Professional Documents
Culture Documents
Test Case 3 H&P - Redacted
Uploaded by
Fernando Galera Jr.Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Test Case 3 H&P - Redacted
Uploaded by
Fernando Galera Jr.Copyright:
Available Formats
Page 1 of9
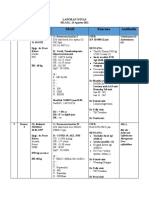
Patient Name MRN
"Progress MD at 12 /18/201810:17 AM (Date of
Service Note Date/Time)"
Author: Service: Internal Medicine Author Type:Physician
MD
Filed: 12/18/2018 3:44PM Note Type:Progress Notes Status: Signed
Editor:
Progress Note
Patient name:
Admit Date: 12/15/2018
Length of Stay: 3 days.
Subjective:
Denies angina
SOB continues to improve
No NN
No fevers
Denies cough
Objective:
Patient Vitals for the past 24 hrs:
Temp
BP Temp Pulse Resp SpO2 Weight
src
77.2 kg
12/18/18 0927 (170 lb
3.1 oz)
96.4 °F
12/18/18 0753 129/75 (35.8 ° Oral 66 18 96%
C)
96.9 °F
12/18/18 0434 103/66 (36.1 ° Oral 65 18 94%
C)
97.1 °F
12/17/18 2300 100/62 (36.2 ° Oral 67 18 99%
C)
96.8 °F
12/17/18 1930 105/61 Oral 67 18 95%
(36 °C)
12/17/18 1458 102/57 67 19 97%
Printed 12/19/2018 9:50:15 AM
Page 2 of9
12/17/18 1214 60 21 96%
12/17/18 1209 91/50
98 °F
12/17/18 1200 (36.7 ° Oral 58 22 97%
C)
12/17/18 1155 (!) 83/43
12/17/18 1050 61 29 97%
Intake/Output Summary (Last 24 hours) at 12/18/2018 1017
Last data filed at 12/18/2018 0818
Gross per 24 hour
Intake 312 ml
Output 1050 ml
Net -738 ml
Gen: sitting, in NAO
HENT: NCAT, MMM, on NC
Eyes: anicteric, conjunctiva clear
Neck: supple, no thyromegaly
CV: RRR, no mrg
Pulm: ctab, no accessory muscle use
Abd: soft, NTND, no masses palpated
Ext: 1 + lower extremity edema, wwp
Neuro: awake and alert, grossly nonfocal CN exam
Mood: stable
Skin: no rash or induration
GU: no foley
Central lines: no
Labs: reviewed
Results for orders placed or performed during the hospital
encounter of 12/15/18 (from the past 24 hour(s))
BUN and Creatinine (Obtain baseline and then every 3 days,
if not already ordered) Status: Abnormal
Collection Time: 12/17/18 10:39 AM
Result Value Ref Range
BUN 32 (H) 7 -21 mg/dL
Creatinine 1.90 (H) 0.57-1.25
mg/dL
EGFR 33 mUmin/1.73 sq
m
Basic Metabolic Panel Status: Abnormal
Collection Time: 12/17/18 10:39 AM
Result Value Ref Range
Sodium 135 (L) 136-145
meq/L
Potassium 3.3 (L) 3.5-5.1 meq/L
Chloride 95 (L) 98-107 meq/L
Printed 12/19/2018 9:50:15 AM
Page 3 of9
CO2 30(H) 22-29 meq/L
BUN 32(H) 7 -21 mg/dl
Creatinine 1.90 (H) 0.57-1.25
mg/dl
Glucose 157 (H) 70-105 mg/dl
Calcium 9.0 8.4 - 10.2
mg/dl
EGFR 33 mUmin/1.73 sq
m
Hemoglobin and hematocrit Status: Abnormal
Collection Time: 12/17/18 5:07 PM
Result Value Ref Range
Hemoglobin 11.0 (L) 13.7-17.5
GM/DL
Hematocrit 34.0 (L) 40.1 - 51.0 %
Hemoglobin and hematocrit Status: Abnormal
Collection Time: 12/18/18 4:38 AM
Result Value Ref Range
Hemoglobin 10.3 (L) 13.7-17.5
GM/DL
Hematocrit 31.0 (L) 40.1-51.0 %
Basic Metabolic Panel Status: Abnormal
