Professional Documents
Culture Documents
(+) Pain and (+) Discharge (-) Pain and (+) Discharge: Red Eye
Uploaded by
Mariel TagazaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
(+) Pain and (+) Discharge (-) Pain and (+) Discharge: Red Eye
Uploaded by
Mariel TagazaCopyright:
Available Formats
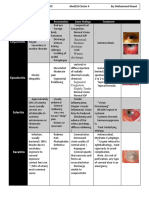
(+)Mucopurulent discharge
H. influenza - most common etiology in children
with URTI; Chlamydia or gonococcus - most
common among newborns; Moraxella and
Staphylococcus are common among adults
BACTERIAL CONJUNCTIVITIS
Most often unilateral and acute in onset
Antibiotic eye drops
TREATMENT
Oral antibiotics - also administered in patients with
Hemophilus, Chlamydia or gonococcal conjunctivitis
(+)Watery discharge
(+)Itchy
(+) mucoid to muco-purulent eye discharge
chronic; immunologic in nature; most patients have
atopy or an atopic predisposition Pneumococcus - most common cause;
Pseudomonas - common among contact lens
wearers
ALLERGIC CONJUNCTIVITIS
(+)pale papillary reaction on the upper bulbar
conjunctivae BACTERIAL KERATITIS
(+)Pain and (+)Discharge (+) blurring vision if the lesion is on central cornea
(-)Pain and (+)Discharge
Removal of environmental triggers
Topical antibiotics applied every 15 minutes to every
hour during first few days of treatment
Cold compress
TREATMENT TREATMENT Keratectomy - done in moderate to severe cases
Antihistamine eye drops - to control symptoms
Idea
Short-term topical steroids - in moderate to severe
cases
(+)Photophobia
(+)Watery discharge
Most cases are idiopathic; others may be cause by
Herpes virus and Mycobacterium tuberculosis
(-)Itchy
(+)keratic precipitates on inner surface of cornea;
UVEITIS (+)iris adhesion to the lens
The most common cause of acute onset eye redness
(+)History of exposure to a person with "sore eyes" Topical steroid drops - if located at the anterior part
of the eye
VIRAL CONJUNCTIVITIS or "sore eyes"
Adenoviral - most common conjunctival infection
Periocular steroid injection - if located in the
TREATMENT
posterior pole
Duration - few days to 2-4 weeks; self-limiting
Oral steroids - used in patients with bilateral
disease/ systemic evidence of inflammation
Hand wash
Red eye
Avoiding direct contact with eye discharge (+)Photophobia
TREATMENT
Antibiotic eyedrops - may be given in patients with (+)Deep boring pain/severe pain
secondary bacterial infection
Purplish sclera or violaceous red; Edema or thinning
Mild steroid drops and cold compress - help reduce of sclera; No change with epinephrine drops
SCLERITIS
inflammation
systemic corticosteroids
a.k.a. keratoconjunctivitis sicca If non-infectious scleritis
NSAIDS
common among elderly TREATMENT
anti-inflammatory therapy should never be started
due to decreased tear production or increased tear without accompanying or prior treatment with
If infectious scleritis antimicrobial therapy
evaporation
DRY EYE
(-)Pain and (-)Discharge
worse with wind and dry climates (+)Pain and (-)Discharge Less or (-) Photophobia
presents with foreign body sensation and mild eye
redness
(+)Mild pain or none
Topical instillation of aqueous tear replacement/
artificial tears TREATMENT
Unaffected sclera, salmon color; No scleral changes;
Blanches with epinephrine drops
EPISCLERITIS
Topical vasoconstrictor
Topical NSAID
TREATMENT
Fluorometholone eye drops 4x/day
Mild to moderate
Lubricating drops
Topical steroid
Prednisolone acetate eye drops 4-6x/day
Severe form
Ibuprofen 400mg 3x/day
(-)Photophobia
Pain is associated with headache; (+)blurring of
vision; some patients complain of seeing rainbow
haloes
ACUTE GLAUCOMA
Eye pressure is abnormally elevated due to an acute
obstruction
Acetazolamide or hyperosmotic oral solutions
TREATMENT Topical ocular hypotensive agents
Laser Iridotomy - definitive management
You might also like
