Professional Documents
Culture Documents
LCR20070416B6
Uploaded by
api-269386240 ratings0% found this document useful (0 votes)
28 views2 pagesadd to final exam lrc's
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentadd to final exam lrc's
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
28 views2 pagesLCR20070416B6
Uploaded by
api-26938624add to final exam lrc's
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
You are on page 1of 2
Case Report B6
(Laboratory interpretation report)
Name of clinician (student): _________________________________ Date: 2007 04 16.
Barbara Miel, a 55-year-old woman, has a seven-month history of fatigue and weakness.
She complain that she is very tired in the morning before eating and also after meals.
About every 2 days she feels lightheaded and has found that eating relieves the
symptoms.
Additional information on request:
Obese.
Laboratory results and differential diagnosis:
Obviously hypoglycaemia is suspected. 5 hour oral glucose tolerance test performed
(100g of glucose)
Fasting 5.7 mmol/L (3.5-5.0)
1 hour 4.8
2 hours 4.9
3 hours 2.2
4 hours 3.8
5 hours.4.3
Symptoms happened at glucose of 2.2 mmol/L
Insulin was performed on this specimen and was 55 IU/L (1-20 fasting)
Elevated insulin with low glucose.
About 25% of normal people with have a glucose of 2.2 mmol/L by 3 hours. 50% of
normal people will have at least one glucose in the 2.8-3.3 nnol/L range.
High insulin level by itself is non-diagnostic as a glucose load provoked it.
Whipple’s triad
1. Low plasma glucose but what is low glucose? Many women have fasting glucose
of 2.6 mmol/L without symptoms.
2. Symptoms at the time of hypoglycaemia.
3. Relief of symptoms by correction of hypoglycaemia
Reactive - low glucose in response to a glucose load
Hypoglycaemia on fasting, extremely rare. True fasting 1 in 250,000.
Best test is 72 hour fast.
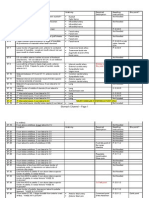
Differential dx Test Result Range Interpretation
Drug induced
Liver disease
Renal disease
Endocrine
Non islet cell
CA
Insulinoma 72 hour fast
Autoimmune
(Working diagnosis underlined).
Comments, qualifications:
Further tests (more invasive or specialized) indicated:
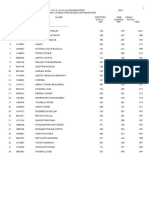
Hours fasting Glucose Insulin mU/L C peptide mg/L Insulin-glucose
mmol/L (0.0-20) (0.50-2.00) ratio (<0.30)
16 5.0 13 3.43 0.14
22 5.3 18 0.19
28 4.8 17 3.42 0.2
34 4.6 21 3.58 0.25
40 4.9 22 3.71 0.26
46 5.2 17 3.44 0.18
52 4.8 20 4.02 0.23
58 4.1 10 3.51 0.14
64 4.2 13 3.38 0.17
72 4.6 9 2.02 0.11
What advice would you give her?
Over weight, she needs to worry about developing NIDDM in the future.
How do you think she will be treated on referral to a specialist?
Nutrition and exercise advice.
Reference(s):
Cryer PE, Glucose homeostasis and hypoglycaemia in Williams Textbook of
Endocrinology 8th edition Philadelphia, Saunders 1992 123-52.
