Professional Documents
Culture Documents
An evidence-based approach to undifferentiated shock
Uploaded by
Hely ICOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
An evidence-based approach to undifferentiated shock
Uploaded by
Hely ICCopyright:
Available Formats
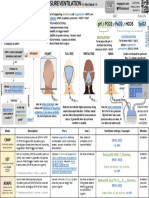
PROACH TO UNDIFFERENTIATED SHOCK
by Nick Mark MD ONE
onepagericu.c
om
Link to the
most current
· Shock occurs when there is inadequate blood flow (CO) & oxygen delivery (DO2) to meet version →
demands. Manifestations can be protean and may not initially include hypotension (cryptic Undifferentiated SHOCK @nickmmark
Hypotension (not required) MAP DETERMINANTS:
shock). Identifying the etiology of undifferentiated shock is essential to determine treatment. Preload Contractility Afterload
Organ dysfunction (AKI, shock liver, etc)
· Shock can be broken into 4 categories: cardiogenic, obstructive, distributive, hypovolemic Altered mental status
· Multiple causes may be present (e.g. sepsis in a patient with decompensated heart failure) and Lactic acidosis SV HR
some etiologies may cause mixed shock: Low urine output
CO SVR
· Endocrine (adrenal insuf., myxedma, thyrotoxicosis) ↓CO ↓SVR ↓ Preload
· Metabolic (hypothermia severe acidosis)
PIPES PROBLEM TANK PROBLEM MAP
PUMP PROBLEM
CARDIOGE OBSTRUCTI DISTRIBUT HYPOVOLE
• RATE/RHYTHM (bradycardia, VF, • TENSION • SEPSIS (may develop low CO later) • HEMORRHAGE (trauma,
NIC VE IVE surgical, GIB) MIC
ETIOLOGY
etc) PNEUMOTHORAX • ANAPHYLAXIS
• RV FAILURE (PE, PHTN) • CARDIAC TAMPONADE • INFLAMMATORY (SIRS, • SKIN LOSSES (burns, heat stroke,
• LV FAILURE (MI, myocarditis, etc) • PULMONARY pancreatitis, post-cardiac arrest, etc)
• VALVES (wide open MR, cordae EMBOLISM amniotic or fat embolism, cytokine • GI LOSSES (diarrhea, vomiting,
tendenae rupture, etc) • OUTFLOW release syndrome) drainage)
• TOXINS (CCB, βB, BRASH syndrome, OBSTRUCTION (HOCM, • NEUROGENIC (SCI, severe TBI, • THIRD-SPACING VOLUME
etc) critical AS) effect of neuraxial anesthesia) LOSS (pancreatitis, low albumin,
• TRAUMA (myocardial contusion) • DYNAMIC • LIVER FAILURE trauma)
HYPERINFLATION ( • ENDOCRINE (adrenal • RENAL LOSSES (salt-wasting,
insufficiency, thyrotoxicosis)
EXAM & POCUS & HEMODYNAMICS
auto- PEEP) hypoaldo, osmotic diuresis, diuretics)
• MEDICATIONS (anesthesia, • LOW PO INTAKE
HD ↑CVP, ↑PCWP, ↓CO, ↑SVR ↑CVP, ↑PCWP, ↓CO, ↑SVR var CVP,) var PCWP, var CO, ↓SVR
sedation ↓CVP, ↓PCWP, ↑CO, ↑SVR
± Reduced contractility ± RV dilation Reduced contractility
(see RUSH exam for more about POCUS in Shock)
Heart ± Wall motion abnormalities RV dilation (PE) ± septal D sign (p/v overload) Hyperdynamic Hyperdynamic
± Valvulopathy Pericardial effusion, RA collapse (tamponade) (hypodynamic in late sepsis)
IVC Plethoric IVC, reversal of flow in HV Plethoric IVC, reversal of flow in HV Variable IVC Small/collapsing IVC
Lungs B-line pattern + pleural effusions Lack of lung sliding ± lung point (PTX) A line pattern A line pattern
Other Pleural effusions (LV failure) DVT or clot in transit (PE) Evidence of infxn (cholecystitis, endocarditis, Blood or fluid in abdomen (FAST), Ectopic
