Professional Documents
Culture Documents
Mechanical Ventilation: Weaning From Mechanical Ventilation Kathia Ortiz-Cantillo, MD
Uploaded by
sarev0 ratings0% found this document useful (0 votes)
34 views25 pagesThe document discusses criteria for assessing a patient's readiness to be weaned from mechanical ventilation, including parameters related to respiratory muscle strength and demand, gas exchange, and methods of gradual weaning using approaches like pressure support ventilation. Factors that could lead to weaning failure are also outlined, as well as potential complications associated with prolonged mechanical ventilation. The goal is to determine when a patient's underlying condition has stabilized enough to allow a trial of breathing without the ventilator.
Original Description:
Original Title
6927696 Mechanical Ventilation
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document discusses criteria for assessing a patient's readiness to be weaned from mechanical ventilation, including parameters related to respiratory muscle strength and demand, gas exchange, and methods of gradual weaning using approaches like pressure support ventilation. Factors that could lead to weaning failure are also outlined, as well as potential complications associated with prolonged mechanical ventilation. The goal is to determine when a patient's underlying condition has stabilized enough to allow a trial of breathing without the ventilator.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
34 views25 pagesMechanical Ventilation: Weaning From Mechanical Ventilation Kathia Ortiz-Cantillo, MD
Uploaded by
sarevThe document discusses criteria for assessing a patient's readiness to be weaned from mechanical ventilation, including parameters related to respiratory muscle strength and demand, gas exchange, and methods of gradual weaning using approaches like pressure support ventilation. Factors that could lead to weaning failure are also outlined, as well as potential complications associated with prolonged mechanical ventilation. The goal is to determine when a patient's underlying condition has stabilized enough to allow a trial of breathing without the ventilator.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 25
Mechanical Ventilation
Weaning from Mechanical
Ventilation
Kathia Ortiz-Cantillo, MD
Mechanical Ventilation
Weaning
• When is a patient ready to be disconnected
from the ventilator?
• Numerous trials performed to develop criteria for
success weaning, however, not useful to predict
when to begin the weaning.
• Physicians must rely on clinical judgment.
• Reversal of initial process that led to respiratory
failure
• Daily screening may reduce the duration of MV
and ICU cost
Mechanical Ventilation
factors that should be corrected before weaning
• CNS; Absence of cough, gag, level of
consciousness
• CVS; Shock, arrhythmias
• Renal; Correction of acid-base/electrolyte disorders
• Hematologic; Anemia
• Infections;
• Nutrition; Poor nutritional status, low phosphorus,
excessive nutrition.
Mechanical Ventilation
Weaning Parameters
• Respiratory Muscle Strength:
• NIF; maximum inspiratory pressure:
• PImax generated by a patient from FRC approximately
20 sec after occluding the inspiratory circuit.
• Index of Rapid Shallow Breathing:
• RR/TV. Inspiratory muscle weakness leads to rapid
shallow breathing
• Paradoxical Breathing:
• Chest and abdomen move outward on inspiration.
• Intercostal muscle fatigue, diaphragmatic fatigue.
Mechanical Ventilation
Weaning Parameters
• Respiratory Muscle Strength
• Vital Capacity VC >15mL/kg body weight
• The maximum amount of gas that can be inhaled from
residual volume or exhaled from total lung capacity
• Requires patient cooperation
Mechanical Ventilation
Weaning Parameters
• Respiratory Muscle Demand
• Minute Ventilation VE;
• the amount of air that must be moved in or out of the
lungs over 1 min to maintain a given PaCO2.
<10L/min
• VE will be determined by CO2 production
• Increased on critical care illness, high fever, over
feeding, excess carbohydrate load, Increase death
space.
• RR;
• Muscle fatigue, patient resorts shallow breathing >35
Mechanical Ventilation
Weaning Parameters
• Respiratory Muscle Demand
• Maximum Voluntary Ventilation; MVV >2 times
the VE
• Requires a motivated and cooperative patient
• The maximum amount of air that can be inhaled or
exhaled over 1 min.
• Respiratory Compliance >33ml/cmH2O
• Work must be performed by inspiratory muscles to
overcome the elastic properties of both the lungs and
chest wall.
Mechanical Ventilation
Weaning Parameters
• Respiratory Gas Exchange
• Significant hypoxemia constitutes a relative
contraindication.
