Professional Documents
Culture Documents
1.12 - The Urinary System
Uploaded by
Uwen NalpOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1.12 - The Urinary System
Uploaded by
Uwen NalpCopyright:
Available Formats
ANAPHY111 FINALS
11
Dr. Ma. Luisa Crisostomo / First Semester
Transcriber: Kathleen Venus 22
THE URINARY SYSTEM
OUTLINE
and Bowman’s capsule,
I. The Urinary System
that filters blood plasma
II. Organs
Outer region of the kidney;
a. Kidney Renal cortex
site of urine production
i. Nephron
Inner region of the kidney;
b. Ureter Renal medulla
site of urine collection
c. Urinary Bladder
d. Urethra Series of tube-like
i. Male Urethra structures within the
Renal tubules
ii. Female Urethra nephron; where urine is
III. Urine Formation and Characteristics formed
IV. Micturition Enzyme released by the
kidneys in response to a
drop in blood pressure that
TERMINOLOGIES Renin
causes the conversion of
Hormone that causes the angiotensinogen into
distal convoluted tubule to angiotensin I
retain sodium, which Measurement that indicates
Aldosterone
leads to the retention of Specific gravity the amount of solid matter
water, resulting in in a liquid
increased blood pressure Process whereby
A plasma protein produced chemicals are removed
when renin is released from Tubular resorption from filtrate in the renal
the kidney; tubules and returned to the
Angiotensin
angiotensin II stimulates blood
the adrenal glands to Process whereby
secrete aldosterone chemicals are added to the
Hormone that inhibits Tubular secretion
filtrate in the renal
diuresis by stimulating the tubules
Antidiuretic hormone
kidneys to Muscular tubes connecting
conserve water Ureters the renal pelvis of each
Two layers of epithelial kidney with the bladder
cells that envelop the Small tube that conveys
Bowman’s capsule glomerulus in an open- Urethra urine away from the
ended covering; also called bladder and out of the body
a glomerular capsule
Collapsible muscular sac
A cup-like structure that
Urinary bladder that stores urine
Calyx collects urine leaving the
papilla of the kidney
Receives drainage from the THE URINARY SYSTEM
distal convoluted tubules of
Collecting duct several different
nephrons; eventually drains
into a minor calyx
Detrusor muscle Wall of the bladder
The secretion of large
Diuresis
amounts of urine
Cluster of capillaries that
Glomerulus are part of the renal
corpuscles in the nephrons
Concave notch on medial
side of kidney; where blood
Hilum vessels, the ureters, and - Composed of the following:
nerves enter and leave the o Kidney
kidney o Ureter
U-shaped portion of the o Urinary Bladder
Loop of Henle o Urethra
renal tubule
Micturition Urination - Functions:
The filtration units of the o Kidneys dispose of waste products in urine
Nephrons
kidney o Kidneys’ regulatory functions include:
- Production of renin to maintain
Network of capillaries
blood pressure
Peritubular capillaries surrounding the renal
- Production of erythropoietin to
tubules
stimulate red blood cell
One of the main
production
Page1
Renal corpuscles components of nephrons,
- Conversion of vitamin D to its
consisting of a glomerulus
active form
[ANPH111] 1.12 THE URINARY SYSTEM – Dr. Ma. Luisa Crisostomo
ORGANS - Collecting ducts collect urine
from both types of nephrons,
KIDNEY through the renal pyramids, to the
- Paired calyces, and then to the renal
- Reddish brown in appearance pelvis
- It has the following coverings: - Two capillary beds associated with each nephron
o Renal Capsule: immediate covering of the o Glomerulus
o kidney - Fed and drained by arterioles
o Perirenal Fat or Perinephric Fat: around ▪ Afferent Arteriole: arises from a
the renal capsule cortical radiate artery and feeds the
o Renal fascia or Gerota’s fascia: external to glomerulus
perirenal fat; continuous with transversalis ▪ Efferent Arteriole: receives blood that
fascia has passed through the glomerulus
o Pararenal or Paranephric Fat: outermost - Specialized for filtration
- 2 parts of kidney: - High pressure forces fluid and solutes out of
o Cortex: outer blood and into the glomerular capsule
o Medulla: inner o Peritubular capillary bed
- Renal Pyramids: triangle - Arise from the efferent arteriole of the
- Renal Column: extension of glomerulus
cortex towards the medulla; - Low-pressure, porous capillaries
between the pyramids - Adapted for absorption instead of filtration
- Renal Pelvis: union of major - Cling close to the renal tubule to receive
calyces solutes and water from tubule cells
- Major Calyx: union of minor - Drain into the interlobar veins
calyces
NEPHRON
- Structural and functional unit of the kidney