etc), cirrhosis, pregnancy, Aortic dissection,
Skin Usually cool, Delayed cap refill Usually cool, Delayed cap refill Warm, flushed, Brisk cap refill Usually cool, Delayed cap refill
Neck Increased JVP Increased JVP Variable Flat neck veins
Weak pulses (narrow pulse pressure) Weak pulses (narrow pulse pressure)
Other Weak pulses (narrow pulse pressure) Lung and heart sounds are unreliable Bounding pulses (wide pulse pressure) Evidence of blood (pallor) or volume loss
indicators of tamponade or PTX. (axillary dryness)
PHYSIOLOGIC RESPONSES TO SHOCK USING GUYTON CURVES: (See Guyton Curves in Shock OnePager for more) CALCULATING SVR:
SVR can be useful to understand etiology. You
v1.0 (2021-05-11) CC BY-SA 3.0
with exercise
Cardiac Output
Cardiac Output
Venous Return
Venous Return
Cardiac Output
Venous Return
Cardiac Output
Venous Return
can either measure CO invasively (e.g. PAC) or
Increased estimate using POCUS (e.g. LVOT VTI)
contractility 𝑴𝑨𝑷=𝑪𝑶×
𝑺𝑽𝑹
initial state ( 𝑴𝑨𝑷 − 𝑪𝑽𝑷)
Venoconstriction 𝑺𝑽𝑹
= × 𝟖𝟎
RAP RAP RAP RAP 𝑪𝑶
Normally cardiac output (CO) CARDIOGENIC/OBSTRUCTIVE DISTRIBUTIVE HYPOVOLEMIC
dyn/cm/sec-5
determined by venous return &
contractility
with low CO, RA filling pressures
rise to (partially) compensate
vasodilation decreases filling,
hyperdynamic CO compensates
with low preload, venoconstriction
increased filling pressure compensates
Wood units
You might also like
- NON-INVASIVE VENTILATION GUIDEDocument1 pageNON-INVASIVE VENTILATION GUIDENicholas HelmstetterNo ratings yet
- Immunization Titer FormsDocument19 pagesImmunization Titer FormsCole GarrettNo ratings yet
- Resume Maximo AvilaDocument3 pagesResume Maximo Avilaapi-709259488No ratings yet
- Professional Nursing ResumeDocument5 pagesProfessional Nursing Resumeapi-556406464No ratings yet
- Nih Stroke Scale Certificate ADocument1 pageNih Stroke Scale Certificate Aapi-302383914No ratings yet
- ResumeDocument2 pagesResumeapi-239581502No ratings yet
- Kellys Letter of RecommendationDocument2 pagesKellys Letter of Recommendationapi-638553003No ratings yet
- CV For WeeblyDocument2 pagesCV For Weeblyapi-267602325No ratings yet
- EUA Abiomed ImpellaLV IFU3Document254 pagesEUA Abiomed ImpellaLV IFU3Angelina LeungNo ratings yet
- Leskovac Nur 460 PGC Reflection PaperDocument9 pagesLeskovac Nur 460 PGC Reflection Paperapi-527774673No ratings yet
- Philosophy of Nursing Practice DNP Timothy Blake BoothDocument2 pagesPhilosophy of Nursing Practice DNP Timothy Blake Boothapi-555804657No ratings yet
- Personal Identity EssayDocument9 pagesPersonal Identity EssayKELLY STOTTSNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Planning Intervention EvaluationDocument2 pagesNursing Care Plan: Assessment Diagnosis Planning Intervention EvaluationLeirza OnibarNo ratings yet
- Grant Application NarrativeDocument3 pagesGrant Application Narrativeapi-241005093No ratings yet
- Running Head: Program Graduate Competencies 1Document10 pagesRunning Head: Program Graduate Competencies 1api-385363448No ratings yet
