Professional Documents
Culture Documents
SC120 Study Guide 3
Uploaded by
REGINA MAE JUNIOOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SC120 Study Guide 3
Uploaded by
REGINA MAE JUNIOCopyright:
Available Formats
FM-AA-CIA-15 Rev.
0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
STUDY GUIDE FOR MODULE NO. ___
3
INTEGRATION AND COORDINATION
MODULE OVERVIEW
The nervous system is made up of all the nerve cells in your body. It is through the nervous
system that we communicate with the outside world and, at the same time, many mechanisms inside
our body are controlled. The nervous system takes in information through our senses, processes the
information and triggers reactions, such as making your muscles move or causing you to feel pain. For
example, if you touch a hot plate, you reflexively pull back your hand and your nerves simultaneously
send pain signals to your brain. Metabolic processes are also controlled by the nervous system.
The sensory nervous system is a part of the nervous system responsible for
processing sensory information. A sensory system consists of sensory neurons (including the sensory
receptor cells), neural pathways, and parts of the brain involved in sensory perception. Commonly
recognized sensory systems are those for vision, hearing, touch, taste, smell, and balance. In short,
senses are transducers from the physical world to the realm of the mind where we interpret the
information, creating our perception of the world around us.
The endocrine system is a chemical messenger system comprising feedback loops of
the hormones released by internal glands of an organism directly into the circulatory system, regulating
distant target organs. In humans, the major endocrine glands are the thyroid gland and the adrenal
glands. In vertebrates, the hypothalamus is the neural control center for all endocrine systems. The
study of the endocrine system and its disorders is known as endocrinology. Endocrinology is a branch
of internal medicine.
NATURE OF ANATOMY AND PHYSIOLOGY
The Nervous System is one of the smallest and yet the most complex of the 11 body systems. It
is also responsible for our perceptions, behaviors, and memories, and it initiates all voluntary
movements.
Two main subdivisions:
A. Central Nervous System- consists of the brain and spinal cord. The Central Nervous
System processes many different kinds of incoming sensory information. It is also the
source of thoughts, emotions, and memories.
The brain is the part of the CNS that is located in the skull and contains about 85 billion
neurons.
The spinal cord is connected to the brain through foramen ovale.
B. Peripheral Nervous System- consist of all nervous tissue outside the CNS.
Components of the PNS:
1. Nerve- a bundle of hundreds to thousands of axons plus associated connective tissue
and blood vessels.
2. Sensory receptors- a structure of the nervous system that monitors changes in the
external or internal environment.
Examples of sensory receptors:
• Touch receptors in the skin
• Photoreceptors in the eye
• Olfactory receptors in the nose
PANGASINAN STATE UNIVERSITY 1
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
Organization of the Nervous System
PANGASINAN STATE UNIVERSITY 2
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
PNS is divided into sensory and motor divisions:
• Sensory or afferent division- conveys input into the CNS from sensory receptors in the body.
-this division provides the CNS with sensory information about the somatic
senses(tactile, thermal, pain, and proprioceptive sensations) and special senses (smell, vision,
hearing, and equilibrium).
• Motor or efferent division- conveys output from the CNS to effectors (muscles and glands).
Motor or Efferent division:
Somatic nervous system- conveys output from the CNS to skeletal muscles only.
Autonomic Nervous System- coveys output from the CNS to smooth muscle, cardiac muscle
and glands.
Autonomic Nervous System two main branches:
A. Sympathetic Nervous System- “fight-or-flight” responses
B. Parasympathetic Nervous System- “rest-and-digest”
Enteric Nervous System- an extensive network of over 100 million neurons confined to the
wall of the gastrointestinal tract.
- Helps regulate the activity of the smooth muscle and glands of the GI tract.
Three basic function of the Nervous System:
1. Sensory function- detect internal stimuli, such as an increase in blood pressure, or
external stimuli. Ex. A raindrop landing on your arm, When you answer your cell phone
after hearing it ring.
2. Integrative function- the nervous system processes sensory information by analyzing it
and making decisions for appropriate responses – an activity known as integration.
3. Motor function- Once sensory information is integrated, the nervous system may elicit an
appropriate motor response by activating effectors (muscles and glands) through cranial
and spinal nerves.
Histology of Nervous Tissue
Two types of cells:
1. Neurons- possess electrical excitability, ability to respond a stimulus and convert it into
an action potential.
Stimulus- any change in the environment that is strong enough to initiate an action
potential.
Action potential- electrical signal that propagates (travels) along the surface of the
membrane of a neuron.
2. Neuroglia- are smaller cells, but they greatly outnumber neurons
- supports, nourish, and protect neurons, and maintain the interstitial fluid that bathes
them.
Three Parts of Neuron:
a. Cell body- also known perikaryon or soma, contains a nucleus surrounded by cytoplasm
that includes typical cellular organelles such as lysosomes, mitochondria, and a Golgi
complex.
Nissl bodies- for neuronal cell bodies contain free ribosomes and prominent cluster of
rough endoplasmic reticulum.
PANGASINAN STATE UNIVERSITY 3
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
Lipofuscin- pigment that occurs as clumps of yellowish brown granules in the cytoplasm.
Ganglion- collection of neuron cell bodies outside the CNS.
Nerve fiber- general term for any neuronal process that emerges from the cell body of a
neuron.
Dendrites- are the receiving or input portions of a neuron.
Axon- propagates nerve impulses toward another neuron, a muscle fiber, or a gland cell.
Axon hillock- long, thin, cylindrical projection that often joins to the cell body at a cone-
shaped elevation.
Initial segment- part of the axon closest to the axon hillock.
Trigger zone- nerve impulses arise at the junction of the axon hillock and the initial segment.
Axoplasm- cytoplasm of axon
Axolemma- surrounded by a plasma membrane.
Axon collaterals- along the length of an axon, side branches.
Axon terminals- axon and its collaterals end by dividing into many fine processes.
Synapse- site of communication between two neurons or between a neuron and an effector
cell.
Synaptic end bulbs- tips of some axon terminals swell into bulb-shaped structures.
Varicosities- exhibit a string of swollen bumps
Synaptic vesicles- contain tiny membrane-enclosed sacs.
Neurotransmitter- molecule released from a synaptic vesicle that excites or inhibits another
neuron, muscle fiber, or gland cell.
Slow axonal transport- the slower system, which moves materials about 1-5mm per day.
Fast axonal transport- capable of moving materials a distance of 200-400mm per day
Anterograde- forward direction moves organelles and synaptic vesicles from the cell body to
the axon terminals.
Retrograde- backward direction moves membrane vesicles and other cellular materials from
the axon terminals to the cell body to be degraded or recycled.
Neural Circuits- the CNS contain billions of neurons organized into complicated networks.
PANGASINAN STATE UNIVERSITY 4
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
Simple series circuit- a presynaptic neuron stimulates a single postsynaptic neuron.
Divergence- a single presynaptic neuron may synapse with several postsynaptic neurons.
Diverging circuits- the nerve impulse from a single presynaptic neuron causes the
stimulation of increasing numbers of cells along the circuit.
Convergence- permits more effective stimulation or inhibition of the postsynaptic neuron.
Converging circuit- the postsynaptic neuron receives nerve impulses from several different
sources.
Reverberating circuit- the incoming impulse stimulates the first neuron, which stimulates the
second, which stimulates the third, and so on.
Parallel after discharge circuit- a single presynaptic cell stimulates a group of neurons, each
of which synapses with a common postsynaptic cell.
Aging and the Nervous System
• As the brain ages, neurons in the central nervous system (CNS), which do not typically
regenerate, are lost. This reduces the brain’s capacity to send and receive nerve
impulses and slows information processing.
• Dementia is the age-related progressive decline in cognitive function. This may affect
memory, attention, language, and problem-solving.
• Alzheimer’s disease is a neurodegenerative disease characterized by progressive
cognitive deterioration, declining activities of daily living, and neuropsychiatric
symptoms or behavioral changes. It is the most common cause of dementia.
• cerebral cortex: The gray, folded, outermost layer of the cerebrum that is responsible for
higher brain processes such as sensation, voluntary muscle movement, thought,
reasoning, and memory.
• dementia: A progressive decline in cognitive function due to brain damage or disease.
Areas particularly affected include memory, attention, judgement, language, and problem
solving.
PANGASINAN STATE UNIVERSITY 5
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
Neuron loss is an effect of aging on the nervous system. By the age of 30, the brain begins to
lose thousands of neurons each day, causing a decreased capacity to send nerve impulses to
and from the brain and slowing information processing. In addition, voluntary motor movements
slow down, reflex time increases, and conduction velocity decreases.
Dementia (from Latin de- “apart, away” + mens (genitive mentis) “mind”) is the progressive
decline in cognitive function due to damage or disease in the brain beyond what is expected from
normal aging. Dementia most commonly affects memory, attention, language, and problem
solving, although those in the later stages in this condition may be disoriented in time, place, and
person. Symptoms of dementia can be classified as either reversible or irreversible depending
upon the etiology of the disease. Less than 10% of all dementia cases are reversible.