Collection Time: 12/18/18 4:38 AM
Result Value Ref Range
Sodium 138 136 -145
meq/L
Potassium 4.1 3.5 - 5.1 meq/L
Chloride 96 (L) 98-107 meq/L
CO2 32(H) 22-29 meq/L
BUN 37 (H) 7-21 mg/dl
Creatinine 2.19(H) 0.57 -1.25
mg/dl
Glucose 113(H) 70-105 mg/dl
Calcium 9.3 8.4 - 10.2
mg/dl
EGFR 28 mUmin/1.73 sq
m
Micro: reviewed
Microbiology Results (last 7 days)
** No results found for the last 168 hours.**
Radiology: reviewed
Radiology Results (last day)
** No results found for the last 24 hours.**
Printed 12/19/2018 9:50:15 AM
Page 4 of9
Meds:
Scheduled Meds:
• aspirin 81 mg Oral Daily 81 mg at
12/18/18 0914
• carvedilol 3.125 mg Oral BID 3.125mg at
12/17/18 2043
• cetirizine 10mg Oral Daily 10mg at
12/17/18 0840
• clopidogrel 75mg Oral Daily 75mg at
12/18/18 0914
• furosemide 20mg Oral Daily 20mg at
12/18/18 0914
• pantoprazole 40mg Oral Daily 40mg at
12/18/18 0914
• pravastatin 40mg Oral Daily 40mg at
12/18/18 0914
• rivaroxaban 10mg Oral BID 10mg at
12/18/18 0909
• spironolactone 25mg Oral Daily 25mg at
12/18/18 0914
• sucralfate 1g Oral 4x Daily 1 g at 12/18/18
0920
Continuous Infusions:
• sodium chloride 0. 9% (NS) Stopped (12/1 6/18 0600)
PRN Meds:.
• acetaminophen
• sodium chloride 0. 9% (NS)
Notable studies to date:
ASSESSMENT
The patient is a 90 y .o . M with h/o AAA s/p EVAR, PAD w/ bilateral occlusion of SFA, HTN,
HLD, ischemic CMY (EF37%), CAD s/p prior CABG, who presented for dyspnea, found to have
NSTEMI and CHF exacerbation .
PLAN
CV-
NSTEMI, CAD with prior ACB - management per cardiology - planned conservative approach
with medical rx
- asa, statin; bb resumed
- on heparin , off nitro gtt
- TIE shows LVEF of 35-39% . LAE, mild right CHF
Acute on chronic systolic CHF/ICMP - diuresis per cardiology, s/p bumex 2mg IV bid - now
transitioned to oral daily Lasix
- volume status is improved
Printed 12/19/2018 9:50:15 AM
Page 5 of9
HTN- monitor bp with resumption of low dose coreg
HLD- statin
H/o AAA sip EVAR, h/o PVD with bilat occlusion of SFA- asa/statin
Pulm
On RA now
GI
GERO- cont ppi and carafate
Heme- monitor cbc
Renal -
AKI on CKD4 - cardiorenal. Diuresis per cardiology. Cr stable.
Hypomag- improved
GU - foleyout
Prophylaxis:
DVT: planned NOAC
Dispo- continue to mobilize. Home soon on medical rx
Discussed this case with pt and dt r
Notes reviewed.
Consultants/Teams on board:
Patient Name MRN
"H&P by 12/15/2018 5:27 PM (Date of Service Note Date/Time)"
Author: Service: Cardiology Author Type: Fellow
PM Note Type: H&P Status: Cosign Needed
Editor: Cosign Required: Yes
Expand All Collapse All
Printed 12/19/2018 9:50:15 AM
Page 6 of9
Cardiology Admission H&P
Name:
Facility: SLEH
Date: 12/15/2018
HPI
CC: Dyspnea
This is a 90 y.o. male with a medical history significant for AAA s/p EVAR, PAD w/ bilateral
occlusion of SFA, HTN, HLD, ischemic CMY (EF37%), CAD s/p prior CABG, who presents to
ER after being dyspneic for 2 days.
