Professional Documents
Culture Documents
NCM 118 Case Analysis #2: 50-year-old Female with Abdominal Pain
Uploaded by
Reyna Mee AhiyasOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCM 118 Case Analysis #2: 50-year-old Female with Abdominal Pain
Uploaded by
Reyna Mee AhiyasCopyright:
Available Formats
NCM 118 Case Analysis #2
Susan Cortez is a 50 – year old female housewife who was brought to the hospital 3 days ago due to
“ahitao pirmi mio bariga”, “ta duele mio bariga y pecho akabar kome” “duele tambien mio costao”. She
also claimed of nausea and vomiting, bitter taste in the mouth, noticeable weight loss, very dark stools,
difficult urination and loss of appetite. She has a medical history of UTI 6 months ago and was treated
with antibiotics for 2 weeks without hospitalization. She admitted she is used to taking over-the-
counter drugs like ibuprofen and aspirin for pain and joint swelling. During admission her vital signs
revealed: Temp – 38.3 degrees Celsius, Pulse rate – 102 bpm, Respiratory rate – 22 br/min and BP –
140/100 mmHg. She was responsive and oriented and could answer questions correctly. She was able
to raise and lower her arms when instructed. She was accompanied by her husband and their son. The
doctor examined her and advised blood tests for renal function test, CBC, electrolytes and blood sugar.
Her random blood sugar result showed 142 mg/dL. A urinalysis was done with result showing “Color-
amber, turbid, pH-4.8, with 5 RBC’s hpf, moderate leukocyte esterase with wbc-11 mm3”. An ECG was
taken which showed minimally shortened RR intervals denoting tachycardia but otherwise normal
sinus rhythm. Her ABG result revealed: pH=7.32, aPCO2=39 mmHg, aPO2=92 mmHg, HCO3=20 mEq/L
and O2Sat=95%. The admitting diagnosis was “Duodenal Ulcer, UTI, Stage 1 Hypertension”. She was
placed in a private room and was kept under observation with her husband as the watcher.
Her orders on the day of admission were:
- Admit in a private room with one watcher 24/7
- NPO
- Strict I and O monitoring
- Repeat urinalysis and FBS in the morning
- Do LFT’s and electrolytes
- Oxygen @ 2 L/min via nasal cannula PRN for dyspnea
- IVF NaCl alternate with D5%LR for a total of 2,500 mL/ day
- Ciprofloxacin (Ciprobay) 200 mg IV q 12 hours (ANST) for 3days
- Esomeprazole Sodium (Nexium) 20 mg to incorporate in 50 mL 0.9% NaCl to run for 30 mins
- Cimetidine (Tagamet) 300 mg in 500 mL NSS to run at 25 mg/h continuous IV infusion
- Urine for C and S
- Refer as necessary
Nursing Assessment upon Admission in the Medical Unit Revealed:
- Conscious, responsive and coherent
- CBC: Hb – 12 mg/dL, Hct – 41%, WBC – 11,000/mm3 and platelets – 360,000/uL
- FBS – 130 mg/dL
- K – 3.9 mEq/L, Na – 142 mEq/L, Ca – 10 mg/dL
- BUN – 23 mg/dL, Serum Creatinine = 2.12 mg/dL
- LFT – ALT= 52 U/L, AST= 43 U/L, ALP= 121 U/L, Albumin= 5.9 g/dL, Total Protein= 8.4 g/dL,
Bilirubin= 1.1 mg/dL, GGT=57 U/L
- VS: T-38.4, PR-103 b/min, RR-22 br/min, BP-140/100 mmHg
- Urine output = 180 (6 hours since admission), no bladder distension, abdomen is soft and bowel
sounds appear 2 – 3x per minute in all 4 quadrants
- Vomited twice (each about 50-80 mL) greenish-yellowish fluids believed to be gastric in origin
- Can recognize her husband and the reason why she was brought to the hospital but kept asking
what was her illness and if she will be operated
- Patient gave the following information:
High school graduate, housewife since before
Married for 24 years, she has 1 son who was delivered NSVD, now married also
Eats three times a day, favorite food is fried fish with “suka”, she also loves chips and
native foods like biko, drinks about 3 – 4 glasses of water per day with 3 – 4 cups of
native coffee almost every day. She loves “balut”. She complains of constipation at
times with some “dark stools” recently. She was also treated of UTI before but no other
history of medical illness or surgery was mentioned.