You might also like
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument3 pagesPhysioex Lab Report: Pre-Lab Quiz ResultsAnggina SiregarNo ratings yet
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument3 pagesPhysioex Lab Report: Pre-Lab Quiz ResultsAnggina SiregarNo ratings yet
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument4 pagesPhysioex Lab Report: Pre-Lab Quiz ResultsAnggina SiregarNo ratings yet
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument4 pagesPhysioex Lab Report: Pre-Lab Quiz ResultsAnggina SiregarNo ratings yet
- PhysioEx Exercise 4 Activity 2Document3 pagesPhysioEx Exercise 4 Activity 2Alesandra Campo SanmartínNo ratings yet
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument4 pagesPhysioex Lab Report: Pre-Lab Quiz ResultsAnggina SiregarNo ratings yet
- Agamree Epar Product Information - enDocument32 pagesAgamree Epar Product Information - endrfperezNo ratings yet
- Práctica - Plasma Glucose, Insulin and Diabetes Mellitus.Document4 pagesPráctica - Plasma Glucose, Insulin and Diabetes Mellitus.RIVALDO ALFREDO RIVEROS POLONo ratings yet
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument3 pagesPhysioex Lab Report: Pre-Lab Quiz ResultsAnggina SiregarNo ratings yet
- Effects of Moringa and Exercise On Cardiovascular PDFDocument125 pagesEffects of Moringa and Exercise On Cardiovascular PDFakano oyedayoNo ratings yet
- Oijesity: W I SP Ec e - ExDocument5 pagesOijesity: W I SP Ec e - ExtangledprincessNo ratings yet
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument4 pagesPhysioex Lab Report: Pre-Lab Quiz ResultsIvana FNo ratings yet
- PhysioEx Exercise 4 Activity 2Document3 pagesPhysioEx Exercise 4 Activity 2PatriNo ratings yet
- Case Study 1Document6 pagesCase Study 1api-612516666No ratings yet
- MPhill Resubmission Young 98100106Document442 pagesMPhill Resubmission Young 98100106Vaggelis ChadoliasNo ratings yet
- Total Caloric Intake Daily ValueDocument4 pagesTotal Caloric Intake Daily Valueapi-397104089No ratings yet
- Thurs2 1Document2 pagesThurs2 1api-397140771No ratings yet
- PhysioEx Exercise 4 Activity 2Document3 pagesPhysioEx Exercise 4 Activity 2Milenka SalcedoNo ratings yet
- PhysioEx Exercise 4 Activity 2Document4 pagesPhysioEx Exercise 4 Activity 2PabloAndresPalaciosAgilaNo ratings yet
- Monday January 29th FoodlogDocument2 pagesMonday January 29th Foodlogapi-396957402No ratings yet
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument5 pagesPhysioex Lab Report: Pre-Lab Quiz ResultsAnggina SiregarNo ratings yet
- LK HaepDocument28 pagesLK HaepaptureincNo ratings yet
- Foodlog Date FebDocument1 pageFoodlog Date Febapi-731840566No ratings yet
- Copy of Foodlog Date 01 25 2022 - Daily IntakeDocument2 pagesCopy of Foodlog Date 01 25 2022 - Daily Intakeapi-595111213No ratings yet
- Japoulres14 0254Document5 pagesJapoulres14 0254Ahmed IsmailNo ratings yet
- Laboratory 8 - Micronutrients and WaterDocument6 pagesLaboratory 8 - Micronutrients and WaterBryner CampilisNo ratings yet
- Laboratory 8 - Micronutrients and WaterDocument6 pagesLaboratory 8 - Micronutrients and WaterJoshua MendozaNo ratings yet
- PhysioEx Exercise 4 Activity 2 - Balamad, Maria Karla MDocument4 pagesPhysioEx Exercise 4 Activity 2 - Balamad, Maria Karla MMaria Karla BalamadNo ratings yet
