Professional Documents
Culture Documents
Surgical Antibiotic Prophylaxis Guideline 220719
Surgical Antibiotic Prophylaxis Guideline 220719
Uploaded by
Agil BredlyCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Surgical Antibiotic Prophylaxis Guideline 220719
Surgical Antibiotic Prophylaxis Guideline 220719
Uploaded by
Agil BredlyCopyright:
Available Formats
Guideline
Surgical Antibiotic Prophylaxis Guideline
1. Purpose
The purpose of this guideline is to optimise the use of antibiotic prophylaxis for surgical procedures at the
Women’s in Parkville and in Sandringham.
Surgical site infections (SSIs) are a common adverse event in hospitalised patients1; 8-10% of gynaecological
surgery patients undergoing an operative procedure will develop an SSI 2. SSIs have been shown to increase
mortality, readmission rate and length of hospital stay3,4. Appropriate and timely antibiotic prophylaxis has been
shown to be highly effective in reducing the incidence of SSI5. The need for surgical antibiotic prophylaxis
varies according to the type of procedure and its associated risk of SSI.
A number of studies across a range of surgical procedures have shown that there is a narrow window of
opportunity for the administration of effective antimicrobial prophylaxis6. Antibiotics need to be present in the
tissue at the time of incision in order to be effective7.
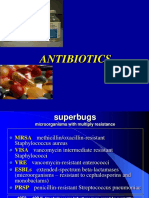
Ideally prophylactic antibiotics should cover the narrowest spectrum of organisms possible in order to minimise
the development of bacterial resistance8. For this reason it is important to consider the likely source of
pathogens in each type of surgery. For most infections that occur after obstetric or gynaecological surgery, the
source of pathogens is the endogenous flora of the patient’s vagina or skin. The endogenous flora of the
genital tract is polymicrobial, consisting of anaerobes, Gram negative aerobes and Gram positive cocci. In
contrast, laparoscopic procedures that do not breach any mucosal surfaces are more commonly contaminated
with skin organisms only (usually Gram positive organisms such as Staphylococci).
2. Definitions
Surgical site infection is an infection that occurs after surgery in the part of the body where the surgery took
place.
Antibiotic prophylaxis is the use of antibiotics before, during, or after a diagnostic, therapeutic, or surgical
procedure to prevent infectious complications. For surgical prophylaxis, these can generally be given prior to
surgical incision.
3. Responsibilities
Surgeons are responsible for requesting the timely administration of appropriate antibiotic prophylaxis for their
surgical patients.
Anaesthetists are responsible for liaison with surgeons and the provision of appropriate and timely antibiotic
prophylaxis.
Pharmacists are responsible for ensuring prompt availability of required antibiotics. They are also responsible
for provision of information to medical and nursing staff regarding doses of antibiotics and administration.
4. Guideline
Table 1 outlines recommended timing and choice of prophylactic antibiotics for surgical procedures at the
Women’s.
An alternative choice of antibiotic is provided where appropriate (e.g. for a patient with penicillin allergy).
The National Health and Medical Research Council (NHMRC) level of evidence for each recommendation is
included in the Table. For some procedures, such as Caesarean section and hysterectomy, antibiotic
prophylaxis is clearly indicated. For other procedures, such as insertion of an intra-uterine device, medical
termination of pregnancy and diagnostic laparoscopy, antibiotic prophylaxis is usually not required. For other
procedures, the evidence is less clear and recommendations are based upon expert agreement until further
research evidence becomes available.
Uncontrolled document when printed Published: (19/07/2019) Page 1 of 7
Guideline
Surgical Antibiotic Prophylaxis Guideline
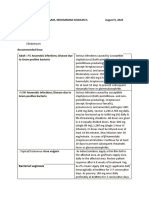
Table 1: Antibiotics for surgical prophylaxis
Patients with immediate hypersensitivity reactions (eg. urticaria, angio-oedema, bronchospasm, anaphylaxis) to
penicillins, avoid use of penicillins and cephalosporins.
Patients allergic to penicillins (excluding immediate hypersensitivity reactions eg. urticaria, angio-oedema,
bronchospasm and anaphylaxis), use of cephalosporins can be considered.
Surgery 1st line Level of Alternative Comments
evidence9
Obstetric
Caesarean section10-13 Cefazolin I Clindamycin 600 mg IV over at Antibiotics
(cephazolin) 2 g IV, least 20 minutes, within 60 prior to skin
within 60 minutes minutes (ideally 15-30 incision reduce
(ideally 15-30 minutes) before surgical maternal
minutes) before skin incision infection rate
incision. in emergency
or
caesarean
Vancomycin 25 mg/kg IV section.
