the terminal stages of shock.
monitoring activities of the macrophage. − Hypotension. The diastolic BP indicates the
17. Gastrointestinal System resistance (systemic vascular resistance
- Under sympathetic stimulation, vagal (SVR) or vasoconstriction) of blood vessels.
stimulation to the GI tract slows or stops, 3. Neuroendocrine System
resulting in ileus with an absence of − Client feels anxious, nervous, and irritable.
peristalsis. A lack of nutrient blood supply to 4. Renal System
the intestines increases the risk of tissue − Decrease in urinary volume (oliguria)
necrosis and sepsis.
- Shock causes serious changes in the function CLINICAL MANIFESTATIONS OF SPECIFIC TYPES
of the liver, the major organ of detoxification. OF SHOCK
The liver suffers from this impaired
circulation and appears to be a source of toxic ● HYPOVOLEMIC SHOCK
materials. o Sympathetic stimulation increases pulse rate
- During shock, the anoxic liver develops and respirations and decreases tissue
metabolic deficiencies, has an impaired ability perfusion to the skin, causing the skin to feel
to detoxify, and may release vasoactive cool, clammy from diaphoresis, and to appear
substances. pale. Clients may sweat profusely, which
- In addition, enhanced bacterial invasion of increases insensible fluid loss, leading to
the liver from the intestines apparently further hypovolemia and temperature
occurs. instability. Cyanosis may indicate either
- During shock, pooling of blood occurs in the decreased tissue perfusion or decreased
viscera. Pooling of blood in the liver and oxygenation.
portal bed may result when masses of ● CARDIOGENIC SHOCK
agglutinated (clotted) blood plug numerous o Jugular venous distention
small hepatic vessels, sinusoids, and o Increased CVP
intrahepatic radicles of the portal vein and o Pulmonary edema – bc of decreased capillary
hepatic artery. permeability
18. Renal System o Crackles in the lungs
- Urine production decreases and levels of urea o Increased pulmonary capillary wedge
nitrogen and creatinine increase. pressure (PCWP)
19. Altered Capillary Blood Pressure and Glomerular ● DISTRIBUTIVE SHOCK
Filtration
- Inadequate perfusion of renal capillaries is o ANAPHYLACTIC SHOCK
believed to be the cause of early prenatal ▪ headache
failure in shock. The afferent and efferent ▪ severe anxiety
arterioles constrict, shunting blood away ▪ dizziness
from the glomeruli. If shock persists, actual ▪ disorientation
renal shutdown occurs from focal tubular ▪ loss of consciousness
necrosis. ▪ most common sign: laryngeal edema
- Vasoconstriction in the kidneys may continue and chest tightness
for a prolonged time after the systemic BP is ▪ feeling of lump in the throat which is
BAUTISTA, BALMES, BELARMINO, BARCELON 6
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
due to laryngeal edema and is tourniquet 9as
followed by hoarseness, coughing, last resort)
dyspnea, and stridor. Diffuse
wheezes and prolonged expiratory
phase ● Reduce
▪ pruritus and urticaria intraabdominal
▪ edema of eyelids, lips, or tongue 9 or
(angioedema) retroperitoneal
bleeding or
o NEROGENIC SHOCK prepare for
▪ Bradycardia and hypotension emergency
▪ Skin temperature takes on the same
surgery.
temperature as the room
(poikilothermia)
▪ Skin is dry to the touch because of
an inability to sweat.
G.I. bleeding
o SEPTIC SHOCK ● Administer
▪ Hypotension lactated
▪ Coagulation disorders Ruptured ringer’s
▪ Multisystem organ dysfunction of Aortic solution or
septic shock due, in part, to a Aneurysm normal saline
dysregulated expression of the
body’s mediators of inflammation.
● Transfuse with
DIAGNOSTICS
1. Complete blood cell count fresh frozen
2. Blood chemistry plasma,
3. Body fluid cultures platelets, or
4. ABG analysis other clotting
− A low PaCO2 along with low pH and factors, if
bicarbonate levels (metabolic acidosis), significant
indicates that hyperventilation is trying to improvement
compensate. ● Does not occur
5. CVP Measurement with crystalloid
− A pulmonary artery or Swan-Ganz Surgery administration.
catheter may also be invested to assist
with assessments of fluid status, cardiac
function, and tissue oxygen consumption
● Use of non-
MEDICAL MANAGEMENT blood plasma
1. correct the causative factor expanders
(albumin,
2. improve oxygenation
hetastarch,
● oxygen can be delivered via nasal dextran) until
cannula, a mask high-flow, a mask, high- blood is
Erosion of the
available,
flow non-rebreathing mask vessel from
Conduct
lesion, tubes
● Endotracheal; intubation or autotransfusion
or other
if appropriate
tracheostomy devices.
