Professional Documents
Culture Documents
A Novel Reporting System To Improve Accuracy in Appendicitis Imaging
Uploaded by
Giga HasabiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Novel Reporting System To Improve Accuracy in Appendicitis Imaging
Uploaded by
Giga HasabiCopyright:
Available Formats
Gastrointestinal Imaging • Original Research
Godwin et al.
A Novel Appendicitis Reporting System
Gastrointestinal Imaging
Original Research
Downloaded from www.ajronline.org by 94.237.69.42 on 06/18/20 from IP address 94.237.69.42. Copyright ARRS. For personal use only; all rights reserved
A Novel Reporting System
to Improve Accuracy in
Appendicitis Imaging
Benjamin D. Godwin1 OBJECTIVE. The purpose of this study was to ascertain if standardized radiologic re-
Frederick T. Drake 2 porting for appendicitis imaging increases diagnostic accuracy.
Vlad V. Simianu2 MATERIALS AND METHODS. We developed a standardized appendicitis reporting
Jabi E. Shriki1,3 system that includes objective imaging findings common in appendicitis and a certainty score
Daniel S. Hippe1 ranging from 1 (definitely not appendicitis) through 5 (definitely appendicitis). Four radiolo-
gists retrospectively reviewed the preoperative CT scans of 96 appendectomy patients using
Manjiri Dighe1
our reporting system. The presence of appendicitis-specific imaging findings and certainty
Sarah Bastawrous1,3 scores were compared with final pathology. These comparisons were summarized using odds
Carlos Cuevas1 ratios (ORs) and the AUC.
David Flum 2 RESULTS. The appendix was visualized on CT in 89 patients, of whom 71 (80%) had patho-
Puneet Bhargava1 logically proven appendicitis. Imaging findings associated with appendicitis included appendi-
ceal diameter (odds ratio [OR] = 14 [> 10 vs < 6 mm]; p = 0.002), periappendiceal fat stranding
Godwin BD, Drake FT, Simianu VV, et al.
(OR = 8.9; p < 0.001), and appendiceal mucosal hyperenhancement (OR = 8.7; p < 0.001). Of 35
patients whose initial clinical findings were reported as indeterminate, 28 (80%) had appendici-
tis. In this initially indeterminate group, using the standardized reporting system, radiologists as-
signed higher certainty scores (4 or 5) in 21 of the 28 patients with appendicitis (75%) and lower
scores (1 or 2) in five of the seven patients without appendicitis (71%) (AUC = 0.90; p = 0.001).
Keywords: appendectomy, appendicitis, CT, CONCLUSION. Standardized reporting and grading of objective imaging findings cor-
s tandardized reporting related well with postoperative pathology and may decrease the number of CT findings re-
DOI:10.2214/AJR.14.13512
ported as indeterminate for appendicitis. Prospective evaluation of this reporting system on a
cohort of patients with clinically suspected appendicitis is currently under way.
Received July 17, 2014; accepted after revision
October 2, 2014.
A
cute appendicitis is the most slightly in retrospective studies [22, 23]. How-
P. Bhargava is Editor in Chief of Current Problems in common cause of right lower ever, the persistently high rate of negative lap-
Diagnostic Radiology, published by Elsevier Inc. quadrant pain presenting to the arotomies suggests the need for additional im-
emergency department [1] and provement in our diagnostic ability.
V. V. Simianu and F. T. Drake are supported by a National remains the most frequent indication for ur- Imaging findings associated with appen-
Institute of Diabetes and Digestive and Kidney Diseases
training grant (5T32DK070555). The Surgical Care and
gent abdominal surgery [2]. Before the ad- dicitis have been widely documented in the
Outcomes Assessment Program (SCOAP) is a vent of advanced imaging, the diagnosis of literature [1, 7, 11, 12, 18, 19, 24–26]. In
Coordinated Quality Improvement Program of the appendicitis was based on clinical symptoms most cases, CT simultaneously shows mul-
Foundation for Health Care Quality (FHCQ). and laboratory markers. Early surgical inter- tiple findings, enabling confident diagnosis
1 vention was preferred, and negative appen- of appendicitis [10, 17]. However, in some
Department of Radiology, University of Washington,
1959 NE Pacific St, UW Mailbox 357115, Seattle, WA dectomy rates between 10–40% were rou- cases, CT findings are equivocal or incon-
98195. Address correspondence to P. Bhargava tinely accepted to avoid delayed diagnosis clusive, but there is high clinical suspicion
(bhargp@uw.edu). and the risk of perforated appendicitis [3–5]. for appendicitis. This subset of patients with
2
Over the past 20 years, CT has revolution- indeterminate or equivocal imaging findings
Department of Surgery, University of Washington,
Seattle, WA.
ized the workup of appendicitis, with reported has been estimated to represent 9–13% of CT
sensitivities and specificities of 88–100% [3– studies for workup of appendicitis, with up to
3
VA Puget Sound Health Care System, Seattle, WA. 21]. Correspondingly, the number of negative 30% of these patients being subsequently di-
laparotomies for appendicitis has decreased, agnosed with appendicitis [17].
AJR 2015; 204:1212–1219
and rates of less than 10% are considered the Because the diagnosis of appendicitis on
0361–803X/15/2046–1212 current standard of care [5]. Over the same CT is not always certain, a clear way of ex-
period, the number of cases of perforated ap- pressing the likelihood of appendicitis is
© American Roentgen Ray Society pendicitis has remained constant or decreased needed. This can be achieved by linking
1212 AJR:204, June 2015
A Novel Appendicitis Reporting System
imaging findings with certainty scores [15, nalized interpretations by body imaging fellow- the outer wall to the inner mucosa; the presence or
27]; categorizing imaging findings as posi- ship–trained radiologists. SCOAP metrics and a absence of mucosal hyperenhancement (relative to
tive, negative, or indeterminate for appendi- data dictionary are available at a secure site [26, small bowel); the presence or absence of adjacent
citis [17, 28]; or weighing imaging findings 30]. Medical records are reviewed for demograph- fat stranding; the presence or absence of an appen-
on the basis of clinical concern [29]. In this ic and clinical variables. dicolith; the presence or absence of focal thicken-
study, we introduce a more systematic ap- The total number of patients who underwent ing of the cecum, at the base of the appendix; the
proach to the diagnosis of appendicitis on appendectomy over the period of the study was presence or absence of extraluminal periappendi-
Downloaded from www.ajronline.org by 94.237.69.42 on 06/18/20 from IP address 94.237.69.42. Copyright ARRS. For personal use only; all rights reserved
CT. This article represents a feasibility study 738. The mean age of this patient population was ceal gas; the presence or absence of gas within the
of our standardized reporting format system, 35 years (range, 15–94 years). A stratified random lumen of the appendix; and the presence or ab-
using a cohort of patients who underwent ap- sample of these patients was selected for inclusion sence of a right lower quadrant collection, defined
pendectomy at two institutions. We under- in the study, where three strata were defined by as an area of fluid attenuation with an enhancing
took this study to assess the diagnostic accu- pathology and CT findings. Specifically, all pa- wall. Radiologists also recorded whether the right
racy of the system, as well as the usefulness tients with negative findings for appendicitis on ovary was visualized and whether there was an
of specific imaging findings, and to evaluate pathology (n = 17; 2.3%) were selected as control abnormality of the right ovary, such as a cyst or
its reproducibility. patients, and all patients with positive findings on mass that might explain the patient’s right lower
pathology but negative (n = 11; 1.5%) or indeter- quadrant pain. Radiologists were also asked to re-
Materials and Methods minate (n = 34; 4.6%) findings on CT were also cord their certainty of appendicitis using a score
This study was approved with a waiver of con- selected to determine if our standardized report- of 1–5, as described.