- 1 million nephron each kidney
- Each nephron consists of two main structures:
o Renal corpuscle
- Glomerulus: A knot of capillaries
made of podocyte
- Glomerular (Bowman’s) capsule
is a cup-shaped structure that
surrounds the glomerulus
o Renal tubule
- Extends from glomerular capsule
and ends when it empties into the
collecting duct
URETER
- From the glomerular (Bowman’s)
- 10 inches long muscular tube
capsule, the subdivisions of the
- 3 anatomical constrictions:
renal tubule are:
o at the uretero-pelvic junction
• Proximal convoluted o where iliac vessels cross the ureter
tubule (PCT) o where it joins the urinary bladder
• Nephron loop (loop of
Henle) URINARY BLADDER
• Distal convoluted tubule - Hollow muscular organ
(DCT) - Temporary storage of urine
- Cortical nephrons - Will contain folds called rugae; without rugae called
- Located entirely in the cortex trigone – smooth area
- Include most nephrons - Inner – trigone occupied by ureteral orifices and
- Juxtamedullary nephrons urethral orifice
- Found at the cortex-medulla - Wall of the urinary bladder
junction o Three layers of smooth muscle collectively
- Nephron loop dips deep into the called the detrusor muscle
Page2
medulla o Mucosa made of transitional epithelium
[ANPH111] 1.12 THE URINARY SYSTEM – Dr. Ma. Luisa Crisostomo
o Walls are thick and folded in an empty URINE FORMATION AND CHARACTERISTICS
urinary bladder Urine formation is the result of three processes
o Urinary bladder can expand significantly 1. Glomerular filtration
without increasing internal pressure - The glomerulus is a filter
- Capacity of the urinary bladder - Filtration is a nonselective passive process
o A moderately full bladder is about 5 inches o Water and solutes smaller than proteins
long and holds about 500 ml of urine are forced through glomerular capillary
o Capable of holding twice that amount of walls
urine o Proteins and blood cells are normally too
large to pass through the filtration
URETHRA membrane
- Thin-walled tube that carries urine from the urinary o Once in the capsule, fluid is called filtrate
bladder to the outside of the body by peristalsis o Filtrate leaves via the renal tubule
- Release of urine is controlled by two sphincters - Filtrate will be formed as long as systemic blood
o Internal urethral sphincter: Involuntary and pressure is normal
made of smooth muscle o If arterial blood pressure is too low, filtrate
o External urethral sphincter: Voluntary and formation stops because glomerular
made of skeletal muscle pressure will be too low to form filtrate
2. Tubular reabsorption
MALE URETHRA - The peritubular capillaries reabsorb useful
1. Prostatic Urethra substances from the renal tubule cells, such as:
- widest, most dilatable, prostate gland o Water
2. Membranous Urethra o Glucose
- traverses’ urogenital diaphragm, shortest and least o Amino acids
dilatable o Ions
3. Penile (Spongy) Urethra - Some reabsorption is passive; most is active (ATP)
- longest, traverses corpus spongiosum - Most reabsorption occurs in the proximal
convoluted tubule
3. Tubular secretion
- Reabsorption in reverse
- Some materials move from the blood of the
peritubular capillaries into the renal tubules to be
eliminated in filtrate
o Hydrogen and potassium ions
o Creatinine
- Secretion is important for:
o Getting rid of substances not already in the
filtrate
o Removing drugs and excess ions
o Maintaining acid-base balance of blood
- Materials left in the renal tubule move toward the
ureter
o Nitrogenous wastes
▪ Nitrogenous waste products are
poorly reabsorbed, if at all
▪ Tend to remain in the filtrate and
are excreted from the body in the
FEMALE URETHRA urine
- About 3 to 4 cm (1.5 inches long) • Urea: end product of
- Located anterior to the vaginal opening protein breakdown
• Uric acid: results from
nucleic acid metabolism
• Creatinine: associated
with creatine metabolism
in muscles
- In 24 hours, about 1.0 to 1.8 liters of urine are
produced
Urine and filtrate are different
- Filtrate contains everything that blood plasma does
(except proteins)
- Urine is what remains after the filtrate has lost most
of its water, nutrients, and necessary ions through
reabsorption
- Urine contains nitrogenous wastes and substances
that are not needed
Urine characteristics
- Clear and pale to deep yellow in color
- Yellow color is normal and due to the pigment
urochrome (from the destruction of hemoglobin) and
solutes
o Dilute urine is a pale, straw color
- Sterile at the time of formation
Page3
- Slightly aromatic, but smells like ammonia with time
[ANPH111] 1.12 THE URINARY SYSTEM – Dr. Ma. Luisa Crisostomo
