Professional Documents
Culture Documents
NCP
Uploaded by
Denise Gabato0 ratings0% found this document useful (0 votes)
16 views5 pagesNursing care plan
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentNursing care plan
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
16 views5 pagesNCP
Uploaded by
Denise GabatoNursing care plan
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 5
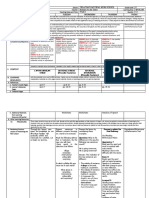
NURSING CARE PLAN FORM
Patient’s Name (Initials): C. M. G. Postoperative Diagnosis: 1. Cystic Hygroma Left 2. Nodular Colloid Goiter Right Non Toxic
Age: 30 years old Sex: Female Physician (Initials): Dr. M. A. L.
Diet: Nothing by Mouth
SUBJECTIV OBJECTIV NURSING SCIENTIFIC PLANNING INTERVENTIONS RATIONALE EVALUATION
E E DIAGNOSI ANALYSIS
S
Impaired Decreased, Short term goal: Independent: 1. Hoarseness and sore The patient
verbal delayed, or absent The patient will 1. Assess throat may occur was able to
communicat ability to receive, communicate speech secondary to tissue communicate
ion may be process, transmit, through eye periodically; edema or surgical through eye
related to and use a system contact, facial encourage damage to recurrent contact, facial
physiologic of symbols. expressions, voice rest. laryngeal nerve and may expressions,
condition as and other last several days. and other
evidenced Source: nonverbal 2. Provide Permanent nerve nonverbal
by total Doenges, M.E., et gestures within alternative damage can occur (rare) gestures within
absence of al. Nurse’s Pocket 1 month. methods of that causes paralysis of 1 month.
language Guide Edition 15. The patient will communicati vocal cords and/or The patient
F.A. Davis attempt to use on as compression of the was able to
Company. language and appropriate, trachea. use language
Philadelphia, begin to e.g., slate and begin to
Pennsylvania. communicate board, 2. Assistive devices such as communicate
2008 with words letter/picture text-to-speech, TTY or with words
within 5 to 6 board. Place TDD assists those with within 5 to 6
months. IV line to speech impairments. months.
The patient will minimize Picture boards and other The patient
have increase interference apps can help children was able to
language skills with written communicate. It learn language
needed for communicati facilitates expression of skills needed
social and on. needs. for social and
emotional 3. Sign emotional
reciprocal language. 3. Nurses can implement reciprocal
interactions important words and interactions
within 6 to 8 4. Use an phrases into their within 6 to 8
months. interpreter. profession to months.
The patient will communicate with The patient
use language or patients. Commonly used was able to
5. Pay attention phrases in the hospital
gestures to use language
to nonverbal such as “pain” “bathroom”
identify self, or gestures to
cues and or “water” can be useful
others, objects, identify self,
gestures. to learn.
feelings, needs, others,
plans, and objects,
desires within 6. Display 4. An interpreter should feelings,
12 months proper always be used when needs, plans,
speech communicating with a and desires
Long term goal: etiquette. patient who does not within 12
The patient will speak the nurse’s months.
communicate to language.
significant 7. Involve the The patient
other/caregiver family. 5. Patients may have was able to
and peers at specific gestures or cues communicate
least four basic 8. Keep they use to communicate. to significant
needs (hunger, communicati It may take time for the other/caregiver
thirst, fatigue, on simple; nurse to learn what these and peers at
pain), verbally ask yes/no are, but should be least four basic
and/or through questions. respected and needs (hunger,
gestures and reciprocated. thirst, fatigue,
body language. pain), verbally
9. Anticipate and/or through
needs as 6. Never speak loudly at a
gestures and
possible. Visit speech-impaired person
body
patient unless they are hard of
language.
frequently. hearing. Maintain eye
contact and allow the
10. Continue patient to see your
speaking to mouth, do not turn away
the patient when speaking. Give the
even if they patient plenty of time to
can’t respond.
respond.