sent from the human subjects division of the Uni- ing system represents an improvement over cur-
versity of Washington institutional review board. rent clinical practice. Last, we randomly selected Statistical Analysis
34 of 676 patients who were positive for appendi- Categoric variables were summarized as num-
Standardized Reporting System citis on both pathology and CT, for a total of 96 ber (percent) of patients, and continuous variables
Our standardized reporting system was based patients. The total of 96 was chosen to be evenly were summarized as mean or median (range).
on consultation with surgical care providers, ex- divisible among four readers, as described in the Variables were compared between patients with
pert opinion, and literature review. Using these next section. After selection, medical records of and without appendicitis on pathology using the
inputs, we developed a standardized reporting all selected patients were reviewed to confirm the Fisher exact test (categoric variables) and the
format with both objective and subjective com- pathologic diagnoses. Mann-Whitney test (continuous and ordinal vari-
ponents. The objective component consists of ables). The odds ratio (OR) was used to evaluate
a checklist of imaging findings previously de- Imaging Review the strength of association between categoric vari-
scribed to have an association with the presence Two separate reviews were performed. For the ables and pathology. The AUC was used to evalu-
or absence of appendicitis (Appendix 1) [1, 7, 11, primary review, preoperative CT scans from the ate how well each continuous or ordinal variable
12, 18, 19, 24–26]. The subjective component is selected patients were reviewed using the standard- could discriminate between those with and with-
a score of the radiologist’s certainty of the pres- ized reporting system by one of four radiologists. out appendicitis on pathology. An AUC of 0.5 is
ence or absence of appendicitis, ranging from 1 Subsequently, a second review was performed to equivalent to a random guess, whereas an AUC
(appendicitis definitely absent) through 5 (appen- evaluate interobserver reproducibility. For each of 1.0 corresponds to perfect separation between
dicitis definitely present). The objective imaging reader, six patients whose scans were previously groups. Precision was summarized using 95% CIs.
findings convey the radiologist’s decision-mak- reviewed by another reader were randomly select- Interreader agreement was assessed using Cohen’s
ing process to the clinician, and the final score re- ed to be rereviewed using the standardized report- kappa and percent agreement. Percent agreement
flects the corresponding implications toward pa- ing system. Selection was restricted such that no was calculated as 100 times the number of patients
tient management. patient was selected to be rereviewed by more than on whose scans readers were agreed divided by the
one reader. Thus, there were 96 patients in the pri- total number of patients whose scans were read by
Patient Population mary review, of whose studies 24 (25%) were re- two readers. Cohen’s kappa is another measure of
Using the Washington State Surgical Care and read in the secondary review by different readers. agreement that has been adjusted for the level of
Outcomes Assessment Program (SCOAP) data- During both reviews, the radiologists were blind- agreement expected by chance. A value of 0 in-
base [30], we identified patients who underwent ed to the patients’ initial imaging reports, patho- dicates no agreement beyond what is expected by
appendectomy over a 4-year period, from January logic diagnoses, and other clinical findings. All of chance, whereas a value of 1 indicates exact agree-
2008 to December 2012, at University of Wash- the radiologists who reviewed studies were board ment in all cases. All statistical calculations were
ington Medical Center and Harborview Medical certified with additional subspecialty fellowship conducted with the R statistical software package
Center. Most hospitals in Washington State par- training in abdominal imaging. Radiologists also (version 2.14.1, R Foundation for Statistical Com-
ticipate in SCOAP, which uses trained chart ab- had between 5 and 10 years of experience in inter- puting). Two-tailed tests were used, with p < 0.05
stractors to review all laparotomies performed at preting abdominal CT scans. denoting statistical significance.
participating hospitals. Data recorded for appen- Transverse, coronal, and sagittal images were
dectomies include preoperative CT findings (pos- retrospectively reviewed. Radiologists recorded Results
itive, negative, or indeterminate for appendici- several imaging findings, including the diameter Ninety-six patients with complete records
tis), surgical findings, and pathologic information of the appendix, measured in the mid portion and of preoperative CT, surgical findings, and
(positive or negative for appendicitis). Determina- at the tip, with instructions to measure the appen- pathologic findings were selected from the
tion of whether a CT study was positive, negative, dix in a short-axis plane; the thickness of the wall SCOAP database. After reviewing the medi-
or indeterminate for appendicitis was based on fi- of the appendix, measured in the mid portion from cal records of all 96 patients, our team cor-
AJR:204, June 2015 1213
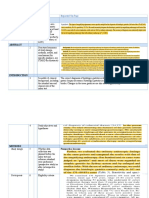
rected the data of nine patients for whom TABLE 1: Patient Characteristics, Imaging Findings, and Appendicitis Score
Godwin et al.
the SCOAP abstractors had inaccurately re- for 95 Patients
corded pathology results, seven were reclas-
Demographic and Clinical Parameters Result N
sified from having positive to having nega-
tive findings for appendicitis, and two were Sex 95
reclassified from having negative to having Male 53 (56)
positive findings. During review, one patient Female 42 (44)
was excluded owing to uninterpretable im-
Age, y 30 (18–72) 95
ages, leaving 95 patients available for anal-
Estimated weight, kg 71 (53–165) 85
Downloaded from www.ajronline.org by 94.237.69.42 on 06/18/20 from IP address 94.237.69.42. Copyright ARRS. For personal use only; all rights reserved
ysis. The mean age of the selected patients
was 33 years (range, 18–72 years) (Table 1). Height, cm 171 (142–198) 66
Of these patients, 74 (78%) had pathologic WBC count, × 10 9 /L 11 (3–24) 95
confirmation of appendicitis, and 21 (22%)
Pathology and original CT group 95
had normal appendixes at pathology. On the
basis of the original CT findings, 15 reports Positive on pathology
(16%) were discordant with pathology, and Positive imaging findings 35 (37)
39 reports (41%) were indeterminate; thus, a Indeterminate imaging findings 30 (32)
total of 54 patients (57%) were not correctly
Negative imaging findings 9 (9)
diagnosed by the CT report.
