Professional Documents
Culture Documents
Diagnostic Methods: Amylase
Diagnostic Methods: Amylase
Uploaded by
claudia mcheikOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diagnostic Methods: Amylase
Diagnostic Methods: Amylase
Uploaded by
claudia mcheikCopyright:
Available Formats
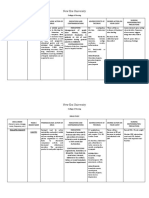
Diagnostic Methods
Test Interpretation
Diagnostic Test Measures Indications Other
Result Parameters
Patient prep involves avoiding
Normal 2 - 9 mg
24 Hour 5- Breakdown product of serotonin-rich foods (bananas,
Carcinoid Syndrome
Hydroxyindolacetic Acid serotonin Carcinoid pineapples, avocados, mushrooms,
50 - 500 mg
Syndrome and walnuts)
Pancreatic cancer Can be obtain through serum, urine,
Acute pancreatitis Pancreatic pseudocyst
Mumps pleural fluid, or peritoneal fluid
Digestive enzyme made Moderately HIGH
Salivary gland
Pancreatic cancer Mumps inflammation
Amylase mostly by the pancreas Acute cholecystitis
and salivary glands Salivary gland
Perforated peptic ulcer
Perforated peptic ulcer Acute pancreatitis
inflammation HIGH
Pancreatic pseudocyst
Pancreatic cancer Serum sample
Digestive enzyme made mostly by Pancreatic cancer Acute pancreatitis Moderately HIGH
Acute cholecystitis
Lipase the pancreas that breaks down
triglycerides Pancreatic pseudocyst Pancreatic disease HIGH
Acute pancreatitis
Pancreatic pseudocyst
Total protein Albumin
Liver Function Group of blood labs designed to
give infomration about the state
ALT AST
HIGH Cholangitis
Alkaline phosphatase Total bilirubin
Tests of the liver Conjugated bilirubin
Normal Hepatitis
Pregnancy
Excessive IV fluid
Cirrhosis
Serum protein disorders
Liver disease
LOW
Chronic alcoholism
Total Serum Total amount of protein
Nutritional status
Heart failure
Nephrotic syndrome
in the serum Burns
Protein Dehydration
Waldenström's
macroglobulinemia
Liver function
HIGH Multiple myeloma
Hyperglobulinemia
Granulomatous diseases
Some tropical disease
The liver makes 12 g of albumin daily.
Normal Hepatitis
Serum prealbumin can be used as a
Major protein Acute hepatocellular more sensitive test to assess rapid
Albumin component of blood
Liver disease Liver damage
LOW
dysfunction liver damage (acute viral or toxic
etiologies)
Cirrhosis
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Diagnostic Methods
Test Interpretation
Diagnostic Test Measures Indications Other
Result Parameters
Normal 10 - 60 U/L Moderate ALT content in kidneys,
heart, and skeletal muscle
Moderately HIGH Acute cholecystitis
Alanine ALT is ubiquitous at lower
Liver damage concentrations.
Aminotransferase Hepatocellular enzyme Liver damage Liver inflammation
Severe muscle injury
(ALT) HIGH Hepatitis
Cirrhosis
Hemolysis
Normal 10 - 60 U/L Some drugs and patient conditions
Liver
alter AST levels.
Moderately HIGH Acute cholecystitis
Hemolysis causes elevation due to
Heart
Aspartate High Level of AST
MI
PE
RBC contents.
Important enzyme in Brain
Aminotransferase amino acid metabolism
Skeletal muscle trauma
Alcholoic cirrhosis
Skeletal muscle HIGH
(AST) Viral hepatitis
Cirrhosis
Moderate Level of AST RBCs Drug-induced hepatitis
Cell necrosis
Only a screening test of coagulation
Prothrombin Effectiveness of the
extrinsic pathway of
Warfarin therapy Liver disease
Will not being to prolong until one of
the PT-based clotting factor
Time coagulation Vitamin K deficiency decreases to < 30 - 40% of normal
Sodium Potassium
Hepatic Group of assays Chloride Carbon dioxide
concerning the function Glucose Urea
Function Panel of the liver Creatinine
Albumin
Calcium
Phosphorus
Normal 30 - 135 U/L
Alkaline Enzyme at high levels in
Active bone formation
Pregnancy
Phosphatase rapidly dividing or Bile duct destruction Liver disease
HIGH
Some intestinal
disorders
metabolically active cells
(ALP) Cirrhosis
Bile duct destruction
Alcohol-induced hepatic
Cholestasis Biliary obstruction
changes
Enzyme involved with the Hepatocellular disease
γ-Glutamyltransferase Liver damage Hepatocellular disease Hepatobillary disease
transport of amino acids HIGH
Hepatitis
(GGT)
into cells (can be normal)
Hepatobillary disease Biliary stasis Cirrhosis
(can be normal)
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Diagnostic Methods
Test Interpretation
Diagnostic Test Measures Indications Other
Result Parameters
Not as subject to elevation from
↑ ALP drugs as ALP/GGT
If ↑ ALP but 5'-nucleotidase is
5'-Nucleotidase Hepatic enzyme Cholestasis
normal, look for a source outside the
Liver metastases liver (bone, kidney, or spleen)
Exposure to light may alter bilirubin
Normal 0.2 - 1.2 U/L
chemical and spectral properties
Acute cholecystitis because of the formation of
Moderately HIGH
Choledocholithiasis photobilirubin
Gallbladder disease Hepatocellular function ↑ Production from
heme
Defective heme removal
Total amount of bilirubin Gilbert syndrome
Total Bilirubin in the blood Neonatal jaundice
Severe Crigler-Najjar
HIGH
syndrome
Alcoholic hepatitis
Degree of hemolytic
Some hereditary disease Infectious hepatitis
disease
Autoimmune conditions
Intrahepatic obstruction
Extrahepatic obstruction
Using conjugated and unconjugated
Conjugated > 50% of elevated total Intrahepatic cholestasis Hepatocellular damage
bilirubin, you can differentiate
bilirubin level is conjugated Extrahepatic biliary between hepatic disease and
Bilirubin obstruction
↑ Total bilirubin
hemolysis
Acclerated RBC
Unconjugated < 15 - 20% of the total hemolysis
Hepatitis
bilirubin is unconjugated
Bilirubin Drugs
Can test for cell counts and chemical
Surgical diagnostic procedure Intraperitoneal
Abdominal trauma analysis
Diagnostic to determine if there is free hemorrhage
floating fluid in the
Peritoneal Lavage abdominal cavity Ruptured intestine Ruptured organs
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Diagnostic Methods
Test Interpretation
Diagnostic Test Measures Indications Other
Result Parameters
↑ WBC
Bacterial
↑ Neutrophils
Peritonitis
Ascites (+) Culture
Pancreatic Ascites ↑ Amylase
Malignant Blood fluid
Peritonitis (nontraumatic tap)
Cell counts Cirrhosis
Procedure to obtain CHF
HIGH SAAG
Paracentesis peritoneal fluid for
Cytology
( ≥ 1.1)
Alcoholic hepatitis
Myxedema
diagnosis or therapeutics Portal vein thrombosis
Testing
Bacterial peritonitis
Gram stain Malignancy
LOW SAAG Nephrotic syndrome
(< 1.1) Pancreatitis
Chemical testing TB
Peritonitis
Epstein-Barr virus WBC Normal or low
Cyctomegalovirus AST Striking ↑
Non-Liver Targeting Herpes simplex virus ALT Striking ↑
Pathogens Yellow fever Follows AST and ALT
Total Bilirubin
Mumps elevations
Inflammation / infection Rubella Alkaline
Hepatitis of the liver Hepatitis A Phosphatase
Parallels bilirubin
Hepatitis B
Antigens and
Liver Targeting Hepatitis C Pathogen-specific
Antibodies
Pathogens Hepatitis D
Hepatitis E Mild proteinuria
Urine
Hepatitis G Bilirubinuria
IgM Acute infection Total anti-HAV may be used to screen
Traveling to endemic Previous exposure people at risk who may need
Anti-HAV Antibody against HAVAg Hepatitis A
areas IgG Noninfectivity vaccination
Immunity
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Diagnostic Methods
Test Interpretation
Diagnostic Test Measures Indications Other
Result Parameters
First evidence of Persists throughout clinical illness
Outer surface coat infection
HBsAg antigen
POSITIVE
Infection with HBV
Implies infectivity
Hepatitis B Recovery from HBV
infection
Anti-HBs Antibodies against HBsAg POSITIVE Noninfectivity
Vaccination
Immunity
Appears soon after
HBsAg but before
IgM anti-HBs
Antibodies against the
Anti-HBc core antigen C
Hepatitis B Acute hepatitis B
Persists 3 - 6 months
Persists beyond IgM
IgG
Immunity
Viral replication
HBeAg Secretory form of HBcAg
Hepatitis B
POSITIVE
Infectivity
Less viral replication
Anti-HBe Antibody for HBeAg POSITIVE
Less infectivity
Parallels HBeAg
Post-recovery from
Pieces of DNA from More sensitive and precise marker of
HBV DNA hepatitis B
Hepatitis B LOW acute hepatitis B in
serum and liver
viral replication and infectivity
Often silently progressive
Anti-HCV by ELISA
Diagnostic
Frequent cause of HCV RNA
Hepatitis C cyroglobulinemia Anti-HCV RIBA
Antibody Levels Rise slowly
Anti-HDV
Requires coinfection with
Hepatitis D hepatitis B
Worsening hepatitis B ↑ Risk for liver cancer
HDV RNA
POSITIVE
Acute hepatitis after Pregnancy
travel to endemic area (10 - 20% mortality rate)
Generally benign and self-
Hepatitis E limiting More severe in patients with underlying chronic
Anti-HEV POSITIVE
liver disease
Acute Hepatitis Assessment of a patient with
Hep C virus antibody Hep B core IgM antibody
acute hepatitis symptoms
Panel Hep B surface antigen Hepatitis A IgM antibody
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Diagnostic Methods
Test Interpretation
Diagnostic Test Measures Indications Other
Result Parameters
Calcifications Foreign bodies
Use of X-rays to view a non-
Radiograph uniformly composed object Free air Obstruction
Fluoroscopy with Use of X-rays to obtain real-
time moving images of Transit times Mucosal abnormalities
Barium internal structures
Enteroscopy
Need to biopsy lesions Any GI disease
"Push" endoscopy of small bowel
Perforation
Gastrointestinal Direct visualization of the Bleeding
Infection
Endoscopy GI tract Risks Cardiopulmonary
complications 2⁰ to
sedation
Death
Dysphagia Odynophagia
Screening for Barrett's
Refractory GERD
esophagus
PUD Upper GI bleeding
Direct visualization of Treatment of varices /
Esophagogastro- Malabsorption
bleeding
esophagus, stomach, and Dilation of esophageal Rupture of esophageal
duodenenoscopy duodenum strictures webs
Removal of polyps /
Stent placement
neoplasms
Radiofrequency ablation
Flexible Visualization descending
colon, sigmoid colon, and Inflammatory diarrhea
Need a view of the distal
colon only
Sigmoidoscopy rectum
Colorectal cancer Requires sedation
Anemia evaluation
Visualization of entire colon screening
Colonoscopy and portion of terminal ileum Bleeding Assesment of IBD
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Diagnostic Methods
Test Interpretation
Diagnostic Test Measures Indications Other
Result Parameters
Pancreatic cancer Choledocholithiasis
Endoscopic Combines the use of Malignant and benign Sphincter of Oddi
endoscopy and fluoroscopy biliary strictures dysfunction
Retrograde Recurrent acute /
to diagnose and treat certain chronic pancreatitis
Pancreatic malignancies
Cholangio- biliary and pancreatic ductal Ampullary adenomas Stone extraction
pancreatography diseases Sphincterotomy Stent placement
Stricture dilation Drain fluid
Biopsy
Staging of rectal,
Endoscopic Ultrasound on an
esophageal, and gastric
tumors Identification of
endoscope pancreatic tumors
Ultrasound Aspiration biopsies
Gold-standard for visualizing small
Tumors Obscure bleeding
bowel
Refractory Avoid in patients with GI distress,
Survey in polyposis
Video Capsule Pill-sized cameras travel
the GI tract and capture
syndromes
malabsorption
syndromes
fistulas, pregnancy, or swallowing
disorders
Endoscopy video
Uncertain diagnosis of Crohn's disease