She enjoys watching “teleserye” and Netflix at home. She also keeps a small garden.
Usually sleeps an average of 5 hours per night and sleeps late from watching movies,
sometimes spends extra time until morning to finish some movie marathon, enjoys the
computer and cellular phones often for online communication with her son and
grandchildren, she had been on prescription glasses for being “myopic” since she was 22
years old. Recent visual acuity revealed OD-20/100, OS-20/60, OU-20/70.
Follows Seventh Day Adventist and goes to church every Saturdays. “I am waiting for the
second coming of Jesus eagerly. I pray for my son, my grandchildren and my husband
every day. I also read the Bible with some friends once in a week”.
Had “regular, monthly menstruation” before; menopause at 47; with no reports of any
unusual vaginal bleeding at present; confided that she is not very much sexually active
as she used to be.
Few days before she was admitted she claimed she noticed “Resyo ta duele mio bariga y
bien negro mio susyo desde cuanto dia ya, ya nerbya man yo. Nuay tambien yo gana
kome y tan luya ya man gayot iyo. Tan digwa tamen yo. Mio miyaw otro otro el olor y ta
duele mio detras, tormento yo miya”.
Husband claimed: “She is a loving and caring wife. She also cooks very well”.
She delivered her son normally in the hospital. Her husband is a retired military colonel.
Husband said that days before admission, the wife was complaining of ‘difficult
urination’ and was very irritable at home but refused to see a doctor. “Poreso ya manda
yo anda kunel di mio anak na casa para ele amo liba con el desu nana na ospital.”
She was brought to the hospital through the private car of their son.
Physical examination revealed:
- Weight = 51 kilograms, height = 5’4”
- Mixed gray and black hair completely distributed in head, with minimal dandruff, no lesions, no
scars, no wounds noted. No offensive smell noted.
- Wears eyeglasses +2.0, pupils revealed PERRLA, corneal blinking reflexes present in both eyes,
sclerae appeared pinkish, minimal peri-orbital edema noted on both sides, complained of
“blurring” but managed to correctly identify letters in the magazine when shown to her.
- Upon whispering, patient was able to repeat all 5 words correctly as what the nurse said. Ears
had intact ear canal with minimal cerumen noted, no discharges noted. No unusual odor noted.
- The nasal passageways were patent, septum was in place, upon illumination, the sinuses
revealed faint red color, able to identify the scent of kalamansi when introduced.
- Mouth was clean, with complete upper and lower dentures (since 5 years). No odor noted from
the mouth, uvula was intact, tonsils not inflamed. On NPO due to nausea; speech was clear. Lips
appeared chappy, tongue had minimal cracks.
- Neck was aligned, no complaints of discomfort claimed, thyroid was hardly palpable, no bruit or
abnormal sounds identified, large vessels were intact and not swollen, carotid pulse rate was
104 b/min.
- The posterior thorax showed no evidence of scars or wounds, percussion sounds showed no
abnormal results, no lesions nor masses palpated, breath sounds were clear. RR – 23 br/min.
- Anterior thorax showed no evidence of lesions, both breasts showed no signs of mass or
discharges during palpation, breath sounds were clear, RR -22 br/min.
- Abdomen was minimally hard on palpation, no scars and lesions noted, bowel sounds were
heard once every minute in all 4 quadrants, percussion sounds were dull at the epigastric
region and at hypochondriac regions; no masses palpated but showed facial grimace during
palpation on epigastric region, claimed of tenderness. Refused further palpation of abdomen.
- Refused to be assessed in her genital area but claimed that she is having difficulty urinating but
feels no itchiness or discomfort in her genitals. She confided she had a history of Gonorrhea
around 10 years back and blamed her husband for the infection. She said she was treated by a
private physician with penicillin injection that time. She said nobody knew about it except her
husband and the doctor.
- Extremities showed muscle strength 2+ scores in both upper and 2+ scores in both lower areas
for resistance.
- Can raise arms & legs but very slowly and can identify dull and sharp stimulations in all 4 limbs.
- Cranial nerves revealed: “difficult swallowing” (needs further data).
