Professional Documents
Culture Documents
Clinpara Lec M2
Uploaded by
eumhir7Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinpara Lec M2
Uploaded by
eumhir7Copyright:
Available Formats
Clinical Parasitology (Lec)
MODULE 2: Nematodes
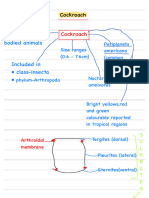
Taxonomic Classification
M
● ale (right) vs Female (left)
● The spicule allow the male worms to latch on to the
ETAZOANS
M females
- Eukaryotic multicellular organisms: have body
systems Classification of Adult Female Worms
- Kingdom Animalia.
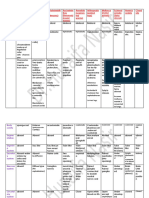
- Lays eggs in unsegmented stage
- Bilaterally symmetrical: left and right parts of the
(unembryonated); eggs need to
body are the same
OVIPAROUS develop when released in soil
- They show division of labour: have males and
- “HAT”: Hookworm, Ascaris,
females
Trichuris
- Cells lack a cell wall
- L ays eggs in segmented stage
NEMATODES (ROUNDWORMS) (embryonated); usually causes
OVOVIVIPA-
autoinfection
ROUS
orphology
M - “ES”: Enterobius vermicularis,
● Have elongated, cylindrical,unsegmented bodies Strongyloides stercoralis
tapering on both ends VIVIPAROUS/ - L
ays full developed larva
● Sexes are separated (dioecious) LARVIPAROUS - All tissue nematodes
● With definite antero-posterior axis (imaginary line
that separates the worm)
● Complete digestive & reproductive system; no hemoreceptors
C
circulatory and respiratory system - Uses sensory organs, no eyes and ears, to detect
chemical signal around them
- Cephalic chemoreceptors (all
AMPHID nematodes have amphid)
- At the anterior (mouth region)
- C audal chemoreceptors (all
nematodes have phasmid EXCEPT:
HASMIDS
P “TCT”- Trichuris-Capillaria-
Trichinella (aphasmids)
- At the posterior (tail region)
ife cycle
L
● Morphological Forms (Eggs → Larvae → Adult)
● Host requirement: Homoxenous (1 host only) &
Heteroxenous (2 or more host)
● Host requirement: Direct & Indirect
Irish Sabile 1
Habitat OVA EXAMINATION
Intestinal tract of man, tissues &
Main Habitat
other sites
Heart to Lung SH - Ascaris, Strongyloides,
A
Migration Hookworms
Animal as Natural
no maturity in the human body
Hosts
Intestinal Roundworms
Tissue & Extra-Intestinal Roundworms
DULT GROSS EXAMINATION
A
● Elongated, cylindrical bodies with
hape &
S
tapered ends
Color
● Whitish or pinkish worms
Cuticle ● with visible fine striations
INTESTINAL ROUNDWORMS (PHASMIDS) Mouth ● Triangular, trilobate lips
M
● ales: 10-31 cm, curved posterior ends
SCARIS LUMBRICOIDES
A Sexes ● Females: 22-35 cm, straight posterior
- the most common & largest intestinal nematode ends
- AKA“giant roundworm” “large intestinal roundworm”
Mouth ● Triangular, trilobate lips
“Eelworm”
- soil-transmitted helminth (STH)
- Produces PI-3 (Pepsin Inhibitor 3 = prevents it from
being digested) & phosphorylcholine (prevents
lymphocyte proliferation, mechanical protection)
- Forms: Egg/ova → Larva → Adult
IFE CYCLE
L
● MOT: Ingestion of embryonated eggs
Habitat: Small intestine (“C-NASA”)
●
● Infective stage: Embryonated eggs
ClinPara Lec M2 2
● D iagnostic stage: Adult worms, Fertilized & ethods
M
Unfertilized egg 1. Direct Fecal Smear
● Humans are the ONLY definitive host 2. Kato Katz & Kato Thick: preferred since more stool
● No intermediate host sample is analyzed
3. Concentration techniques
● Formalin-ether/ ethyl acetate concentration
technique
TREATMENT
ntihelminthic drugs(prevent the uptake of glucose
A
by the parasite = no energy)
1. Albendazole (400 mg single dose)
2. Mebendazole (500 mg single dose)
ATHOGENESIS AND CLINICAL MANIFESTATIONS
P 3. Pyrantel pamoate (10 mg/kg single dose)
● Ascariasis (“Sandbox Infection”)
● Pulmonary = Ascaris pneumonitis, Loeffler’s PREVENTION
Syndrome
● Intestinal = Pot belly, Ascaris bolus (obstruction) WASHED Framework
● Extra-intestinal = Biliary ● Access to potable water