(maximum 2g)
Termination of Screen patient for Consensus If STI screening not performed
pregnancy (surgical)13- STIs: C. trachomatis, or results unavailable:
16 N. gonorrhoeae, M.
Azithromycin 1 g oral stat
genitalium and
bacterial vaginosis.
Treat the woman
and her partner(s)
prior to ToP17.
Termination of Not indicated I
pregnancy (medical)13
Manual removal of Cefazolin III-3 Clindamycin 600 mg IV
placenta18-19 (cephazolin) 2 g IV,
+
at the time of
induction Gentamicin 2 mg/kg IV
(maximum 560 mg)
+
Metronidazole 500
mg IV, ending the
infusion at the time
of induction
3rd and 4th degree Cefazolin Consensus Clindamycin 600 mg IV
vaginal tears13,20-24 (cephazolin) 2 g IV
+
within 60 minutes
(ideally 15-30 15-30 Gentamicin 2 mg/kg IV
minutes) before the (maximum 560 mg) within 60
repair minutes (ideally 15-30
minutes) before the repair
+
Followed by
Metronidazole 500
trimethoprim/sulfamethoxazole
mg IV within 60
160/800 orally BD +
minutes (ideally 15-
Uncontrolled document when printed Published: (19/07/2019) Page 2 of 7
Guideline
Surgical Antibiotic Prophylaxis Guideline
30 minutes) before metronidazole 400mg orally
the repair BD for 7 days
Followed by
amoxicillin/clavulanic
acid 875/125 orally
BD for 7 days
Cefalexin
(cephalexin) 500mg
orally QID +
metronidazole
400mg orally BD can
be used as an
alternative regimen)
Gynaecological
Note: Prophylactic antibiotics for vaginal packs can be administered for the duration of vaginal pack use which is
usually 24-48 hours.33
Hysterectomy Cefazolin I Clindamycin 600mg IV + Patients
(cephazolin) 2 g IV, should be
(vaginal)13,25 Gentamicin 2mg/kg IV
within 60 minutes screened and
(maximum 560 mg)
(ideally 15-30 treated for
minutes) before bacterial
surgical incision vaginosis
(repeat dose if before
procedure > 3 hours) hysterectomy27
+
Metronidazole 500
mg IV, within 60
minutes (ideally 15-
30 minutes) before
surgical incision
Hysterectomy Cefazolin I Clindamycin 600mg IV over at
(cephazolin) 2 g IV, least 20 minutes, within 60
(abdominal) 13,26
within 60 minutes minutes (ideally 15-30
(ideally 15-30 minutes) before surgical
minutes) before incision
surgical incision
or
(repeat dose if
procedure > 3 hours) Vancomycin 25 mg/kg IV
(maximum 2g)
Urogynaecological Cefazolin III-3 Clindamycin 600mg IV +
procedures (mid- (cephazolin) 2 g IV,
Consensus Gentamicin 2mg/kg IV
urethral sling/TVT, within 60 minutes
(maximum 560 mg)
colposuspension, (ideally 15-30
vaginal prolapse minutes) before
surgery +/- surgical incision
mesh/SSF)28 (repeat dose if
procedure > 3 hours)
Uncontrolled document when printed Published: (19/07/2019) Page 3 of 7
Guideline
Surgical Antibiotic Prophylaxis Guideline
+
Metronidazole 500
mg IV, within 60
minutes (ideally 15-
30 minutes) before
surgical incision
Hysterosalpingography Azithromycin 1 g oral Consensus
or Hysterosocopy or stat
Chromotubation for
patients with dilated
tubes or a history of PID
or tubal damage28
Hysterosalpingography Not indicated IV
or Hysterosocopy or
Chromotubation with
NO history of PID and
normal tubes on
visualisation29
IUD insertion30 Not indicated I Patients
should be
screened and
treated for
STIs prior to
insertion: C.
trachomatis,
N.
gonorrhoeae,
M. genitalium
and bacterial
vaginosis.
