Professional Documents
Culture Documents
Srg5a CM6
Srg5a CM6
Uploaded by
Mikhail LamayoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Srg5a CM6
Srg5a CM6
Uploaded by
Mikhail LamayoCopyright:
Available Formats
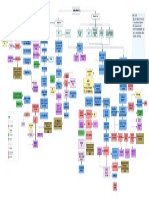
Surgery Group 5 A:
BALATERO, ANNA MAE
BALETA, CHRISTINE
BALLENER, JE OLIVE
BECIOS, ENA MAE
INFECTIONS OF
SIGNIFICANCE
PREVENTION AND
TREATMENT OF SURGICAL
INFECTIONS
Surgical Site Intra-Abdominal Organ-Specific Skin and Soft tissue
Primary microbial Pyogenic Liver Superficial/Skin
Risk factors Pre-Operative Intraoperative Postoperative
peritonitis abscesses structure infections
Factors Factors Factors
Age, DM, Carrier state,
Obesity, Immunosuppression, MC agents: E coli, K MC agents: E coli, K + Cellulitis
Patient Anemia, Renal failure, CSD and S pneumoniae, pneumoniae, Enteric + Erysipelas
+ > 250 neutrophils/L bacilli, Enterococci, + Lymphangitis
Blood transfusion, Hypoxia, Pseudomonas spp., Sterile technique in
Pre-Operative Hair Operating Room Surgical instruments sterilized Incisional care
Local Hypothermia, Local tissue Bacteroides spp., No hair should be removed changing dressing
Removal Environment Ventilation
necrosis, IAP, PSP Diagnosis: PE anaerobic Treatment: Antibiotics unless necessary
Maintained at positive pressure
findings streptococci,
Toxin secretion, Prolonged + > 250 neutrophils/L Fusobacterium spp., Hair Clipping>Hair shaving
Microbial Community-acquired
hospitalization, Clearance C albicans -Maintain Integrity of healing
MRSA incision
resistance Discharge Teaching
Treatment: Antibiotic Core Body Patient maintained at -Educate patient about S/S of
Patient Skin Aseptic Agents:
Wound class administration for 14- Splenic abscesses Management: -Iodophors Temperature > 36.5°C infection
Operation
21 days Adequate drainage -Alcohol containing agents
Ex. Hernia repair,
and administration of -Biguanides
breast biopsy extremely rare and first-line antibiotics
Clean (Class I) EIR: 1-2 % Secondary microbial are treated in a
peritonitis similar fashion liver Increased Oxygen Facilitate phagocytic eradication
Ex. Cholecystectomy, Aggressive Soft Delivery of microbes
Elective GI surgery abscess tissue infections
Clean/Contaminated Pre-operative Hand Aseptic agents
EIR: 2.1-9.5 % due to perforation or Alcohol hand rub
(Class II) severe inflammation Anti-sepsis
Ex. Colorectal surgery Recurrent abscesses Sterile gloves
EIR: 4-14 % and infection of intra- Meleney's synergistic
may require operative
abdominal organ gangrene Eradicating dead space
Contaminated Ex. PAT, LTI, Enterotomy intervention-- Good Surgical
Fournier's gangrene Removing devitalized tissues
(Class III) during bowel obstruction unroofing and technique
Gas gangrene Using drains,suture materials correctly
EIR: 3.4-13.2 % marsupialization or Keep fingernails short
Management: Resect Necrotizing fasciitis Other Preparations
splenectomy Remove hand accessories
Dirty or repair the diseased
(Class IV) Ex. Perforated diverticulitis, organ; debridement of
Necrotizing soft tissue Management:
necrotic, infected Secondary pancreatic Require immediate
infections tissue and debris, Sutures Monofilament sutures>braided sutures
infections surgical intervention
EIR: 3.1-12.8 % administration of plus administration of Aqueous Povidone-iodine