ascariasis, acute appendicitis ● Drainage and disposal/re-use/
Water
or pancreatitis, acute recycling of household wastewater
peritonitis (also referred to as gray water)
● A ccess to safe and sanitary
SCARIS PNEUMONITIS
A sanitation facilities
- Due to larval migration as they enter the air sacs ● Safe collection, storage, treatment,
causing immune hypersensitivity anitation
S
and disposal (feces and urine)
- Initial symptoms: difficulty of breathing, fever, ● Management/re-use/recycling of
eosinophilia solid waste
- Severe: dyspnea, dry productive cough, X-ray
scattered infiltration, ● A ppropriate information regarding
- occasional hemoptysis prevention and treatment of STH
infections
OEFFLER’S SYNDROME
L ● Dissemination of key messages to
promote the following practices:
- Symptoms: Hygiene
a. Safe water storage
1. Marked eosinophilia + pneumonitis Education
b. Safe handwashing and bathing
2. Mild respiratory symptoms
practices
3. Transient migratory pulmonary infiltrates
c. Safe treatment of foodstuffs
d. Latrine use
OT BELLY/ASCARIS BOLUS
P
e. Use of footwear
- Obstruction of adult worms in the intestine
- Common complaint: vague abdominal pain ● R
egular mass drug administration
Deworming
- Moderate infections: lactose intolerance and (twice a year for school-age children)
vitamin A malabsorption
- Heavy infections: bowel obstruction, EPIDEMIOLOGY
intussusception, bowel infarction and intestinal ● G eographical distribution: Cosmopolitan but occurs
perforation. more in tropical regions (Southeast Asia, Africa,
Central & South America)
XTRA-INTESTINCAL ASCARIASIS
E ● Age Group: Children ages 5 to 15 years have the
- Biliary ascariasis, acute appendicitis or pancreatitis, highest intensities of infection
acute peritonitis ● 1.2 billion individuals are infected, (70% from Asia)
● 2,000 die annually
LABORATORY DIAGNOSIS
pecimen
S
● Stool, sputum, duodenal aspirate
ClinPara Lec M2 3
NTEROBIUS VERMICULARIS
E PATHOGENESIS AND CLINICAL MANIFESTATIONS
- “Pinworm”,“Seatworm”
- Old Name:Oxyuris vermicularis NTEROBIASIS - PRURITUS ANI
E
- Nocturnal parasite ● Perianal itching
- Causative agent of Pruritus ani (perianal itching) ● Other Symptoms: insomnia, restlessness, poor
appetite, weight loss, irritability, grinding of teeth, &
VA EXAMINATION
O abdominal pain
● Asymmetrical, with one side flattened and the other ● Cases are more common on children
side convex (“D shaped”) ● Familial disease
● Translucent shell consists of: ● Autoinfection is possible
● outer triple albuminous covering
● inner embryonic lipoidal membrane LAB DIAGNOSIS
pecimen:
S
● Eggs on perianal
region, stool (adults &
ova)
ethods
M
LARVA & ADULT EXAMINATION 1. Direct Fecal Smear
2. Graham’s Scotch Tape
dult
A Swab
● Cuticular alar expansions (cephalic alae)
● Esophageal bulb
● Male→ 2-5 mm, w/ curved tail and
a single spicule
● Female → 8-13 mm, w/ long
pointed tail
TREATMENT
M
● ebendazole (100 single dose)
arva
L ● Albendazole (400 mg PO single dose)
● has the characteristic esophageal bulb, but has no ● Pyrantel pamoate
cuticular expansion on the anterior end
revention
P
LIFE CYCLE ● Personal cleanliness and personal hygiene
● M OT: Ingestion of embryonated eggs (fecal-oral ● WASHED framework
route), inhalation, retroinfection
● Habitat: Large intestine (E.T) EPIDEMIOLOGY
● Infective stage: Embryonated eggs ● O ccurs in both temperate and tropical regions of
● Diagnostic stage: Eggs on perianal folds the world
● Humans are the ONLY definitive host ● The only intestinal nematode infection that cannot
● No intermediate host be controlled through sanitary disposal of human
feces
● 208.8 million infected persons in the world
● Locally, prevalence is consistently higher in
females(16%)compared to males (9%). Eggs were
found in nail clippings of school children.