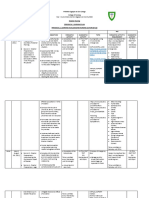
SUMMARY OF MANAGEMENT OF
HYPOVOLEMIC SHOCK ● Administer low-
dose
cadiotonics
Etiology Clinical Intervention
(dopamine,
situation
dobutamine)
Blood loss Massive ● Stop external;
trauma bleeding with
direct pressure, ● Administer
with pressure lactated
dressing, ringer’s
BAUTISTA, BALMES, BELARMINO, BARCELON 7
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
solution or (eg: diabetic
normal saline ketoacidosis,
Crystalloid heat
loss exhaustion)
● Administer
DIC
albumin, fresh
frozen plasma, Protracted
hetastratch, or vomiting,
dextran if diarrhea
cardiac output
still low
Nasogastric
suction
● Administer
isotonic
hypotonic
saline with
electrolytes as
needed to
maintain
normal
circulating
volume and
electrolyte
balance
SUMMARY OF THE MANAGEMENT OF
CARDIOGENIC SHOCK
Burns
Plasma loss
Etiology Clinical Intervention
Situation
Myocardia Acute M.I. ● Fluid challenge
l Disease with up to 300
or injury Myocardial mL of saline
contusion
solution or
Cardiomyopath lactated ringer’s
Accumulation solution to rule
ies
of intra- out
abdominal fluid hypovolemia,
unless heart
failure of
pulmonary
edema is
present.
Malnutrition ● Insert CVP or
pulmonary
artery catheter;
monitor cardiac
Severe
output,
dermatitis
pulmonary
artery pressure
and PCWP
DIC pressure, and
PCWP,
administer IV
fluids to
maintain left
ventricular
falling pressure
of 15-20 mmHg.
Dehydration ● Administer
BAUTISTA, BALMES, BELARMINO, BARCELON 8
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
inotopics. External paracentesis.
(Dobutamine, Pressure Reduce
Pericardial
dopamine) on heart inspiratory
tamponade
vasodilators interferes pressure.
caused by
(Sodium with hear
trauma,
nitroprusside) interferen
aneurysm,
● Nitroglycerin, ces with
cardiac
Calcium channel heart
surgery, Treat
blockers filling or ●
pericarditis dysrhythmias;
(morphine) emptying
● Diuretics (eg: be prepared to
Mannitol or initiate CPR.
furosemide) Massive Cardiac pacing.
● Cadiotonics pulmonary
beta-blockers embolus
(eg:
Tension
propranolol)
pneumothorax
● Gluococorticoste
roids Intar- Ascites
aortic balloon
pump or Hemoperitoneu
external counter m
pulsation device Mechanical
if unresponsive Ventilation
to other
therapies
● Same as above:
if rapid response
does not occur,
prepare for
prompt cardiac
surgery
Cardiac
Dysrhyth Tachydysrythm
mia ias
● Relieve
tamponade with Bradydysrhyth
ECG assisted mias
pericardiocentes Pulseless
is; repair electrical
surgically if it activity
occurs.
● Thrombolytic
(streptokinase)
or anticoagulant
(heparin) SUMMARY OF THE MANAGEMENT OF
Valvular Ruptured aortic
therapy; surgical DISTRIBUTIVE SHOCK
Diseases cusp
or Injury for removal of
Etiology Clinical Interventions
Ruptured clot. Relieves air
Situation
papillary accumulation
muscle with needle Anaphylacti Allergy to food, ● Prepare for
thoracostomy or c shock medicines, surgical
Ball Thrombus
chest tube dyes, insect, management of
insertion. bites, stings, on airway.
● Relieve fluid latex Decrease
accumulation further
with
BAUTISTA, BALMES, BELARMINO, BARCELON 9
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
absorption of cardiotonic
antigen (eg: agents
stop IV fluid, (dopamine or
place dobutamine,
tourniquet norepinephrine;
between isoproterenol,
injection or digitalis,
sting site and calcium
heart if feasible. ● Naloxone
Epinephrine (narcotic
1:100. antagonist)
● 2 inhalations ● Prostaglandins
every 3 hrs, or monoclonal
epinephrine antibodies
(1:1000) 0.2- Drotrecogin alfa
0.5 mL every 3- ● Temperature
15 minutes control (both
given hypothermia
Subcutaneously and
, or epinephrine hyperthermia
(1:10,000) 0.5- are noted)
1.0 mL every 5- ● Heparin,
15 minutes clotting factors,
given at a rate blood products
of 1 mg/min if DIC develops
● IV fluid ● Normal saline to
resuscitation restore volume
with isotonic
solution
Diphenhydrami
ne HCL or
● Theophylline IV ● Treat
drip from bradycardia
Septic Often gram-
bronchospasm with atropine
shock negative
Steroids IV ● Vasopressors
septicemia but
Vasopressors (norepinephrine
also caused by
(eg: , metaraminol
other organism
norepinephrine, bitartrate, high
in debilitated,
metaraminol dose dopamine,
immunodeficien
bitartrate. High and
t, or chronically
dose dopamine) phenylephrine)
ill clients
gastric lavage may be given.
for ingested ● Place client in
antigen ice pack modified
to injection or Trendelenburg
sting site position
● Meat tenderizer ● Place client in
paste to sing head down or
site recumbent
position
● Vigorous Iv fluid
resuscitation ● Give atropine if
with normal bradycardia and
saline profound
● Empirical hypotension
antibiotic ● Eliminate pain
therapy until
sensitivities are
reported
● Administer
BAUTISTA, BALMES, BELARMINO, BARCELON 10
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
Severe pain
Severe
emotional
Vasovagal stress
reaction
3. Restore and maintain adequate perfusion
● Maintain an adequate circulating blood
volume
4. Nitric oxide
5. Vasoconstrictors
● They do favorably increase blood flow to
the brain and heart in severely
hypotensive clients
6. Vasodilators
● Include adrenergic blocking agents,
ganglionic blocking agents, and direct-
acting peripheral vasodilators.