Endometrial biopsy31 Not indicated IV
Laparoscopy32 Not indicated II
(diagnostic or
laparoscopy without
breaching
bowel/uterine/vaginal
cavity)
Laparoscopy Cefazolin Consensus Clindamycin 600 mg IV +
(cephazolin) 2 g IV,
(breach of Gentamicin 2 mg/kg IV
within 60 minutes
bowel/uterine/vaginal (maximum 560mg)
(ideally 15-30
cavity or conversion to
minutes) before
operative laparotomy)
surgical incision
(repeat dose if
procedure > 3 hours)
+
Metronidazole 500
mg IV, within 60
minutes (ideally 15-
Uncontrolled document when printed Published: (19/07/2019) Page 4 of 7
Guideline
Surgical Antibiotic Prophylaxis Guideline
30 minutes) before
surgical incision
NHMRC Levels of Evidence9:
Level I: A systematic review of level II studies
Level II: A randomised controlled trial
Level III-1: A pseudo-randomised controlled trial
Level III-2: A comparative study with concurrent controls
Level III-3: A comparative study without concurrent controls
Level IV: A case series with either post-test outcomes or pre-test/ post-test outcomes
5. Evaluation, monitoring and reporting of compliance to this guideline
Compliance to this guideline or procedure will be monitored, evaluated and reported through:
1. Review of hysterectomy and caesarean surgical site infection rate
2. Spot audits of practice under the Quality Use of Medicines program
3. Laboratory review of infection clusters and antimicrobial resistance
6. References
1. ACOG practice bulletin No. 104: antibiotic prophylaxis for gynecologic procedures. Obstet Gynecol
2009;113:1180-9.
2. Kamat AA, Brancazio L, Gibson M. Wound infection in gynecologic surgery. Infect Dis Obstet Gynecol
2000;8:230-4.
3. Australian Council for Safety and Quality in Health Care. Preventing Surgical Site Infection: Toolkit. In;
2011.
4. Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ. The impact of surgical-site infections in the
1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp
Epidemiol 1999;20:725-30.
5. Steinberg JP, Braun BI, Hellinger WC, et al. Timing of antimicrobial prophylaxis and the risk of surgical site
infections: results from the Trial to Reduce Antimicrobial Prophylaxis Errors. Ann Surg 2009;250:10-6.
6. Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, Burke JP. The timing of prophylactic
administration of antibiotics and the risk of surgical-wound infection. N Engl J Med 1992;326:281-6.
7. Burke JF. The effective period of preventive antibiotic action in experimental incisions and dermal lesions.
Surgery 1961;50:161-8.
8. Weinstein JW, Roe M, Towns M, et al. Resistant enterococci: a prospective study of prevalence, incidence,
and factors associated with colonization in a university hospital. Infect Control Hosp Epidemiol 1996;17:36-
41.
9. National Health and Medical Research Council. NHMRC levels of evidence and grades for
recommendations for developers of guidelines: National Health and Medical Research Council; 2009.
10. Smaill FM, Gyte GM. Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean
section. Cochrane Database Syst Rev 2014:CD007482.
11. Costantine MM, Rahman M, Ghulmiyah L, et al. Timing of perioperative antibiotics for cesarean delivery: a
Uncontrolled document when printed Published: (19/07/2019) Page 5 of 7
Guideline
Surgical Antibiotic Prophylaxis Guideline
metaanalysis. Am J Obstet Gynecol 2008;199:301 e1-6.
12. Gyte GM, Dou L, Vazquez JC. Different classes of antibiotics given to women routinely for preventing
infection at caesarean section. Cochrane Database Syst Rev 2014:CD008726.
13. eTG July 2016 edition: Antibiotics. Accessed via
https://tgldcdp.tg.org.au.acs.hcn.com.au/topicTeaser?guidelinePage=Antibiotic&etgAccess=true on 6 Jan
2019
14. Low N, Mueller M, Van Vliet HAAM, Kapp N. Perioperative antibiotics to prevent infection after first-
trimester abortion. Cochrane Database Syst Rev 2012:CD005217.
15. The care of women requesting induced abortion. RCOG Evidence-based Clinical Guideline, Number 7.
November 2011. (Accessed at https://www.rcog.org.uk/globalassets/documents/guidelines/abortion-
guideline_web_1.pdf - Copy and Paste into browser to view)
16. Sawaya GF, Grady D, Kerlikowske K, Grimes DA. Antibiotics at the time of induced abortion: the case for
universal prophylaxis based on a meta-analysis. Obstet Gynecol 1996;87:884-90.
17. Cameron ST, Sutherland S. Universal prophylaxis compared with screen-and-treat for Chlamydia
trachomatis prior to termination of pregnancy. BJOG 2002;109:606-9.
18. Ely JW, Rijhsinghani A, Bowdler NC, Dawson JD. The association between manual removal of the
placenta and postpartum endometritis following vaginal delivery. Obstet Gynecol 1995;86:1002-6.