Per daughter and patient, over the past week has had worsening heart failure symptoms
including DOE, NYHA II -> Ill symptoms. Called Dr. Lufschanowski's office and had his GDMT
held. Yesterday had an episode of epigastric discomfort and possible CP similar to his prior
angina, became dyspneic with minimal exertion and presented to the ER.
Initial EKG showed AVR elevation with some diffuse ST depressions with a troponin of 15,
determined to be not a STEMI and high risk for elective PCI given SFA occlusions. Decision
was made for medical management of his NSTEMI currently given anatomy and co-morbidities.
ROS: 10 systems reviewed negative aside from HPI
Assessment and CV Plan
#NSTEMI
#HTN
# lschemic CMY (EF 37% prior), not tolerating medical therapies, NYHA class IV
symptoms
#CAD s/p CABG
- holding all guideline directed medical therapies currently given concern of developing
shock
- bumex 2 IV BID
- nitro drip
- heparin
- ASA/Plavix
- trend troponins
- repeat echo
- medical management for now, low threshold for ionotropes
History
Medical
Past Medical History:
Printed 12/19/2018 9:50:15 AM
Page 7 of9
Diagnosis Date
• Coronary artery disease
• Hyperlipemia
• Hypertension
• Myocardial infarction (HCC)
Surgical
Past Surgical History:
Procedure Laterality Date
• ABDOMINAL AORTIC ANEURYSM REPAIR
• CARDIAC SURGERY
bypass 1984
• CORONARY STENT PLACEMENT
• RELEASE,CARPAL TUNNEL
Converted from SIS-04/18/2012
• RELEASE,TRIGGER FINGER
Converted from SIS-04/18/2012
Social: He reports that he has quit smoking. he has never used smokeless tobacco. He
reports that he drinks alcohol. He reports that he does not use drugs.
Family: His family history is not on file.
Allergies I Medications
Allergies
Allergies
Allergen Reactions
• Iodine And Iodide Containing Products Rash
Home CV Meds
Medications Prior to Admission
Medication Sig Dispense Refill Last Dose
• bumetanide (BUMEX) 1 MG Take 1 mg by
tablet mouth daily.
• amLODIPine (NORVASC) 5 Take 5 mg by 10/5/2017 at
MG tablet mouth daily. Unknown time
• aspirin 81 MG EC tablet Take 81 mg by 10/5/2017
mouth daily.
• benzonatate (TESSALON) Take 100 mg by 10/6/2017 at
100 MG capsule mouth 3 (three) Unknown time
times daily as
needed for Cough.
• cetirizine (ZYRTEC) 10 MG Take 10 mg by 10/5/2017 at
tablet mouth daily. Unknown time
• clopidogrel (PLAVIX) 75 mg Take 75 mg by 10/4/2017
tablet mouth daily.
• cyanocobalamin 2000 MCG Take 2,500 mcg by 10/5/2017 at
tablet mouth daily. Unknown time
• esomeprazole (NEXIUM) 20 Take 20 mg by 10/6/2017 at
MG capsule mouth daily. Unknown time
Printed 12/19/2018 9:50:15 AM
Page 8 of9
• furosemide (LASIX) 20 MG Take 20 mg by 10/6/2017 at
tablet mouth 2 (two) Unknown time
times daily.
