Professional Documents
Culture Documents
Nicanor Reyes Medical Foundation: Far Eastern University
Uploaded by
gAARaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nicanor Reyes Medical Foundation: Far Eastern University
Uploaded by
gAARaCopyright:
Available Formats
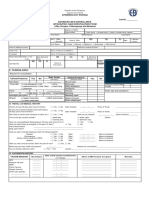
Far Eastern University History and Physical Examination
Nicanor Reyes Medical Foundation
Department of Internal Medicine Proctor’s Signature:
Faderugao, Martina Patient
Name of Interviewer: Informant:
August 14, 2020 90%
CD - A Section G Date of Interview: Reliability:
I. General Data
ACOSTA, Alden 28/F SINGLE FILIPINO Completeness
(Name of Patient) (Age) (Sex) (Civil Status) (Nationality) (0) N/A (1) <9 data
(2) >9 data (3) Complete
ROMAN CATHOLIC Call Center Agent 02/23/1992
2/3/1992 Manila
(Religion) (Occupation) (Birthdate) (Birthplace) Recorded in a telegraphed
West Fairview, Quezon City manner
(0) N/A (1) No (2) Yes
(Present Address)
NONE
(No. of times admitted) (Date Admitted)
II. Chief Complaint Briefly written using phrases,
“Sumasakit kanang binti”
and not sentences
(0) N/A (4) No (8) Yes
III. History of Present Illness
8 days prior to consultation the patient experienced an “insect bite” on her right leg, 2 inches below the knee. The Recorded time of onset
patient experience pruritus that provoked her to scratch the area then the area started to bleed. The pain is localized on her properly
right leg. She describes the pain as sponataneuous and increasingly painful. She rated the pain as 8/10 on a pain scale
For the first few days the patient put alcohol as a means to alleviate the pain (0) N/A (3) No (6) Yes
6 days ago she felt a burning sensation on the area and her friend suggested to her a chinese menthol topical solution
and amoxicillin which she is now taking 3 time a day for 5 days, she stated that the pain was reduced only for about 10%.
Observed chronology of
1 day ago, the patient couldn’t walk and can’t her daily tasks because of the pain
symptoms
(0) N/A (4) No (8) Yes
Described symptoms
adequately
(2) <25% (5) 25-50%
(7) 50-75% (10) >75%
Included all pertinent positive
and negative information
regarding the system that may
be associated with each
symptom
(2) <25% (5) 25-50%
(7) 50-75% (10) >75%
Noted consultation done
(0) N/A
(2) Recorded, but inadequate
(4) Recorded data is adequate
Noted medications given
(0) N/A
(2) Recorded, but inadequate
(4) Recorded data is adequate
THE WRITTEN HISTORY IS:
Neat
(1) <50% (2) 50% (3) >50%
Legible
(1) <50% (2) 50% (3) >50%
Properly paragraphed
(1) <50% (2) 50% (3) >50%
Grammatically correct
(2) <50% (3) 50% (5) >50%
With minimal use of
universally accepted
abbreviations
(1) <50% (2) 50% (3) >50%
Brief and concise
(2) <50% (3) 50% (5) >50%
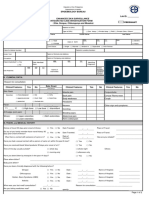
I. Past Medical History [[ ifClick
present,
on theleave
( ) tothe ( )amark.