Alzheimer’s disease (AD) is a neurodegenerative disease characterized by progressive cognitive
deterioration, declining activities of daily living, and neuropsychiatric symptoms or behavioral
changes. It is the most common cause of dementia. The most striking early symptom is short
term memory loss (amnesia), which usually manifests as minor forgetfulness that becomes
steadily more pronounced with illness progression. Older memories are often preserved. As the
disorder progresses, cognitive (intellectual) impairment extends to the domains of language
(aphasia), skilled movements (apraxia), recognition (agnosia), and functions (such as decision-
making and planning) closely related to the frontal and temporal lobes of the brain as they become
disconnected from the limbic system, reflecting extension of the underlying pathological
process.
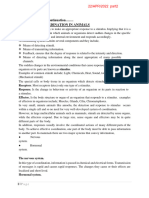
Effects of Alzheimer’s Disease: Comparison of a normal aged brain (left) and the brain of a
person with Alzheimer’s (right). Differential characteristics are pointed out in the hippocampus,
cerebral cortex, and ventricles.
The symptoms of Alzheimer’s are triggered by neuron loss and an inflammatory response to the
deposition of amyloid plaques and neurofibrillary tangles. Alzheimer’s has a genetic component,
and autosomal dominant mutations in three different genes have been identified that account for
a small number of cases of familial, early-onset AD. For late onset AD (LOAD), only one
susceptibility gene has so far been identified: the epsilon 4 allele of the apolipoprotein E gene.
Age of onset itself has a heritability of around 50%.
PANGASINAN STATE UNIVERSITY 6
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
NERVOUS SYSTEM MEDICAL TERMS
Cephal/o Head Cephalgia (a headache)
Encephal/o Inside the head (brain) Encephalitis (inflammation of the brain)
Anencephalic (born without a
brain)
Mening/o Membranes surrounding the brain and spinal cord Meningitis (inflammation of
the membranes)
Myel/o Spinal cord Myelogram (X-ray of the spinal cord)
Neur/o Nerve Neuroma (tumor) Neuritis (inflammation)
Dys Difficult, painful, abnormal Dyslexia (difficulty reading)
-cele Hernia, abnormal protrusion of structure Meningomyelocele (protrusion of membranes
out of normal anatomical position and spinal cord)
-pathy Disease, abnormality Encephalopathy (disease of the brain)
Neuropathy (disease of the nerves)
-plasia Development, formation, growth Aplasia (no development)
Hyperplasia (over development)
-plegia Paralysis Hemiplegia (paralysis of one side of the body)
Quadriplegia (paralysis of all four limbs)
Sensory System
A sensory system is a part of the nervous system responsible for
processing sensory information. A sensory system consists of sensory receptors,
neural pathways, and parts of the brain involved in sensory perception.
Somatic sensory pathways(somatosensory)- relays information from spmatic sensory receptors
to the primary somatosensory area in the parietal lobe of the cerebral cortex and
to the cerebellum.
Somatic sensory pathway to the cerebral cortex consist of thousands of sets of three neurons:
1. First order (primary) neurons- are sensory neurons that conducts impulses from somatic
sensory receptors into the brainstem or spinal cord.
2. Second order (secondary) neurons- conduct impulses from the brainstem or spinal cord
to the thalamus.
3. Third order (tertiary) neurons- conduct impulses from the thalamus to the primary
somatosensory area on the same side.
Somatic sensory impulses ascend to the cerebral cortex via three general pathways:
a. The posterior column-medial lemniscus pathways- nerve impulses for touch, pressure,
vibration, and proprioception.
-name of the pathway comes from the names of two white-matter tracts that convey the
impulses: the posterior column of the spinal cord and the medial lemniscus of the
brainstem.
Two tracts of Posterior column:
1. Gracile fasciculus
2. Cuneate fasciculus
PANGASINAN STATE UNIVERSITY 7
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
b. The anterolateral (spinothalamic) pathway- nerve impulses for pain, temperature, itch
and tickle from the limbs, trunk, neck and posterior head
c. The trigeminothalamic pathway- nerve impulses for most somatic sensations (tactile,
thermal and pain)
PANGASINAN STATE UNIVERSITY 8
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
CHARACTERISTICS OF SENSATIONS:
1. Projection—the sensation seems to come from the area where the receptors were stimulated. If you
touch this book, the sensation of touch seems to be in your hand but is actually being felt by your cere-
bral cortex. That it is indeed the brain that feels sensations is demonstrated by patients who feel phantom
pain after amputation of a limb. After loss of a hand, for example, the person may still feel that the hand
is really there. Why does this hap-pen? The receptors in the hand are no longer pres-ent, but the severed
nerve endings continue to generate impulses. These impulses arrive in the parietal lobe area for the
hand, and the brain does what it has always done and creates the projection, the feeling that the hand is
still there. For most amputees, phantom pain diminishes as the severed nerves heal, but the person often
experiences a phantom “presence” of the missing part. This may be helpful when learning to use an
artificial limb.
2. Intensity—some sensations are felt more distinctly and to a greater degree than are others. A weak
stimulus such as dim light will affect a small num-ber of receptors, but a stronger stimulus, such as bright
sunlight, will stimulate many more recep-tors. When more receptors are stimulated, more impulses will
arrive in the sensory area of the brain. The brain “counts” the impulses and projects a more intense
sensation.
3. Contrast—the effect of a previous or simultaneous sensation on a current sensation, which may then
be exaggerated or diminished. Again, this is a func-tion of the brain, which constantly compares sensa-
tions. If, on a very hot day, you jump into a swimming pool, the water may feel quite cold at first. The
brain compares the new sensation to the previous one, and since there is a significant differ-ence
between the two, the water will seem colder than it actually is.
4. Adaptation—becoming unaware of a continuing stimulus. Receptors detect changes, but if the stim-
ulus continues it may not be much of a change, and the receptors will generate fewer impulses. The
water in the swimming pool that seemed cold at first seems to “warm up” after a few minutes. The water
PANGASINAN STATE UNIVERSITY 9
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
has not changed temperature, and the recep-tors for cold have no changes to detect, therefore they
generate fewer impulses. The sensation of cold lessens, and we interpret or feel that as increasing
warmth. For another example, look at your left wrist (or perhaps the right one). Many of us wear a watch
and are probably unaware of its presence on the arm most of the time. The cuta-neous receptors for
touch or pressure adapt very quickly to a continuing stimulus, and if there is no change, there is nothing
for the receptors to detect.
5. After-image—the sensation remains in the con-sciousness even after the stimulus has stopped. A
familiar example is the bright after-image seen after watching a flashbulb go off. The very bright light
strongly stimulates receptors in the retina, which generate many impulses that are perceived as an
intense sensation that lasts longer than the actual stimulus.
Classification of Sensations
Visual Sensations
Any vision, sight or ocular experience that could loosely be described as grayish is called an
achromatic visual sensation. Any sight that could be roughly described as reddish or greenish
is called an organic chromatic sensation. And any image that could be described as yellowish
or bluish is called an inorganic chromatic visual sensation.
Thermal Sensations
Strong feelings that are so hot or cold that they are hazardous are called dangerous thermal
sensations. Warm or cool feelings that happen during routine human activity are safe thermal
sensations.
Somatic Sensations
Any tactile or auditory perception associated with a sense of touch, pressure, hearing or sound.
Taste Sensations
Flavors or gustatory perceptions that are produced when a substance in the mouth reacts with
nerves of the tongue and palate. We specifically consider sweet, sour and salty flavors. But
bitter, pungent and metallic tastes are other well-known examples from among hundreds of
distinctly recognizable flavors.
Types of Sensory Receptors:
1. Microscopic structure
Sensory receptor maybe:
a. Free nerve endings of first-order sensory neurons
b. Encapsulated nerve endings of first-order sensory neurons
c. Separate cells that synapse with first-order sensory neurons
2. Location of receptors and the origin of stimuli that activate them
•Exteroreceptors- located at or near the external surface of the body
- sensitive to stimuli originating outside the body and provide information about the
external environment.
•Interoceptors- located in blood vessels, visceral organs, muscles, and the nervous
system and monitor conditions in the internal environment.
•Proprioceptors- located in muscles, tendons, joints, and the inner ear.
3. Type of stimulus detected
•Mechanoreceptors- sensitive to mechanical stimuli such as the deformation, stretching,
or bending of cells.
•Thermoreceptors- detect changes in temperature
•Nociceptors- respond to painful stimuli resulting from physical or chemical damage to
tissue
•Photoreceptors- detect light that strikes the retina of the eye.
•Chemoreceptors- detect chemicals in the mouth, nose and body fluids.