• isosorbide mononitrate TK2 TS PO QD. 3
(IMDUR) 30 MG 24 hr tablet
• metoprolol (LOPRESSOR) Take 25 mg by 10/5/2017 at
25 MG tablet mouth daily. 1200time
• multivit-iron-min-folic acid Take by mouth. 10/5/2017 at
(MULTIVITAMIN-IRON- Unknown time
MINERALS-FOLIC ACID)
3,500-18-0.4 unit-mg-mg
Chew
• pravastatin (PRAVACHOL) Take 40 mg by 10/5/2017 at
20 MG tablet mouth daily . Unknown time
• sucralfate (CARAFATE) 100 Take 1 g by mouth 10/5/2017 at
mg/ml suspension 4 (four) times daily. Unknown time
• UBIDECAR/FISH Take by mouth 10/5/2017 at
OIL/OMEGA-3NITE (CO Omega Q plus 100 Unknown time
Q10-FISH OIL-OMEGA 3-E w/ resveratrol .
ORAL)
Physical Exam
Vitals:
Temp: [97.7 °F (36.5 °C)] 97.7 °F (36.5 °C)
Heart Rate: [74-81] 75
Resp: [18-27] 19
BP: (109-128)/(76-83) 127/80
Gen: Sitting upright
Neck: JVP elevated
Chest wall: No deformity or tenderness
Pulm: Bilateral crackles
CV: RRR, S3, S4
Abd: Soft, non-distended
Ext: Warm, well-perfused, 1+ pitting edema
Pulses: 2+ and symmetric throughout
Neuro: Awake and alert without gross deficits
Labs
CBC
Recent Labs
12/15/18
1458
WBC 9.7
HGB 11.2*
HCT 34.1*
PLT 257
BMP
Printed 12/19/2018 9:50:15 AM
Page 9 of9
Recent Labs
12/15/18
1458
NA 138
K 3.6
CL 96*
CO2 30*
BUN 35*
CREATININE 1.90*
CALCIUM 9.5
Coags
Recent Labs
12/15/18
1458
INR 1.1
PTT 25.9
Cardiac
Recent Labs
12/15/18
1458
BNP 3,001*
TROPONINI 15.77*
Studies
EKG: AVR elevation with some diffuse ST depressions
CXR: Pending
TIE - prior recorded EF 37 % per notes:
Angiography - October 2017
Coronary Anatomy
Coronary Comments
LMCA Calcified, mild plaquing
LAD Proximal occlusion; mid LAD supplied by SVG
Diagonal Filled retrograde from mid LAD
LCx Mild proximal plaque
OM Patent proximal stent; 90% distal stenosis of large OM1
RCA Not injected, known occlusion
SVG-LAD 70% ostial stenosis; 90% stenosis of the SVG-LAD anastomosis
Printed 12/19/2018 9:50:15 AM
You might also like
- Pharmacotherapeutics-2: Case PresentationDocument20 pagesPharmacotherapeutics-2: Case PresentationHarish KamarajNo ratings yet
- Mapping Arafah 2 (Senin, 17 Desember 2018)Document4 pagesMapping Arafah 2 (Senin, 17 Desember 2018)Putri Rahmadhani Ngakpaniklage AsdsNo ratings yet
- Mapping Iccu 20 Desember 2021Document4 pagesMapping Iccu 20 Desember 2021Hilma NazaruddinNo ratings yet
- Nursing Care Plan: Ha Noi Medical UniversityDocument17 pagesNursing Care Plan: Ha Noi Medical UniversityThảo LÊNo ratings yet
- No - No. RM Pasien/Je NIS Kelamin/ Usia U/ B/ A ICD 10 Diagnosis LAM A RAW At/P L-PB Keterangan/Masalah DPJPDocument3 pagesNo - No. RM Pasien/Je NIS Kelamin/ Usia U/ B/ A ICD 10 Diagnosis LAM A RAW At/P L-PB Keterangan/Masalah DPJPNama ManaNo ratings yet
- Amprahan HCU Kamis Pagi, 15 Februari 2024Document6 pagesAmprahan HCU Kamis Pagi, 15 Februari 2024alfaz zamzamiNo ratings yet
- Mapping Aqsha 1 DPJP: Dr. Masralena Siregar, SP - PD Rabu, 02 Januari 2019Document6 pagesMapping Aqsha 1 DPJP: Dr. Masralena Siregar, SP - PD Rabu, 02 Januari 2019Fauzan AzimaNo ratings yet