• A PaO2 <60mmHG with and FIO2>.040.
• Arterial to Inspired O2 ratio (PaO2/FIO2)
• >200
Mechanical Ventilation
Weaning Parameters
• Respiratory Rate < 30/min
• Spontaneous Vt > 4 ml/kg
• Inspiratory Pressure > - 30 cm H2O
• Breathing Index (f/Vt) < 105
• PEEP < 8 cmH2O
• PaO2/FIO2 > 200
• FIO2 < .50
Mechanical Ventilation
Methods of weaning
• No one or method of weaning has been
definitely found to be superior:
• Initial Trial of Spontaneous Ventilation
• T-piece trial
• Spontaneous trial on ventilator (CPAP = 0)
• Gradual Weaning
• SIMV
• Pressure Support Ventilation (PSV)
• SIMV + PSV
• Extubation + noninvasive ventilation
Weaning
Pressure Support Ventilation (PSV)
• Fixed pressure during inspiration
• Patient initiated and terminated
• More comfortable
• Depth & length of breath controlled by patient
• Counteract work/resistance of ETT &
ventilator circuit
SIMV Protocol
• Switch to SIMV from assist mode or decrease
RR
• Begin with RR 8/min decrease SIMV rate by
two breaths per hour unless clinical
deterioration
• if assume to fail, increase SIMV rate to
previous level, until stable
• if stable at least 1 hour of rate 0/ min extubate
• in patient without respiratory disorders,
decrease rate with half an hour interval, 2 hr
extubate
Weaning
ACCP/AARC
A. Stable/resolved pulmonary process
B. PEEP < 8; FIO2 < .50
C. Cardiovascular stability
D. Spontaneous breathing trial
A. T-piece or PSV (~ 5 cm H2O)
B. Up to 2 hours every 24 hrs.
Weaning
• How often will the patient need to be re-
intubated?
• Accepted rate: 5% - 15%
Failed to Wean
• Associated with intrinsic lung disease
• Associated with prolonged critical illness
• Increased risk in patient with longer
duration of mechanical ventilation
• Increased risk of complications, mortality
Weaning
Failure Criteria
• Rapid shallow breathing
• RR > 35/min or > 10/min increase
• Tachycardia
• > 120 bpm or > 20 bpm increase
• BP change > 20%
• Mental status change
Weaning
Failure Criteria
• Clinical signs of distress:
• Increased dyspnea
• Diaphoresis
• Accessory muscle use
• Paradoxical breathing
• Hypoxemia and/or hypercapnea
Fatigue Criteria
•Hypoxia (PaO2 < 60, SpO2 <90%) 11 (31%)
•Hypercarbia (PaCO2 > 50 mmHg) 9 (25%)
•Pulse rate > 120/min 17 (47%)
•SBP > 180 or < 90 mmHg 2 (6%)
•Respiratory rate > 30/min 33 (92%)
•Clinical respiratory distress 27 (75%)
Evidence-based medicine
• Patients receiving MV who fail an SBT
should have the cause determined.
• Once causes are corrected, and if the patient
still meets the criteria of DS, subsequent
SBTs should be performed every 24 hours.