19. WHO guidelines for the management of postpartum haemorrhage and retained placenta 2009.
20. Duggal N, Mercado C, Daniels K, Bujor A, Caughey AB, El-Sayed YY. Antibiotic prophylaxis for prevention
of postpartum perineal wound complications: a randomized controlled trial. Obstet Gynecol 2008;111:1268-
73.
21. Robson S, Higgs P. Third- and fourth-degree injuries. RANZCOG O&G Magazine 2011; 13(2): 20-22.
22. The management of third- and fourth-degree perineal tears. RCOG Green-top Guideline No.29. June 2015.
23. Monash Health Clinical Guideline: Perineal trauma management. 2015.
24. Buppasiri P, Lumbiaganon P, Thinkhamrop J, Thinkhamrop B. Antibiotic prophylaxis for third- and fourth-
degree perineal tear during vaginal birth. Cochrane Database Systematic Reviews. 2014.
25. Duff P, Park RC. Antibiotic prophylaxis in vaginal hysterectomy: a review. Obstet Gynecol 1980;55:193S-
202S.
26. Tanos V, Rojansky N. Prophylactic antibiotics in abdominal hysterectomy. J Am Coll Surg 1994;179:593-
600.
27. Larsson PG, Carlsson B. Does pre- and postoperative metronidazole treatment lower vaginal cuff infection
rate after abdominal hysterectomy among women with bacterial vaginosis? Infect Dis Obstet Gynecol
2002;10:133-40.
28. Antibiotic prophylaxis in gynaecologic procedures. SOGC Clinical Practice Guideline No.275. April 2012
29. Kasius JC, Broekmans FJ, Fauser BC, Devroey P, Fatemi HM. Antibiotic prophylaxis for hysteroscopy
evaluation of the uterine cavity. Fertil Steril 2011;95:792-4.
30. Grimes DA, Schulz KF. Prophylactic antibiotics for intrauterine device insertion: a metaanalysis of the
randomized controlled trials. Contraception 1999;60:57-63.
31. Foden-Shroff J, Redman CW, Tucker H, et al. Do routine antibiotics after loop diathermy excision reduce
morbidity? Br J Obstet Gynaecol 1998;105:1022-5.
32. Kocak I, Ustun C, Emre B, Uzel A. Antibiotics prophylaxis in laparoscopy. Ceska Gynekol 2005;70:269-72.
33. Georgiou C. Balloon tamponade in the management of postpartum haemorrhage: a review. BJOG
2009;116:748-757.
Uncontrolled document when printed Published: (19/07/2019) Page 6 of 7
Guideline
Surgical Antibiotic Prophylaxis Guideline
7. Legislation/Regulations related to this guideline
C. trachomatis and N. gonorrhoeae infection are Department of Health notifiable conditions. Forms for
notification can be found at http://ideas.health.vic.gov.au/notifying/what-to-notify.asp.
Please ensure that you adhere to the below disclaimer:
PGP Disclaimer Statement
The Royal Women's Hospital Clinical Guidelines present statements of 'Best Practice' based on thorough evaluation of
evidence and are intended for health professionals only. For practitioners outside the Women’s this material is made
available in good faith as a resource for use by health professionals to draw on in developing their own protocols, guided by
published medical evidence. In doing so, practitioners should themselves be familiar with the literature and make their own
interpretations of it.
Whilst appreciable care has been taken in the preparation of clinical guidelines which appear on this web page, the Royal
Women's Hospital provides these as a service only and does not warrant the accuracy of these guidelines. Any
representation implied or expressed concerning the efficacy, appropriateness or suitability of any treatment or product is
expressly negated
In view of the possibility of human error and / or advances in medical knowledge, the Royal Women's Hospital cannot and
does not warrant that the information contained in the guidelines is in every respect accurate or complete. Accordingly, the
Royal Women's Hospital will not be held responsible or liable for any errors or omissions that may be found in any of the
information at this site.
You are encouraged to consult other sources in order to confirm the information contained in any of the guidelines and, in
the event that medical treatment is required, to take professional, expert advice from a legally qualified and appropriately
experienced medical practitioner.
NOTE: Care should be taken when printing any clinical guideline from this site. Updates to these guidelines will take place
as necessary. It is therefore advised that regular visits to this site will be needed to access the most current version of these
guidelines.