•Osmoreceptors- detect the osmotic pressure of body fluids
PANGASINAN STATE UNIVERSITY 10
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
Somatic sensation and Proprioception
Somatic sensation- arise the stimulation of sensory receptors embedded in the skin or
subcutaneous layer, in mucous membranes of the mouth, vagina, and anus and in skeletal
muscles, tendons and joints.
Cutaneous sensation- somatic sensations that arise from stimulating the skin surface.
Four modalities of somatic sensation:
a. Tactile sensations- include touch, pressure, vibration, itch, and tickle.
Touch sensation- result from stimulation of tactile receptors in the skin or subcutaneous
layer.
Two types of touch receptors:
1. Corpuscles of touch or Meissner corpuscles- touch receptors that are located in the
dermal papillae of hairless skin.
2. Hair root plexuses- rapidly adapting touch receptors found in hairy skin.
- consist of free nerve endings wrapped around hair follicles.
Two types of slowly adapting touch receptors:
1. Type I cutaneous mechanoreceptors- also known as tactile discs
- saucer-shaped, flattened free nerve endings that make contact with tactile epithelial
cells of the stratum basale.
2. Type II cutaneous mechanoreceptors or Ruffini corpuscles- elongated, encapsulated
receptors located in the dermis, subcutaneous layer, and other tissues of the body.
b. Thermal sensations
Thermoreceptors- free nerve endings that have receptive fields about 1 mm in diameter on
the skin surface.
Two distinct thermal sensation:
PANGASINAN STATE UNIVERSITY 11
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
1. Cold receptors- located in the stratum basale of the epidermis and are attached to
medium-diameter, myelinated A fibers, although a few connect to small-diameter,
unmyelinated C fibers.
2. Warm receptors- located in the dermis and are attached to small-diameter, unmyelinated
C fibers.
c. Pain Sensation
Nociceptors- receptors for pain, free nerve endings found in every tissue of the body
except the brain
Types of Pain:
1. Fast pain- occurs very rapidly, usually within 0.1 second after a stimulus is applied.
2. Slow pain- begins a second or more after a stimulus is applied.
Superficial somatic pain- pain that arises from stimulation of receptors in the skin
Deep somatic pain- stimulation of receptors in skeletal muscles, joints, tendons, and fascia
Visceral pain- results from stimulation of nociceptors in visceral organs.
Localization of Pain:
Referred Pain- pain is felt in or just deep to the skin that overlies the stimulated organ, or in
surface area far from the stimulated organ.
d. Proprioceptive Sensations- also called proprioception
- allows us to recognize that parts of our body belong to us
Kinesthesia- perception of body movements
Weight discrimination- ability to assess the weight of an object.
Three types of Proprioceptors:
1. Muscle spindles- proprioceptors that monitors changes in the length of skeletal muscles
and participate in stretch reflexes
2. Tendon organ- slowly adapting receptors located at the junction of a tendon and a
muscle
3. Joint kinesthetic receptors- present within and around the articular capsules of synovial
joints
Aging and the Senses
HEARING
Your ears have two jobs. One is hearing and the other is maintaining balance. Hearing occurs
after sound vibrations cross the eardrum to the inner ear. The vibrations are changed into nerve
signals in the inner ear and are carried to the brain by the auditory nerve.
Balance (equilibrium) is controlled in the inner ear. Fluid and small hair in the inner ear
stimulate the auditory nerve. This helps the brain maintain balance.
As you age, structures inside the ear start to change and their functions decline. Your ability to
pick up sounds decreases. You may also have problems maintaining your balance as you sit,
stand, and walk.
Age-related hearing loss is called presbycusis. It affects both ears. Hearing, often the ability to
hear high-frequency sounds, may decline. You may also have trouble telling the difference
between certain sounds. Or, you may have problems hearing a conversation when there is
background noise. If you are having trouble hearing, discuss your symptoms with your health
care provider. One way to manage hearing loss is by getting fitted with hearing aids.
PANGASINAN STATE UNIVERSITY 12
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
Persistent, abnormal ear noise (tinnitus) is another common problem in older adults. Causes of
tinnitus may include wax buildup or medicines that damage structures inside the ear. If you
have tinnitus, ask your provider how to manage the condition.
Impacted ear wax can also cause trouble hearing and is common with age.
VISION
Vision occurs when light is processed by your eye and interpreted by your brain. Light passes
through the transparent eye surface (cornea). It continues through the pupil, the opening to the
inside of the eye. The pupil becomes larger or smaller to control the amount of light that enters
the eye. The colored part of the eye is called the iris. It is a muscle that controls pupil size. After
light passes through your pupil, it reaches the lens. The lens focuses light on your retina (the
back of the eye). The retina converts light energy into a nerve signal that the optic nerve carries
to the brain, where it is interpreted.
As you age, the sharpness of your vision (visual acuity) gradually declines. The most common
problem is difficulty focusing the eyes on close-up objects. This condition is called presbyopia.
Reading glasses, bifocal glasses, or contact lenses can help correct presbyopia.
You may be less able to tolerate glare. For example, glare from a shiny floor in a sunlit room can
make it difficult to get around indoors. You may have trouble adapting to darkness or bright
light. Problems with glare, brightness, and darkness may make you give up driving at night.
As you age, it gets harder to tell blues from greens than it is to tell reds from yellows. Using
warm contrasting colors (yellow, orange, and red) in your home can improve your ability to see.
Keeping a red light on in darkened rooms, such as the hallway or bathroom, makes it easier to
see than using a regular night light.
Reduced peripheral vision (side vision) is common in older people. This can limit your activity
and ability to interact with others. It may be hard to communicate with people sitting next to you
because you cannot see them well. Driving can become dangerous.
Weakened eye muscles may prevent you from moving your eyes in all directions. It may be hard
to look upward. The area in which objects can be seen (visual field) gets smaller.
Common eye disorders that cause vision changes that are NOT normal include:
• Cataracts -- clouding of the lens of the eye
• Glaucoma -- rise in fluid pressure in the eye
• Macular degeneration -- disease in the macula (responsible for central vision) that causes vision
loss
• Retinopathy -- disease in the retina often caused by diabetes or high blood pressure
TASTE AND SMELL
The senses of taste and smell work together. Most tastes are linked with odors. The sense of
smell begins at the nerve endings high in the lining of the nose.
You have about 10,000 taste buds. Your taste buds sense sweet, salty, sour, bitter, and umami
flavors. Umami is a taste linked with foods that contain glutamate, such as the seasoning
monosodium glutamate (MSG).
Smell and taste play a role in food enjoyment and safety. A delicious meal or pleasant aroma
can improve social interaction and enjoyment of life. Smell and taste also allow you to detect
danger, such as spoiled food, gases, and smoke.
If your senses of taste and smell have diminished, talk to your provider. The following may help:
PANGASINAN STATE UNIVERSITY 13
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
• Switch to a different medicine, if the medicine you take is affecting your ability to smell and
taste.
• Use different spices or change the way you prepare food.
• Buy safety products, such as a gas detector that sounds an alarm you can hear.
TOUCH, VIBRATION, AND PAIN
The sense of touch makes you aware of pain, temperature, pressure, vibration, and body
position. Skin, muscles, tendons, joints, and internal organs have nerve endings (receptors)
that detect these sensations. Some receptors give the brain information about the position and
condition of internal organs. Though you may not be aware of this information, it helps to
identify changes (for example, the pain of appendicitis).
Your brain interprets the type and amount of touch sensation. It also interprets the sensation as
pleasant (such as being comfortably warm), unpleasant (such as being very hot), or neutral
(such as being aware that you are touching something).
With aging, sensations may be reduced or changed. These changes can occur because of
decreased blood flow to the nerve endings or to the spinal cord or brain. The spinal cord
transmits nerve signals and the brain interprets these signals.
Health problems, such as a lack of certain nutrients, can also cause sensation changes. Brain
surgery, problems in the brain, confusion, and nerve damage from injury or long-term (chronic)
diseases such as diabetes can also result in sensation changes.
If you have noticed changes in touch, pain, or problems standing or walking, talk with your
provider. There may be ways to manage the symptoms.
The following measures can help you stay safe:
• Lower the water heater temperature to no higher than 120°F (49°C) to avoid burns.
• Check the thermometer to decide how to dress, rather than waiting until you feel overheated or
chilled.
• Inspect your skin, especially your feet, for injuries. If you find an injury, treat it. DO NOT assume
the injury is not serious because the area is not painful.