Varices
Screening GERD complications
Esophagitis
Requires general anesthesia (can take
Double Balloon Allow visualization of entire
Allows procedures (when compared to VCE)
3 hours)
small bowel in most patients Two balloons are attached to distal
Endoscopy end of the enteroscope
High-Resolution
Magnifiable endoscopy Flat lesions Barrett's esophagus
Endoscopy
Dyes / stains applied to tissue to
Chromoendoscopy enhance location and diagnosis of Occult lesions
lesions
Narrow Band Enhances mucosal
Neoplasia Adenoma
morphology and vascularity
Imaging
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Diagnostic Methods
Test Interpretation
Diagnostic Test Measures Indications Other
Result Parameters
Uses short light wave source
Autofluorescence to exploit natural tissue
fluorescence
Transabdominal Ultrasound through the Liver disease
Biliary disease
Ultrasound abdominal wall Pediatric appendicitis
Radionuclide Tagged (technitum-99m) red
blood cells to detect obscure Gastrointestinal bleed
Imaging bleeding
Use of Tc-iminodiacetic acid
Cholescintigraphy (IDA) to visualize the Cystic duct obstruction by gall stone
gallbladder
Trauma Unexplained pain
Infectious /
Computerized Computer-processed x-rays
produce tomographic images
inflammatory lesions
Pancreatitis
Obstruction Liver malignancies
Topography of specific areas in an object
Pancreas malignancies
Strong magnetic fields and
Magnetic Resonance
radiowaves are used to form Liver lesions Biliary tract lesions
Imaging images of the body
CT / MR Use of contrast to
Mucosal abnormalities
Enterography distend small bowel
Low specificity and sensitivity (but
Virtual Computer-assisted high-resolution
two-dimensional image of abdomen / Colon cancer screening
being constantly improved)
Requires prep and rectal tube
Colonoscopy pelvis generated by spiral CT
Contraindications
Abnormal LFTs Suspected neoplasm ↑ PT
Thrombocytopenia
Ascites
Confirmation of
Evaluation of Difficult body habitus
Histologic analysis of diagnosis /
Liver Biopsy hepatic tissue prognostication
granulomatous disease Suspected hemangioma
Complications
RUQ, brief pain
Unexplained jaundice or Management of post- Bleeding
suspected drug reaction transplantation care Biliary peritonitis
Bacteremia
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Diagnostic Methods
Test Interpretation
Diagnostic Test Measures Indications Other
Result Parameters
The oxidation of guaiac by hydrogen
perioxide causes blue color when
Fecal Occult Qualitiative method of
determine the presence Cancer GI bleeding
exposed to "heme" found in stool
Sensa FOBT
Enhancer that allows greater
Blood Testing of blood in stool sensitivity and ease of interpretation
Requires 3 serial stools
Hemoccult Sensa Part of the screening for
↑ Risk of colon cancer
Avoid NSAIDs or aspirin prior to or
colon cancer during specimen collection
Screening
False Positives Specimens innoculated onto card ≥ 3
Red meats Aspirin days (ideally) prior to development
Hemoccult Method for detecting
NSAIDs
Other drugs
Alcohol in excess
Iodine preparation
For immediate results, wait at least 3 -
5 minutes before development
non-visible blood in stool False Negatives
Sensa Testing Ascorbic acid ↑ Citrus fruit / juice
> 250 mg/day intake
Iron supplements
Norovirus Bacterial stool culture re not
Rotavirus routinely gram stained due to futility.
CMV* Entamoeba histolytica causes
ETEC attacking WBC rupture, and fecal
EHEC leukocytes may not be seen.
NEGATIVE
Microorganism Giardia lamblia
Bowel infection
overgrowth Entamoeba histolytica*
Crytosporidium
S. aureus
Fecal WBCs in stool
C. perfringens
Salmonella
Yersinia
Leukocytes Variable Vibrio parahemo.
C. difficile
Aeromonas
Shigella
Camplyobacter
Inflammatory bowel disorders
EIEC
POSITIVE Ulceraive colitis
Crohn's disease
Radiation colitis
Ischemic colitis
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Diagnostic Methods
Test Interpretation
Diagnostic Test Measures Indications Other
Result Parameters
Clostridium Predominant causative
enterotoxin for Diarrhea Recent antibiotic use ELISA
93 - 100% specific
Difficile Toxin pseudomembranous colitis 63 - 99% specific
Rarely performed
Gold-standard test for
Tissue Culture C. difficile infection
Pseudomemberanous colitis
Fresh stool to lab < 2
Salmonella Shigella
hours
Bacterial Stool Identification of bacteria Campylobacter
Acceptable
Preserved in Cary-Blair
medium < 96 hours
in stool Vibrio
Cultures Require a Special
Request for
Aeromonas
Yersinia Rejected Hospitalized > 3 days
Indentification
E. coli O157:H7
Animal contact Children at daycare
Fecal Acid-Fast Acid-fast stain of stool Immunocompromised "Ghost" Cells Cyclospora oocytes
Stain Cryptosporidium parvum Cyclospora cayetanensis
Superior sensitivity and equal
Use of fluorescent monoclonal
IFA Indirect Immuno- specificity to O&P if performed < 1
antibodies to identify Giardia lamblia Cryptosporidium parvum
hour
Fluorescence Assay microorganisms
H. Pylori Serologic Gastritis
Antibodies can persist for years
Detects either IgG or IgA to Active / past H. pylori 50% of adults > 60 years old are
Enzyme-Linked Helicobacter pylori infection positive
Peptic ulcers
Immunoassay
Excellent sensitivity and specificity
Urea Breath Radioactively labeled CO2 (by
ingesting radioactive 13C urea) is H. pylori infection
Non-invasive test of choice to
document successful treatment of H.
Test exhaled and detected
pylori
Sensitivity 93%
Rotavirus EIA Detection of rotavirus Gastroenteritis
Specificity 96%
Detection of norovirus that is Nursing homes
Norovirus PCR only performed for
Cruise ships
Long-term care facilities
epidemiologic reasons
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Diagnostic Methods
Test Interpretation
Diagnostic Test Measures Indications Other
Result Parameters
Quantitative Stool Fat Test
Malabsorption disorders Celiac / tropical sprue Gold-standard
↑ Fat diet for 2 days before and
Measures amount of fat during collection
Fecal Fat present in stools Whipple's disease
Zolinger-Ellison
syndrome
Qualitative Stool Fat Test
Sudan stain of stool sample and
microscopic evaluation
Crohn's disease
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Causes
Functional Common GI disorders Atypical chest pain IBS Altered gut motility
Exaggerated visceral responses to
Abdominal without discernable noxious stimuli
cause Dyspepsia Altered processing of visceral stimuli
Disorders Diagnoses of exclusion
Dyspepsia
Abdominal Pain
Diverticulitis
Diarrhea
Gastrointestinal Any disease of the Altered Bowel Habits
Constipation
gastrointestinal system Nausea ± vomiting Bleeding
Disease Pyrosis Dysphagia
Odynophagia Early satiety
Jaundice Anorectal symptoms
Visceral Abdominal Pain
Acute Etiologies
Poorly localized
Acute pancreatitis Acute cholecystitis Produced by dermatome
Pain as a result from Acute appendicities Diverticulitis Somatic Abdominal Pain
Abdominal complex interaction of Intestinal ischemia PUD Well localized
Bowel obstruction Infectious diarrhea Initiated by pain receptors in parietal
sensory receptors in the Incarcerated hernia Gynecological causes peritoneum
Pain GI tract, spinal cord Chronic Etiologies
Referred Abdominal Pain
nuclei, and CNS Poorly localized
GERD Non-ulcer dyspepsia Felt in areas that may be remote
IBS IBD from disease site
Chronic pancreatitis Infectious diarrhea
Only patients with chronic symptoms
require management
> 55 years old OR
Painful, difficult, or Endoscopy
Dyspepsia disturbed digestion
Pain Discomfort alarm symptoms
Test and treat for
Non-Endoscopic
H. pylori
Indicated Patients
Initiate trial of PPI
Risk Factors
Group of disease that are
Diverticular characterized by pouch
Diverticulosis Diverticulitis
↓ Low fiber diet
Red meat
formation in the weak spots Obesity
Disease in the colonic wall ↑ Age
LLQ pain Leukocytosis with Co-morbidities increase the
Suprapubic pain CBC Clear liquids
± palpable mass left shift likelihood of severity.
May present as an acute Gold-standard Complications
"Left-sided" appendicitis 7 - 10 days of antibotics
Inflammation of colonic GI bleed CT Assess disease Ciprofloxacin + Bleeding
Diverticulitis diverticula Fever Malaise severity
Close follow-up
Metronidazole Intra-abdominal abscesses
Constipation Diarrhea Free air Fistulas
Nausea Vomiting X-Ray Ileus Surgical consult Obstruction
Dysuria ↑ Urinary frequency Obstruction (if not improved in 72 hours)
Infrequent stools Difficult-to-pass stools CBC R/O Underlying causes Rome Criteria (> ¼ of defecations)
Functional defecation Sense of incomplete
Abdominal distention
TSH Laxatives
Lubiprostone
Straining
evacuation BMP Medical therapy Lumpy or hard stools
disorder due to slowed
Bloating Pain Colon Transit ↑ Fiber diet (≈ 30 g / day) Sense of incomplete evacuation
Constipation transit through the colon, Etiologies Study
Evaluation
Adequate hydration Sense of anorectal obstruction
obstruction, or irritable Functional Drugs Anorectal Regular exercise Manual maneuvers
Prokinetic Agents
bowel syndrome Endocrine / metabolic Neurologic Manometry Bowel training And/or < 3 defecations and no loose
Structural lesions Colonoscopy Digital disimpaction stools
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Acute Etiologies
Appendicitis Cholecystitis
Nausea and Sensation and action of Pancreatitis Peritonitis
ejecting stomach Small or large bowel obstruction
Vomiting contents Chronic Etiologies
Esophageal disorders Gastric malignancy
PUD
Difficulty swallowing Etiology can be outside the GI tract.
Motility Disorders
both liquids and solids
Dysphagia Difficult swallowing
Mechanical Disorders
Difficulty swallowing
solids
Etiologies
Pill-induced esophagitis
Painful swallowing due to AIDS
Infection Immunosuppressive
Odynophagia the inflammation of disease
esophageal mucosa Ingestion of caustic substances
Doxycycline
Medications
Tetracycline
EGD
Exposure of esophageal Barium
Studies
epithelium to gastric acid
Pyrosis causes a burning
Heartburn Esophageal
Manometry
Diagnostic
sensation 24 Hour
Esophageal
Probes
Malignancy (especially in older patients)
Delayed gastric
emptying
Gastric outlet
obstruction caused by
Early Satiety Decreased appetite Non-Malignant
Etiologies
PUD
Adhesions of small
bowel obstruction
Small bowel obstruction
of Crohn's disease
Systemic Illness Tomatoes, citrus foods and
Diabetes Malignancies Exquisite hygiene beverages, and caffienated drinks can
Thyroid disease cause pruritus ani.
Mechanical Triggers / Irritants Xylocaine
Diarrhea / constipation Soaps Remove offending agents
Anorectal lesions Wipes
Irritation of the skin at
Pruritus Ani the exit of the rectum
Tight-fitting clothes Over-cleansing
Dermatologic Conditions
Mild topical steroids
(1% hydrocortisone)
Atopic dermatitis Lichen planus
Psoriasis Antihistamines
Pramoxine
Infections
Intertrigo HPV / HSV
Antipruritics
Scabies Pinworms
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Stool softeners Posterior anal fissures are the more
Tenderness Bleed easily Protective ointments common form, followed by anterior.