ClinPara Lec M2 4
OOKWORMS
H ADULT MALE HOOKWORM
● Necator americanus: New World Hookworm,
American murderer ale copulatory bursa
M
● Ancylostoma duodenale: ● N. americanus →
Old World Hookworm, Bipartite: fused &
Germ of Laziness barbed spicules
● Soil-transmitted helminths ● A. duodenale → Tripartite: unfused & not barbed
● Blood-sucking nematodes spicules
OVA EXAMINATION
S
● ame for all species
● bluntly rounded ends
● single thin, transparent
hyaline shell
● “Morula ball” (2-8 cell
stages
LARVAE EXAMINATION
HOOKWORM ADULT BUCCAL CAPSULE
arvae/Juvenile Worms
L
● Rhabditiform Larvae &
Filariform Larvae
● difficult to differentiate
habditiform Larvae(L1)
R
● feedingstage
● long oral cavity (buccal
cavity/capsule)
● Small genital primordium
ilariform Larvae (L3)
F
● infective, nonfeeding
stage
● shorter esophagus
● pointed tail
uccal Spears
B
● N.americanus → conspicuous and parallel
throughout their lengths
● A. duodenale → inconspicuous buccal spears and
transverse striations on the sheath in the tail region
ADULT GROSS EXAMINATION
LIFE CYCLE
M
● OT: Skin penetration of filariform larva
● Habitat: Small intestine
(“C-NASA”)
● Infective stage:
Filariform larva (L3)
● Diagnostic stage:
Egss, adults, larvae
● Humans are the ONLY
definitive host
● No intermediate host
ClinPara Lec M2 5
PATHOGENESIS AND CLINICAL MANIFESTATIONS REVENTION
P
● Access to potable water
NTRY SITE
E ● Drainage and disposal/re-use/
● Maculopapular lesions, localized erythema Water
recycling of household wastewater
● S/S: Itching, edema, erythema, and later (also referred to as gray water)
● papulovesicular eruptions
● “Dew itch” “Ground itch” ● A ccess to safe and sanitary
sanitation facilities
ULMONARY
P ● Safe collection, storage, treatment,
anitation
S
and disposal (feces and urine)
● Loeffler’s Syndrome
● Management/re-use/recycling of
● Symptoms
solid waste
1. Marked eosinophilia + pneumonitis
2. Mild respiratory symptoms ● A ppropriate information regarding
3. Transient migratory pulmonary infiltrates prevention and treatment of STH
● Cases are rare in the tropics infections
● Dissemination of key messages to
INTESTINAL promote the following practices:
Hygiene
● Always chronic f. Safe water storage
Education
● S/S: abdominal pain, steatorrhea, diarrhea with g. Safe handwashing and bathing
blood and mucus, eosinophilia practices
h. Safe treatment of foodstuffs
UE TO BLOOD LOSS:
D i. Latrine use
● “Iron Deficiency Anemia” = main pathology j. Use of footwear
● “Hypoalbuminemia” ● R
egular mass drug administration
Deworming
(twice a year for school-age children)
LABORATORY DIAGNOSIS
EPIDEMIOLOGY
pecimen
S
● G eographical distribution: Tropical and subtropical
● Stool, sputum, duodenal aspirate
countries
● Age Group: Farmers, paramilitary personnel,
ethods:
M
indigenous and school children
1. Direct Fecal Smear
● 576 to 740 million are infected, (50,000 deaths due
2. Kato Katz & Kato Thick
to anemia)
3. Concentration Techniques
● Zinc sulfate floatation
● Formalin-ether/ethyl acetate concentration STRONGYLOIDES STERCORALIS
4. Harada Mori CultureTechnique: for the visualization A
● KA “Threadworm”
of larva ● “Smallest intestinal nematode”
(1-2.2mm by 0.4mm)
● Soil-transmitted helminth (STH)
acultative nematode: (changes
F
depends on their need)
● Parasitic female only: small intestine
● Free-living male & female: soil
OVA EXAMINATION
W
● ith clear thin shell
● Similar to those of
hookworms except that
TREATMENT they measure only
about 50 to 58 μm by
ntihelminthic drugs
A 30 to 34 μm. (smaller)
1. Albendazole (400 mg single dose) ● “Chinese lantern ova”:
2. Mebendazole ( 500 mg single dose) causes Cochin-China Disease
3. Pyrantel pamoate (10 mg/kg single dose)
ClinPara Lec M2 6
FREE-LIVING LARVAE EXAMINATION PULMONARY STRONGYLOIDIASIS
○ Due to larval migration causing destruction and
systemic hypersensitivity
● Lobar pneumonia with hemorrhage
○ One or 2 lobes in the lungs are affected
○ Symptoms: blood in lungs, cough, tracheal
irritation, hemoptysis (blood in stool)
● Loeffler's Syndrome