antimicrobial agents antimicrobial agents Antimicrobial Soaps Chlorhexidine
occur approximately
10- 15 % of patients
Tertiary microbial who develop severe
peritonitis pancreatitis with Drains Closed suction drains>Open drains
necrosis Optimal time: 60 min before
Antimicrobial
incision
Prophylaxis
MC agents: E faecalis Timing is very important
and faecium, S
epidermidis, C
albicans
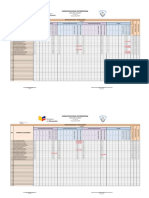
Biologic Warfare
SURGICAL INFECTIONS Incubation
Text Agents
1 to 6 days
Postoperative S/Sx malaise, myalgia, fever,
Bacillus anthracis respiratory distress, chest pain,
Nosocomial
Infection (Anthrax) diaphoresis, widened
mediastinum, pleural effusions
Microbiology of
Pathogenesis Treatment
Infectious Agents Ciprofloxacin,
Doxycycline,
Infection associated
Prolonged Amoxicillin,
with Indwelling
Bacteria Fungi Viruses Prevent microbial Postoperative UTI Mechanical Clindamycin,
goal Host Defenses intravascular
infection Ventilation Rifampin
catheters
Responsible for Identified Identified
initially by culture by the presence of Limit proliferation of
majority of surgical Barriers
and lastly by media at viral DNA or RNA microbes Incubation
infections Used for Prevention
different temperature using PCR Diagnosis Treatment Prevention 10 to 12 days
Contain or eradicate Nosocomial
Identified using Gram invading microbes Epithelial surface Mucosal surface > 10^4 CFU/mL in Pneumonia Physiological monitoring,
Polymicrobial full barrier precautions and
stain and culture for Cause nosocomial Adenovirus symptomatic Single Antibiotic for 3-5 immediate indwelling vascular access, drug
infections or fungemia Chlorhexidine skin prep
classification of infections in surgical Cytomegalovirus days catheter removal delivery, & hyperalimentation
bacteria C. albicans and Maintain sterility in S/Sx
patients Epstein-Barr Virus Integument >10^5 in asymptomatic malaise, fever, vomiting,
related species the distal bronchi and Respiratory Tract Urogenital, biliary, Gastrointestinal Tract Smallpox
Herpes Simplex Virus headache, centripetal rash
Varicella-Zoster Virus alveoli pancreatic, distal
Gram (+) Gram (-) respiratory tracts
Mucor Rare causes of Diagnosis Prevention
Chemical secretes by Vast number of
Rhizopus aggressive soft tissue Respiratory mucus Oropharynx
sebaceous gland microbes Treatment
Absidia infections traps larger particles,
Stained BLUE Stained RED/PINK Upper Respiratory No resident microflora Cidofovir
Microbes are held including microbes Purulent Sputum, elevated leukocyte immediate weaning of
Tract
and is cleared by Due to acidic, low- count, fever, chest X-ray abnormalities Mechanical Ventilator
Aspergillus fumigatus, coughing motility environment,
Constant shedding of
Aerobic skin Bacilli niger, terreus, and organisms are
Opportunistic epithelial cells
commensals Enterobacteriaceae other spp. routinely killed after Transmission
pathogens that cause
Contribute to a large Staphylococcus E. coli Blastomyces ingestion flea bites from
infection to Small particles are
percent of surgical aureus Klebsiella dermatitidis Lower Respiratory rodents
immunocompromised cleared by
site infection (SSIs) Staphylococcus pneumoniae Coccidioides immitis Blocks attachment Tract Stomach
host phagocytosis