Uncontrolled document when printed Published: (19/07/2019) Page 7 of 7
You might also like
- Paediatric Cardiac Surgical Antibiotic Prophylaxis: PurposeDocument9 pagesPaediatric Cardiac Surgical Antibiotic Prophylaxis: PurposeZamzam DomaNo ratings yet
- Antibiotic ProphylaxisDocument2 pagesAntibiotic Prophylaxisabdelhamed aliNo ratings yet
- AHS антибиотики рекомендацDocument42 pagesAHS антибиотики рекомендацMaksym DemianchukNo ratings yet
- Guideline For Antimicrobial Use in The Orthopaedic and Trauma Department..Document8 pagesGuideline For Antimicrobial Use in The Orthopaedic and Trauma Department..Long Nguyễn HoàngNo ratings yet
- Misoprostol Dosages For Reproductive HealthDocument1 pageMisoprostol Dosages For Reproductive HealthAnonymous b6xAErNo ratings yet
- Antibiotics Surgical ProphylaxisDocument4 pagesAntibiotics Surgical ProphylaxisAshraf AlbhlaNo ratings yet
- Dosage Guidelines: Misoprostol in Obstetrics and GynaecologyDocument1 pageDosage Guidelines: Misoprostol in Obstetrics and GynaecologyFlorantia Setya NugrohoNo ratings yet
- Antibiotic/Antiviral Policy - Paediatric PCF (EWMSCDocument9 pagesAntibiotic/Antiviral Policy - Paediatric PCF (EWMSCLizbet parrondoNo ratings yet
- Antibiotic PolicyDocument10 pagesAntibiotic Policykrutarth shahNo ratings yet
- Fournier's Gangrene GuidelinesDocument2 pagesFournier's Gangrene GuidelinesDavid Morales ZepedaNo ratings yet
- AntibiocardDocument25 pagesAntibiocardchildicuNo ratings yet
- Dwita Erca 2016-096 NASKAH PUBLIKASIDocument6 pagesDwita Erca 2016-096 NASKAH PUBLIKASIDwita Erca CintikaNo ratings yet
- Iraqi Ministry of Health Medical City Baghdad Teaching Hospital Training Center of Clinical PharmacyDocument12 pagesIraqi Ministry of Health Medical City Baghdad Teaching Hospital Training Center of Clinical PharmacyDergam HaithamNo ratings yet
- Adult Antibiotic Prophylaxis For Urological SurgeryDocument1 pageAdult Antibiotic Prophylaxis For Urological Surgeryalexander renandhaNo ratings yet
- Sepsis and Catheter Infections: Early Conversion From IV To Oral AntibioticsDocument4 pagesSepsis and Catheter Infections: Early Conversion From IV To Oral AntibioticsChaim HerreraNo ratings yet
- SHC Antimicrobial Prophylaxis in Surgery RecommendationsDocument3 pagesSHC Antimicrobial Prophylaxis in Surgery RecommendationsCatherine MorrisNo ratings yet
- Antibiotic Prophylaxis OrthoDocument4 pagesAntibiotic Prophylaxis OrthoDonNo ratings yet
- Antimicrobial PDFDocument7 pagesAntimicrobial PDFvhonNo ratings yet
- Paclitaxel With EC Adjuvant or Neoadjuvant Protocol V1.1Document7 pagesPaclitaxel With EC Adjuvant or Neoadjuvant Protocol V1.1smokkerNo ratings yet
- SHC Open Fracture ABX Prophylaxis GuidelineDocument2 pagesSHC Open Fracture ABX Prophylaxis GuidelineAulia OkhidNo ratings yet
- Antibiotic Guidelines For PediatricsDocument33 pagesAntibiotic Guidelines For PediatricsVarshini Tamil SelvanNo ratings yet
- Seminar On Standing Orders and Protocols and Use of Selected Life SavingDocument18 pagesSeminar On Standing Orders and Protocols and Use of Selected Life Savingmalathi100% (1)
- Obstetrics / Gynaecological Infections: Indications First Line AlternateDocument2 pagesObstetrics / Gynaecological Infections: Indications First Line AlternateAli ShanNo ratings yet
- Guia Antibioticos UssDocument31 pagesGuia Antibioticos UssSilvia Pancca AmadoNo ratings yet
- D-6-12 Sanaani, Mohammad Khaisar H. August 9, 2020: Bacterial VaginosisDocument4 pagesD-6-12 Sanaani, Mohammad Khaisar H. August 9, 2020: Bacterial VaginosisKenMNo ratings yet
