Professional Documents
Culture Documents
1P.1.Derm-Introduction To Dermatology
Uploaded by
Marlon BauagOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1P.1.Derm-Introduction To Dermatology
Uploaded by
Marlon BauagCopyright:
Available Formats
1P.
01
SEPTEMBER 04,2021
INTRODUCTION TO DERMATOLOGY
DR. KAREL HELDEN M. CLORES-DATOR
TOPIC OUTLINE Cells of the Epidermis
I. THE SKIN III. DERMATOLOGIC Cells Function
A. Layers of the skin EXAMINATION
Keratinocytes Produces keratin, a
1. Epidermis A. Cutaneous signs
2. Dermis 1. Primary lesions
complex filamentous
3. Hypodermis 2. Secondary protein that forms the
B. Skin appendages lesions surface coat of the
1. Sweat glands B. Diagnostic details epidermis, hair, and nails
2. Sebaceous of lesions Melanocytes Dendritic cell that
glands C. Documenting a produces melanin, (skin
3. Hair dermatologic exam pigmentation)
4. Nail IV. MEDICATIONS IN
5. Muscle DERMATOLOGY
Langerhans cells Recognition, uptake,
II. HISTORY TAKING V. REFERENCES processing and
A. General data presentation of antigens to
B. Chief complaint sensitized T lymphocytes,
and History of [Antigen presenting cells
present illness of the skin]
C. PMH Merkel Cells Act as slow adapting
D. Medication history
touch receptors
E. Allergies
F. Social History (mechanoreceptors)
G. Family history
Layers of Epidermis
I. THE SKIN
Heaviest single organ of the body > 15% of total
body weight
Functions:
o Protection
o Regulation of body temp [producing sweat
when hot]
o Metabolic Function
o Sense organ
Meissner corpuscle-light touch
Paccinian corpuscle-pressure
Free nerve endings-pain [palm and sole Stratum Corneum/ Horny Layer
mostly kya masakit pag nasugat] Outermost
Ruffini’s cells-heat Structureless, hydrated keratinized dead cells
Krause cells-cold flattened into horny plates which are continuously
sloughed off or desquamated [skin ngpapalit every 13
A. LAYERS OF THE SKIN days]
A1. EPIDERMIS [In dermatitis or any skin condition where there is
scaling that is the composed of stratum corneum]
Derived from ectoderm
Stratum Lucidum
Stratified squamous keratinizing epithelium
[Not always present in the cross section of skin, only
Cells:Keratinocytes(90%),Melanocytes,
found on the thick skin of palms and soles]
Langerhans cells, Merkel cells
Few layers of flattened closely compacted cells
Thickest: Palms and soles
Absent nuclei, increased amount of intercellular
substance, refractile droplets in the cytoplasm make it
look translucent
Seen only in thick skin (palms and soles)
[Mas homogenous color compare sa S. corneum]
Stratum granulosum
3 layers of flattened, rhombic cells with their long axis
parallel with the surface of the skin
Contain basophilic keratohyaline granules which are
rich in proline and sulfur containing amino acids [resp.
for CHON synthesis in the skin]
CABULAY, ELEPANIO, FLORES, MAMAUAG,PUNO Page 1 of 10
Stratum spinosum or prickle cell layer B.SKIN APPENDAGES
Polyhedral shaped keratinocytes with delicate
processes or spines projecting from their surfaces
Spines serve as intracellular bridges for attachment
and nutrient diffusion
[Seen in dermapathology in cases like dermatitis (cells
are separated from each other)]
Stratum basale
Lowermost single layer
Made up of columnar cells resting perpendicular to a
well- defined basement membrane
Highest mitotic activity Sebaceous gland produces sebum
1 melanocyte: 10 basal keratinocytes Apocrine gland produces sweat, both are attached to
Difference in skin color of different races is due to hair follicle.
quantity and quality if melanosomes and not due to Eccrine gland empties directly into the skin surface.