At present (day 3 since admission) (Morning):
- Vital signs T-37.6, PR-99 b/min, RR-19 br/min, BP-140/90 mmHg
- Urine C and S result showed “E.Coli” and sensitive to ciprofloxacin
- Latest CBC: Hb – 12 mg/dL, Hct – 42%, WBC – 9,800/mm3 and platelets – 340,000/uL
- FBS – 152 mg/dL
- K – 3.9 mEq/L, Na – 145 mEq/L, Ca – 10.2 mg/dL
- BUN – 20 mg/dL, Serum Creatinine = 1.62 mg/dL
- LFT – ALT= 51 U/L, AST= 45 U/L, ALP= 119 U/L, Albumin= 5.6 g/dL, Total Protein= 8.1 g/dL,
Bilirubin= 1.2 mg/dL, GGT=56 U/L
- Latest ABG result revealed: pH=7.35, aPCO2=44 mmHg, aPO2=94 mmHg, HCO3=22 mEq/L and
O2Sat=96%
- Latest urinalysis: Color-amber, minimally turbid, pH-5.7, with 4 RBC’s hpf, leukocyte esterase
with wbc-9.5 mm3”.
- On low protein soft diet; able to take 45% of breakfast, with 1 episode of nausea early morning
- Able to move within the room with some assistance from watcher
- Still complained of some flank pain and abdominal cramps, but “hinde mas gayot bien duele
egual del primero”
- Oxygen saturation at 96% on room air; no oxygen supplement since 2 days
- 24 hours input – 2,800 mL and urine output – 1, 600 mL (measured in urinal)
- Doctor came and discussed with the patient and husband about the case, agreed to prepare the
patient for possible shifting to oral meds if symptoms improve in the next 24 hours, for
endocrinology consultation of blood sugar.
- Patient asks the nurse: “No kyere pa yo muri. Kyere pa yo mira ta gradua mio mga apo.”
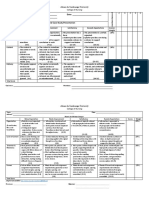
Students’ Tasks per GROUP
1. Analyze the given case. Work on a case study using the given data.
2. Using the nursing process, transfer the given data into power point presentation and fill in the
assessment (Gordon’s, Physical and Laboratory) emphasizing the significant cues.
3. Create the patient’s profile using the available information.
4. Present the case in a sequential manner. Begin with a short introduction of the case, the
significance of the case study, definition of important terms, review of the anatomy and physiology
of structures involved, review of literature, pathophysiology (general and specific), disease
management (not only based on the case scenario; you may also add information using other
reliable sources in terms of disease management).
5. Include a drug study and relate the drugs to the case.
6. Create a Nursing Care Plan (NCP) with 3 problems; to be presented according to sequence based on
priority. Use any nursing theory or model as basis. Use NANDA as guide in formulating the care
plan. The assessment data to be used should be based on the case scenario. Nursing diagnosis until
evaluation should come from you.