11. Post notice of 7. Family members often
patient’s know how to best
voice communicate with the
limitations at patient and can teach the
central nurse what the patient is
station and trying to say. Though the
answer call nurse should always
bell promptly. speak directly to the
patient, they can ask the
family for assistance to
12. Hang clarify information.
signage and
document
accordingly. 8. Patients who have
difficulty forming words or
who are aphasic may
13. Maintain require longer to process
quiet speech and respond. Try
environment. sticking to shorter
questions and allow
Collaborative: plenty of time to respond.
Do not ask multiple
14. Incorporate questions together.
speech- Asking questions that
language only require a “yes” or
therapy and “no” answer may be best
support
services. when possible.
9. Reduces anxiety and
patient’s need to
communicate.
10. Patients with a
tracheostomy or physical
barrier or who have
dysphagia or dementia
should still be spoken to
as a person.
11. Prevents patient from
straining voice to make
needs known/summon
assistance.
12. Once the best form(s) of
communication have
been discovered,
document in the chart
and hang signage so
other staff members are
aware of how to best
communicate with the
patient.
13. Enhances ability to hear
whispered
communication and
reduces necessity for
patient to raise/strain
voice to be heard.
14. Speech-language
therapists can assist by
using language and
articulation activities for
children. They can teach
exercises to strengthen
the mouth and tongue
muscles and breathing
exercises to help with
resonance issues.
You might also like
- "What I Mean Is..." A Structured Program to Improve Mild to Moderate Retrieval/Fluency Problems 3rd EditionFrom Everand"What I Mean Is..." A Structured Program to Improve Mild to Moderate Retrieval/Fluency Problems 3rd EditionRating: 5 out of 5 stars5/5 (1)
- Nursing Care Plan: Assessment Nursing Diagnosis Inference Planning Intervention Rationale EvaluationDocument2 pagesNursing Care Plan: Assessment Nursing Diagnosis Inference Planning Intervention Rationale EvaluationIrish LigayaNo ratings yet
- THE SILENT CONVERSATION: Understanding the Power of Nonverbal Communication in Everyday Interactions (2024 Guide for Beginners)From EverandTHE SILENT CONVERSATION: Understanding the Power of Nonverbal Communication in Everyday Interactions (2024 Guide for Beginners)No ratings yet
- NCP Klinefelter Syndrom (Dumagal)Document2 pagesNCP Klinefelter Syndrom (Dumagal)Criza May DumagalNo ratings yet
- ONE: One-Handed Non-Traditional Expression for Patients who had a StrokeFrom EverandONE: One-Handed Non-Traditional Expression for Patients who had a StrokeNo ratings yet
- As Needed.: Environmental Stimuli 6Document4 pagesAs Needed.: Environmental Stimuli 6Nicole GumolonNo ratings yet
- Decoding Body Language: Crack the Code of Human Behavior, Speed Read People Like a Book, and Learn How to Analyze People with NLP, Manipulation, Dark Psychology, Mind Control, and Persuasion Skills.From EverandDecoding Body Language: Crack the Code of Human Behavior, Speed Read People Like a Book, and Learn How to Analyze People with NLP, Manipulation, Dark Psychology, Mind Control, and Persuasion Skills.Rating: 5 out of 5 stars5/5 (43)
- Nursing Care Plan Autism Spectrum DisorderDocument1 pageNursing Care Plan Autism Spectrum DisorderHarold Peranduz100% (5)