- Ophthalmia NeonatorumDocument30 pagesOphthalmia NeonatorumManish ShresthaNo ratings yet
- HEPADNAVIRIDAEDocument14 pagesHEPADNAVIRIDAEnur qistina humaira zulkarshamsiNo ratings yet
- Nclex DiseasesDocument6 pagesNclex Diseasesshangguanlongkui95% (21)
- Ocular Emergencies-Sept2013 PDFDocument22 pagesOcular Emergencies-Sept2013 PDFKaramsi Gopinath NaikNo ratings yet
- Pharmacology FinalsDocument43 pagesPharmacology FinalsJustine Vens G. AgustinNo ratings yet
- ConjunctivitisDocument4 pagesConjunctivitisKumar ShivamNo ratings yet
- Classification of InjuriesDocument7 pagesClassification of InjuriesSajin AlexanderNo ratings yet
- PediaDocument2 pagesPediaCamille ButaoNo ratings yet
- ConjungtivitisDocument86 pagesConjungtivitisIvo AfianiNo ratings yet
- Conjunctivitis 2016 - 1Document2 pagesConjunctivitis 2016 - 1Rida RahayuNo ratings yet
- Drug StudyDocument3 pagesDrug StudyNicole Rachelyn MartinNo ratings yet
- Endophthalmitis: Current Trends, Drugs and Protocols: Aditya Verma, Vinata Muralidharan and Eesh NigamDocument10 pagesEndophthalmitis: Current Trends, Drugs and Protocols: Aditya Verma, Vinata Muralidharan and Eesh NigamHerman Kurt Ludvik100% (1)
- Conjunctivitis: Radang Konjungtiva Yang Menutupi Belakang Kelopak Dan Bola Mata, Dalam Bentuk Akut Maupun KronisDocument18 pagesConjunctivitis: Radang Konjungtiva Yang Menutupi Belakang Kelopak Dan Bola Mata, Dalam Bentuk Akut Maupun KronisnasikaceliaNo ratings yet
- Communicable DiseaseDocument12 pagesCommunicable DiseaseFatema Tuzzannat BrishtyNo ratings yet
- Name of Drug Mechanism of Action Contraindication Side Effects Adverse Effects Nursing ResponsibilitiesDocument2 pagesName of Drug Mechanism of Action Contraindication Side Effects Adverse Effects Nursing ResponsibilitiesMichelle Dona MirallesNo ratings yet
- Conjunctiva (Hira FJ)Document26 pagesConjunctiva (Hira FJ)Minahil ShahidNo ratings yet
- Rash Diagnosis Cheat Sheet: EmergencyDocument1 pageRash Diagnosis Cheat Sheet: Emergencykdlsfk kajjksolsNo ratings yet
- Micro Chart #3 - Italics OnlyDocument27 pagesMicro Chart #3 - Italics Onlyapi-26938624100% (1)
- 1.02 Sugical Conditions of The Skin and Subcutaneous Tissue (Part2)Document6 pages1.02 Sugical Conditions of The Skin and Subcutaneous Tissue (Part2)Klyn Agagon GayodanNo ratings yet
- Conjunctivitis - Dita LSDocument17 pagesConjunctivitis - Dita LSMeNo ratings yet
- # Diseases of ConjunctivaDocument4 pages# Diseases of Conjunctivaameerabest100% (1)
- Selected Differential Diagnosis of Red Eye: Table 1Document3 pagesSelected Differential Diagnosis of Red Eye: Table 1Rian DamayantiNo ratings yet
- Exanthems TableDocument3 pagesExanthems TableYana CovarNo ratings yet
- Opthalmology - Summary TableDocument4 pagesOpthalmology - Summary TableJYGNo ratings yet
- Managing Otitis ExternaDocument34 pagesManaging Otitis ExternaramaNo ratings yet
- The Red EyeDocument42 pagesThe Red EyeDenise CarbonellNo ratings yet
- Catatan Koass MataDocument6 pagesCatatan Koass MataYPramudiyaNo ratings yet
- 12 - Ocular Pharmacology - 343 - 64Document37 pages12 - Ocular Pharmacology - 343 - 64ณัฐ มีบุญNo ratings yet
- Conjunctivitis 120201025034 Phpapp02Document34 pagesConjunctivitis 120201025034 Phpapp02Ilham RafisNo ratings yet
- Skin PathogensDocument4 pagesSkin PathogensEhi EdialeNo ratings yet
- Antifungal TheraphyDocument4 pagesAntifungal TheraphyOrhan AsdfghjklNo ratings yet
- WHO AWaRe Antibiotic Book 2022Document150 pagesWHO AWaRe Antibiotic Book 2022indri100% (1)
- Red Eye TableDocument2 pagesRed Eye TableFatimah AlsultanNo ratings yet
- Skin Care For HealthDocument3 pagesSkin Care For HealthGin MananganNo ratings yet
- 2 Susceptible: Transmission Based Precautions GuidelineDocument2 pages2 Susceptible: Transmission Based Precautions GuidelinepaulaNo ratings yet
- Berongoy VirusDocument2 pagesBerongoy VirusGlaiza Mae BerongoyNo ratings yet