○ Symptoms
1. Marked eosinophilia + pneumonitis
● genital primordium = immature sex organs 2. Mild respiratory symptoms
3. Transient migratory pulmonary infiltrates
PARASITIC/FILARIFORM FEMALE
● S ize & Appearance: 2.2 mm by 0.04 mm, colorless, INTESTINAL STRONGYLOIDIASIS
semi-transparent, with a finely ● Adult female worms reside in duodenum & jejunum
striated cuticle (outer covering, ● Moderate S/S: diarrhea alternating with
skin) constipation
● Anterior: slender tapering ● Heavy infection (Cochin-China Diarrhea)
anterior end ○ painless, intermittent diarrhea
● Buccal cavity: Short with four ○ episodes of watery and bloody stools
indistinct lips
● Posterior: short conical pointed tail YPERINFECTION
H
● accelerated autoinfection
FREE LIVING MALE & FEMALE ADULT WORM ● occurs in immunocompromised px (people living
with AIDS, people of old age, children especially
ree Living (Female)
F newborns)
● smaller than the parasitic female ● mix of pulmonary & gastrointestinal symptoms
● muscular double-bulbed esophagus ● Inc. larvae in stool & sputum
● intestine is a straight cylindrical tube
HRONIC STRONGYLOIDIASIS
C
ree Living (Male)
F ● intermittent vomiting, diarrhea, constipation, and
● smaller than the females borborygmi, anal pruritus, urticaria, and larva
● has a ventrally curved tail currens rashes
● two copulatory spicules ● Recurrent asthma and nephritic syndrome
● gubernaculum
● not usually identified LABORATORY DIAGNOSIS
LIFE CYCLE pecimen:
S
M
● OT: Skin penetration of filariform larva ● Stool, sputum, urine,
● Habitat: Small intestine duodenal aspirate (Beale’s
(“C-NASA”) String Test)
● Infective stage:
Filariform larva (L3) ethods:
M
● Diagnostic stage: 1. Direct Fecal Smear
Rhabditiform larvae 2. Concentration techniques
● Humans & Dogs are - separates fecal debris from parasites
the definitive hosts ● Sedimentation= uses lower specific gravity
● No intermediate host solution (e.g. Ethyl acetate) against an
increased specific gravity of parasite
PATHOGENESIS AND CLINICAL MANIFESTATIONS ● Floatation= uses higher specific gravity
against an decreased specific gravity
TRONGYLOIDIASIS/ENTRY SITE
S ● Baermann funnel gauze method (Sedimentation
● due to larval invasion of the skin technique)
● S/S: erythema (reddening of the skin), pruritic 3. Modified Harada Mori Culture Technique
elevated hemorrhagic papules (itchy and bloody) 4. Nutrient Agar Plate Technique
5. Serologic Testing (serum)
ClinPara Lec M2 7
eale’s String Test
B emale
F
- Done when the patient cannot defacate ● 35 to 50 mm long
- The patient swallow the capsule with the string ● blunt posterior end
attached at the cheek
- The capsule absorbs the fluid for analysis oth
B
● attenuated anterior three-fifths traversed by a
TREATMENT & PREVENTION narrow esophagus resembling a string of beads
● robust posterior two-fifths contain the intestine and
ntihelminthic drugs
A a single set of reproductive organs
1. Albendazole
2. Thiabendazole
3. Ivermectin
revention
P
● WASHED Framework
EPIDEMIOLOGY
● C osmopolitan distribution (tropics & subtropical, IFE CYCLE
L
europe, USA)
● MOT: Ingestion of embryonated egg
● 50 to 100 million people affected ● Habitat: Large intestine (“E.T”)
● Rare in the Philippines ● Infective stage: Embryonated egg
● Age Group: more common on male children 7 to 14 ● Diagnostic stage:
years old Unembryonated egg,
adults
actors that affect transmission
F ● Humans are the
● poor sanitation definitive hosts
● indiscriminate disposal of human feces ● No intermediate host
● Autoinfection (>30 years)
L
● 1 = mitosis (2 cells)
INTESTINAL ROUNDWORMS (APHASMIDS) ● L2 = cleavage
● L3 = infective stage
RICHURIS TRICHIURA
T
● “Trichocephalus trichiurus” PATHOGENESIS AND CLINICAL MANIFESTATIONS
● AKA “whipworm”
● Aphasmid: no caudal INTESTINAL TRICHURIASIS
chemoreceptors ● Light Infection(<5,000 eggs per gram of stool)
● Soil-transmitted helminth (STH) ○ petechial hemorrhages: due to adult worms
● Secrete TT47 (released to help ○ predisposed to amebic dysentery (collab with E.