Weaning
Failure to Wean
• Auto-PEEP
• Cardiac disease
• CHF, ischemic heart disease
• Nutrition and electrolyte imbalance
• Inadequate rest following previous trial
• May need up to 24 hours
• Muscle weakness
• Paralysis or polyneuropathy of critical illness
Mechanical Ventilation
Complications
• Barotrauma
• 4% - 15%
• Highest in ARDS
• Reductions in cardiac output
• Impaired right ventricular preload
Mechanical Ventilation
Complications
• Renal effects
• GI bleeding
• 20% - 30% without prophylaxis
• DVT
• 40% - 80% without prophylaxis
• Ventilator induced pneumonia
Mechanical Ventilation
Sudden Airway Pressure
• Tension pneumothorax
• ETT/tubing obstruction
• Mucous plugging - common
• Acute bronchospasm
• Mainstem migration of ETT
You might also like
- Kriya - Three Exercises For Energy, Creativity and ProsperityDocument2 pagesKriya - Three Exercises For Energy, Creativity and Prosperitydrundrun100% (1)
- Weaning from Mechanical Ventilation ProtocolsDocument37 pagesWeaning from Mechanical Ventilation ProtocolsNadiya AshifNo ratings yet
- Basics of Ventilatory SupportDocument43 pagesBasics of Ventilatory SupportAdhithya BhatNo ratings yet
- WEANING FROM MECHANICAL VENTILATION GUIDEDocument55 pagesWEANING FROM MECHANICAL VENTILATION GUIDEKamal Mohamed100% (1)
- Weaning From Mechanical VentilationDocument33 pagesWeaning From Mechanical VentilationMuhammad UmairNo ratings yet
- Mechanical Ventilation, Pulmonary Rehab & Patient CareDocument35 pagesMechanical Ventilation, Pulmonary Rehab & Patient Careadamu mohammadNo ratings yet
- Basics of Mechanical Ventilation: Pediatric Critical Care DivisionDocument41 pagesBasics of Mechanical Ventilation: Pediatric Critical Care DivisionKatrina PiczonNo ratings yet
- Mechanical Ventilation Handout - AllenhoDocument22 pagesMechanical Ventilation Handout - Allenhofriyaz8197100% (1)
- Mechanical Ventilation 101: DR Paul Healey ICU Fellow John Hunter Hospital NewcastleDocument95 pagesMechanical Ventilation 101: DR Paul Healey ICU Fellow John Hunter Hospital NewcastlePatrick ValentinoNo ratings yet
- Mechanical Ventilation Handout - AllenhoDocument23 pagesMechanical Ventilation Handout - AllenhoCarmen HerediaNo ratings yet
- Which Dial Do I Turn!? Essence of Mechanical VentilationDocument54 pagesWhich Dial Do I Turn!? Essence of Mechanical VentilationKang Wisit TheaNo ratings yet
- Initiating of Mechanical Ventilation 7-3-10Document38 pagesInitiating of Mechanical Ventilation 7-3-10KrysnaNo ratings yet
- Mechanical Ventilation: EMS Professions Temple CollegeDocument27 pagesMechanical Ventilation: EMS Professions Temple Collegemarie100% (2)
- Weaning From Mechanical VentilationDocument25 pagesWeaning From Mechanical VentilationSaras SinghNo ratings yet
- Mechanical Ventilation 8.2.17Document41 pagesMechanical Ventilation 8.2.17SyafiqAziziNo ratings yet
- Mechanical Ventilation Handout - AllenhoDocument23 pagesMechanical Ventilation Handout - AllenhoTahani SulNo ratings yet
- Nursing Care of Ventilated PatientDocument53 pagesNursing Care of Ventilated PatientVenkatesan Annamalai100% (2)
- CPAP SlidesDocument52 pagesCPAP SlidesAnusha Verghese100% (1)
- Mechanical Ventilation Settings and Parameters/TITLEDocument71 pagesMechanical Ventilation Settings and Parameters/TITLESonaly KoiriNo ratings yet
- Basic Mecahnical Ventilation - Critical Concepts - PulmonaryDocument54 pagesBasic Mecahnical Ventilation - Critical Concepts - PulmonaryMarcela Catalina Fandiño VargasNo ratings yet
- DT Ventilasi MekanikDocument53 pagesDT Ventilasi MekanikRadinal MauludiNo ratings yet
- Approaches For AsthmaDocument35 pagesApproaches For AsthmaasupicuNo ratings yet