number of melanocytes
Pale skin: fewer, smaller, packaged B1. SWEAT GLAND
Dark skin: more melanosomes, larger, singly dispersed a. Eccrine gland
Small sweat glands found predominantly on
A2. DERMIS palms, soles and forehead
Derived from the mesoderm Functions for thermoregulatory control
Composed of dense, irregularly arranged connective Stimulus is heat
tissue b. Apocrine gland
Principal component: collagen (type I) Large sweat glands located in axilla, mammary
Provides mechanical support and vascular bed for glands, areola, genital area
metabolic exchange processes Apocrine sweat: odorless until it reaches the skin
Thickest at the base surface where it is altered by bacteria (when
acted upon by bacteria, responsible for the body
odor)
B2. SEBACEOUS GLANDS
Produces lipids that contribute to barrier function
Found all over the body except palms and soles
Largest concentration on the face and scalp –
“seborrheic areas” [even the chest and upper back]
Divided into 2 layers
o Papillary layer or sub epithelial layer
Superficial layer consists of loose connective
tissue with collagenous and elastic fibers, and
nervous papillae
o Reticular layer
Deeper, relatively thick layer consists of
coarse collagenous fibers [mas makakapal
ang collagen fiber]
A3. SUBCUTANEOUS TISSUE/HYPODERMIS/PANNICULUS
Consist mainly of adipose tissue B3. HAIR
Provides mobility Protection, regulation of body temperature
Thickest: abdomen and buttocks Stages of development
Thinnest: eyelids and scrotum [kaya manipis ang o Anagen – active growth phase; 85-90% of scalp
eyelids natin] hair
o Catagen – involution phase [stop in growth]
o Telogen – total arrest in growth
INTRODUCTION TO DERMATOLOGY Page 2 of 10
B4. NAIL History of surgical procedures
act to assist in grasping small objects and in Immunosuppression (esp. HIV or genital lesions)
protecting the fingertip from trauma Pregnancies (restrict medications)
Fingernails growth: 0.1 mm/day (4–6 months to Psychiatric disease (just evaluate by yourself)
replace a complete nail plate) History of blistering sunburns, exposure to arsenic or
Toenail growth: slower,12–18 months required to ionizing radiation (if suspecting CA) [how to quantify
replace the great toenail allergies? Wheal/ “pantal”]
D. MEDICATION HISTORY
Prescription
Over-the-counter medications
Vitamins and dietary supplements (may sometimes
cause hypersensitivity reactions)
Herbal remedies (if overdone, may aggravate erosion
of lesion)
E. ALLERGIES
B5. MUSCLES Medications
arrectores pilorum (erectors of the hairs) = Food
gooseflesh Environmental antigens
tunica dartos (or dartos) of the scrotum Contactants - can be elicited if patient have had
in the areolas around the nipples patch test before
F. SOICIAL HISTORY
hobbies and leisure activities
alcohol and tobacco use
illicit drug use
sexual history
dietary history
bathing habits [longer bathing time skin becomes
drier]
pets [consider pediculosis]
living conditions [e.g scabies]
II. HISTORY TAKING history of travel [e.g deep wounds- consider
cryptococcosis or histoplasmosis]
A. GENERAL DATA
G. FAMILY HISTORY
Age
Gender skin disease
Occupation [eg. Nurses always use gloves – consider atopy (atopic dermatitis, asthma, allergic rhinitis) –
contact dermatitis secondary to gloves] Atopic triad
skin cancer
B. CHIEF COMPLAINT AND HISTORY OF PRESENT ILLNESS
Duration [acute or chronic] III. DERMATOLOGIC EXAMINATION
Periodicity [time of the day it gets worse]
Evolution [first lesion that appeared, usually a vesicle or A. CUTANEOUS SIGNS
bulla] Primary lesion - original lesion
Location [arthropod bite – extremities] Secondary lesion - result of modification of primary
Symptoms (pruritus, pain, bleeding – malignancies lesions by regression, trauma or other factors
(SCC)
A.1. PRIMARY LESIONS
Severity [not so pruritic: psoriasis; very pruritic: atopic
1. MACULE
dermatitis]
Flat, non-palpable lesions <1 cm in diameter
Ameliorating and Exacerbating Factors [oil, pressure
Macules represent a change in color and are not
eg. Tinea infections mas lalong kumakati pag
raised or depressed compared to the skin surface
nakukulob]
Preceding illness, new medications, new topical
products, or exposures
Therapies tried, including over-the counter or home
remedies, and response to therapy [e.g use of
hydroquinone]
Prior similar problems, prior diagnosis, results of biopsies
or other studies performed [e.g psoriasis, scleroderma]
C. PAST MEDICAL HISTORY e.g Lentigo
chronic illnesses (diabetes, renal and hepatic disease, Decription: solitary, hyperpigmented macule
infection with HIV or hepatitis viruses, polycystic ovarian
syndrome, lupus, thyroid disease)
those that are associated with skin disease (asthma,
allergies)
INTRODUCTION TO DERMATOLOGY Page 3 of 10
2. PATCH 7. WHEAL [“Pantal” in Tagalog]
• Flat, non-palpable lesions >1 cm in diameter. Evanescent, edematous, plateau-like elevation of
• e.g Impetigo various sizes
Oval or arcuate contours, pink to red surrounded
by a flare of macular erythema that may be
discrete or coalesce [Appears when bitten by an
insect and you scratched it]
3. PAPULE
Elevated lesions <1 cm in diameter that can be felt
or palpated
e.g Molluscum contagiosum
8. VESICLE
• Circumscribed, small, clear, fluid-filled blister <1 cm