OTHER CHANGES
As you grow older, you will have other changes, including:
• In organs, tissues, and cells
• In skin
• In the bones, muscles, and joints
• In the face
• In the nervous system
Key medical terms associated with somatic senses
Sense
1.a faculty by which the conditions or properties of things are perceived. Five major senses wer
e traditionally considered: VISION, HEARING, SMELL, TASTE, and TOUCH. In addition, EQUILIBRIUM, HU
PANGASINAN STATE UNIVERSITY 14
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
NGER, THIRST, MALAISE, PAIN, and other types of senses have been distinguished. The operation o
f all senses involves the reception of stimuli by sense ORGANS, each of which is sensitive to a pa
rticular kind of stimulus. The eyes are sensitive to light; the ears, to sound; the olfactory organs
, to odor; and the taste buds, to taste. Various sense organs of the skin and other tissues are se
nsitive to touch, pain, temperature, and other sensations. On receiving stimuli, the sense organ
translates them into nerve impulses that are transmitted along the sensory nerves to the brain. I
n the cerebral cortex, the impulses are interpreted, or perceived, as sensations. The brain assoc
iates them with other information, acts upon them, and stores them as memory. See also NERVO
US SYSTEM and BRAIN.
2. pertaining to the sense STRAND of a nucleic acid.
sense of equilibrium the sense of maintenance of or divergence from an upright position, contro
lled by receptors in the vestibule of the ear.
kinesthetic sense muscle sense.
light sense the faculty by which degrees of brilliancy are distinguished.
muscle sense (muscular sense) the faculty by which muscular movements are perceived.
pain sense nociception.
position sense (posture sense) a variety of muscular sense by which the position or attitude of t
he body or its parts is perceived.
pressure sense the faculty by which pressure upon the surface of the body is perceived.
sixth sense the general feeling of consciousness of the entire body; cenesthesia.
somatic s's senses other than the special SENSES; these include TOUCH, KINESTHESIA, NOCICEPTION
, pressure SENSE, temperature SENSE, and muscle SENSE, among others.
space sense the faculty by which relative positions and relations of objects in space are perceiv
ed.
special s's the senses of VISION, HEARING, TASTE, and SMELL; EQUILIBRIUM is sometimes considere
d a special sense, but TOUCH usually is not. See also somatic SENSES.
stereognostic sense the sense by which form and solidity are perceived.
temperature sense the ability to recognize differences in TEMPERATURE; called also thermesthesi
a.
sense
The faculty of perceiving any stimulus.
sense
a. Any of the faculties by which stimuli from outside or inside the body are received and felt, as
the faculties of hearing, sight, smell, touch, taste, and equilibrium.
b. A perception or feeling produced by a stimulus; sensation: a sense of fatigue and hunger.
sensed, sensing, senses
1. To become aware of; perceive: organisms able to sense their surroundings.
2. To detect automatically: sense radioactivity.
adj.
Genetics Of or relating to the portion of the strand of double-
stranded DNA that serves as a template for and is transcribed into RNA.
Sense
The National Deafblind and Rubella Association. The leading national (UK) charity that support
s and campaigns for children and adults who are deafblind, providing expert advice and informa
tion as well as specialist services to deafblind people, their families, carers and the professional
s who work with them. Sense also supports people with sensory impairments and additional dis
abilities.
sense
Neurology The ability to perceive a stimulus.
sense
The faculty of perceiving any stimulus.
sense
Any faculty (or ability) by which some aspect of the environment is perceived. The five main sen
ses are those of sight, hearing, smell, taste and touch. The sense of sight may be further divide
d into the colour sense, the form sense, the light sense, the space sense, etc.
PANGASINAN STATE UNIVERSITY 15
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
Endocrine System
Endocrine system- a network of glands and organs located throughout the body.
It’s similar to the nervous system in that it plays a vital role in controlling and regulating many
of the body’s functions. However, while the nervous system uses nerve impulses and
neurotransmitters for communication, the endocrine system uses chemical messengers called
hormones.
Endocrine system function:
The endocrine system is responsible for regulating a range of bodily functions through the
release of hormones.
Hormones are secreted by the glands of the endocrine system, traveling through the
bloodstream to various organs and tissues in the body. The hormones then tell these organs
and tissues what to do or how to function.
Some examples of bodily functions that are controlled by the endocrine system include:
• metabolism
• growth and development
• sexual function and reproduction
• heart rate
• blood pressure
• appetite
• sleeping and waking cycles
• body temperature
Endocrine system organs
The endocrine system is made up of a complex network of glands, which are organs that
secrete substances.
The glands of the endocrine system are where hormones are produced, stored, and released.
Each gland produces one or more hormones, which go on to target specific organs and tissues
in the body.
The glands of the endocrine system include:
PANGASINAN STATE UNIVERSITY 16
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
• Hypothalamus. While some people don’t consider it a gland, the hypothalamus produces
multiple hormones that control the pituitary gland. It’s also involved in regulating many
functions, including sleep-wake cycles, body temperature, and appetite. It can also
regulate the function of other endocrine glands.
• Pituitary. The pituitary gland is located below the hypothalamus. The hormones it
produces affect growth and reproduction. They can also control the function of other
endocrine glands.
• Pineal. This gland is found in the middle of your brain. It’s important for your sleep-wake
cycles.
• Thyroid. The thyroid gland is located in the front part of your neck. It’s very important for
metabolism.
• Parathyroid. Also located in the front of your neck, the parathyroid gland is important for
maintaining control of calcium levels in your bones and blood.
• Thymus. Located in the upper torso, the thymus is active until puberty and produces
hormones important for the development of a type of white blood cell called a T cell.
• Adrenal. One adrenal gland can be found on top of each kidney. These glands produce
hormones important for regulating functions such as blood pressure, heart rate, and
stress response.
• Pancreas. The pancreas is located in your abdomen behind your stomach. Its endocrine
function involves controlling blood sugar levels.
Some endocrine glands also have non-endocrine functions. For example, the ovaries and testes
produce hormones, but they also have the non-endocrine function of
producing eggs and sperm, respectively.
Endocrine system hormones
Hormones are the chemicals the endocrine system uses to send messages to organs and tissue
throughout the body. Once released into the bloodstream, they travel to their target organ or
tissue, which has receptors that recognize and react to the hormone.
Below are some examples of hormones that are produced by the endocrine system.
Secreting
Hormone Function
gland(s)
increases blood pressure, heart rate, and
adrenaline adrenal
metabolism in reaction to stress
aldosterone adrenal controls the body’s salt and water balance
cortisol adrenal plays a role in stress response
dehydroepiandrosterone aids in production of body odor and growth
adrenal
sulfate (DHEA) of body hair during puberty
estrogen ovary works to regulate menstrual cycle, maintain
PANGASINAN STATE UNIVERSITY 17
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
pregnancy, and develop female sex
characteristics; aids in sperm production
follicle stimulating hormone
pituitary controls the production of eggs and sperm
(FSH)
glucagon pancreas helps to increase levels of blood glucose
insulin pancreas helps to reduce your blood glucose levels
controls estrogen and testosterone
luteinizing hormone (LH) pituitary
production as well as ovulation
melatonin pituitary controls sleep and wake cycles
helps with lactation, childbirth, and mother-
oxytocin pituitary
child bonding
parathyroid hormone parathyroid controls calcium levels in bones and blood
helps to prepare the body for pregnancy
progesterone ovary
when an egg is fertilized
prolactin pituitary promotes breast-milk production
contributes to sex drive and body density in
ovary, teste,
testosterone males and females as well as development
adrenal
of male sex characteristics
help to control several body functions,
thyroid hormone thyroid including the rate of metabolism and energy
levels
Regulation of Hormone Production
Hormone production and release are primarily controlled by negative feedback. In negative
feedback systems, a stimulus elicits the release of a substance; once the substance reaches a
certain level, it sends a signal that stops further release of the substance. In this way, the
concentration of hormones in blood is maintained within a narrow range. For example, the
anterior pituitary signals the thyroid to release thyroid hormones. Increasing levels of these
hormones in the blood then give feedback to the hypothalamus and anterior pituitary to inhibit
further signaling to the thyroid gland. There are three mechanisms by which endocrine glands
are stimulated to synthesize and release hormones: humoral stimuli, hormonal stimuli, and
neural stimuli.
The anterior pituitary stimulates the thyroid gland to release thyroid hormones T3 and T4.
Increasing levels of these hormones in the blood results in feedback to the hypothalamus and
anterior pituitary to inhibit further signaling to the thyroid gland. (credit: modification of work by
Mikael Häggström)
Humoral Stimuli
The term “humoral” is derived from the term “humor,” which refers to bodily fluids such as
blood. A humoral stimulus refers to the control of hormone release in response to changes in
extracellular fluids such as blood or the ion concentration in the blood. For example, a rise in
blood glucose levels triggers the pancreatic release of insulin. Insulin causes blood glucose
levels to drop, which signals the pancreas to stop producing insulin in a negative feedback
loop.
Hormonal Stimuli
Hormonal stimuli refers to the release of a hormone in response to another hormone. A number
of endocrine glands release hormones when stimulated by hormones released by other
endocrine glands. For example, the hypothalamus produces hormones that stimulate the
anterior portion of the pituitary gland. The anterior pituitary in turn releases hormones that
PANGASINAN STATE UNIVERSITY 18
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
regulate hormone production by other endocrine glands. The anterior pituitary releases the
thyroid-stimulating hormone, which then stimulates the thyroid gland to produce the hormones
T3 and T4. As blood concentrations of T3 and T4 rise, they inhibit both the pituitary and the
hypothalamus in a negative feedback loop.