them attached to the intestinal mucosa) histolytica)
○ mucosa is hyperemic (bloody) and edematous
OVA EXAMINATION (inflammation); enterorrhagia (intestinal
B
● arrel, lemon-shaped w/ bipolar hyaline plugs bleeding) is common
● Yellowish outer and a ● Heavy Infection(>5,000 eggs per gram of stool)
transparent inner shell ○ Trichuris Dysentery Syndrome
● Fertilized eggs are ○ chronic dysentery and rectal prolapse
unsegmented at ○ S/S: blood
oviposition (3,000- streaked
10,000 per day) diarrheal
● “Japanese lantern ova” stools,
abdominal
ADULT WORM EXAMINATION pain and
tenderness,
ale
M nausea &
● 30 to 45 mm (shorter) vomiting, weight loss
● Coiled posterior with a single spicule and retractile ○ Anemia (blood loss of 0.8-8.6 mL per day)
sheath
ClinPara Lec M2 8
LABORATORY DIAGNOSIS ADULT WORM EXAMINATION
A
● nterior: thin filamentous
pecimen
S ● Posterior: slightly thicker and
● Stool shorter
● Esophagus: has rows stichocytes
ethods
M (stichosome; unicellular cells that
1. Direct Fecal Smear produces granules for detecting
2. Kato Katz & Kato Thick chemical signals around their
3. Concentration techniques body)
● Formalin-ether/ethyl acetate concentration
technique ale
M
● FLOTAC ● 1.5 to 3.9 mm in length
● male spicule is 230 to 300 μm
long and has an unspined sheath
emale
F
● vulva in females is located at the junction of
anterior and middle thirds
LIFE CYCLE
TREATMENT & PREVENTION ● M OT: Ingestion of infective larvae through
undercooked fish
ntihelminthic drugs
A ● Habitat: Small intestine
1. Mebendazole (100mg (2) for 3 days) (C-NASA)
2. Albendazole ● Infective stage: Infective
larvae
revention
P ● Diagnostic stage:
● WASHED Framework Unembryonated egg,
adults
EPIDEMIOLOGY ● Birds are the definitive
● T emperate and tropical countries but is more widely hosts
distributed in warm, moist ● Humans are incidental
areas of the world hosts
● 604 to 795 million people ● Freshwater fishes are intermediate hosts (Ipon,
affected Birot, Bagsang, Bagtu)
● Age Group: children 5 to
15 years of age PATHOGENESIS AND CLINICAL MANIFESTATIONS
● Co-infection with Ascaris
(19.1%); found in the INTESTINAL CAPILLARIASIS
same stool sample ● “Mystery Disease” = not well documented
● Abdominal pain, diarrhea & borborygmi (gurgling
sound of the stomach)
APILLARIA PHILIPPINENSIS
C
● S/S: intermittent diarrhea, weight loss, malaise
● AKA “pudoc worm”; first discovered in Barangay (uneasy, irritable), anorexia, vomiting, and edema
Pudoc, Ilocos
● First reported by Chitwood et al. in 1963 in a 29 ab Findings
L
year old male from Northern Luzon 1. Severe protein-losing enteropathy and
● Aphasmid: no caudal hypoalbuminemia
chemoreceptors 2. Malabsorption of fats & sugars
● Acquired through eating 3. Dec. excretion of xylose
undercooked fish 4. LowK,Na,Ca
5. High IgE
OVA EXAMINATION
s
● imilar to those of Trichuris trichiura but smaller LABORATORY DIAGNOSIS
● Guitar, peanut-shaped with striated shells and
flattened bipolar plugs pecimen
S
● Stool, duodenal aspirate
ClinPara Lec M2 9
ACRONYMS
ethods
M
1. Direct Fecal Smear viparous: HAT (pabebe worms)
O
2. Concentration techniques (FECT) ● Hookworm
3. Sandwich enzyme-linked immunosorbent assay ● Ascaris lumbricoides
(ELISA): fastest ● Trichuris trichiura
TREATMENT & PREVENTION voviviparous: ES
O
● Enterobius vermicularis
reatment
T ● Strongyloides stercolaris
● mebendazole (200 mg twice a day for 20 days)
● albendazole (400 mg may be given once daily for
10 days) In Small intestine: C-NASA
● For severe cases: give electrolyte replacement and ● Capillaria philippinensis
a high protein diet ● Necator americanus
● Ancylostomo duodenale
revention
P ● Ascaris lumbricoides
● WASHED framework
In Large intestine: ET
PIDEMIOLOGY
E ● Enterobius vermicularis