leave check If absent,
mark. click
Unclick to to remove
remove ( )mark
check mark] ]
measles and chicken pox
Childhood Diseases: (✔) Childhood diseases /
Immunizations: (✔) Hepa B and BCG Immunizations / Adult
Adult Diseases: Diseases / Psychiatric Illnesses
Hypertension: ( ) none (0) (1) (3)
Diabetes: ( ) none
Bronchial Asthma: ( ) none
COPD: ( ) none
Pulmonary Tuberculosis: ( ) none
Myocardial Infarction: ( ) none
Cerebrovascular Accident: ( ) none
Malignancy: ( ) none
Allergies: ( ) none
Psychiatric Illnesses: ( ) none
Previous Surgery: ( ) none Surgical diseases / Gynecologic
Gynecologic Diseases: ( ) none Diseases / Accidents and
Injuries / History of blood
Accidents / Injuries: ( ) none
transfusion
Blood Transfusion: ( ) none
(0) (2) (4)
Others (please specify):
II. Family History Family History
Father: 50 y/o; Hypertensive (0) (1) (3)
Mother: 52y/o; No illness
Siblings: 19; No illness, 18; no illness, 16; no illness
Others: N/A
III. Personal and Social History Personal and Social History
Education: currently in university Marital Status: single (0) (3) (5)
Occupation: part-timer in a call cernter company Lives with: None
Living Condition: Safe, not prone to flood Food Preference: Fatty foods e.g. chicharon
Leisure Activities: take naps Exercise Regimen: 1-2 times per month
Sexual Practices: none Smoking History: 0.4 - 0.6 pack years (2-3 stick 4yrs)
Alcohol Intake: occasional Use of Illicit Drugs: N/A
Others (if applicable):
IV. Obstetric and Menstrual History Obstetric / Menstrual History
12years
Menarche: 12 y/o Interval: regular
Duration: 3-5 days Amount: 2-3 pads / day
(0) (1) (3)
Symptoms: N/A G: 0 P: 0 (T: 0 P: 0 A: 0 L: 0 )
Manner of Delivery: N/A Complications: N/A
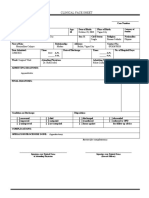
V. Review of Systems [[ ifClick
present,
on theleave
( ) tothe ( )amark.
leave check If absent,
mark. click
Unclick to to remove
remove ( )mark
check mark] ] Review of Systems
Constitutional: ( ) weight loss (0) (3) (5)
Skin: (✔) itchiness, ( ) change in color, ( ) dryness
Head: ( ) vertigo, ( ) dizziness
Eyes: ( ) pain, ( ) blurring of vision, ( ) double vision,
( ) excessive lacrimation, ( ) photophobia, (✔) use of eyeglasses (Reading glasses)
Ears: ( ) earache, ( ) deafness, ( ) tinnitus, ( ) ear discharge
Nose / Sinuses: ( ) change in smell, ( ) nose bleeding, ( ) nasal obstruction, TOTAL SCORE: ___________
( ) nasal discharge, ( ) pain over paranasal sinuses REMARKS:
Mouth / Throat: ( ) toothache, ( ) gum bleeding, ( ) disturbance in taste,
( ) sore throat, ( ) hoarseness
Neck: ( ) pain, ( ) limitation of movement, ( ) presence of mass
Respiratory: ( ) shortness of breath, ( ) difficulty of breathing
Cardiovascular: ( ) substernal pain, ( ) orthopnea, ( ) syncope,
( ) paroxysmal nocturnal dyspnea
Gastrointestinal: ( ) dysphagia, ( ) melena, ( ) hematochezia, ( ) regurgitation
Genitourinary: ( ) anuria, ( ) incontinence, ( ) dysuria, ( ) urinary frequency,
( ) urethral discharge
Extremities: ( ) stiffness, ( ) intermittent claudication,
( ) limitation of movements
Nervous ( ) syncope, ( ) loss of consciousness, ( ) focal weakness,
System: ( ) paralysis, ( ) numbness, ( ) paresthesia, ( ) speech disorder,
( ) loss of memory, ( ) confusion
Hematopoietic: ( ) bleeding tendency, ( ) easy bruising, ( ) pallor
Endocrine: ( ) intolerance to heat and cold, ( ) polyuria, ( ) polydipsia
You might also like
- Nicanor Reyes Medical Foundation: Far Eastern UniversityDocument3 pagesNicanor Reyes Medical Foundation: Far Eastern UniversityEllah GutierrezNo ratings yet