Split, tear, or erosion in Sitz baths
Topical steroids
Anal Fissure the epithelium of anal Pain
Nitroglycerin 2% ointment
canal Large or hard-to-pass Botulinum toxin
Etiologies stools Surgical referral
Trauma (rarely) (if fissure fails to heal)
Pain treatment
Venous edema in the Painless bleeding after defectation Topical steroids
Internal Rubber band
anus that breaches the ligation
Hemorrhoid anal wall Visible with anoscopy
For Prolapse
Infrared
coagulation
Sitz baths Recovery is often prolonged
External Increased venous pressure
within the external
Rarely bleed Painful
Topical steroids compared to internal hemorrhoids.
Stool softeners
Hemorrhoid hemorrhoidal veins Readily seen on perianal exam
Removal of clot (if thrombosed)
< 50 3.5 g NaCl 2 million deaths / year worldwide
Usually self-limited and last less than one day Stool Anion (secretory) 1.5 g KCl
Reversal of the normal Loperamide
Gap > 125 20 g glucose
Oral Rehydration
net absorptive status of Dehydration (osmotic)
Solution Optional 2.5 g
Monitor Symptoms For… Duration Persistent or
water and electrolytes Inflammation recurring
sodium bicarb
Bismuth
that results in water Stool Studies History of fever or
Diarrhea secretion into the gut and
Warning Signs
Indications tenesmus
1 L water
Bananas
Subsalicylate
Other warning Rice
enhanced anion Severe abdominal pain
Hopsitalized patients /
signs exist
BRAT Diet
Applesause
recent antibiotic use
secretion from Fecal
73% sensitive
Toast
Systemic illness with Leukocytes in Lomotil
enterocytes In elderly (> 70 years
diarrhea (especially in Inflam. Avoid milk products
old) or in I-C patients 84% specificity
pregnant) Diarrhea
Bloody Diarrhea (MESSY CACA) Enteropathogens Tracked by CDC
Medical disease E. coli E. coli
Shigella Salmonella Salmonella
Diarrheal medications
Yersinia Campylobacter Shigella
(except with Shigella, C. difficilie, and
Amoeba C. difficile Y. enterocolitica, Vibro histolytica /
E. coli O157)
(E. histolytica) Aeromonas cholera, Listeria, Cyclospora
Infectious Diarrhea caused by a
Watery Diarrhea
Rotavirus
Campylobacter
Cryptosporidium
pathogen Viral Norovirus
Diarrhea Adenovirus
S. aureus
Bacterial B. cereus
Antibiotic therapy
Vibrio
Giardia
Parastic Cryptosporidia
E. histolytica
Transmission
Diarrhea Abdominal pain
Fecal-oral
Inflammation of the Familial outbreaks Person-to-person
Viral Noroviruses / Norwalk
Nursing homes Contaminated foods
gastrointestinal tract due Virus
Cruise ships Most common in the US during the
Gastroenteritis to viral infection Rotaviruses
Highly contagious winter months
Vaccine available
Adenovirus Year-round
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Nausea 20,000 cases / year in US
Foul-smelling watery
Flagellated protozoa diarrhea
Cramps
50% rate of spontaneous resolution
Giardia associated water
transmission in
Life Cycles
Flatulence
Giardia
Antigen Stool POSITIVE
Cysts are ingested
Lamblia contaminated streams, day Gastric acid releases trophozoites into duodenum
Testing
Metronidazole treatment
care centers, or well water and jejunum
Attachment to villi
Abdominal pain Cramping More common in tropical and
Entamoeba Anaerobic parastic protozoan that
causes necrosis of the large Colitis
Diarrhea Metronidazole treatment subtropical regions
(may be bloody) (even if asymptomatic)
Histolytica intestine
Travelers Homosexual
Infectious diarrhea that does Many of these organisms are present
Cyclospora Isospora Albendazole
Parastic Diarrhea in the HIV with CD4 in the environment and water supply.
not usually affect normal Count
< 100 Antiprotozoal treatment
Immunocompromised hosts Cryptosporidium Microsporidia TMP / SMX
Watery diarrhea Abdominal cramping Patients with liver disease and iron
Vibrio Symptoms no more than 3 days after seafood or
No treatment necessary Deoxycycline
overload states are more
Gram negative rods contaminated water ingestion susceptible.
Parahaemolyticus Wound infection
Antibiotics (if required) Floroquinolone
12 - 24 hour incubation
Gram negative rod that 50% mortality if untreated
Abdominal cramping Rice-water stools Oral rehydration solution
Toxins have a dose effect.
Vibrio Cholera activates adenylate cyclase Hypotension Single-dose fluoroquinilone /
enzyme in intestinal cells (< 2 hours due to severe diarrhea) doxycycline
Mild or severe Incubation is dependent on whether
Hemorrhagic colitis
Gram negative rod that is symptoms
Supportative care
the organism is toxin-producing or
E. Coli tranmitted through
undercooked beef,
Severe abdominal pain Bloody diarrhea
not.
Associated with warm weather
No fever (usually) 20,000 cases / year in US
O157:H7 unpasteurized juices (apple
ciders), or spinach
Hemolytic Uremic Syndrome
Acute renal failure Microangiopathic
Antibiotics are not beneficial
No anti-motility medications
Thrombocytopenia hemolytic anemia
Traveler's Microbial contamination of
food and water usually by Watery diarrhea
History of travel in Antibiotic therapy
Cirpofloxacin
less-developed areas (may decrease the duration of illness)
Diarrhea enter-toxigenic E. coli Rifaximin
Diarrhea Fever Associations
(maybe bloody) Myalgia Incidence is higher in children < 5
Gram negative rod that is Abdominal cramping Headache years old and adults > 60 years old.
one of the most common Diseases is worse in old, young, and
Salmonella causes of infectious
Septicemia / bacteremia
(2 - 14%)
Osteomyelitis
(10%)
Ciprofloxacin (in severe cases)
immunosuppressed.
diarrhea Endocarditis Arthritis
(10%) (10%)
Pulse-temperature 10 - 14 days after Vaccine for travelers
Samonella Gram negative rod that
discordance
Fever
ingestion
Headaches
Ciprofloxacin for 10 days
Asymptomatic carrier state is
possible.
causes typhoid fever Bacteria will pass through cells lining
Typhi Myalgia Malaise
the small intesting and go to liver,
Anorexia spleen, and bone marrow.
Lower abdominal Diarrhea Children are prone to infection.
Gram negative rod cramps Fever Floroquinolone No anti-motility medications
associated with day
Shigella cares, nurseries, and long-
Bloody, purulent stools Tenesmus Antibiotic therapy
1 - 3 days after ingestion TMP/SMX
term care Usually self-limited to < 7 days
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Diarrhea Fever Systemic disease with high mortality.
Gram negative rod
Yersinia acquired after ingestion Abdominal pain
Symptoms for
1 - 2 weeks
No treatment is indicated
Doxycycline
of contaminated food Chronic form can Can mimic
Enterocolitica (pork) or water
last months Crohn's disease Antibiotic treatment (if severly ill)
Lymphadenopathy
Associations
Dysentery
Self-limiting but may last Guillain-Barre Syndrome
Azithromycin
Gram negative rod that is > 1 week (ascending paralysis)
Campylobacter Bacteremia
Reactive arthritis
a very common cause of Contaminated food,
Antibiotic treatment
Up to 1 week incubation period
Jejuni infectious diarrhea Transmission
water, or milk
Fluoroquinolone
Animal contact
(½ from chickens)
75% sensitivity Alcohol foam does not kill the spores.
Spore-forming, Gram positive Diarrhea from hell Flagyl
Clostridium rods that are the most Clindamycin
EIA Testing for Need 3 (-) tests to
Toxins A and B rule out Oral vancomycin
No anti-motility medications
common cause of Fluoroquinolones Highly specific (severe disease or refractory)
Difficile nosocomial diarrhea
Antibiotic-Induced
PCN
PCR
> 99% sensitivity
Fidaxomicin
Cephalosporins Highly specific
Pre-formed toxin Symptoms < 4 hours
Food contact with
Staphococcus infected skin or human
Gram positive cocci carrier
Aureus Transmission Potato salad
Meats
Custard-filled pastries
Ice cream
1 - 6 hour incubation Refrigeration prevents germination
(emetic form) of spores.
Pre-formed toxin
> 6 hour incubation
Bacillus Cereus Gram positive rods (diarrheal illness)
Fried rice
Transmission Meats
Sauces
Abdominal cramping Watery diarrhea
Clostridium Gram positive rods
No fever, nausea, or
vomiting
Symptoms last
< 24 hours Heat Labile
POSITIVE
Pigbell (rare) Toxin
Perfringens Transmission
Meats
Poultry
2♂:1♀
≈ 55 years old
Reflux Screening and surveillance Whites > hispanics
(at diagnosis)
Barrett's Intestinal metaplasia of Pathogenesis Endoscopic
Diagnostic
the esophagus Chronic gastroesophageal reflux Biospy Endoscopic ablation therapy
Esophagus Reflux esophagitis
Squamous epithelial injury
Esophagectomy
Intestinal metaplasia
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Type and extent of Symptom onset in ages > 50 warrants
Regurgitation PPI (empirical)
tissue damage further investigation
Heatburn Upper
Normal in ½ cases Etiologies
(30 - 60 minutes after Sour brash Endoscopy
Does not detect Lifestyle modifications Incompetent lower esophageal
meals)
mild disease sphincter
Dysphagia
Detects strictures, Prokinetics TLESR
ulceration, and H2RA Irritant effects of refluxate
Chronic symptom of Extraesophageal / Atypical Symptoms
Barium abnormal folds Medical Antacids Delayed gastric emptying
mucosal damage caused Radiography Reveals abnormal Treatment Mucosal Abnormal esophageal clearance
Gastroesophageal Asthma Cough
motility or protectants Scleroderma
by stomach acid coming clearance TLESR inhibitors
Reflux Disease up from the stomach into Non-cardiac chest pain Laryngitis
Ambulatory Detects pathologic
pH Testing acid reflux Nissen fundoplication
the esophagus Hoarseness Loss of dental enamel
Function of
Symptoms > 10
Complicated Disease / Alarm Symptoms esophageal
years
muscle
Manometry Barrett's
Dysphagia Weight loss contractions and Age > 50
Screening EGD
esophageal
Hematemesis Melena sphincters White ♂
Common Etiologies
Infectious Inflammation of the Odynophagia Candida
EGD with CMV
esophagus due to Dysphagia
Biopsies
Diagnostic
Herpes simplex
Esophagitis infection Chest pain HIV idiopathic ulceration
Recurs in 60 - 90% of patients 3 - 6
Internal diameter < 13 mm Dilation
Narrowing of the lower years after dilation
Schatzki's Ring part of the esophagus GERD symptoms PPIs
Cervical web
Plummer-Vinson
Dysphagia
Syndrome
Esophageal Thin membranes in the
Iron-deficient anemia
Etiologies
Correct iron-deficiency anemia
esophagus Congenital Bullous pephigoid
Web Epidermolysis bullosa Pemphigus vulgaris
Post-Barrett's ablation GVHD
Post-perforation Post-surgical
Regurgitation Dysphagia
Zenker's Outpouching of the Halitosis ♂ > 60 years old
Diverticulum upper esophagus Involves the posterior wall of the pharynx
Usually contiguous with the gastroesophageal
Narrowing of the esophagus as a Acid suppression PPIs
junction
Peptic Strictures result of healing ulcerative
esophagitis
Reflux esophagitis
Dilation H2RA
(8 - 20%)
PPIs Associations
Dysphagia
Food impaction Swallowed fluticasone Asthma
Barium
"Reflux" Abnormal Leukotriene inhibitors Allergic rhinitis
Eosinophilic infiltration of Swallow
Eosinophilic the esophagus from Strictures Mucosal rings Mast cell inhibitors / antihistamines
Urticaria
Hay fever
allergic or idiopathic Atopic dermatitis
Esophagitis etiology
Linear furrowing Ulceration
> 15 eosinophils
Endoscopic dilation
Food allergy
Histology Elimination diets Medicine allergy
"Feline" esophagus Eosinophilic abscess / HPF
Viscous budesonide suspension Higher concern for perforation with
Esophageal polyps Systemic steroids dilation
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Gradual, progressive Regurgitation of Only method
Medical treatment
dysphagia undigested foods conclusively for Nifedipine
Disease of unknown etiology
Ages 25 - 60 Symptoms are chronic diagnosis
characterized by the absence of Pneumatic dilation
Achalasia esophageal smooth muscle
peristalsis with increased tonus of
Weight loss
Substernal discomfort /
Chest pain
Poor esophageal
Manometry Complete absence
of peristalsis Surigcal myotomy
Nitrates
fullness after eating emptying
the lower esophageal sphincter Low amplitude
Nocturnal regurgitation Botulinum toxin injection Botox
waves
Simultaneous cork
Barisum screw
Esophago- contractions
Anterior chest pain Intermittent dysphagia Nitrates
Diffuse Simultaneous, graphy "Rosary bead"
appearance
nonperistaltic Intermittent,
Esophageal contractions of the simultaneous
Symptom reduction and reassurance
contractions of
Spasm esophagus Provoked by stress, large food boluses, Manometry high amplitdue
CCBs
or hot or cold liquids along with periods
of normal
peristalsis
Intermittent high
Nutcracker Esophageal movement disorder
characterized by peristaltic waves of Chest pain Manometry
pressure
Strong
Esophagus abnormally high amplitude
contractions
↓ or absent LES Most common connective tissue
Atrophy and fibrosis of the
pressure disorder involving the esophagus.