● Adrenergic blockade prevents harmful
effects of prolonged vasoconstriction
such as increased pressure in capillaries,
promoting fluid loss from the vascular to
the interstitial compartment, and altered
blood flow, especially in the splanchic
area.
● Also used to keep the coronary arteries
open
● May be administered to inhibit
Spinal vasoconstriction of peripheral blood
anesthesia vessels (the result of norepinephrine
from sympathetic stimulation) so that
Spinal cord blood can be redistributed to enhance
injury tissue perfusion and increase vascular
volume
● Rapid and adequate fluid replacement
Neurogenic ● Keep clients who are receiving
(spinal) vasodilators lying relatively flat
Shock ● Elevation of the head can produce
dangerous orthostatic hypotension
7. Assist circulation
8. Intra-aortic balloon pump (IABP)
● Balloon-tipped catheter placed in the
descending thoracic aorta
● The catheter is attached to a unit that
inflate during diastole and deflates just
before the systole.
● Counter pulsation displaces blood back
into the aorta and improves coronary
artery circulation
● In cardiogenic shock, use of the IABP
reduces afterload, allowing the heart to
more efficiently empty, thereby,
increasing cardiac output.
9. Modified Trendelenburg position
BAUTISTA, BALMES, BELARMINO, BARCELON 11
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
● Lower extremities elevated 30-45 colloid has been used to treat
degrees hypovolemic shock and may provide
● Knees straight, trunk horizontal or very alternatives to blood administration. Its
slightly raised and the neck comfortably effect last between 3 and 24 hours.
positioned with the head level with the ● Pentastarch is also available as volume
chest or slightly higher. expander
● The traditional Trendelenburg position 16. Evaluate fluid replacement
(head down, with legs elevated at least 17. Prevent renal impairment
30 degrees above the head), was once 18. Prevent gastrointestinal bleeding
the classic shock position but is no longer 19. Provide pharmacologic management
used for shock management because it ● Antibiotic (ex: gentamicin, amikacin) are
compresses the abdominal contents common first line choice for antibiotic
against the diaphragm, interfering with therapy
pulmonary excursuion ● Drotrecogin alfa
● And promotes congestion of blood in the, ▪ Drotrecogin alfa (xigris) I used
possibly contributing to cerebral for severe sepsis and SIRS.
10. Replace fluid volume Drotrecogin alfa is recombinant
● Aggressive fluid replacement should be form of human activated protein
tapered off when urine output is at least C and has the ability to inhibit
0.5 mL/kg/hr, systolic BP is greater than inflammation, inhibit
100 mmHg, or the heart rate is 60 to 100 coagulation, and promote
bpm fibrinolysis. The main effect of
11. Blood protein C is to reduce the
● Rapid administration of large volumes of production of thrombin by
packed cells or whole blood may be inactivating factors Va and VII
necessary ● Heparin
● Crystalloid is usually given as an initial ▪ The anticoagulant effect of
emergency treatment to sustain BP. heparin may help prevent
12. Autotransfusion complications or treat DIC
● Involves collecting and retransfusing ▪ The treatment if DIC may include
blood into the same client heparin administration to
● Used to prevent or treat hypovolemic minimize consumption of clotting
shock cause by hemorrhage factors.
13. Crystalloid or balanced salt solutions ● Steroids
● Warmed crystalloids or balance salt ▪ Are given to reduce edema in the
solutions, colloids, and blood cord and have been shown to
● Dextrose and water should not be used improve recovery. They assist in
to resuscitate a client; once the dextrose treatment by stabilizing
is metabolized, only hypotonic water lysosomal membrane and
remains, which leads to greater fluid preventing intracellular release
shifts. Electrolyte solutions such as of enzymes
ringer’s lactate help expand extracellular ● Naloxone
volume reduce viscosity and prevent ▪ Used to treat opioid and
sludging. In a client with impaired liver synthetic opioid over dosages
function, a solution containing lactate ▪ During stress, opioid like
could further compound the problem of substances known as
lactic acidosis enkephalins and endorphins are
● Lactate is converted to bicarbonate and released from the brain
does not accumulate ▪ May play a role in capillary bed
14. Colloid solution vasodilation found in all forms of
● Most commonly used colloid solutions shock
include plasma and its components, ● Insulin
plasma substitutes (dextran), oxygen- ● Epinephrine
carrying solutions other than blood (eg: ▪ Drug choice for treatment of
perfluorocarbons and ultra-purified, allergic reaction
stroma-free hemoglobin solution), and ▪ Inhibits histamine release and
hetastarch antagonizes its effects on end
● Fresh frozen plasma (FFP) is the form organs, resulting in reversal of
commonly used to improve serum the bronchial constriction,
protein levels increased capillary permeability
15. Blood substitutes and vasodilation that occur with
● Perfluorocarbon (eg: fluosol, oxygen) are acute anaphylactic reactions.