● Location: Pudoc West, Tagudin, Ilocos Sur (19666) ● Trichuris trichiura
● 1967 to 1990: 2,000 cases
● “Mystery Disease”: Monkayo, Compostela Valley y Egg Ingestion: ATE
B
Province outbreak (1998) ● Ascaris lumbricoides
● Thailand, Iran, Japan, Indonesia, United Arab ● Trichuris trichiura
Emirates, South Korea, India, Taiwan, Egypt, and ● Enterobius vermicularis
Lao People’s Democratic Republic
auses Autoinfection: Cool CHEST
C
● Capillariasis
LIFE CYCLE SUMMARIES ● Cryptosporidium
● Hymenolepis nana
scaris lumbricoides
A ● Enterobius vermicularis
● Small intestine → bloodstream → liver → heart → ● Strongyloides stercolaris
trachea ● Tenia
nterobius vermicularis
E
● Large intestine → perianal region
ookworms
H
● Skin → small intestine → bloodstream → lungs →
trachea → small intestine to develop
trongyloides stercolaris
S
● Skin → bloodstream → small intestine → lungs →
trachea → small intestine to develop
richuris trichiura
T
● Small intestine → intestinal wall → large intestine
→ feces
apillaria philippinensis
C
● Eggs → fish (larvae) → small intestine (adult)
ClinPara Lec M2 10
You might also like
- Animal Kingdom-Phylums of Animal Kingdom-Class IXDocument1 pageAnimal Kingdom-Phylums of Animal Kingdom-Class IXMonika Mehan89% (9)
- VDR G4 Manual Steinsohn PDFDocument185 pagesVDR G4 Manual Steinsohn PDFVariya Dharmesh100% (1)
- Wolfgang KohlerDocument16 pagesWolfgang KohlerMaureen JavierNo ratings yet
- NematodesDocument2 pagesNematodesRheila DuyaNo ratings yet
- RMTnotes PARASITOLOGYDocument68 pagesRMTnotes PARASITOLOGYArvin O-CaféNo ratings yet
- Trematodes General CharacteristicsDocument1 pageTrematodes General CharacteristicseseyesmontecalvosabanalNo ratings yet
- Malaria - Parasitosis Pediculosis Escabiosis - Toxo LeishmaniosisDocument163 pagesMalaria - Parasitosis Pediculosis Escabiosis - Toxo LeishmaniosisUC SergioNo ratings yet
- Animal Kingdom Mind MapDocument4 pagesAnimal Kingdom Mind MapVedanti Naik100% (1)
- CockroachDocument26 pagesCockroachVaiditNo ratings yet
- Week 2 (Lec-Lab) Mls 306 Clinical Parasitology Bsmls 3A: Ascaris LumbricoidesDocument4 pagesWeek 2 (Lec-Lab) Mls 306 Clinical Parasitology Bsmls 3A: Ascaris LumbricoidesHannah Beatrice Adame TamayoNo ratings yet
- Unit 3 - Invertebrates Summary - 1stESO - Filled - With InformationDocument6 pagesUnit 3 - Invertebrates Summary - 1stESO - Filled - With InformationEloisa Navas FernandezNo ratings yet
- Characteristics and Systems of AnnelidsDocument1 pageCharacteristics and Systems of Annelidsjonathan102890No ratings yet
- CockroachDocument13 pagesCockroachVaiditNo ratings yet
- Parasitology Metazoa: ProtozoaDocument7 pagesParasitology Metazoa: ProtozoaTrishaNo ratings yet
- Animal Kingdom - Mind Maps - Arjuna NEET 2024Document3 pagesAnimal Kingdom - Mind Maps - Arjuna NEET 2024Ramervetugamer s100% (1)
- NotesDocument7 pagesNotesVermillion ZedNo ratings yet
- Parasites by Apple TanDocument16 pagesParasites by Apple TanOlivia LimNo ratings yet
- 3-Intstinal HelminthesDocument27 pages3-Intstinal Helminthesademabdella38No ratings yet
- 6.2 2021para ReviewlocalwactsDocument35 pages6.2 2021para ReviewlocalwactsHeyzel joy FabianNo ratings yet
- Nematodes Lab Reviewer PDFDocument7 pagesNematodes Lab Reviewer PDFRobi Alegre MedinaNo ratings yet
- Animal Kingdom - Part 1.ppsxDocument59 pagesAnimal Kingdom - Part 1.ppsxShiyan Shirani0% (1)
- Animal Kingdom ClassificationDocument9 pagesAnimal Kingdom ClassificationBrilliant Cloudprint100% (1)
- Helminth Identification and Treatment GuideDocument3 pagesHelminth Identification and Treatment GuideOmphile DansonNo ratings yet
- Clinical+Parasitology-Module+8Document15 pagesClinical+Parasitology-Module+8Geresh MagsinoNo ratings yet
- Animalia File 2023-1Document12 pagesAnimalia File 2023-1Syed Zee Waqar GillaniNo ratings yet