esophageal smooth muscle Severe acid reflux Dysphagia Manometry
Scleroderma common in patients with
Markedly
diminished
progressive systemic
Esophagus sclerosis, Raynaud's Strictures Erosion
Barium Markedly dilated,
Swallow flaccid esophagus
phenomena, or CREST
Staging
Mediastinal
Progressive solid food 20 - 50% 5-year Tis - Carcinoma in situ
Weight loss widening Surgery
dysphagia survival T1 - Invades lamina propria or
CXR
submucosa
Lung or bony
T2 - Invades muscularis propria
metastases Unresectable Cisplatin / 5 FU
Most present in late T3 - Invades adventitia
50 - 70 years old disease for
stages T4 - Invades adjacent structures
palliation
Radiation Nx - Cannot be assessed
Polypoid,
Esophageal Neoplasm of the Complications
Barium
Esophogram
infiltrative, or
ulcerative lesion
21% 5-year
survival
N0 - No regional nodal metastases
N1 - Regional nodal metastases
esophagus M0 - No distant metastases
Cancer Local tumor extension into the traceo-bronchial
↑ Life expectancy M1 - Distant metastases
Cisplatin / 5 FU to 33 weeks from Stage Groupings
tree
27 weeks I - T1 N0 M0
Chest CT Assessment
IIA - T2-3 N0 M0
Stenting for ChemoRad
Chest / back pain Pneumonia IIB - T1-2 N1 M0
palliation
Endoscopic III - T3 N1 M0, T4 any N M0
Endoscopic Treatment IV - Any T Any N M1
Staging Photodynamic
Hoarsness Malnutrition Ultrasound IVA - Any T Any N M1a
therapy
IVB - Any T Any N M1b
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Bloody emesis 100 new cases / 100k
Stabilize patient
Hematemesis Correlates with Etiologies of Upper GI Bleed
Sign of upper GI bleeding
severity of bleed EGD Peptic ulcer disease
at initial Colonoscopy Varices
Intraluminal blood loss Coffee Ground Emesis Old blood from stomach evaluation Determine Source NG lavage Arteriovenous malformation
of Bleeding Radionuclide Mallory Weiss tear
anywhere from the Red blood ± stool
Hematocrit
imaging Tumors and erosions
oropharynx to anus Hematochezia Bright red blood per
May take 2 days to
Angiography Dieulafoy's lesion
rectum Esophagitis
reflect the extent Treat underlying source
Aorto-enteric fistula
Dark tarry stools of bleeding
Etiologies of Lower GI Bleeding
Gastrointestinal Melena
Foul, unforgettable smell
Prevent re-bleeding
Diverticular disease
Neoplastic disease
Bleeding Resting tachycardia Orthostasis
Fluid resuscitation
Colitis
Upper GI Bleed (10% volume loss) (10 - 20% volume loss)
MCV
Normal in acute Blood transfusion Unknown
Above the ligament of Treitz Shock blood loss Discontinue all anticoagulants and anti- Angiodysplasia
(20 - 40% volume loss) platelet agents Hemorrhoids / fissures
NSAIDs
PPIs (if suspect upper bleed)
Steriods in the setting of
NSAIDs Octreotide drip
Rise out of
Lower GI Bleed Associated Medications Warfarin
BUN proportion to
Variceal Bleeds Protonix drip
Below the ligament of Treitz Heparin Antibiotics
creatinine level
Plavix Platelets (for renal disease or Plavix
Pradaxa patients)
Bleeding
PPIs
(erosion into a vessel)
Discontinuity or break in NSAIDs
Gastrointestinal Helicobacter pylori
Eradication of H. pylori (if present)
the epithelium of the GI Acid
Ulcers tract Risk Factors
Steroids with NSAIDs
Endoscopic therapy
Anti-coagulation If endoscopic Angiogram
Ethanol therapy fails… Surgery
Airway management
Octreotide
Medical
Antibiotics
Abnormally dilated vessel Treatment
Esophageal or with a tortuous course Massive upper GI bleed with hemodynamic
(for cirrhotics)
EGD with
secondary to portal instability endoscopic
Gastric Varices hypertension
banding
Intervetions
Compression with
Minnesota tube
TIPS
Dilated submucosal artery erodes
Dieulafoy's Lesion into the muscosa with subsequent Bleeding is often massive and recurrent
rupture of the vessel
80 - 90% stop bleeding spontaneously
Mallory-Weiss Laceration in the mucosa
Occurs after retching Supportative care
usually near the GE junction
Tear
Most diverticular bleeds are right-
Diverticular Rupture of an outpouching of the
mucosa and submucosa through the Acute, painless hematochezia Usually stops spontaneously
sided.
Risk of rebleed appears to increase
Bleeding muscular layer of the colon
with time.
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Diarrhea Ulcerative Colitis Descriptions of UC by Extent of
Fatigue CBC
(nocturnal or bloody) Corticosteroids Involvement
Mesalamine
5-ASA proctitis - anus / rectum
Weight loss Fever CMP
Immunomodulators proctosigmoiditis - to sigmoid colon
TNF-α inhibitors left-sided colitis - to splenic flexure
Anorexia Nausea / vomiting SED / CRP
Leukocyte trafficking inhibitors pancolitis / universal colitis - total
Workup for Sulfasalazine
Janus kinase inhibitors colon
Abdominal pain Arthralgias diarrhea
TSH with Crohn's Disease Descriptions of CD by Extent of
Erythema nodosum Reflex T4 Corticosteroids Involvement
Episcleritis Pyoderma gangrenosum Immunomodulators ileitis - ileal
6-MP
Uveitis 5-ASA ileocolitis - ileal and colonic
Celiac
TNF-α inhibitors colitis - colon only
Worrisome Signs Serologies
Leukocyte trafficking inhibitors perianal - worse prognosis
Dysplasia Use as little steroid as possible
Frequent UTIs / High fever / abdominal Small Bowel Azathioprine
Malignancy ↑ Risk for Colon Cancer in IBD
pneumaturia mass Follow-
UC Surgical Toxic colitis Colitis
Through
Differentiate CD Indications Hemorrhage Concomitant PSC
Severe abdominal pain Nausea / vomiting
Inflammatory Group of inflammatory and UC Intractable
Adalimumab
Family history of colon cacer
CT / MR symptoms ↑ Time and degree of inflammation
conditions of the colon Obstruction Severe rectal pain
Enterography Fibrotic strictures
Bowel Disease and small intestines Crohn's Disease
CD Surgical Obstruction
Indications Fistulae
Infliximab
Avoid if possible
Can affect any portion of Stool culture
Tends to skip areas DEXA
the GI tract
Lifestyle
modifications
Transmural Stricturing Osteoporosis Golimumab
Clostridium Vitamin D and
Prevention
Fistulizing difficile calcium
Minimize steriods
Ulcerative Colitis
Stool Studies Biphosphonates
Vedolizumab
Limited to the colon Starts in the rectum Ova and parasite Rule out infection
Routine labs
Usually continuous
Flare Follow-up Tofacitinib
More superficial disease
Fecal leukocytes Management
Tenesmus 5-ASA (UC) or
or fecal
budesonide (CD)
calprotectin Methotrexate
Fecal urgency Hematochezia
Anti-TNF
Alkaline High-risk for colon cancer
Primary Stricturing of the bile Phosphate
HIGH
No effective medical therapy
LFTs
Sclerosing ducts with risk for Asymptomatic Itching
p-ANCA
Diagnostic
cholangitis Hepatologist referral
Cholangitis MRCP / ERCP
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
H. pylori Eradication 500k new cases / year
Burning pain localized to PPIs
Pain in non-radiating H. Pylori PPI 4 million recurrences / year
the epigastrium Triple Therapy for
Serology False Clarithromycin > 80% prev. in developed nations
Antibiotics 2 Weeks
Asymptomatic Negatives Amoxicillin
Nighttime awakenings
(30 - 40% of NSAID users Bismuth
from pain Confirmation of eradication
with ulcers) Allows
characterization of
COPD EGD May require retreatment in 20%
the lesion and
biopsy
Cirrhosis Antacids
Associations GI bleeding
Peptic Ulcer Breach in the mucosa of Systemic mastocytosis H2 blockers
Unintended
the stomach that leads to weight loss
Disease ulcer formation Uremia
Family Hx of GI
PPIs
Age > 65 Gastrectomy
malignancy Surgery (rare)
Higher dose NSAIDs Vagotomy
High-Risk Patients for Indications for
Corticosteroids
NSAID Damage EGD Odynophagia Preventing Complications of NSAIDs
Anticoagulants
H. pylori infection
Dysphagia Cox-2 selective therapy
Complications
Misoprostol
Iron deficiency
Mucosal PPI
Hemorrhage Perforation
Protection High-dose H2
Age > 55
Gastric outlet obstruction blockers
Gastrinoma Triangle (90%)
PUD High-dose PPI
Fasting Serum Pancreas ductular epithelium (50%)
(majority in duodenal Diarrhea > 1000 pg/mL
Gastrin Surgical resection Duodenum (40%)
bulb)
(if not metastatic) Stomach, liver, bones, and LN (<10%)
Zollinger- Indications to Check Serum Gastrin
Secretin Most sensitive
Vagotomy
30 - 50% metastasize
83% 15-year survival without
Tumor of gastrin- Ulcers in distal Stimulation (94%) and specific Somatostatin metastasis
Ellison secreting G cells
Multiple ulcers
duodenum and jejunum Test (100%) analogs 30% 10-year survival with metastasis
Interferon α
Syndrome Ulcers associated with severe esophagitis
Endoscopic Metastatic Cytotoxic
Extensive family history Ulcer resistant to Ultrasound Disease chemotherapy
of PUD medical treatment and Successful in 90% Surgical resection
Unexplained diarrhea Somatostatin Chemo-
Post-op ulcer recurrence
Hypercalcemia Receptor embolization
Typically found at the gastric fundus
Stress-Induced Ulcers due to multifactorial, mucosal
ischemia due to decreased
Multiple, swallow ulcers Histamine-2 blockers
Extensive burns
Ulcers mesenteric blood flow Critically Ill
Cranial trauma
PPIs
Asymptomatic Indigestion Adenocarcinoma 2nd most common cancer with very
(early disease) Early satiety (95%) high incidence in Korea, Japan, and
Surgical resection
Nausea Anorexia Histology Carcinoid, China
Weight loss Virchow and sister Mary squamous cell ♂>♀
Palpable stomach Joseph nodes Lymphoma
Pallor Hepatomegaly Safe, easy, and Neoadjuvant chemotherapy and
Late Symptoms EGD able to obtain radiation therapy
Gastric Cancer Neoplasm of the stomach Pleural effusions GOO tissue
GE obstruction SBO Able to obtain
5-FU
Bleeding EUS tissue and good
Etiologies for staging Adjuvant
Doxorubicin
Diet H. pylori Barium Chemotherapy
Atrophic gastritis Polyps (rare) Swallow Diagnostic
Cisplatin
Radiation CT / MRI
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
10% of general population
RUQ pain after a fatty
Asymptomatic Risk Factors (5 F's, 2 C's, 2 D's)
meal
Gold-standard No treatment for asymptomatic Female, fat, fertile, age > 40, and
Types of Stones family history
Cholesterol Stones 5 F's Gallbladder Crohn's disease or cirrhosis
Cholelithiasis Gallstone (gallbladder) Drugs Ultrasound Diabetes or Drugs
Black Pigment Stones Cirrhosis
Ideally after 8
(gallbladder) Chronic hemolysis Cholecystectomy
hour fast
Brown Pigment Stones
Bile duct infection
(bile ducts)
WBC HIGH Impacted stone leads to acute
NPO
AST HIGH gallbladder inflammation and may
Fever Nausea
AP HIGH or Normal cause a secondary bacterial infection
Supportative Care IV fluids
Gallbladder
Impacted stone in the Ultrasound
1st line test
Analgesics
Cholecystitis gallbladder neck or cystic Vomiting
Severe RUQ / epigastric
If GU is (-) but still
duct pain
HIDA suspect IV antibiotics
cholecystitis
(> 6 hours)
(+) Murphy's sign Cholecystectomy (48 - 72 hours)
CT / MRI Not ideal choices
IV antibiotics
Acalculous Cholecystitis in the
Critically ill
Same labs as cholecystitis
Cholecystectomy
absence of gallstones
Cholecystitis AP HIGH Percutaneous cholecystostomy
(if too ill for surgery)
Emphysematous Type of acalculous cholecystitis
due to gallbladder infection by a See Acalculous Cholecystitis
Gallbladder Bubbles in
Emergent surgery
Ultrasound gallbladder wall
Cholecystitis gas-forming organism
Alkaline
HIGH
Intermittent RUQ discomfort similar to Phosphatase ERCP with stone extraction
Gallstone in the common bile cholelithiasis Gallbladder
Choledocholithiasis duct Ultrasound
Stone ± dilated
ducts proximal of
Cholangitis CT / MRI Cholecystectomy after ERCP
Complications stome
Pancreatitis MRCP
Fever WBC HIGH IV antibiotics Narrowing causes bile stasis proximal
Ascending Stone, occluded stent, or
Charcot's Triad RUQ pain
Jaundice
Direct
Bilirubin
HIGH
IV fluids
ERCP
to stone that leads to bile duct
infection.