in diameter
• e.g. Herpes simplex or varicella
4. PLAQUE
Palpable lesions >1 cm in diameter that are
elevated or depressed compared to the skin surface
[Equivalent of patch but it is elevated]
9. BULLAE [Bigger version of vesicle]
• Circumscribed, small, clear, fluid-filled blister >1 cm
in diameter [Sometimes it can be hemorrhagic]
• When you touch it, it can be tense, fluctuant or
flaccid
Psoriasis - Erythematous plaque with white scales
5. NODULE
Firm papule or lesion that extend into the dermis or
subcutaneous tissue [If you touch the lesion, it is
deep into the dermis]
e.g Furuncle 10. PUSTULE [Very common]
Small elevations of the skin that contain purulent
material
e.g Folliculitis
6. TUMOR
Firm and freely movable or fixed masses of various
size and shape, generally are 2 cm in diameter
[Merkel cell carcinoma: rare carcinoma of the
skin] A.2. SECONDARY LESIONS
1. SCALES
Dry or greasy laminated masses of keratin
Fine, delicate, branny, coarse [Stratum corneum
that became thick is the one that is sloughing off]
INTRODUCTION TO DERMATOLOGY Page 4 of 10
Right upper Picture: White laminar scaling of
psoriasis (laminar means they peel in layers)
Lower picture: Tinea corporis – firm and delicate
Right lower Picture: Sebborheic dermatitis (yellowish
and greasy)]
2. CRUSTS
• Dried serum, pus or blood usually mixed with
epithelial or bacterial debris
Previously a bullae but it ruptured and the top of the
• Dry, golden yellow, soft, friable
bullae was removed
6. ULCERS
Rounded or irregularly shaped excavations that
result from complete loss of the epidermis plus
portions of the dermis & subcutis
Left picture: Impetigo contigiosa caused by S. aureus
that produces golden yellow crustings (initially there
can be papules and vesicles, that’s why it is important
to ask the patient the initial appearance of the lesion)
Right picture: Discoid lupus erythematosus Cause scarring because it reach the subcutaneous
(erythematous to hyperpigmented plaque with 7. SCAR
hemorrhagic crust) • Composed of new connective tissue that replaced
3. EXCORIATIONS AND ABRASIONS lost substance in the dermis or deeper parts as a
Punctate or linear abrasion produced by result of injury or disease, as part of the reparative
mechanical means [like sratching], usually process
involving the epidermis but not uncommonly
reaching the papillary layer of the dermis
Can be depressed (scars in acne vulgaris) or
elevated (hypertrophic scar and keloid)
Patients with atopic dermatitis can also present with Right picture: keloid from vaccination scar
excoriations as a secondary lesion, also those with Keloid can become very large and if it is on the
lichen simplex chronicus or those with chronic dermatitis chest due to acne, it can merge and form larger
can present with excoriations as a sign that the patient masses.
scratched the lesion.
4. FISSURES B. DIAGNOSTIC DETAILS OF LESIONS
Linear cleft through the epidermis or into the dermis Number – single, multiple, few (2-3 lesions)
May be single or multiple and vary from Distribution – generalized/localize, discrete/confluent,
microscopic clefts several centimeters in lengths group
with sharply demarcated margins Color – erythematous, hyper/hypopigmented
Configuration – annular, linear, serpiginous, targetoid
Primary lesion – macule, patch, papule, etc.
Secondary lesion- scale, crust, ulcer, etc.
Location – flexurals, extensors, sun-exposed, etc.
Diagnostic details of lesion are used to described
lesion.
These terminologies will be put together to be able
Heel fissures or cracked heel to form a complete dermatological physical
Usually happens because of a very dry skin examination
accompanied by pressure on the area
Common especially in the elderly
5. EROSIONS
Loss of all portions of the epidermis
May or may not become crusted, but it heals
without a scar [contrary to ulcer which heals with
scarring because it reaches the dermis]
INTRODUCTION TO DERMATOLOGY Page 5 of 10
1. Number
Solitary/multiple
1st picture: Solitary hyperpigmented papule
2nd picture: Multiple hyperpigmented papules Case of epidermal nevus following lines of blaschko
2. Distribution Epidermal nevus follows dermatomal and lines of
Generalized/localized blaschko
3. Evolution [Usually, it was not reported in the derma
physical exam]
Development from primary lesion to a secondary
lesion
Generalized – no need to put location of lesion
Localized – need to put location of lesion
Symmetrical/asymmetrical
1st picture: primary lesion – bullae and vesicle
2nd picture – bullae ruptured – formed crusts and
erosion (roof of bullae was removed exposing skin)
4. Involution [What happened to skin condition when it
heals]
Resolution - No marks at all, skin back to normal
Psoriasis with Symmetrical lesion after it heals
Symmetrical if you put a line in the midline, right Hyperpigmentation - Darkening of skin after skin
side is like left side. condition; Acne marks from acne vulgaris
Dermatomal
Hypopigmentation
o Skin with lesion is lighter than the normal skin
Can Happen when treated with topical
steroid
o Hypo/hyperpigmentation not permanent, go
back to normal within 6 months.
Dermatomal seen in herpes zoster, sometimes in
incontinentia pigmenti (rare congenital condition),
epidermal nevus.