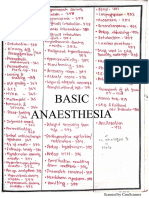
- Rony Basic Anesthesia PDFDocument85 pagesRony Basic Anesthesia PDFRobiul AlamNo ratings yet
- Peng Resume v2Document1 pagePeng Resume v2api-620640264No ratings yet
- Eportfolio Resume CVDocument4 pagesEportfolio Resume CVapi-577441503No ratings yet
- ICU Registered Nurse Resume Brick RedDocument2 pagesICU Registered Nurse Resume Brick RedAngelNo ratings yet
- Vaccination Schedule For HorsesDocument3 pagesVaccination Schedule For HorsesKikiNo ratings yet
- Patient AssessmentDocument3 pagesPatient AssessmentYemaya84100% (1)
- Duke Micu ResumeDocument2 pagesDuke Micu Resumeapi-88442147No ratings yet
- Medical CertificateDocument2 pagesMedical CertificateAbhijeet0% (1)
- Hsus Complete-Guide-To-Horse-CareDocument194 pagesHsus Complete-Guide-To-Horse-Careapi-666724462No ratings yet
- Nursing ResumeDocument2 pagesNursing Resumeapi-259457383No ratings yet
- Jshawn - Haralson: SuperintendentDocument3 pagesJshawn - Haralson: SuperintendentWTXL ABC27No ratings yet
- Cataldo Defense Request For Lesser SentencingDocument4 pagesCataldo Defense Request For Lesser Sentencingjafranklin-1No ratings yet
- Mentoring Guidebook 2016Document38 pagesMentoring Guidebook 2016JM EspararNo ratings yet
- Animal Health CertificateDocument9 pagesAnimal Health Certificatenelyy7No ratings yet
- ICU One Pager Undifferentiated ShockDocument1 pageICU One Pager Undifferentiated ShockHely ICNo ratings yet
- Autonomic Peripheral Neuropathy: Review ArticleDocument14 pagesAutonomic Peripheral Neuropathy: Review ArticleAlaa MishrifNo ratings yet
- DR Najeeb HFDocument20 pagesDR Najeeb HFCanan YilmazNo ratings yet
- ElectrochemistryDocument12 pagesElectrochemistryHunter DracolusNo ratings yet
- Autonomic Peripheral Neuropathy.7Document14 pagesAutonomic Peripheral Neuropathy.7thomashenrryNo ratings yet
- NephrologyDocument177 pagesNephrologyKabbuNo ratings yet
- Diabetes and Metabolic Disorders and The.5 PDFDocument23 pagesDiabetes and Metabolic Disorders and The.5 PDFTallulah Spina TensiniNo ratings yet
- 4.1.4: Negative-Electrode Aging Processes in Bulk and Composite ElectrodeDocument2 pages4.1.4: Negative-Electrode Aging Processes in Bulk and Composite Electrodesajjad saberiNo ratings yet
- Ataxia 10Document19 pagesAtaxia 10Cristina GhizdavetNo ratings yet
- Rhythms of Death MD1TALKDocument1 pageRhythms of Death MD1TALKAmalNo ratings yet
- Chem P1 JournalDocument51 pagesChem P1 Journalyara hazemNo ratings yet
- Blank SyllabusDocument13 pagesBlank Syllabusapi-521413030No ratings yet
- Slug force calculationsDocument1 pageSlug force calculationsJ A S JASNo ratings yet
- Metabolism of NeurotransmittersDocument9 pagesMetabolism of Neurotransmitterspotro patoNo ratings yet
- Brain Death Death by Neurologic Criteria.15Document21 pagesBrain Death Death by Neurologic Criteria.15Anusha PervaizNo ratings yet
- PEDIATRIC RESUSCITATION PARAMETERS AND ECMO CRITERIADocument2 pagesPEDIATRIC RESUSCITATION PARAMETERS AND ECMO CRITERIAwalkingthewardsNo ratings yet
- Adobe Scan 29-Mar-2023Document1 pageAdobe Scan 29-Mar-2023NAMAN SONINo ratings yet