stricture in bile duct Charcot's triad AP HIGH
Cholangitis Reynold's Pentad Hypotension
Blood Cultures Can be (+)
Cholecystectomy after ERCP
AMS (if stones)
LFTs
Sphincter of Oddi Stenosis or dyskinesia of
Biliary colic type of pain
Gallbladder
Diagnostic
ERCP with manometry
the sphincter of Oddi Ultrasound
Dysfunction HIDA
Sphincterotomy
AP HIGH Poor prognosis
Direct Surgery
Malignant Insidious onset of painless jaundice Bilirubin
HIGH
> 10 more likely to
Neoplasm blocks the Total Bilirubin
Biliary biliary duct
be from cancer Chemotherapy (for later stages)
Dilated duct
Obstruction (+) Courvoisier sign CT / MRI
proximal to
obstructions ERCP with stent placement (pallative)
Double duct sign
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Change in bowel CBC Luminal Phase
Weight loss
movements CMP Nutrients are hydrolyzed and
Bacterial overgrowth PT / INR solubilized
Mucosal disease TSH Helpful in Mucosal Phase
Steatorrhea
Pancreatic insufficiency Folate determining Futher processing takes place at the
Fat absorption issue B12 severity brush border of the epithelial cell
Pale Skin Anemia Lipid Panel with transfer into the cell
Petechiae Vitamin K Qualitative Transport Phase
Vitamin deficiency Stool Fat Test Nutrients are moved from the
Mouth Changes
Dental changes Quantitative epithelium to the portal venous or
Gold-standard
Stool Fat Test lymphatic circulation
Peripheral Neuropathy Vitamin B12
Abnormality in the Identifies mucosal Associated Drugs and Foods
Malabsorption absorption of nutrients Muscle Wasting /
Protein malabsorption
D-Xylose Test malabsorption Cholestyramine
Edema in SI ↑ Fiber diets
Carbohydrate Most useful for Tetracycline
Abdominal Distention
malabsorption Breath Test diagnosing lactase Antacids
Associated Clinical Syndromes deficiency Sorbitol
Lactase deficiency Giardiasis Distinguishes Fructose
Celiac disease Tropical sprue Schilling Test causes of B12 Xenical
Amyloidosis Lymphoma deficiency Metformin
Hypoparathyroidism Hyperthyroidism Colchicine
Whipple's disease Lymphoma CT / MRI / Helpful in Methotrexate
Bacterial overgrowth Short gut syndrome ERCP diagnosis Sulfasalazine
Adrenal insufficiency Carcinoid syndrome Phenytoin
Diarrhea with Anti- Common in Middle East and India
Weight loss
steatorrhea Endomysial Most specific Rare in Japan and China
Bloating IgA 10% of US American
Nutritional deficiencies
Chronic diarrhea Serology test of Gluten-Free Diet Gluten is found in wheat, rye, barley,
Flatulence Lactose intolerance choice and any foods made with these
Anti-tTGA
Nutrient deficiencies Borborygmi > 90% sensitivity grains.
> 95 specificity There is a higher incidence of
Persistent diarrhea resembling traveler's diarrhea
IgA or IgG lymphoma associated with celiac
Less sensitive
Extra-Intestinal Manifestations Antigliadin disease.
Short stature Fatigue Malignancy
May be indicated
Intestinal mucosal injury Amenorrhea ↓ Fertility Total IgA
if IgA deficient
Arthropathy Iron deficiency anemia
secondary to an immune Folate / vitamin K Osteopenia / DQ2 / DQ8
Not fully
Celiac Disease response to gluten in deficiency
Muscle atrophy
osteoporosis
Neurologic symptoms
Genetic
Screen
necessary
Other
autoimmune
genetically susceptible Dental enamel Autoimmune Gold-standard diseases
individuals hypoplasia myocarditis
Villous atrophy Complications
Definite Associated Conditions
Autoimmune thyroid
Dermatitis herpetiformis Lymphocytic Nutritional
disease
infiltration of deficiencies
Type 1 DM RA Mucosal
lamina propria
Sjögren's syndrome Down's syndrome Biopsy
Probable Associated Conditions
Crypt hyperplasia
Sarcoidosis Musculoskeletal
Congenital heart disease
Cystic fibrosis injuries and
↑ Intraepithelial
IBD deformities
Autoimmune hepatitis lymphocytes
Myasthenia gravis
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Multiple intensely Life-long condition
pruritic papules and
Skin
vesicles that occur in
Strict gluten-free diet
groups
Dermatitis Chronic blistering skin Oral (rare)
Vesicles
Erosions
condition Erythematous macules
Herpetiformis Abdominal bloating
Cramping
Dapsone therapy
Gastrointestinal Pain
Diarrhea
Constipation
Inflammatory disease of Most common in India and southeast
Extended antibiotic therapy
Asia
Tropical Sprue small bowel secondary to Diarrhea Megaloblastic anemia
Folate / B12 supplementation
Also known as bacterial overgrowth
overgrowth of coliforms syndrome
Amylase HIGH Acute intersitial pancreatitis
HIGH Mild pancreatitis with pancreatic
Abdominal pain Lipase Emergent ERCP to removed stones
More specific edema
BUN > 25 Acute necrotizing pancreatitis
(+) Gray Turner's sign
Hct > 44 Severe pancreatitis with necrosis of
parenchyma and blood vessels
(+) Cullen's sign Calcified gallstone Pancreatic rest
Complications
Abdominal "Sentinel loop ARDS, sepsis, renal failure
X-Ray of SB" Fluid collections
Etiologies
"Colon cut-off IV fluids Pancreatic necrosis (sterile)
sign" Pancreatic necrosis (infected)
Gallstones (35%) Alcohol (30%)
Enlarged Pancreatic abscess
hypoechoic Pain medications Pseudocyst
Obstruction Medications
pancreas
Ultrasound
Gallstones
Infections Metabolic
Biliary ductal
Monitor in ICU
Acute Inappropriate activation Toxins Vascular
dilation
of trypsinogen causing Modality of choice
Pancreatitis inflammation
Trauma Post-ERCP for pancreatic
parenchyma
Abdominal CT in
Inherited Idiopathic
Pancreatic 72 hours to assess
Ranson Criteria enlargement necrosis /
Admission CT Peripancreatic complications
Age > 55 WBC > 16 edema Severe
Glucose > 200 LDH > 350 Necrosis Pancreatitis
AST > 250 Extrapancreatic
48 Hours Later fluid Prophylatic
↓ Hct > 10 ↑ BUN > 5 Assesses antibiotics if
Calcium < 8 Fluid deficit > 6 L complications > 30% necrosis
PO2 < 60 Base deficit > 4 Evaluate biliary
Criteria MRCP tree and
<2 3-4 pancreatic duct
Jejunal feeds
(< 5% mortality) (15 - 20% mortality) Evaluate biliary
early
5-6 >7 ERECP tree and
(40% mortality) (> 99% mortality) pancreatic duct
Collection of pancreatic juice
Pancreatic encased by granulation tissue that
Abdominal pain Abdominal pressure Drainage (if infected)
persists > 4 weeks after episode of
Pseudocyst acute pancreatitis
Infection Rupture Surveillance
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Most acute pancreatitis does not go
Amylase Abstince from alcohol
Usually not to chronic pancreatitis.
Persistent / recurrent episodes of epigastsric and
elevated Pancreatic Tropical Chronic Pancreatitis
LUQ pain Lipase
enzymes Due to childhood malnutrition in
replacement + H2 underdeveloped countries
Fecal Fat blocker / PPI + ↓ Chronic Obstruction of Pancreatic
fat diet Duct
Pain with no radiologic
Steatorrhea Pancreatic duct strictures
evidence Narcotics
Fecal Elastase Diagnostic Pancreatic tumor
Pain Papillary stenosis
ERCP with
Secretin There are no blood tests to diagnose
sphincterotomy or
Stimulation chronic pancreatits.
stent placement
Diabetes Test
Chronic inflammatory
Chronic process leading to Abdominal
X-Ray
Pancreatic
calcifications
Celiac plexus or
splanchnic nerve
irreversible fibrosis of block
Pancreatitis pancreas Etiologies Pancreatic
Surgery
calcifications Pancreatic enzyme replacement
CT
Atrophied Insulin therapy
Chronic alcohol use Chronic obstruction of
pancreas
(70%) pancreatic duct Puestow
procedures
Subtotal
Tropical chronic Autoimmune "Chain of lakes" pancreatectomy
pancreatitis pancreatitis (areas of dilation Surgery Total
MRCP / ERCP
and stenosis along pancreatectomy
pancreatic duct) (± autologous islet
Idiopathic
Genetic cell
(20%)
transplantation)
Alkaline 4th leading cause of cancer-related
Jaundice Weight loss Whipple
Phosphatase deaths
procedure
1.3 ♂ : 1 ♀
Painless Abdominal pain Bilirubin Diagnostic (if in head)
15 - 20% of patients are candidates
(in pancreatic head) (in pancr. body / tail) Resection
for pancreatectomy.