7. Make a Learning Plan for the client/family. One topic will be enough.
8. Give your conclusion and possible recommendations.
9. Include a short acknowledgement, appendices and references at the last part.
10. Present and defend your case as scheduled.
11. Submit a hard copy to your instructors when you submit your outputs for FINAL TERM.
12. Note that an online orientation will be done prior to starting this activity. Attendance is required.
You might also like
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Ethico - Moral Aspect of NursingDocument37 pagesEthico - Moral Aspect of NursingMarichu Bajado100% (1)
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Assessment of Immune FunctionDocument3 pagesAssessment of Immune Functionhalloween candyNo ratings yet
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- Acute Biologic Crisis: Nina Hamili G. Piao RNDocument62 pagesAcute Biologic Crisis: Nina Hamili G. Piao RNNina OaipNo ratings yet
- Postoperative Nursing CareDocument2 pagesPostoperative Nursing CareYeana AlonNo ratings yet
- Acute Biologic CrisisDocument106 pagesAcute Biologic CrisisLisette Grace Umadhay CabalangNo ratings yet
- Perioperative Nursing: Rose Delia P. Ocariza, RN, MANDocument66 pagesPerioperative Nursing: Rose Delia P. Ocariza, RN, MANDeva HiyasNo ratings yet
- Operating Room RenstahDocument2 pagesOperating Room RenstahRubi BorromeoNo ratings yet
- CASE SCENARIO 3 PreopDocument3 pagesCASE SCENARIO 3 PreopEdgarNo ratings yet
- Disaster NursingDocument4 pagesDisaster NursingMary Angel Nicka LuayonNo ratings yet
- Practice Test Questions Downloaded From FILIPINO NURSES CENTRALDocument20 pagesPractice Test Questions Downloaded From FILIPINO NURSES CENTRALFilipino Nurses CentralNo ratings yet
- Perception & Coordination NCM 104Document162 pagesPerception & Coordination NCM 104bianqueeNo ratings yet
- Concept Communicable DiseasesDocument477 pagesConcept Communicable DiseasesrimeoznekNo ratings yet
- START Triage Training PresentationDocument85 pagesSTART Triage Training PresentationPandu Putra Wijaya RestaNo ratings yet
- OrchiectomyDocument35 pagesOrchiectomyYosa Angga OktamaNo ratings yet
- Pediatric Oncology Case StudyDocument12 pagesPediatric Oncology Case StudyromelynNo ratings yet
- Perioperative Nursing ModuleDocument2 pagesPerioperative Nursing ModulerosanowardNo ratings yet
- Cardiology Medsurg LectureDocument9 pagesCardiology Medsurg LectureTine GuibaoNo ratings yet
- 118 Skills Lab-Week 1-Responses To Altered Ventilatory FunctionsDocument8 pages118 Skills Lab-Week 1-Responses To Altered Ventilatory FunctionsKeisha BartolataNo ratings yet
- Medical-Surgical Nursing: An Integrated Approach, 2E: Nursing Care of The Client: Responding To EmergenciesDocument25 pagesMedical-Surgical Nursing: An Integrated Approach, 2E: Nursing Care of The Client: Responding To EmergenciesRS Buenavista100% (1)
- Disaster Nursing P1 Learning PlanDocument5 pagesDisaster Nursing P1 Learning PlanPamela GastalaNo ratings yet
- Mental Health Nursing II NURS 2310: Unit 1 Basic Concepts of Mental Health and Mental IllnessDocument41 pagesMental Health Nursing II NURS 2310: Unit 1 Basic Concepts of Mental Health and Mental IllnessRocky Domingo LazaroNo ratings yet
- St. Mary's College Nursing Program Teaches Critical Care ConceptsDocument33 pagesSt. Mary's College Nursing Program Teaches Critical Care ConceptsAlyssa Gaile EspirituNo ratings yet
- Fundamentals of Nursin Final Examination-Answer Keys (March 18,2013Document13 pagesFundamentals of Nursin Final Examination-Answer Keys (March 18,2013marsan12No ratings yet
- 6 Alterations On Tissue Perfusion Poleno Serrano TajalaDocument18 pages6 Alterations On Tissue Perfusion Poleno Serrano TajalaSophia A. GoNo ratings yet
- Disaster Nursing: Norman G. CalderonDocument79 pagesDisaster Nursing: Norman G. Calderonelaine_reodica100% (1)