- Lec 1 - Intro To ElectrostaticsDocument3 pagesLec 1 - Intro To ElectrostaticsFatemeh KeshavarzNo ratings yet
- DISORDERS OF SODIUM: HYPONATREMIA CAUSES BRAIN INJURY IF CORRECTED TOO RAPIDLYDocument22 pagesDISORDERS OF SODIUM: HYPONATREMIA CAUSES BRAIN INJURY IF CORRECTED TOO RAPIDLYfaiza anwerNo ratings yet
- Introduction To Plasma EtchingDocument58 pagesIntroduction To Plasma EtchingParashara Panduranga100% (1)
- Augenheilkunde FragenDocument3 pagesAugenheilkunde FragenWise AmroNo ratings yet
- Perturbation Methods in Fluid - Mechanics - MiltonVanDykeDocument143 pagesPerturbation Methods in Fluid - Mechanics - MiltonVanDyke700120No ratings yet
- ICU One Pager Fluid Responsiveness v1 2Document1 pageICU One Pager Fluid Responsiveness v1 2liz mNo ratings yet
- E-Mergency Activity KitDocument9 pagesE-Mergency Activity KitChronicleBooksNo ratings yet
- Kinetic Isotope EffectsDocument22 pagesKinetic Isotope EffectsAdjieDarmawanNo ratings yet
- Management of Stroke in The NCCUDocument25 pagesManagement of Stroke in The NCCUsaudNo ratings yet
- Vol. 7 No. 2 (2022) : JOP (Journal Online of Physics) Vol 7 No 2 - JOURNAL ONLINE OF PHYSICSDocument2 pagesVol. 7 No. 2 (2022) : JOP (Journal Online of Physics) Vol 7 No 2 - JOURNAL ONLINE OF PHYSICSFachri ZainuddinNo ratings yet
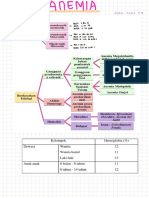
- MCV FT 91dL: AromaDocument9 pagesMCV FT 91dL: AromaEka NarendraNo ratings yet
- BLOOD PRODUCT TRANSFUSIONS DEFINITIONS AND TRANSFUSION REACTIONSDocument1 pageBLOOD PRODUCT TRANSFUSIONS DEFINITIONS AND TRANSFUSION REACTIONSjuan ramon milanes grageraNo ratings yet
- Making Sense of Oxygen Quantum Leaps With Physics-Iology': EditorialDocument5 pagesMaking Sense of Oxygen Quantum Leaps With Physics-Iology': EditorialAlyssa HarperNo ratings yet
- Modelling The Neuroanatomical Progression of Alzheimers Disease and Posterior Cortical AtrophyDocument38 pagesModelling The Neuroanatomical Progression of Alzheimers Disease and Posterior Cortical AtrophyRazvan Valentin MarinescuNo ratings yet
- Basic Calculus L2Document14 pagesBasic Calculus L2Abbie MalutoNo ratings yet
- Kolkata Thika Tenancy ActDocument15 pagesKolkata Thika Tenancy Actadv123No ratings yet
- Analysis and Adaptive Control of EDM Sinking Process Using The Ignition Delay Time and Fall TimeDocument4 pagesAnalysis and Adaptive Control of EDM Sinking Process Using The Ignition Delay Time and Fall TimeResearch AssistanceNo ratings yet
- CS602 Current Final Term Papers 2018 To 2020Document3 pagesCS602 Current Final Term Papers 2018 To 2020Jawad AliNo ratings yet
- ACCFA V CUGCO Case DigestDocument2 pagesACCFA V CUGCO Case DigestLoren yNo ratings yet
- Tinea - The DermatophytesDocument67 pagesTinea - The Dermatophytesmansoor aliNo ratings yet
- Legal Counselling defined in broad and narrow sensesDocument5 pagesLegal Counselling defined in broad and narrow sensesRegie Rey AgustinNo ratings yet
- Marketing Research An Applied Orientation 7th Edition Malhotra Solutions ManualDocument33 pagesMarketing Research An Applied Orientation 7th Edition Malhotra Solutions Manualtitusotis7s8yba100% (27)