CA 19-9 (no vascular
Distal 50% metastatic at time of diagnosis
(+) Courvoisier's sign (+) Trousseau's sign invasion,
pancreatectomy + Medial Survival
CT Double duct sign lymphatic
Signs of Metastatic Disease splenectomy Resectable - 15 - 17 months
involvement, or
(if in tail) Locally-advanced - 6 - 10 months
Sister Mary Joseph node Supraclavicular LN MRI Assessment metastasis)
Metastatic - 3 - 6 months
Lungs Liver If no lesion seen
Also get 5-FU
Peritoneum Bone Endoscopic on CT / MRI and
Pancreatic Ultrasound still have high
chemoradiation
Cancer of the pancreas Risk Factors
suspicion
Adenocarcinoma 5-FU chemoradiation
Tobacco use Chronic pancreatitis Not always (if locally advanced and not
needed if imaging resectable)
Exposure to B- Non-insulin dependent is convincing
naphthylamine or DM arising in nonobese
Gemcitabine
benzidine person > 50 years old ERCP with
Tissue
brushing +
Hereditary chronic Diagnosis
intraductal biopsy
pancreatitis Metastatic Pain control
H/O Partial gastrectomy CT-guided biopsy
Peutz-Jeghers
or cholescystectomy (risk of seeding)
EU with FNA Palliative stents
BRCA 2 mutation
(best option)
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
10% of new cancer diagnoses
Colectomy / hemicolectomy +
1 in 18 people will develop colorectal
Abdominal pain Change in bowel habit lymph node dissection
cancer.
(44%) (43%)
Colonsopy Gold-standard 19% of cases have metastatic disease
Colostomy (sometimes required) 5-FU / Leukovorin at the time of diagnosis.
/ Oxaliplatin Metastatizes most commonly to liver
and lung
Hematochezia / melena Weakness
Endoscopic removal (early stages) Staging
(40%) (20%)
T1 - Through muscularis mucosa,
extends into submucosa
Abdominal Metastatses resection
Staging T2 - Through the submucosa and into
Anemia without other GI and Pelvis CT (primarily liver)
Weight loss musclaris propria
symptoms
(6%) Radiofrequency T3 - Through the muscularis propria
(11%)
ablation and into subserosa but not to any
neighboring organs
Ethanol ablation Capecitabine
Unusual Presentations Ablation of T4 - Through the wall of the colon or
Metastases rectum and into nearby tissues and
Cryosurgery
Local invasion or CXR Diagnostic organs
malignant fistula Fever of unknown origin Hepatic artery N0 - No LN involvement
formation into adjacent embolization N1 - 1 - 3 nearby LN involvement
N2 - ≥ 4 nearby LN involvement
Resected stage II
Intra-abdominal or retroperitoneal abscesses M0 - No distant spread
Colorectal Neoplasm of the colon
Streptococcus bovis Clostridium septicum If suspected to be
Chemotherapy Resected stage III
M1 - Distant spread present
Stage Grouping
and/or rectum Needle Biopsy Metastatic / I - T1-2 N0 M0
Cancer bacteremia sepsis metastatic disease
unresectable
5-FU / Leukovorin
IIa - T3 N0 M0
IIb - T4 N0 M0
Risk Factors
Radiation therapy (rectal cancer) IIIa - T1-2 N1 M0
IIIb - T3-4 N1 M0
Personal history of colon
Age Healthy diet with IIIc - T3-4 N1 M0
polyps or cancer
emphasis on plant IV - T3-4 N2 M1
CBC
sources Radiation is not typically used for
Family history of colon cancer Maintain healthy colon cancer due to its high toxicity
BMI to the gut.
Diagnostic
Prevention FOLFIRI Colonoscopy Screening
Inherited syndromes Type II diabetes Limit red meats
Q 1 year - IBD once disease present
Encourage for > 15 years
Metabolic syndrome Ethnicity CMP
physical activity Q 3 - 5 years - Cancer or
Vitamin D / adenomatous polyps have already
Inflammatory bowel Diets ↑ red and
calcium been detected
disease processed meats
Occult blood Q 5 years - Family history of
Stool DNA colorectal cancer
Physcial inactivity Obesity
Colonoscopy Q 10 years - Everyone else
If suspected to be CT colonoscopy FOLFOX Polyps
Smoking Heavy alcohol use PET Screening
metastatic disease Flexible Some are adenomatous and some
Hereditary Non- sigmoidoscopy are hyperplastic
Familial adeomatous
Polyposis Colorectal Double-contrast Hyperplastic polyps are not
polyposis
Cancer barium enema considered pre-malignant
24 Hour Urine Arise from enterochromaffin cells
± Intermittent Surgery (localized disease)
Abdominal pain HIAA Metastatic potential of localized
obstruction
Rare neuroendocrine Chromogranin Surgery carcinoid tumors correlates with
Ileum A, B, and C Hepatic artery tumor size, location, and histologic
Carcinoid tumor that arise at
Locations in GI Tract
Rectum
Biopsy
Diagnostic
Metastatic embolization grade.
several body sites (most common first)
Appendix Disease No great evidence Appendiceal carcinoids are the most
Colon for systemic common neoplasm found in the
Imaging
Stomach therapy appendix.
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Yellowing of the oral mucosa, conjunctiva,
and skin
Jaundice Hyperbilirubinemia
Dark urine Very light stool
Bilirubin HIGH
ALT HIGH Risk Factors
RUQ pain Nausea / vomiting
AST HIGH Travelers to intermediate and ↑
Hepatitis A HAV-endemic countries
± Jaundice Acute infection
IgM Antibody Homo- / bisexual ♂
Inflammation of the liver Transmission Fecal-oral Drug users
Hepatitis A due to HAV infection Incubation Period
Average = 30 days
Prior infection
Chronic liver disease
15 - 30 days Hepatitis A ↑ Rate communities (Alaska natives
Vaccination
Fulminant hepatitis IgG Antibody and Amercian Indians)
Complications
Cholestatic hepatitis
Immunity
Chronic Sequelae None
Parenteral HbSAg Infection Prevention
Transmission Blood Prior infection Interferon Prevent perinatal HBV transmission
Body fluids HbSAb Vaccination Routine vaccination of all infants
Immunity Vaccination of adolescents
Average = 60 - 90 days Hepatologist referral
Active or prior Lamivudine Vaccination of high risk groups
Incubation Period
infection High Risk Groups
45 - 180 days HbCAb
Not positive with Houshold member of HBV-infected
Inflammation of the liver
Hepatitis B due to HBV infection 30 - 50% < 5 years old
vaccination
Active replication
Entacavir patients
Sexual parteners of HBV-infected
Chronic Infection HbEAg
2 - 10% teenagers / of virus patients
adults Chronic infection Tenofovir Health care workers
HbEAb No active Antiviral therapy Prisoners
Premature Mortality
replication Travelers to endemic areas visiting ≥
from Chronic Liver 15 - 25%
HBV DNA in Telbivudine 6 months
Disease Infection
Blood
#1 indication for liver transplant
Parental Pegylated
Present or cleared Prevention
Transmission HbCAb interferon-α + Interferon-α
infection No vaccine
Very little sexual ribavirin
Avoid sharing needles
Genotype 2 / 3
24 weeks of Use barrier protection if multiple
Average = 6 - 7 weeks
treatment Ribavirin sexual partners
Incubation Period HCV RNA HCV infection
Inflammation of the liver Treatment difficult
Hepatitis C due to HCV infection
2 - 26 weeks
to tolerate
Telaprevir Telaprevir
Predicts response
Chronic Hepatitis 70% Boceprevir
and guides
Combination with
HCV Genotype duration Genotype 1
pegylated
Boceprevir
Persistent Infection 85 - 100% interferon-α +
6 Phenotypes
ribavirin
2x ALT Calculated discriminant function (uses
Alcoholic Liver Liver damage due to
RUQ pain Nausea / vomiting
AST
Neither go above
bilirubin and INR)
heavy alcohol use 500 U/L
Disease Jaundice
History of heavy alcohol
use / binge drinking
Bilirubin HIGH
Prednisone ± pnetoxyfylline
(if DF > 32)
INR HIGH
Non-Alcoholic Chronic alcohol liver Asymptomatic Obesity ALT
Weight loss and exercise
disease without
Fatty Liver significant alcohol Diabetes /
Mildly elevated Tight glucose control
Hyperlipidemia AST Management of hyperlipidemia and
Disease consumption insulin resistance
hypertension
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Other Etiologies
Chronic Persistent / recurrent Hemochromatosis Autoimmune hepatitis
hepatitis
Hepatitis Wilson's disease α-1-antitrysin deficiency
Medication effects
Pathologic Diagnosis
Portal hypertension Ascites CBC ↓ Platelets
End result of chronic Fibrosis
Gastro-esophageal Albumin LOW Regenerated nodules
Cirrhosis inflammation from a varices
Splenomegaly
INR HIGH Vascular distortion
variety of etiologies Lack of toxin clearance Encephalopathy Bilirubin HIGH
See PowerPoints for grading of
cirrhosis.
Hematemesis Melena All patients with cirrhosis should
IV octreotide
Breached abnormally- have an upper endoscopy to look for
Bleeding Varices dilated blood vessels
Hematochezia in a patient with cirrhosis
Emergent endoscopy
β-Blockers
varices.
Hypotension Tachycardia
60% develop ≤ 10 years of cirrhosis
Check for fluid
Salt restriction (2 g / day) diagnosis
Spironolactone
Check for portal
Ultrasound
vein thrombosis Diuretic therapy
Accumulation of fluid in Shifting abdominal (with acute
Ascites the peritoneal cavity
Fluid wave
dullness accumulation)
Large volume paracentesis
Serum
Portal Furosemide
Albumin -
hypertension if
Ascities TIPS for refractory ascites
> 1.1
Albumin
CBC with Antibiotics
Abdominal pain Fever > 250 PMNs
Spontaneous Differential (3rd generation cephalosporin)
Bacterial infection of ascites Ascites
Bacterial Peritonitis Renal insufficiency
Culture
Identify organism Hold diuretics
Euphoria Confusion
R/O Infection
Asterixis Coma
Correct electrolytes
Encephalopathy Brain disease Precipitating Factors
Lactulose
Infection Bleeding
Hyponatremia Hypokalemia
Sedatives Azotemia Rifaximin
Blood transfusion TIPS
85% 1-year survival
Indications
70% 3-year survival
Replacement of a Alcohol
Liver Hepatitis C
(abstinent ≥ 6 months)
diseased liver with a PBC
Transplantation healthy liver
Cyrptogenic / NASH
PSC
Autoimmune hepatitis Hepatitis B
Most are very small.
Most common benign
Hemangioma tumor of the liver
Asymptomatic Found incidentally
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Clinical Medicine
Laboratory
Condition / Disease Cause Signs and Symptoms Treatment Medications Other
Test Result
Hepatic Liver cancer associated with
Possible rupture Bleeding Resection
long-term estrogen use
Adenoma
Focal Nodular Nonneoplastic response to a
congential vascular Asymptomatic
Hyperplasia malformation
Must be Milan Criteria for Transplant
Resection
multphasic 1 HCC < 5 cm
Chronic liver injury or cirrhosis (80%)
Cancer secondary to 3 HCCs with none that are > 3 cm
Hepatocellular Arterial phase Embolization
either viral hepatitis Imaging hypervascularity
Radiofrequency ablation
Carcinoma infection or cirrhosis Cirrhosis symptoms Delayed phase
(possibly curative)
"wash-out" Transplantation (curative)
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Pharmacology
Generic Examples /
Drug Mechanism of Action Indications Pharmacokinetics Contraindications Adverse Effects Monitoring / Other
Brand Name
Eradication: 70 - 85% GI effects Considerations
Triple Therapy for Metronidazole / PPI /
Clarithromycin
Altered taste PCN allergy
Disulfiram reaction Previous antibiotic use
Heliobacter Amoxicillin / PPI /
Kill Heliobacter pylori Peptic ulcer disease
Pill count
Side effects
Eradication Clarithromycin
Cost
Eradication: 75 - 90% GI effects Considerations
Quadruple Therapy Pepto Bismol / Metallic taste PCN allergy
Metronidazole / Disulfiram reaction Previous antibiotic use
for Heliobacter Tetracycline /
Kill Heliobacter pylori Peptic ulcer disease Triple therapy failure
Photosensitivity Pill count
Eradication Randitidine Black tongue / stools Side effects
Cost
O: 5 - 15 minutes Renal failure Fluid overload
Alka-Seltzer
Duration: 1 - 2 hours CHF Alkalosis
Peptic ulcer disease
Maalox Hypertension Diarrhea / constipation
Neutralize gastric Hypermagnesemia
Antacids Mylanta
acid Hypercalcemia
Amphojel Aluminum neurotoxicity
GERD
Drug interactions
Tums
A: Oral, IV, or IM Headache Heal 90% of DU at 8 weeks and
cimetidine
O: 30 min Nausea 80% of GU at 12 weeks.