The appendix could be visualized in 89 of Negative on pathology
95 patients (94%). Clinical characteristics and Positive imaging findings 6 (6)
objective findings were compared between Indeterminate imaging findings 9 (9)
these patients with and without appendicitis by
Negative imaging findings 6 (6)
pathology (Table 2). WBC counts were signif-
icantly higher in cases with positive findings Perforated appendicitis 8 (8) 95
(median, 12 vs 7 × 109/L; p = 0.001). Of the Standardized report for appendicitis
objective CT findings, outer-outer wall diam- Appendix was visualized 89 (94) 95
eter (OR = 1.9 [6–10 vs < 6 mm], and OR =
Outer-outer wall diametera, mm 10 (3–19) 89
14 [> 10 vs < 6 mm]; p = 0.002), tip diameter
(OR = 2.7 [6–10 vs < 6 mm], and OR = ∞ [> < 6 mm 14 (16)
10 vs < 6 mm]; p = 0.007), and the presence 6–10 mm 36 (40)
of surrounding fat stranding or thickening of > 10 mm 39 (44)
pararenal or lateroconal fascia (OR = 8.9; p < Tip diametera, mm 8 (2–23) 89
0.001) all correlated significantly with the pres-
< 6 mm 27 (30)
ence of appendicitis on pathology. The pres-
ence of focal cecal thickening (OR = 3.7; p = 6–10 mm 45 (51)
0.057) was marginally significantly associat- > 10 mm 17 (19)
ed with positive findings on pathology. In the Single wall thicknessa, mm 3 (1–7) 87
82 patients who were imaged after contrast ad-
≤ 3 mm 36 (41)
ministration, the presence of mucosal hyper-
enhancement was also significantly associated > 3 mm 51 (59)
with appendicitis (OR = 8.7; p < 0.001). Mucosal hyperenhancementa,b 56 (68) 82
In the 89 patients in whom the appendix Surrounding fat stranding or thickening of pararenal or lateroconal fascia 66 (69) 95
could be visualized, the AUC of the appendi-
Appendicolitha 28 (31) 89
citis score for diagnosis of appendicitis was
0.84 (95% CI, 0.74–0.94; p < 0.001) (Table Focal cecal thickening at base 35 (37) 94
3). In the subset with indeterminate reports Periappendiceal air 7 (8) 92
(n = 35), the AUC was 0.90 (95% CI, 0.80– Right lower quadrant fluid collection, phlegmon, or abscess 9 (9) 95
0.99; p = 0.002), which was similar to the
Gas in lumen of appendixa 30 (34) 89
AUC in the group (n = 40) with reports con-
cordant with pathology (AUC = 0.95 [95% Right ovary abnormality 4 (4) 93
CI, 0.88–0.99]; p < 0.001). In the subset for Appendicitis score 95
whom the original reports were discordant 1 15 (16)
with pathology (n = 14), the AUC was 0.54
2 7 (7)
(95% CI, 0.22–0.86; p = 0.8).
Twenty-four patients were randomly se- 3 12 (13)
lected to undergo a secondary review to 4 10 (11)
evaluate interobserver reproducibility of our 5 51 (54)
reporting system (Table 4). Despite having
Note—Except where otherwise indicated, data are given as no. (%) or median (range).
more than 50% agreement in all objective aEvaluated only in cases where appendix was visualized.
findings between readers (including > 80% bExcluding seven patients who were not administered contrast material.
1214 AJR:204, June 2015
A Novel Appendicitis Reporting System
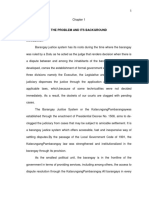
TABLE 2: Associations Between Clinical Characteristics and Objective Imaging Findings Among 89 Patients With and
Without Appendicitis in Whom Appendix Was Visualized
Result
Odds Ratio or AUCa
Demographics and Clinical Results Positive Findings (n = 71) Negative Findings (n = 18) (95% CI) pb N
Male sex 39 (55) 10 (56) 1.0 (0.3–3.1) > 0.99 89
Downloaded from www.ajronline.org by 94.237.69.42 on 06/18/20 from IP address 94.237.69.42. Copyright ARRS. For personal use only; all rights reserved
Age, y 30 (18–72) 28 (19–53) 0.56 (0.42–0.70) 0.43 89
Weight, kg 72 (53–134) 71 (54–134) 0.52 (0.37–0.66) 0.84 81
Height, cm 170 (142–198) 172 (150–193) 0.53 (0.36–0.70) 0.71 63
WBC count 12 (3–24) 7 (5–16) 0.75 (0.62–0.87) 0.001 89
Outer-outer wall diameter 0.002 89
< 6 mm 8 (11) 6 (33) Reference
6–10 mm 26 (37) 10 (56) 1.9 (0.5–7.1)
> 10 mm 37 (52) 2 (11) 14 (2.4–82)
Tip diameter 0.007 89
< 6 mm 17 (24) 10 (56) Reference
6–10 mm 37 (52) 8 (44) 2.7 (0.9–8.1)
> 10 mm 17 (24) 0 (0) ∞
Single wall thickness > 3 mm 31 (44) 5 (31) 1.7 (0.5–6.9) 0.41 87
Mucosal hyperenhancementc 51 (78) 5 (29) 8.7 (2.3–36) < 0.001 82
Surrounding fat stranding or thickening of pararenal or 58 (82) 6 (33) 8.9 (2.5–34) < 0.001 89
lateroconal fascia
Appendicolith 24 (34) 4 (22) 1.8 (0.5–8.2) 0.41 89
Focal cecal thickening at base 30 (42) 3 (17) 3.7 (0.9–21) 0.057 89
Periappendiceal air 5 (7) 0 (0) ∞ 0.58 89
Right lower quadrant fluid collection, phlegmon, or abscess 7 (10) 0 (0) ∞ 0.34 89
Gas in lumen of appendix 26 (37) 4 (22) 2.0 (0.6–9.3) 0.28 89
Absence of right ovary abnormalityd 29 (94) 5 (71) 5.8 (0.3–92) 0.15 38
Note—Except where otherwise indicated, data are given as no. (%) or median (range).
aOdds ratio was calculated for binary variables and AUC for continuous variables.
bFisher exact test was used for binary variables.
cIn only those patients administered contrast material.
dIn female patients only.
TABLE 3: ROC Analysis of Appendicitis Score for 89 Patients in Whom Appendix Was Visualized and Subgroups
Appendicitis Score
Mean
Group (Range) 1 2 3 4 5 AUC (95% CI) p
All cases (N = 89) 0.84 (0.74–0.94) < 0.001
Positive (n = 71) 4.3 (1–5) 6 (8) 1 (1) 8 (11) 8 (11) 48 (68)
Negative (n = 18) 2.3 (1–5) 6 (33) 5 (28) 4 (22) 1 (6) 2 (11)
Original report concordant with pathology (N = 40) 0.95 (0.88–0.99) < 0.001
Positive (n = 35) 4.6 (1–5) 1 (3) 1 (3) 2 (6) 2 (6) 29 (83)
Negative (n = 5) 2.0 (1–4) 2 (40) 2 (40) 0 (0) 1 (20) 0 (0)
Original report indeterminate (N = 35) 0.90 (0.80–0.99) 0.001
Positive (n = 28) 4.1 (1–5) 3 (11) 0 (0) 4 (14) 5 (18) 16 (57)
Negative (n = 7) 1.9 (1–3) 3 (43) 2 (29) 2 (29) 0 (0) 0 (0)
Note—Except where otherwise indicated, data are given as no. (%).
AJR:204, June 2015 1215
Godwin et al.