- Assessment Nursing Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Independent: Short TermDocument3 pagesAssessment Nursing Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Independent: Short TermhelloaNo ratings yet
- Assessment NX Diagnosis Planning Intervention Rationale EvaluationDocument4 pagesAssessment NX Diagnosis Planning Intervention Rationale EvaluationLady Daphne LandichoNo ratings yet
- X. Nursing Care Plan: ObjectiveDocument6 pagesX. Nursing Care Plan: ObjectiveRenea Joy ArruejoNo ratings yet
- Nursing Care Plan For Cerebrovascular AccidentDocument4 pagesNursing Care Plan For Cerebrovascular AccidentJobelle AcenaNo ratings yet
- 8-18 Topic 2 Communication and Self-AwarenessDocument7 pages8-18 Topic 2 Communication and Self-AwarenessGhianx Carlox PioquintoxNo ratings yet
- Speech Delay - Nursing Care Plan 1Document7 pagesSpeech Delay - Nursing Care Plan 1Natipal FlordelizaNo ratings yet
- NCP Impaired Verbal CommunicationDocument2 pagesNCP Impaired Verbal CommunicationLovelie Grace GalarpeNo ratings yet
- Cerebrovascular Accident (CVA) N C P BY BHERU LALDocument1 pageCerebrovascular Accident (CVA) N C P BY BHERU LALBheru LalNo ratings yet
- Nursing Care Plan For Patient With Stroke Assessment Diagnosis Outcomes Intervention Rationale EvaluationDocument4 pagesNursing Care Plan For Patient With Stroke Assessment Diagnosis Outcomes Intervention Rationale EvaluationJeza VargasNo ratings yet
- NCP Autism101Document5 pagesNCP Autism101Gio Padallan PisquizaNo ratings yet
- Care Plan On AlzheimerDocument4 pagesCare Plan On Alzheimeranimesh pandaNo ratings yet
- Imprecise:: Speech Gesture Advantages Disadvantages Advantages DisadvantagesDocument5 pagesImprecise:: Speech Gesture Advantages Disadvantages Advantages Disadvantagesapi-361794810No ratings yet
- NCP On Impaired Verbal CommunicationDocument3 pagesNCP On Impaired Verbal CommunicationArdiene Shallouvette GamosoNo ratings yet
- Nursing Care Plan CVADocument4 pagesNursing Care Plan CVAhermesdave175% (4)
- Group NCPDocument17 pagesGroup NCPNiña Noreen Torres VallegaNo ratings yet
- SPD-560 Lang Milestone Chart - LoarDocument5 pagesSPD-560 Lang Milestone Chart - LoarJeannine62V100% (1)
- Sam MyDocument1 pageSam MySammy D. SanoriaNo ratings yet
- Impaired Verbal CommunicationDocument2 pagesImpaired Verbal CommunicationMart AlunanNo ratings yet
- Assessment Nursing Diagnosis Planning Interventions Rationale Evaluation Subjective: Short Term Goal: Independent: Short Term Goal: Successfully MetDocument2 pagesAssessment Nursing Diagnosis Planning Interventions Rationale Evaluation Subjective: Short Term Goal: Independent: Short Term Goal: Successfully Metdominoredwing2024No ratings yet
- Language and CommunicationDocument3 pagesLanguage and Communicationonlineo6400No ratings yet
- Lesson PlanDocument3 pagesLesson PlanlianaNo ratings yet
- Grade 10: Modular Distance Learning S.Y. 2020-2021Document10 pagesGrade 10: Modular Distance Learning S.Y. 2020-2021John Cyrus DizonNo ratings yet
- Research ProblemDocument4 pagesResearch Problemjohn carlo bengalaNo ratings yet
- NCP CvaDocument3 pagesNCP CvaJey PangilinanNo ratings yet
- NCP CvaDocument3 pagesNCP CvaJey PangilinanNo ratings yet
- Assessment Cva Verb1Document2 pagesAssessment Cva Verb1JhiLy 사랑의 케빈 우No ratings yet