- Helminths and Protozoa: Parasitic Worms and Single-Celled ParasitesDocument6 pagesHelminths and Protozoa: Parasitic Worms and Single-Celled ParasitesSuzanne RibsskogNo ratings yet
- Animal Division and Tissue TypesDocument6 pagesAnimal Division and Tissue TypesCharles GuillermoNo ratings yet
- Animal Kingdom Classification and CharacteristicsDocument11 pagesAnimal Kingdom Classification and CharacteristicsAnusree M.SNo ratings yet
- 107 ANIMALS PhylaDocument1 page107 ANIMALS Phylasamsung galaxyNo ratings yet
- Non-Chordates AnimalDocument58 pagesNon-Chordates AnimalToushik Ahamed MollaNo ratings yet
- Phasmid 1 Vo23Document7 pagesPhasmid 1 Vo23njdomaubNo ratings yet
- Introduction To ParasitologyDocument2 pagesIntroduction To ParasitologySherwin BumanglagNo ratings yet
- Taxis - Arrange Nomla - Method: Taxonomy ClassificationDocument7 pagesTaxis - Arrange Nomla - Method: Taxonomy ClassificationMarvin Lucky AllasNo ratings yet
- Helminths 12Document34 pagesHelminths 12malakaiad212No ratings yet
- Introduction To Cestodes and Minor CestodesDocument8 pagesIntroduction To Cestodes and Minor CestodesJustin TayabanNo ratings yet
- CH 4Document9 pagesCH 4Ruchika Kumari, VIII-A, 3956No ratings yet
- Class Nematoda: Ascaris LumbricoidesDocument6 pagesClass Nematoda: Ascaris LumbricoidesGeorge FogNo ratings yet
- 3.-Helminthes 2Document17 pages3.-Helminthes 2Sherwin BumanglagNo ratings yet
- Sexual Versus Asexual Reproduction: Sexual (Sperm Meet Egg) 2 ParentsDocument33 pagesSexual Versus Asexual Reproduction: Sexual (Sperm Meet Egg) 2 ParentsNazim AliNo ratings yet
- Animal Evolution and DiversityDocument20 pagesAnimal Evolution and DiversityRob YickNo ratings yet
- Parasitology: An Introduction to Nematodes, Cestodes, Trematodes and ProtozoaDocument8 pagesParasitology: An Introduction to Nematodes, Cestodes, Trematodes and ProtozoaRuthenie RedobleNo ratings yet
- NematodesDocument4 pagesNematodesjannapradooNo ratings yet
- Week 7 Introduction To Nematodes PDFDocument5 pagesWeek 7 Introduction To Nematodes PDFewmedtechNo ratings yet
- Helminths (Parasitic worms) Kingdom Animalia Phylum PlatyhelminthsDocument11 pagesHelminths (Parasitic worms) Kingdom Animalia Phylum Platyhelminthsemil diogoNo ratings yet
- Helminth Introduction 160619043259Document12 pagesHelminth Introduction 160619043259JaneYlNo ratings yet
- Animal KingdomDocument13 pagesAnimal KingdomAanchal Pandey100% (2)
- Enperiment For Spotting-3Document18 pagesEnperiment For Spotting-3Debayan Bhattacharyya class:- 11-ANo ratings yet
- 7 - Nematodes (Aphasmids and Phasmids)Document9 pages7 - Nematodes (Aphasmids and Phasmids)Scarlet WitchNo ratings yet
- TrematodesDocument30 pagesTrematodesJezzah Mae CañeteNo ratings yet
- Kingdom AnimaliaDocument2 pagesKingdom AnimaliaZoology InterestsNo ratings yet
- Kingdom Animalia SummaryDocument2 pagesKingdom Animalia Summaryaqeel abdullahNo ratings yet
- Kingdom Animalia summaryDocument2 pagesKingdom Animalia summaryaayzah2005No ratings yet
- Nematodes Cestodes, Trematodes NoteDocument3 pagesNematodes Cestodes, Trematodes NoteJanielle Medina FajardoNo ratings yet
- Platyhelminthes - 6th Class PDFDocument23 pagesPlatyhelminthes - 6th Class PDFAbdulla Hil KafiNo ratings yet
- Platyhelminthes (Flatworms, Tapeworms) : Diversity of Life - AnimalsDocument21 pagesPlatyhelminthes (Flatworms, Tapeworms) : Diversity of Life - AnimalskingNo ratings yet
- Parasitology: Helminthology: HelminthsDocument21 pagesParasitology: Helminthology: Helminthstony montanNo ratings yet
- Class XI, Chp4-Animal Kingdom-1Document5 pagesClass XI, Chp4-Animal Kingdom-1anirudhgupta5050No ratings yet
- TERMINOLOGIESDocument3 pagesTERMINOLOGIESYsabella PolanaNo ratings yet