Following lines of cleavage [Lines produce when
stand against gravity, and the skin sags]
Scar
Hypertrophic or keloidal
Pityriais rosea follows line of cleavage, triangular acne on the chest in keloid former
Christmas tree pattern individual.
Individual acne marks merge forming a
Lines of Blaschko [Embryonic in origin, not visible; large keloid.
Left by epidermal migration of the cells of the skin]
INTRODUCTION TO DERMATOLOGY Page 6 of 10
5. Configuration Guttate
Linear
Resembles line
Resembles water drops
Striae distensae / stretch marks
Guttate psoriasis
Description: erythematous to hyperpigmented
linear plaques Nummular
Annular
Circular lesion with central flaring
Resembles ring Also known as Discoid or Coin shape
Tinea corporis Circular lesion
Description: solitary annular erythematous Nummular dermatitis
plaque with scaling Description: solitary nummular erythematous plaques
with crust and scales
Arcuate
6. Color
Erythematous [Red]
Like annular but not complete circle
Erythema gyratum repens- a rare condition,
inflammatory skin condition associated to lesion of psoriasis
malignancy Violaceous
Description: multiple arcuate erythematous
plaques
Polycyclic
Picture above: Senile purpura seen in elderly
Skin of elderly are fragile when you put friction
can cause bruising
multiple annular lesions that are closed together Other conditions: lichen planus – present like
wheals of urticarial psoriasis with scales but violaceous
Description: multiple polycyclic erythematous Yellow
wheals
Serpiginous
Xanthelasma - Yellowish plaques over eyelids
(upper and lower)
Resembles snake Can also occur in other parts of the body, not
Cutaneous larva migrans (migration of hookworm usually appreciated
larva in the skin that leaves tract)
INTRODUCTION TO DERMATOLOGY Page 7 of 10
Salmon colored extravascular, or the RBCs are already
extravasated)
Lighter version of erythematous
Pityriasis rosasea
Hyperpigmented
8. TESTING FOR ANESTHESIA/HYPOSTHESIA
Dark
Pigmented Nevus
Hypopigmented Lesions [lesion that is lighter than
Tool used to assess sensation of the skin. The pins are
the color of the skin]
of different sharpness (pointed/dull) and thickness.
This is usually done if the patient is suspected of
having Leprosy or Hansen’s Disease
In lieu of this specific tool, tip of ballpen or pencil
can be used instead and assess the patient by
asking whether they can feel the sensation as blunt
(eraser part) or sharp (tip of the pencil/pen)
If the patient reported negative sensation, or even
diminished sensation (hyposthetic) it is a
Document as: Multiple, hypopigmented macules
characteristic of an anesthetic lesion (Hansen’s
and patches at the back
Disease or Leprosy)
Diagnosis: Pityriasis versicolor (an-an
Depigmented Lesions (devoid of pigment/no C. DOCUMENTING A DERMATOLOGIC EXAMINATION
melanin)
[combination of classifying the lesion]
1. Number (solitary or multiple)
2. Distribution (Generalized or Localized)
3. Configuration
4. Color
5. Primary lesion
6. Secondary lesion
7. Location (usually, when the lesion is generalized,
Document as: Multiple, depigmented patches on the localization can be omitted)
face SAMPLE DERMATOLOGIC DIAGNOSIS
Diagnosis: Vitiligo Diagnosis: Psoriasis
7. Consistency [Touching the lesion is not usually advised, Document as:
especially if the lesion is suspected to be infectious] Multiple, generalized, guttate,
Soft erythematous papules and
Firm or indurated plaques with whitish scaling
Often disregarded unless you are considering lesions Tinea corporis
like furuncles/nodules to assess whether these lesions Multiple, localized,
are fluctuant or not polycyclic/annular
erythematous plaques with
Dermoscopy [Done by using a glass slide and
scales on the left axilla
pressing it on top of the lesion]
o Blanching - if the lesion is erythematous but
not a vasculitis, the lesion will blanch
(meaning the erythema is intravascular)
o Non blanching - if the lesion is pressed but
retains its erythematous or violaceous color,
then it is vasculitis (the color of the lesion is
INTRODUCTION TO DERMATOLOGY Page 8 of 10
Vitiligo