- FAR EASTERN UNIVERSITY NURSING CARE PLANDocument3 pagesFAR EASTERN UNIVERSITY NURSING CARE PLANDesiree Deleon Guerrero0% (2)
- PurCom MidtermsDocument5 pagesPurCom MidtermshaneenamaedediosNo ratings yet
- NCPDocument12 pagesNCPJoshuaNo ratings yet
- Subjective Data: "Mag Lisud Raba Na Siya Og Storya Unya Magka Rumble Ang Mga Words " As Verbalized by The CaregiverDocument6 pagesSubjective Data: "Mag Lisud Raba Na Siya Og Storya Unya Magka Rumble Ang Mga Words " As Verbalized by The CaregiverflorenzoNo ratings yet
- Therapeutic Communication With Older AdultsDocument4 pagesTherapeutic Communication With Older AdultsACERET, IVAN LAURENTINE G.No ratings yet
- Project 7 Plannification BGUDocument8 pagesProject 7 Plannification BGUNyah VegaNo ratings yet
- 4.01-PDR-Physician Communication SkillsDocument5 pages4.01-PDR-Physician Communication SkillsJoher MendezNo ratings yet
- "Hindi Ko Kayo Masyadong Marinig Sa Kanang Tenga Ko, Pwede Bang Sa Kaliwang Side Ko Kayo Magsalita?" As Verbalized by The PatientDocument2 pages"Hindi Ko Kayo Masyadong Marinig Sa Kanang Tenga Ko, Pwede Bang Sa Kaliwang Side Ko Kayo Magsalita?" As Verbalized by The PatientMussaib Mushtaq100% (1)
- Impaired Verbal CommunicationDocument4 pagesImpaired Verbal CommunicationDharylle CariñoNo ratings yet
- Sistema AumentativoDocument9 pagesSistema Aumentativolaura valentina castillo sanchezNo ratings yet
- Chapter 9 ReportDocument11 pagesChapter 9 ReportEmerald IsleNo ratings yet
- Soft Skills and Interpersonal CommunicationDocument20 pagesSoft Skills and Interpersonal Communicationradhemadhav0907No ratings yet
- What's New: A Control and RegulationDocument6 pagesWhat's New: A Control and RegulationDonela Miriam Onal EscosoraNo ratings yet
- Trans - PDR - Moy 2Document1 pageTrans - PDR - Moy 2JOSLIN ROZ GALILEANo ratings yet
- PlanningDocument11 pagesPlanningairelorenzoNo ratings yet
- Speak App A Development of Mobile ApplicationDocument6 pagesSpeak App A Development of Mobile ApplicationWemerson MonteiroNo ratings yet
- HST 660028Document5 pagesHST 660028osama.alawadhi313No ratings yet
- A. Linguistic in Nature: Ed Danielle N Prieto Ge2 BscoeDocument6 pagesA. Linguistic in Nature: Ed Danielle N Prieto Ge2 BscoeEd Danielle PrietoNo ratings yet
- Bells Palsy NCPDocument3 pagesBells Palsy NCPLeonardo Martin FrivaldoNo ratings yet
- PC- REVIEWERDocument4 pagesPC- REVIEWERqwbh72b6dvNo ratings yet
- Speech-Language Concerns 1Document7 pagesSpeech-Language Concerns 1api-291426388No ratings yet
- Motor Speech ChartDocument5 pagesMotor Speech Chartapi-433239461No ratings yet
- Geed05 Pur. Com. l1Document3 pagesGeed05 Pur. Com. l1Daennise Louiseanna SebastianNo ratings yet
- Submitted By: Group 1 Bagundang Bernan Quimado Lapitan Lu Learning Activity 7Document10 pagesSubmitted By: Group 1 Bagundang Bernan Quimado Lapitan Lu Learning Activity 7Benhur Leithold LapitanNo ratings yet
- 1 Konsep Komunikasi Dan Self AwarenessDocument21 pages1 Konsep Komunikasi Dan Self AwarenessRizki Odzan C'pecandu CintaNo ratings yet
- Communication in Context For Senior High School. Quezon CityDocument2 pagesCommunication in Context For Senior High School. Quezon CityRoy AlaNo ratings yet
- Gabato - Drug Study 1-3Document6 pagesGabato - Drug Study 1-3Denise GabatoNo ratings yet
- Nursing Care Plan 1Document2 pagesNursing Care Plan 1Denise GabatoNo ratings yet