- FerrAurum-22: NanoSystem For Control of Symptomatic Diabetes MellitusDocument42 pagesFerrAurum-22: NanoSystem For Control of Symptomatic Diabetes MellitusdrashtiNo ratings yet
- AMARACHI WORK FinalizedDocument67 pagesAMARACHI WORK FinalizedocNo ratings yet
- 978 1 941926 24 6 - Chapter03Document14 pages978 1 941926 24 6 - Chapter03Federico GaleanoNo ratings yet
- Clinical Chemistry Assignment 2Document3 pagesClinical Chemistry Assignment 2Lana ZyoudNo ratings yet
- Sunday Jan15Document3 pagesSunday Jan15api-397124399No ratings yet
- Pex 04 02Document5 pagesPex 04 02Nada Nabila Wahida PutriNo ratings yet
- Steady-State: Acute and Insulin Responses Glucose Nonobese Diabetic SubjectsDocument8 pagesSteady-State: Acute and Insulin Responses Glucose Nonobese Diabetic SubjectsDea PermataNo ratings yet
- FoodlogDocument4 pagesFoodlogapi-541474235No ratings yet
- Foodlog Date Friday 01 28 22 - Daily IntakeDocument6 pagesFoodlog Date Friday 01 28 22 - Daily Intakeapi-593708395No ratings yet
- Health Intervention. EditedDocument14 pagesHealth Intervention. EditedDENICENo ratings yet
- Foodlog Date Tuesday 02 01 22 - Daily IntakeDocument6 pagesFoodlog Date Tuesday 02 01 22 - Daily Intakeapi-593708395No ratings yet
- High Caloric Intake at Breakfast Vs Dinner Differentially Influences Weight LossDocument9 pagesHigh Caloric Intake at Breakfast Vs Dinner Differentially Influences Weight LossMónica CarrilloNo ratings yet
- Foodlogtemplate Tue Feb 6Document1 pageFoodlogtemplate Tue Feb 6api-397660625No ratings yet
- MODULE 03 Types of DataDocument12 pagesMODULE 03 Types of DataSindhuja VigneshwaranNo ratings yet
- Diabetes Dan PJK, Farmasi DR - DjokoDocument39 pagesDiabetes Dan PJK, Farmasi DR - DjokoimbangNo ratings yet
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument4 pagesPhysioex Lab Report: Pre-Lab Quiz ResultsNovanza RayhanNo ratings yet
- Body SurfaceareaCCLGChart1Document1 pageBody SurfaceareaCCLGChart1Jhoel Zuñiga LunaNo ratings yet
- Foodlog Date Monday February 6thDocument4 pagesFoodlog Date Monday February 6thapi-654020081No ratings yet
- Foodlog Date 02Document1 pageFoodlog Date 02api-731840566No ratings yet
- Nutrient Requirements of Beef Cattle: WWW - Aces.eduDocument8 pagesNutrient Requirements of Beef Cattle: WWW - Aces.eduFajar Sang RevolusionerNo ratings yet
- Foodlog Date Feb 3 - Daily IntakeDocument1 pageFoodlog Date Feb 3 - Daily Intakeapi-657556333No ratings yet
- FoodlogDocument3 pagesFoodlogapi-542842424No ratings yet
- Water Lab ReportDocument8 pagesWater Lab ReportMonica GellerNo ratings yet
- Lab - nr.3. Insulina Si Glucoza PDFDocument4 pagesLab - nr.3. Insulina Si Glucoza PDFAlexandru BurdeniucNo ratings yet
- Hbm2103 Lab 2Document5 pagesHbm2103 Lab 2nganleo5801No ratings yet
- Day 14 - Sunday 2 11Document2 pagesDay 14 - Sunday 2 11api-397125493No ratings yet
- Pex 04 02Document4 pagesPex 04 02Aliifah HanantikaNo ratings yet
- Foodlog Date Sunday 02 11 24 - Daily IntakeDocument1 pageFoodlog Date Sunday 02 11 24 - Daily Intakeapi-732121826No ratings yet
- Lab 2 3Document11 pagesLab 2 3api-347340507No ratings yet
- J. Biol. Chem.-1942-Somogyi-567-74Document9 pagesJ. Biol. Chem.-1942-Somogyi-567-74gibrambo5770No ratings yet