Multiple, generalized, (no A particular potency is used for a certain part of
pattern=no configuration), the body
depigmented, patches (no Superpotent corticosteroids (Class I Steroids)
secondary lesion) o Clobetasol propionate
(generalized, therefore no o Halobetasol propionate
need to mention location) o Betamethasone diproprionate
Mid Potent Corticosteroid
o Betamethasone valerate
Psoriasis o Mometasone furoate (Elica)
Multiple, localized, (no o Fluocinolone acetonide
configuration), erythematous o Fluticasone propionate
papules and plaques with Least potent Corticosteroid
whitish scaling over the left o Hydrocortisone
hand Superpotent ones are used in atopic dermatitis
that are resistant (usually, atopic dermatitis
responds to mid potent corticosteroid)
Discoid lupus erythematosus and other dermatitis
IV. MEDICATIONS USED IN DERMATOLOGY – Class 1 corticosteroids
A. TOPICAL CORTICOSTEROIDS Least to mild potent are used in areas that are thin
[most commonly prescribed medication in skin (e.g. face, neck, axilla and inguinal area)
dermatology, almost all dermatologic conditions If the lesion is thick and it involves the thick skin like
respond to topical medications] palms and soles, extremities or trunk, superpotent
Reduces the symptoms of inflammation but may not corticosteroids may be used)
address the underlying cause of the disease DO NOT GIVE CLOBETASOL FOR LESIONS LOCATED
MOA: ON THE FACE FOR A LONG TERM (may be
o mediated by binding of the corticosteroid to its considered if the lesion is discoid lupus
receptor in the cytosol - translocation to the erythematosus)
nucleus at the corticosteroid response element -
inhibit transcription of inflammatory proteins B. SYSTEMIC ANTIHISTAMINES
Topical steroids are divided into groups based on their
MOA:
strengths:
o Inverse agonists that reversibly bind and stabilize
o strongest steroids are in group I
the inactive form of H1 receptor
o weakest steroids are in group VII
o Anti-pruritic effects
o important to know the potency of the medication
Classes
because it has different uses. A particular potency
1. First generation – not protein bound therefore can
is used in a certain part of the body
cross the BBB=Sedating)
Risks and precautions
Chlorphenamine
o Highly potent steroids should be used for short
Diphenhydramine
periods of time intermittently (2-3 weeks)
Hydroxyzine
o Do not stop immediately, taper it
2. Second generation – protein bound = cannot
o It should be avoided on ulcerated or atrophic or
cross BBB= non-sedating)
infected skin (may aggravate infection and
Cetirizine
atrophy)
Desloratidine
o Sudden discontinuation after prolonged use
Ebastine
should be avoided to prevent rebound
Levocetirizine
phenomena
Loratidine
o Superpotent topical steroids should be used with
Must know if you are giving a sedating or non-
caution in children and elderly as well as in thin
sedating antihistamine
areas of the skin such as the face and genital
C. ANTIBIOTICS
region
Complications 1. TOPICAL
o Acne (common) Used in impetigo, acne vulgaris, rosacea
o Atrophic changes, telangiectasia, purpura, easy Examples
bruising, striae formation (common in psoriasis px o Mupirocin ointment –[impetigo]
with continuously using steroid), ulceration MOA: inhibition of tRNA;
o Acneiform eruptions [common in COVID patients Used for G (+) infections such as
due to giving of systemic steroids] Staphylococcus sp.
o Hypertrichosis o Oxytetracycline ointment -[impetigo]
o Hypopigmentation MOA: inhibition of 30s ribosome;
o Development of infections For G (+/-) organisms
o Allergic reactions (most common: Budesonide) o Clindamycin gel - [acne vulgaris, rosacea]
o Systemic effects such as glaucoma and MOA: inhibition of 50s ribosome;
suppression of HPA axis.
INTRODUCTION TO DERMATOLOGY Page 9 of 10
For G (+) organisms such as
Propionibacterium acnes
2. SYSTEMIC
Skin infections are usually caused by
Staphylococcus and Streptococcus sp.
Examples:
o Cefalexin
Adults
- 250 and 500 mg tablets
- Q6
Pediatric
- 125mg/5mL or 250mg/5mL
- 20-50 mg/kg/ day
- Q6
o Cloxacillin
Adults
- 250 and 500 mg tablets
- Q6
Pediatric
- 125mg/5mL
- 50-100 mg/kg/day