non-blood, oxygen-carrying solutions ● Proton pump inhibitors, Sucralfate, and
that remain in the circulation for about Histamine H2-Receptor Antagonists
12-24 hours ▪ Inhibits gastric acid secretion
● Hetastarch, a glycogen-like synthetic ▪ Stress ulcers are often lethal
BAUTISTA, BALMES, BELARMINO, BARCELON 12
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
complications of severe illness or DIAGNOSIS
injury produced by continuous ● Ineffective tissue perfusion
shunting of blood from the GI ● Interrupted family processes
tract due to extended ● Activity intolerance
sympathetic nervous system ● Acute pain
stimulation. ● Anticipatory grieving
● Opioids ● Anxiety
● Cardiotonic Medications ● Bathing/hygiene, dressing/grooming,
▪ Beta blockers and calcium toileting, self-care deficit
channel blockers ● Compromised family coping
▪ Amiodarone, lidocaine, ● Constipation
bretylium, quinidine, and ● Decreased cardiac output
procainamide may treat ● Deficient fluid volume
dysrhythmias that tend to reduce ● Disturbed body image
cardiac efficiency ● Disturbed personal identity
● Calcium ● Disturbed sleeping pattern
● Disturbed sensory perception: visual
auditory, kinesthetic, gustatory, tactile,
NURSING MANAGEMENT OF THE MEDICAL olfactory.
CLIENTS ● Fear
● Imbalanced nutrition: less than body
1. Oxygenation monitoring requirements
2. Perfusion monitoring ● Impaired gas exchange
→ Assess the client’s pulse, BP, skin, ● Impaired physical mobility
temperature, heart sounds, peripheral ● Impaired or risk for impaired skin integrity
pulses, state of hydration, and skin ● Impaired verbal communication
perfusion (ex: capillary refill time less ● Ineffective airway clearance
than 3 seconds) ● Ineffective breathing pattern
3. BP monitoring ● Ineffective protection
4. Temperature monitoring ● Ineffective tissue perfusion: cerebral,
5. Cardiac monitoring cardiopulmonary, gastrointestinal, renal,
→ ECG monitor peripheral
→ CVP line placement ● Interrupted family processes
6. Hemodynamic monitoring ● Spiritual distress
→ Measurement of CVP
→ Pulmonary artery and pulmonary MULTIPLE ORGAN DYSFUNCTION
capillary wedge pressure (PCWP)
SYNDROME
→ Measurement are monitored to assess
left-sided heart function and to guide
fluid administration. ● Multiple Organ Dysfunction Syndrome (MODS),
7. Cardiac output monitoring Multiple Organ System Failure, r Multi-organ
→ Swan-Ganz catheters and the ease of system failure
obtaining measurements.
→ Is considered to be present when two
8. Prevent complications
→ Additional assessments important in
or more organs fail
preventing complications include
evaluation of the following : ETIOLOGY AND RISK FACTORS
- Level of consciousness and orientation → Dead tissue
- Ability to move extremities → Injured tissue
- Sensation in all extremities → Infection
- Hand grasps → Perfusion deficit
- Response to verbal and painful stimuli → Persistent sources of inflammation such
- Pupil size and reaction to light
as pancreatitis or pneumonitis.
- Bowel sounds
- Abdominal distention
→ Acute lung injury
- Bone deformities ● People known to be at high risk*
- Older adults
9. Prevent renal impairment - Clients with chronic illnesses
→ Indwelling catheter - Clients with malnutrition
→ Assess the client’s urine output routinely - Clients with cancer
and recore it at least every hour.
- Prolonged or exaggerated inflammatory
10. Prevent gastric ulceration
● Guaiac solution can be used to check for
responses
blood; litmus paper checks the pH to - Victims of severe trauma
determine the acidity of the stomach. - Clients with sepsis
BAUTISTA, BALMES, BELARMINO, BARCELON 13
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
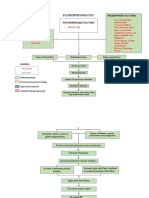
PATHOPHYSIOLOGY: → Body engages in auto catabolism, which
→ Integrated inflammatory immune response (IIR) causes profound changes in the body’s
protects tissue from microbial invasion and rids metabolic processes
the body of cellular debris and foreign material’ → Outcome for the client is death.