TABLE 4: Interreader Agreement of the Standardized Reporting Format in 24 Patients Randomly Selected for
Secondary Review
Result
Primary Secondary
Parameter Reader Reader κ (95% CI) % Agreement Na
Appendicitis score
Downloaded from www.ajronline.org by 94.237.69.42 on 06/18/20 from IP address 94.237.69.42. Copyright ARRS. For personal use only; all rights reserved
1–2 8 (33) 10 (42) 0.30 (–0.03 to 0.63) 58 24
3 3 (12) 3 (12)
4–5 13 (54) 11 (46)
Appendix visualized 22 (92) 21 (88) 0.33 (–0.37 to 0.99) 88 24
Outer-outer wall diameter 0.36 (0.02–0.70) 60 20
< 6 mm 5 (25) 3 (15)
6–10 mm 9 (45) 11 (55)
> 10 mm 6 (30) 6 (30)
Tip diameter 0.20 (–0.18 to 0.59) 55 20
< 6 mm 6 (30) 6 (30)
6–10 mm 11 (55) 12 (60)
> 10 mm 3 (15) 2 (10)
Single wall thickness > 3 mm 7 (39) 3 (17) -0.04 (–0.58 to 0.50) 56 18
Mucosal hyperenhancementb 13 (72) 11 (61) 0.01 (–0.50 to 0.52) 56 18
Surrounding fat stranding or thickening of pararenal or lateroconal fascia 13 (54) 11 (46) 0.17 (–0.22 to 0.56) 58 24
Appendicolith 5 (25) 5 (25) 0.73 (0.38–0.99) 90 20
Focal cecal thickening at base 9 (39) 6 (26) 0.32 (–0.10 to 0.74) 70 23
Periappendiceal air 1 (4) 1 (4) -0.05 (–1.43 to 0.99) 91 23
Right lower quadrant fluid collection, phlegmon, or abscess 1 (4) 2 (8) -0.06 (–1.18 to 0.99) 88 24
Gas in lumen of appendix 5 (25) 6 (30) 0.62 (0.23–0.99) 85 20
Right ovary abnormalityc 1 (9) 2 (18) 0.62 (–0.09 to 0.99) 91 11
Note—Except where otherwise indicated, data are given as no. (%).
aNo. of patients for whom both readers reported measurements.
bIn only those patients administered contrast material.
cIn female patients only.
reproducibility in findings of extraluminal jective score expresses the readers’ degree of Communication of objective findings in a
periappendiceal air, the presence of a right certainty regarding the presence or absence radiology report serves two purposes. First,
lower quadrant fluid collection, and the pres- of appendicitis and had good sensitivity and radiologists are more accurate when system-
ence of an appendicolith), the correspond- specificity for appendicitis in our study. ically weighing the presence or absence of
ing Cohen’s kappa for the certainty score κ = The need for standardization of reporting specific imaging findings before coming to a
0.30 (95% CI, –0.03 to 0.65; p = 0.07), and has been recognized since the inception of ra- final conclusion. In a series of 53 CT exam-
the percent agreement was 58%. diology [31]. It was not until the creation of inations, Kim et al. [28] showed improved
the BI-RADS that this problem was wide- diagnostic accuracy for appendicitis cases
Discussion ly and effectively addressed. BI-RADS was with previously indeterminate findings when
Our appendicitis standardized reporting created to combine literature-derived objec- radiologists reevaluated the studies using a
format was created to increase accuracy in tive findings with recommendation to clini- 4-point scale. Second, a clear list of findings
the diagnosis of appendicitis and to improve cians for further management on the basis of documents the information the radiologist
communication between radiologists and cli- the likelihood of malignancy. BI-RADS has used to determine the final likelihood of ap-
nicians. The objective checklist includes im- shown that the standardization of terminology pendicitis, allowing the referring clinician or
aging findings that are highly associated with and management recommendations improves surgeon to understand the radiologist’s deci-
appendicitis. In our study, increased appen- communication and patient outcomes [32]. sion-making process.
diceal diameter, periappendiceal fat strand- The success of BI-RADS led to the creation of Our results confirm that the CT findings
ing, and appendiceal mucosal hyperenhance- the Liver Imaging Reporting and Data System of increased appendiceal body diameter, in-
ment had a statistically significant association (LI-RADS), with the intention to standardize creased appendiceal tip diameter, mucosal
with appendicitis on pathology. The final sub- hepatic diagnostic imaging [33]. hyperenhancement, and periappendiceal fat
1216 AJR:204, June 2015
A Novel Appendicitis Reporting System
stranding or lateroconal fascia thickening for the presence or absence of right ovar- ing it prospectively in a cohort of patients
were significantly associated with appendi- ian abnormalities; however, because these undergoing CT evaluation for the indication
citis. These findings have been frequently imaging findings were uncommon, Cohen’s of ruling out appendicitis. Another poten-
documented in the literature [1, 12, 15, 18, kappa values were low (κ = –0.05, 0.06, and tial limitation may arise from differences in
34], and the present study adds to the avail- 0.62, respectively). Interestingly, the pres- reader experience; radiologists of different
able data. In our study, imaging findings sug- ence of fat stranding or fascial thickening, training levels provided the initial clinical
gesting perforated appendicitis—including mucosal hyperenhancement, and increased reports, whereas all of the readers in our ret-
Downloaded from www.ajronline.org by 94.237.69.42 on 06/18/20 from IP address 94.237.69.42. Copyright ARRS. For personal use only; all rights reserved
periappendiceal air and a right lower quad- appendiceal diameter had only moderate in- rospective analysis were fellowship-trained
rant fluid collection—were always associ- terobserver agreement (percent agreement, radiologists. The improvement in accura-
ated with appendicitis at pathology, but the 58%, 56%, and 60%, respectively) and low cy that we found could be attributed to the
number of cases where these findings were Cohen’s kappa values (κ = 0.17, 0.01, and use of a systematic approach to objective
present was too low to reach statistical sig- 0.36, respectively). Given that these imag- and subjective findings, or it could reflect
nificance. Similarly, there were insufficient ing findings have been reported as being as- the higher experience level of our readers
cases of ovarian pathology to evaluate an as- sociated with appendicitis both by sever- [17, 25, 29]. Furthermore, the determina-
sociation. The presence of appendiceal wall al previous studies [7, 8, 10, 12, 15, 17–19, tion of whether a CT report is positive, neg-
thickening and gas in the lumen of the ap- 24, 35, 36] and in our analysis, the lack of ative, or indeterminate for appendicitis was
pendix have previously been reported as hav- agreement is notable. made by chart review performed by a non-
ing associations with appendicitis [8, 18, 24, Furthermore, despite the high agreement radiologist and nonphysician abstractor as
25, 34] but did not have a significant associa- in many objective findings, the agreement of part of the SCOAP initiative. It is possible
tion in our study. subjective scores, assigned by our four read- that CT findings considered as indetermi-
One encouraging result seen in this study ers, was only moderate, at 58% (κ = 0.30). nate for appendicitis by a SCOAP abstrac-
is that, through the standardized reporting This may reflect the subjective nature of our tor might have been considered as positive
approach, the appendicitis score had a good scoring system. In clinical settings, some of findings for appendicitis by a trained sur-
correspondence with pathology, even in the the variability in subjective scoring might be geon or emergency department physician.