- Introduction To Invasive VentilationDocument29 pagesIntroduction To Invasive VentilationfdvojmocNo ratings yet
- Mechanical Ventilation 1Document59 pagesMechanical Ventilation 1Deepak Solanki100% (1)
- Ventilator, Weaning, SuctioningDocument81 pagesVentilator, Weaning, SuctioningwaqarNo ratings yet
- Basic Modes of Mechanical VentilationDocument52 pagesBasic Modes of Mechanical VentilationSuma AhmadNo ratings yet
- Invasive Respiratory Support - SeblewongelDocument34 pagesInvasive Respiratory Support - SeblewongelSeblewongel AsemeNo ratings yet
- Lp3 Ventilatia MecanicaDocument43 pagesLp3 Ventilatia MecanicaAlexandra SerbanNo ratings yet
- 4 Weaning Ventilator-NIADocument31 pages4 Weaning Ventilator-NIAResyana Widyayani100% (1)
- EX Basics of Mechanical VentilationDocument32 pagesEX Basics of Mechanical VentilationNahom GirmaNo ratings yet
- Nursing Care of Clients On Mechanical Ventilator For BSN IV StudentsDocument52 pagesNursing Care of Clients On Mechanical Ventilator For BSN IV Studentsspanishthingz01No ratings yet
- Guidelines of Mechanic Ventilation in Newborn InfantsDocument62 pagesGuidelines of Mechanic Ventilation in Newborn InfantsJairo UrielNo ratings yet
- Stewart 9 Artifact2Document9 pagesStewart 9 Artifact2api-260357356No ratings yet
- ARDS / COVID General ManagementDocument45 pagesARDS / COVID General ManagementJoe WildNo ratings yet
- Presentation 1Document22 pagesPresentation 1ANT-Sudais UddinNo ratings yet
- 13.acute Respiratory FailureDocument34 pages13.acute Respiratory Failurekarim hassan100% (1)
- Difficult Weaning in COVID 19Document53 pagesDifficult Weaning in COVID 19rkapatworkNo ratings yet
- Mechanical VentilationDocument52 pagesMechanical VentilationShaliniNo ratings yet
- Introduction To Pediatric VentilationDocument41 pagesIntroduction To Pediatric Ventilationedderj2585No ratings yet
- Weaning From VentilatorDocument45 pagesWeaning From VentilatorJerinNo ratings yet
- Mechanical Ventilation: Kenney Weinmeister M.DDocument36 pagesMechanical Ventilation: Kenney Weinmeister M.DAjay PrasadNo ratings yet
- Respiratory FailureDocument22 pagesRespiratory Failureeiuj497No ratings yet
- Intra-Operative PEEP Vs ZEEPDocument37 pagesIntra-Operative PEEP Vs ZEEPMohamed RifanNo ratings yet
- Weaning Ventilator Protocol For LiberationDocument3 pagesWeaning Ventilator Protocol For LiberationBonny ChristianNo ratings yet
- Ventilasi MekanikDocument47 pagesVentilasi MekanikzahrahNo ratings yet
- Mechanical VentilationDocument86 pagesMechanical Ventilationremjith rajendranNo ratings yet
- Ventilator BasicsDocument38 pagesVentilator Basicsgina contrerasNo ratings yet
- Icu Initial Ventilator SettingsDocument40 pagesIcu Initial Ventilator SettingsantreaspetsasNo ratings yet
- Mechanical VentilationDocument43 pagesMechanical VentilationdesikristiyantiNo ratings yet
- Understanding Mechanical Ventilation Modes & WeaningDocument52 pagesUnderstanding Mechanical Ventilation Modes & WeaningDeepa BhattacharjeeNo ratings yet
- Ventilator - ken sarasDocument41 pagesVentilator - ken sarasAlvian DwiNo ratings yet
- Weaning From Mechanical Ventilation: Moderator - Dr. Arvind Khare Presented by - Dr. Aji Kumar JLN Medical College, AjmerDocument28 pagesWeaning From Mechanical Ventilation: Moderator - Dr. Arvind Khare Presented by - Dr. Aji Kumar JLN Medical College, AjmerDiadema BorjaNo ratings yet
- Mechanical Ventilation For NursingDocument55 pagesMechanical Ventilation For NursingAmira AttyaNo ratings yet
- Mechanical Ventilation - Monitoring & TroubleshootingDocument62 pagesMechanical Ventilation - Monitoring & Troubleshootingabdallah100% (3)
- Basics of Mechanical VentilationDocument208 pagesBasics of Mechanical VentilationAnonymous ORleRr100% (1)