→ Bacteria introduced into the wound or allowed
to grow in necrotic tissue because of a CLINICAL MANIFESTATION
decreased immune response activate the → Aspiration
systemic inflammatory responses → Ruptured aneurysm
→ Bacteria release txins that activate systemic → Septic shock
medications of inflammation → Hypotension
→ Once the inflammatory response becomes → Low grade fever
systemic, it is controlled by chemical mediators → Tachycardia
of inflammation. → Increased numbers of banded and
→ Mediators include bradykinin complement, Segmented Neutrophils
histamine, interleukin-1, prekallikrein, → Dyspnea – Intubation And
prostaglandins and tumor necrosis factor (TNF) Mechanical Ventilation Are
→ These powerful mediators of inflammations Required
induce a systemic response. → DIC Is Usually Present
→ The endothelium is destroyed and blood flow is → Increased Cardiac Index (Greater
reduced to the tissues Than 4.5 L/Min)
→ Endothelial damage is produced by endotoxins → Systemic Vascular Resistance Of Less
from bacteria, tumor necrosis factor, Than 600 Dynes Cm-5
interleukin-1, platelet activating factors and → Increased Blood Glucose
many others → Bilirubin Level Increases
→ It produces damage to organs and tissues by → Increase In Serum Creatinine
altering perfusion, disturbing oxygen supply or → Blood Glucose And Lactate Levels
demand or hanging metabolic dysfunctions Continue To Increase Because Of
→ Metabolism increases under the direction of The Hypermetabolic State
mediators such as cortisol and the → Excretion Of Urinary Nitrogen And
catecholamines Protein
→ The lungs are usually the first to malfunction, → Decreased Levels Of Serum Albumin,
because of the large surface area of pulmonary Pre-Albumin And Retinol
epithelium combined with the presence of → Candida And Viruses
bacterial contamination from systemic blood → Cytomegalovirus
return → Surgical Wounds To Fail To Heal
→ The GI tract is general the second system to → Pressure Ulcers May Develop
malfunction, and it propagates conditions for → Renal Failure Worsens
further deteriorations of other organs. → Edema May Be Present Because Of
→ The hypermetabolic state increases gastric acid Low Serum Protein Levels
production, increasing the risk of ulceration and → Lactic Acidosis Worsens, Liver
bleeding. Enzymes Continue To Increase.
CLASSIFICATION: MEDICAL MANAGEMENT
1. Primary MODS 1. Restrain The Activators
→ Results directly from “a well-defined → Antibiotics
insult in which organ dysfunction occurs → Large Infected Wound Incised And
early and is directly attributed to the Drained Or Necrotic Tissue Excised
insult itself. → Nutrient Intake Is Usually 30 To 35
→ The direct insult initially causes to Kcal/Kg/Day Of Carbohydrates
localized inflammatory response that → Proteins Are Given To The Client Via
may or may not progress to SIRS. Modified Amino Acids
2. Secondary MODS 2. Control The Mediators
→ Is a consequence of widespread → Maintenance of A Positive Nitrogen
systemic inflammation, which develops Balance Via Nutrition, Promotion Of
after a variety of insults and results in Sleep And Rest And Management Of
dysfunction of organs not involved in the Pain.
initial insult → Monoclonal Antibodies To Control
Mediators Such As Interleukin-1,
Endotoxins And Tumor Necrosis Factor
BAUTISTA, BALMES, BELARMINO, BARCELON 14
1P
SHOCK AND MULTISYSTEM DISORDERS
1.5 NCM 118: Critical Care Nursing
Dr. Socorro S. Gasco, RN, MN, DM • January 14, 2022
3. Protect The Affected Organs Treatment of infection ● Monoclonal
→ Client Is Intubated An Mechanically antibodies
Ventilated To Maintain Adequate ● Positive antibody
Oxygenation protection
→ Fluids And Inotropic Drugs Are Used To ● Gut
Support Hemodynamic Parameters
decontamination
→ Nutritional Supports Also Critical To
regimens
Reduce the Catabolism That
Accompanies Hyper Metabolism. Support of Gut functions ● Mucosal trophic
Dialysis Is Often Used To Reduce agents:
Azotemia From Renal Failure.
e.g glutamine,
Modified Apache II Criteria for Diagnosis of Multiple bombesin, ketone
Organ Dysfunction Syndrome bodies
● Cardiovascular Failure (Presence of One or More ● Early enteral
of the Following) feeding
→ Heart rate <54 beats/min ● Regulation of gut
→ Mean arterial pressure ≤ 49 mmHg (systolic microbial flora
pressure ≤ 60 mmHg)
→ Occurrence of ventricular tachycardia or Improved resuscitation ● Hypertonic saline
ventricular fibrillation ● In-line sensors