pyogenes Serratia marcescens Cryptococcus and invasion of non Resident microflora Small numbers of
and epidermidis Enterobacter neoformans commensal microbes microbes populate
Citrobacter gastric mucosa S/Sx
Acinetobacter Sepsis Resistant Organisms Blood-Borne Pathogens Yersinia pestis painful enlarged lymph node,
Nosocomial (~102 to 103
infections in Enteric organisms Pseudomonas Gram (+) aerobic (Plague) fever, severe malaise
P. aeruginosa and microbes colony forming units
immunocompromised E. faecalis CFU/mL)
flourescens Genus
or chronically ill E. faecium
Stenotrophomonas Staphylococcus
patients Treatment
Streptococcus Treatment
Microbes populate Resuscitation Doxycycline,
Corynebacterium Treatment Streptomycin,
gastric mucosa endpoints
Propionibacterium Cellular Mechanisms 1st, 2nd, or 3rd Cephalosporins Aminoglycoside,
Enterococcus Terminal ileum (105 to 108 of resistance
Transmission of HIV
Carbapenem Fluoroquinolone,
E. coli colony forming units MAP: > 65mmHg
Broad-spectrum antibiotics Chloramphenicol
Enterobacteriaceae CFU/mL) UO: > 0.5 mL/kg/hr
Vasopressor Therapy
Candida albicans Normalization of Serum lactate
Prevention
Due to low oxygen,
static environment, Target site
modification Transmission
Facultative anaerobic there is exponential
microbes Aerobic microbes growth of microbes Universal Precaution Tick
Bacteriodes fragilis E. coli Anerobes:Aerobes
and ditasonis Enterobacteriaceae 100:1
Distal colon Changes in bacterial
Eubacterium E. faecalis
Fusobacterium and faecium permeability or S/Sx
Lactobacillus C. albicans antibiotic intake Francisella tularensis cough, pneumonia, enlarged
Feces microbes are (Tularemia) lymph nodes
Peptostreptococcus careful handling &
~1011 to 1012 CFU/g washing hands and
routine use of barriers disposal of sharp
other skin surfaces
instruments
activation of drug
efflux systems Treatment
Aminoglycoside,
Doxycycline,
Ciprofloxacin
drug deactivation
You might also like
- Batteries: Color Code For Schematic LinesDocument2 pagesBatteries: Color Code For Schematic LinesIsaac NewtonNo ratings yet
- Chronic Traumatic Encephalopathy.12Document21 pagesChronic Traumatic Encephalopathy.12wmtxbbNo ratings yet
- Two Storey Residential House PDF 5 PDF FreeDocument9 pagesTwo Storey Residential House PDF 5 PDF FreeRiowin GamboaNo ratings yet
- General Notes: Abbrevations: Symbols: Fire Protection:: Schedule of Equipments Vicinity MapDocument12 pagesGeneral Notes: Abbrevations: Symbols: Fire Protection:: Schedule of Equipments Vicinity MapHelios100% (1)
- Immune Mediated Myopathies.5Document22 pagesImmune Mediated Myopathies.5wahby khatir100% (1)
- Viral Transport in Plants - E. Waigman, M. Heinlein (Springer, 2007) 3540698426Document195 pagesViral Transport in Plants - E. Waigman, M. Heinlein (Springer, 2007) 3540698426GabrielNo ratings yet
- Floor Plan: India Exposition Mart, Greater Noida, NCR, IndiaDocument1 pageFloor Plan: India Exposition Mart, Greater Noida, NCR, IndiaManoj KumarNo ratings yet
- Master Rotation Plan (GNM 3Rd Year) 2019-2020: Aug SepDocument1 pageMaster Rotation Plan (GNM 3Rd Year) 2019-2020: Aug SepJyoti Prem Uttam100% (1)
- Retrofit Measures Interaction MatrixDocument1 pageRetrofit Measures Interaction Matrixbari116No ratings yet
- 14 AMF THERMATEX Aquatec ENDocument6 pages14 AMF THERMATEX Aquatec ENkajiru.qatarNo ratings yet