- FEU History and Physical ExaminationDocument4 pagesFEU History and Physical Examinationdonna dominnoNo ratings yet
- ESR Verification Form ReviseDocument4 pagesESR Verification Form ReviseRouella DoverteNo ratings yet
- Coronavirus Disease (COVID-19) : Case Investigation FormDocument2 pagesCoronavirus Disease (COVID-19) : Case Investigation FormJudeLaxNo ratings yet
- DOH PIDSR COVID-19 CIF TemplateDocument1 pageDOH PIDSR COVID-19 CIF TemplateMargaux Faith CCNo ratings yet
- Coronavirus Disease (COVID-19) : Case Investigation FormDocument1 pageCoronavirus Disease (COVID-19) : Case Investigation FormPresinto Dos Parañaque KnightsNo ratings yet
- ZIKA ICIFDocument2 pagesZIKA ICIFMarav SymbNo ratings yet
- CoViD19-CIF-v6-Fillable QCv3-2Document1 pageCoViD19-CIF-v6-Fillable QCv3-2Patrice De CastroNo ratings yet
- Philippine COVID-19 Case Investigation FormDocument2 pagesPhilippine COVID-19 Case Investigation FormChamee MallillinNo ratings yet
- Philippine COVID-19 Case Investigation FormDocument2 pagesPhilippine COVID-19 Case Investigation FormShiela E. EladNo ratings yet
- 2019 Coronavirus Disease (Covid-19) : 1. Patient ProfileDocument1 page2019 Coronavirus Disease (Covid-19) : 1. Patient ProfileMarythel CamachoNo ratings yet
- CoViD19-Covid Investigation FormDocument1 pageCoViD19-Covid Investigation FormMc Arem PaghunasanNo ratings yet
- Coronavirus Disease (COVID-19) : Case Investigation FormDocument1 pageCoronavirus Disease (COVID-19) : Case Investigation FormHerbert Tierra Ponce Jr.100% (1)
- CIF TemplateDocument2 pagesCIF Templateluvaire23No ratings yet
- New Enhanced Zika CIFDocument3 pagesNew Enhanced Zika CIFMarav SymbNo ratings yet
- Coronavirus Disease (COVID-19) : Case Investigation FormDocument1 pageCoronavirus Disease (COVID-19) : Case Investigation FormMizraim TupazNo ratings yet
- CCMC Fwri Sur Report 2022Document3 pagesCCMC Fwri Sur Report 2022CCMC HESUNo ratings yet
- 5 - Causality Assessment FormDocument7 pages5 - Causality Assessment Formramanan13No ratings yet
- Health Registration Form - InternationalDocument3 pagesHealth Registration Form - Internationaldolapo BalogunNo ratings yet
- Coronavirus Disease (COVID-19) : Philippine National Police Health Service PNP General HospitalDocument1 pageCoronavirus Disease (COVID-19) : Philippine National Police Health Service PNP General HospitalKarsenley Cal-el Iddig BurigsayNo ratings yet
- Philippine Chikungunya Case Report FormDocument2 pagesPhilippine Chikungunya Case Report FormTin Causaren-Gertos100% (1)
- Philippine Disease Surveillance Form GuideDocument2 pagesPhilippine Disease Surveillance Form GuideNovie FeneciosNo ratings yet
- Typhoid Fever Surveillance ReportDocument2 pagesTyphoid Fever Surveillance ReportMarketing HydNo ratings yet
- Media Bulletin 17-04-2021Document36 pagesMedia Bulletin 17-04-2021Venkatraman PoreddyNo ratings yet
- RECORDING Form 1: MR-TD (6-7 Years Old) : Community-Based Immunization ActivityDocument2 pagesRECORDING Form 1: MR-TD (6-7 Years Old) : Community-Based Immunization ActivityLiza Domingo100% (2)
- Clinical Treatment PDFDocument1 pageClinical Treatment PDFDanielle YoderNo ratings yet
- Clinical Face Sheet: October 23, 2003 Vigan City Single Roman Catholic FilipinoDocument15 pagesClinical Face Sheet: October 23, 2003 Vigan City Single Roman Catholic FilipinoCaitlynNo ratings yet
- Coronavirus Disease (COVID-19) : Case Investigation FormDocument1 pageCoronavirus Disease (COVID-19) : Case Investigation FormBabiejoy Beltran AceloNo ratings yet