- DS LosartanDocument2 pagesDS LosartanDenise GabatoNo ratings yet
- BIPERIDENDocument3 pagesBIPERIDENDenise GabatoNo ratings yet
- Week 1Document5 pagesWeek 1Kimberley Sicat BautistaNo ratings yet
- Vocabulary List - Life Intermediate: Unit 1 - ColourDocument4 pagesVocabulary List - Life Intermediate: Unit 1 - ColourZaira LombardoNo ratings yet
- CS2305 - PP Notes - CSE TUBEDocument158 pagesCS2305 - PP Notes - CSE TUBELakshmi NarayananNo ratings yet
- Introduction To RAPID: Operating ManualDocument58 pagesIntroduction To RAPID: Operating ManualObed BardalesNo ratings yet
- English Exam Practice 2Document10 pagesEnglish Exam Practice 2Samer Idris ElayyanNo ratings yet
- BT Project Team TCS, Kolkata: ConfidentialDocument99 pagesBT Project Team TCS, Kolkata: ConfidentialChandni KumariNo ratings yet
- SQL Engine ReferenceDocument608 pagesSQL Engine ReferenceIndra AnggaraNo ratings yet
- Look 5 Unit 1-5Document44 pagesLook 5 Unit 1-5Jipa Ioana100% (1)
- Mandarin Lesson 3 - Common ExpressionsDocument5 pagesMandarin Lesson 3 - Common ExpressionscelesteNo ratings yet
- Formatting Gridview Based On Row Data - Part 9: Support Us C# Programs Subscribe Buy DVDDocument3 pagesFormatting Gridview Based On Row Data - Part 9: Support Us C# Programs Subscribe Buy DVDshradha11No ratings yet
- Jamaica LessonsDocument5 pagesJamaica Lessonsapi-253473780No ratings yet
- Adrian Underhill Teaching Pronunciation SkillsDocument18 pagesAdrian Underhill Teaching Pronunciation SkillstalleringlesNo ratings yet
- Filologia AngielskaDocument7 pagesFilologia AngielskaAnna CostaNo ratings yet
- Grey Larsen Notation SystemDocument18 pagesGrey Larsen Notation SystemBrad MaestasNo ratings yet
- NÉSTOR CÁCERES VELÁSQUEZ ANDEAN UNIVERSITY - Test 7Document4 pagesNÉSTOR CÁCERES VELÁSQUEZ ANDEAN UNIVERSITY - Test 7evelin espinoza mamaniNo ratings yet
- Use of The ImperativeDocument34 pagesUse of The Imperativeakhilesh sahooNo ratings yet
- Introduction To African LiteratureDocument63 pagesIntroduction To African Literaturekawaii100% (1)
- FLED315 PresentationDocument28 pagesFLED315 PresentationFeyza ÇapaNo ratings yet
- Telling Story Lesson PlanDocument3 pagesTelling Story Lesson PlanivyredredNo ratings yet
- String Manipulation: Cc3 Cluster 2 SEM A.Y. 2019-2020Document16 pagesString Manipulation: Cc3 Cluster 2 SEM A.Y. 2019-2020Rovell AsideraNo ratings yet
- PRACTICE First ConditionalDocument2 pagesPRACTICE First Conditionalkaren timanaNo ratings yet
- Linguistic ImperialismDocument10 pagesLinguistic ImperialismNam PhanNo ratings yet
- Regular VerbsDocument1 pageRegular VerbsMarco Antonio Villavicencio SánchezNo ratings yet
- 8r Priprema Unit4 TestDocument3 pages8r Priprema Unit4 TestDejan LazicNo ratings yet
- DLL in English (Week 3)Document10 pagesDLL in English (Week 3)Rodalyn Joy Dizon100% (1)
- The Nirukta of YaskaDocument542 pagesThe Nirukta of YaskaTina BhatNo ratings yet
- WritingOutput2Final CecilioDocument9 pagesWritingOutput2Final CecilioStephanie CecilioNo ratings yet
- Understanding Rejoinders Through ECRIF and PPUDocument10 pagesUnderstanding Rejoinders Through ECRIF and PPUlearnerivan100% (1)
- 02 GXP B1 Progress Test 2 PDFDocument9 pages02 GXP B1 Progress Test 2 PDFDusan PetrovicNo ratings yet
- The Firelight Fairy BookDocument114 pagesThe Firelight Fairy BookJay.ashaNo ratings yet