Professional Documents
Culture Documents
Embriologi Skin
Uploaded by
AIDAN AsigraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Embriologi Skin
Uploaded by
AIDAN AsigraCopyright:
Available Formats
HEAD & NECK CME
ABBREVIATION KEY
AMPK ⫽ 5= adenosine
monophosphate-activated protein
kinase is an enzyme that plays a
role in cellular energy homeostasis
ATP ⫽ adenosine triphosphate
BAT ⫽ brown adipose tissue
BMP ⫽ bone morphogenetic protein
Embryology and Anatomy of the Skin, BMZ ⫽ basement membrane zone
cadherin ⫽ Cadherins are a class of
Its Appendages, and Physiologic type-1 transmembrane proteins
that play a role in cell adhesion
Changes in the Head and Neck CNS ⫽ central nervous system
dermo1 ⫽ dermal marker
Dsg ⫽ desmoglein a family of
P.M. Som, J.T. Laitman, and K. Mak cadherins that play a role in the
formation of desmosomes
ECM ⫽ extracellular matrix
FGF ⫽ fibroblast growth factor
IL ⫽ interleukin
CME Credit keratin ⫽ K a family of fibrous
The American Society of Neuroradiology (ASNR) is accredited by the Accreditation Council for Continuing Medical Education structural proteins that protects
(ACCME) to provide continuing medical education for physicians. The ASNR designates this enduring material for a maximum of one epithelial cells from damage or
AMA PRA Category one creditTM. Physicians should claim only the credit commensurate with the extent of their participation in the
stress
activity. To obtain credit for this activity, an online quiz must be successfully completed and submitted. ASNR members may access
this quiz at no charge by logging on to eCME at http://members.asnr.org. Nonmembers may pay a small fee to access the quiz and LTMR ⫽ low-threshold
obtain credit via http://members.asnr.org/ecme. mechanoreceptor
MC1R ⫽ melanocortin 1 receptor
melanocortin ⫽ melanocortins are a
group of peptide hormones, which
ABSTRACT include adrenocorticotropic
Although often overlooked as a significant factor in the head and neck, the skin plays an hormone and the different forms
of melanocyte-stimulating
important role in body thermoregulation as well as in detecting pain, pressure, and itch.
hormone they are derived from
Knowledge of the embryology of the skin allows a better understanding of the role that skin the pituitary gland
plays not only during gestation but also in everyday life and how skin changes with certain MITF ⫽ melanogenesis associated
nonpathologic circumstances. This review was illustrated to help the reader follow the text. transcription factor
MSH ⫽ melanocyte-stimulating
Learning Objective: The reader will learn about the development of the skin and the critical hormone
role that skin plays in both prenatal and postnatal life. MYF5 ⫽ myogenic factor 5
MYFS ⫽ myogenic regulatory factor
myogenic regulatory factors are
INTRODUCTION cles, and sebaceous glands but does have basic helix-loop-helix transcription
This review discussed the embryology of sweat glands. It varies in thickness from factors that regulate myogenesis
the integumentary system, which consists 400 to 1400 m (equivalent to 1.4 mm). It
of the skin and its appendages. The skin is is also known as glabrous skin (nonhairy
Received December 22, 2015;
the largest organ in the body, which aver- skin). The focus of this review was on thin accepted October 11, 2016.
ages 12%–15% of the total body weight, skin because it is the type of skin that cov- From the Departments of
and it plays a critical role in human life, ers the head and neck. Thin skin contains Radiology (P.M.S.), Otolaryngology
(P.M.S., J.T.L.), and Medical
acting as a protective barrier to separate hair follicles, arrector hair muscles, seba- Education (J.T.L., K.M.), the Ichan
the body from the environment.1 The skin ceous glands, and sweat glands, and it var- School of Medicine at Mount Sinai,
New York, New York.
is also impervious to water and most infec- ies in thickness from 75 to 150 m.2-4
Please address correspondence to
tions, and it plays an important role in reg- Peter M. Som, MD, Department
ulating body temperature and detecting THE EPIDERMIS of Radiology, The Mount Sinai
Hospital, One Gustave Levy Place,
pressure and pain. The skin is composed of The development of the ectoderm was dis- New York, NY 10029; e-mail:
2 layers: the epidermis, which is derived cussed in an earlier review in this series.5 Peter.Som@MSSM.edu
http://dx.doi.org/10.3174/ng.9170210
from the ectoderm, and the dermis, which, By 2–3 weeks, the ectoderm that covers the
in the head and neck, is derived from neu- surface of the embryo consists of a single Disclosures
Based on information received
ral crest mesenchyme. layer of cuboidal undifferentiated cells sep- from the authors, Neurographics
Based on the thickness of the epidermis, arated from the underlying mesenchyme by has determined that there are no
Financial Disclosures or Conflicts of
the skin is classified as being either thick or a basement membrane. Initially, as as- Interest to report.
thin. Thick skin covers the palms and soles, sessed on light microscopy, the basement
and lacks hair follicles, arrector hair mus- membrane was thought to be a thin band
390 兩 Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org
immediately beneath the basal layer) then develops under the periderm. This forms a
NOTCH ⫽ A transmembrane
ectoderm. However, with
receptor for Delta and Serrate,
continuous layer, usually only 1 cell deep. The cells of the
the use of the electron mi-
mediating cell–cell interactions periderm are continually undergoing desquamation due to
PAR2 ⫽ protease-activated croscope, it became clear apoptosis and are primarily replaced by cells that arise from
receptor 2 that this “membrane” was the basal layer, although there may be some replacement
protein kinase C ⫽ plays a crucial
actually a specialized struc- of the periderm from the peridermal cells themselves.9 With
role in signal transduction for a
variety of biologically active
ture, and early in its devel- the development of this bilaminar epidermis, the periderm
opment, it is composed of
substances that activate cellular and the basal layer become defined (Fig 1).2,4,10,11 Initially,
functions and proliferation collagen fibers and lamin- these epidermal cells are widely separated, being connected
SHH ⫽ sonic hedgehog, a protein, a
ins attached to the ectoder- only by interlocking villous processes and a few desmo-
ligand in the Hedgehog pathwaymal cells through binding somes. The cells in the basal layer are poorly stabilized, with
TYR ⫽ tyrosinase
UCP ⫽ uncoupling of protein
of both integrin and nonin- the cells being flattened and containing a band of cytoplas-
UCP1 ⫽ mitochondrial carrier tegrin cell membrane re- mic filaments adjacent to the BMZ. This may compensate
ceptors, with infrequent
proteins that catalyze a regulated for the limited support of the epidermis until the hemides-
proton leak across the inner desmosomes, which lack mosomes develop. The BMZ is also incomplete until the
mitochondrial membrane the typically associated fil-
UV ⫽ ultraviolet
mesenchymal cells of the dermis produce a connective tissue
UVA⫽ the longest wave length of
aments.6 However, by the matrix.12
UV 12th week, the basement In the 8th–11th weeks, proliferation of the basal layer
WAT ⫽ white adipose tissue membrane has nearly ma- produces a new intermediate layer, deep to the periderm.
WNT ⫽ Wingless/int1 family of tured, and, with the devel- This intermediate layer is the forerunner of the outer layers
secreted signaling opment of additional lay- of the mature epidermis. The basal layer, or stratum germi-
ers, it is often referred to as nativum, constitutes the layer of stem cells that will con-
the basement membrane tinue to replenish the epidermis throughout life. By the 10th
zone (BMZ). This is an important site for the mutual induc- week, the cells in the basal layer already have hemidesmo-
tions that occur between the BMZ and the future epidermis, somal and desmosomal proteins. Between the 12th and
both pre- and postnatally. The BMZ is also critical to the 16th weeks, the intermediate layer gradually thickens and
integrity and stability between the epidermis and the future eventually differentiates into typical stratified keratinizing
dermis because the BMZ is responsible for the binding of squamous epithelium. By 14 weeks, basal keratins are ex-
the epidermis to the dermis (Fig 1). pressed by the basal cells and the cells of the intermediate
In the fourth to sixth weeks, this ectoderm proliferates to layer contain keratin proteins and tonofilaments, which are
form a new outer layer of flattened simple squamous epi- characteristic of differentiated epidermis. These cells are
thelium, which is the primordium of the epidermis. This now known as keratinocytes (Fig 3).2-4,10,13
new layer is the periderm, and it represents the first stage in The BMZ has matured and now has hemidesmosomes,
epidermal formation. The periderm seems to act as a tem- which act as anchoring bridges between the keratin cyto-
porary protective membrane for the future underlying epi- skeleton of the early basal epidermal cells, or keratinocytes,
dermis, and it initially plays a role in water, sodium, and and the basement membrane. Within the cytoplasm of the
glucose exchange between the embryo and the surrounding keratocytes, tonofilaments cluster at the site of the hemides-
amniotic fluid. This fluid exchange occurs in both directions mosome and form a plaque that anchors the hemidesmo-
across the interface of the periderm and reaches a peak at some. These hemidesmosomes extend from the deepest ker-
12–16 weeks, after which the periderm undergoes a trans- atinocytes, down toward a layer that has developed in the
formation into a layer of flattened squamous cells with a upper BMZ, the lamina densa, which contains fibrillary
purely filamentous internal structure. The periderm is sug- structures known as anchoring filaments. From the lower
gested to play a major role in the production of the amniotic lamina densa, anchoring fibrils extend into the uppermost
fluid during the period of maximal development of the per- papillary layer of the developing underlying dermis, or the
iderm, and its associated regression corresponds with the fibrillar zone, where they associate with basement mem-
taking over of this function by the umbilical cord epithelium branelike structures known as anchoring plaques, which
(Fig 1).7 are in the papillary dermis. The lamina densa represents a
During the first trimester, each flattened periderm cell stable sheetlike meshwork primarily composed of collagen
develops a superficial bulge, which enlarges into a single IV.
elevated vesicle or bleb. In the second trimester, the single By the second month, there is a continuous lamina densa;
bleb becomes modified into multiple blebs that project from the hemidesmosomes appear in the third month. The BMZ
each cell. Near the end of the second trimester, all of these constitutes the anchorage zone for both the anchoring fila-
surface modifications regress and the periderm transforms ments that originate in the epidermis and the anchoring
into an ineffective cellular layer that is sloughed into the fibrils in the fibrillar zone of the dermis (Figs 1B and 4). The
amniotic fluid (Fig 2).8 A second layer, the basal or germi- lamina densa is thicker in men than in women, with an
native layer (stratum germinativum or the stratum basale or average thickness of 30 – 60 nm. The anchoring filaments
Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org 兩 391
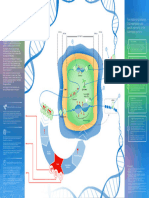
Fig 1. A, Serial drawings illustrate the basic development of the layers of the epidermis and the development of the dermis (modified with permission
from Carlson BM. Human Embryology and Developmental Biology. 4th ed. China: Mosby Elsevier; 2009:176 [Fig 9 –1]). B, The illustration shows the
components of the BMZ between the basal layer of the epidermis and the upper layer (papillary layer) of the dermis (modified from http://www.
cram.com/flashcards/mss-08-basement-membrane-zone-bmz-3433975, accessed in 2013).
Fig 2. A diagrammatic representation of the bleb formation on the peridermal cells from approximately 3 months to approximately 4 months of
gestation.
are composed of collagen types IV and VII. In thin skin, the roles of determining the polarity of the basal keratinocytes
type of skin that covers the head and neck, there is no and serving as a selective barrier that controls the molecular
lamina lucida. However, in thick skin, as found in the soles and cellular exchanges between the 2 compartments.14
and palmer regions, immediately under the epidermis and Keratin is an intermediate cytoskeleton filament protein
above the lamina densa is the lamina lucida. Within the of epithelial cells that is required for the mechanical stability
lamina lucida is the hemidesmosomes complex, with and integrity of the epidermis. Humans have 54 functional
threadlike anchoring filaments that extend down into the keratin genes, and the keratins are divided into 2 types: type
lamina densa. The role of the BMZ is not only to tightly I, the acid keratins (K9 –K28 in epithelial cells and K31–
bind the epidermis to the dermis, but it has the additional K40 in hair and nails); and type II, the basic keratins (K1–
392 兩 Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org
Fig 3. A drawing, illustrating the various levels of the epidermis and the location of some cellular and extracellular proteins that help stabilize the
epidermis (modified with permission from http://www.rci.rutgers.edu/⬃uzwiak/AnatPhys/APFallLect7.html, accessed in 2013).