- 2040 - Cut-Off-Points - 2020 - 2021 of The Special Provision For Students Who Have Excelled in Extra Curricular Activities - New SyllabusDocument5 pages2040 - Cut-Off-Points - 2020 - 2021 of The Special Provision For Students Who Have Excelled in Extra Curricular Activities - New SyllabusGayanuka MendisNo ratings yet
- Systemic Lupus ErythematosusDocument1 pageSystemic Lupus ErythematosusKim BadillesNo ratings yet
- Course OF Study: University Grants Commission 14.08.2018Document4 pagesCourse OF Study: University Grants Commission 14.08.2018simo vonnerNo ratings yet
- E Poster - Idiopathic Spontaneous PneumothoraxDocument1 pageE Poster - Idiopathic Spontaneous PneumothoraxMuyiwa AremuNo ratings yet
- Un1529648 BDocument2 pagesUn1529648 BCB NitrideNo ratings yet
- ICU RehabilitationDocument10 pagesICU RehabilitationKarina Saldivia TecaNo ratings yet
- 1 Azad Nagar, Kanpur 2 Kidwai Nagar, Kanpur: Dr. Ajay Kumar Verma (Ms-Pipri - Up@esic - Nic.in)Document1 page1 Azad Nagar, Kanpur 2 Kidwai Nagar, Kanpur: Dr. Ajay Kumar Verma (Ms-Pipri - Up@esic - Nic.in)Ajay Kumar VermaNo ratings yet
- Mensual IessDocument67 pagesMensual IessdanielagranizoNo ratings yet
- Board - Conceptual SiteDocument1 pageBoard - Conceptual SiteRaizel CustodioNo ratings yet
- 47 Fsed 52bf Narofseiaasaofcfc For Business Operations Rev00Document1 page47 Fsed 52bf Narofseiaasaofcfc For Business Operations Rev00Trash 2No ratings yet
- DW M8推荐书Document6 pagesDW M8推荐书NAYAN PATELNo ratings yet
- CMTM FCD Ee 47Document1 pageCMTM FCD Ee 47carylNo ratings yet
- Plan SIMEM 2023 CATALOGUE Plan SIMEM 2023 1 1 PDFDocument1 pagePlan SIMEM 2023 CATALOGUE Plan SIMEM 2023 1 1 PDFzakaria abedNo ratings yet
- Kohort Dita PratDocument7 pagesKohort Dita PratFitria VarishaNo ratings yet
- Registros 2023 AmautasDocument23 pagesRegistros 2023 AmautasDiego EnriqueNo ratings yet
- Organigrama Final 166Document1 pageOrganigrama Final 166diablo2289No ratings yet
- Neurologic Complications of Lyme Disease: Review ArticleDocument11 pagesNeurologic Complications of Lyme Disease: Review ArticleHenry DanielNo ratings yet
- PDF Hoja de Registro Anestesico Gava CompressDocument2 pagesPDF Hoja de Registro Anestesico Gava CompressEDITH NATHALY CUMBAJIN PANELUISANo ratings yet
- Anxitatea Periop - Review - 2018Document11 pagesAnxitatea Periop - Review - 2018Fiorel Loves EveryoneNo ratings yet
- FinalDocument1 pageFinalaligamers70No ratings yet
- Digital BiogasTech2020Document25 pagesDigital BiogasTech2020kakangmasNo ratings yet
- Ef 025 Cidco PTR ST 109 FDocument1 pageEf 025 Cidco PTR ST 109 FAshok PalNo ratings yet
- Panasonic RR-US360 - Operating Instructions (English)Document2 pagesPanasonic RR-US360 - Operating Instructions (English)mivamoura100% (2)
- Maxillofacial Trauma in The Emergency Department: Pearls and Pitfalls in Airway ManagementDocument13 pagesMaxillofacial Trauma in The Emergency Department: Pearls and Pitfalls in Airway ManagementWahyuNo ratings yet
- Restaurant Risk MatrixDocument2 pagesRestaurant Risk MatrixScribdTranslationsNo ratings yet
- Areas of Study: Saturday, 20 November 2021Document1 pageAreas of Study: Saturday, 20 November 2021CINITA SATISH CSA CBENo ratings yet
- Angeline D. Alabastro, M.D.: CNS Pharmacology I: AntiepilepticsDocument10 pagesAngeline D. Alabastro, M.D.: CNS Pharmacology I: AntiepilepticsMiguel C. DolotNo ratings yet