- Coronavirus Disease (COVID-19) : Case Investigation FormDocument1 pageCoronavirus Disease (COVID-19) : Case Investigation FormBabiejoy Beltran AceloNo ratings yet
- Requisition For Medical Imaging and Interventional ProceduresDocument2 pagesRequisition For Medical Imaging and Interventional ProceduresokamiotokoNo ratings yet
- COMMUNITY - Based Immunization Activity RECORDING Form 1: MR - TD (6 - 7 Years Old)Document8 pagesCOMMUNITY - Based Immunization Activity RECORDING Form 1: MR - TD (6 - 7 Years Old)MarhonKarlCabildoNo ratings yet
- Practice Fusion - PrintChartDocument10 pagesPractice Fusion - PrintChartGet Well SoonNo ratings yet
- Apollo Lighthouse-CarmDocument4 pagesApollo Lighthouse-CarmN dasNo ratings yet
- Entry Medical Examination: ConfidentialDocument4 pagesEntry Medical Examination: ConfidentialTamba KendemaNo ratings yet
- LDSS-2221A Report of Suspected Child Abuse or MaltreatmentDocument3 pagesLDSS-2221A Report of Suspected Child Abuse or Maltreatmentjaydoc_paed@yahoo.co.inNo ratings yet
- Clinical Face Sheet: 8:13 A.M. - P.M. - A.M. - P.MDocument19 pagesClinical Face Sheet: 8:13 A.M. - P.M. - A.M. - P.MKyle Audrie ArcalasNo ratings yet
- REGISTER PELAYANAN KORBAN KEKEJAMANDocument33 pagesREGISTER PELAYANAN KORBAN KEKEJAMANSulikaNo ratings yet
- Whatcom County Health Department: Confidential Sexually Transmitted Disease Case ReportDocument2 pagesWhatcom County Health Department: Confidential Sexually Transmitted Disease Case Reportfuck youNo ratings yet
- Case Lnvestigation FormDocument3 pagesCase Lnvestigation FormChum ChitaruNo ratings yet
- Respon Dalam Pelaporan SKDRDocument26 pagesRespon Dalam Pelaporan SKDRMoh Syukron Khaerudin SKMNo ratings yet
- Clinical Treatment Form: I DIAGNOSES (Must Be To The Highest Level of Specificity)Document1 pageClinical Treatment Form: I DIAGNOSES (Must Be To The Highest Level of Specificity)Danielle YoderNo ratings yet
- 3 Chronic or Inactive Conditions: UnableDocument4 pages3 Chronic or Inactive Conditions: UnableMargaretNo ratings yet
- ESR Verification FormDocument2 pagesESR Verification Formlance tabinas83% (6)
- MediExpress Medical Reimbursement FormDocument2 pagesMediExpress Medical Reimbursement FormAtiko Atochi100% (1)
- Broqueza, Jonnel Regoris: Philippine Children's Medical CenterDocument1 pageBroqueza, Jonnel Regoris: Philippine Children's Medical CenterRica RegorisNo ratings yet
- TYPED-medical SoftDocument5 pagesTYPED-medical SoftynrajambaNo ratings yet
- ESR Form GrezDocument2 pagesESR Form Grezlizabernard.hernandezNo ratings yet
- The Benefits Center P.O. Box 100158 Columbia, SC 29202-3158 Toll-Free: 1-800-858-6843 Fax: 1-800-447-2498 Call Toll-Free Monday Through Friday, 8 A.M. To 8 P.M. (Eastern Time)Document2 pagesThe Benefits Center P.O. Box 100158 Columbia, SC 29202-3158 Toll-Free: 1-800-858-6843 Fax: 1-800-447-2498 Call Toll-Free Monday Through Friday, 8 A.M. To 8 P.M. (Eastern Time)paul geyerNo ratings yet
- Moderators Mediators and Other Predictors of Risperidone Response in Children With Autistic Disorder and IrritabilityDocument12 pagesModerators Mediators and Other Predictors of Risperidone Response in Children With Autistic Disorder and IrritabilityRobson ZazulaNo ratings yet
- Ely. Delirium SlidesDocument51 pagesEly. Delirium SlidesParvathy R NairNo ratings yet
- 7 M None X R-11/1/21 Religion: RECORDING FORM 1. MR-TD (6-7 Years Old)Document3 pages7 M None X R-11/1/21 Religion: RECORDING FORM 1. MR-TD (6-7 Years Old)Jasmin Kerre Villarin100% (1)
- Dr. Nur Farhanah - SPEED TetanusDocument24 pagesDr. Nur Farhanah - SPEED TetanusJonathan IngramNo ratings yet