K8, K71–K80 in epithelial cells and K81–K86 in hair and and an outer stratum corneum (horny or cornified layer).
nails). Keratins form heterodimers that assemble into het- This transformation starts at the cranial end of the fetus and
eropolymeric keratin filaments.15 proceeds caudally (Fig 3). In areas that have thick skin,
By the 15th–16th weeks, the greater part of the periderm which do not occur in the head and neck, there is an addi-
has been desquamated, in part, due to the eruption of the tional layer, the stratum lucidum, which is a thin, clear layer
hairs. Because the periderm remains, in part, with the epi- of dead cells immediately below the stratum corneum and
dermis after the growth of hairs, it was originally termed the above the stratum granulosum. Although the stratum spi-
epitrichium. To the layer of castoff peridermal cells are nosum is permeable to water, the overlying stratum granu-
added sebaceous secretions, and, as development continues, losum and stratum corneum are impermeable to water.
more ectodermal cells from the outermost layer of the skin. However, damage to the epidermis may render areas of
The stratum disjunctum refers to the surface cells that are the skin permeable, and this may constitute a medical emer-
partially detached from the outer skin layer. Together, they gency.18 As the basal keratinocytes extend upward and
form a whitish cheesy substance, the vernix caseosa, which reach the stratum granulosum, they release specialized epi-
often persists to full term, and covers most of the skin, dermal organelles or lamellar bodies that contain free fatty
especially in the hair, back, and the joint creases. The vernix acids, cholesterols, and ceramides. They bud off the Golgi
may have a function in protecting the underlying epidermis complex and at the transition from the granular layer to the
from maceration by the amniotic fluid and from the high cornified layer, the lamellar bodies fuse with the cell mem-
urine content in the amnion.3,10 When much of the vernix brane and extrude their contents into the extracellular space
remains on the neonate infant, these children are referred to as lamellar granules, which form an intercellular lipid sheet
as collodion babies. This vernix will either shed spontane- that seals off the intercellular space, especially in the stra-
ously or is easily removed.1-4,16,17 In summary, by the end tum corneum.19
of the first trimester, all of the epidermally derived primor- The periderm cells do not produce keratohyalin, which is
dia are present, and they will differentiate into definitive essential for keratin formation and is a signature of epider-
structures in the second and third trimesters. At this time, mal cells. However, as development proceeds, the earlier
the epidermis is 3 to 4 cell layers thick and relatively undif- cells to appear just deep to the future stratum corneum
ferentiated, except on the head, where hair follicles have contain less keratohyalin than those cells that are deeper
already begun to develop.12 and thus are developed later in the epidermis. This reflects
During the early fifth month, after the periderm is shed, the fact that the deeper cells are derived from more mature
the intermediate layer is replaced by the 3 definitive layers basal cells that contain larger amounts of keratohyalin, and
of keratinocytes: an inner stratum spinosum (spinous their more completely keratinized state indicates that kera-
layer), a middle stratum granulosum (granular layer, so tohyalin plays an essential role in the maturation of the
named because of the cellular granules of keratohyalin), epidermis (Fig 3).7
Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org 兩 393
Fig 4. A, A drawing, illustrating the various types of cell-to-cell junctions that occur in the epidermis (modified from http://higheredbcs.wiley.com/legacy/
college/tortora/0470565101/hearthis_ill/pap13e_ch04_illustr_audio_mp3_am/simulations/figures/cell_junctions.jpg, accessed 2013). B, The drawing il-
lustrates both the desmosomes and hemidesmosomes that stabilize the epidermis and the epidermal-dermis interface (modified from https://www.
studyblue.com/notes/note/n/02-epithelium-i/deck/7484110, open access).
Presumptive keratinocytes are constantly produced by The cells of the stratum germinativum are the only divid-
the stratum germinativum. These keratinocytes are the pre- ing cells of the normal epidermis. These cells contain a
dominant cell type in the epidermis, which represents number of keratin filaments specific to this layer, including
⬎90% of the cells.14 As they pass outward to the stratum K5 and K14. These cells are also connected by desmosomes
corneum, they differentiate and are finally sloughed from and adherens junctions that together result in a tight struc-
the surface of the skin. Specifically, keratohyalin granules ture resistant to water and infection (Fig 4). The desmo-
begin to appear in the cells of the stratum spinosum and are somes also help distribute forces evenly throughout the
prominent components of the stratum granulosum. These epidermis. As already noted, the cells of the stratum germi-
keratohyalin granules are composed of protein aggregates nativum are connected to the basement membrane by hemi-
rich in either histidine or sulfur, and they are closely asso- desmosomes. This attachment is essential for cell survival
ciated with bundles of keratin filaments. As the keratino- and determines the orientation of cell divisions. As the cells
cytes move into the stratum granulosum, their nuclei be- in the stratum germinativum move into the overlying 4 – 8-
come flattened with attenuated masses of chromatin. These cells-thick stratum spinosum, K5 and K14 are replaced by
are signs of apoptosis and terminal differentiation.2-4,10 K1 and K10. These keratins are cross-linked by disulphide
394 兩 Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org
bonds to provide further strength. As already noted, lipid- they receive nutrients, they start to die and form the stratum
containing granules (lamellar granules) are also produced in corneum, a tough and relatively impermeable layer of hard-
cells in the stratum spinosum. As the cells ascend into the ened, dead cells. Eventually, as the cells are sloughed off,
stratum granulosum and eventually the stratum corneum, they are replaced within approximately 2 weeks.
the lipid is extruded and helps seal the skin.2-4,10
This progression, from a single-layered ectoderm to a Intercellular Junction
stratified epithelium, requires the activation of the tran- There are several types of cellular junctions that link kera-
scription factor p63, possibly in response to signals from the tinocytes together and which are responsible for the me-
underlying dermal mesenchyme. Subsequently, p63 tran- chanical, biochemical, and signaling interactions between
scription must be turned off for cells within the stratified these cells. These junctions include desmosomes, hemides-
epidermis to embark on their terminal differentiation pro- mosomes, adherens junctions, gap junctions, and tight junc-
gram, which involves leaving the cell cycle.2-4,10 Once the tions. Desmosome can be thought of as “rivets” through the
cells are in the stratum granulosum, in addition to the la- plasma membrane of adjacent cells. Intermediate filaments
mellar granules, these cells produce envelope proteins, such of keratin attached to membrane-associated proteins within
as involucrin, loricrin, and envoplakin, which line the inner the cytoplasm of a cell form an attenuated plaque on the
surface of the plasma membrane, and the enzyme transglu- inner plasma cell membrane. Cadherin molecules form the
taminase, which cross-links these envelope proteins. At actual anchor by attaching to the cytoplasmic plaque in 1
week 15, this layer also produces the histidine-rich protein cell and then extending through the cell membrane to
filaggrin, which is derived from one of the granular compo- strongly bind to cadherins that extend from an adjacent cell.
nents of keratohyalin. Within the stratum granulosum, the This strong adhesive state distinguishes the desmosomes
cells contain profilaggrin as inactive granules. Through a from other intercellular junctions. These junctions are also
multistep process, filaggrin is formed and creates aggregates dynamic structures whose adhesiveness can alternate be-
with the keratin filaments to form tight bundles that inter- tween high and low affinity states during processes such as
connect the cells in this layer. Together with other lipids and embryonic development and wound healing. This switching
cornified proteins, filaggrin forms the “skin barrier.” The between adhesive states is controlled by signaling of protein
cells of the stratum corneum, depending on the region of the kinase C. Desmosomes may also act as signaling centers,
body, accumulate from 15–20 layers of dead cells, which, as regulating the availability of signaling molecules and
noted, are eventually shed. This shedding, or desquamating thereby participating in fundamental processes such as cell
process, involves degradation of the lamellated lipid in the proliferation, differentiation, and morphogenesis (Fig 4).14
intercellular spaces and loss of the residual intercellular des- Hemidesmosomes have a strong electron microscopic re-
mosomal interconnections.14 semblance to one-half of a desmosome and thus the name.
The final process in cornification occurs when lytic en- However, they are quite distinct. Although, as with desmo-
zymes are released within the cells, which results in the some, they attach to intermediate filaments within the cell
ceasing of metabolic activity and enucleation, with the re- cytoplasm, their transmembrane anchors are integrins
sulting loss of all cell contents. When the keratinocytes fi- rather than cadherins. Within the cytoplasm of a keratino-
nally enter the stratum corneum, they are flattened, densely cyte, there is a plaque to which the cell’s tonofilaments
packed, terminally differentiated keratinocytes or squames. converge. On the outside of the cell is a second plaque, the
It is a calcium gradient that promotes keratinocyte differ- subbasal plaque, and the plasma membrane is sandwiched
entiation, with the lowest concentration of calcium in the between these plaques. Integrins are transmembrane gly-
stratum basale and the highest concentration in the stratum coproteins that are a major component of the hemides-
granulosum. The stratum corneum has a very low or non- mosome, which mediate the transfer of information be-
existent calcium concentration because these cells are dry tween the extracellular matrix and the cell’s interior.
and unable to dissolve the calcium ions. Vitamin D3 also These hemidesmosomes thus aid in modulating the orga-
regulates keratinocyte proliferation and differentiation by nization of the cytoskeleton, its proliferation, and its
modulating the calcium concentrations and by regulating differentiation (Fig 4).
the expression of the genes involved in keratinocyte differ- Adherens junctions are similar to desmosomes in that
entiation. The keratinocyte is the only cell in the body that they are anchored to cytoplasmic actin filaments. However,
contains the entire vitamin D metabolic pathway from vi- their transmembrane anchors are E-cadherins, and the for-
tamin D synthesis to catabolism and receptor expression.4 mation of the mature junction requires a reorganization of
In summary, the formation of new keratinocytes in the the cell’s actin cytoskeleton. The cytoskeleton actin fila-
basal layer gradually pushes the previously formed cells ments that tie to the adherens junctions are contractile pro-
upward through the stratum spinosum. As the cells ap- teins, and, in addition to providing anchoring, these junc-
proach the stratum granulosum, they accumulate intracel- tions are believed to participate in folding and bending of
lular keratin and they secrete a waxy lipid that contains epithelial sheets (Fig 4). Tight junctions regulate the para-
material into the intercellular space. As the maturing kera- cellular pathway for the movement of ions and solutes in
tinocytes seal off the intercellular spaces through which between cells. Tight junctions consist of the transmembrane
Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org 兩 395
Fig 5. A, A drawing, illustrating the extensions of a melanocyte into the epidermis (modified from Le Physique, Personal Training. http://www.
lephysique.com/sunburnt-again. Open access). B, The drawing shows the positions of a Langerhans cell, a melanocyte, a Merkel cell, and a Meissner
corpuscle within the layers of the epidermis (modified from https://www.studyblue.com/notes/note/n/02-epithelium-i/deck/7484110, accessed
2013).
proteins occludin and claudin as well as cytoplasmic scaf- prabasal keratinocytes via elongated dendrites and cell-to-
folding proteins (Fig 4).20 Gap junctions are clusters of cell contact (Fig 5). As the keratinocytes migrate to the
intercellular channels that allow direct diffusion of ions and surface, they carry with them the ingested melanin to form
small molecules between adjacent cells. The intercellular a critical barrier against the environment. It is not only the
channels are formed by head-to-head docking of hexam- melanin within the basal melanocytes but also the melanin
eric assemblies called connexons (Fig 4). The close mem- within the keratinocytes in the more superficial layers that
brane apposition required to allow the docking between gives the skin its characteristic color.22
connexons sterically excludes most other membrane pro- Recognizable pigment does not occur until 4 –5 months,
teins, which leaves only approximately a 2-nm extracel- and the production of melanin begins earlier and is more
lular “gap,” for which the junction is named. The gap extensive in individuals with darker pigmentation than it is
junctions allow various molecules, ions, and electrical in people with lighter skin. In lightly pigmented skin, the
impulses to pass directly through a regulated gate be- melanosomes are small, aggregated in membrane-bound
tween cells (Fig 4).21 clusters. In darker pigmented skin, there is increased
melanization, decreased melanosome degradation, and
Melanocytes larger melanosomes singly distributed, and there are larger
In addition to cells that originate from the ectoderm, the and more dendritic melanocytes. There, however, are no
epidermis also contains cells that are derived from the neu- differences in the number of melanocytes between different
ral crest and mesoderm. In the early second month, neural races; the differences are in the size, distribution, and num-
crest– derived melanoblasts migrate into the mesenchyme of ber of melanosomes. The synthesis of melanin, which oc-
the embryonic dermis. As their migration reaches the der- curs in the melanosomes, is stimulated by melanocyte-stim-
moepidermal junction, these cells differentiate into melano- ulating hormone (MSH). The melanin produced can be
cytes. Under the regulation of Wingless/int1 family of se- either pheomelanin (creating a red-to-yellow color) or eu-
creted signaling (WNT), the process of differentiation from melanin (occurring as either brown or black in color).
melanoblasts into melanocytes proceeds, and this involves During fetal life, melanocytes are also present in the un-
the transition of premelanosomes (nonpigmented mem- derlying dermis. However, most of these cells are likely in
brane-bound vesicles) to melanosomes (intracellular organ- the process of migrating to the epidermis, a migration that
elles that are the site of synthesis, storage, and transport of may only take a few days. It is between 40 and 50 days that
melanin) and, finally, the production of pigment granules. the melanocytes finally enter the epidermis. In the 10th
The epidermal melanocytes occur in an approximately 1:10 week, a number of these melanocytes become associated
ratio with the basal keratinocytes, and each melanocyte with the developing hair follicles, where they donate pig-
distributes melanin to approximately 40 overlying su- ment to the follicles. The melanocytes also provide the
396 兩 Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org
deeper skin layers with protection from solar radiation. tion, epidermal-mesenchymal (dermal) interactions are nec-
Overall, melanocytes represent 5%–10% of the cells in the essary for the development of the dermal papillae and their
epidermis in the adult.2-4,10 relationship to the hair follicles and the dermal ridges.12
The dermis, or corium, contains blood vessels, hair follicles,
Langerhans Cells nerve endings, and sensory receptors. There is very little
Although the skin was initially thought to be a passive bar- vascularization of the dermis before 10 weeks. The dermis
rier between the body and the environment, it is now clear and the hypodermis (subcutis) in the head and neck origi-
that the skin has a highly sophisticated system of immune nate from neural crest cells.25 In the second month, under
surveillance. Key to this system are the Langerhans cells, the influence of ectodermal WNT signaling, neural crest–
which are a specialized subset of dendritic antigen-present- derived mesenchymal cells closest to the ectoderm are
ing immune cells that populate the skin. They are derived specified to become dermal cells, which express the der-
from the bone marrow monocyte–macrophage– histiocyte mal marker dermo1. The embryonic dermis is very cellu-
lineage and are present in the epidermis at approximately lar, and, by the second month, the dermis and subcutis
12 weeks. They are present in all of the layers of the skin, are indistinguishable.