- Animal Kingdom - Platyhelminthes & NematodaDocument14 pagesAnimal Kingdom - Platyhelminthes & NematodaJoanna Susan JojiNo ratings yet
- Zoology LT 3Document6 pagesZoology LT 3Jonathan CuezonNo ratings yet
- Camp's Zoology by the Numbers: A comprehensive study guide in outline form for advanced biology courses, including AP, IB, DE, and college courses.From EverandCamp's Zoology by the Numbers: A comprehensive study guide in outline form for advanced biology courses, including AP, IB, DE, and college courses.No ratings yet
- Optical Fiber Communication Case Study on Material DispersionDocument5 pagesOptical Fiber Communication Case Study on Material DispersionAyush SharmaNo ratings yet
- Annual Report 18Document363 pagesAnnual Report 18Safeer UllahNo ratings yet
- Cebuano LanguageDocument15 pagesCebuano LanguageIsla PageNo ratings yet
- A Review of The Management of Cerebral Vasospasm After Aneurysmal Subarachnoid HemorrhageDocument15 pagesA Review of The Management of Cerebral Vasospasm After Aneurysmal Subarachnoid HemorrhageAlanNo ratings yet
- Daftar Pustaka DaniDocument3 pagesDaftar Pustaka Danidokter linggauNo ratings yet
- Unit 5 EstándarDocument2 pagesUnit 5 EstándardechillbroNo ratings yet
- Active Directory: Lab 1 QuestionsDocument2 pagesActive Directory: Lab 1 QuestionsDaphneHarrisNo ratings yet
- CD 1 - Screening & DiagnosisDocument27 pagesCD 1 - Screening & DiagnosiskhairulfatinNo ratings yet
- Dream Life - Allan HobsonDocument307 pagesDream Life - Allan HobsonJose MuñozNo ratings yet
- Mercury Poisoning Symptoms and TreatmentsDocument1 pageMercury Poisoning Symptoms and TreatmentsRakheeb BashaNo ratings yet
- Temenos Brochure - FormpipeDocument5 pagesTemenos Brochure - FormpipeDanial OngNo ratings yet
- EBSD Specimen Prep PaperDocument36 pagesEBSD Specimen Prep PaperPaul RosiahNo ratings yet
- Fisher - Techincal Monograph 42 - Understanding DecibelsDocument8 pagesFisher - Techincal Monograph 42 - Understanding Decibelsleslie.lp2003No ratings yet
- A Report On Kantajew MandirDocument21 pagesA Report On Kantajew MandirMariam Nazia 1831388030No ratings yet
- Lecture01 PushkarDocument27 pagesLecture01 PushkarabcdNo ratings yet
- TLM4ALL@1 Number System (EM)Document32 pagesTLM4ALL@1 Number System (EM)jkc collegeNo ratings yet
- St. Francis de Sales Sr. Sec. School, Gangapur CityDocument12 pagesSt. Francis de Sales Sr. Sec. School, Gangapur CityArtificial GammerNo ratings yet
- Introduction To Drug DiscoveryDocument45 pagesIntroduction To Drug Discoveryachsanuddin100% (5)
- 6 Construction of ShoeDocument33 pages6 Construction of ShoevedNo ratings yet
- The Mysteries of Plato: Lunar NotebookDocument2 pagesThe Mysteries of Plato: Lunar NotebookDavor BatesNo ratings yet
- Is Iso 2692-1992Document24 pagesIs Iso 2692-1992mwasicNo ratings yet
- JKSTREGIESDocument59 pagesJKSTREGIESmss_singh_sikarwarNo ratings yet
- Ventilator Modes - WEANINGDocument3 pagesVentilator Modes - WEANINGAlaa OmarNo ratings yet
- Crashing Pert Networks: A Simulation ApproachDocument15 pagesCrashing Pert Networks: A Simulation ApproachRavindra BharathiNo ratings yet
- Assessmentof Safety Cultureand Maturityin Mining Environments Caseof Njuli QuarryDocument12 pagesAssessmentof Safety Cultureand Maturityin Mining Environments Caseof Njuli QuarryAbdurrohman AabNo ratings yet
- Senior High School Tracks: Free Powerpoint Templates Free Powerpoint TemplatesDocument11 pagesSenior High School Tracks: Free Powerpoint Templates Free Powerpoint TemplatesGeraldineNo ratings yet
- A Generation of Contradictions-Unlocking Gen Z 2022 China FocusDocument25 pagesA Generation of Contradictions-Unlocking Gen Z 2022 China FocusCindy Xidan XiaoNo ratings yet
- CHM131 Presentation - Oxidation of MetalsDocument11 pagesCHM131 Presentation - Oxidation of MetalsNazrul ShahNo ratings yet