- NCM 118 Midterms ReviewerDocument7 pagesNCM 118 Midterms ReviewerKai SamaNo ratings yet
- OB2 - Renal and Urinary Tract Disorders in Pregnancy - Dr. TanDocument6 pagesOB2 - Renal and Urinary Tract Disorders in Pregnancy - Dr. TanHazel Fernandez VillarNo ratings yet
- NCM 112-Mod2Document9 pagesNCM 112-Mod2Samantha BolanteNo ratings yet
- NUR100 Sherpath CH 44 PainDocument23 pagesNUR100 Sherpath CH 44 Paincaloy2345caloyNo ratings yet
- Prof. AdjustmentDocument111 pagesProf. AdjustmentDianne Kate CadioganNo ratings yet
- C C C M MMMM MM M MMM 3mm MMMMM MM M MMMMMDocument4 pagesC C C M MMMM MM M MMM 3mm MMMMM MM M MMMMMjohkieNo ratings yet
- M1 - Urinary DisordersDocument2 pagesM1 - Urinary DisordersjuiceNo ratings yet
- Transcultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodDocument5 pagesTranscultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodeuLa-mayzellNo ratings yet
- Cellular AberrationDocument71 pagesCellular AberrationMichael CoronadoNo ratings yet
- Biologic Crisis: Prepared By: Ronnie M. Amazona, RN, ManDocument162 pagesBiologic Crisis: Prepared By: Ronnie M. Amazona, RN, ManLex CatNo ratings yet
- NCM 118Document8 pagesNCM 118Zanie CruzNo ratings yet
- Pleural Fluid Analysis: How The Test Is PerformedDocument4 pagesPleural Fluid Analysis: How The Test Is PerformedKevin LlorenteNo ratings yet
- PANCREATITISDocument38 pagesPANCREATITISVEDHIKAVIJAYANNo ratings yet
- NCMB 314 - M2-Cu10Document10 pagesNCMB 314 - M2-Cu10Giselle EstoquiaNo ratings yet
- Acute Renal FailureDocument5 pagesAcute Renal FailureJean De Vera MelendezNo ratings yet
- Depressive Disorder - OdpDocument24 pagesDepressive Disorder - OdpShielamae PalalayNo ratings yet
- Schizophrenia and Mental Health Nursing InterventionsDocument10 pagesSchizophrenia and Mental Health Nursing InterventionsRosie CuasitoNo ratings yet
- Eteeap - NCM 106 Page 1Document5 pagesEteeap - NCM 106 Page 1Marisol Jane JomayaNo ratings yet
- Chapter 8 - Emergency CareDocument16 pagesChapter 8 - Emergency CareAlyssa MadriagaNo ratings yet
- Acute Biologic CrisisDocument143 pagesAcute Biologic CrisisAprylL22100% (5)
- Disaster Nursing - Icn Position and Recommendation - Rotone, Lycah v. - BSN 4yb-4Document3 pagesDisaster Nursing - Icn Position and Recommendation - Rotone, Lycah v. - BSN 4yb-4Lycah RotoneNo ratings yet
- Perioperative Nursing Med-SurgDocument3 pagesPerioperative Nursing Med-SurgKarla Fralala100% (1)
- Osteoporosis Prevention and Fracture Risk ReductionDocument21 pagesOsteoporosis Prevention and Fracture Risk ReductionrihamNo ratings yet
- Diana's Renal DiseasesDocument9 pagesDiana's Renal DiseasesdhyltonNo ratings yet
- Acute Poisoning in Adults: Dr. S.P. Hewawasam MBBS, MDDocument76 pagesAcute Poisoning in Adults: Dr. S.P. Hewawasam MBBS, MDSamapriya Pasan Hewawasam100% (1)
- Clinical Nursing Care ScenarioDocument1 pageClinical Nursing Care ScenarioLeary John Herza TambagahanNo ratings yet
- Activity 3Document1 pageActivity 3Windi Dawn SallevaNo ratings yet
- Module Ncm112 ACID BASE 1Document25 pagesModule Ncm112 ACID BASE 1CHARMAGNE ABAÑO. CAMINS100% (1)
- At LTC N Theories Models 1Document35 pagesAt LTC N Theories Models 1Darin BransonNo ratings yet
- COURSE UNIT - CU5 Nurses Role in Disaster Part 2 - Copy-2Document4 pagesCOURSE UNIT - CU5 Nurses Role in Disaster Part 2 - Copy-2Danica FrancoNo ratings yet
- NCM of Clients With Endocrine DisordersDocument24 pagesNCM of Clients With Endocrine DisordersArgee Alonsabe100% (1)
- Level 3 1ST Sem OrientationDocument73 pagesLevel 3 1ST Sem OrientationLeslie CruzNo ratings yet
- Cardiac Cath Procedure ExplainedDocument25 pagesCardiac Cath Procedure ExplainedReyna Mee AhiyasNo ratings yet
- This Study Resource WasDocument6 pagesThis Study Resource WasReyna Mee AhiyasNo ratings yet