most numerous in the stratum spinosum. They also are Early in the third month, the developing dermis under-
present in the papillary dermis, especially about the blood goes a transition from its initial highly cellular embryonic
vessels. These cells are the immune macrophage cells of the composition to one that has mesenchymal cells differenti-
skin, and they function in immune surveillance as well as in ated into fibroblasts with the production of increasing
contact sensitivities. The Langerhans cells are present in low amounts of a fibrous intercellular matrix. This matrix is
numbers in the first 2 trimesters but then increase several primarily composed of type I and III collagen fibers and
fold to comprise 2%– 6% of the total number of epidermal elastic fibers. When compared with the adult extracellular
cells in the adult epidermis. They will continue to migrate matrix (ECM), the fetal ECM principally has collagen type
into the epidermis throughout life (Fig 5B).23 In addition, I and a higher ratio of collagen type III than in the adult
mast cells are located in the subpapillary dermis, mainly ECM. The fetal ECM also has higher levels of glycosami-
around blood vessels, nerves, and appendages, and they can noglycans, hyaluronic acids, and chondroitin sulfates than
migrate through the basal lamina into the epidermis. They in the adult ECM.26 The progressive differentiation of the
play a role in innate and adaptive immunity, and are asso- dermis also includes the organization and maturation of
ciated with atopic dermatitis, celiac disease, scleroderma, nerves and the vascular plexuses. At about the time that the
and immune-bullous disorders. epidermis is forming the intermediate layer, the morpho-
genesis of the skin appendages commences.9
Merkel Cells The predominant connective tissue component of the
The Merkel cells are generally believed to arise from neural dermis is collagen. The texture of the collagen distinguishes
crest cells and appear between 4 and 6 months.2,4 They are 2 layers of the dermis. The papillary layer lies adjacent to
slow-reacting pressure-detecting mechanoreceptors that lie the epidermis and consists of relatively small, finely tex-
at the basal layer of the epidermis and are associated with a tured collagen fibers. This is the dermal layer, which forms
single underlying nerve ending from the dermis. Cytoplas- the dermal papillae that protrude up into the epidermis. The
mic protrusions of the Merkel cell and hemidesmosomes reticular layer of the dermis lies beneath the papillary layer
physically link the Merkel cells to the surrounding keratin- and consists of larger, more coarsely textured collagen fi-
ocytes. These are the only “immigrant” cells that form des- bers. The connective tissue of the dermis then grades into
mosomes with the adjacent basal layer keratinocytes and the hypodermis (subcutaneous tissues) without a sharp or
hemidesmosomes with the BMZ. In the prevalent theory of distinct boundary (Figs 1A, 3, and 6).
the neural crest origin of the Merkel cells, it is thought that By the fifth month, the papillary and reticular layers be-
they arise in the dermis and then “travel” into the epider- come distinct, and soon the connective tissue sheaths are
mis. However, an alternate theory of their origin has been formed around the hair follicles. At 22 weeks, elastic fibers
proposed in which the Merkel cell is derived from epidermal are present. Thus, this future dermis is initially a loose ag-
cells, which then migrate into the upper dermis. Support for gregate of mesenchymal cells that are highly interconnected
this etiology comes from the observation that Merkel cells by focal tight junctions on their cellular processes. These
are not present in the dermis before week 12 and that their early dermal precursors secrete a watery intercellular ma-
epithelial nature is demonstrated by the presence of desmo- trix that is rich in water, glycogen, ions, fibronectin, elastin,
somes and desmosomal proteins (eg, cytokeratin), whereas and hyaluronic acid.2-4 This embryonic dermis is richer in
neural markers, neurofilaments, and glial filaments are not cells than the adult dermis, with many of the mesenchymal
present.24 cells being involved in essential signaling, which regulates
the ectodermal differentiation. On average, the dermis is
THE DERMIS only 1- to 2-mm thick. In the eyelids, it is only 0.5-mm
Without the presence of the dermis, the epidermis does not thick, whereas it is thicker (several millimeters) in the
divide, differentiate, or maintain its orientation. In addi- back.7,10,14
Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org 兩 397
Fig 6. A drawing of an oblique section of skin, which illustrates the various layers of the epidermis and dermis; note the dermal papillae that cause the
dermal ridges (modified with permission from Shier DN, Bulter JL, Lewis R, eds. Hole’s Human Anatomy and Physiology. 8th ed. Albany, NY: Skin and
the Integumentary System. McGraw-Hill; 1999 [Fig 6.3]).
The dermis is fully differentiated by the second and third with an early capillary network transformed into layers
trimesters. It is thin at birth and thickens progressively of larger vessels.2 Between 7 and 10 weeks, a second
through infancy and childhood. The papillary layer is richly deeper horizontal plexus develops and both plexuses ex-
supplied by capillaries, whereas larger vessels are found in tend by budding to attain their final prenatal pattern of
the reticular layer. As noted, deep to the dermis is the sub- arterioles, venules, and capillaries (Fig 7). Pericytes then
cutaneous fatty connective tissue or the hypodermis (sub- appear, arising from mesenchymal cells. The adult mor-
corium). Between the third and fifth months, the papillary phology is reached after birth.
layer of the developing dermis proliferates to form upward The dermal blood vessels branch and then follow nerves
protruding ridgelike dermal papillae that extend into the within the dermis to become associated with hair follicles. It
overlying epidermis. Between these dermal protrusions, the has been estimated that neonatal skin contains 20 times
overlying epidermis extends downward, and this process more blood vessels than it needs to support its own metab-
results in the creation of surface epidermal ridges and olism. This excess is believed to be required for thermoreg-
grooves. The patterns of these skin ridges and grooves pro- ulation. It is during the first few weeks of postnatal life that
duced by the dermal papillae varies from one area of the most of the definitive vasculature of the skin develops.4 The
body to another. Thus, in palmer and plantar surfaces of the eventual blood supply to the skin has 3 sources. There is the
hands and feet, the pattern is one of whorls and loops. In
direct cutaneous system, the musculocutaneous system, and
the eyelids, there is a diamond-shaped pattern, whereas, on
the fasciocutaneous system. In the direct cutaneous system,
the upper surface of the trunk, the ridges resemble cobwebs.
the vessels are derived from the main arterial and venous
During the 10th–12th weeks, the first skin ridges to appear
vessels that course in the subcutaneous fat and parallel the
are the whorls on the palmar and plantar surfaces of the
skin surface.
digits. By the early fifth month, the entire system of surface
ridge patterns is established, and the epidermal ridges are In the musculocutaneous system, perforating vessels
permanently established by 17 weeks.2-4 arise from the intramuscular vasculature and pass from the
muscle to pierce the deep fascia and then reach the skin by
BLOOD SUPPLY spreading out in the subcutaneous tissues. In the fasciocu-
In the fourth week, dermal blood vessels that originate taneous system, perforating branches from deeply located
from the mesenchyme start as simple endothelial-lined vessels below the fascia pass along intermuscular septa and
structures. By the fifth week, via angiogenesis, new cap- then fan out at the level of the deep fascia to finally reach the
illaries develop from the primordial vessels.3 That is, the skin (Fig 7A). It was the knowledge that the main blood
dermal vasculature is generally thought to develop in situ supply of the skin comes from the perforating vessels from
by transformation of angiogenic mesenchymal cells. By 6 the underlying muscles and fascia that heralded the use of
weeks, underneath the ectoderm, the closed endothelial the myocutaneous flaps that are so often used in surgical
channels contain nucleated red blood cells. By 8 weeks, reconstructions.11 In the deeper layers of the dermis, arte-
the primitive vessels are arranged in a single plane paral- riovenous anastomoses are common and are under auto-
lel to the epidermis. They ultimately form a subpapillary nomic vasomotor control. When these vascular shunts are
plexus. The dermis then becomes highly vascularized, relaxed, blood is diverted away from the superficial plexus
398 兩 Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org
Fig 7. A, A drawing of the layers of the vascularity within the skin. B, The drawing illustrates the papillary and reticular vascular plexuses and their
interconnecting vessels (modified with permission from https://www.carecreations.basf.com/news-media/photos-and-illustrations/photosand
illustrations-detail/2006/1/14/the-skin-s-blood-vessel-system, accessed 2013). Credit www.skin-care forum.basf.com.
Fig 8. A, A drawing, illustrating the lymphatics of the skin. B, The close layered relationship of the lymphatic and blood vessels in the skin is shown; red
indicates the arteries, blue are veins, and yellow are the lymphatics (modified with permission from Ref 27, Fig 1).
of vessels, which reduces heat loss and at the same time develop around the primary area. This phenomenon is ex-
ensures deep cutaneous circulation to the nerves. plained by the long reach of the collecting lymphatic
vessels.27,28
The Lymphatics
With specific reference to the lymphatics of the skin, the HYPODERMIS
lymphatics start with closed endothelial lymphatic capillar- The hypodermis, or subcutis, lies immediately below the
ies in the papillary layer of the dermis. They are formed by skin and, depending on the location in the body, may be
mesenchymal cells, which become organized to enclose primarily adipose or fibrous. Over most of the body,
pools of proteinaceous fluid that has leaked from the devel- the hypodermis is characterized by a thick layer of adi-
oping capillaries. These pools drain into a superficial plexus pose tissue. However, at the sites of “dimples,” the hy-
just deep to the subpapillary dermal venous plexus. The podermis is fibrous and binds the dermis to the underly-
lymph then drains via vertically oriented branches into a ing structures. In general, the transition from dermis to
series of larger lymphatic vessels, which form the deeper hypodermis is irregular and poorly defined. Adipocytes
plexus at the level of the reticular layer and the subcutis. or “fat cells” comprise approximately one-third of adi-
From this deeper plexus of lymphatic vessels, the collecting pose tissue, with the remaining portions being composed
vessels may extend over considerable distances before of small blood vessels, nerves, fibroblasts, and adipocyte
draining into the deeper lymphatic channels (Fig 8). When precursor cells or preadipocytes. The adipocytes exist in
there is extension of a cancer to the skin or there is a dermal 2 cytotypes, white and brown. White adipose tissue
metastasis, after the metastasis has been surgically re- (WAT) is colored white or yellow and contains predom-
moved, soon, numerous additional dermal metastases often inately white adipocytes. Brown adipose tissue (BAT)
Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org 兩 399
appears brown and contains predominantly brown adi- monal control. The adipocytes also function by secreting
pocytes, which have a high content of metabolically ac- factors known to play roles in immunologic responses,
tive large mitochondria. Both BAT and WAT have vas- vascular diseases, and appetite regulation. In fact, leptin,
cular and nerve supplies.29 the obese gene product, is a hormone that is primarily
made and secreted by mature adipocytes, and binds to its
WAT receptor in the hypothalamus. Leptin may function in
Several studies on multipotent clonal cell lines have indi- regulating body mass. Taken together, the white adi-
cated that the adipocyte lineage derives from an embry- pocyte behaves not only in regulating energy balance but
onic stem cell precursor with the capacity to differentiate also has the potential to play a dynamic role in a variety
into the mesodermal cell types of adipocytes, chondro- of other physiologic processes.30 During the final phase
cytes, osteoblasts, and myocytes.30 Before week 14, the of differentiation, adipocytes markedly increase their li-
tissue that will become fat consists of a loose connective pogenesis and acquire sensitivity to insulin.30
tissue composed of an amorphous ground substance and
fibers. Adipogenesis is first recognized by the aggregation BAT
of an attenuated mass of mesenchymal cells. This mesen- The development of BAT begins in week 20 and contin-
chymal condensation marks the end of an undifferenti- ues until shortly after birth.31,32 Unlike the white adi-
ated stage in adipocyte development, and it is associated pocyte, the brown adipocyte has a thermogenic potential
with the proliferation of primitive blood vessels. During that is the result of the uncoupling of protein (UCP) 1,
this stage, from each small vessel, a rich capillary net- which “uncouples” adenosine triphosphate (ATP) syn-
work develops, around which mesenchymal cells differ- thesis from energy substrate oxidation. That is, brown
entiate into stellate preadipocytes. These mesenchymal adipose tissue has been shown to be a major source of
lobules, which do not contain lipid droplets at this stage, nonshivering heat production, especially as seen in neo-
are organized within a vascular structure or glomerulus, nate babies.33 The brown fat cells in classic BAT share
and will ultimately form the definitive fat lobule. The their origin with myogenic factor 5 (MYF5) expressing
future development of early fat cells within the mesen- myoblasts. The development of these progenitor cells
chymal lobules coincides with further development of the into a brown adipocyte lineage apparently is triggered by
vascular network. Within the mesenchymal lobular prea- bone morphogenetic protein 7, which stimulates inducers
dipocytes, fine fat vacuoles form in the cytoplasm and of brown fat cell differentiation. The control of brown fat
soon increase in number. At this time, the primitive fat cell development and activity is under the supervision of
lobule includes the vascular glomerulus and densely the sympathetic nervous system, which densely inner-
packed vacuolated fat cells adjacent to small vessels. In vates the BAT. The sympathetic system mediation of
the final stage of adipogenesis, definitive fat lobules are thermogenesis is primarily governed by hypothalamic
surrounded by perilobular mesenchyme, which rapidly and brain stem neurons. In addition, the leptin–melano-
condenses and progressively thickens to form interlobu- cortin pathway seems to be a major factor in controlling
lar septae. brown adipocyte thermogenesis. The involvement of this
It is between the 14th and 16th weeks that fat tissue homeostatic pathway further supports the role of the
differentiates, and fat lobules are the earliest structures to be brown adipocyte in energy balance regulation. Brown fat
identified before typical vacuolated fat cells appear. After is present in the neck and shoulder, and in the floor of the
the 23rd week, the total number of fat lobules remains mouth, especially in young, lean female subjects.34
relatively constant. From the 23rd to the 29th week, the As with the unilocular white adipocytes in WAT, the
growth of adipose tissue is mainly determined by an in- multilocular brown adipocytes in BAT also accumulate and
crease in the size of the lobules. Thus weeks 14 –23 are the store lipids. However, the brown adipocytes are distinct in
most-sensitive period for fat lobule development.29 The fat that their more abundant mitochondria are enriched with
lobules become more densely packed and become more ir- UCP1, which, as noted, uncouples substrate oxidation from
regular in shape as the fetus gets older. It is after week 14 ATP production so that heat can be produced. Although
that the first adipose tissue in the face occurs in the cheek WAT is far more common than BAT in terms of percentage
(the future buccal fat pad). The development of this adipose of body mass, when activated, BAT is an important con-
tissue then progresses from the deep subcutaneous region tributor to nutrient partitioning and utilization as well as
toward the more superficial dermis. Later, adipose tissue body weight regulation. UCP1 expressing thermogenic
appears in the limbs and the retroperitoneal region. The adipocytes can also be found in WAT in the form of beige
expansion of WAT takes place rapidly after birth as a result adipocytes. Under conditions of chronic cold exposure,
of both increased fat cell size and an increase in fat cell these beige adipocytes can be recruited in the WAT,
numbers. which results in the “browning” of WAT.35 With partic-
The mature adipocytes, which are the main compo- ular attention to the origins of these adipocytes, the cur-
nent of WAT, are uniquely equipped to function in en- rent understanding is that WAT adipocyte precursors can
ergy storage and balance, and they are under tight hor- be derived from either MYF5⫹ or MYF5⫺ lineages,
400 兩 Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org
whereas BAT adipocyte precursors are derived exclu- these arrector muscles contract, they aid in squeezing the
sively from a MYF5⫹ lineage. The beige adipocytes sebum from the gland follicle. The bulb can be divided into
can be derived from WAT adipocyte precursors and po- 2 distinct portions, above and below a line drawn through
tentially directly from mature white adipocytes. Brown the widest part of the bulb (critical level of Auber). The cell
adipocytes can also be generated from stem-cell–like matrix below the line remains undifferentiated, with a high
skeletal muscle satellite cells, and both brown and white cellular turnover rate, whereas the cells above the line retain
adipocytes may derive from endothelial precursors some mitotic activity but differentiate to give rise to the hair
(Fig 9).35 shaft and the inner root sheath.38
By the middle of the second trimester, it is the epidermal
SKIN DERIVATIVES cells lining the developing follicular canal that constitute the
In the head and neck, the skin has specialized structures that inner epidermal root sheath, while the surrounding mesen-
include sebaceous glands; hair and sweat glands, and tem- chymal cells differentiate into the dermal outer root sheath.