- Paclitaxel Trastuzumab Breast Cancer ProtocolDocument9 pagesPaclitaxel Trastuzumab Breast Cancer ProtocolsmokkerNo ratings yet
- Mistaprostal Cytotec Antiulcer Agents, Cytoprotective Agents Preg. Cat XDocument1 pageMistaprostal Cytotec Antiulcer Agents, Cytoprotective Agents Preg. Cat Xgeorgeloto12100% (1)
- Premedikasi Dan Cinv: (Chemotherapy Induced Nausea and Vomiting)Document22 pagesPremedikasi Dan Cinv: (Chemotherapy Induced Nausea and Vomiting)Yulian 53No ratings yet
- DR Atiq Homeopathic AlternativesDocument3 pagesDR Atiq Homeopathic AlternativessillymindsNo ratings yet
- Surgical Site Infection (SSI)Document3 pagesSurgical Site Infection (SSI)Sahrul RiadiNo ratings yet
- PDF Surgical Prophylaxis Poster Dec 2021Document1 pagePDF Surgical Prophylaxis Poster Dec 2021Midhun KishorNo ratings yet
- Drug Study CytotecDocument2 pagesDrug Study CytotecJahmil DulatreNo ratings yet
- Ny Diabetic Foot Infection Antibiotic Treatment Guidelines 2020Document1 pageNy Diabetic Foot Infection Antibiotic Treatment Guidelines 2020Aliyu labboNo ratings yet
- AminoglycosidesDocument3 pagesAminoglycosidesAbo DowiaNo ratings yet
- Oxaciline PDFDocument7 pagesOxaciline PDFamatoryfictionliteraNo ratings yet
- Pumonary Tuberculosis in Pregnancy PALLAVIDocument42 pagesPumonary Tuberculosis in Pregnancy PALLAVIJyothsna DeepNo ratings yet
- Central Nervous System InfectionsDocument9 pagesCentral Nervous System InfectionsSaddamNo ratings yet
- Antibiotic Prophylaxis in Gustilo Grade I To III Open Fractures of The Lower LimbV5 - April18th2012Document1 pageAntibiotic Prophylaxis in Gustilo Grade I To III Open Fractures of The Lower LimbV5 - April18th2012Yopi ArdhiaswariNo ratings yet
- AminoglycosideDocument16 pagesAminoglycosideDr. Afreen NasirNo ratings yet
- Wound Infections: Common PathogensDocument1 pageWound Infections: Common PathogensAnonymous KGxzow5zxhNo ratings yet
- Antimicrobial Regimens For The Treatment of Streptococcus Anginosus GDocument2 pagesAntimicrobial Regimens For The Treatment of Streptococcus Anginosus GKhor Chin PooNo ratings yet
- Infeksi Saluran KemihDocument2 pagesInfeksi Saluran KemihFredNo ratings yet
- Antibiotics-Generation OperationDocument5 pagesAntibiotics-Generation OperationZamzami Ahmad FahmiNo ratings yet
- Azithromycin NMFv1.0 Full 20180620Document5 pagesAzithromycin NMFv1.0 Full 20180620Lütfiye ÖzlemNo ratings yet
- Programmed Labour: Dr. Bharti KalraDocument13 pagesProgrammed Labour: Dr. Bharti KalraYoser ThamtonoNo ratings yet
- FLCCC Alliance I Maskplus Protocol EnglishDocument2 pagesFLCCC Alliance I Maskplus Protocol EnglishAlan NNo ratings yet
- Clinical Audit Proposal Form: Obstetrics & GynecologyDocument4 pagesClinical Audit Proposal Form: Obstetrics & GynecologyWeam AlsouriNo ratings yet
- Antibiotic ConversionDocument9 pagesAntibiotic ConversionfabianNo ratings yet
- Antibiotic Guidelines For SKIN AND SOFT TISSUE INFECTIONSDocument11 pagesAntibiotic Guidelines For SKIN AND SOFT TISSUE INFECTIONSlaptopgreyNo ratings yet
- Gui Iia Uk PDFDocument2 pagesGui Iia Uk PDFluckevNo ratings yet
- Amoxicillin - Drug Information - UpToDateDocument47 pagesAmoxicillin - Drug Information - UpToDateMikaela lNo ratings yet
- Profil Ampicillin SulbactamDocument12 pagesProfil Ampicillin SulbactamasriNo ratings yet
- Kodok 123Document2 pagesKodok 123Ferry SukinataNo ratings yet
- FLCCC Alliance I Maskplus Protocol EnglishDocument2 pagesFLCCC Alliance I Maskplus Protocol EnglishThe BFDNo ratings yet
- List of Animal Health Products: Kooperatibang Pangkabuhayan NG Sta. MariaDocument9 pagesList of Animal Health Products: Kooperatibang Pangkabuhayan NG Sta. MariaAlle LunagNo ratings yet