- Exercise and Sport in DiabetesFrom EverandExercise and Sport in DiabetesDinesh NagiNo ratings yet
- 13ffd1fa Eda0 4eb8 Bb3a 7802feec40daDocument40 pages13ffd1fa Eda0 4eb8 Bb3a 7802feec40daapi-26938624No ratings yet
- Endocrine System IVDocument3 pagesEndocrine System IVapi-26938624No ratings yet
- Diabetes Mellitus and HypoglycemiaDocument4 pagesDiabetes Mellitus and Hypoglycemiaapi-26938624No ratings yet
- B0dfbaf2 Beed 4ca7 99fb Ff3588d75dc0Document3 pagesB0dfbaf2 Beed 4ca7 99fb Ff3588d75dc0api-26938624No ratings yet
- c1fd6bbd Ff7a 480d A20e C93bd3a3cedfDocument35 pagesc1fd6bbd Ff7a 480d A20e C93bd3a3cedfapi-26938624No ratings yet
- Endocrine System IIIDocument3 pagesEndocrine System IIIapi-26938624No ratings yet
- Endocrine System IDocument2 pagesEndocrine System Iapi-26938624No ratings yet
- Lecture 50 April 20th-DiabetesDocument2 pagesLecture 50 April 20th-Diabetesapi-26938624No ratings yet
- Nervous System IIDocument2 pagesNervous System IIapi-26938624No ratings yet
- Endorcine System IIDocument4 pagesEndorcine System IIapi-26938624No ratings yet
- Lecture 47 April 13th-EndocrineDocument1 pageLecture 47 April 13th-Endocrineapi-26938624No ratings yet
- Lecture 46 April 11th-EndocrineDocument3 pagesLecture 46 April 11th-Endocrineapi-26938624No ratings yet
- Nervous System IDocument4 pagesNervous System Iapi-26938624No ratings yet
- Lecture 49 April 18th-DiabetesDocument3 pagesLecture 49 April 18th-Diabetesapi-26938624No ratings yet
- Lecture 48 April 17th-Endocrine (Extra Class)Document4 pagesLecture 48 April 17th-Endocrine (Extra Class)api-26938624No ratings yet
- Lecture 41 March 16th-NervousDocument2 pagesLecture 41 March 16th-Nervousapi-26938624No ratings yet
- Lecture 45 April 4th-EndocrineDocument2 pagesLecture 45 April 4th-Endocrineapi-26938624No ratings yet
- Conditions of The Musculoskeleltal SystemDocument4 pagesConditions of The Musculoskeleltal Systemapi-26938624No ratings yet
- Lecture 44 March 30th - NO NOTESDocument1 pageLecture 44 March 30th - NO NOTESapi-26938624No ratings yet
- Lecture 42 March 23rd-NervousDocument2 pagesLecture 42 March 23rd-Nervousapi-26938624No ratings yet
- Lecture 43 March 28th-NervousDocument3 pagesLecture 43 March 28th-Nervousapi-26938624No ratings yet
- OP & OA ChartDocument3 pagesOP & OA Chartapi-26938624100% (1)
- Lecture 36 February 28th-Male Genetalia and ReproductionDocument3 pagesLecture 36 February 28th-Male Genetalia and Reproductionapi-26938624No ratings yet
- Lecture 40 March 14th-MSKDocument5 pagesLecture 40 March 14th-MSKapi-26938624No ratings yet
- Lecture 39 March 9th-MSKDocument3 pagesLecture 39 March 9th-MSKapi-26938624No ratings yet
- Lecture 37 March 2nd-RenalDocument2 pagesLecture 37 March 2nd-Renalapi-26938624No ratings yet
- DDX - Gastrointestinal Disorders ChartDocument21 pagesDDX - Gastrointestinal Disorders Chartapi-26938624100% (2)
- Lecture 35 February 16th-Male Genetalia and ReproductionDocument3 pagesLecture 35 February 16th-Male Genetalia and Reproductionapi-26938624No ratings yet
- Extra DDX NotesDocument1 pageExtra DDX Notesapi-26938624No ratings yet
- Lecture 33 February 7th-Breast and AxillaDocument4 pagesLecture 33 February 7th-Breast and Axillaapi-26938624No ratings yet