perature, pressure, and pain receptors.4 The glandular Proliferation of the germinal matrix produces cells that then
structures all arise as a result of epithelial–mesenchymal undergo keratinization and are added to the base of the hair
interactions that are secondary to inductive stimuli from the shaft. The growing hair shaft thus is pushed outward
dermis and which cause the development of an ectodermal through the follicular canal. The hair shaft becomes kera-
placode. After this, there is condensation of the underlying tinized, with the process of keratinization forming granules
mesenchyme and then invagination of the epithelium into of trichohyalin, a protein that imparts hardness to the hair.
the underlying dermis.4 The hair shaft thus is a column of dead keratinized cells that
are gradually extruded from the hair follicle. The elonga-
Hair tion of the presumptive hair follicle into the mesenchyme
The earliest development of the hair rudiments occurs be- takes an oblique direction, and this seems to be directed by
tween 9 and 12 weeks in the regions of the eyebrow, upper the cluster of mesenchymal cells, which accumulate beneath
lip, and chin.36 This occurrence represents the initial re- it. If the hair is to be colored, then the maturing keratino-
sponse to the first of 3 discrete mesenchymal– epithelial ex- cytes incorporate pigment produced by the melanocytes of
changes that orchestrate hair follicle formation.37 The first the hair bulb.4 The different mesenchymal– epithelial cues
sign of a hair follicle is a crowding of nuclei in the basal involve several signaling pathways, including NOTCH,
layer or stratum germinativum of the epidermis. This is sonic hedgehog (SHH), and WNT as well as contributions
referred to as the primitive hair germ or pregerm stage (Fig from fibroblast growth factors (FGF) and bone morpho-
10), which occurs in response to signaling from the subja- genetic proteins (BMP). There also are marked changes in
cent mesenchyme. The hair pregerm is also believed to in- certain cell adhesion proteins, notably E-cadherin and
duce the aggregation of dermal cells that form a dermal P-cadherin.14
condensate under it and that promotes further differentia- The primary hair germs appear randomly at rather reg-
tion of the hair germ. The pregerm then rapidly passes into ular distances from each other and develop in a scattered
the hair germ stage as the basal cells become high and their manner on the surface of the body. As the fetus grows, the
nuclei become elongated. These hair germ cells then prolif- distance between the first hair germs enlarges, and when a
erate and grow downward into the dermis. critical distance between the original hair germs is reached,
At the same time, in response to a second series of signals new primary hair germs appear. Later, secondary hair
from the enlarging epithelial cells, the mesenchymal cells germs develop and form hair groups, usually arranged in
and fibroblasts near the base of the hair germ increase in groups of 3, in short lines perpendicular to the slant of the
number to form the rudiment of the hair papilla beneath the hair follicle. The melanocytes associated with the hair bulb
hair germ. This stage, which occurs in the fifth month of develop from melanoblasts that migrate into the hair bulbs
development, is known as the hair peg. As the hair peg and then differentiate into melanocytes. The melanin pro-
develops further, it grows obliquely downward, and the duced by these cells is transferred to the hair-forming cells
advancing lower portion becomes bulbous and concave in the germinal matrix several weeks before birth, and the
downward, and gradually envelops the mesodermal pa- relative amount of melanin transferred accounts for the
pilla. The bulbous region is known as the hair bulb, and the different hair colors.14,38
epithelial cells of the hair bulb from the overlying prolifer- The arrector muscles of hairs are small collections of
ating ectoderm will constitute the germinal matrix that will smooth-muscle fibers that differentiate from the mesen-
later produce the hair shaft. Proliferation and differentia- chyme surrounding the hair follicles in the papillary layer of
tion are then enhanced by a third series of signals emanating the dermis. Contractions of the arrector muscle lifts the hair
from the dermal papillae. It is at this bulbous hair-peg stage, shaft to a nearly vertical position while depressing the skin
that 2 epithelial swellings appear on the posterior wall of over its attachments. This results in small pockets of de-
the follicle. The lower one is the bulge to which the arrector pressed skin with normal intervening skin, and this creates
pili muscle will attach, and the upper one is the rudiment of the tiny “goose bumps” on the surface of the skin, especially
the associated sebaceous gland (Fig 10).2,14,25,38 When noted when the skin is exposed to cold. The hairs that
Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org 兩 401
Fig 9. A, A diagram of the lineages of white, brown, and beige adipocytes, and a representation of the development of the adipocyte (modified with
permission from Ref 35, Fig 1). B, The diagram illustrates the different responses of WAT and BAT to cold stimulation (modified with permission from
Harms M, Seale, P. Brown and beige fat: development, function and therapeutic potential. Nat Med 2013;10:1252– 63 [Fig 2]).
develop in the face have poorly developed arrector pili mus- the follicular epithelium that periodically regenerate the fol-
cles, and the hairs that form the eyebrows and the cilia of licle during postnatal life are located near the attachments
the eyelashes have no arrector muscles.3 The stem cells of of the arrector pili muscles.
402 兩 Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org
Fig 10. A, The serial drawing illustrates the development of the hair follicle and its associated sebaceous gland (modified with permission from Carlson
BM. Human Embryology and Developmental Biology. 4th ed. China: Mosby Elsevier; 2009:182 [Fig 9 – 8]). B, Drawings illustrate the anatomy of the hair
follicle as seen in a frontal view and in cross-section of the hair root (modified from https://image.slidesharecdn.com/biol121-chp5-pp-fall10-
101011140901-phpapp01/95/biol-121-chp-5-the-integumentary-system-64-638.jpg?cbⴝ1408031385, accessed 2013). C, The drawing illustrates the
various normal phases of hair cell replacement as noted in the text (modified from http://www.clevelandclinicmeded.com/medicalpubs/disease
management/dermatology/hair-disorders/, accessed 2013).
Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org 兩 403
By 15–17 weeks, the hair canal is fully patent within the At this time, the hair-associated melanocytes also stop
dermis and the epidermis, but it neither pierces the epider- growing. Toward the end of the catagen stage, the dermal
mal surface nor contains hair. The first hairs appear on the papilla condenses and moves upward to come to rest under-
brow and forehead at 16 –17 weeks and cover the entire neath the hair follicle bulb. If the dermal papilla fails to
scalp by 18 weeks.12 Hair follicles do not appear in the reach the bulb, then the follicle stops cycling and the hair is
remaining body until the fourth month. By the fifth month, lost. The hair shaft then fully detaches from the germinal
most, if not all, hair follicles are present. Overall, it is esti- matrix. The catagen phase usually lasts approximately 1–2
mated that approximately 5 million hair follicles develop in weeks. In the next phase, or telogen phase, the dermal pa-
both males and females, with the differences in distribution pilla separates from the follicle and the hair goes into a
and the various kinds of hair found in boys and girls at resting phase, which last 5– 6 weeks. In the last or exogen
puberty, which results from differing concentrations of cir- phase, the hair follicle falls out and a new hair root begins
culating sex steroid hormones.4 Thus, in males, the finer making a new hair as the anagen phase starts anew. Be-
body hair is replaced by coarser hair in the axilla and pubic tween the telogen phase and the exogen phase, the club hair
region as well as on the face and back.4 There are different may wedge itself into the follicle until it gets brushed or
types of hair, ranging from the coarse hairs of the eyelashes washed out. Alternately, the club hair remains in the follicle
and eyebrows, the axillae, and the pubis to the barely visible until the follicle restarts the growth cycle (anagen phase)
and the new hair shaft pushes the club hair out (Fig
hairs on the abdomen and back.
10C).4,39 At any one time, 90%–95% of the scalp hairs are
The first generation of hairs formed are fine-downy, soft,
in the anagen phase, ⬍1% are in the catagen phase, and
and lightly pigmented or unpigmented. They are collec-
5%–10% are in the telogen phase. In the exogen phase,
tively called lanugo. The lanugo hairs are closely spaced and
normally, 50 –100 hairs fall out per day.
may be first noted by the end of the 12th week. They are
plentiful by 17–20 weeks. These lanugo hairs help to hold
GLANDS
the vernix caseosa on the skin. During the perinatal period,
the lanugo is replaced by either vellus hair or terminal hair.2 Several types of glands are produced by the downward
Vellus hair is soft and short, usually ⬍2 mm long. It is the growth of the epidermis. Three types of glands are the fol-
lowing: the sebaceous glands, the apocrine glands, and the
general surface hair and is usually colorless. Terminal hair is
sweat glands are widely spread over the body. Of these,
large and coarse, with a medulla and pigment. It is of vary-
only the sweat and sebaceous glands occur in the head and
ing length and is found at birth in the scalp, eyebrows, and
neck.
eyelashes. During life, the same hair follicle can produce
first vellus hair and then terminal hair. This is most event in
Sebaceous Glands
the axillary hair of both male and female children and
in the beard of males as they attain puberty. In male bald- The sebaceous glands first appear as hemispherical protu-
ness, the terminal follicles regress and give origin to vellus berances on the posterior surface of the hair peg. The cells
contain moderate amounts of glycogen, but the cells in the
hair.38 The normal cycle of hair growth has been character-
center lose this and become larger and foamy as they accu-
ized into 4 stages. The first stage refers to the growth of the
mulate droplets of lipid. Between 13 and 15 weeks, the
hair and is referred to as the anagen phase. The next stage is
sebaceous glands become differentiated. The gland bud
the regression or catagen phase, which is followed by the
grows into the dermal tissue and branches to form a small
resting or telogen phase. The final phase is the shedding or
system of ducts that end in expanded secretory acini. The
exogen phase.4,39
acini secrete by a holocrine mechanism, that is, the entire
The anagen phase is the active hair growing phase and it
secretory cell is filled with vesicles of secretory product that
usually lasts 2– 6 years. It is in this phase that the hair shaft then are released by rupturing the cell membrane and thus
is at its maximum length. In the anagen phase, hair growth destroying the cell. The basal layer of the acinar epidermis
recapitulates normal hair follicle development, with the for- consists of proliferating stem cells that constantly renew the
mation of a new lower hair follicle that begins with the supply of maturing secretory cells.14
proliferation of the secondary germ cells in the hair bulge. The sebaceous glands produce the oily sebum (a mixture
The germinal matrix will form the hair shaft while the bulb of lipids) that is released into the hair follicle and then
will provide the stem cells that migrate down to form the passes to the surface of the skin, which lubricates both the
lateral disk and thus provide germ cells for the next hair skin and the hair. Thus, cells formed by mitosis at the base
growth cycle. When the growth phase is completed, the of the gland are pushed toward the surface as new cells are
hair stops growing and the catagen phase is entered. The formed beneath. Along the way, the cells become packed
hair shaft becomes small and round and detached from with lipid and then undergo apoptosis. The secretions con-
the germinal matrix and is referred to as a club hair. The sist of breakdown products of the cells, which are extruded
lower two-thirds of the hair follicle goes through a highly into the lumen of the associated hair follicle (Fig 11). The
controlled process of involution, primarily reflecting the prenatal and early postnatal growth of the sebaceous gland
onset of rapid apoptosis in most follicular keratinocytes. is thought to be controlled by steroid hormone metabolism
404 兩 Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org
cretory cells secrete fluid directly across the plasma mem-
brane. That is, in eccrine glands, the secretions are the result
of the secretory intracytoplasmic vesicles fusing with the
cell membrane and then being released without destruction
of the membrane of the secretory cell.4 The epithelial at-
tachment of the developing gland to the epidermis forms the
primordium of the sweat duct, and the sweat glands begin
to function shortly after birth.3 The sweat glands are espe-
cially plentiful in the scalp.