- Q6
o Co-amoxiclav
Adults
- 375 and 625 mg tablets
- Q8 to Q12
Pediatric
- 156.25mg/5mL
- 40 mg/kg/day
- Q8
REFERENCES
1. Dator, K., Introduction to Dermatology. [powerpoint slides]
2. Sidenotes
INTRODUCTION TO DERMATOLOGY Page 10 of 10
You might also like
- Quick Study Guide To The Integumentary SystemDocument3 pagesQuick Study Guide To The Integumentary SystemMc Luis Glen AserdanoNo ratings yet
- The Integumentary System: Prepared byDocument12 pagesThe Integumentary System: Prepared byErick Torres Gozum100% (1)
- Lab Act 3 - Integumentary SystemdocxDocument8 pagesLab Act 3 - Integumentary SystemdocxmendozakaceeyNo ratings yet
- CH 5: Integumentary SystemDocument36 pagesCH 5: Integumentary SystemHurtlock HurtlockNo ratings yet
- Integumentary Lab ActDocument5 pagesIntegumentary Lab ActJASMINE LAURONNo ratings yet
- Burns SemDocument29 pagesBurns SemEsther Marie SazonNo ratings yet
- Journal Written Report - Scar Prevention With Prolonged Use of Tissue AdhesiveDocument13 pagesJournal Written Report - Scar Prevention With Prolonged Use of Tissue AdhesiveNeill CelesteNo ratings yet
- Integument System ActivityDocument5 pagesIntegument System ActivityeywatsarawatNo ratings yet
- Chapter 4 Integumentary SystemDocument5 pagesChapter 4 Integumentary SystemClarisse Anne QuinonesNo ratings yet
- SkinDocument22 pagesSkinloginhani40No ratings yet
- Topic 5 & 6Document18 pagesTopic 5 & 6PhoebeNo ratings yet
- Anatomy and Physiology of the Integumentary SystemDocument5 pagesAnatomy and Physiology of the Integumentary SystemVERGEL, Sophia Luis V.No ratings yet
- HUMAN ORGAN SYSTEMS: INTEGUMENTARY AND SKELETALDocument3 pagesHUMAN ORGAN SYSTEMS: INTEGUMENTARY AND SKELETALDenine Dela Rosa OrdinalNo ratings yet
- CH - 04 - SKIN AND BODY MEMBRANESDocument76 pagesCH - 04 - SKIN AND BODY MEMBRANESCheska DillupacNo ratings yet
- Skin Structure and FunctionsDocument25 pagesSkin Structure and FunctionsUniversal DiscoveringNo ratings yet
- Anaphy Mia Rev4Document4 pagesAnaphy Mia Rev4antonettevegamia3No ratings yet
- Anaphy Lab QuizDocument12 pagesAnaphy Lab QuizScout Beauty JHOINo ratings yet
- Anatomy & Physiology With Pathophysiology Lecture (Midterms)Document4 pagesAnatomy & Physiology With Pathophysiology Lecture (Midterms)Millen ArenasNo ratings yet
- Safari - Feb 21, 2024 at 11:56 AMDocument1 pageSafari - Feb 21, 2024 at 11:56 AMsyansyncNo ratings yet
- A&P Replaced Cheat SheetDocument6 pagesA&P Replaced Cheat SheetNihal AlamNo ratings yet
- Histology Department Medical Faculty Padjadjaran UniversityDocument40 pagesHistology Department Medical Faculty Padjadjaran Universityanisya venyNo ratings yet
- The Integumentary SystemDocument2 pagesThe Integumentary SystemKARYLLE JUNE PONTERASNo ratings yet
- IntegumentaryDocument5 pagesIntegumentaryNovie Roycell Fernandez RueloNo ratings yet
- Structure of Skin, Skin Problems, Hair Structure and Hair Growth CycleDocument8 pagesStructure of Skin, Skin Problems, Hair Structure and Hair Growth CycleRakshita GroverNo ratings yet
- Chapter 9: Skin and ITS APPENDAGES: (Vital Organs)Document4 pagesChapter 9: Skin and ITS APPENDAGES: (Vital Organs)Hannah Beatrice Adame TamayoNo ratings yet
- NeoNotes Derma HighlightedDocument32 pagesNeoNotes Derma Highlightedyomna.saaNo ratings yet
- Chapter 6: Integumentary SystemDocument12 pagesChapter 6: Integumentary SystemHoney VargasNo ratings yet
- 10 Patho Skin PathologyDocument27 pages10 Patho Skin PathologyMartin Tan100% (1)
- Activity 2 Part 1Document4 pagesActivity 2 Part 1Alejandra IndaNo ratings yet
- Workbook Activity #13: Integumentary System (Skin) General ObjectiveDocument5 pagesWorkbook Activity #13: Integumentary System (Skin) General ObjectiveAmbaw PutiiNo ratings yet
- Structure & Function of The SkinDocument9 pagesStructure & Function of The SkincNo ratings yet
- 5 - IntegDocument8 pages5 - IntegGel Austin PascuaNo ratings yet
- Skin and Its AppendagesDocument3 pagesSkin and Its AppendagesMarchylle Faye JimenezNo ratings yet
- Schwartz Cpap 16 Skin and Subcutaneous TissueDocument16 pagesSchwartz Cpap 16 Skin and Subcutaneous TissueRem AlfelorNo ratings yet