- Complication CL OsceDocument6 pagesComplication CL OsceAdam EdzelNo ratings yet
- Orbital and Ocular TumorsDocument13 pagesOrbital and Ocular TumorsstarlytexpressNo ratings yet
- Reviewer Finals Maternal and Child NursingDocument15 pagesReviewer Finals Maternal and Child NursingChristine Airah TanaligaNo ratings yet
- 0000 0000:Dr Manlapig MergedDocument51 pages0000 0000:Dr Manlapig MergedAj Christian Lacuesta IsipNo ratings yet
- TOPNOTCH Microbiology-Supertable-by-Dr - Cocoy-Calderon-Jaffar-Pineda-Troy-Soberano-UPDATED-NOVEMBER-2017 PDFDocument34 pagesTOPNOTCH Microbiology-Supertable-by-Dr - Cocoy-Calderon-Jaffar-Pineda-Troy-Soberano-UPDATED-NOVEMBER-2017 PDFWaiwit KritayakiranaNo ratings yet
- A Painful Red Eye: Case StudyDocument2 pagesA Painful Red Eye: Case StudyAmber WangNo ratings yet
- Parasitic Infections Affected Body Parts Causative Agents Mode OF Transmission Signs AND Symptoms Drug of ChoiceDocument23 pagesParasitic Infections Affected Body Parts Causative Agents Mode OF Transmission Signs AND Symptoms Drug of ChoiceCindy Mae de la TorreNo ratings yet
- Ceh 12 30 019 PDFDocument2 pagesCeh 12 30 019 PDFHerwandiNo ratings yet
- Case ReportDocument43 pagesCase ReporttsazuuNo ratings yet
- CorneaDocument5 pagesCorneaMohamed GhanemNo ratings yet
- Red Eye - Conjunctivitis I Dr. Nuke Erlina Mayasari, SPMDocument23 pagesRed Eye - Conjunctivitis I Dr. Nuke Erlina Mayasari, SPMismkipendprowil2No ratings yet
- As 14 OutlineDocument16 pagesAs 14 OutlineLarebNo ratings yet
- Microbial Diseases of The Skin and EyesDocument29 pagesMicrobial Diseases of The Skin and EyesqueennieNo ratings yet
- MicroLec GroupWork1Document10 pagesMicroLec GroupWork1A18- Jessa Mae DayagNo ratings yet
- Conjunctivitis and Other Ocular Lesions Opthalmology ClassDocument43 pagesConjunctivitis and Other Ocular Lesions Opthalmology ClassJaikrit SinghNo ratings yet
- CH 068 Ophthalmia NeonatorumDocument7 pagesCH 068 Ophthalmia NeonatorumrehanaNo ratings yet
- Lecture 10 Antibiotics & Antiinfectives-1Document39 pagesLecture 10 Antibiotics & Antiinfectives-1Dr Haris AwanNo ratings yet
- 3) Bacterial Skin Infections Semi NotesDocument2 pages3) Bacterial Skin Infections Semi NotesIssa MoodNo ratings yet
- Guide ZonaOphtalmique Web EN VFDocument6 pagesGuide ZonaOphtalmique Web EN VFsiti rumaisaNo ratings yet
- The Newborn at Risk of A Maternal Infection Opthalmia NeonatorumDocument2 pagesThe Newborn at Risk of A Maternal Infection Opthalmia NeonatorumIren Rose PañaNo ratings yet
- Icietet 63Document5 pagesIcietet 63Peruru Famida NajumunNo ratings yet
- Viral (Aseptic) Meningitis) Main Cause of Common ColdDocument4 pagesViral (Aseptic) Meningitis) Main Cause of Common ColdKatie Anne SaylerNo ratings yet
- OpthalDocument15 pagesOpthalWaiwit KritayakiranaNo ratings yet
- Bacterial Skin Infections BmlsDocument5 pagesBacterial Skin Infections Bmls97w25v8c82No ratings yet
- TEARING PDF Final PDFDocument1 pageTEARING PDF Final PDFMariel TagazaNo ratings yet
- Worksheet MteabDocument3 pagesWorksheet MteabMariel TagazaNo ratings yet
- Heart and Mediastinum NotesDocument2 pagesHeart and Mediastinum NotesMariel TagazaNo ratings yet
- Fetal CirculationDocument2 pagesFetal CirculationMariel TagazaNo ratings yet
- Bacteriology Bacterial Classification:: Sequencing Produced by The BodyDocument2 pagesBacteriology Bacterial Classification:: Sequencing Produced by The BodyMariel TagazaNo ratings yet
- TEARING PDF Final PDFDocument1 pageTEARING PDF Final PDFMariel TagazaNo ratings yet
- HolaDocument1 pageHolaMariel TagazaNo ratings yet
- Ralph 35Document18 pagesRalph 35Mariel TagazaNo ratings yet
- Resolution of (Co (En) As ( (+) - Co (En) : Synthesis and Characterization of Cobalt Complexes (Day 3) Part 1. SynthesisDocument2 pagesResolution of (Co (En) As ( (+) - Co (En) : Synthesis and Characterization of Cobalt Complexes (Day 3) Part 1. SynthesisMariel TagazaNo ratings yet