- MAPING DR - NASRUL MUSADIR, SP.S FINA, 5/3/2021Document4 pagesMAPING DR - NASRUL MUSADIR, SP.S FINA, 5/3/2021Desty PurnamasariNo ratings yet
- Chronic Kidney DiseaseDocument21 pagesChronic Kidney DiseaseHarish KamarajNo ratings yet
- Mapping Dr. Ika Sp.s (K)Document3 pagesMapping Dr. Ika Sp.s (K)ifanda80No ratings yet
- Pemeriksaan Lab/ Penunjang (05/03)Document4 pagesPemeriksaan Lab/ Penunjang (05/03)ipd limabersaudaraNo ratings yet
- Aqsha 2 16-12-2018Document7 pagesAqsha 2 16-12-2018Jody Fajar HibatullahNo ratings yet
- Mortality Meet CASEDocument29 pagesMortality Meet CASEArnavjyoti DasNo ratings yet
- List Pasien 15 FebDocument8 pagesList Pasien 15 Febyenny purbaNo ratings yet
- Pemeriksaan Lab/ Penunjang (09/03) : LapageiDocument6 pagesPemeriksaan Lab/ Penunjang (09/03) : Lapageiipd limabersaudaraNo ratings yet
- Rekapitulasi Bedah Anak Rsup Ham Medan 31 JULI 2018 Rb2ADocument11 pagesRekapitulasi Bedah Anak Rsup Ham Medan 31 JULI 2018 Rb2AGokull ShautriNo ratings yet
- Hasil Nilai Normal 12.500 : Follow Up Sdr. SDocument8 pagesHasil Nilai Normal 12.500 : Follow Up Sdr. SArfin RamadhanNo ratings yet
- Amprahan PICU Sabtu, 20 Feb 2021Document6 pagesAmprahan PICU Sabtu, 20 Feb 2021muhammadrikiNo ratings yet
- Mapping DR Herry P 10-12-2022Document1 pageMapping DR Herry P 10-12-2022nina purnamasariNo ratings yet
- Lal Pathlabs ReportDocument2 pagesLal Pathlabs ReportindianroadromeoNo ratings yet
- Lal Passthlabs ReportDocument2 pagesLal Passthlabs ReportpramodkumarduvasuNo ratings yet
- Mapping Bedah Urologi Rabu 13-12-2018: NO Kamar Nama Terapi Planning LAB 1 K4B1Document3 pagesMapping Bedah Urologi Rabu 13-12-2018: NO Kamar Nama Terapi Planning LAB 1 K4B1Muhammad IlhaamNo ratings yet
- Coass: Ilham, Tari, NurhabibahDocument3 pagesCoass: Ilham, Tari, NurhabibahharzalinaNo ratings yet
- Case Report: Ni Ketut Puspa Sari DR - IDA Putri Wirawati, SP - PK (K)Document12 pagesCase Report: Ni Ketut Puspa Sari DR - IDA Putri Wirawati, SP - PK (K)ekaNo ratings yet
- Procedure For Production of Cryoprecipitate: Table 15-2 Blood Component CharacteristicsDocument2 pagesProcedure For Production of Cryoprecipitate: Table 15-2 Blood Component Characteristicssam mohNo ratings yet
- MORNING REPORT ICU 22 SeptemberDocument5 pagesMORNING REPORT ICU 22 SeptemberThaharatin GizaNo ratings yet
- Dari TB Dots Adjusting Dose 1x2 Tablet: AlergiDocument12 pagesDari TB Dots Adjusting Dose 1x2 Tablet: Alergiabu amarNo ratings yet
- DR Auladi Halim Umar Lubis - MALARIADocument37 pagesDR Auladi Halim Umar Lubis - MALARIAAuladi Lubis ∑No ratings yet
- Pemeriksaan Lab/ Penunjang (10/03) : LapageiDocument8 pagesPemeriksaan Lab/ Penunjang (10/03) : Lapageiipd limabersaudaraNo ratings yet
- List Pasien 15 Feb 2018Document8 pagesList Pasien 15 Feb 2018yenny purbaNo ratings yet
- Lapsus ICU (Meningitis + Bronchopneumonia + Susp. Sepsis)Document32 pagesLapsus ICU (Meningitis + Bronchopneumonia + Susp. Sepsis)ditaNo ratings yet