35 cases with indeterminate diagnoses on related to differences in detection of specific This potential pitfall in our study highlights
initial CT, where the AUC was 0.90. How- findings, but this did not appear to be a sig- the for need for standardization of radiolo-
ever, 13% (12 of 89) of our cases were as- nificant contributing factor in our analysis, gy reports and is a reason for the creation of
signed a score of 3, indeterminate for ap- given that readers reported objective find- our standardized format.
pendicitis. Most other published studies ings with similar rates of detection. Muco- In summary, our standardized report-
evaluating the diagnostic accuracy of CT sal hyperenhancement and periappendiceal ing system for appendicitis performed well
have not included such a CT-indeterminate fat stranding are often obvious, but in more in identifying cases of appendicitis. Fu-
group [6, 10–12, 18, 24, 27, 35–38]. Oth- subtle cases, radiologists will have differ- ture retrospective and prospective studies
er studies have also acknowledged the dif- ing thresholds for reporting a finding. Varia- with larger patient populations will guide
ficulty of decreasing the number of indeter- tion can be mitigated by establishing clearer in the development of the system and will
minate cases, using the presence or absence guidelines. Future studies will also include likely provide a large enough dataset for
of imaging findings [17, 26, 28]. Daly et al. several training cases, so that readers can multivariate analysis of appendicitis-spe-
[17] found that 10% of CT examinations practice using this reporting system. cific imaging findings. For now, our data
will remain equivocal even after thorough There were several limitations to our suggest that the likelihood for appendicitis
review, similar to our results. Our readers study. First, because our study population can be more confidently based on the pres-
used the standardized report to successfully was restricted to patients who underwent ence or absence of specific imaging find-
reduce the number of CT scans deemed in- appendectomy, that introduces a selection ings, rather than relying on overall gestalt.
determinate while improving accuracy. bias compared with the population of pa- Although CT has revolutionized the work-
Despite the strong correlations with path- tients being evaluated for possible appen- up of appendicitis with a substantial drop
ologic findings, as well as an incremen- dicitis. Our patients may have been more in the number of missed appendicitis cas-
tal improvement in accuracy where initial likely to have clinical features of appendi- es and the number of negative appendec-
clinical interpretations are indeterminate, citis and a high pretest probability, because tomies [5, 7, 8, 11, 12, 15, 19, 24], further
correlation between multiple readers was all underwent laparotomy and appendec- development and adoption of a standard-
variable in our study. Several objective im- tomy. This limitation was somewhat miti- ized reporting format may continue to im-
aging findings in our standardized report gated given that we preferentially included prove accuracy of appendicitis diagnosis,
had high agreement between readers, in- analysis of CT reports that were interpret- increase the quality of radiologist-clinician
cluding the presence of an appendicolith, ed as being either indeterminate or negative communication, and ultimately optimize
focal cecal thickening, and the presence for the presence of appendicitis. We chose patient management.
of gas within the appendix (percent agree- to evaluate patients who underwent sur-
ment, 90%, 70%, and 85%, respectively). gery as an initial test of the reporting sys- References
Agreement was also high on findings sug- tem, so that comparison could be made to 1. Rosen MP, Ding A, Blake MA, et al. ACR Appro-
gesting perforated appendicitis (includ- the pathologic reference standard of appen- ®
priateness Criteria right lower quadrant pain:
ing extraluminal periappendiceal gas and dicitis. To assess the generalizability of this suspected appendicitis. J Am Coll Radiol 2011;
right lower quadrant fluid collections) and reporting system, we are currently evaluat- 8:749–755
AJR:204, June 2015 1217
Godwin et al.
2. Flum DR, Koepsell T. The clinical and economic mance of nonfocused helical computed tomogra- niques for appendiceal imaging. AJR 2001;
correlates of misdiagnosed appendicitis: nation- phy in the diagnosis of acute appendicitis. J Com- 176:933–941
wide analysis. Arch Surg 2002; 137:799–804; dis- put Assist Tomogr 2003; 27:583–589 28. Kim HC, Yang DM, Kim SW, Park SJ. Reassess-
cussion, 804 15. Jacobs JE, Birnbaum BA, Macari M, et al. Acute ment of CT images to improve diagnostic accura-
3. Hale DA, Molloy M, Pearl RH, Schutt DC, Jaques appendicitis: comparison of helical CT diagnosis cy in patients with suspected acute appendicitis
DP. Appendectomy: a contemporary appraisal. focused technique with oral contrast material versus and an equivocal preoperative CT interpretation.
Ann Surg 1997; 225:252–261 nonfocused technique with oral and intravenous Eur Radiol 2012; 22:1178–1185
Downloaded from www.ajronline.org by 94.237.69.42 on 06/18/20 from IP address 94.237.69.42. Copyright ARRS. For personal use only; all rights reserved
4. Krajewski S, Brown J, Phang PT, Raval M, Brown contrast material. Radiology 2001; 220:683–690 29. Blackmore CC, Terasawa T. Optimizing the inter-
CJ. Impact of computed tomography of the abdo- 16. Drake FT, Florence MG, Johnson MG, et al. Prog- pretation of CT for appendicitis: modeling health
men on clinical outcomes in patients with acute ress in the diagnosis of appendicitis: a report from utilities for clinical practice. J Am Coll Radiol
right lower quadrant pain: a meta-analysis. Can J Washington State’s Surgical Care and Outcomes 2006; 3:115–121
Surg 2011; 54:43–53 Assessment Program. Ann Surg 2012; 256:586–594 30. SCOAP: Surgical Care and Outcomes Assessment
5. Drake FT, Flum DR. Improvement in the diagno- 17. Daly CP, Cohan RH, Francis IR, Caoili EM, Ellis Program. www.SCOAP.org/. Accessed March 3, 2015
sis of appendicitis. Adv Surg 2013; 47:299–328 JH, Nan B. Incidence of acute appendicitis in pa- 31. Reiner BI, Knight N, Siegel EL. Radiology report-
6. Walker S, Haun W, Clark J, McMillin K, Zeren F, tients with equivocal CT findings. AJR 2005; ing, past, present, and future: the radiologist’s per-
Gilliland T. The value of limited computed to- 184:1813–1820 spective. J Am Coll Radiol 2007; 4:313–319
mography with rectal contrast in the diagnosis of 18. Choi D, Park H, Lee YR, et al. The most useful 32. Reiner BI. Medical imaging data reconciliation.
acute appendicitis. Am J Surg 2000; 180:450– findings for diagnosing acute appendicitis on con- Part 4. Reconciliation of radiology reports and
454; discussion, 454–455 trast-enhanced helical CT. Acta Radiol 2003; clinical outcomes data. J Am Coll Radiol 2011;
7. Ives EP, Sung S, McCue P, Durrani H, Halpern EJ. 44:574–582 8:858–862
Independent predictors of acute appendicitis on 19. Birnbaum BA, Wilson SR. Appendicitis at the 33. Purysko AS, Remer EM, Coppa CP, Leao Filho
CT with pathologic correlation. Acad Radiol millennium. Radiology 2000; 215:337–348 HM, Thupili CR, Veniero JC. LI-RADS: a case-
2008; 15:996–1003 20. Flum DR, McClure TD, Morris A, Koepsell T. Mis- based review of the new categorization of liver
8. Horton MD, Counter SF, Florence MG, Hart MJ. diagnosis of appendicitis and the use of diagnostic findings in patients with end-stage liver disease.
A prospective trial of computed tomography and imaging. J Am Coll Surg 2005; 201:933–939 RadioGraphics 2012; 32:1977–1995
ultrasonography for diagnosing appendicitis in the 21. Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ. 34. van Randen A, Lameris W, van Es HW, et al. Pro-
atypical patient. Am J Surg 2000; 179:379–381 Diagnostic performance of multidetector comput- files of US and CT imaging features with a high
9. Stroman DL, Bayouth CV, Kuhn JA, et al. The ed tomography for suspected acute appendicitis. probability of appendicitis. Eur Radiol 2010;
role of computed tomography in the diagnosis of Ann Intern Med 2011; 154:789–796 20:1657–1666
acute appendicitis. Am J Surg 1999; 178:485–489 22. Seetahal SA, Bolorunduro OB, Sookdeo TC, et al. 35. Krishnamoorthi R, Ramarajan N, Wang NE, et al.