- Public Health IT Unit 6: Biosurveillance Lecture aDocument44 pagesPublic Health IT Unit 6: Biosurveillance Lecture aBobNo ratings yet
- Esr TemplateDocument2 pagesEsr TemplateR'mon Ian SantosNo ratings yet
- (Pink) /merah Muda Victim Identification Form/ B0: Jenis Bencana Tempat Bencana Tanggal BencanaDocument21 pages(Pink) /merah Muda Victim Identification Form/ B0: Jenis Bencana Tempat Bencana Tanggal BencanaUsbahNo ratings yet
- Tracking Gastro OutbreakDocument3 pagesTracking Gastro OutbreakHANS BENNo ratings yet
- MRI of Degenerative Disease of the Spine: A Case-Based AtlasFrom EverandMRI of Degenerative Disease of the Spine: A Case-Based AtlasNo ratings yet
- One Step Med: General Medical Information Record Keeping ManualFrom EverandOne Step Med: General Medical Information Record Keeping ManualNo ratings yet
- Sexual Assault: A Color AtlasFrom EverandSexual Assault: A Color AtlasRating: 5 out of 5 stars5/5 (1)
- Clinical Applications of Optical Coherence Tomography AngiographyFrom EverandClinical Applications of Optical Coherence Tomography AngiographyNo ratings yet
- Typhoid Fever Final 2Document28 pagesTyphoid Fever Final 2gAARaNo ratings yet
- Study Skills HandoutDocument7 pagesStudy Skills Handoutapi-358787203No ratings yet
- Alcoholism FinalDocument41 pagesAlcoholism FinalgAARaNo ratings yet
- Future of The Medication Use SystemDocument7 pagesFuture of The Medication Use SystemgAARaNo ratings yet
- How Typhoid Fever Spreads Through Contaminated Food and WaterDocument1 pageHow Typhoid Fever Spreads Through Contaminated Food and WatergAARaNo ratings yet
- Vii - Sacraments IntroductionDocument28 pagesVii - Sacraments IntroductiongAARaNo ratings yet
- USP Specific Gravity Test GuideDocument1 pageUSP Specific Gravity Test GuideSarah TahirNo ratings yet
- Typhoid FeverDocument4 pagesTyphoid FevergAARaNo ratings yet
- Differences Between Prokaryotic and Eukaryotic CellsDocument15 pagesDifferences Between Prokaryotic and Eukaryotic CellsgAARaNo ratings yet
- Hong Kong KalachuchiDocument3 pagesHong Kong KalachuchigAARaNo ratings yet
- Baptism: Gateway to New Life in ChristDocument29 pagesBaptism: Gateway to New Life in ChristgAARaNo ratings yet
- Logic - 2Document12 pagesLogic - 2gAARa100% (1)
- Xiii MatrimonyDocument17 pagesXiii MatrimonygAARaNo ratings yet
- 8 Muscles IntroDocument102 pages8 Muscles IntrogAARaNo ratings yet
- Xiv Holy OrdersDocument25 pagesXiv Holy OrdersDiane ApostolNo ratings yet
- Xi ReconciliationDocument17 pagesXi ReconciliationgAARaNo ratings yet
- X EucharistDocument24 pagesX EucharistgAARaNo ratings yet
- Logic - 1Document17 pagesLogic - 1gAARaNo ratings yet
- How Can I Improve My Emotional Health?Document6 pagesHow Can I Improve My Emotional Health?gAARaNo ratings yet
- SeizuresDocument18 pagesSeizuresgAARaNo ratings yet
- Noli Me Tangere: A Diagnosis of Our Filipino SocietyDocument15 pagesNoli Me Tangere: A Diagnosis of Our Filipino SocietyHowo4Die100% (10)
- Hand Out Rizal Law & HistoryDocument4 pagesHand Out Rizal Law & HistorygAARaNo ratings yet
- Logic - IDocument14 pagesLogic - IgAARaNo ratings yet
- Histology and Physiology of Bones: OsteonDocument54 pagesHistology and Physiology of Bones: OsteonAnwar815100% (2)
- Hand Out Definition of A HeroDocument12 pagesHand Out Definition of A HerogAARaNo ratings yet
- 12-13 Spectroscopy LabDocument8 pages12-13 Spectroscopy LabgAARaNo ratings yet
- Flow Charting LectureDocument12 pagesFlow Charting Lectureyoej2121No ratings yet