- Osteoarthritis Concept MapDocument1 pageOsteoarthritis Concept MapJanselle H ArmaNo ratings yet
- Karlien Vanhouteghem, Annelies Aerssens, Dirk Ommeslag, Jerina Boelens, Steven Callens, Anne-Marie Van Den AbeeleDocument1 pageKarlien Vanhouteghem, Annelies Aerssens, Dirk Ommeslag, Jerina Boelens, Steven Callens, Anne-Marie Van Den AbeeleAfien MuktiNo ratings yet
- GVM ST300R User ManualDocument1 pageGVM ST300R User ManualPaco Jiménez BarbaNo ratings yet
- Unidad Educativa Fiscomisional: No. Nomina de AlumnosDocument9 pagesUnidad Educativa Fiscomisional: No. Nomina de AlumnosMayrita AlbanNo ratings yet
- Project GenesisDocument1 pageProject Genesisrobert28No ratings yet
- Nursing Care Plan: University of Tabuk Faculty of Applied Medical Science Department of NursingDocument3 pagesNursing Care Plan: University of Tabuk Faculty of Applied Medical Science Department of NursingZedoo AlmaroaaneNo ratings yet
- 1° Trim-Insumos Básica Media-1-1Document14 pages1° Trim-Insumos Básica Media-1-1Rina Lisbeth VeraNo ratings yet
- SIMON18012: Call Before You DigDocument1 pageSIMON18012: Call Before You DigBALAKRISHNANNo ratings yet
- LPT - Construction Contract AdministrationDocument22 pagesLPT - Construction Contract AdministrationAngela CalayoNo ratings yet
- Back Elevation 3 Side East Elevation 4: 3D ViewDocument1 pageBack Elevation 3 Side East Elevation 4: 3D ViewNgonidzashe ChirevaNo ratings yet
- 2021 RoadmapDocument2 pages2021 RoadmapSathia ShekarNo ratings yet
- M.4-1-201a - Mall Mechanical Services Chilled Water System Schematic DiagramDocument1 pageM.4-1-201a - Mall Mechanical Services Chilled Water System Schematic Diagramdiki anggriawanNo ratings yet
- WK.2 - CEBDLG20 - NBCP Section 301Document11 pagesWK.2 - CEBDLG20 - NBCP Section 301ThePepperManNo ratings yet
- Dela Cruz For Blueprint Checking 12-05-2022Document14 pagesDela Cruz For Blueprint Checking 12-05-2022Patrick Jerald CamilonNo ratings yet
- Seepage BEDs On Site Layout Plan-M-DE-A-012Document1 pageSeepage BEDs On Site Layout Plan-M-DE-A-012nimodi lankaNo ratings yet
- Nhs Bronchiolitis Pathway Acute Setting South East Coast SCNDocument2 pagesNhs Bronchiolitis Pathway Acute Setting South East Coast SCNdrgrizahNo ratings yet
- Evolution of RevolutionDocument1 pageEvolution of Revolutionalexa.2023120077No ratings yet
- (PIDST) - 391 - Pidst - 20111020114358 - Filejou 2Document20 pages(PIDST) - 391 - Pidst - 20111020114358 - Filejou 2Nareunart KongkaNo ratings yet
- SURG - BurnsDocument1 pageSURG - BurnsMikhail LamayoNo ratings yet
- Pneumonia Due To Animal or Environmental ExposureDocument1 pagePneumonia Due To Animal or Environmental Exposurefsdfsdf sdfsdfNo ratings yet
- Microbiology Homework Unit III N IVDocument7 pagesMicrobiology Homework Unit III N IVYazmin CoatlNo ratings yet
- Cub Badge SheetDocument1 pageCub Badge SheetguyrupertNo ratings yet
- Va Medica: Consensus Report Italiano Sul Trattamento Con Tossina Botulinica Per Uso EsteticoDocument13 pagesVa Medica: Consensus Report Italiano Sul Trattamento Con Tossina Botulinica Per Uso EsteticoEmiliano Prandelli100% (1)
- 3 s2.0 B9781455748013003301 MainDocument120 pages3 s2.0 B9781455748013003301 MainInzamam Ul HaqNo ratings yet
- Antigen-Antibody Reaction 1Document133 pagesAntigen-Antibody Reaction 1ShineeNo ratings yet