Peptic ulcer disease Duodenal ulcer
H2 Receptor ranitidine Block histamine Duration: 10 hours Abdominal pain Cimetidine has drug
Thrombocytopenia interactions with CYP450
production in inhibitors (theophylline,
Antagonist nizatidine
parietal cells Gastric ulcer GERD
lidocaine, phenytoin, and
warfarin).
famotidine
DU maintenance A: Oral or IV CYP450 inhibitors Headache Do not cut, crush, or chew pills
Peptic ulcer disease
(lansoprazole) Adminster: 30 min (omeprazole, Zegerid, and Nausea because they are enteric-
omeprazole
Esophageal erosion before breakfast esomeprazole) Abdominal pain coated.
GERD
healing Peak: 1 - 2 hours Metabolic alkalosis Diarrhea Breakdown symptoms
Omeprazole (Zegerid = 30 min) (Zegerid) Long-Term Effects (particularly at night) can
lansoprazole Omeprazole / NaHCO3 Duration: Longer B12 / calcium dysabsorption happen while on PPI therapy
Acute Duodenal Ulcer
Lansoprazole Fractures PPIs may fail to heal moderate
Rabepazole C. difficile-associated diarrhea to severe esophagitis.
Omeprazole Pneumonia
rabeprazole
Proton Pump Inhibit active proton
Acute Gastric Ulcers Omeprazole / NaHCO3
Lansoprazole
pumps Lansoprazole
Inhibitors esomeprazole
NSAID Ulcers
Esomeprazole
Omeprazole
Lansoprazole
Heliobacter Eradication
Rabepazole
dexlansoprazole
Esomeprazole
Omeprazole
Omeprazole / NaHCO3
Esophageal Erosion
Lansoprazole
pantoprazole Maintenance
Dexlansoprazole
Rabepazole
A: Oral on empty Constipation Drug Interactions
Forms cytoprotective Duodenal ulcer healing stomach Gastric bezoar Warfarin
D: 1 g QID Aluminum accumulation Digoxin
Sucralfate Carafate complex that covers Hypophosphatemia Quinolones
ulcers Duodenal ulcer maintenance These drugs need to be
separated by ≥ 2 hours.
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Pharmacology
Generic Examples /
Drug Mechanism of Action Indications Pharmacokinetics Contraindications Adverse Effects Monitoring / Other
Brand Name
Pregnancy Diarrhea
Synthetic Abdominal cramping
Need to reduce risk for Flatulence
Misoprostol Cytotec prostglandin E1 NSAID ulcers
NSAID ulcer Nausea
analog Headache
CNS effects Modest efficacy
Blocks dopamine receptors
GERD Diarrhea
in the gut
Chemotherapy-induced Headache
Metoclopramide Reglan
Increases LES tone, gastric
nausea and vomiting Sedation
Diabetic gastroparesis EPS (especially in elderly)
tone, and transit time
Requires an IND permit from
Peripherally-acting the FDA
Domperidone Motilium
dopamine agonist
GERD
GABA agonist that Symptoms refractory to
Baclofen Lioresal
reduces tLESs
GERD
PPIs
psyllium Increase stool bulk A: Oral with ≥ 8 oz of Bowel obstruction Bloating / gas Shoud be titrated
Decrease transit time water Stricture Mechanical obstruction of colon and
Bulk Laxatives methycellulose
Increase motility
Constipation
O: 1 - 3 days Crohn's disease esophagus
polycarbophil Retain water
A: Oral Bloating
Osmotic PEG 3350 Draws water into O: 1 - 3 days Nausea
Gas
intestines along an Constipation
Cramping
Laxatives lactulose osmotic gradient (lactulose > PEG 3350)
Docusate Colace
Surfactant agent that allows
water to enter the bowel
Constipation (ineffective)
A: Oral
Patients that need to avoid straining or prevent
Sodium more readily
constipation
A: Oral Elderly Anal seepage Mineral oil and docusate are
O: 1 - 3 days Children < 6 years old Pruritus useful in same clinical situation,
Incontinence but docusate is safer.
Malabsorption of fat-soluble vitamins ↑ Risk of aspiration and lipoid
Mineral Oil Lubricant laxative Constipation
(long-term use) pneumonia if taken before bed
or in a recumbent position
A: Oral < 1 hour of antacid or milk Severe cramping
Duclolax
O: 6 - 12 hours ingestion Diarrhea
Bisacodyl Correctol
Stimulant laxative Constipation
D: Not recommended for Electrolyte imbalance
daily use
A: Oral Abdominal cramping
Ex-Lax
O: 6 - 12 hours Melanosis coli
Anthraquinones Senokot-S
Stimulant laxative Constipation
A: Oral Fluid / electrolyte depletion
magnesium hydroxide
Saline Pulls water into the O: 1 - 6 hours
D: Not for daily use
Cramping / bloating
Hypermangesemia /
magnesium citrate intestines along an Acute evacuation of stool
hyperphosphatemia
Laxatives sodium phosphate
osmotic gradient (in renal disease)
A: Oral Elderly Cramping
O: 1 - 6 hours Severe diarrhea
Castor Oil Stimulant laxative Constipation
D: Not for daily use Dehydration
Premature labor
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Pharmacology
Generic Examples /
Drug Mechanism of Action Indications Pharmacokinetics Contraindications Adverse Effects Monitoring / Other
Brand Name
A: Rectal :-( Hyperphosphatemia
Distends the rectum
Enemas and glycerin suppositories
Softens hard stool
Acute constipation O: 15 - 30 min (NaPO4 enema)
Electrolyte abnormalities
Suppositories sodium phosphate
enema
Stimulates colonic mucose Fecal impaction
contraction
A: Oral with meals Nausea (29%) Pills cannot be crushed or
Locally activates ClC-2
Bowel Movements: Diarrhea (12%) chewed.
chloride channels in the
Every 1 - 2 days Headache (11%)
microvilli cell membrane Chronic idiopathic
Lubiprostone Amitiza
Increase luminal fluid secetion
constipation
IBS constipation
Acclerate intestinal transit
Activates gyanylate A: Oral ≥ 30 minutes Children < 6 years old Diarrhea (16%)
before first meal Abdominal pain (7%)
cyclase C in the Chronic idiopathic constipation
D: 145 μg daily
interstinal epithelium
Linaclotide Linzess
Increase luminal fluid secretion
IBS constipation
Acclerate intestinal transit
loperamide Acute bacterial diarrhea Dizziness Loperamide is the drug of
Antimotility diphenoxylate / Opiate derivative that
Diarrhea
Constipation choice for most cases of
atropine slows intestinal transit diarrhea.
Agents paregoric
attapulgite Absorb toxins, Safe, but efficacy not well
established
Absorbents calcium polycarbophil
bacteria, gases, and Diarrhea
fluids
Children / teenagers with viral Black tongue and stools Less effective than loperamide
Bismuth Decrease water illness
Aspirin sensitivity
in most cases.
Drug Interactions
Pepto-Bismol secretion into the Traveler's diarrhea Diarrhea
Pregnancy Warfarin
Subsalicylate bowel Probenecid
MTX
Decrease water secretion into Diarrhea associated with Not more effective than
AIDS-related diarrhea
the bowel carcinoid tumors opioids in chronic idiopathic
Octreotide Sandostatin
Blocks release of SE and other
Short-gut syndrome
Chronic idiopathic diarrhea
peptides diarrhea
Abdominal pain Minimal efficacy
Mixture of fructose, Nausea
Diarrhea
Emetrol dextrose, and
phosphoric acid
Unknown
Vomiting
Dysglycemia (in diabetics)
Sedation Caution in…
meclizine
Anticholinergic effects Narrow-angle glaucoma
Antihistamines / dimenhydrinate
Motion sickness
BPH
diphenhydramine CV disease
Anticholinergics scopolamine
Seizure disorders
chlopromazine A: Oral, IV, IM, or rectal EPS
Nausea Vomiting
Sedation
Phenothiazines prochlorperazine Block D2 receptors
Chemotheapy-induced nausea and vomiting
Anticholinergic effects
promethazine Drug interactions
A: Oral or IV Headache Better treating vomiting than
Serotonin dolasteron Chemotheapy-induced
nausea and vomiting
Post-operative nausea
and vomiting
Dizziness nausea
granisetron Block serotonin Constipation Not as effective for motion
Receptor (5-HT3) ondansetron receptors in gut wall Radiotherapy-induced nausea and vomitting
Asthenia sickness
↑ LFTs
Antagonist palonosetron (granisteron and ondansetron)
QT prolongation (rare)
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Pharmacology
Generic Examples /
Drug Mechanism of Action Indications Pharmacokinetics Contraindications Adverse Effects Monitoring / Other
Brand Name
Increase the efficacy of other
antiemetics
Corticosteroids dexamethasone Unknown Moderately emetogenic chemotherapy
A: Oral, IV, or IM Not 1st line
Chemotheapy-induced
haloperidol
nausea and vomiting
Blocks dopamine Post-operative nausea
Butyrophenones stimulation of CTZ and vomiting
droperidol Pallative care
dronabinol Inhibits A: Oral Euphoria
Chemotherapy-induced nausea and vomiting Drowsiness
Cannabinoids nabilone
neurotransmitter (when other agents fail) Hallucination
release Paranoia
A: Oral Anamnestic effects
alprazolam
Benzodiazepines lorazepam
Enhance GABA Anticipatory nausea and vomiting
CYP3A4 substrates
Neurokinin-1 aprepitant
Inhibits substance P /
Chemotherapy-induced nausea and vomiting
CYP2C9 inducers
neurokinin 1 receptors
Antagonist fosaprepitant Post-operative nausea and vomiting
Compiled by Drew Murphy, Duke Physician Assistant Class of 2015
Antiemetics Anti-Diarrheal Agents / Laxatives
Class Generic Name Brand Name Class Generic Name Brand Name
dimenhydrinate Dramamine loperamide Imodium A-D
Antihistamine Antivert Antimotility
meclizine diphenoxylate / atropine Lomotil
Bonine
Anticholinergic Scopolamine TransdermScop Stimulant bisacodyl Dulcolax
Phenothiazine promethazine Phenergan Emollient ducosate sodium Colace
ondansetron Zofran Osmotic PEG 3350 Miralax
Serotonin Receptor
granisteron Kytril Chloride Channel
(5-HT3) Antagonist lubiprostone Amitiza
palonosetron Aloxi Activator
Guanylate Cyclase-C
Neurokinin-1 Antagonist aprepitant Emend linaclotide Linzess
Agonist
PUD / GERD
Class Generic Name Brand Name Class Generic Name Brand Name
cimetidine Tagament HB esomeprazole Nexium
Histamine H2
famotidine Pepcid lansoprazole Prevacid
Antagonist
ranitidine Zantac Prilosec
omeprazole
GI Protectant sucralfate Carafate Proton Pump Inhibitor Zegerid
rabeprazole AcipHex
Prostaglandin E1 Analog misoprostol Cytotec
pantoprazole Protonix
Prokinetic Agent metoclopramide Reglan
You might also like
- Family Medicine Shelf Review - PPTX (Read-Only)Document142 pagesFamily Medicine Shelf Review - PPTX (Read-Only)Alejandro Bocanegra Osuna58% (19)