→ Serum pH ≤7.24 with a PaCO2 of ≤40 mmHg ● Tissue-specific
sensors
● Respiratory Failure (Presence of One or More of ● Noninvasive
the Following) monitoring
→ Respiratory rate ≤5 breaths/min or ≤49
breaths/min PaCO2 ≥ mmHg Endothelial cell ● PAF inhibitors
→ Alveolar – arterial oxygen difference ≥350 mmHg protection ● WBC adherence
(calculate as follows, at sea level (713 x % oxygen inhibition
in inspired gas) – PaCO2 – PaO2 ) ● Antioxidant
→ Dependent on ventilator or CPAP on the second therapy
day ● Eicosanoid
modulation
● Renal Failure (Presence of One or More of the
Following) Modulation of ● N3
→ Urine output ≤479 ml/24 hr or ≤1.59 ml/8 hr macrophage function polyunsaturated
→ Serum BUN ≥100 mg/dl (35.7 mmol/L) fatty acids
→ Serum creatinine ≥3.5 mg/dl (309 umol/L) ● Signal
● Hematologic Failure (Presence of One or More of transduction
the following)
modulation
→ WBC count ≤1000/µl (1 x 10^9/L)
→ Platelets ≤20,000/µl (20 x 10^9/L) Stimulation of ● Arginine
→ Hematocrit ≤20% lymphocyte function ● W3
polyunsaturated
● Neurologic Failure fatty acids
→ Glasgow Coma Scale score ≤ 6 ( in absence of
sedation )
● Hepatic Failure (Presence of Both the Following) ⎯
→ Serum bilirubin ≥6 mg%
→ Prothrombin time ≥4 sec over control in the
absence of systemic anticoagulation
Summary of Potentially Useful Therapies for multiple
Organ Dysfunction Syndrome
Rationale Therapy
BAUTISTA, BALMES, BELARMINO, BARCELON 15
1P
You might also like
- Semifinals NCM 118 - NotesDocument25 pagesSemifinals NCM 118 - NotesBokNo ratings yet
- Disaster Triage NursingDocument2 pagesDisaster Triage NursingJohiarra TabigneNo ratings yet
- Emergency and Disaster NursingDocument9 pagesEmergency and Disaster NursingDempsey AlmirañezNo ratings yet
- Pneumonia Nursing Care and TreatmentDocument4 pagesPneumonia Nursing Care and TreatmentBobby Christian DuronNo ratings yet
- Frando-Detailed Learning Module 7.2.Document15 pagesFrando-Detailed Learning Module 7.2.Ranz Kenneth G. FrandoNo ratings yet
- Cardiovascular Emergencies Nursing CareDocument6 pagesCardiovascular Emergencies Nursing CareRENEROSE TORRESNo ratings yet
- PDF DocumentDocument31 pagesPDF Documentirish felixNo ratings yet
- Notes I III Life Threatening ConditionsDocument5 pagesNotes I III Life Threatening ConditionsFaye MontenegroNo ratings yet
- NCM118 Lecture 1Document18 pagesNCM118 Lecture 1mirai desuNo ratings yet
- Finals Reviewer and Activities NCM 116 LecDocument24 pagesFinals Reviewer and Activities NCM 116 LecMary CruzNo ratings yet
- Lesson 3 Responses To Altered Ventilatory FunctionDocument136 pagesLesson 3 Responses To Altered Ventilatory FunctionMonasque PamelaNo ratings yet
- NCM 118 Midterms ReviewerDocument7 pagesNCM 118 Midterms ReviewerKai SamaNo ratings yet
- Communicable Disease Nursing2Document43 pagesCommunicable Disease Nursing2CAÑADA, JOHANNELYN M.No ratings yet
- MS Eent (Nle)Document3 pagesMS Eent (Nle)Maginalyn CangasNo ratings yet
- Disaster Nursing IntroductionDocument5 pagesDisaster Nursing IntroductionCARL ANGEL JAOCHICONo ratings yet
- Foundation of Nursing Practice Exam For Infection Asepsis Basic Concept of Stress and IllnessDocument34 pagesFoundation of Nursing Practice Exam For Infection Asepsis Basic Concept of Stress and IllnessAdrian MiguelNo ratings yet
- Fundamentals of Nursing Midterm ReviewDocument29 pagesFundamentals of Nursing Midterm ReviewCharisse CaydanNo ratings yet
- Final Written RevalidaDocument7 pagesFinal Written RevalidaRowena Lalongisip De LeonNo ratings yet
- 118 RLE Mechanical Ventilation PDFDocument5 pages118 RLE Mechanical Ventilation PDFclaire yowsNo ratings yet
- Sirs ModsDocument10 pagesSirs ModsRENEROSE TORRESNo ratings yet
- NCM 118 - Lesson 4 (ARDS)Document4 pagesNCM 118 - Lesson 4 (ARDS)Bobby Christian DuronNo ratings yet
- B .Focused Assessment Body Part Examined Normal Findings Actual Findings Clinical Significance Inspection InspectionDocument13 pagesB .Focused Assessment Body Part Examined Normal Findings Actual Findings Clinical Significance Inspection InspectionIsabella SamsonNo ratings yet
- 6 Alterations On Tissue Perfusion Poleno Serrano TajalaDocument18 pages6 Alterations On Tissue Perfusion Poleno Serrano TajalaSophia A. GoNo ratings yet
- Pharma NotesDocument18 pagesPharma Notesseanne kskwkwkaNo ratings yet
- Nelec2 Week 17Document13 pagesNelec2 Week 17Michelle MallareNo ratings yet
- Detailed Learning Module 7.2.PdDocument14 pagesDetailed Learning Module 7.2.PdRanz Kenneth G. FrandoNo ratings yet