- Guia Presente Perfecto (Sin Have Been)Document8 pagesGuia Presente Perfecto (Sin Have Been)Nataly BarreraNo ratings yet
- Individual Project Instructions - 5aDocument1 pageIndividual Project Instructions - 5aIkhram JohariNo ratings yet
- Problem Based Learning Integrating 21 Century Skills: Prepared By:-Alamelu Manggai Ponnusamy Santha Kumari KrishnanDocument18 pagesProblem Based Learning Integrating 21 Century Skills: Prepared By:-Alamelu Manggai Ponnusamy Santha Kumari KrishnanAlamelu Manggai PonnusamyNo ratings yet
- Hospital Visit ReportDocument8 pagesHospital Visit ReportSuraj JadhavNo ratings yet
- GrammarDocument10 pagesGrammarRidhan RahmahNo ratings yet
- Y4A Practice Book Answers White Rose Maths EditionDocument20 pagesY4A Practice Book Answers White Rose Maths EditionNgọc YếnNo ratings yet
- Cruz Vs Dir. of PrisonDocument3 pagesCruz Vs Dir. of PrisonGeeanNo ratings yet
- Emergency Department (Ed) Overcrowding: Evidence-Based Answers To Frequently Asked QuestionsDocument7 pagesEmergency Department (Ed) Overcrowding: Evidence-Based Answers To Frequently Asked QuestionsNurul AidaNo ratings yet
- Significant Figures and Unit Conversion Practice ProblemsDocument17 pagesSignificant Figures and Unit Conversion Practice ProblemsMichael Damian100% (3)
- UntitledDocument23 pagesUntitledjaanharafNo ratings yet
- (Day 77) (Final) The Prisoners (Attendance in Courts) Act, 1955Document4 pages(Day 77) (Final) The Prisoners (Attendance in Courts) Act, 1955Mayur MalviyaNo ratings yet
- OMCC Board ResolutionDocument1 pageOMCC Board ResolutionOrient MansionNo ratings yet
- Ozark River Bank Cases: 20210821 - Case AnalysisDocument6 pagesOzark River Bank Cases: 20210821 - Case AnalysisTresna AswinNo ratings yet
- The Pen Pal ProjectDocument1 pageThe Pen Pal ProjectMelanie Yosiris Mayorga FonsecaNo ratings yet
- 3 Affect Regulation, Mentalization, and The Development of The Self (Peter Fonagy, Gyorgy Gergely, Elliot L. Jurist Etc.) - 211-259Document49 pages3 Affect Regulation, Mentalization, and The Development of The Self (Peter Fonagy, Gyorgy Gergely, Elliot L. Jurist Etc.) - 211-259Sergio Andres Rico AvendanoNo ratings yet
- De Onde Eu Te VejoDocument2 pagesDe Onde Eu Te VejoBianca Oliveira CoelhoNo ratings yet
- American Ceramic: SocietyDocument8 pagesAmerican Ceramic: SocietyPhi TiêuNo ratings yet
- SHCT 167 Reeves - English Evangelicals and Tudor Obedience, C. 1527-1570 2013 PDFDocument222 pagesSHCT 167 Reeves - English Evangelicals and Tudor Obedience, C. 1527-1570 2013 PDFL'uomo della Rinascitá100% (1)
- Contemporary ArtDocument2 pagesContemporary ArtXpertz PrintingNo ratings yet
- Impala Job Application 2Document3 pagesImpala Job Application 2EXXARO MATLANo ratings yet
- Lecture NotesDocument12 pagesLecture NotesSabina Ioana AioneseiNo ratings yet
- Journal of Cleaner Production: Fabíola Negreiros de Oliveira, Adriana Leiras, Paula CerynoDocument15 pagesJournal of Cleaner Production: Fabíola Negreiros de Oliveira, Adriana Leiras, Paula CerynohbNo ratings yet