- Ateneo de Zamboanga Nursing RubricDocument3 pagesAteneo de Zamboanga Nursing RubricReyna Mee AhiyasNo ratings yet
- DU UTI Stage 1 Hypertension Case - Analysis FinalDocument87 pagesDU UTI Stage 1 Hypertension Case - Analysis FinalReyna Mee AhiyasNo ratings yet
- Vital signs and lab results reveal medical conditionDocument14 pagesVital signs and lab results reveal medical conditionReyna Mee AhiyasNo ratings yet
- NCM 118 Case Analysis #2: 50-year-old Female with Abdominal PainDocument4 pagesNCM 118 Case Analysis #2: 50-year-old Female with Abdominal PainReyna Mee AhiyasNo ratings yet
- Chapter 5 The Nineteenth Century Philippine Economy Society and The Chinese MestizosDocument27 pagesChapter 5 The Nineteenth Century Philippine Economy Society and The Chinese MestizosJuMakMat Mac50% (2)
- ASTHMADocument2 pagesASTHMAReyna Mee AhiyasNo ratings yet
- Ateneo de Zamboanga University College of Nursing Oral Case Study RubricDocument2 pagesAteneo de Zamboanga University College of Nursing Oral Case Study RubricReyna Mee AhiyasNo ratings yet
- The Family With A Toddler ToddlerDocument5 pagesThe Family With A Toddler ToddlerReyna Mee AhiyasNo ratings yet
- Case Study GuidelinesDocument1 pageCase Study GuidelinesReyna Mee AhiyasNo ratings yet
- Ahiyas - Reproductive SystemDocument1 pageAhiyas - Reproductive SystemReyna Mee AhiyasNo ratings yet
- Editor'S Copy: Voice-Over: in Administering ORAL MEDICATIONS, FirstDocument5 pagesEditor'S Copy: Voice-Over: in Administering ORAL MEDICATIONS, FirstReyna Mee AhiyasNo ratings yet
- Learning Module 1 - Reproductive Health FormsDocument3 pagesLearning Module 1 - Reproductive Health FormsReyna Mee AhiyasNo ratings yet
- Nutritional AssessmentDocument6 pagesNutritional AssessmentReyna Mee AhiyasNo ratings yet
- Performing Urethral Urinary CatheterizationDocument4 pagesPerforming Urethral Urinary CatheterizationReyna Mee AhiyasNo ratings yet
- Maternal and Child CareDocument1 pageMaternal and Child CareReyna Mee AhiyasNo ratings yet
- In Our Status QouDocument5 pagesIn Our Status QouReyna Mee AhiyasNo ratings yet
- Ahiyas - Reproductive SystemDocument1 pageAhiyas - Reproductive SystemReyna Mee AhiyasNo ratings yet
- Significance of The StudyDocument2 pagesSignificance of The StudyReyna Mee AhiyasNo ratings yet
- Assessing Fetal and Maternal HealthDocument6 pagesAssessing Fetal and Maternal HealthReyna Mee AhiyasNo ratings yet
- Weekly Course Learning Objectives (Postpartum)Document4 pagesWeekly Course Learning Objectives (Postpartum)Reyna Mee AhiyasNo ratings yet
- Physiologic Changes of PregnancyDocument7 pagesPhysiologic Changes of PregnancyReyna Mee AhiyasNo ratings yet
- Chronic Diseases (Seminar)Document4 pagesChronic Diseases (Seminar)Reyna Mee AhiyasNo ratings yet
- GreetingsDocument1 pageGreetingsReyna Mee AhiyasNo ratings yet
- Case Study (HOSPITAL)Document4 pagesCase Study (HOSPITAL)Reyna Mee AhiyasNo ratings yet
- Child Growth and DevelopmentDocument2 pagesChild Growth and DevelopmentReyna Mee AhiyasNo ratings yet
- Color Coding of Medication CardDocument1 pageColor Coding of Medication CardReyna Mee AhiyasNo ratings yet
- Activity 1Document1 pageActivity 1Reyna Mee AhiyasNo ratings yet
- Appliedmicro Micro d&Amp;r AgamDocument83 pagesAppliedmicro Micro d&Amp;r Agamjanijkson29No ratings yet
- BF & C Info (Bone, Flesh, & Cartilage) Recipe & AnecdotesDocument12 pagesBF & C Info (Bone, Flesh, & Cartilage) Recipe & Anecdotesmickelle100% (1)
- Thomas M Hooton, MD Kalpana Gupta, MD, MPH Stephen B Calderwood, MD Allyson Bloom, MDDocument14 pagesThomas M Hooton, MD Kalpana Gupta, MD, MPH Stephen B Calderwood, MD Allyson Bloom, MDMusicBestLiveNo ratings yet
- Interstitial Cystitis (Bladder Inflammation) - ColumbiaDoctors - New YorkDocument6 pagesInterstitial Cystitis (Bladder Inflammation) - ColumbiaDoctors - New YorkJimmy GillNo ratings yet