- Uso de Miso en Obstetricia Ipas Mexico PDFDocument39 pagesUso de Miso en Obstetricia Ipas Mexico PDFthedNo ratings yet
- Tetanus Treatment & Management - Approach Considerations, Initial Supportive Therapy and Wound Care, Pharmacologic TherapyDocument11 pagesTetanus Treatment & Management - Approach Considerations, Initial Supportive Therapy and Wound Care, Pharmacologic TherapyFuad Adi PrasetyoNo ratings yet
- Obstetrics and Gynecology Cap17 Man InfDocument8 pagesObstetrics and Gynecology Cap17 Man InfMaría José VallejoNo ratings yet
- My Mifespristone and Misoprostol Story: How I used mifepristone and misoprostol for a successful medical abortion and all you must know about these abortion pillsFrom EverandMy Mifespristone and Misoprostol Story: How I used mifepristone and misoprostol for a successful medical abortion and all you must know about these abortion pillsNo ratings yet
- Intrapartum Ultrasonography for Labor Management: Labor, Delivery and PuerperiumFrom EverandIntrapartum Ultrasonography for Labor Management: Labor, Delivery and PuerperiumNo ratings yet
- A Robust Summary ToDocument2 pagesA Robust Summary ToMuathNo ratings yet
- 0716CP Newman CovDocument7 pages0716CP Newman CovMuathNo ratings yet
- Acute DivetriculitisDocument17 pagesAcute DivetriculitisMuathNo ratings yet
- LP Study GuideDocument45 pagesLP Study GuideMuath100% (1)
- Pre-Internship Module: (Type Here)Document27 pagesPre-Internship Module: (Type Here)MuathNo ratings yet
- Effectiveness of Horizontal Peer-Assisted Learning in Physical Examination PerformanceDocument7 pagesEffectiveness of Horizontal Peer-Assisted Learning in Physical Examination PerformanceMuathNo ratings yet
- SPSS SummaryDocument2 pagesSPSS SummaryMuathNo ratings yet
- 06-Dr. Bajammal Hip Disorders 2017Document48 pages06-Dr. Bajammal Hip Disorders 2017MuathNo ratings yet
- Bowel Obstruction: Abdulqader Taha Almuallim, MBBS General Surgery ResudentDocument19 pagesBowel Obstruction: Abdulqader Taha Almuallim, MBBS General Surgery ResudentMuathNo ratings yet
- Ophthalmology Question: Rheumatoid ArthritisDocument40 pagesOphthalmology Question: Rheumatoid ArthritisMuathNo ratings yet
- Australian Version - Manual and Questionnaires - WHOQOL-100 and BREFDocument89 pagesAustralian Version - Manual and Questionnaires - WHOQOL-100 and BREFMuath100% (1)
- AKI, CKD SummaryDocument4 pagesAKI, CKD SummaryMuathNo ratings yet
- Breech - Management Of: 1. PurposeDocument15 pagesBreech - Management Of: 1. PurposeMuathNo ratings yet
- Emerging Infection SummaryDocument1 pageEmerging Infection SummaryMuathNo ratings yet
- Fetal Blood Sampling: 1. PurposeDocument7 pagesFetal Blood Sampling: 1. PurposeMuathNo ratings yet
- Hypertension Management of Acute 51118Document10 pagesHypertension Management of Acute 51118MuathNo ratings yet
- Postpartum-Haemorrhage 220719 PDFDocument16 pagesPostpartum-Haemorrhage 220719 PDFMuathNo ratings yet
- Vaginal Birth After Caesarean Intrapartum Management 220719Document4 pagesVaginal Birth After Caesarean Intrapartum Management 220719MuathNo ratings yet
- Rupture of Membranes Preterm Premature Pprom 220719Document5 pagesRupture of Membranes Preterm Premature Pprom 220719MuathNo ratings yet
- Drug Study Cefazolin and Vit KDocument2 pagesDrug Study Cefazolin and Vit KFrancis Lawrence AlexanderNo ratings yet
- Cefazolin and DexamethasoneDocument2 pagesCefazolin and Dexamethasonelaude.francesNo ratings yet
- Patzakis Open Fracture Management PDFDocument15 pagesPatzakis Open Fracture Management PDFNurul AtiahNo ratings yet
- Cefazolin Drug StudyDocument2 pagesCefazolin Drug StudyAj GoNo ratings yet