- Rodriguez, Jellica Castillo 2216042496Document6 pagesRodriguez, Jellica Castillo 2216042496jellica rodriguezNo ratings yet
- Whole Body Report - 1 June 2023Document5 pagesWhole Body Report - 1 June 2023NitishPaudelNo ratings yet
- Pinere 1 30 Juli 2021Document1 pagePinere 1 30 Juli 2021Rina SyafritaNo ratings yet
- FIXx Prof SY 03 Desember 2022Document6 pagesFIXx Prof SY 03 Desember 2022Fitri DicyNo ratings yet
- Kamala DeathDocument12 pagesKamala DeathLANKAPATRUDU6772No ratings yet
- Data Klinik Nilai Normal: TanggalDocument4 pagesData Klinik Nilai Normal: TanggalArina RNo ratings yet
- Laporan Jaga Bangsal 3-5-2017Document9 pagesLaporan Jaga Bangsal 3-5-2017rezaNo ratings yet
- Laporan Jaga Bangsal Rabu, 26 Desember 2018Document8 pagesLaporan Jaga Bangsal Rabu, 26 Desember 2018oyomziicNo ratings yet
- Jaring, Josephine Rivera 1816085500Document3 pagesJaring, Josephine Rivera 1816085500Analiza Rivera JaringNo ratings yet
- Morning Case Report: Thursday, December 16 2021Document71 pagesMorning Case Report: Thursday, December 16 2021dikiprestya391No ratings yet
- Its Just HoaxDocument10 pagesIts Just HoaxArkhan HanafiNo ratings yet
- TD: 120/80 MMHG Nyeri Kepala (-), Pandangan Kabur (-)Document3 pagesTD: 120/80 MMHG Nyeri Kepala (-), Pandangan Kabur (-)Matias SetyawanNo ratings yet
- 55122505241#5852#55122505241#9 - 16 - 2022 12 - 00 - 00 AmDocument2 pages55122505241#5852#55122505241#9 - 16 - 2022 12 - 00 - 00 AmAdham ZidanNo ratings yet
- MAPPINGDocument2 pagesMAPPINGPratiwi ARHNo ratings yet
- AQSHA 2, 15 Juli '19Document6 pagesAQSHA 2, 15 Juli '19Hiya Ulfi MuniraNo ratings yet
- Begapara Premsagar Chowk House No 149 Ward No 6 DURG, 490023: Page: 1 of 17Document17 pagesBegapara Premsagar Chowk House No 149 Ward No 6 DURG, 490023: Page: 1 of 17Dani Shashwat100% (1)
- KAMIS, 18-02-2021: Lantai 2: Hcu: 1 Ruang Rawatan: 2 Lantai 2 HCUDocument22 pagesKAMIS, 18-02-2021: Lantai 2: Hcu: 1 Ruang Rawatan: 2 Lantai 2 HCUBella DirkNo ratings yet
- HANDOVER ICU HCU 23 Agustus 2021 PagiDocument4 pagesHANDOVER ICU HCU 23 Agustus 2021 PagiNur Izdihar HadiNo ratings yet
- Mappimg Kamar 1 Dan 5Document4 pagesMappimg Kamar 1 Dan 5Satrya DitaNo ratings yet
- Mapping PDP 11 SeptDocument7 pagesMapping PDP 11 Septranti putri ayuNo ratings yet
- Aerobic Testing Lab ReportDocument25 pagesAerobic Testing Lab Reportapi-734755901No ratings yet
- Sensus Neuro 21 Agustus 2018Document3 pagesSensus Neuro 21 Agustus 2018wardahNo ratings yet
- List Pasien Isolasi 08072020 SALAM SEHAT SEMUADocument26 pagesList Pasien Isolasi 08072020 SALAM SEHAT SEMUAsylvesterbenyNo ratings yet
- Mapping Aqsa 3 (20 Februari 2019)Document6 pagesMapping Aqsa 3 (20 Februari 2019)Egi Atika HandayaniNo ratings yet
- BED Nama Pasien Sbar Rencana Antibiotik: Laporan DinasDocument3 pagesBED Nama Pasien Sbar Rencana Antibiotik: Laporan DinasRizal arisandiNo ratings yet