- E TalesDocument1 pageE TalesMariel TagazaNo ratings yet
- LyricsDocument1 pageLyricsMariel TagazaNo ratings yet
- Background of The Experiment Results and DiscussionDocument1 pageBackground of The Experiment Results and DiscussionMariel TagazaNo ratings yet
- Cheat SheetDocument2 pagesCheat SheetMariel TagazaNo ratings yet
- HWDocument2 pagesHWMariel TagazaNo ratings yet
- Simbahan NG MakaraigDocument1 pageSimbahan NG MakaraigMariel TagazaNo ratings yet
- RXN PaperDocument1 pageRXN PaperMariel TagazaNo ratings yet
- PracticallyyDocument1 pagePracticallyyMariel TagazaNo ratings yet
- BallsDocument20 pagesBallsMariel TagazaNo ratings yet
- Serious Adverse Events Chapter 8: The Rebel GeniusDocument8 pagesSerious Adverse Events Chapter 8: The Rebel GeniusChelsea Green PublishingNo ratings yet
- Corti Et Al., 2021Document38 pagesCorti Et Al., 2021LunaNo ratings yet
- 641-Article Text-1162-1-10-20171110Document19 pages641-Article Text-1162-1-10-20171110Krishan Kumar sharmaNo ratings yet
- Epidemiologia AlzheimerDocument31 pagesEpidemiologia AlzheimerSergio GarcíaNo ratings yet
- PrometricDocument68 pagesPrometricAjurs UrsabiaNo ratings yet
- Histones and Histone Modifications: PrimerDocument6 pagesHistones and Histone Modifications: PrimerE mailNo ratings yet
- HDACDocument10 pagesHDACfarihameetsworldNo ratings yet
- Griffiths Introduction To Genetic Analysis 12th EditionDocument3,002 pagesGriffiths Introduction To Genetic Analysis 12th Editionmartin.kv4No ratings yet
- Repurposing Chlorpromazine To Treat COVID-19Document5 pagesRepurposing Chlorpromazine To Treat COVID-19wiwiNo ratings yet
- Heredity (Inheritance and Variation)Document3 pagesHeredity (Inheritance and Variation)Jazel SalesNo ratings yet
- 104 - Neurology Physiology) Spinal Cord - Golgi Tendon Organ Reflex (GTO)Document3 pages104 - Neurology Physiology) Spinal Cord - Golgi Tendon Organ Reflex (GTO)Nikki Lin LiuNo ratings yet
- Anti - Tubercular DrugsDocument88 pagesAnti - Tubercular DrugsEscitalopram 5mgNo ratings yet
- Immunology FirecrackerDocument45 pagesImmunology FirecrackerMariam A. KarimNo ratings yet
- Pathophysiology of Meningiomas 2003Document18 pagesPathophysiology of Meningiomas 2003Klinik medan DeliNo ratings yet
- Laboratory Diagnosis of MeningitisDocument28 pagesLaboratory Diagnosis of Meningitissangeetha_v100No ratings yet
- Clinical Review: The Specific Dermatoses of PregnancyDocument8 pagesClinical Review: The Specific Dermatoses of PregnancyAhmad AbulegiNo ratings yet
- Universidad Vasco de Quiroga Morelia Infectología: NeuroinfeccionDocument43 pagesUniversidad Vasco de Quiroga Morelia Infectología: NeuroinfeccionJane LeonNo ratings yet
- Bio-Energetic Frequency ChartsDocument37 pagesBio-Energetic Frequency ChartsHayden JamesNo ratings yet
- E-Poster PresentationDocument1 pageE-Poster PresentationOvamelia JulioNo ratings yet
- Crp-DikonversiDocument13 pagesCrp-DikonversiKurnia FitriasariNo ratings yet
- A Case Study On Multi Drug Resistant Infection: January 2018Document6 pagesA Case Study On Multi Drug Resistant Infection: January 2018esti mNo ratings yet
- Chapter6 MC QuizDocument16 pagesChapter6 MC Quizsmishra_97100% (1)
- Life Sciences IV Final Exam - Set 4 Flashcards - QuizletDocument11 pagesLife Sciences IV Final Exam - Set 4 Flashcards - QuizletVizhiNo ratings yet
- Biology 11 NotesDocument219 pagesBiology 11 NotesShitalPatilNo ratings yet
- Special Collection ProceduresDocument6 pagesSpecial Collection ProceduresB12 Clifford GarciaNo ratings yet
- IMMU Lecturee Notes 6Document15 pagesIMMU Lecturee Notes 6jzho9697No ratings yet
- David Martin ConvertDocument24 pagesDavid Martin Convertbun lunNo ratings yet
- 456789Document78 pages456789Sultan AyyanNo ratings yet