Neural Stimuli
In some cases, the nervous system directly stimulates endocrine glands to release hormones,
which is referred to as neural stimuli. Recall that in a short-term stress response, the hormones
epinephrine and norepinephrine are important for providing the bursts of energy required for
the body to respond. Here, neuronal signaling from the sympathetic nervous system directly
stimulates the adrenal medulla to release the hormones epinephrine and norepinephrine in
response to stress.
Summary
Hormone levels are primarily controlled through negative feedback, in which rising levels of a
hormone inhibit its further release. The three mechanisms of hormonal release are humoral
stimuli, hormonal stimuli, and neural stimuli. Humoral stimuli refers to the control of hormonal
release in response to changes in extracellular fluid levels or ion levels. Hormonal stimuli refers
to the release of hormones in response to hormones released by other endocrine glands. Neural
stimuli refers to the release of hormones in response to neural stimulation.
Mechanisms of Hormone Action
The endocrine system acts by releasing hormones that in turn trigger actions in specific target
cells. Receptors on target cell membranes bind only to one type of hormone. More than fifty
human hormones have been identified; all act by binding to receptor molecules. The binding
hormone changes the shape of the receptor causing the response to the hormone. There are
two mechanisms of hormone action on all target cells.
Aging changes in hormone production
The endocrine system is made up of organs and tissues that produce hormones. Hormones are natural
chemicals produced in one location, released into the bloodstream, then used by other target organs
and systems.
Hormones control the target organs. Some organ systems have their own internal control systems
along with, or instead of, hormones.
As we age, changes naturally occur in the way body systems are controlled. Some target tissues
become less sensitive to their controlling hormone. The amount of hormones produced may also
change.
Blood levels of some hormones increase, some decrease, and some are unchanged. Hormones are
also broken down (metabolized) more slowly.
Many of the organs that produce hormones are controlled by other hormones. Aging also changes this
process. For example, an endocrine tissue may produce less of its hormone than it did at a younger
age, or it may produce the same amount at a slower rate.
AGING CHANGES
The hypothalamus is located in the brain. It produces hormones that control the other structures in the
endocrine system. The amount of these regulating hormones stays about the same, but the response
by the endocrine organs can change as we age.
The pituitary gland is also located in the brain. This gland reaches its maximum size in middle age and
then gradually becomes smaller. It has two parts:
• The back (posterior) part stores hormones produced in the hypothalamus.
PANGASINAN STATE UNIVERSITY 19
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
• The front (anterior) part produces hormones that affect growth, the thyroid gland (TSH), adrenal cortex,
ovaries, testes, and breasts.
The thyroid gland is located in the neck. It produces hormones that help control metabolism. With
aging, the thyroid may become lumpy (nodular). Metabolism slows over time, beginning at around age
20. Because thyroid hormones are produced and broken down (metabolized) at the same rate, thyroid
function tests are most often still normal. In some people, thyroid hormone levels may rise, leading to
an increased risk of death from cardiovascular disease.
The parathyroid glands are four tiny glands located around the thyroid. Parathyroid hormone affects
calcium and phosphate levels, which affect bone strength. Parathyroid hormone levels rise with age,
which may contribute to osteoporosis.
Insulin is produced by the pancreas. It helps sugar (glucose) go from the blood to the inside of cells,
where it can be used for energy.
The average fasting glucose level rises 6 to 14 milligrams per deciliter (mg/dL) every 10 years after age
50 as the cells become less sensitive to the effects of insulin.
The adrenal glands are located just above the kidneys. The adrenal cortex, the surface layer, produces
the hormones aldosterone, cortisol, and dehydroepiandrosterone.
• Aldosterone regulates fluid and electrolyte balance.
• Cortisol is the "stress response" hormone. It affects the breakdown of glucose, protein, and fat, and it
has anti-inflammatory and anti-allergy effects.
Aldosterone release decreases with age. This decrease can contribute to lightheadedness and a drop
in blood pressure with sudden position changes (orthostatic hypotension). Cortisol release also
decreases with aging, but the blood level of this hormone stays about the same.
Dehydroepiandrosterone levels also drop. The effects of this drop on the body are not clear.
The ovaries and testes have two functions. They produce the reproductive cells (ova and sperm). They
also produce the sex hormones that control secondary sex characteristics, such as breasts and facial
hair.
• With aging, men sometimes have a lower level of testosterone.
• Women have lower levels of estradiol and other estrogen hormones after menopause.
EFFECT OF CHANGES
Overall, some hormones decrease, some do not change, and some increase with age. Hormones that usually
decrease include:
-Aldosterone
-Calcitonin
-Growth hormone
-Renin
In women, estrogen and prolactin levels often decrease significantly.
Hormones that most often remain unchanged or only slightly decrease include:
- Cortisol
- Epinephrine
- Insulin
- Thyroid hormones T3 and T4
Testosterone levels usually decrease gradually as men age.
Hormones that may increase include:
Follicle-stimulating hormone (FSH)
Luteinizing hormone (LH)
Norepinephrine
Parathyroid hormone
PANGASINAN STATE UNIVERSITY 20
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
Key Medical Terms Associated with the Endocrine System
Acromegaly—Acromegaly is a hormonal disorder where the pituitary gland produces excess amounts
of growth hormone.
Adrenal Cortex—The adrenal cortex is the outer portion of the adrenal gland and it produces steroid
hormones, which regulate carbohydrate and fat metabolism, and mineralocorticoid hormones, which
regulate salt and water balance in the body.
Adrenal Glands—Adrenal glands are triangle-shaped glands that sit on top of the kidneys. They
regulate stress response through the synthesis of hormones, including cortisol and adrenaline.
Adrenaline—Adrenaline is a hormone that triggers the body’s fight-or-flight response. It is produced in
the medulla in the adrenal glands as well as some of the central nervous system’s neurons.
Adrenocorticotropin (ACTH)—Adrenocorticotropin is a hormone produced by the anterior pituitary
gland that stimulates the adrenal cortex.
Amenorrhea—Amenorrhea is the term used when a woman or adolescent girl is not having menstrual
periods.
Androgens—Androgens are hormones that help to develop sex organs in men. They also contribute
to sexual function in men and women.
Andropause—Andropause is a biological change characterized by a gradual decline in androgens
experienced by men during and after their mid-life. Andropause is sometimes inaccurately described
as male menopause.
Angiotensin—Angiotensin is the common name of four hormones: angiotensin I-IV, which play an
important role in the body’s overall health and blood pressure regulation.
Antiandrogens—Antiandrogens are substances that inhibit the biological effects of androgenic
hormones.
Benign Prostatic Hyperplasia (Enlarged Prostate)—Benign prostatic hyperplasia is non-
cancerous enlargement of the prostate gland, a common occurrence in older men.
Bioavailable Testosterone—Bioavailable testosterone represents the fraction of circulating
testosterone that readily enters cells and better reflects the bioactivity of testosterone than does the
simple measurement of serum total testosterone.
Bioidentical Hormones—Bioidentical hormones are compounds that have exactly the same
chemical and molecular structure as hormones that are produced in the human body. Though any
hormone can be made to be "bioidentical," the term is often used to describe allegedly custom-
compounded formulations containing estrogens, progesterone, and androgens. There is no evidence
that they are any safer or more effective than FDA-approved hormone preparations.
Bone Mineral Density—A bone mineral density (BMD) test measures the density of minerals (such as
calcium) in bones using a special X-ray, computed tomography (CT) scan, or ultrasound. This
information is used to estimate the strength of bones.
PANGASINAN STATE UNIVERSITY 21
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
Calcitonin—Calcitonin is a protein hormone secreted by cells in the thyroid gland. It inhibits cells that
break down bone and helps to regulate the blood’s calcium and phosphate levels.
Cholescystokinin—Cholecystokinin, otherwise known as CCK or CCK-PZ, is able to improve
digestion and affects appetite.
Cholesterol—Cholesterol is a white crystalline substance found in animal tissues and various foods
that is normally synthesized by the liver. Cholesterol levels can be a risk factor for heart disease.
Congenital Adrenal Hyperplasia—Congenital adrenal hyperplasia refers to a group of inherited
adrenal gland disorders. People with this condition do not produce enough of the
hormones cortisol and aldosterone, and produce too much of androgen.
Cortisol—Cortisol is a hormone produced by the adrenal gland. It is involved in the stress response
and increases blood pressure and blood sugar levels.
Cushing Syndrome—Cushing syndrome is a hormonal disorder caused by prolonged exposure of
the body's tissues to high levels of the hormone cortisol. Sometimes called "hypercortisolism," it is
relatively rare and most commonly affects adults aged 20 to 50.
Diabetes—Diabetes is a disease in which blood glucose levels are above normal. The body of a
person with diabetes either doesn't make enough insulin or can't use its own insulin as well as it should.