- Learning: St. Mary'S College of Tagum, IncDocument37 pagesLearning: St. Mary'S College of Tagum, IncAlyssa Gaile EspirituNo ratings yet
- Emergency NursingDocument29 pagesEmergency NursingLouise NicoleNo ratings yet
- 3 Common Neurologic Problems of Altered PerceptionDocument10 pages3 Common Neurologic Problems of Altered PerceptionSTEFFANIE VALE BORJANo ratings yet
- MSN Communicable DiseaseDocument29 pagesMSN Communicable DiseaseLuis LazaroNo ratings yet
- NP5 Recalls5Document9 pagesNP5 Recalls5AhrisJeannine EscuadroNo ratings yet
- Respiratory Emergencies: Amy Bullock Amy - Bullock@students - Plymouth.ac - UkDocument34 pagesRespiratory Emergencies: Amy Bullock Amy - Bullock@students - Plymouth.ac - UkThea BerteaNo ratings yet
- Requirement in PathophysiologyDocument38 pagesRequirement in PathophysiologyckathreenahNo ratings yet
- Ms Pain and Surgery ModulesDocument30 pagesMs Pain and Surgery ModulesweissNo ratings yet
- High Acuity and Emergency SituationDocument9 pagesHigh Acuity and Emergency SituationRENEROSE TORRESNo ratings yet
- Advanced Psychiatric Nursing SyllabusDocument2 pagesAdvanced Psychiatric Nursing SyllabusAlexandra T Manzano100% (1)
- PALMRDocument9 pagesPALMRCai SolanoNo ratings yet
- Alternative & Complementary Therapies for WellnessDocument32 pagesAlternative & Complementary Therapies for WellnessVanetNo ratings yet
- Pulmonary Hypertension Lesson Assessment, Treatment, and Nursing GoalsDocument3 pagesPulmonary Hypertension Lesson Assessment, Treatment, and Nursing GoalsBobby Christian DuronNo ratings yet
- Disaster Nursing P1 Learning PlanDocument5 pagesDisaster Nursing P1 Learning PlanPamela GastalaNo ratings yet
- Cardiomyopathy: Mrs. D. Melba Sahaya Sweety M.SC Nursing GimsarDocument55 pagesCardiomyopathy: Mrs. D. Melba Sahaya Sweety M.SC Nursing GimsarD. Melba S.S ChinnaNo ratings yet
- Psychiatric Nursing Set 1 Oct 27Document8 pagesPsychiatric Nursing Set 1 Oct 27Jayrald CruzadaNo ratings yet
- NCM 118 - Lesson 2 (COPD)Document6 pagesNCM 118 - Lesson 2 (COPD)Bobby Christian DuronNo ratings yet
- Post Test - Prof Ad - Prof. Fuentes (SC)Document2 pagesPost Test - Prof Ad - Prof. Fuentes (SC)Kristen FajilanNo ratings yet
- Pharma - SkinDocument8 pagesPharma - Skinreference books100% (1)
- Neurology Lectures 1 5 DR - Rabo 2Document20 pagesNeurology Lectures 1 5 DR - Rabo 2Miguel Cuevas DolotNo ratings yet
- Pneumothorax Lesson GuideDocument4 pagesPneumothorax Lesson GuideBobby Christian DuronNo ratings yet
- NCM 118Document8 pagesNCM 118Zanie CruzNo ratings yet
- Lesson 2 Gemst Assessment PabilloreDocument7 pagesLesson 2 Gemst Assessment PabilloreInward Demons CommunityNo ratings yet
- NCM101 Health Assessment ExaminationDocument11 pagesNCM101 Health Assessment ExaminationJonah R. Merano100% (1)
- Reviewer Funda LecDocument71 pagesReviewer Funda LecCorillo, Fionnula JeanNo ratings yet
- Management of Patients With Respiratory DisordersDocument14 pagesManagement of Patients With Respiratory DisordersJhosita Flora LarocoNo ratings yet
- Frenle Revie Np3 and Np4-1Document49 pagesFrenle Revie Np3 and Np4-1erjen gamingNo ratings yet
- NCM 118 - Lesson 3 (Pulmonary Embolism)Document4 pagesNCM 118 - Lesson 3 (Pulmonary Embolism)Bobby Christian DuronNo ratings yet
- Lec Activity12 Cardiovascular SystemDocument14 pagesLec Activity12 Cardiovascular SystemAlyssa GerioNo ratings yet
- Head and Neck Anatomy MCQDocument73 pagesHead and Neck Anatomy MCQMacy BesasNo ratings yet
- Test DrillsDocument103 pagesTest DrillsOlive NNo ratings yet
- Communicable Diseases of the Nervous SystemDocument11 pagesCommunicable Diseases of the Nervous SystemMilcah NuylesNo ratings yet
- Module 1C - Speed ReadingDocument2 pagesModule 1C - Speed ReadingTrina RiveraNo ratings yet
- StrokeDocument28 pagesStrokeBEA RADANo ratings yet
- Atenolol Drug CardDocument4 pagesAtenolol Drug CardNicko Pazon AranasNo ratings yet
- Philippines NCD and Family Planning ProgramsDocument11 pagesPhilippines NCD and Family Planning ProgramsNicko Pazon AranasNo ratings yet
- Drug Gordons PeDocument6 pagesDrug Gordons PeNicko Pazon AranasNo ratings yet
- Drug Mechanisms, Indications, Contraindications and Nursing ResponsibilitiesDocument5 pagesDrug Mechanisms, Indications, Contraindications and Nursing ResponsibilitiesNicko Pazon AranasNo ratings yet
- Patho SahDocument1 pagePatho SahNicko Pazon AranasNo ratings yet