- UTI in A Pregnant Woman - NCPDocument6 pagesUTI in A Pregnant Woman - NCPella joyce75% (4)
- Problem Solving With AnswersDocument50 pagesProblem Solving With Answersapi-3814958No ratings yet
- Big Drugs!!Document2,145 pagesBig Drugs!!Solomon Seth SallforsNo ratings yet
- Model MBBS Syllabus (DR Apurba Sastry, DR Sandhya Bhat) PDFDocument22 pagesModel MBBS Syllabus (DR Apurba Sastry, DR Sandhya Bhat) PDFmajoragarwal1195No ratings yet
- Bladder IrrigationDocument14 pagesBladder Irrigationpatlekhilesh8No ratings yet
- 2 Pre Gestation and Gestational ConditionsDocument88 pages2 Pre Gestation and Gestational Conditionslermacornel61No ratings yet
- CPM17th Urinary Tract InfectionDocument9 pagesCPM17th Urinary Tract InfectionBenj GilbuenaNo ratings yet
- Sterile PyuriaDocument7 pagesSterile PyuriaLuiggi D. Chambi MaidaNo ratings yet
- Renal System Functions and DisordersDocument4 pagesRenal System Functions and DisordersLordgelyn Diane ViernesNo ratings yet
- Renal and Urological Disorders: A Concise GuideDocument30 pagesRenal and Urological Disorders: A Concise GuideIrma HermaliaNo ratings yet
- Air in The Urinary Tract: Images in Clinical MedicineDocument1 pageAir in The Urinary Tract: Images in Clinical MedicineSamira LizarmeNo ratings yet
- Dr. Blyden: Urinary Tract Infection (Uti)Document24 pagesDr. Blyden: Urinary Tract Infection (Uti)Blyden NoahNo ratings yet
- Identifying Healthcare-Associated Infections (HAI) For NHSN SurveillanceDocument27 pagesIdentifying Healthcare-Associated Infections (HAI) For NHSN SurveillanceInter 4DMNo ratings yet
- Cases Journal: Acquired Nonobstructive Urinary Bladder Diverticulum: A CaseDocument3 pagesCases Journal: Acquired Nonobstructive Urinary Bladder Diverticulum: A CaseIrma Suriani DarwisNo ratings yet
- CHN Ailyn and Lai& RealDocument6 pagesCHN Ailyn and Lai& RealNylia AtibiNo ratings yet
- Kidney TransplantDocument73 pagesKidney TransplantwatztanjaNo ratings yet
- Conrad Fischer MCQsDocument328 pagesConrad Fischer MCQsPopescu Tina100% (1)
- Vitamin E May Relieve Symptoms of Urinary Tract InfectionDocument9 pagesVitamin E May Relieve Symptoms of Urinary Tract InfectionTri UlfaNo ratings yet
- Problem - Solving - Collected 2Document64 pagesProblem - Solving - Collected 2mulyadiNo ratings yet
- CL7 Urinary Tract Infection 20192020-20191212060056Document50 pagesCL7 Urinary Tract Infection 20192020-20191212060056Nur Ain IzzatiNo ratings yet
- Care Plan Risk For Infection 2Document3 pagesCare Plan Risk For Infection 2Chander KantaNo ratings yet
- Cephalosporin Antibiotics: From 7-Aminocephalosporanic Acid - Produced by FermentationDocument23 pagesCephalosporin Antibiotics: From 7-Aminocephalosporanic Acid - Produced by FermentationVeChrist PharmacistoLshopNo ratings yet
- Urology Special Notes on Upper and Lower Urinary Tract SymptomsDocument36 pagesUrology Special Notes on Upper and Lower Urinary Tract SymptomsYiba Zul100% (4)
- Transforming insurance underwriting with AI-powered predictive modelsDocument26 pagesTransforming insurance underwriting with AI-powered predictive modelsLukas FagoloNo ratings yet
- Cassandra Kinser PDFDocument4 pagesCassandra Kinser PDFKim Corpuz100% (1)
- Ob Final Exam GuideDocument30 pagesOb Final Exam GuideSarah Elizabeth WalkerNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (403)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (20)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- Daniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisFrom EverandDaniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisRating: 3.5 out of 5 stars3.5/5 (130)
- Algorithms to Live By: The Computer Science of Human DecisionsFrom EverandAlgorithms to Live By: The Computer Science of Human DecisionsRating: 4.5 out of 5 stars4.5/5 (722)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)