- CASE STUDY Acute PancreatitisDocument12 pagesCASE STUDY Acute PancreatitisRichelle Sandriel C. de Castro79% (19)
- Zollinger EllisonDocument2 pagesZollinger EllisonFrama Intan MiguelNo ratings yet
- Breast MCQDocument55 pagesBreast MCQAhmad Adel Qaqour94% (16)
- Mantak Chia - Sexual AlchemyDocument2 pagesMantak Chia - Sexual AlchemyUniversal Healing Tao80% (20)
- Question Preparation Exam-1-1Document281 pagesQuestion Preparation Exam-1-1SONGA AmriNo ratings yet
- Chronic Pancreatitis: Causes ComplicationsDocument1 pageChronic Pancreatitis: Causes ComplicationsNikey LimNo ratings yet
- MS A - Mod 1 Cont Hepatobiliary and Pancreatic DisorderDocument1 pageMS A - Mod 1 Cont Hepatobiliary and Pancreatic DisorderCrisanta Grace OpondaNo ratings yet
- DRUG STUDY: Rocephin - Ceftriaxone SodiumDocument1 pageDRUG STUDY: Rocephin - Ceftriaxone SodiumYum C100% (1)
- Hepato BiliaryDocument47 pagesHepato BiliaryMikaela Ysabel CañaNo ratings yet
- Drug NameDocument4 pagesDrug Namejeyceemee0% (1)
- Pancreatiti S Aguda: Catedra: Docente: EstudianteDocument35 pagesPancreatiti S Aguda: Catedra: Docente: EstudianteMaybelline Ruiz ReyesNo ratings yet
- Omeprazole (FSW)Document3 pagesOmeprazole (FSW)khelxoNo ratings yet
- Acute Chronic PancreatitisDocument17 pagesAcute Chronic Pancreatitisjimjose antonyNo ratings yet
- PathyDocument3 pagesPathyTRIXY MAE HORTILLANO100% (1)
- Disorders of PancreasDocument43 pagesDisorders of Pancreasindu mathiNo ratings yet
- Neuro TumoresDocument14 pagesNeuro TumoresCarlos SotoNo ratings yet
- Acute PancreatitisDocument31 pagesAcute PancreatitisAmoroso, Marian Corneth D.No ratings yet
- Enzymes in Clinical DiagnosisDocument2 pagesEnzymes in Clinical DiagnosisShobe ChuaNo ratings yet
- Cefoxitin, Metronidazole, RanitidineDocument2 pagesCefoxitin, Metronidazole, RanitidineDaryl PaglinawanNo ratings yet
- Drug Study (Med Ward Duty)Document6 pagesDrug Study (Med Ward Duty)Kimberly Abellar LatoNo ratings yet
- Revised Concept MapDocument1 pageRevised Concept MapCathryn luv QuisidoNo ratings yet
- Case Pre Drug StudyDocument22 pagesCase Pre Drug StudyBenjie DimayacyacNo ratings yet
- Acute PancreatitisDocument8 pagesAcute PancreatitisAthan AntonioNo ratings yet
- Complications: Acute PancreatitisDocument2 pagesComplications: Acute PancreatitisNikey LimNo ratings yet
- Pancreas RobbinsDocument13 pagesPancreas RobbinsAndrea PescosolidoNo ratings yet
- DRUG STUDY: Amoxicillin - AmoxilDocument1 pageDRUG STUDY: Amoxicillin - AmoxilYum CNo ratings yet
- Acute Pancreatic RGB 2023Document16 pagesAcute Pancreatic RGB 2023NohemaVMNo ratings yet
- NUR 3032 Pancreatic, Biliary, and Hepatic Disorders Study PlanDocument6 pagesNUR 3032 Pancreatic, Biliary, and Hepatic Disorders Study PlanThalia FortuneNo ratings yet
- Drug Ana Pedia WardDocument2 pagesDrug Ana Pedia WardMark Christian CuiNo ratings yet
- PEDIA GastroDocument20 pagesPEDIA GastroJoanna :DNo ratings yet
- Pendekatan Dan Diagnosis DispepsiaDocument16 pagesPendekatan Dan Diagnosis DispepsiaJual Beli PromosiNo ratings yet
- Pathophysiology of GastroenteritisDocument1 pagePathophysiology of GastroenteritisNathaniel SupanNo ratings yet
- Drugs Classification / Indication Dose/Route/ Frequency Action Contratindication Adverse Reaction Nursing ConsiderationDocument3 pagesDrugs Classification / Indication Dose/Route/ Frequency Action Contratindication Adverse Reaction Nursing ConsiderationnealantonetteNo ratings yet
- Gastrointestinal and Hepatobiliary SystemDocument11 pagesGastrointestinal and Hepatobiliary SystemRhealyn LegaspiNo ratings yet
- Patofisiologi Tumor KolonDocument2 pagesPatofisiologi Tumor Kolonnur hijriahNo ratings yet
- 66 - Prevention and Early Detection of CancersDocument1 page66 - Prevention and Early Detection of CancersRica Alyssa PepitoNo ratings yet
- Ketorolac DRUG STUDYDocument3 pagesKetorolac DRUG STUDYA.No ratings yet
- PancreATITIS OCT. 21, 2021Document33 pagesPancreATITIS OCT. 21, 2021Alyssa NicoleNo ratings yet
- m1 Kamad Ds RanitidineDocument2 pagesm1 Kamad Ds Ranitidinekkd nyleNo ratings yet
- بدور قاسم كطامي تقرير انسجةDocument21 pagesبدور قاسم كطامي تقرير انسجةnawarNo ratings yet
- Drug Study (Ranitidine, Citicoline, Enalapril, Aspilet, Cefuroxime Etc)Document9 pagesDrug Study (Ranitidine, Citicoline, Enalapril, Aspilet, Cefuroxime Etc)gino_23_28No ratings yet
- Drug StudyDocument2 pagesDrug StudyKeiNo ratings yet
- Valstar Drug StudyDocument2 pagesValstar Drug StudyNathalie kate petallarNo ratings yet
- Pancreatitis Group 3 NCM 116Document21 pagesPancreatitis Group 3 NCM 116Diana Jane LauretaNo ratings yet
- Pancreatitis & Pseudocyst in ChildrenDocument56 pagesPancreatitis & Pseudocyst in ChildrendrkiranmNo ratings yet
- Omeprazole Drug StudyDocument4 pagesOmeprazole Drug StudyjoanneNo ratings yet
- Colorect: Patient's Name: F.V Age: 64 Years OldDocument3 pagesColorect: Patient's Name: F.V Age: 64 Years OldGenynne Ragasa100% (1)
- Pathophysiology of CushingDocument3 pagesPathophysiology of CushingAj MacotoNo ratings yet
- Cholelithiasis CholecystitisDocument1 pageCholelithiasis Cholecystitissamliebareng77No ratings yet
- Drugn Study 2 0Document15 pagesDrugn Study 2 0Ken ChavezNo ratings yet
- BurgerDocument4 pagesBurgerHungry Aubreeey100% (1)
- Drug StudyDocument11 pagesDrug StudyDbktNo ratings yet
- Presentation From Today's Meeting !Document67 pagesPresentation From Today's Meeting !chaitanya varmaNo ratings yet
- 2-The Digestive ProcessDocument8 pages2-The Digestive ProcessYo1No ratings yet
- PancreatitisDocument6 pagesPancreatitisMary AmaliaNo ratings yet
- Republic of The Philippines Cavite State University Don Severino Delas Alas Campus Indang, CaviteDocument12 pagesRepublic of The Philippines Cavite State University Don Severino Delas Alas Campus Indang, Caviteaaron tabernaNo ratings yet
- Peptic Ulcer DiseaseDocument119 pagesPeptic Ulcer DiseaseJoy LacunaNo ratings yet
- Drug StudyDocument8 pagesDrug StudyNo EulNo ratings yet
- Drug StudyDocument8 pagesDrug StudyNo EulNo ratings yet
- Coli, Klebsiella Pneumoniae, Pseudomonas Aeruginosa, Bacteroides Fragilis, B. Thetaiotaomicron, and Peptostr Eptococcus SpeciesDocument8 pagesColi, Klebsiella Pneumoniae, Pseudomonas Aeruginosa, Bacteroides Fragilis, B. Thetaiotaomicron, and Peptostr Eptococcus SpeciesJonna Mae TurquezaNo ratings yet
- Review of Digestive SystemDocument3 pagesReview of Digestive SystemIris MambuayNo ratings yet
- Heptobillary, PancerasaDocument218 pagesHeptobillary, PancerasaHuda Al-Anabr100% (1)
- The Perfect Pancreatitis Diet Cookbook; The Complete Nutrition Guide To Managing And Healing Pancreatitis With Delectable And Nourishing Recipes;From EverandThe Perfect Pancreatitis Diet Cookbook; The Complete Nutrition Guide To Managing And Healing Pancreatitis With Delectable And Nourishing Recipes;No ratings yet
- Lycopene and Heart HealthDocument8 pagesLycopene and Heart HealthDr. HeleNo ratings yet
- Urology DNB Old QuestionsDocument8 pagesUrology DNB Old QuestionssjulurisNo ratings yet
- Clinical Chemistry Review SetDocument4 pagesClinical Chemistry Review SetMarie MontemarNo ratings yet
- Breast - Dr. HammouriDocument12 pagesBreast - Dr. HammouriMohammad PropensityNo ratings yet
- BiojampiDocument4 pagesBiojampiYukendranNo ratings yet
- Analysis The Extracts of Microalgae Nannochloropsis Sp. BioactivityDocument14 pagesAnalysis The Extracts of Microalgae Nannochloropsis Sp. BioactivitySabrina JonesNo ratings yet
- Dpa Cross Sectional Study On The Prevalence of Thyroid Disorders in The Urban Community of DelhiDocument54 pagesDpa Cross Sectional Study On The Prevalence of Thyroid Disorders in The Urban Community of DelhiGurmeet SinghNo ratings yet
- Thyroid ScintigraphyDocument7 pagesThyroid ScintigraphyadaniNo ratings yet
- Genbio 2Document4 pagesGenbio 2Mhariane MabborangNo ratings yet
- Physiology of ParturitionDocument85 pagesPhysiology of ParturitionDark MomentzNo ratings yet
- PRIME Nitric Oxide Activator - QivanaDocument12 pagesPRIME Nitric Oxide Activator - QivanaNikolas SeveridtNo ratings yet
- Management and Complications of Short Bowel SyndromeDocument13 pagesManagement and Complications of Short Bowel Syndromenadill92No ratings yet
- Newborn Screening in The PhilippinesDocument10 pagesNewborn Screening in The PhilippinesMIKAELLA BALUNANNo ratings yet
- Sciences 7Document15 pagesSciences 7Alex ArrietaNo ratings yet
- Endocrine System NCM116 Midterm - XCDocument4 pagesEndocrine System NCM116 Midterm - XCXia CabilloNo ratings yet
- G10 Science DLP COTDocument3 pagesG10 Science DLP COTBernard Maluto GratelaNo ratings yet
- Pediatrics Endocrine DisordersDocument33 pagesPediatrics Endocrine DisordersfatimaNo ratings yet
- Mosby PharmacologyDocument3 pagesMosby PharmacologyMillene Aurelle SaavedraNo ratings yet
- Hipoparatiroidismo Postquirurgico. ATA 2018Document12 pagesHipoparatiroidismo Postquirurgico. ATA 2018Nani HendrianiNo ratings yet
- Erwin-Sheppard Autopsy Report - Redacted by Medical ExaminerDocument17 pagesErwin-Sheppard Autopsy Report - Redacted by Medical ExaminerCheryl Sullenger100% (1)
- Worksheet Packet May 2023Document50 pagesWorksheet Packet May 2023Julie AnnNo ratings yet
- Insulinas de OsmosisDocument3 pagesInsulinas de OsmosisDennise A. Hernández JuárezNo ratings yet
- Osteoporosis Prevention: Exercise Your BonesDocument8 pagesOsteoporosis Prevention: Exercise Your BonesAdhiraj singhNo ratings yet
- Model Paper Set-B Medicinal Chemistry-I Bp402T: Section A MM 75 1. Attempt All Questions in Brief. 10 X 1 20Document1 pageModel Paper Set-B Medicinal Chemistry-I Bp402T: Section A MM 75 1. Attempt All Questions in Brief. 10 X 1 20SwarnA TamtaNo ratings yet
- Ubah HpaDocument1 pageUbah HpaChidiebereNo ratings yet
- Bmifa Boys Z 5 19 LabelsDocument1 pageBmifa Boys Z 5 19 LabelsRhea JavierNo ratings yet