10. Kamel IR, Goldberg SN, Keogan MT, Rosen MP, Negative appendectomy: a 10-year review of a na- Effectiveness of a staged US and CT protocol for
Raptopoulos V. Right lower quadrant pain and tionally representative sample. Am J Surg 2011; the diagnosis of pediatric appendicitis: reducing
suspected appendicitis: nonfocused appendiceal 201:433–437 radiation exposure in the age of ALARA. Radiol-
CT—review of 100 cases. Radiology 2000; 23. Teixeira PG, Demetriades D. Appendicitis: chang- ogy 2011; 259:231–239
217:159–163 ing perspectives. Adv Surg 2013; 47:119–140 36. Seo H, Lee KH, Kim HJ, et al. Diagnosis of acute
11. Rao PM, Rhea JT, Novelline RA, et al. Helical CT 24. Moteki T, Horikoshi H. New CT criterion for appendicitis with sliding slab ray-sum interpreta-
technique for the diagnosis of appendicitis: pro- acute appendicitis: maximum depth of intralumi- tion of low-dose unenhanced CT and standard-
spective evaluation of a focused appendix CT ex- nal appendiceal fluid. AJR 2007; 188:1313–1319 dose IV contrast-enhanced CT scans. AJR 2009;
amination. Radiology 1997; 202:139–144 25. Cabarrus M, Sun YL, Courtier JL, Stengel JW, 193:96–105
12. Rao PM, Rhea JT, Novelline RA. Sensitivity and Coakley FV, Webb EM. The prevalence and pat- 37. Soyer P, Dohan A, Eveno C, et al. Pitfalls and
specificity of the individual CT signs of appendicitis: terns of intraluminal air in acute appendicitis at mimickers at 64-section helical CT that cause
experience with 200 helical appendiceal CT exami- CT. Emerg Radiol 2013; 20:51–56 negative appendectomy: an analysis from 1057
nations. J Comput Assist Tomogr 1997; 21:686–692 26. Webb EM, Wang ZJ, Coakley FV, Poder L, West- appendectomies. Clin Imaging 2013; 37:895–901
13. Raja AS, Wright C, Sodickson AD, et al. Negative phalen AC, Yeh BM. The equivocal appendix at 38. Weyant MJ, Eachempati SR, Maluccio MA, et al.
appendectomy rate in the era of CT: an 18-year CT: prevalence in a control population. Emerg Interpretation of computed tomography does not
perspective. Radiology 2010; 256:460–465 Radiol 2010; 17:57–61 correlate with laboratory or pathologic findings in
14. Raman SS, Kadell BM, Vodopich DJ, Sayer J, 27. Wise SW, Labuski MR, Kasales CJ, et al. Com- surgically confirmed acute appendicitis. Surgery
Cryer H, Lu DS. Patient gender-related perfor- parative assessment of CT and sonographic tech- 2000; 128:145–152
(Appendix starts on next page)
1218 AJR:204, June 2015
A Novel Appendicitis Reporting System
APPENDIX 1: Standardized Imaging Report for Appendicitis
1. Appendix visualized? Yes No
2. Outer-outer wall diameter _ mm
3. Tip diameter _ mm
4. Single wall thickness _ mm
Downloaded from www.ajronline.org by 94.237.69.42 on 06/18/20 from IP address 94.237.69.42. Copyright ARRS. For personal use only; all rights reserved
5. Mucosal hyperenhancement? Yes No
6. Surrounding fat stranding or thickening of pararenal or lateroconal fascia? Yes No
7. Appendicolith? Yes No
8. Focal cecal thickening at base of appendix? Yes No
9. Periappendiceal air? Yes No
10. Right lower quadrant fluid collection, phlegmon, or abscess? Yes No
11. Gas in lumen of appendix? Yes No
12. Right ovary (in female patients) Normal Abnormal
13. Certainty score 1, Appendicitis definitely absent
2, Appendicitis unlikely
3, Indeterminate
4, Appendicitis likely
5, Appendicitis definitely present
AJR:204, June 2015 1219
You might also like
- Oral Radiology Principles and Interpretation 7th Ed PDFDocument14 pagesOral Radiology Principles and Interpretation 7th Ed PDFLaura Victoria Alvarez RodriguezNo ratings yet
- Speak Up An Illustrated Guide To Public Speaking 4th Edition Fraleigh Test BankDocument7 pagesSpeak Up An Illustrated Guide To Public Speaking 4th Edition Fraleigh Test Bankngocalmai0236h100% (26)
- Cuiosity CabinetDocument425 pagesCuiosity CabinetDRagonrouge50% (2)
- Guo 2019Document10 pagesGuo 2019cifha rajesh saldanhaNo ratings yet
- PDF History Physical Examination Laboratorytesting and Emergency Department DDDocument17 pagesPDF History Physical Examination Laboratorytesting and Emergency Department DDNurul FatimahNo ratings yet
- Acute Appendicitis in Young AdultsDocument9 pagesAcute Appendicitis in Young AdultsAtika RahmahNo ratings yet
- PIIS1590865822004741Document7 pagesPIIS1590865822004741cifha rajesh saldanhaNo ratings yet
- 2018 A Systematic: SNP EncodingDocument5 pages2018 A Systematic: SNP EncodingShreyash DattaNo ratings yet
- PIIS258975002200070XDocument13 pagesPIIS258975002200070XAnonymous HUY0yRexYfNo ratings yet
- Improvement of Gastroscopy Classification Performance Through Image Augmentation Using A Gradient-Weighted Class Activation MapDocument9 pagesImprovement of Gastroscopy Classification Performance Through Image Augmentation Using A Gradient-Weighted Class Activation Maphalouane omarNo ratings yet
- Cheng, P. M. Et Al 2018Document9 pagesCheng, P. M. Et Al 2018Anonymous N7KGZx9rNo ratings yet
- Radiol 2503080541Document10 pagesRadiol 2503080541Dương Tiến TrungNo ratings yet
- Ajr 16 17413 PDFDocument11 pagesAjr 16 17413 PDFSashaNo ratings yet
- Elevating Diagnostic Precision With ResNet Models and Fastai Framework in Gastrointestinal Pathology RecognitionDocument10 pagesElevating Diagnostic Precision With ResNet Models and Fastai Framework in Gastrointestinal Pathology RecognitionselvaNo ratings yet
- Apendiks AlvaradoDocument5 pagesApendiks AlvaradoRendy Grinaldi FadilahNo ratings yet
- Decreased Use of Computed Tomography With A Modified Clinical Scoring System in Diagnosis of Pediatric Acute AppendicitisDocument4 pagesDecreased Use of Computed Tomography With A Modified Clinical Scoring System in Diagnosis of Pediatric Acute AppendicitisHugoNogueiraPereiraNo ratings yet
- Jurnal 1Document6 pagesJurnal 1Ahmad Fari Arief LopaNo ratings yet
- Artigo 01 Model-Based Iterative Reconstruction in CT EnterographyDocument9 pagesArtigo 01 Model-Based Iterative Reconstruction in CT EnterographyKleytonSilvaNo ratings yet