- Sah PathoDocument1 pageSah PathoNicko Pazon AranasNo ratings yet
- Aranas - Geriatric Assessment ToolDocument14 pagesAranas - Geriatric Assessment ToolNicko Pazon AranasNo ratings yet
- Educational Status of Barangay Ruby, Tacloban City, Leyte January 2019-December 2019 Educational Status Frequency PercentageDocument6 pagesEducational Status of Barangay Ruby, Tacloban City, Leyte January 2019-December 2019 Educational Status Frequency PercentageNicko Pazon AranasNo ratings yet
- RTRMF's History, Connections & Leaders During COVID-19Document5 pagesRTRMF's History, Connections & Leaders During COVID-19Nicko Pazon Aranas100% (1)
- 27 GuytonDocument6 pages27 GuytonBianca Louise Chan LimNo ratings yet
- Cambridge IGCSE: Biology 0610/41Document20 pagesCambridge IGCSE: Biology 0610/41dharshini_perumalNo ratings yet
- Various Clinical Consideration of Sira: Anatomical Considerations, Sira Vedhan and Sira Gata VataDocument3 pagesVarious Clinical Consideration of Sira: Anatomical Considerations, Sira Vedhan and Sira Gata VataRaptor EaglesNo ratings yet
- Connective Tissue TumorsDocument60 pagesConnective Tissue TumorsRahul Nagda67% (3)
- Circulatory and Respiratory SystemDocument2 pagesCirculatory and Respiratory Systemclarisse100% (1)
- November 2017 (v3) QP - Paper 2 CIE Biology IGCSEDocument20 pagesNovember 2017 (v3) QP - Paper 2 CIE Biology IGCSEsansNo ratings yet
- The circulatory and excretory systems in humansDocument12 pagesThe circulatory and excretory systems in humanssuvashreeNo ratings yet
- MORE THAN 3000 QUESTION BANK OF Dr. MOHAMED YAHIADocument775 pagesMORE THAN 3000 QUESTION BANK OF Dr. MOHAMED YAHIAسماح صلاح100% (1)
- Lower Extremity Arterial Protocol 14 1Document2 pagesLower Extremity Arterial Protocol 14 1api-3494022400% (1)
- Artikel Pembuluh Darah Dan Tekanan DarahDocument13 pagesArtikel Pembuluh Darah Dan Tekanan DarahSiska TiaraNo ratings yet
- Strength For Life After 40Document930 pagesStrength For Life After 40Luis100% (3)
- Epiglu - Instructions For UseDocument2 pagesEpiglu - Instructions For Usezeinabhabeeb100% (1)
- Pathophysiology of Pulmonary Embolism (Loria.J)Document2 pagesPathophysiology of Pulmonary Embolism (Loria.J)Justine Mae Loria0% (1)
- Adventure in Science Book 4Document270 pagesAdventure in Science Book 4safia qureshi100% (1)
- SCIENCE 9 Q1-WK 1-2.b FOR STUDENTDocument16 pagesSCIENCE 9 Q1-WK 1-2.b FOR STUDENTErra PeñafloridaNo ratings yet
- Acute and Critical Care Formulas and Laboratory Values 2013Document196 pagesAcute and Critical Care Formulas and Laboratory Values 2013Mădălina SilaghiNo ratings yet
- General Pathology Lecture NotesDocument29 pagesGeneral Pathology Lecture NotesMohd Syaiful Mohd ArisNo ratings yet
- CH 19 Transport in HumanDocument49 pagesCH 19 Transport in HumanRay PeramathevanNo ratings yet
- New Town Secondary SA2 2021 Sec 2 ScienceDocument36 pagesNew Town Secondary SA2 2021 Sec 2 Scienceok kkNo ratings yet
- Natural Science 1 PrimariaDocument13 pagesNatural Science 1 PrimariaMaria BNo ratings yet
- Anestesi Pada Hipertensi PulmonalDocument3 pagesAnestesi Pada Hipertensi Pulmonalibunqumaira100% (1)
- Long Test 2 - Science 6: Match The Excretory Organs in COLUMN B With Its Description in COLUMN ADocument3 pagesLong Test 2 - Science 6: Match The Excretory Organs in COLUMN B With Its Description in COLUMN Akatherine corveraNo ratings yet
- COVID Thrombosis: Mitochondria, The Endothelial Glycocalyx and Platelets Are KeyDocument10 pagesCOVID Thrombosis: Mitochondria, The Endothelial Glycocalyx and Platelets Are KeyMercedes BouterNo ratings yet
- RTPC101 Body System RootsDocument40 pagesRTPC101 Body System RootsJazther CapiliNo ratings yet
- Adverse Effects of Fillers and TheirDocument16 pagesAdverse Effects of Fillers and Theirt3klaNo ratings yet
- Coronary Microvascular Disease Pathogenic Mechanisms and Therapeutic OptionsDocument17 pagesCoronary Microvascular Disease Pathogenic Mechanisms and Therapeutic OptionsZuleynny TellesNo ratings yet
- Anatomical structures in Cells at Work animeDocument3 pagesAnatomical structures in Cells at Work animeRochele ForondaNo ratings yet
- Secondary Progression Test - Stage 8 Science Paper 2 PDFDocument16 pagesSecondary Progression Test - Stage 8 Science Paper 2 PDFstrictlythomas73% (22)
- Circulatory and respiratory reviewDocument5 pagesCirculatory and respiratory reviewTristan PereyNo ratings yet
- Enzyme 20pagesDocument20 pagesEnzyme 20pagesEddie Optin100% (1)