- Reverse Transcription and Polymerase Chain Reaction: Principles and Applications in DentistryDocument11 pagesReverse Transcription and Polymerase Chain Reaction: Principles and Applications in Dentistryinvestbiz optionstarNo ratings yet
- Articulo BiologíaDocument6 pagesArticulo BiologíaJulieta Juárez OchoaNo ratings yet
- Mulusew Proposal 2Document20 pagesMulusew Proposal 2Kalkidan Daniel100% (1)
- Mock Test (PhuongLinh12Anh2)Document5 pagesMock Test (PhuongLinh12Anh2)Linh HoàngNo ratings yet
- Frequently Asked Questions (Faqs) : What Is Malaria?Document3 pagesFrequently Asked Questions (Faqs) : What Is Malaria?Dummy1 AccountNo ratings yet
- Gens and Cardiovascular FunctionDocument264 pagesGens and Cardiovascular FunctionHimani PandyaNo ratings yet
- Pharm-Immuno 9-11 Cell Mediated Immunity: Dr. Saber HusseinDocument48 pagesPharm-Immuno 9-11 Cell Mediated Immunity: Dr. Saber Husseinmmoney1No ratings yet
- Science 2020Document96 pagesScience 2020ParadoxNo ratings yet
- HandHygiene AssessmentDocument2 pagesHandHygiene AssessmentAninditaNo ratings yet
- Antiviral Agents: Unit - 2 Pharmaceutical Chemistry - I (Advanced Medicinal Chemistry) Topic: Antiviral AgentsDocument20 pagesAntiviral Agents: Unit - 2 Pharmaceutical Chemistry - I (Advanced Medicinal Chemistry) Topic: Antiviral AgentsGunjan Kalyani100% (1)
- ACTIVIDAD INGLES Reading ComprehensionDocument3 pagesACTIVIDAD INGLES Reading Comprehensionyulis mesaNo ratings yet
- Introduction To Infection ControlDocument9 pagesIntroduction To Infection ControlLast YearNo ratings yet
- BK Case ReportDocument4 pagesBK Case ReportEngidaNo ratings yet
- Biotechnology Application BiohackDocument6 pagesBiotechnology Application Biohacksatyasamal676No ratings yet
- Coronavirus RNA Proofreading: Molecular Basis and Therapeutic TargetingDocument18 pagesCoronavirus RNA Proofreading: Molecular Basis and Therapeutic TargetingJose QuinteroNo ratings yet
- Reading-Subtcst A: InfluenzaDocument5 pagesReading-Subtcst A: InfluenzaPrasoon PremrajNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care PlanAnnahNo ratings yet
- Microorganisms From The Environment: Microbiology and Parasitology Lab Activity 6 Group 1Document11 pagesMicroorganisms From The Environment: Microbiology and Parasitology Lab Activity 6 Group 1ALDRISCHE TYRONNE TORIBIO JINGCONo ratings yet
- Compare Influenza and COVIDDocument1 pageCompare Influenza and COVIDntnquynhproNo ratings yet
- Week 4: Genetic Engineering and Its Applications in ReproductionDocument19 pagesWeek 4: Genetic Engineering and Its Applications in ReproductionDonna RemitarNo ratings yet
- MODULE 6 BiosafetyDocument10 pagesMODULE 6 BiosafetyLaurice Nicole ConcepcionNo ratings yet
- Assignment 2 Fermentation PDFDocument2 pagesAssignment 2 Fermentation PDFPhú NguyễnNo ratings yet
- A. Background and ObjectivesDocument10 pagesA. Background and ObjectivesAas HandayaniNo ratings yet
- Lab Report Exp 5Document5 pagesLab Report Exp 5Brilliant SiemaNo ratings yet
- A Short History of VaccinationDocument16 pagesA Short History of VaccinationAlejandro MotoliníaNo ratings yet
- Dairy Processing StagesDocument7 pagesDairy Processing StagesirfanilNo ratings yet
- Infectious CoryzaDocument9 pagesInfectious CoryzaPraveen KumarNo ratings yet