- Steering RotaryDocument5 pagesSteering RotaryRahul RavindranNo ratings yet
- Sports Lighting en 12193-2007Document3 pagesSports Lighting en 12193-2007snseshadri100% (1)
- Krav Maga Technique Categories and FamiliesDocument17 pagesKrav Maga Technique Categories and FamiliesRuzek100% (2)
- Ahq-Revamping Squad'S Workshop: Doorway-Exploit Fix For Advanced HeroquestDocument2 pagesAhq-Revamping Squad'S Workshop: Doorway-Exploit Fix For Advanced Heroquestphil roiNo ratings yet
- Qualified GroupC 19-01-2023Document104 pagesQualified GroupC 19-01-2023Raj YadavNo ratings yet
- MksRcdCndts NDA I 19 PDFDocument16 pagesMksRcdCndts NDA I 19 PDFRishi YadavNo ratings yet
- This Model Only Can Support Original 6.5" TFT Screen With Serial NO. 8T0909603A/8T0919603E/8T0919603FDocument1 pageThis Model Only Can Support Original 6.5" TFT Screen With Serial NO. 8T0909603A/8T0919603E/8T0919603FlPiNGUSlNo ratings yet
- Powerpoint PresentationDocument6 pagesPowerpoint PresentationSumithra KrishnanNo ratings yet
- Fly 1Document12 pagesFly 1snka100% (4)
- 60 Day Speed Training PlanDocument101 pages60 Day Speed Training Planxceelent100% (7)
- Vehicle Handover ChecklistDocument2 pagesVehicle Handover Checklistbitben17No ratings yet
- Charlton 27Document20 pagesCharlton 27gladtan0511No ratings yet
- Destroy RKC BiofeedbackDocument10 pagesDestroy RKC Biofeedbacksamyb.am425893No ratings yet
- Comics To CartoonsDocument2 pagesComics To Cartoonsapi-630600853No ratings yet
- Ingles Ejercicios PDFDocument32 pagesIngles Ejercicios PDFcarlos100% (1)
- ACPlus Survival Mode FAQDocument11 pagesACPlus Survival Mode FAQMimeblade100% (1)
- T900 Pre Test Inspection BookletDocument51 pagesT900 Pre Test Inspection Bookletdeming9120100% (1)
- Assignment in Pathfit 4Document3 pagesAssignment in Pathfit 4shinamaevNo ratings yet
- Sayers, A. (2008) - The Nordic Eccentric Hamstring Exercise For InjuryDocument3 pagesSayers, A. (2008) - The Nordic Eccentric Hamstring Exercise For InjuryMarko BrzakNo ratings yet
- Bondarchuk Experiments With StrengthDocument6 pagesBondarchuk Experiments With StrengthBrandy Malone100% (4)
- S-Works Camber 29 S-Works Camber 29 Frame: Specs Key Features Specs Key FeaturesDocument4 pagesS-Works Camber 29 S-Works Camber 29 Frame: Specs Key Features Specs Key FeaturesSickLinesNo ratings yet
- Malzeme Cetveli̇Document1 pageMalzeme Cetveli̇sitehabNo ratings yet
- #53 February 2015Document76 pages#53 February 2015OutdoorUAENo ratings yet
- Taneks Brake CatalogueDocument31 pagesTaneks Brake CatalogueeCommerce SAJID AutoNo ratings yet
- Bunnies and Burrows Print Able Maps and TokensDocument29 pagesBunnies and Burrows Print Able Maps and TokensDaveDM100% (1)
- China Team Selection Test 1998 47Document2 pagesChina Team Selection Test 1998 47Biswarup BurmanNo ratings yet
- Warrior Within Card Game RulebookDocument12 pagesWarrior Within Card Game RulebookVincent LeoneNo ratings yet
- Confidential. Not To Be CirculatedDocument10 pagesConfidential. Not To Be CirculatedbeniNo ratings yet
- Automa - Shadow Empire RulesDocument1 pageAutoma - Shadow Empire RulesBurke HartNo ratings yet
- Combate HYperboreaDocument10 pagesCombate HYperborealenusricard21No ratings yet