Dehydroepiandrosterone—Dehydroepiandrosterone (DHEA) is the highest circulating steroid
present in the human body. It is a precursor hormone that can be converted into hormones such as
testosterone and estradiol.
Dihydrotestosteronemdash;Dihydrotestosterone is a male hormone more potent than testosterone
that is converted from testosterone within the prostate.
Endocrine-disrupting Chemicals—Endocrine-disrupting chemicals (EDCs) are natural and man-
made chemicals that can either mimic, block, or disrupt the action of hormones. EDCs are associated
with numerous adverse human health issues, including reproductive health problems, obesity,
diabetes, hormone-related cancers, neurological issues, and other disorders.
Endocrinologist—Endocrinologists are specially trained physicians who diagnose diseases related
to the glands. Because these doctors specialize in these conditions, which can be complex and have
hard-to-spot symptoms, an endocrinologist is your best advocate when dealing with hormonal issues.
Erectile Dysfunction (ED)—Erectile dysfunction is the inability to achieve penile erection or to
maintain an erection until ejaculation.
Erythropoietin—Erythropoietin is a hormone directly connected to red blood cell production and
maintenance. Low levels of this hormone occur when someone has chronic kidney diseases.
Estradiol—Estradiol, a type of estrogen, is a female sex hormone produced mainly by the ovaries. It is
responsible for growth of breast tissue, maturation of long bones, and development of the secondary
sexual characteristics.
PANGASINAN STATE UNIVERSITY 22
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
Estrogen—Estrogens are a group of steroid compounds that are the primary female sex hormones.
They promote the development of female secondary sex characteristics and control aspects of
regulating the menstrual cycle.
Estrogen Therapy (ET)—Estrogen therapy is a hormone therapy treatment program in which women
take estrogen orally, transdermally, or vaginally to treat certain menopausal symptoms.
Estrone—Produced by the ovaries, the estrone hormone is one of three types of estrogen. It is a
weaker estrogen, commonly found in higher quantities in postmenopausal women.
Free Testosterone—Free testosterone is testosterone in the body that is biologically active and
unbound to other molecules in the body, such as sex hormone binding globulin.
Follicle Stimulating Hormone (FSH)—In women, FSH helps control the menstrual cycle and the
production of eggs by the ovaries. The amount of FSH varies throughout a woman's menstrual cycle
and is highest just before she ovulates. Problems with FSH release can contribute to female infertility.
In men, FSH helps control the production of sperm.
Gastrin—Gastrin is a hormone the stomach produces. When you eat, gastrin stimulates the release of
gastric acid, an important part of the digestive process.
Ghrelin —Ghrelin is central to appetite and the release of growth hormone. Produced in the
stomach and small intestine, ghrelin has been called the "hunger hormone" because of its role
in controlling appetite.
Glands—Glands produce and secrete hormones that the body uses for a wide range of functions.
These control many different bodily functions, including respiration, metabolism, reproduction, sensory
perception, movement, sexual development, and growth.
Glucagon—Glucagon is a hormone that works with other hormones and bodily functions to control
glucose levels in the blood. It comes from alpha cells found in the pancreas and is closely related to
insulin-secreting beta cells, making it a crucial component that keeps the body’s blood glucose levels
stable.
Glucagon-Like Peptide 1 – Glucagon-like peptide 1 (GLP-1) helps regulate your appetite, especially
after eating. It also helps enhance the production of insulin.
Gonads—A gonad is an organ that produces sperm and egg cells known as gametes. The gonads in
males are the testes, and the gonads in females are the ovaries.
Graves Disease—Graves disease is the most common form of hyperthyroidism. It occurs when your
immune system mistakenly attacks your thyroid gland and causes it to overproduce the hormone
thyroxine.
Growth Hormone—Growth hormone is a substance that controls your body’s growth. Growth
hormone is made by the pituitary gland, located at the base of the brain. Growth hormone helps
children grow taller, increases muscle mass, and decreases body fat.
Gynecomastia—Gynecomastia is breast enlargement in boys or men due to a benign increase in
breast tissue. This condition results from an imbalance between the hormones testosterone and
estrogen.
PANGASINAN STATE UNIVERSITY 23
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
Hirsutism—Hirsutism is excessive "male" pattern hair growth that appears on the face, back, chest,
abdomen, and thighs in women.
Hormones—Made by endocrine glands, hormones are chemical messengers that travel in the
bloodstream to tissues or organs. They affect many processes, including growth, metabolism, sexual
function, reproduction, and mood.
Hormone Therapy—Hormone therapy is the use of hormones in medical treatment. For example,
doctors may use hormone therapy to boost estrogen levels in menopausal women. Other examples
include thyroid hormone replacement for thyroid deficiency, insulin therapy for diabetes,
and transgender hormone therapy.
Hot Flashes—Hot flashes refer to the sudden wave of mild or intense body heat caused by dilation of
capillaries in the skin resulting from decreased levels of estrogen. Hot flashes affect about 75 percent
of women as they go through menopause.
Human Chorionic Gonadotropin Hormone—The human chorionic gonadotropin (hCG) hormone
is important in the early stages of pregnancy. It is produced by cells that are surrounding a growing
embryo, which eventually forms the placenta.
Hypoglycemia—Hypoglycemia, also called low blood sugar, occurs when your blood glucose level
drops too low to provide enough energy for your body's activities. Patients with severe hypoglycemia
may experience unconsciousness or seizures due to low blood sugar.
Hypogonadism—Hypogonadism, or low testosterone, occurs when a man’s testes fail to produce
sufficient quantities of testosterone and/or sperm quality is impaired.
Hypothalamus—The hypothalamus is an area of the brain that regulates vital autonomic centers and
produces hormones that control thirst, hunger, body temperature, sleep, moods, sex drive, and the
release of hormones from various glands, primarily the pituitary gland.
Insulin—Insulin is a protein pancreatic hormone involved in the metabolism of carbohydrates and the
regulation of glucose levels in the blood. Diabetes occurs when the body doesn’t produce enough
insulin or use the hormone effectively.
IGF-1—IGF-1, or insulin-like growth factor 1, is a polypeptide protein hormone similar in molecular
structure to insulin. It plays an important role in childhood growth and continues to have anabolic
effects in adults. IGF-1 has been identified as a performance-enhancing drug.
SUMMARY
Nervous system
The nervous system has two distinct parts: the central nervous system (the brain and spinal cord)
and the peripheral nervous system (the nerves outside the brain and spinal cord).
The basic unit of the nervous system is the nerve cell (neuron). Nerve cells consist of a large cell
body and two types of nerve fibers:
• Axon: One elongated extension for sending messages as electrical impulses
• Dendrites: Usually many branches for receiving impulses
Normally, nerves transmit impulses electrically in one direction—from the impulse-sending axon of
one nerve cell (also called a neuron) to the impulse-receiving dendrites of the next nerve cell. At
PANGASINAN STATE UNIVERSITY 24
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
contact points between nerve cells, (synapses), the axon secretes tiny amounts of chemical
messengers (neurotransmitters). Neurotransmitters trigger the receptors on the next nerve cell
dendrites to produce a new electrical current. Different types of nerves use different
neurotransmitters to convey impulses across the synapses. Some of the impulses stimulate the next
nerve cell, whereas others inhibit it.
The brain and spinal cord also contain support cells called glial cells. There are several types,
including the following:
• Astrocytes: These cells provide nutrients to nerve cells and control the chemical composition
of fluids around nerve cells, enabling them to thrive. They also influence how often nerve cells
send impulses and thus regulate how active groups of nerve cells may be.
• Oligodendrocytes: These cells make myelin, a fatty substance that insulates nerve axons and
speeds the conduction of impulses along nerve fibers.
• Glial progenitor cells: These cells can produce new astrocytes and oligodendrocytes to
replace those destroyed by injuries or disorders. Glial progenitor cells are present throughout
the brain in adults.
• Microglia: These cells help protect the brain against infection and help remove debris from
dead cells.
The brain and spinal cord consist of gray and white matter.
Gray matter consists of nerve cell bodies, dendrites and axons, glial cells, and capillaries (the
smallest of the body’s blood vessels).
White matter contains relatively very few neurons and consists mainly of axons that are wrapped
with many layers of myelin and of the oligodendrocytes that make the myelin. Myelin is what makes
the white matter white. (Myelin speeds the conduction of nerve impulses)
Nerve cells routinely increase or decrease the number of connections they have with other nerve
cells. This process may partly explain how people learn, adapt, and form memories. But the brain and
spinal cord rarely produce new nerve cells. An exception is the hippocampus, an area of the brain
involved in memory formation.
The nervous system is an extraordinarily complex communication system that can send and receive
voluminous amounts of information simultaneously. However, the system is vulnerable to diseases
and injuries, as in the following examples:
• Nerve cells can degenerate, causing Alzheimer disease, Huntington disease, or Parkinson
disease.