- Lapjag 20 Okrober 2020Document11 pagesLapjag 20 Okrober 2020Ardina MaristaNo ratings yet
- Rekapitulasi Pasien Dept. Orthopaedi RSUP HAM Hari/Tgl: Kamis/5 Juli 2018 No Identitas TGL Masuk Place Diagnosis Terapi Rencana Keterangan 03/07/2018Document5 pagesRekapitulasi Pasien Dept. Orthopaedi RSUP HAM Hari/Tgl: Kamis/5 Juli 2018 No Identitas TGL Masuk Place Diagnosis Terapi Rencana Keterangan 03/07/2018Chairul andikaNo ratings yet
- Math 9 - Evaluating Operations On Trigonometric Expression of Special AnglesDocument3 pagesMath 9 - Evaluating Operations On Trigonometric Expression of Special AnglesFernando Galera Jr.No ratings yet
- Math-9-LP - Q1 - W1C Solves Quadratic Equations by (A) Extracting Square Roots - (B) Factoring - (C) CompDocument3 pagesMath-9-LP - Q1 - W1C Solves Quadratic Equations by (A) Extracting Square Roots - (B) Factoring - (C) CompFernando Galera Jr.No ratings yet
- Math-9-LP - Q1 - W2 Characterizes The Roots of A Quadratic Equation Using The DiscriminantDocument3 pagesMath-9-LP - Q1 - W2 Characterizes The Roots of A Quadratic Equation Using The DiscriminantFernando Galera Jr.No ratings yet
- Math-9-LP - Q1 - W1 Illustrates Quadratic EquationsDocument2 pagesMath-9-LP - Q1 - W1 Illustrates Quadratic EquationsFernando Galera Jr.100% (1)
- John MarkDocument19 pagesJohn MarkFernando Galera Jr.No ratings yet
- Finah Feb B. Cabual - Docx2Document18 pagesFinah Feb B. Cabual - Docx2Fernando Galera Jr.No ratings yet
- Finah Feb B. CabualDocument1 pageFinah Feb B. CabualFernando Galera Jr.No ratings yet
- John Mark KadusaleDocument1 pageJohn Mark KadusaleFernando Galera Jr.No ratings yet
- MLTMHS Nat10Document2 pagesMLTMHS Nat10Fernando Galera Jr.No ratings yet
- For DisplayDocument3 pagesFor DisplayFernando Galera Jr.No ratings yet
- AOE - Hiral Labs LTD Company Brochure 20180416170521Document20 pagesAOE - Hiral Labs LTD Company Brochure 20180416170521Dr VENKAT1 LUNo ratings yet
- Progressive Addition Lens Design and The Short of Stature (Shan-Yu, S.)Document3 pagesProgressive Addition Lens Design and The Short of Stature (Shan-Yu, S.)Valentina PereaNo ratings yet
- Sandy Hill CHC SIS Letter WatsonDocument3 pagesSandy Hill CHC SIS Letter WatsonJon WillingNo ratings yet
- BPM Feb 14-18 2016Document23 pagesBPM Feb 14-18 2016lendelNo ratings yet
- 74 - SHE Specification Matla Reheat Attemperator Scope (Boiler) - 25102012 Rev0 PDFDocument85 pages74 - SHE Specification Matla Reheat Attemperator Scope (Boiler) - 25102012 Rev0 PDFvenkatrangan2003No ratings yet
- Logic ModelDocument2 pagesLogic ModelstojannaNo ratings yet
- Baba Farid University of Health Sciences, Faridkot Provisional Merit List of Candidates Applied For Admission To MBBS/BDS Courses Under NEET UG-2021Document130 pagesBaba Farid University of Health Sciences, Faridkot Provisional Merit List of Candidates Applied For Admission To MBBS/BDS Courses Under NEET UG-2021Nitish GargNo ratings yet