- IJGM 310577 Modified Chest X Ray Scoring System in Evaluating Severity oDocument7 pagesIJGM 310577 Modified Chest X Ray Scoring System in Evaluating Severity otaki takiwNo ratings yet
- Classifying Patients Suspected of Appendicitis With Regard To LikelihoodDocument6 pagesClassifying Patients Suspected of Appendicitis With Regard To LikelihoodabybmusNo ratings yet
- HealthDocument1 pageHealthUp ApNo ratings yet
- To Determine Validity of Ultrasound in Predicting Acute Appendicitis AmongDocument6 pagesTo Determine Validity of Ultrasound in Predicting Acute Appendicitis AmongIkki DongNo ratings yet
- Research ArticleDocument6 pagesResearch ArticleCostin VrabieNo ratings yet
- Can Enhanced Techniques Improve The Diagnostic Accuracy of Transvaginal Sonography and Magnetic Resonance Imaging For Rectosigmoid Endometriosis? A Systematic Review and Meta-AnalysisDocument16 pagesCan Enhanced Techniques Improve The Diagnostic Accuracy of Transvaginal Sonography and Magnetic Resonance Imaging For Rectosigmoid Endometriosis? A Systematic Review and Meta-AnalysisNelson Carvas JrNo ratings yet
- DaSilva 2021Document12 pagesDaSilva 2021goldfishxNo ratings yet
- LancetDocument12 pagesLancetBiblioteca Centro Médico De Mar del PlataNo ratings yet
- Publicação ICSDocument7 pagesPublicação ICSProdutos IntraviewNo ratings yet
- CEKLIST STARD PENUGASAN 2.5 Beta 1Document38 pagesCEKLIST STARD PENUGASAN 2.5 Beta 1Arnetta NovitaliaNo ratings yet
- 10 1016@j Joen 2018 08 006Document6 pages10 1016@j Joen 2018 08 006Jorge OrbeNo ratings yet
- Radiologic Assessment of Periapical Health: Comparison of 3 Different Index SystemsDocument5 pagesRadiologic Assessment of Periapical Health: Comparison of 3 Different Index SystemsHari PriyaNo ratings yet
- Video Capsule EndosDocument3 pagesVideo Capsule EndosRobert GodeanuNo ratings yet
- E001595 FullDocument7 pagesE001595 FullBriana Cerna TerronesNo ratings yet
- E000428 FullDocument9 pagesE000428 FullPilar CabelloNo ratings yet
- 1618 4726 1 PB PDFDocument6 pages1618 4726 1 PB PDFDrive IyasNo ratings yet
- Reddan 2018Document9 pagesReddan 2018Meris JugadorNo ratings yet
- GMC List of Skills 2019Document4 pagesGMC List of Skills 2019Harry DeanNo ratings yet
- BF 01887304Document4 pagesBF 01887304zuhdi azzyumar dhiniNo ratings yet
- An Asian Consensus On Standards of Diagnostic Upper Endoscopy For NeoplasiaDocument12 pagesAn Asian Consensus On Standards of Diagnostic Upper Endoscopy For NeoplasiaVanessa BecerraNo ratings yet
- Jurnal InternasionalDocument11 pagesJurnal InternasionalFitri MahmudahNo ratings yet
- Wang 2020Document9 pagesWang 2020cifha rajesh saldanhaNo ratings yet
- Identifikasi QRS Kompleks Pada EKG Non-StasionariDocument6 pagesIdentifikasi QRS Kompleks Pada EKG Non-StasionariMuhammad SyaifullahNo ratings yet
- Does Acupressure Help Reduce NDocument7 pagesDoes Acupressure Help Reduce NUtami DewiNo ratings yet
- Radiol 221894Document10 pagesRadiol 221894JEFFERSON MUÑOZNo ratings yet
- The Learning Curve For In-Vivo Characterisation of Small Colonic Polyps: Number Needed To Train (NNT) Is 200 PolypsDocument1 pageThe Learning Curve For In-Vivo Characterisation of Small Colonic Polyps: Number Needed To Train (NNT) Is 200 Polypsrussell153No ratings yet
- Jurnal 2Document12 pagesJurnal 2Zella ZakyaNo ratings yet
- Jehle1989 Emergency Department Sonography byDocument7 pagesJehle1989 Emergency Department Sonography byMohammed NgNo ratings yet
- Pediatric Appendicitis Score For Identifying Acute Appendicitis in Children Presenting With Acute Abdominal Pain To The Emergency DepartmentDocument5 pagesPediatric Appendicitis Score For Identifying Acute Appendicitis in Children Presenting With Acute Abdominal Pain To The Emergency DepartmentShikya AbnasNo ratings yet
- Real-Life Chromoendoscopy For Neoplasia Detection and Characterisation in Long-Standing IBDDocument9 pagesReal-Life Chromoendoscopy For Neoplasia Detection and Characterisation in Long-Standing IBDdeniadillaNo ratings yet
- Near-Infrared-Based Cerebral Oximetry For Prediction of Severe Acute Kidney InjuryDocument9 pagesNear-Infrared-Based Cerebral Oximetry For Prediction of Severe Acute Kidney InjuryOğuz KayıkçıNo ratings yet
- Diagnostic Accuracy of Magnetic Resonance Imaging in Assessing Placental Adhesion Disorder in Patients With Placenta Previa: Correlation With Histological FindingsDocument66 pagesDiagnostic Accuracy of Magnetic Resonance Imaging in Assessing Placental Adhesion Disorder in Patients With Placenta Previa: Correlation With Histological FindingsTiara FebrinaNo ratings yet
- Validation of The Oscillometric Blood Pressure MonDocument6 pagesValidation of The Oscillometric Blood Pressure MonPkarlNo ratings yet
- Main - 10 37 28Document4 pagesMain - 10 37 28Yavuz CarasoNo ratings yet
- Volume Imaging in The Abdomen With Ultrasound: How We Do ItDocument7 pagesVolume Imaging in The Abdomen With Ultrasound: How We Do Itlehoainam8744No ratings yet
- Deepaaa: Clinically Applicable and Generalizable Detection of Abdominal Aortic Aneurysm Using Deep LearningDocument10 pagesDeepaaa: Clinically Applicable and Generalizable Detection of Abdominal Aortic Aneurysm Using Deep LearningIzzHyukNo ratings yet
- World Neurosurg 2021 Apr 2 Camino-Willhuber GDocument6 pagesWorld Neurosurg 2021 Apr 2 Camino-Willhuber GFernando SousaNo ratings yet
- Automated Technique To Measure Noise in Clinical CT ExaminationsDocument7 pagesAutomated Technique To Measure Noise in Clinical CT ExaminationsJavieraNo ratings yet
- Application of Computer-Aided Diagnosis On Breast UltrasonographyDocument8 pagesApplication of Computer-Aided Diagnosis On Breast UltrasonographySummrina KanwalNo ratings yet
- Section & Topic No. X Item Reported On Page: Title orDocument7 pagesSection & Topic No. X Item Reported On Page: Title orRatihNo ratings yet
- Automated Detection of Fundus PhotographDocument6 pagesAutomated Detection of Fundus PhotographAldrin KarunaharanNo ratings yet