• Oligodendrocytes may become inflamed and lost, causing multiple sclerosis.
• Bacteria or viruses can infect the brain or spinal cord, causing encephalitis or meningitis.
• A blockage in the blood supply to the brain can cause a stroke.
• Injuries or tumors can cause structural damage to the brain or spinal cord.
The Sensory System
The sensory system is a group of subsystems used for detecting and understanding the world around
you. We just discussed the auditory and the visual system in brief, but there is also smell, taste,
balance, proprioception (or the position of your body), and at least half a dozen types of touch
sensations.
I was doing some thinking as I wrote this, and I realized you've already been handed the sensory
systems as discrete units - the eyes do this; the ears do that. You've most likely had that kind of
information before. What you haven't had is a holistic view of how these systems are similar. Let's look
at the systems as a whole and maybe shake up some stuff.
PANGASINAN STATE UNIVERSITY 25
FM-AA-CIA-15 Rev. 0 10-July-2020
Study Guide in Sci 120 – ANATOMY and PHYSIOLOGY Module No. 3
Receptors
What makes the sensory system unique is its ability to sense things, which sounds kind of stupid and
'no duh' because you haven't ever realized how limited your sensory organs are. Let's say I have a
chopstick, one chopstick, and some local anesthetic. I spray the anesthetic on your scalp and proceed
to cut a hole in your head, exposing your brain. I then take my chopstick and push it into your brain. My
question is, 'What do you feel?'
The answer is, 'Nothing.' Your brain doesn't feel pain, pressure, or touch. Your brain, the great and
powerful human brain, lacks receptors, which are specialized neurons designed to obtain a particular
type of information that is then sent to a particular part of the brain. Your brain, which interprets pain,
does not actually feel pain. There are no pain receptors in your brain.
If you find this a bit maddening and hard to believe, you aren't alone. Many people I have met in
graduate school find this impossible. Receptors have been divided up into five different types. Let's look
at each one and which sensory system they can be found in:
• Chemoreceptors detect ionic and molecular changes or presence. Think smell and taste.
• Mechanoreceptors detect changes and fluctuations in pressure, position, and movement.
Think hearing, touch, balance, and stretching.
• Electromagnetic receptors detect light, radiation, and magnetic fields. Humans only have
visible light detection in their eyes, but sharks have specialized organs for detecting bodily
electricity.
• Thermoreceptors detect hot and cold temperatures. Obviously, this is a temperature detection,
both of the outside world and inside the body, since you need to keep a constant temperature.
• Pain receptors detect pressure, chemicals, and severe heat. These are found all over your skin
and tell you if something is wrong.
Signals
When a receptor is triggered, it sends a signal. How the receptor is triggered, though, depends on what
type it is. Let's look at a fairly common way and then in a more unusual way.
The Endocrine System
The endocrine system is a system of ductless glands that secretes hormones directly into the
circulatory system to be carried long distances to other target organs regulating key body and organ
functions. For example, the pineal gland, located at the base of the brain, secretes the hormone
melatonin, responsible for regulating sleep patterns.
Endocrine glands are typically well vascularized and the cells comprising the tissue are typically rich in
intracellular vacuoles or granules that store hormones prior to release. Endocrine signaling is typically
slow to initiate but is prolonged in response; this provides a counterpoint to the more rapid and short-
lived nervous system signals.
The endocrine system is in contrast to the exocrine system, which features ducted glands that secrete
substances onto an epithelial surface; for example, a sweat gland. Additionally the endocrine system is
differentiated from shorter distance signaling such as autocrine (a cell affecting itself), juxtacrine (a cell
affecting it’s direct neighbors), and paracrine (a cell affecting other nearby cells) signaling.
Key Endocrine Glands
The major endocrine glands include the pituitary, pineal, ovaries, testes, thyroid, hypothalamus and
adrenal glands, additionally other tissues such as the kidney and liver also display secondary adrenal
functions.
PANGASINAN STATE UNIVERSITY 26
You might also like
- Nervous System NotesDocument6 pagesNervous System NotesAlex Whitwam100% (3)
- Plasticity FascialDocument13 pagesPlasticity FascialMichael DuranNo ratings yet
- Harrys CosmetologyDocument80 pagesHarrys CosmetologyNidhi100% (3)
- Nervous System - Cabil (G6)Document96 pagesNervous System - Cabil (G6)Lady Ann CabilNo ratings yet
- 2 Neurophysiology of Somatic Sensations 2012Document6 pages2 Neurophysiology of Somatic Sensations 2012Nephritery Joy Espiritu JimenezNo ratings yet
- Physiology & Anatomy Nervous System: MuscleDocument2 pagesPhysiology & Anatomy Nervous System: MuscleEllah GutierrezNo ratings yet
- Sensory and Motor SystemDocument12 pagesSensory and Motor SystemrobertoNo ratings yet
- @MBS MedicalBooksStore 2019 Pain PDFDocument499 pages@MBS MedicalBooksStore 2019 Pain PDFRay MaudyNo ratings yet
- Proprioception Changes With InjuryDocument32 pagesProprioception Changes With InjuryGeorge M. PamborisNo ratings yet
- Oral Physiology and Occlusion ReviewerDocument100 pagesOral Physiology and Occlusion ReviewerNUELLAELYSSE DELCASTILLO100% (3)
- UNIT 4 (Nervous System)Document14 pagesUNIT 4 (Nervous System)Workinesh Kaynabo KambaloNo ratings yet
- Physiology Chapter 1 & 2 ReviewDocument193 pagesPhysiology Chapter 1 & 2 ReviewRichardNo ratings yet
- Articular NeurologyDocument14 pagesArticular Neurologykinj100% (1)
- Ganong 23rd Ed End of Chapter Questions WITH ANSWERSDocument20 pagesGanong 23rd Ed End of Chapter Questions WITH ANSWERSGianina RafaelNo ratings yet
- CNS 1 - Part 1Document151 pagesCNS 1 - Part 1Qamariah IbrahimNo ratings yet
- Oral Exam ReviewerDocument48 pagesOral Exam ReviewerFayena JoseNo ratings yet
- Organization of the Nervous System: Neurons, Glia & ClassificationDocument33 pagesOrganization of the Nervous System: Neurons, Glia & ClassificationOctavio Mancini100% (2)
- Chapter 12 - An Introduction To The Nervous System: Peripheral Nerves)Document7 pagesChapter 12 - An Introduction To The Nervous System: Peripheral Nerves)tomorrow.today.yesterday .yesterdayNo ratings yet
- Chapter 2 NeuroscienceDocument5 pagesChapter 2 NeuroscienceMarco RagaNo ratings yet
- IM AnSci 111 Module 3Document21 pagesIM AnSci 111 Module 3Riza Mae Duran RangasNo ratings yet
- ANP PHYSIOLOGYDocument8 pagesANP PHYSIOLOGYElijah KamaniNo ratings yet
- General Psychology - Biological FoundationDocument55 pagesGeneral Psychology - Biological FoundationKomala PodapatiNo ratings yet
- 4.nervous System IDocument12 pages4.nervous System IPatricia TeyeNo ratings yet
- Anatomy of The Sympathetic Nervous SystemDocument12 pagesAnatomy of The Sympathetic Nervous SystemNanda 9300No ratings yet
- NUR112 Nervous System OverviewDocument30 pagesNUR112 Nervous System OverviewAngel CauilanNo ratings yet
- Nervous System - All NotesDocument6 pagesNervous System - All NotesJNo ratings yet
- Oral Exam ReviewerDocument39 pagesOral Exam ReviewerFayena JoseNo ratings yet
- FINALS 2 5-Nervoustissue-161014172642Document56 pagesFINALS 2 5-Nervoustissue-161014172642Maika Ysabelle RavaloNo ratings yet
- CNS NoteDocument203 pagesCNS NoteAhmad Khair Ahmad BazliNo ratings yet
- Integration and Coordination - SG3Document180 pagesIntegration and Coordination - SG3Marcos AlbaridaNo ratings yet