- 05 Soares+et+al V3Document7 pages05 Soares+et+al V3Elsa Marta SoaresNo ratings yet
- Aqucar IG 50 PDFDocument4 pagesAqucar IG 50 PDFSteven Reuben PurnomoNo ratings yet
- Coca Cola The Water Stewardship and Replanish Report1 2012Document80 pagesCoca Cola The Water Stewardship and Replanish Report1 2012CSRmedia.ro NetworkNo ratings yet
- Cancer - 2011 - Hajdu - A Note From History Landmarks in History of Cancer Part 2Document10 pagesCancer - 2011 - Hajdu - A Note From History Landmarks in History of Cancer Part 2Pilar AufrastoNo ratings yet
- Scientific Point of ViewDocument2 pagesScientific Point of Viewpavans EnglishNo ratings yet
- Hazmat Transportation Training RequirementsDocument12 pagesHazmat Transportation Training RequirementsSafety IezzproNo ratings yet
- Public Health Community Health Nursing: Goal: To Enable EveryDocument10 pagesPublic Health Community Health Nursing: Goal: To Enable Everyjamie carpioNo ratings yet
- The Book of BulkDocument16 pagesThe Book of BulkpopeyeballinaNo ratings yet
- Understanding and Completing The Reversion (25pp)Document25 pagesUnderstanding and Completing The Reversion (25pp)Tony Lambert100% (3)
- BTPB RepertoryDocument24 pagesBTPB Repertoryanamika mishra100% (1)
- Brubaker 2001Document5 pagesBrubaker 2001Residencia OftalmologíaNo ratings yet
- Root Caries: A Periodontal Perspective: Review ArticleDocument21 pagesRoot Caries: A Periodontal Perspective: Review ArticleIlmia AmaliaNo ratings yet
- Red Hill ComplaintDocument109 pagesRed Hill ComplaintHonolulu Star-AdvertiserNo ratings yet
- Aspiracion Destornillador Implanto Roa-V1-Id1018Document3 pagesAspiracion Destornillador Implanto Roa-V1-Id1018CesarAmorotoNo ratings yet
- Sps PPR CleaningDocument5 pagesSps PPR CleaningManutençãoTI TechNo ratings yet
- MalariaDocument170 pagesMalariatummalapalli venkateswara rao100% (4)
- Essay (DUNGARAN, JOHN KLENN) (BSCE-1CDocument2 pagesEssay (DUNGARAN, JOHN KLENN) (BSCE-1CJohn KlennNo ratings yet
- Panangbigbig Ken Panangisurat Kadagiti Numero Manipud 0 Aginggana 100Document4 pagesPanangbigbig Ken Panangisurat Kadagiti Numero Manipud 0 Aginggana 100EVANGELINE DARRASNo ratings yet
- FDP Form 7 - 20% Component of The IRA Utilization 20% Component of The Ira Utilization For The First Quarter, Cy 2017Document32 pagesFDP Form 7 - 20% Component of The IRA Utilization 20% Component of The Ira Utilization For The First Quarter, Cy 2017Juna Majistad CrismundoNo ratings yet
- Apply Appropriate Safety Measures While Working inDocument28 pagesApply Appropriate Safety Measures While Working inNanette A. Marañon-Sansano100% (5)
- Cen Cenelec Wp2016 enDocument80 pagesCen Cenelec Wp2016 enVamsi Pavan PavuluriNo ratings yet
- Spelling 101Document10 pagesSpelling 101Arellano CheireyNo ratings yet
- MoH - Uganda RBF Program Hospital Quartely Quality Assessment Tool - Jan 2019Document31 pagesMoH - Uganda RBF Program Hospital Quartely Quality Assessment Tool - Jan 2019Steven SsemwangaNo ratings yet