The sweat ducts are uniquely lined by 2 layers of cuboi-
dal epithelial cells. This stratified cuboidal epithelium is
rarely found elsewhere in the body, and these cells function
in mediation of sodium from the sweat to prevent loss of
electrolytes. As noted, the sweat glands are vital to thermo-
regulation. When the ambient temperature is higher than
the body temperature, evaporation of sweat can cool the
skin below the core temperature. Often, normal thermoreg-
ulation occurs insensibly because sweat evaporates as
Fig 11. The drawing illustrates the relationship of a hair follicle, its asso- quickly as it is formed. However, dripping sweat, as occurs
ciated sebaceous gland, and, next to it, a sweat gland (modified from
http://www.lucianoschiazza.it/Documenti/Eruptive_syringoma_eng.
during exercise, is much less efficient because the body at-
html, open access). tempts ineffectively to compensate for the rising core tem-
perature.26 A normal hair follicle, a sweat gland, and a
sebaceous gland are compared in Figure 11.
by the fetal epidermis as well as maternal androgens and by
endogenous steroid synthesis of the fetus.12 Mature seba-
INNERVATIONS
ceous glands are present on the face by 6 months. Sebaceous
glands are highly active in the fetus, and the sebum they
produce combines with desquamating epidermal cells and Dermal Corpuscles
remnants of the periderm to form a waterproof protective The skin is the largest sensory organ of the body, recogniz-
coating for the fetus, the vernix caseosa. After birth, the ing and transmitting the sensations of pain, temperature,
sebaceous glands become relatively inactive, but, at pu- itch, and touch to the central nervous system (CNS). In
berty, they again begin to secrete large quantities of sebum addition, there are nerves that control blood flow, secretion
in response to the surge in circulating sex steroids. The of sweat, and piloerection. In particular, there are 4 primary
sebaceous glands are especially plentiful in the skin of the types of encapsulated mechanoreceptors that are special-
nose and the forehead. ized to provide the CNS with information regarding touch,
pressure, vibration, and cutaneous tension, and these recep-
Sweat Glands tors are Meissner corpuscles, Pacinian corpuscles, Merkel
There are several million sweat glands that cover the human cells, and Ruffini corpuscles, respectively. These mechano-
body. They serve as the primary source of cooling and hy- receptors are collectively referred to as low-threshold or
dration of the skin. The sweat glands (eccrine or merocrine high-sensitivity receptors because even weak mechanical
glands) first appear at approximately 14 –15 weeks as buds stimulation of the skin can induce these to produce an ac-
of stratum germinativum that grow down into the underly- tion potential. All of these low-threshold mechanoreceptors
ing dermis to form unbranched, highly coiled glands. The (LTMR) are innervated by relatively large myelinated ax-
intraepidermal portion of the gland duct develops as a result ons (type A), which ensure a rapid transmission of the
of a coalescence of groups of intracytoplasmic cavities tactile information to the CNS. In addition, there are noci-
formed within adjacent inner cells. However, the intrader- ceptors that sense painful stimuli, pruriceptors that convey
mal portion of the duct portion forms by dissolution of the the sense of itch, thermoreceptors that detect temperature,
desmosomal attachments between the cells that comprise and LTMRs that sense nonpainful stimuli or touch. These
the inner core of the duct germ.14 The peripheral cells dif- LTMRs are divided into subtypes that are distinguished by
ferentiate into an inner layer of secretory cells and an outer their unique sensitivities and conduction velocities, and
layer of myoepithelial cells, which are innervated by sym- their adaptation to sustained mechanical stimulation.40
pathetic fibers. These cells contract to expel sweat from the The tactile Meissner corpuscles are the last corpuscular
gland (Fig 12). The inner layer of cells of the developing mechanoreceptors to develop. The initial wave of sensory
sweat duct gradually lose their initial expression of the ker- innervation is directed to the Merkel cells and later on to the
atins K5/K14 and differentiate into K8/K18 expressing lu- Pacinian and Ruffini corpuscles. The differentiation of
minal cells. The outer basal layer cells remain positive for Meissner corpuscles occurs only after the dermal papillae
K5/K14 and differentiate into myoepithelial cells. The se- and epidermal papillary ridges have formed. Meissner cor-
Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org 兩 405
Fig 12. Drawings illustrate the development of a sweat gland (modified with permission from Moore KL, Persaud TV. The Developing Human Clinically
Oriented Embryology. 8th ed. China: Saunders Elsevier; 2008:443 [Fig 19 – 4]).
Table: Sensory skin receptors in the head and necka
Receptor Type Location Function Adaption Rate Threshold
Free nerve endings All of the skin Pain, temperature Slow High
Meissner corpuscles Lips and nonhairy skin Touch, dynamic pressure, crude touch Rapid High
Pacinian corpuscles Subcutaneous tissues Deep pressure, dynamic vibrations Rapid Low
Merkel cells All of the skin and the hair follicles Static pressure touch Rapid Low
Ruffini corpuscles All of the skin Stretching of skin Rapid Low
a
Modified from Ref 43, Table 9.1.
puscles are LTMRs that are responsible for sensitivity to shaped receptors located in the deeper skin, with their long
light touch. They have the highest sensitivity and thus the axis aligned with the stretch lines in the skin. As such, they
lowest threshold when sensing vibrations between 10 and are believed to respond to stretching of the skin.40 The
50 Hz. They are rapidly adaptive receptors, and, in the head primary skin receptors, their function, and adaptation and
and neck, they are most concentrated in the lips. Meissner threshold rates are summarized in Table 2.
corpuscles begin their differentiation at the apices of the There are a number of classes of primary afferent nerves
dermal papillae, and they project axonal processes into the that respond to thermal stimuli. The afferent nerve fibers
epidermis, with Schwann cells growing along and making that mediate the sensation of nonpainful warmth or cold
contact with the epidermal cells. The intraepidermal axonal seem adapted to convey this thermal information over a
processes characteristic of Meissner corpuscles may deter- particular temperature range. In contrast, nociceptive affer-
mine and ensure their position at the top of the dermal ents are often activated by both painful cold and heat stim-
papillae, close to the epidermis. uli.42 Nociceptors are unspecialized nerve endings, “free
Pacinian, or lamellar, corpuscles are the only other pha- endings” that initiate the sensation of pain. They arise from
sic tactile LTMRs. They are located deeper in the dermis, cells in the dorsal root ganglia of a spinal nerve or, in the
and they detect deep, quick pressure changes and vibrations case of the face, from the trigeminal ganglion. They send
in the skin. They do not detect pain, which is exclusively one axon to the periphery and the other into the spinal cord
signaled by free nerve endings. The optimal sensitivity of or directly into the brain stem. The axons associated with
Pacinian corpuscles is 250 Hz. There also are some free nociceptors conduct the impulses slowly, being either
nerve endings that may detect deep pressure. The Pacinian lightly myelinated or unmyelinated. This is in distinction to
corpuscles start as a cylindrical sensory terminal sur- the LTMRs described above, which are myelinated and fast
rounded by a layer of cells that are the presumptive inner conducting. Thus, axons that convey pain stimuli can fol-
core cells, which will accumulate around the terminal and low either a fast- or slow-conducting pathway.43 These no-
which are derived from Schwann cells. By birth and shortly ciceptors may also play a role in the sensation of itch. These
thereafter, the inner core lamellae increase in number and free nerve endings have no specialized associated structures
become concentrically tightly packed together.41 and terminate in the epidermis, penetrating almost to the
As previously mentioned, Merkel cells are slow reacting stratum corneum.
pressure-detecting mechanoreceptors that lie at the basal More specifically, the sensory nerves in the skin fall into
layer of the epidermis and are associated with a single un- 2 categories. In the epidermis, skin–nerve organs consist of
derlying nerve ending from the dermis. They identify static “free” nerve endings, or hederiform (ivy-shaped) nerve or-
touch stimuli. Ruffini corpuscles are elongated, spindle- gans, such as the Merkel cells. In this case, the term free
406 兩 Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org
In summary, the third trimester is a period of quiescence
in the ontogeny of the epidermis. All of the epidermis has
become keratinized, whereas the periderm has completely
sloughed. The subcutaneous appendages are formed and
are functioning. It is only as the fetus nears birth that there
is a sudden increase in thickness of the stratum corneum.12
The major events in the development of the skin and its
appendages, and when they occur during embryogenesis are
summarized in Figure 16.
PHYSIOLOGIC SKIN CHANGES
Age-Related Skin Changes
The functions of the skin, such as protection, thermoregu-
lation, and perceiving touch and itch, are all compromised
with aging. There is an overall tendency for atrophy, espe-
Fig 13. A drawing of the corpuscles and nerves in the skin (modified from
cially in the upper dermis, and the aging of the skin vascu-
https://en.wikipedia.org/wiki/Tactile_corpuscle. Open access).
lature produces changes in skin structure and distribution.
In normal skin, the blood capillaries have perpendicular
terminal nerve refers to a slight axon expansion that still loops that drain into a horizontal venous plexus (Figs 7 and
contains perineural cells, including cytoplasm of Schwann 8). In normal young skin, there are approximately 60 loops
cells and multiple cell organelles. In the dermis, free sensory to every square centimeter. However, with aging, there are
nerve endings are either associated with the hair complex far fewer loops, and this results in thinning of the upper
(Pinkus disk) or they have encapsulated nerve endings as dermis, which may become transparent so that a poorly
found in Ruffini and Meissner corpuscles, and so forth44 supported and dilated subpapillary plexus may be visible to
The different structures of these nerves and corpuscles and an observer. As an example, in the head and neck, there may
their primary locations within the skin are illustrated in be a 40% reduction of papillary loops in the forehead. In
Figure 13. addition to the capillary changes, the adnexal structures,
It is well known that the itch sensation can be reduced by such as the hair follicles and sebaceous and sweat glands, all
the “painful” sensation caused by scratching. However, not atrophy at different rates.46
only is itch inhibited by the enhanced input of pain stimuli, As already noted, the skin has adipose tissue that projects
the opposite is true. Thus, the inhibition of pain processing into the dermis. This fat has numerous blood capillaries but
may also reduce its inhibitory effect, which results in an no lymphatics. Rather, the lymphatics pass deeply through
enhancing itch. There clearly are complex interactions be- the skin septa along with the arterioles that supply the der-
tween pain and itch, and, although there is an obvious an- mis and the veins that drain it. The adipose tissue also
tagonistic interaction between pain and itch under normal shows increasing heterogeneity with aging, much of it re-
conditions, the patterns of peripheral and central sensitiza- lated to sex differences and the affects of sex hormones.
tion phenomena for pain and itch are surprisingly similar, These changes affect the function of the fat as a determinant
and, in the periphery, anti-inflammatory therapy will re- of body shape as well as its role in pressure dispersal and
duce both the sensitization for pain and for itch.45 insulation. In each of these functions, an aging blood supply
also plays a role. The endothelial cells respond to the me-
Cutaneous Innervations chanical forces of blood pressure and flow by regulating
The cutaneous innervation of the head and neck primarily vascular tone and by shape change. The capillaries become
lies in the dermis, and it comes from the branches of the less well supported by the age-related epidermal rete ridges
trigeminal nerve and from the upper 4 or 5 cervical spinal and the decrease in dermal connective tissue, and, as a re-
nerves (Figs 14 and 15). The sensory nerves are derived sult, senile purpura tears and pressure ulcers are a conse-
from outgrowths from the neural crest via the dorsal root quence. With aging, body shape, thermoregulation, and
ganglia. The autonomic system supplies the motor fibers to pressure from weight bearing all alter the skin texture, func-
the arterioles, arrector pili muscles, and myoepithelial cells tion and appearance.46
of the sweat glands. Within the dermis, the autonomic The lymphatic vessels also have a greater attenuation
nerves form a deep reticular plexus that has branches ex- and wider lumen in young people than in older subjects, and
tending into the papillary layer. Small axons are present there is an involution of the lymphatics that occurs with
early when the epidermis is bilaminar, and, by 8 weeks, age. Sclerosis and varicosity of the main lymphatic trunks
there already are functioning plexuses. By the fourth also occur. To function effectively, the lymphatic endothe-
month, the dermal plexuses are very well developed, and lial cell must be sensitive to any deforming tissue stresses so
Meissner and Pacinian corpuscles are present.8 that lymph is encouraged to move easily into the lymphat-
Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org 兩 407
Fig 14. The drawing illustrates the nerves that supply innervation to the skin.
Fig 15. A drawing of the ansa cervicalis and the cervical nerves (in green) that supply the skin of the neck and posterior scalp (modified with permission
from Netter FH. Atlas of Human Anatomy. 5th ed. Saunders Elsevier; 2011 [Fig 32]).
ics. In healthy skin, this process is helped by the “snap In addition, the vascularization of the dermis is also re-
back” provided by a closely applied and appropriately ori- duced, and, in people with light skin, the skin color gradu-
entated elastin fiber network. The orientation of elastin in ally becomes pale, even yellowish, especially in the neck and
the upper dermis allows it to take up some of the strain in an nape area. There also is a diminution of dermal and epider-
expanded upper dermis and to restore it rapidly to its nor- mal hydration, primarily due to age-related decreases of
mal width. However, with age, elastin tends to be replaced glycosaminoglycans. The dermis is the most deeply altered
by a less flexible degenerated form that provides rigidity compartment of the skin during the process of aging; how-
instead of pliability and elasticity. These age-related ever, there also is a reduction of epidermal thickness while,
changes are also highly associated with an overload of the at the same time, the thickness of the stratum corneum layer
lymphatics by a failing venous system.46 increases. With progressive aging, melanocytes are less
In summary, in the third decade of life, the skin slowly active and have larger melanosomes. This causes pig-
begins to show the consequences of aging. These changes mented “age” spots to occur mainly in the hands. The
occur slowly and almost imperceptibly. The first signs of hypodermis is also thinner, which results in the collaps-
aging are seen in the skin of the face, where tiny lines of ing of the skin.
expression result from the repeated tensions of the facial Ultraviolet (UV) exposure also affects the changes asso-
muscles that draw on the deepest parts of the dermis. Over ciated with aging, and, in effect, UV radiation amplifies and
time they form deeper wrinkles. Often, this is first noticed in speeds the chronological aging. Typically, in covered areas,
the corners of the eye as “crows’ feet.” This process evolves wrinkles are finer and not as deep as in exposed areas. In the
over years before becoming visible, and the wrinkles then face and neck, UV exposure causes deep wrinkles, rough-
spread slowly over the entire face and neck. The underlying ness, loose skin, and pigmentation as well as damage to
loss of dermal elasticity is not only seen in the appearance of fibroblasts and elastic fibers. A few weeks after sun expo-
wrinkles but also as looseness of the skin, commonly noted sure, the tan fades, but the deep rooted harmful effects to
in the neck.47 Some of the skin changes associated with the skin remain. These affects accumulate over years and
aging are summarized in Figure 17. end up producing deep wrinkles and spots of pigmentation.