- Autonomic Nervous System: Prof. DRDocument65 pagesAutonomic Nervous System: Prof. DRGo HellNo ratings yet
- Lesson 7 Part I Control and CoordinationDocument6 pagesLesson 7 Part I Control and CoordinationDragonAffire 1No ratings yet
- Asia Pacific College of Advanced Studies A.H. Banzon ST, Ibayo, Balanga CityDocument7 pagesAsia Pacific College of Advanced Studies A.H. Banzon ST, Ibayo, Balanga CityLore Anne Mhae SantosNo ratings yet
- Nervous Tissue (NT) : Functions of Nerve TissueDocument14 pagesNervous Tissue (NT) : Functions of Nerve TissuekimNo ratings yet
- Topic 3 - Nervous Control in Plants and AnimalsDocument5 pagesTopic 3 - Nervous Control in Plants and AnimalsYara Jeah Ingay BaliliNo ratings yet
- CNS 1Document63 pagesCNS 1Prabhu KiranNo ratings yet
- Chapter 12 Neural TissueDocument15 pagesChapter 12 Neural TissueKatherine De San AgustinNo ratings yet
- Introduction To The Nervous System and Nerve TissueDocument42 pagesIntroduction To The Nervous System and Nerve TissueNicole Anne TungolNo ratings yet
- Neurology HandbookDocument28 pagesNeurology HandbookPeter KaiserNo ratings yet
- hphy228Document12 pageshphy228moses samuelNo ratings yet
- General Biology 2: 2 Quarter - Module 2Document2 pagesGeneral Biology 2: 2 Quarter - Module 2Veronica RojasNo ratings yet
- Nervous SystemDocument15 pagesNervous SystemSatrioNo ratings yet
- Nervious System 2Document12 pagesNervious System 2Amina DinarNo ratings yet
- Nervous System and Brain Structures OverviewDocument43 pagesNervous System and Brain Structures OverviewDweep BajajNo ratings yet
- Nervous System1Document43 pagesNervous System1human anatomy100% (1)
- ???????-??????-H.-Idris-N.-Macmod-A.-Mangondato-M.-OmarDocument70 pages???????-??????-H.-Idris-N.-Macmod-A.-Mangondato-M.-OmarHestia GreyertNo ratings yet
- CH 7 The Nervous System NotesDocument21 pagesCH 7 The Nervous System Notesbiswa217No ratings yet
- Anatomical Divisions of The Nervous SystemDocument11 pagesAnatomical Divisions of The Nervous SystemDamianNo ratings yet
- Module 9-10Document8 pagesModule 9-10alexandra martinNo ratings yet
- Nervous SystemDocument69 pagesNervous SystemZekiah MagsayoNo ratings yet
- Study Guide 5Document39 pagesStudy Guide 5Amina Rose AlghamdiNo ratings yet
- 2 NSDocument65 pages2 NSLilaNo ratings yet
- Week 004 Animal-Nervous-SystemDocument8 pagesWeek 004 Animal-Nervous-SystemMark Lorens StaanaNo ratings yet
- The Nervous System-13 Dr. Hazim AL-RawiDocument16 pagesThe Nervous System-13 Dr. Hazim AL-RawiDrAli Al-FendiNo ratings yet
- HHB1070 Cells DefinitionsDocument3 pagesHHB1070 Cells DefinitionsgeorgeNo ratings yet
- G10-Science-Q3-Week-3-Nervous-SystemDocument29 pagesG10-Science-Q3-Week-3-Nervous-Systemhimotoumaruchan009No ratings yet
- ANSDocument7 pagesANSKim VilleneuveNo ratings yet
- Nervous System Physiology Lectures: 2 Year English ModuleDocument25 pagesNervous System Physiology Lectures: 2 Year English Moduleaqwe11No ratings yet
- Summary NeurobiologyDocument42 pagesSummary NeurobiologytjNo ratings yet
- S6 BIO (Nervous Coordination) Part2Document35 pagesS6 BIO (Nervous Coordination) Part2ivanpatrick658No ratings yet
- PSYCHOLOGYDocument6 pagesPSYCHOLOGYgunjandas7846No ratings yet
- Unit 2 - Nervous SystemDocument39 pagesUnit 2 - Nervous SystemzulieyanaNo ratings yet
- LG-4 Nervous TissueDocument32 pagesLG-4 Nervous TissueAnonymous gh5UWZJSNo ratings yet
- Discussion Notes (Anaphy)Document49 pagesDiscussion Notes (Anaphy)jade tanNo ratings yet
- The Nervous SystemDocument124 pagesThe Nervous SystemKeanan GwapoNo ratings yet
- Unit A - The Nervous and Endocrine SystemsDocument54 pagesUnit A - The Nervous and Endocrine Systemsdutritinh0806No ratings yet
- Module 2: Physiological Basis of BehaviorDocument23 pagesModule 2: Physiological Basis of BehaviorRoxie May Theresse AbagatnanNo ratings yet
- Nerve SystemDocument5 pagesNerve SystemRekesh SaeedNo ratings yet
- The Nervous SystemDocument69 pagesThe Nervous SystemKilles SmileNo ratings yet
- FS1 Activity 3Document15 pagesFS1 Activity 3Fatima SorianoNo ratings yet
- Assessing Learning OutcomesDocument8 pagesAssessing Learning OutcomesAirabellNo ratings yet
- Module 1 Entrepreneurship Its Opportunities and RewardsDocument6 pagesModule 1 Entrepreneurship Its Opportunities and RewardsWanda CaserNo ratings yet
- (REVIWER) TTL For Unit TestDocument5 pages(REVIWER) TTL For Unit TestREGINA MAE JUNIONo ratings yet
- LP Ni SirDocument2 pagesLP Ni SirREGINA MAE JUNIONo ratings yet
- 10 Principles For BuildingDocument19 pages10 Principles For BuildingREGINA MAE JUNIONo ratings yet
- Environmetal ScienceDocument8 pagesEnvironmetal ScienceREGINA MAE JUNIONo ratings yet
- RIZAL (Chapter 2) ReviewerDocument28 pagesRIZAL (Chapter 2) ReviewerREGINA MAE JUNIONo ratings yet
- Atmospheric Pressure and Wind: Study Guide For Module No. 3Document11 pagesAtmospheric Pressure and Wind: Study Guide For Module No. 3REGINA MAE JUNIONo ratings yet
- Chapter 3: Chemical Basis of Heredity: Study Guide For Module No.Document13 pagesChapter 3: Chemical Basis of Heredity: Study Guide For Module No.REGINA MAE JUNIONo ratings yet
- Earth's Energy and Seasons: Science 111: METEOROLOGY Irene J. Urbano InstructorDocument15 pagesEarth's Energy and Seasons: Science 111: METEOROLOGY Irene J. Urbano InstructorREGINA MAE JUNIONo ratings yet
- Study Guide For Module No. 2: Earth's Energy and SeasonsDocument9 pagesStudy Guide For Module No. 2: Earth's Energy and SeasonsREGINA MAE JUNIONo ratings yet
- ANA 6.01 General Somatic Afferents Dr. EsguerraDocument22 pagesANA 6.01 General Somatic Afferents Dr. EsguerraNinna Ricci San JuanNo ratings yet
- Physiology ReviewDocument424 pagesPhysiology ReviewLytiana WilliamsNo ratings yet
- Workshop ProceedingsDocument71 pagesWorkshop ProceedingsAndualem TadesseNo ratings yet
- Somatosensory function and sensationDocument25 pagesSomatosensory function and sensationAhmed TarekNo ratings yet
- Sensory Nerve Sprouting May Improve Merkel Cell Survival Independent of Direct ContactDocument8 pagesSensory Nerve Sprouting May Improve Merkel Cell Survival Independent of Direct Contactsaito sakaguchiNo ratings yet
- Assuit - MCQs (NeDocument84 pagesAssuit - MCQs (NeMax TraderNo ratings yet
- Midterm 1 2017 questionsDocument11 pagesMidterm 1 2017 questionsDerrick ThompsonNo ratings yet
- Loomis Leder Man Handbook GoodDocument41 pagesLoomis Leder Man Handbook Goodp223884894No ratings yet
- Active Touch Sensing PDFDocument174 pagesActive Touch Sensing PDFmb1979dz7828No ratings yet
- Notes On CNS Physiology by Medical Study CenterDocument99 pagesNotes On CNS Physiology by Medical Study CenterHifza Faqeer KambohNo ratings yet
- Comparative Animal Physiology Class SyllabusDocument82 pagesComparative Animal Physiology Class SyllabusJoe Xavier ReidyNo ratings yet
- Multiple Choice Questions: A. B. C. DDocument37 pagesMultiple Choice Questions: A. B. C. DwanderagroNo ratings yet
- The Giant First YearDocument1,234 pagesThe Giant First YearEthan DyerNo ratings yet
- Nsci Exam 3 Study SheetDocument8 pagesNsci Exam 3 Study SheetHan TaubNo ratings yet
- Periodontal ReceptorsDocument18 pagesPeriodontal Receptorsrozha88% (16)
- Articular NeurologyDocument11 pagesArticular NeurologyMitali ChhayaNo ratings yet
- Kinesiotaping Fundamentalsforthe Equineathlete: Sybille MolleDocument11 pagesKinesiotaping Fundamentalsforthe Equineathlete: Sybille MolleAnnisa Rahma SariNo ratings yet
- Kinesiotaping TechniquesDocument26 pagesKinesiotaping TechniquesSuhana hidayat100% (1)
- HCI Chap 2Document37 pagesHCI Chap 2alemneh bayehNo ratings yet
- Somatovisceral Sensory Physiology: The Sensory Modality Sensory Pathway PainDocument29 pagesSomatovisceral Sensory Physiology: The Sensory Modality Sensory Pathway PainDean100110No ratings yet