- Overview On Mechanical Ventillation Mechanical Ventilation Overview On Mechanical Ventillation Mechanical VentilationDocument27 pagesOverview On Mechanical Ventillation Mechanical Ventilation Overview On Mechanical Ventillation Mechanical VentilationNabin pokhrelNo ratings yet
- Advance Cardiac Life Support: Short, Sweet and to the PointFrom EverandAdvance Cardiac Life Support: Short, Sweet and to the PointRating: 3 out of 5 stars3/5 (2)
- Nursing care process in patients with chronic obstructive pulmonary diseaseFrom EverandNursing care process in patients with chronic obstructive pulmonary diseaseNo ratings yet
- Lung Anatomy Physiology PDFDocument6 pagesLung Anatomy Physiology PDFCharmie GandaNo ratings yet
- Blue Shield 4-5 MSDSDocument7 pagesBlue Shield 4-5 MSDSsalcabesNo ratings yet
- Week 7Document28 pagesWeek 7Joshua JanerNo ratings yet
- Chakras N Their ColoursDocument11 pagesChakras N Their ColoursSachin KhotNo ratings yet
- Nakshatras- SWATI (SWORD OR INDEPENDENCE)-SELF GOING STAR (38 charactersDocument8 pagesNakshatras- SWATI (SWORD OR INDEPENDENCE)-SELF GOING STAR (38 charactersAstroSunil100% (1)
- I-Science g9 Lesson Plans g9 by D. PhiriDocument49 pagesI-Science g9 Lesson Plans g9 by D. PhiriJoseph NyoniNo ratings yet
- Biodata of The PatientDocument8 pagesBiodata of The PatientRuchika KaushalNo ratings yet
- Pews Charts 0 3 MonthsDocument2 pagesPews Charts 0 3 MonthsThiaNo ratings yet
- International Emergency NursingDocument6 pagesInternational Emergency NursingAtika AlfiaNo ratings yet
- Ventilogic Ls Ver 1 EditedDocument38 pagesVentilogic Ls Ver 1 Editedcbel_23yNo ratings yet
- Chapter 14 Regulation of BreathingDocument18 pagesChapter 14 Regulation of Breathingalzaydi saidilNo ratings yet
- Emulsifier Blend MSDSDocument4 pagesEmulsifier Blend MSDSemeka2012No ratings yet
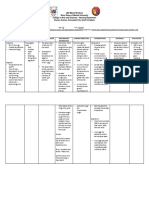
- Assessment Nursing Diagnosis Planning Implemantation Rationale EvaluationDocument2 pagesAssessment Nursing Diagnosis Planning Implemantation Rationale EvaluationChloie Marie Rosalejos100% (1)
- Orr Leonard ItsElementalAir2012Document16 pagesOrr Leonard ItsElementalAir2012shamanjagNo ratings yet
- Sa Aking Mga KababataDocument5 pagesSa Aking Mga KababataCarla Jamina IbeNo ratings yet
- Day 9 Time: 3 Hours Level of Understanding Participant MaterialsDocument51 pagesDay 9 Time: 3 Hours Level of Understanding Participant MaterialsAmit Singh UppNo ratings yet
- Everyday Enlightenment PDFDocument26 pagesEveryday Enlightenment PDFMarcela SanchezNo ratings yet
- 1 Ineffective Breathing PatternDocument8 pages1 Ineffective Breathing PatternNoel MontemayorNo ratings yet
- Spesifikasi Bellavista Icu Complete 2021Document3 pagesSpesifikasi Bellavista Icu Complete 2021Ervan FutrantoNo ratings yet
- VIP Product Manual WsDocument32 pagesVIP Product Manual WsevilplueNo ratings yet
- 3 Rituals OF: Sex MagicDocument14 pages3 Rituals OF: Sex Magicjoel100% (1)
- BOYLESDocument17 pagesBOYLESRaincel mae AbreraNo ratings yet
- Sungazing HandoutDocument4 pagesSungazing HandoutAlina Dospinescu Psiholog SdsNo ratings yet
- LSP - Life Support ProductDocument2 pagesLSP - Life Support ProductMedika Plaza Rig 9No ratings yet
- NCM 101B - NCP - Miguel, Roenth Rhene D - BSN 1DDocument2 pagesNCM 101B - NCP - Miguel, Roenth Rhene D - BSN 1DRiri MiguelNo ratings yet
- Relaxation Technique #1: Deep BreathingDocument6 pagesRelaxation Technique #1: Deep BreathingSangkaran KumarNo ratings yet
- Voice Therapy For The Professional VoiceDocument17 pagesVoice Therapy For The Professional Voiceapi-19500641100% (5)
- SCIENCEDocument12 pagesSCIENCE羅天佑100% (1)
- A Basic Breathing TechniqueDocument6 pagesA Basic Breathing TechniqueFebbe Nadia Okky LucianaNo ratings yet