- Dosages and SolutionDocument68 pagesDosages and SolutionRuan MarchessaNo ratings yet
- Ocular Antibiotics and Anti-Infectives: Regis P. Kowalski, MS, M (ASCP)Document16 pagesOcular Antibiotics and Anti-Infectives: Regis P. Kowalski, MS, M (ASCP)Maria SpatariNo ratings yet
- Recent Trends in Staph Bacteremia (AUREUS)Document12 pagesRecent Trends in Staph Bacteremia (AUREUS)lakshminivas PingaliNo ratings yet
- Antibiotic For CellulitisDocument13 pagesAntibiotic For CellulitissinarwatiNo ratings yet
- Antibiotic Prophylaxis in Obstetric ProceduresDocument7 pagesAntibiotic Prophylaxis in Obstetric Proceduresbel4ronaldoeNo ratings yet
- Antibiotic Cross-Sensitivity ChartDocument1 pageAntibiotic Cross-Sensitivity ChartAji YudhaNo ratings yet
- Antibiotics:: Sulfonamides Penicillins Cephalosporins Tetracyclines Aminoglycosides Quinolones MacrolidesDocument67 pagesAntibiotics:: Sulfonamides Penicillins Cephalosporins Tetracyclines Aminoglycosides Quinolones MacrolidesMarcky_467100% (7)
- Cephalosporins, Flouroquinolones and SulfonamidesDocument7 pagesCephalosporins, Flouroquinolones and SulfonamidesErum JanNo ratings yet
- Antimicrobials in A Nutshell 27 JuneDocument37 pagesAntimicrobials in A Nutshell 27 JuneNikita NanwaniNo ratings yet
- Jama Shenoy 2019 RV 180010Document12 pagesJama Shenoy 2019 RV 180010GustavoCalderinNo ratings yet
- CephalexinDocument4 pagesCephalexinCHIEF DOCTOR MUTHUNo ratings yet
- Help Me Pass Nursing School..... Ask Me Anything - Information For Nursing Student and New Nurses From The Dean of A Nursing Program in Texas With 30Document44 pagesHelp Me Pass Nursing School..... Ask Me Anything - Information For Nursing Student and New Nurses From The Dean of A Nursing Program in Texas With 30RizkiWikantyasningNo ratings yet
- Antibiotics and Antibacterial Drugs SDocument67 pagesAntibiotics and Antibacterial Drugs Somar hameed100% (1)
- Acute Management of Open Fractures An Evidence Based Review PDFDocument9 pagesAcute Management of Open Fractures An Evidence Based Review PDFSusPa Naraha100% (1)
- Therapeutic Controversies: Antmi Yric Prophylaxis in Cesarean SectionDocument6 pagesTherapeutic Controversies: Antmi Yric Prophylaxis in Cesarean Sectionnurul wahyuniNo ratings yet
- Medication List and InformationDocument9 pagesMedication List and InformationHealthAndFitnessGuyNo ratings yet
- Antibiotic Prophylaxis: Francis Neil C. CaranayDocument11 pagesAntibiotic Prophylaxis: Francis Neil C. CaranayNdor BariboloNo ratings yet
- Drug Study Cefazolin Module 13Document1 pageDrug Study Cefazolin Module 13Daryl Joy Cortez100% (1)
- 1 SmithKline Corp. Vs Eli Lilly and CompanyDocument3 pages1 SmithKline Corp. Vs Eli Lilly and CompanyKim CajucomNo ratings yet
- CefuroximeDocument14 pagesCefuroximeBentoys StreetNo ratings yet
- Infective EndocarditisDocument18 pagesInfective EndocarditisLee Foo WengNo ratings yet
- Antibiotic Sensitivity December 2015Document1 pageAntibiotic Sensitivity December 2015Jeffery WangNo ratings yet
- Analysis of Prophylactic Antibiotics Usage in Caesarean Section DeliveryDocument6 pagesAnalysis of Prophylactic Antibiotics Usage in Caesarean Section DeliveryyuriNo ratings yet
- Infective Endocarditis Wallet CardDocument2 pagesInfective Endocarditis Wallet CardDani CastilloNo ratings yet
- NCPDocument9 pagesNCPYesha Mae MartinNo ratings yet
- Cellulitis in Adults - Guideline Flowchart Hospital in The Home Guideline For Management at HomeDocument2 pagesCellulitis in Adults - Guideline Flowchart Hospital in The Home Guideline For Management at HomeAnonymous 4txA8N8etNo ratings yet