- Giải phẫu ứng dụngDocument54 pagesGiải phẫu ứng dụngDũng Hoàng Nghĩa TríNo ratings yet
- Integumentary System IncludesDocument29 pagesIntegumentary System IncludesRhena TogoresNo ratings yet
- 0.07 - 0.12 MM in Thickness But May Reach UpDocument8 pages0.07 - 0.12 MM in Thickness But May Reach UpCoy NuñezNo ratings yet
- Lai Cheong2013Document4 pagesLai Cheong2013Nirwana SeptianiNo ratings yet
- Activity 2 Part 1Document5 pagesActivity 2 Part 1Alejandra IndaNo ratings yet
- Chap3 Integ Anaphy NotesDocument11 pagesChap3 Integ Anaphy NotesAxel Neil VidalNo ratings yet
- Microscopic Analysis of The Integumentary SystemDocument9 pagesMicroscopic Analysis of The Integumentary SystemAgatha joy MadrazoNo ratings yet
- Integuementary System ReviewerDocument10 pagesInteguementary System ReviewerChloe Mikaela MonsantoNo ratings yet
- Anatomical Layers of The SkinDocument5 pagesAnatomical Layers of The SkinRyzelle Louise SorianoNo ratings yet
- Integumentary and Nervous System: 5141 CN 111 - Anatomy and PhysiologyDocument8 pagesIntegumentary and Nervous System: 5141 CN 111 - Anatomy and PhysiologyAlthea Joyce OngNo ratings yet
- Skin Appendages and FunctionsDocument24 pagesSkin Appendages and FunctionsChris Jardine LiNo ratings yet
- Intergumentary SystemDocument8 pagesIntergumentary SystemJSeasharkNo ratings yet
- Integumentary System (Lecture Outline) PDFDocument4 pagesIntegumentary System (Lecture Outline) PDFAndrea Yzabell CortezNo ratings yet
- PowerPoint - Presentation - About - Integumentary - SystemDocument27 pagesPowerPoint - Presentation - About - Integumentary - SystemPrayl Hope NapanoNo ratings yet
- Integumentary SystemDocument3 pagesIntegumentary SystemCarmela Cordon FelixNo ratings yet
- Integumentary System Epidermis Dermis: Stratum Corneum Stratum Lucidum Stratum Granulosum Papillary LayerDocument4 pagesIntegumentary System Epidermis Dermis: Stratum Corneum Stratum Lucidum Stratum Granulosum Papillary LayerNu Ri LeeNo ratings yet
- Structure and Function of the Skin ExplainedDocument9 pagesStructure and Function of the Skin Explainednh2411No ratings yet
- BM1011 2020 Study Guide For Module 3 The Integumentary SystemDocument14 pagesBM1011 2020 Study Guide For Module 3 The Integumentary SystemLaetitia ReyesNo ratings yet
- Skin and Its AppendagesDocument7 pagesSkin and Its AppendagesSheena PasionNo ratings yet
- Physical Assessment Final 1Document1 pagePhysical Assessment Final 1Shane ann BragaNo ratings yet
- Integumentary SystemDocument7 pagesIntegumentary Systemkuroko tetsuya100% (2)
- General Anatomy 1 With NotesDocument23 pagesGeneral Anatomy 1 With NotesCesar marquesesNo ratings yet
- Safari - Feb 21, 2024 at 11:49 AM 2Document1 pageSafari - Feb 21, 2024 at 11:49 AM 2syansyncNo ratings yet
- Reviewer Integumentary DigestiveDocument11 pagesReviewer Integumentary DigestiveMariah Alexa LibaoNo ratings yet
- (OB) 1.03 Maternal Physiology - Dr. QuilangDocument6 pages(OB) 1.03 Maternal Physiology - Dr. QuilangMarlon BauagNo ratings yet
- (OB) 1.02 Maternal Anatomy - Dr. DamasoDocument10 pages(OB) 1.02 Maternal Anatomy - Dr. DamasoMarlon BauagNo ratings yet
- Principles of Agglutination ReactionsDocument5 pagesPrinciples of Agglutination ReactionsMarlon BauagNo ratings yet
- Serological Test On Bacterial Infections-Streptococcal InfectionDocument5 pagesSerological Test On Bacterial Infections-Streptococcal InfectionMarlon BauagNo ratings yet
- Principles of Precipitation ReactionsDocument6 pagesPrinciples of Precipitation ReactionsMarlon BauagNo ratings yet
- Blood Flukes: Schistosomiasis JaponicaDocument6 pagesBlood Flukes: Schistosomiasis JaponicaMarlon BauagNo ratings yet
- Lung Fluke Disease: ParagonimiasisDocument4 pagesLung Fluke Disease: ParagonimiasisMarlon BauagNo ratings yet
- Principles of Precipitation Reactions-Part 2Document3 pagesPrinciples of Precipitation Reactions-Part 2Marlon BauagNo ratings yet
- (Pcol) 5.01 Chemotherapeutic DrugsDocument10 pages(Pcol) 5.01 Chemotherapeutic DrugsMarlon BauagNo ratings yet
- (PARA) 2.04 - Intestinal Flukes - Dr. AlvaradoDocument4 pages(PARA) 2.04 - Intestinal Flukes - Dr. AlvaradoMarlon BauagNo ratings yet