- Analysis of Diabetic Retinopathy Using Naive Bayes Classifier TechniqueDocument3 pagesAnalysis of Diabetic Retinopathy Using Naive Bayes Classifier TechniqueherantiNo ratings yet
- Evaluation of Australian National Surveillance UnitDocument7 pagesEvaluation of Australian National Surveillance UnitAna Paula BetaressiNo ratings yet
- How to Perform Ultrasonography in EndometriosisFrom EverandHow to Perform Ultrasonography in EndometriosisStefano GuerrieroNo ratings yet
- Miller-Fisher Syndrome: Is The Ataxia Central or Peripheral?Document3 pagesMiller-Fisher Syndrome: Is The Ataxia Central or Peripheral?Giga HasabiNo ratings yet
- SEOM TTCC Clinical Guideline in Nasopharynx Cancer 2021Document11 pagesSEOM TTCC Clinical Guideline in Nasopharynx Cancer 2021Giga HasabiNo ratings yet
- PIRS 20 ScoringDocument1 pagePIRS 20 ScoringGiga HasabiNo ratings yet
- CafeatedenDocument15 pagesCafeatedenGiga HasabiNo ratings yet
- Menu Mediterranea DESEMBER 2022Document20 pagesMenu Mediterranea DESEMBER 2022Giga HasabiNo ratings yet
- GSAQDocument1 pageGSAQGiga HasabiNo ratings yet
- Pasien 4Document2 pagesPasien 4Giga HasabiNo ratings yet
- Jurnal IGDDocument6 pagesJurnal IGDGiga HasabiNo ratings yet
- 4 Irfan Nanda, 20th MRS 6/8/22 No RM 020217 09 SK HA S Lab 06/08/22 Plan UPD Plan NeuroDocument2 pages4 Irfan Nanda, 20th MRS 6/8/22 No RM 020217 09 SK HA S Lab 06/08/22 Plan UPD Plan NeuroGiga HasabiNo ratings yet
- Toxoplasmaencephalitisin AIDSpatientsadmittedtothe Douala General Hospitalbetween 2004 and 2009 AcrosssectionalstudyDocument6 pagesToxoplasmaencephalitisin AIDSpatientsadmittedtothe Douala General Hospitalbetween 2004 and 2009 AcrosssectionalstudyGiga HasabiNo ratings yet
- Untitled 4Document1 pageUntitled 4Giga HasabiNo ratings yet
- Oamjms 9b 1111Document6 pagesOamjms 9b 1111Giga HasabiNo ratings yet
- Stunting, BMJDocument10 pagesStunting, BMJGiga HasabiNo ratings yet
- Running Head: Practicing Nurse Self-ReflectionDocument9 pagesRunning Head: Practicing Nurse Self-ReflectionMorgan OkothNo ratings yet
- Creswell 2005 Literature ReviewDocument5 pagesCreswell 2005 Literature Reviewaflsiosbe100% (1)
- 1.2 Statement of The ProblemDocument5 pages1.2 Statement of The Problem20PCM131- VIDHYADEVI.SNo ratings yet
- Advanced MarketingDocument13 pagesAdvanced Marketingjme_pescasioNo ratings yet
- Research Methodology MCQ (Multiple Choice Questions) - JavaTpointDocument17 pagesResearch Methodology MCQ (Multiple Choice Questions) - JavaTpointManjunath SPNo ratings yet
- Pulverized Anahaw Leaf Saribus Rotundifolius As A Main Component in Making Portland Pozzolana CementDocument40 pagesPulverized Anahaw Leaf Saribus Rotundifolius As A Main Component in Making Portland Pozzolana CementAnabelleNo ratings yet
- Ge 5 EthicsDocument59 pagesGe 5 EthicsWell WellNo ratings yet
- What Is A Null Hypothesis8Document6 pagesWhat Is A Null Hypothesis8a d100% (1)
- 1834 Census of Höizel in The District of Saratov, RussiaDocument25 pages1834 Census of Höizel in The District of Saratov, RussiaMateus CoutoNo ratings yet
- The Cognitive Neuroscience of Apraxia: GlossaryDocument10 pagesThe Cognitive Neuroscience of Apraxia: GlossaryDiane MxNo ratings yet
- Multi-Objective Optimization of Milling Parameters e The Trade-Offs Between Energy, Production Rate and Cutting QualityDocument10 pagesMulti-Objective Optimization of Milling Parameters e The Trade-Offs Between Energy, Production Rate and Cutting QualityJesvin AbrahamNo ratings yet
- Chapter 2 Issues in Ex-Ante and Ex-Post Evaluations: Outline of This ChapterDocument86 pagesChapter 2 Issues in Ex-Ante and Ex-Post Evaluations: Outline of This ChapterReashiela LucenaNo ratings yet
- Eruption! Discussion GuideDocument5 pagesEruption! Discussion GuideHoughton Mifflin HarcourtNo ratings yet
- Two Different Notions of Value-FormDocument11 pagesTwo Different Notions of Value-FormppphhwNo ratings yet
- Patient Satisfaction and Benefts of Music Therapy Services To Manage Stress and Pain in The Hospital Emergency DepartmentDocument25 pagesPatient Satisfaction and Benefts of Music Therapy Services To Manage Stress and Pain in The Hospital Emergency DepartmentBapak Sunaryo SPBU100% (1)
- Design Lab 4 UDocument2 pagesDesign Lab 4 UCátia Tiago RijoNo ratings yet
- CO - MSc28 - FM - Avanced Corporate Finance 2019-2020 DEFDocument12 pagesCO - MSc28 - FM - Avanced Corporate Finance 2019-2020 DEFshalabh_hscNo ratings yet
- Fidia Oktarisa, 2023Document14 pagesFidia Oktarisa, 2023AUFA DIAZ CAMARANo ratings yet
- Curriculum Process.: D. K. Wheeler. London: University of LondonDocument1 pageCurriculum Process.: D. K. Wheeler. London: University of LondonArslan Ahmad BhuttaNo ratings yet
- Module 1 - Concept PresentationDocument4 pagesModule 1 - Concept PresentationCherylyn BenoliraoNo ratings yet
- Unit - IV - Spearman Rank CorrelationDocument31 pagesUnit - IV - Spearman Rank CorrelationmishtiismeNo ratings yet
- Epidemiology and Individual, Household and Geographical Risk Factors of Podoconiosis in Ethiopia Results From The First Nationwide Mapping. AJTMH 2015Document11 pagesEpidemiology and Individual, Household and Geographical Risk Factors of Podoconiosis in Ethiopia Results From The First Nationwide Mapping. AJTMH 2015Sara Merino EgidoNo ratings yet
- Taguchi's Loss FunctionDocument12 pagesTaguchi's Loss FunctionEdmund F. AlvarezNo ratings yet
- Abordaje Deltopectoral Vs TransdeltoideoDocument10 pagesAbordaje Deltopectoral Vs TransdeltoideoNinhoTonyOfficialNo ratings yet
- A. What Proportion of Aircrafts Can Be Expected To Travel BetweenDocument7 pagesA. What Proportion of Aircrafts Can Be Expected To Travel Betweenmaen dnNo ratings yet
- Thesis Feb4Document57 pagesThesis Feb4Ralph CelesteNo ratings yet
- Technology Integrated Fdu Lesson Plan-Ne ColoniesDocument9 pagesTechnology Integrated Fdu Lesson Plan-Ne Coloniesapi-677159802No ratings yet
- SKKU HandbookDocument50 pagesSKKU HandbookHaNo ratings yet