- List of Parasitic OrganismsDocument4 pagesList of Parasitic OrganismsgAARaNo ratings yet
- Mga Piling Terminolohiyang Ginagamit Sa Farmasia ThesisDocument2 pagesMga Piling Terminolohiyang Ginagamit Sa Farmasia ThesisgAARaNo ratings yet
- DapusDocument3 pagesDapussutisnoNo ratings yet
- Most Common Medical ErrorsDocument4 pagesMost Common Medical ErrorsAlNo ratings yet
- Pulmonary FibrosisDocument4 pagesPulmonary FibrosisDimpal Choudhary100% (2)
- RATHL Trial SummaryDocument5 pagesRATHL Trial SummaryDr.ImaanNo ratings yet
- AlugbatiDocument2 pagesAlugbatiFaith WangNo ratings yet
- Chapter 4 - Technologies That Enable MobilityDocument48 pagesChapter 4 - Technologies That Enable Mobilitysara sallaqNo ratings yet
- Bio Project On Immunity Class 12Document19 pagesBio Project On Immunity Class 12fizakouser1216100% (1)
- 3RD Term S1 BiologyDocument37 pages3RD Term S1 Biologyabdulsalam musharrafNo ratings yet
- Ucspshs q1 Mod4 HumanBioCulturalEvolutionDocument34 pagesUcspshs q1 Mod4 HumanBioCulturalEvolutionTosee istosee100% (1)
- JCI TT BidDocument9 pagesJCI TT BidJanis Medina ReginioNo ratings yet
- General Animal Surgery and Anaesthesiology (VetBooks - Ir)Document430 pagesGeneral Animal Surgery and Anaesthesiology (VetBooks - Ir)Giovana BragaNo ratings yet
- (Tim Lang, Michael Heasman) Food Wars The GlobalDocument385 pages(Tim Lang, Michael Heasman) Food Wars The GlobalNitish Gautam100% (1)
- Urethral StrictureDocument35 pagesUrethral StrictureDoctors PodcastNo ratings yet
- Pathology, Lecture 7 (Lecture Notes)Document15 pagesPathology, Lecture 7 (Lecture Notes)Ali Al-Qudsi100% (3)
- Covid Truth Resources - 8-21-2021Document18 pagesCovid Truth Resources - 8-21-2021Todd Herman93% (27)
- HS 3311 W5 Summary of The Article Effect of Cheese Intake On Cardiovascular Diseases and Cardiovascular BiomarkersDocument6 pagesHS 3311 W5 Summary of The Article Effect of Cheese Intake On Cardiovascular Diseases and Cardiovascular BiomarkersAdanigbo MagretNo ratings yet
- 326 Musculoskeletal Assessment Fa10Document36 pages326 Musculoskeletal Assessment Fa10arjetahoward100% (1)
- Assisting in Thoracostomy Tube InsertionDocument54 pagesAssisting in Thoracostomy Tube Insertioncoosa liquorsNo ratings yet
- Initial Patient AssessmentDocument13 pagesInitial Patient AssessmentJolly RancherNo ratings yet
- Chapter 30 DISORDERS OF THE SLEEPDocument6 pagesChapter 30 DISORDERS OF THE SLEEPZahra Margrette SchuckNo ratings yet
- 3 Features of Public HealthDocument12 pages3 Features of Public HealthMoreiyamNo ratings yet
- Att 1446693658204 المذكرة-الذهبيةDocument80 pagesAtt 1446693658204 المذكرة-الذهبيةShady KhamisNo ratings yet
- Hip Dysplasia ResearchDocument119 pagesHip Dysplasia ResearchAnand RajNo ratings yet
- DR Jockers Cleanse Your Liver Now UpdatedDocument102 pagesDR Jockers Cleanse Your Liver Now UpdatedfizzNo ratings yet
- Pre-Test Psychiatric NursingDocument17 pagesPre-Test Psychiatric NursingDefensor Pison Gringgo100% (1)
- Sarvangasana (All Member's Pose) : TechniqueDocument1 pageSarvangasana (All Member's Pose) : TechniqueKarisma SenapatiNo ratings yet
- PhysioEx Exercise 11 Activity 3Document3 pagesPhysioEx Exercise 11 Activity 3MEGAN NICOLE PERNILLA HERNANDEZNo ratings yet
- Bataan National High School Genre IdentificationDocument10 pagesBataan National High School Genre IdentificationMarc Andrei MirandaNo ratings yet
- Selective Androgen Receptor ModulatorsDocument7 pagesSelective Androgen Receptor ModulatorsRafael HelenoNo ratings yet
- Neonatal JaundiceDocument36 pagesNeonatal JaundiceJenaffer Achamma JohnNo ratings yet