408 兩 Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org
Fig 16. The figure summarizes the timing of major events in epidermal differentiation (modified from Table 1, p 311 in Holbrook KA. Human epidermal
embryogenesis. Int J Dermatol 1979;18:329 –56).
These changes are primarily due to an excessively slow der- fibers, which, rather than being positioned perpendicular to
mal renewal. The most striking change in the dermis caused the skin surface, as in young healthy skin, are positioned
by UV exposure is the accumulation of bundles of elastin parallel to the skin surface.47
Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org 兩 409
Fig 17. Drawings illustrate the major skin changes associated with aging.
Obesity Obese fat is immunologically different from lean fat.
Obesity has become a public health problem, especially in Macrophages that encourage local inflammation are re-
the United States, where it is estimated that one-fourth to ferred to as M1 macrophages, whereas those that are asso-
one-third of adult Americans and one-sixth of adolescents ciated with decreased inflammation and that encourage tis-
are obese.48 In addition to its impact on numerous health sue repair are referred to as M2 macrophages. This
issues and diseases, obesity is related to a number of effects difference results from the macrophage’s unique ability to
on skin physiology. Skin barrier functions are altered in metabolize the amino acid arginine into either nitric acid,
people who are obese, with an increase in transdermal wa- which can be considered a “killer-type” molecule, or orni-
ter loss and an increase in erythema, with a tendency to- thine, a repair-type molecule. In lean adipose tissue, there
ward dry skin. Obesity also affects the sebaceous glands, are small adipocytes and alternatively activated M2 mac-
with an increased proliferation of basal keratinocytes rophages that secrete adipocytokines such as interleukin
within the pilosebaceous duct. There is an incomplete sep- 10 (IL-10) and adiponectin, a protein hormone produced
aration of the ductal corneocytes from one another, which and secreted exclusively by adipocytes that regulate the
leads to subsequent obstruction of the pilosebaceous duct. metabolism of lipids, fatty acids, and glucose. It is the
This, in turn, is related to an increase in acne.49,50 activation of 5= adenosine monophosphate-activated
Compared with people who are not obese, people who protein kinase (AMPK), an enzyme that plays a role in
are obese have larger skin folds and sweat more profusely cellular energy, that inhibits the production of proin-
after becoming overheated. This is likely due to thicker flammatory cytokines and chemokines, increases adi-
layers of subcutaneous fat, with an increase in both the ponectin secretion, and inhibits macrophage recruitment
frictional and moisture components of the skin. Obesity and M1 polarization. These proteins all help maintain an
also impedes lymphatic flow in the subcutaneous tissues, anti-inflammatory environment.
which often results in lymphedema. Lymphedema is associ- It has also been postulated that physical damage to blood
ated with dilatation of tissue channels and reduced oxygen- vessel endothelium as a result of either the sheer increased
ation, and, in this setting, progressive fluid accumulation size of the adipocytes, crowding as a result of the adipocyte
can lead to fibrosis and chronic inflammation.49 Obesity is size, and the number or oxidative damage from an increas-
associated with altered collagen structure and function, and ing lipolytic environment could play a role in macrophage
thus impaired wound healing. This may be secondary to a recruitment, similar to that seen in atherosclerosis.53 How-
failure of collagen deposition to match the increase in skin ever, in obese adipose tissue, the adipocytes enlarge due to
surface area.51 Obesity is also associated with significant increased storage of triglycerides, become hypertrophic,
changes in cutaneous micro- and macrocirculation. Specif- and then necrotic. There is an associated infiltration of M1
ically, obesity is one of the primary causes of dysfunction of macrophages, which tend to accumulate around necrotic
the skin microcirculation, and this likely contributes to mi- adipocytes that form crownlike structures. The secretory
croangiopathy and hypertension.49 Lastly, in adults who products produced by the M1 macrophages and the hyper-
are not obese, the subcutaneous fat is composed almost trophic adipocytes further exacerbate the local inflamma-
entirely of white (yellow) fat, which provides insulation and tory environment. In addition, T cells accumulate in obese
acts as an energy depot. In contrast, brown fat, which is fat. Together, this adipose inflammation has been linked
more prevalent in people who are obese is not as effective in to obesity-related insulin resistance and type 2 diabetes (Fig
these roles.31,52 18).53,54
410 兩 Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org
Fig 18. Schematic drawing, illustrating the differences between lean and obese fat, and the different metabolic environments that they present. Also
listed are some of the receptor sites known to be on adipocytes.
Adipose tissue has also been shown to play a major role There are 2 primary theories regarding the etiology of
in energy homeostasis, lipid metabolism, the immune re- cellulite. In the most prevalent theory, the etiology may be
sponse, and reproduction. Steroids, and, in particular, es- based on sex differences in the structural characteristics of
trogens, promote, maintain, and control the typical distri- the subcutaneous fat lobules and the connective tissue septa
bution of body fat, overall fat mass, adipose deposition, that divide them. The cause of the dimpling is the result of
adipose differentiation, and adipocyte metabolism. A defi- herniation of fat, termed “papillae adiposae,” that pro-
ciency in estrogen leads to an increase in adipose tissue, trudes from the subcutis through the inferior surface of a
especially in visceral fat, and these changes have, in turn, weakened dermis at the dermo– hypodermal interface (Fig.
been linked to adipose dysfunction and a variety of diseases, 19). In fact, women have been shown to have a discontin-
including type 2 diabetes, hyperlipidemia, hypertension, uous dermo– hypodermal interface, whereas men have a
and cardiovascular diseases as well as a number of continuous interface. A second suggested etiology main-
malignancies.55,56 tains that the skin dimpling results from continuous and
progressive vertically oriented stretching within the hypo-
Cellulite dermal collagen fibrous strands that are well below the
The term cellulite describes a peau d’orange (peel of the dermo– hypodermal interface, a process that weakens the
orange) or a cottage cheese-type dimpling of the skin that connective tissue buttress, and this allows the fat hernia-
occurs most commonly in women who are postmeno- tion. There are 2 less-accepted theories: one that relates the
pausal, primarily in their thighs and buttocks. Some degree dimpling to vascular changes, and the other relates to the
of cellulite is present in 85%–90% of women who are post- presence of inflammation in the fibrous septae.52,57,58
menopausal but is rarely found in men. The actual term
cellulite comes from the French literature from 1920 and Postmenopausal Skin Changes
synonyms include the following: adipose edematosa, der- Sex-steroid hormones have effects on skin elastic fibers and
mopanniculosis deformans, status protrusus cutis, and gy- collagen content. There is a decrease in the amount of skin
noid lipodystrophy. Because there is no known morbidity collagen by approximately 2% each year after menopause,
or mortality associated with cellulite, it truly cannot be and the mean skin collagen content was ⬎48% in women
described as a pathologic condition of the skin.52 who are postmenopausal and treated with estrogen therapy
Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org 兩 411
to autosomal recessive hypotrichosis. Autoantibodies
against plakoglobin and plakophilin-1 (desmosomal plaque
proteins) cause Naxos disease (a recessive association of
arrhythmogenic right ventricular cardiomyopathy with
wooly hair and palmoplantar keratoderma or similar skin
disorder) and ectodermal dysplasia and skin fragility syn-
drome, respectively.64 In addition, mutations in the various
forms of keratin have been associated with specific diseases.
Thus, mutations in K5 and K14 are related to epidermolysis
bullosa simplex. Mutations in K1 and K10 cause epidermo-
lytic hyperkeratosis, whereas mutations in K1 and K9 cause
palmoplantar keratoderma epidermolytic disease.
Fig 19. The drawing illustrates the herniation of fat through the fascia, Melanocyte Abnormalities
which results in enlargement of the fat lobule and pushing of the overly- Human skin pigmentation normally varies greatly from ex-
ing epidermis upward; the septations between the lobules shorten, de- tremely fair to extremely dark, depending primarily on ra-
pressing the overlying skin; together, these changes cause the dimpling
cial and ethnic backgrounds. However, the constitutive me-
associated with cellulite.
lanocyte attenuation in the skin can also be affected by the
than in women who were not treated. Similarly, there is a environment so that chronic UV exposure can increase me-
decrease in the number and thickness of elastic fibers in the lanocyte attenuation 3– 4 –fold, whereas, conversely, toxic
skin by nearly 50% in women who are postmenopausal. compounds, for example, hydroquinone, can selectively
These estrogen-related deficiencies lead to an increase in and permanently destroy melanocytes in the skin.22 UV
“age-associated” skin changes, such as wrinkling and thin- radiation is the most significant factor that influences
ning, and dryness, all of which are increased in the post- changes in human skin pigmentation. As a direct effect of
menopausal years or in cases of estrogen deficiency.59-63 UV exposure, especially UVA (the longest wave length of
UV), there is an immediate pigment darkening that occurs
WHEN THINGS GO WRONG within minutes and persists for several hours. This is fol-
There are a great number of dermatologic diseases and con- lowed by persistent pigment darkening, which occurs
ditions. This section only mentioned a few that often are within several hours and lasts for several days. These rapid
related to the embryology of the skin and its aging. increases in pigmentation are not the result of acute melanin
synthesis but rather the result of oxidation and polymeriza-
Desmosomal Abnormalities tion of existing melanin and the redistribution of the exist-
Examination of the fundamental mechanisms by which the ing melanosomes. Delayed tanning also occurs several days
cytoskeletal proteins contribute to the architecture and after UV exposure, but this takes longer because it actually
function of the skin has revealed the role that keratin gene involves the activation of the melanocyte function.
mutations play in skin diseases, especially in autoimmune UV exposure leads to an increased expression of mi-
epidermal blistering disorders. The major cell-surface at- crophthalmia-associated transcription factor (MITF) (the
tachment sites for these intermediate filament networks are master transcriptional regulator of pigmentation) and its
the desmosomes and hemidesmosomes.64 Because these downstream melanogenic proteins, which eventually lead
structures play a key role in maintaining tissue integrity, to increases in melanin content. In addition, UV exposure
perturbations in their structure and function are responsible also increases levels of PAR2 (protease-activated receptor
for epidermal autoimmune diseases, such as alopecia 2) in keratinocytes, and this increases the uptake and distri-
areata, bullous pemphigoid, epidermolysis bullosa, pem- bution of melanosomes by keratinocytes in the epidermis.
phigus foliaceous, pemphigus vulgaris, and vitiligo; and Melanocytes protect the skin from UV exposure damage as
skin fragility syndromes, such as ectodermal dysplasia–skin noted by the fact that lightly pigmented skin has a 15–70 –
fragility syndrome and epidermolysis bullosa simplex fold increased risk of developing skin cancers compared
(Fig 20).64 with dark skin.65 The pigmentation of the skin is primarily
As examples, autoantibodies directed against the desmo- regulated by melanocortin 1 receptor (MC1R) (or alpha
somal proteins result in diseases such as pemphigus for melanocyte stimulating hormone receptor), which regulates
example, whereas autoantibodies against hemidesmosomal MITF and melanogenesis and dendricity. As such, MC1R is
proteins result in diseases such as bullous pemphigoid for often referred to as the susceptibility gene for melanoma
example. More specifically, autoantibodies against specific and other skin cancers.22 By comparison, albinism results
adhesion interface proteins, for example, desmogleins from dysfunctional tyrosinase (TYR) and other melano-
(Dsg), play a role in disruption of cell– cell adhesion. Thus, genic proteins, and leads to impaired pigmentation of the
autoantibodies against Dsg3 are implicated in pemphigus skin, hair, and eyes. Diminished skin color most commonly
vulgaris, whereas autoantibodies against Dsg4 are related is caused by decreases in epidermal melanin content as a
412 兩 Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org
Fig 20. A, The drawing illustrates some of the autoimmune bullous diseases and genodermatoses bullous diseases that are related to the cell– cell
attachments (modified from https://www.slideshare.net/DrYugandar/inflammatory-cells-of-skin. Open access). B, The drawings illustrate more
specifically the differences in the targets of autoimmune blistering diseases; when the autoantibodies are targeted against desmosomes, the blistering
occurs in the epidermis in diseases, for example, pemphigus. when the autoantibodies are directed against the hemidesmosomes, the blistering occurs
at the epidermal-dermal interface in diseases, for example, bullous pemphigoid (modified from https://www.mblintl.com/products/skin-blistering-
diseases/?_storeⴝdefault).
result of defects in melanin formation (leukoderma and hy- sive, it has been called the “werewolf syndrome,” and it has
popigmentation). In addition, the absence or loss of mela- a congenital form (present at birth) or an acquired form that
nocytes is found in vitiligo, whereas increased numbers of appears later in life. Hirsutism is a type of hypertrichosis
melanocytes that produce excessive amounts of melanin are exclusive to women and children, and it is related to exces-
seen in epidermal melanosis and freckles.22 sive male hormone levels. The causes of hypertrichosis in-
In summary, constitutive skin pigmentation is deter- clude transforming hair from the small vellus type to the
mined by a number of factors, including the migration of larger terminal type and an increase in the anagen phase of
melanoblasts during development, their survival and differ- hair growth.66
entiation into melanocytes, the attenuation of melanocytes,
the expression of enzymatic and structural constituents of
Sebaceous Gland Abnormalities
melanosomes, the synthesis of different types of melanin,
the transport of melanosomes to dendrites, the transfer of Some disorders that affect the sebaceous glands include the
melanosomes to keratinocytes, and, finally, the distribution following: comedones or blackheads, milia or whiteheads,
of melanin in epidermal layers above the basal layer.22 acne (overactive sebaceous glands related to hormonal
changes during adolescence), seborrhea (overactivity and
Dermal and Hypodermal Abnormalities and Aging excessive secretions of the sebaceous glands), rosacea, ker-
As previously noted, after the age of 20 –30 years, the skin atosis pilaris, steatoma or sebaceous cyst, sebaceous hyper-
slowly begins to show the consequences of chronological plasia, asteatosis (partial or absolute deficiency in sebum),
aging, which causes the appearance of the skin to slowly and furuncle.
and imperceptibly change. Examples of abnormalities that
effect the dermis and subcutaneous fat include the follow- Sweat Gland Abnormalities
ing: striae, solar elastosis or senile atrophy, white fibrous Hyperhidrosis is an abnormal increase in the amount of
papulosis of the neck, lichen sclerosus et atrophicus, Wer- sweat, and it may occur in a generalized or local form.
ner syndrome or adult progeria, and acrogeria. Many of Bromhidrosis is the production of malodorous sweat
these entities are related to decreased fibroblastic and col- mainly in the feet and axillary regions. Hypohidrosis or
lagen production, and faulty elastic fibers as well as gene anhidrosis is the retention or limitation in sweat produc-
dysfunctions. tion. The sweat glands are no longer functioning properly,
and this condition can result in overheating, heat stroke, or
Hair Follicle Abnormalities
even death. These conditions can be either congenital or
Abnormalities of the hair follicle can occur; some examples
acquired.
are as follows: androgenetic alopecia, which is due to min-
iaturization of genetically predisposed follicles as seen in
male baldness; alopecia areata, which is the result of an CONCLUSION
autoimmune response of hair follicles in the anagen stage; The function of the skin and its importance to human ho-
and telogen effluvium, in which an increased proportion of meostasis were reviewed. The embryology of the skin and
follicles enter the telogen stage, commonly caused by med- its appendages were reviewed as were skin changes that
ications and fevers.39 Hypertrichosis or Ambras syndrome occur as a result of aging, hormonal changes, and geneti-
is the abnormal growth of hair over the body. When exten- cally related disorders.
Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org 兩 413
REFERENCES granule extrusion and stratum corneum intercellular lamellae
1. De Falco M, Pisano MM, De Luca A. Embryology and anat- in murine keratinocyte cultures. J Invest Dermatol 1988;90:
omy of the skin. Curr Clin Pathol 2013;2013:1–15 110 –16. 10.1111/1523-1747.ep12462065
2. Carlson BM. Human Embryology and Developmental Biol- 20. Hartsock A, Nelson WJ. Adherens and tight junctions: struc-
ogy. In: Integumentary, Skeletal, and Muscular Systems. 4th ture, function and connections to the actin cytoskeleton.
ed. China: Mosby Elsevier, 2009:175–212 Biochim Biophys Acta 2008;1778:660 – 69. 10.1016/j.
3. Moore K. The developing human-clinically oriented embry- bbamem.2007.07.012
ology. In: The Integumentary System. 8th ed. Philadelphia, 21. Goodenough DA, Paul DL. Gap junctions. Cold Spring Harb
PA: WB Saunders; 2008:439 –56 Perspect Biol 2009;1:a002576
4. Schoenwolf GC, Bleyl SB, Brauer PR, et al. Larsen’s Human 22. Yamaguchi Y, Brenner M, Hearing VJ. The regulation of skin
Embryology. In: Schoenwolf GC, Bleyl SB, Brauer PR, Fran- pigmentation. J Biol Chem 2007;282:27557– 61. 10.1074/
cis-West PH, eds. Development of the Skin and Its Deriva- jbc.R700026200
tives. 4th ed. Philadelphia: Elsevier; 2001:155–71 23. Merad M, Ginhoux F, Collin M. Origin, homeostasis and
5. Som PM, Streit A, Naidich TP. Illustrated review of the em- function of Langerhans cells and other langerin-expressing
bryology and development of the facial region, part 3: an dendritic cells. Nat Rev Immunol 2008;8:935– 47. 10.1038/
overview of the molecular interactions responsible for facial nri2455
development. AJNR Am J Neuroradiol 2014;35:223–29. 24. Moll I, Moll R, Franke WW. Formation of epidermal and
10.3174/ajnr.A3453 dermal Merkel cells during human fetal skin development.
6. Fleischmajer R, Utani A, MacDonald ED, et al. Initiation of J Invest Dermatol 1986;87:779 – 87. 10.1111/1523-1747.
skin basement membrane formation at the epidermo-dermal ep12458993
interface involves assembly of laminins through binding to 25. Schoenwolf GC, Bleyl SB, Brauer PR, et al. Development of
the Skin and its Derivatives. In: Schoenwolf GC, Bleyl SB,
cell membrane receptors. J Cell Sci 1998;111(pt 14):1929 – 40
Brauer PR, Francis-West PH, eds. Larsen’s Human Embryol-
7. Breathnach AS. The Herman Beerman lecture: embryology of
ogy. Philadelphia, PA: Elsevier; 2001:155– 69
human skin, a review of ultrastructural studies. J Invest Der-
26. Introduction to Skin Histology. Southern Illinois University
matol 1971;57:133– 43. 10.1111/1523-1747.ep12261482
School of Medicine, 2014. http://www.siumed.edu/⬃dking2/
8. Holbrook KA, Odland GF. The fine structure of developing
intro/skin.htm
human epidermis: light, scanning, and transmission electron
27. Skobe M, Detmar M. Structure, function, and molecular con-
microscopy of the periderm. J Invest Dermatol 1975;65:16 –
trol of the skin lymphatic system. J Investig Dermatol Symp
38. 10.1111/1523-1747.ep12598029
Proc 2000;5:14 –19. 10.1046/j.1087-0024.2000.00001.x
9. Polakowska RR, Piacentini M, Bartlett R, et al. Apoptosis in
28. Ryan TJ, Mortimer PS, Jones RL. Lymphatics of the skin.
human skin development: morphogenesis, periderm, and stem
Neglected but important. Int J Dermatol 1986;25:411–19.
cells. Dev Dyn 1994;199:176 – 88. 10.1002/aja.1001990303
10.1111/j.1365-4362.1986.tb03443.x
10. Hamilton WJ, Boyd JD, Mossman HW. Human Embryology
29. Poissonnet CM, Burdi AR, Bookstein FL. Growth and devel-
(Prenatal Development of Form and Function). In: Integu- opment of human adipose tissue during early gestation. Early
mentary System the Skin and Its Derivatives. 2nd ed. Balti- Hum Dev 1983;8:1–11. 10.1016/0378-3782(83)90028-2
more, MD: Williams and Wilkins; 1952. 30. Gregoire FM, Smas CM, Sul HS. Understanding adipocyte
11. Stranding S. Skin and its appendages. In: Stranding S, ed. differentiation. Physiol Rev 1998;78:783– 809
Gray’s Anatomy. The Anatomical Basis of Clinical Practice. 31. Avram AS, Avram MM, James WD. Subcutaneous fat in nor-
40th ed. Spain: Churchill Livingston Elsevier; 2008:145– 64 mal and diseased states: 2. Anatomy and physiology of white
12. Holbrook KA. Human epidermal embryogenesis. Int J Der- and brown adipose tissue. J Am Acad Dermatol 2005;53:
matol 1979;18:329 –56. 10.1111/ijd.1979.18.5.329 671– 83. 10.1016/j.jaad.2005.05.015
13. Yoon KH, Yoon M, Moir RD, et al. Insights into the dynamic 32. Avram MM, Avram AS, James WD. Subcutaneous fat in nor-
properties of keratin intermediate filaments in living epithelial mal and diseased states: 1. Introduction. J Am Acad Dermatol
cells. J Cell Biol 2001;153:503–16. 10.1083/jcb.153.3.503 2005;53:663–70. 10.1016/j.jaad.2005.05.014
14. McGrath JA, Eady RA, Pope FM. Rook’s Textbook of Der- 33. Aherne W, Hull D. Brown adipose tissue and heat production
matology. In: Burns T, Breathnach S, Cox N, Griffiths C, eds. in the newborn infant. J Pathol Bacteriol 1966;91:223–34.
Anatomy and Organization of Human Skin. 7th ed. NJ: Wiley 10.1002/path.1700910126
Online Library; 2008. 34. Richard D, Carpentier AC, Doré G, et al. Determinants of
15. Alam H, Sehgal L, Kundu ST, et al. Novel function of keratins brown adipocyte development and thermogenesis. Int J Obes
5 and 14 in proliferation and differentiation of stratified epi- (Lond) 34(suppl 2):S59 – 66, 2010
thelial cells. Mol Biol Cell 2011;22:4068 –78. 10.1091/ 35. Peirce V, Carobbio S, Vidal-Puig A. The different shades of
mbc.E10-08-0703 fat. Nature 2014;510:76 – 83. 10.1038/nature13477
16. Fuchs E. Scratching the surface of skin development. Nature 36. Breathnach AS, Smith J. Fine structure of the early hair germ
2007;445:834 – 42. 10.1038/nature05659 and dermal papilla in the human foetus. J Anat 1968;102:
17. Olivera-Martinez I, Viallet JP, Michon F, et al. The different 511–26
steps of skin formation in vertebrates. Int J Dev Biol 2004; 37. Fuchs E, Merrill BJ, Jamora C, et al. At the roots of a never-
48:107–15. 10.1387/ijdb.15272376 ending cycle. Dev Cell 2001;1:13–25. 10.1016/S1534-
18. Narasimhan MJ Jr, Ganla VG. The permeability of the hu- 5807(01)00022-3
man skin to water. Indian J Physiol Pharmacol 1965;9: 38. Serri F, Cerimele D. Hair and Hair Diseases. In: Orfanos CE,
193–95 Happle R, eds. Embryology of the Hair Follicle. Germany:
19. Madison KC, Swartzendruber DC, Wertz PW, et al. Lamellar Springer-Verlag; 1990.
414 兩 Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org
39. Paus R, Cotsarelis G. The biology of hair follicles. N Engl 54. Ouchi N, Parker JL, Lugus JJ, et al. Adipokines in inflamma-
J Med 1999;341:491–97. 10.1056/NEJM199908123410706 tion and metabolic disease. Nat Rev Immunol 2011;11:85–
40. Zimmerman A, Bai L, Ginty DD. The gentle touch receptors 97. 10.1038/nri2921
of mammalian skin. Science 2014;346:950 –54. 10.1126/ 55. Gao H, Dahlman-Wright K. Implications of estrogen receptor
science.1254229 alpha and estrogen receptor beta for adipose tissue functions
41. Zelen J. The development of Pacinian corpuscles. J Neurocy- and cardiometabolic complications. Horm Mol Biol Clin In-
tol 1978;7:71–91. 10.1007/BF01213461 vestig 2013;15:81–90
42. Schepers RJ, Ringkamp M. Thermoreceptors and thermosen- 56. Pallottini V, Bulzomi P, Galluzzo P, et al. Estrogen regulation
sitive afferents. Neurosci Biobehav Rev 2009;33:205–12. of adipose tissue functions: involvement of estrogen receptor
10.1016/j.neubiorev.2008.07.009 isoforms. Infect Disord Drug Targets 2008;8:52– 60.
43. Purves D, Augustine GJ, Fitzpatrick D, et al. Neuroscience. 10.2174/187152608784139631
2nd ed. Sunderland, MA: Sinauer Associates; 2001 57. Nrnberger F, Mller G. So-called cellulite: an invented disease.
44. Roosterman D, Goerge T, Schneider SW, et al. Neuronal con- J Dermatol Surg Oncol 1978;4:221–29. 10.1111/j.1524-
trol of skin function: the skin as a neuroimmunoendocrine 4725.1978.tb00416.x
organ. Physiol Rev 2006;86:1309 –79. 10.1152/physrev. 58. Pirard GE, Nizet JL, Pirard-Franchimont C. Cellulite: from
00026.2005 standing fat herniation to hypodermal stretch marks.