- (Pcol) Cancer ChemotherapyDocument23 pages(Pcol) Cancer ChemotherapyMarlon BauagNo ratings yet
- Basal Ganglia and Telencephalon AnatomyDocument11 pagesBasal Ganglia and Telencephalon AnatomyMarlon BauagNo ratings yet
- (PARA) 2.06 - Liver Flukes - Dr. AlvaradoDocument7 pages(PARA) 2.06 - Liver Flukes - Dr. AlvaradoMarlon BauagNo ratings yet
- Neuro 3.06 Neurologic Exam DR - CalimagDocument16 pagesNeuro 3.06 Neurologic Exam DR - CalimagMarlon BauagNo ratings yet
- NEURO 3.04 ANSLimbic System HypothalamusDocument10 pagesNEURO 3.04 ANSLimbic System HypothalamusMarlon BauagNo ratings yet
- How to Get a High Score on the OET Writing Sub-TestDocument6 pagesHow to Get a High Score on the OET Writing Sub-TestRosselini EspinedaNo ratings yet
- Klinik Utama Ilona Daftar ItemDocument12 pagesKlinik Utama Ilona Daftar ItemListia NingsihNo ratings yet
- Chapter IV - Dermatology: Common Skin Procedures BiopsyDocument6 pagesChapter IV - Dermatology: Common Skin Procedures BiopsyIndranil SinhaNo ratings yet
- No Product Name Qty: Berita Acara Uji FungsiDocument7 pagesNo Product Name Qty: Berita Acara Uji FungsiAditya-Oza PNo ratings yet
- Surgical Pathology of the Skin: Diseases and DisordersDocument11 pagesSurgical Pathology of the Skin: Diseases and DisordersPipoy Amy100% (1)
- Ask A Dermatologist Online For FreeDocument1 pageAsk A Dermatologist Online For FreeVispera HealthNo ratings yet
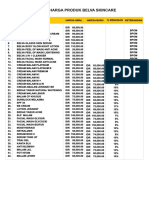
- Belva Skincare Product Prices ListDocument1 pageBelva Skincare Product Prices Listmas adiNo ratings yet
- qt5xd8t1t3 NosplashDocument3 pagesqt5xd8t1t3 NosplashDeb halderNo ratings yet
- Photographic Illustrations of Skin DiseasesDocument316 pagesPhotographic Illustrations of Skin DiseasessfranchiniNo ratings yet
- 10 Effective Homeopathic Medicines For Pityriasis Alba - DrHomeoDocument4 pages10 Effective Homeopathic Medicines For Pityriasis Alba - DrHomeoGer DersenNo ratings yet
- Rash Diagnosis Cheat Sheet: EmergencyDocument1 pageRash Diagnosis Cheat Sheet: Emergencykdlsfk kajjksolsNo ratings yet
- Fungal Skin Infections-1Document27 pagesFungal Skin Infections-1Fabb Nelson100% (1)
- Sunscreen PresentationDocument10 pagesSunscreen PresentationNurin Insyirah ShafieeNo ratings yet
- Disorders of Hair FollicleDocument41 pagesDisorders of Hair Folliclerejuven100% (2)
- Hair RemovalDocument28 pagesHair RemovalMARIALUPE ESTOQUENo ratings yet
- 15 Amazing Benefits of Beeswax for Skin HealthDocument8 pages15 Amazing Benefits of Beeswax for Skin HealthInspire NationsNo ratings yet
- Understanding Burn DegreesDocument2 pagesUnderstanding Burn DegreesAnu TripathiNo ratings yet
- Fitzpatricks Dermatology 9th Edition 3121Document1 pageFitzpatricks Dermatology 9th Edition 3121DennisSujayaNo ratings yet
- Doctor LLLLL 4Document54 pagesDoctor LLLLL 4loveNo ratings yet
- Daftar Harga CV FaeysaDocument4 pagesDaftar Harga CV FaeysaMo Kas Ku GarageNo ratings yet
- Skin Cancer Types, Risk Factors, Diagnosis & TreatmentDocument53 pagesSkin Cancer Types, Risk Factors, Diagnosis & TreatmentMohammadSAL-RawashdehNo ratings yet
- Heat Rash Prickly Heat Customer Version V2Document4 pagesHeat Rash Prickly Heat Customer Version V2Fitri 1997No ratings yet
- Nimisha Parekh's Narayani Remedies ExcerptDocument3 pagesNimisha Parekh's Narayani Remedies ExcerptFaomix de la House0% (1)
- Rosacea Fulminans Triggered by High-Dose Vitamins B6 and B12Document2 pagesRosacea Fulminans Triggered by High-Dose Vitamins B6 and B12PlantBasedNutritionNo ratings yet
- Dermatology 2010 2011Document28 pagesDermatology 2010 2011Qasim HaleimiNo ratings yet
- Treatment of PsoriasisDocument2 pagesTreatment of PsoriasisB.R SinghNo ratings yet
- Dermoscopy Guide Skin Cancer Non-MelanomaDocument63 pagesDermoscopy Guide Skin Cancer Non-MelanomaZain ButtNo ratings yet
- PL Jastiper MSBB JXB (Excel)Document3 pagesPL Jastiper MSBB JXB (Excel)Milou BeatriceNo ratings yet
- Pityriasis AlbaDocument6 pagesPityriasis AlbaLee Eng SiangNo ratings yet
- GROUP 2 Turmeric Facial SoapDocument3 pagesGROUP 2 Turmeric Facial SoapG20 Sumibcay FionaNo ratings yet