45. Schmelz M. Itch and pain. Dermatol Ther 2005;18:304 – 07. Am J Dermatopathol 2000;22:34 –37. 10.1097/00000372-
10.1111/j.1529-8019.2005.00039.x 200002000-00007
46. Ryan T. The ageing of the blood supply and the lymphatic 59. Brincat M, Moniz CF, Studd JW, et al. Sex hormones and skin
drainage of the skin. Micron 2004;35:161–71. 10.1016/j. collagen content in postmenopausal women. Br Med J (Clin
micron.2003.11.010 Res Ed) 1983;287:1337–38. 10.1136/bmj.287.6402.1337
47. Farage MA, Miller KW, Elsner P, et al. Intrinsic and extrinsic 60. Castelo-Branco C, Duran M, Gonzlez-Merlo J. Skin collagen
factors in skin ageing: a review. Int J Cosmet Sci 2008;30:87– changes related to age and hormone replacement therapy. Maturi-
95. 10.1111/j.1468-2494.2007.00415.x tas 1992;15:113–19. 10.1016/0378-5122(92)90245-Y
48. Baskin ML, Ard J, Franklin F, et al. Prevalence of obesity in 61. Bolognia J. Aging skin, epidermal and dermal changes. Prog
the United States. Obes Rev 2005;6:5–7. 10.1111/j.1467- Clin Biol Res 1989;320:121–35
789X.2005.00165.x 62. Bolognia JL, Braverman IM, Rousseau ME, et al. Skin
49. Yosipovitch G, DeVore A, Dawn A. Obesity and the skin: skin changes in menopause. Maturitas 1989;11:295–304.
physiology and skin manifestations of obesity. J Am Acad 10.1016/0378-5122(89)90026-1
Dermatol 2007;56:901–16; quiz 917–20 63. Dunn LB, Damesyn M, Moore AA, et al. Does estrogen pre-
50. Lffler H, Aramaki JU, Effendy I. The influence of body mass vent skin aging? Results from the First National Health and
index on skin susceptibility to sodium lauryl sulphate. Skin Nutrition Examination Survey (NHANES I). Arch Dermatol
Res Technol 2002;8:19 –22. 10.1046/j.0909-752x 1997;133:339 – 42
51. Enser M, Avery NC. Mechanical and chemical properties of 64. Kottke MD, Delva E, Kowalczyk AP. The desmosome: cell
the skin and its collagen from lean and obese-hyperglycaemic science lessons from human diseases. J Cell Sci 2006;119:
(ob/ob) mice. Diabetologia 1984;27:44 – 49 797– 806. 10.1242/jcs.02888
52. Avram MM. Cellulite: a review of its physiology and treat- 65. Baccarelli A, Bertazzi PA, Landi MT. Molecular epidemiology
ment. J Cosmet Laser Ther 2004;6:181– 85. 10.1080/ for the study of the environment-genome interaction [in Ital-
14764170410003057 ian with English abstract]. G Ital Med Lav Ergon 2003;25:
53. Wellen KE, Hotamisligil GS. Obesity-induced inflammatory 424 –25
changes in adipose tissue. J Clin Invest 2003;112:1785– 88. 66. Mofid A, Seyyed Alinaghi SA, Zandieh S, et al. Hirsutism. Int
10.1172/JCI20514 J Clin Pract 2008;62:433– 43
Neurographics 2017 September/October; 7(5):390 – 415; www.neurographics.org 兩 415
You might also like
- Embriology, Variations and Innervations of The Human Neck MusclesDocument28 pagesEmbriology, Variations and Innervations of The Human Neck Musclesmloureiro17No ratings yet
- CanalsDocument25 pagesCanalsJurgen suarez moncaleanoNo ratings yet
- Anatomy - Endocrine System - HormonesDocument21 pagesAnatomy - Endocrine System - HormonesShereen AlobinayNo ratings yet
- EOC Review Packet StudentDocument15 pagesEOC Review Packet Studentjjman epicNo ratings yet
- Pluripotent Stem Cell GuidebookDocument52 pagesPluripotent Stem Cell GuidebookJonathan Torralba TorrónNo ratings yet
- Biochemistry Image BankDocument122 pagesBiochemistry Image BankRishik Rana100% (1)
- Mind Maps???Document58 pagesMind Maps???Talal MohammedNo ratings yet
- Week 1 of IGEMDocument68 pagesWeek 1 of IGEMXuejing DuNo ratings yet
- 21 - PDFsam - Robbins & Cotran Pathologic Basis of Disease, 9eDocument20 pages21 - PDFsam - Robbins & Cotran Pathologic Basis of Disease, 9eRizky Angga PerdanaNo ratings yet
- Cell StructureDocument3 pagesCell Structures2128226No ratings yet
- The Cell: The Cytoplasm and Nucleus: Cytoplasmic Organelles MitochondriaDocument5 pagesThe Cell: The Cytoplasm and Nucleus: Cytoplasmic Organelles Mitochondriavinnie0905No ratings yet
- L4 the+Endomembrane+SystemDocument21 pagesL4 the+Endomembrane+Systembmnyandu2003No ratings yet
- Presentation-The Nature of Life-Stage 2Document33 pagesPresentation-The Nature of Life-Stage 2Manuel CastroNo ratings yet
- Eukaryotic Cell Organelles and Their FunctionsDocument1 pageEukaryotic Cell Organelles and Their FunctionsShein GonzalesNo ratings yet
- Illumina DNA Methylation Infographic ST9Document1 pageIllumina DNA Methylation Infographic ST9201 101No ratings yet
- Motor proteins use ATP to power cellular movementsDocument16 pagesMotor proteins use ATP to power cellular movementserichaasNo ratings yet
- ANA LAB Cell MembraneDocument30 pagesANA LAB Cell MembraneAlessandra Franchesca CortezNo ratings yet
- AP Bio CH 15Document17 pagesAP Bio CH 15Jhun Banual ZaspaNo ratings yet
- GegwegwDocument27 pagesGegwegwSaverioFortunatoNo ratings yet
- Endocrine SystemDocument123 pagesEndocrine SystemZussette Corbita VingcoNo ratings yet
- 1 LezioneDocument17 pages1 Lezioneapi-3863584No ratings yet
- 2019 Recent Insights Into Natural Product Inhibitors of Matrix MetalloproteinasesDocument14 pages2019 Recent Insights Into Natural Product Inhibitors of Matrix MetalloproteinasescumbredinNo ratings yet
- Amino Acids and Protein Structure SummaryDocument3 pagesAmino Acids and Protein Structure SummaryANGEL JOY RAVALONo ratings yet
- Huntingtons PresentationDocument3 pagesHuntingtons Presentationapi-341316130No ratings yet
- Membrane Structure and DynamicsDocument1 pageMembrane Structure and DynamicsMaureen SisonNo ratings yet
- 3.2 Interaction Between Cells and The ECMDocument20 pages3.2 Interaction Between Cells and The ECMJays MartinezNo ratings yet
- Cheatt Sheet #2Document2 pagesCheatt Sheet #2layanhaliloNo ratings yet
- Termofisher Guide Stem CellDocument60 pagesTermofisher Guide Stem Cellnadhifa akNo ratings yet
- Eukaryotic Genomes: Organization, Regulation, and Evolution: Powerpoint Lectures ForDocument66 pagesEukaryotic Genomes: Organization, Regulation, and Evolution: Powerpoint Lectures Forxo_simpledreamNo ratings yet
- Mod 9 CC of Proteins Part 1Document9 pagesMod 9 CC of Proteins Part 1Benson PaglinawanNo ratings yet
- Lecture 9 & 10 - Endomembrane System I & IIDocument8 pagesLecture 9 & 10 - Endomembrane System I & IILujainNo ratings yet
- FULL Download Ebook PDF Human Reproductive Biology 4th Edition PDF EbookDocument41 pagesFULL Download Ebook PDF Human Reproductive Biology 4th Edition PDF Ebookkurt.klingenberger942100% (30)
- Lab Assignment - CH 14 HHMI Central Dogma of Genetic Medicine - TaggedDocument3 pagesLab Assignment - CH 14 HHMI Central Dogma of Genetic Medicine - TaggedashantiNo ratings yet
- Nurse Cheung - Life & Physical SciencesDocument5 pagesNurse Cheung - Life & Physical SciencesDuyen LeNo ratings yet
- FMS1 Cell Lecture 1 Handout-1Document16 pagesFMS1 Cell Lecture 1 Handout-1Muliana AzkiyaNo ratings yet
- Domains PDFDocument4 pagesDomains PDFSoumava PalitNo ratings yet
- Pathophysiology of KeratinizationDocument6 pagesPathophysiology of KeratinizationMario RodriguezySilvaNo ratings yet
- Module 2 Basic GeneticsDocument9 pagesModule 2 Basic GeneticsRaiza AwatNo ratings yet
- Advances in Hematology: The Red Cell Membrane, Part 1: The Role of The Red Cell MembraneDocument3 pagesAdvances in Hematology: The Red Cell Membrane, Part 1: The Role of The Red Cell MembraneroozNo ratings yet
- The Cell as a Unit of Health and DiseaseDocument120 pagesThe Cell as a Unit of Health and DiseaseRoscelie KhoNo ratings yet
- Endocrine System: Chemical ControlDocument36 pagesEndocrine System: Chemical ControlDrayton. Al sandraNo ratings yet
- 3 Dawson EpigenomeDocument7 pages3 Dawson EpigenomeMichelle GNo ratings yet
- L1 Gene ExpressionDocument5 pagesL1 Gene Expressiontowalovesports920No ratings yet
- La Célula. Conceptos Generales. Técnicas Básicas en Biología MolecularDocument111 pagesLa Célula. Conceptos Generales. Técnicas Básicas en Biología MolecularRaul Matute MartinNo ratings yet
- BiologyDocument4 pagesBiologyZam PamateNo ratings yet
- Normal Menstrual Cycle LectureDocument41 pagesNormal Menstrual Cycle LectureMorita Taka100% (1)
- 11.1 Nucleic Acid Chemistry Part 1Document7 pages11.1 Nucleic Acid Chemistry Part 1ChonaNo ratings yet
- Cytoskeleton 1Document75 pagesCytoskeleton 1Abdul Rehman IrfanNo ratings yet
- The Cell:: Fundamental Medical Science 1 CytologyDocument16 pagesThe Cell:: Fundamental Medical Science 1 CytologyezebelluciNo ratings yet
- Hemodynamic management in critical careDocument5 pagesHemodynamic management in critical carerabilaNo ratings yet
- Syndrome Cloned Gene Function Chromoso Mal Location Tumor TypesDocument7 pagesSyndrome Cloned Gene Function Chromoso Mal Location Tumor TypesElena PopaNo ratings yet
- Medical Embryology 1-76Document12 pagesMedical Embryology 1-76Aliya TambacNo ratings yet
- Instant Download Cell Biology 3rd Edition Ebook PDF PDF ScribdDocument36 pagesInstant Download Cell Biology 3rd Edition Ebook PDF PDF Scribdconstance.whitesell736100% (42)
- GENEDocument5 pagesGENEhanthuyNo ratings yet
- Genpath 1 5Document26 pagesGenpath 1 5yzzamedina44No ratings yet
- Cell CommunicationDocument42 pagesCell Communicationmegamemory14No ratings yet
- Hormones: College of Arts and Sciences Norzagaray CollegeDocument48 pagesHormones: College of Arts and Sciences Norzagaray CollegeKristopher OngNo ratings yet
- Alkylating agents and antimetabolites mechanisms of actionDocument2 pagesAlkylating agents and antimetabolites mechanisms of actionVianca Mae LopezNo ratings yet
- Cell Structures of Eukaryotes and ProkaryotesDocument3 pagesCell Structures of Eukaryotes and ProkaryotesCristian Kenneth TrillanesNo ratings yet
- Mock NewDocument15 pagesMock NewHosni ShowikeNo ratings yet
- Plant Growth and Development. Botany. FinalDocument47 pagesPlant Growth and Development. Botany. FinalMelanie Lequin CalamayanNo ratings yet
- Photosynthesis TestDocument4 pagesPhotosynthesis TestLester Eslava OrpillaNo ratings yet
- Medical Biology: T I L Ea A K - 1 G A M A TaDocument376 pagesMedical Biology: T I L Ea A K - 1 G A M A Tatiffylola100% (1)
- Annotated BibliographyDocument5 pagesAnnotated Bibliographyapi-399404406100% (2)
- Tumor Reg10Document9 pagesTumor Reg10Srinivas Reddy BoreddyNo ratings yet
- Biology HL Student GuideDocument134 pagesBiology HL Student GuideYesenia JassoNo ratings yet
- Intro To Eng Assignment 2Document3 pagesIntro To Eng Assignment 2legenddanny404No ratings yet
- Fragile X SyndromeDocument23 pagesFragile X SyndromeVincent ScorsinniNo ratings yet
- Discover Magazine - April 2011-TVDocument84 pagesDiscover Magazine - April 2011-TVViorel Petre100% (1)
- English CG (GR 7-8)Document17 pagesEnglish CG (GR 7-8)Rebell Mutya TanNo ratings yet
- The Effectiveness of Evening Primrose Oil Gel Capsule As A Cervical Ripening Agent During Labor InductionDocument4 pagesThe Effectiveness of Evening Primrose Oil Gel Capsule As A Cervical Ripening Agent During Labor InductionHazel Anne Ison Dumayas100% (1)
- Why Is The Penis Shaped Like That? and Other Reflections On Being HumanDocument11 pagesWhy Is The Penis Shaped Like That? and Other Reflections On Being HumanMacmillan Publishers0% (1)
- Phylogeny and Systematics: Powerpoint Lectures ForDocument35 pagesPhylogeny and Systematics: Powerpoint Lectures ForDimo PratannaNo ratings yet
- Cup, Insect Diversity Conservation (2005) PDFDocument357 pagesCup, Insect Diversity Conservation (2005) PDFjuanchotiradorNo ratings yet
- X Science QPDocument7 pagesX Science QPhritikaray4475No ratings yet
- LatinDocument22 pagesLatinabeer bouakelNo ratings yet
- Energy Efficient Landscape Forests of Nilgiris, Tamil NaduDocument8 pagesEnergy Efficient Landscape Forests of Nilgiris, Tamil NaduHues of SundropNo ratings yet
- NEURO Myasthenia GravisDocument25 pagesNEURO Myasthenia GravisNasrah N. MusaNo ratings yet
- Physiology, Lecture 6, Urinary SystemDocument74 pagesPhysiology, Lecture 6, Urinary SystemAli Al-QudsiNo ratings yet
- (English) Vision - Crash Course A&P #18 (DownSub - Com)Document8 pages(English) Vision - Crash Course A&P #18 (DownSub - Com)bank townNo ratings yet
- TEKNIKDocument16 pagesTEKNIKMahwestie PwarnasoekmaNo ratings yet
- Methods For Studying VirusesDocument24 pagesMethods For Studying VirusesFatima FarooqNo ratings yet
- Aakash Rank Booster Test Series For NEET-2020Document17 pagesAakash Rank Booster Test Series For NEET-2020Indian VanguardsNo ratings yet
- Final Report of Plantation CropsDocument870 pagesFinal Report of Plantation Cropsbharath dbNo ratings yet
- Mini-CLIA SystemDocument6 pagesMini-CLIA SystemVictoria AnnaNo ratings yet
- Dermatopathology Quick Reference Guide for Inflammatory Superficial Perivascular DisordersDocument2 pagesDermatopathology Quick Reference Guide for Inflammatory Superficial Perivascular DisordersBob LoblawNo ratings yet
- GA-02 Encoding TechniquesDocument42 pagesGA-02 Encoding TechniqueskiranNo ratings yet
- HS Grade 6 Exam 2020Document7 pagesHS Grade 6 Exam 2020Aditya PrasetyoNo ratings yet
- Balaytigue National High SchoolDocument2 pagesBalaytigue National High School3 stacksNo ratings yet