- Slightly acidic (pH of 6)
- Specific gravity of 1.001 to 1.035
Solutes normally found in urine
- Sodium and potassium ions
- Urea
- Uric acid
- creatinine
- Ammonia
- Bicarbonate ions
Solutes NOT normally found in urine
- Glucose
- Blood proteins
- Red blood cells
- Hemoglobin
- WBCs (pus)
- Bile
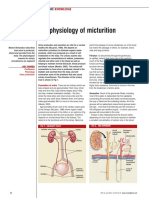
MICTURITION
- Voiding, or emptying of the urinary bladder
- Two sphincters control the release of urine, the
internal urethral sphincter and external urethral
sphincter
o Bladder collects urine to 200 ml
o Stretch receptors transmit impulses to the
sacral region of the spinal cord
o Impulses travel back to the bladder via the
pelvic splanchnic nerves to cause bladder
contractions
o When contractions become stronger, urine
is forced past the involuntary internal
sphincter into the upper urethra
o Urge to void is felt
o The external sphincter is voluntarily
controlled, so micturition can usually be
o delayed
o Fluid, Electrolyte, and Acid-Base Balance
o Blood composition depends on three
factors
▪ Diet
▪ Cellular metabolism
▪ Urine output
Page4
You might also like
- EXCRETORY PHYSIOLOGYDocument6 pagesEXCRETORY PHYSIOLOGYKUMAR SUMITNo ratings yet
- Excretion in Humans IX NOTESDocument6 pagesExcretion in Humans IX NOTESEalaf AliNo ratings yet
- Renal Physiology PDFDocument12 pagesRenal Physiology PDFLolitaNo ratings yet
- Final Exam Review - Bio 172Document21 pagesFinal Exam Review - Bio 172Erin McElhaney QuirkNo ratings yet
- Clinical Chemistry 1 - The Functions and Parts of the KidneyDocument1 pageClinical Chemistry 1 - The Functions and Parts of the KidneyShania DawnNo ratings yet
- The Urinary System & Fluid BalanceDocument8 pagesThe Urinary System & Fluid BalanceMarianne DugosNo ratings yet
- Seeley's Essentials of Anatomy & Physiology Chapter 18: Urinary System and Fluid BalanceDocument20 pagesSeeley's Essentials of Anatomy & Physiology Chapter 18: Urinary System and Fluid BalanceAce Khiel Peralta100% (1)
- Formation of Urine: Formation of UrineDocument14 pagesFormation of Urine: Formation of UrineMegbaruNo ratings yet
- Renal-FunctionDocument11 pagesRenal-FunctionJanely EstreraNo ratings yet
- Excretory System 2.0Document6 pagesExcretory System 2.0Kim DahyunNo ratings yet
- Urinary SystemDocument2 pagesUrinary SystemIzelwyn DaguioNo ratings yet
- 3.4 Homeostasis in Humans (Volume 2) : Prepared By: PN Nadhirah Binti Abdul Haziz Biology Teacher SMK Puteri WilayahDocument15 pages3.4 Homeostasis in Humans (Volume 2) : Prepared By: PN Nadhirah Binti Abdul Haziz Biology Teacher SMK Puteri WilayahPutri MalayaNo ratings yet
- Aubf Lec 2 Trans 2Document4 pagesAubf Lec 2 Trans 2Aj MondejarNo ratings yet
- Chapter 18: Urinary System and Fluid Balance: TH RDDocument3 pagesChapter 18: Urinary System and Fluid Balance: TH RDPrecious Faith RodriguezNo ratings yet
- Compare and Contrast Process in Plants and Animals PDFDocument32 pagesCompare and Contrast Process in Plants and Animals PDFLyca Gunay100% (4)
- Anph FinalsDocument42 pagesAnph FinalsVincent BustamanteNo ratings yet
- Human excretion and the urinary systemDocument30 pagesHuman excretion and the urinary system20I1190 G-7CNo ratings yet
- Urinalysis Anatomy and PhysiologyDocument3 pagesUrinalysis Anatomy and PhysiologyMonica DomingoNo ratings yet
- Anatomy and Physiology Handout # 17 Urinary SystemDocument8 pagesAnatomy and Physiology Handout # 17 Urinary SystemJounri Arsted Dimabuyu (Kaiz)No ratings yet
- Urinary-systemDocument3 pagesUrinary-systempsychelastwishNo ratings yet
- Anph FinalsDocument44 pagesAnph FinalsVincent BustamanteNo ratings yet
- Urinary SystemDocument5 pagesUrinary Systemydnic alykPNo ratings yet
- MC I Modular Reviewer Urinary SystemDocument12 pagesMC I Modular Reviewer Urinary SystemSteiner LimNo ratings yet
- Anatomy Excretory System NotesDocument5 pagesAnatomy Excretory System NotesrincyNo ratings yet
- The Nephrons and Urine FormationDocument8 pagesThe Nephrons and Urine FormationOdessa RatioNo ratings yet
- Excretion in Humans IgcseDocument30 pagesExcretion in Humans IgcseAdrian KW NGNo ratings yet
- Chapter 26: Introduction To The Urinary SystemDocument37 pagesChapter 26: Introduction To The Urinary Systemmaatela7sasNo ratings yet
- Renal Medulla: BloodDocument4 pagesRenal Medulla: BloodLindsay GabrielNo ratings yet
- Urina Rysystem: FunctionsDocument3 pagesUrina Rysystem: FunctionsGracia Dela CruzNo ratings yet
- Excretion in Humans Igcse BiologyDocument26 pagesExcretion in Humans Igcse BiologyThe PassionNo ratings yet
- YU - Activity 11 - Urinary SystemDocument5 pagesYU - Activity 11 - Urinary SystemDenise Kyla Bernadette YuNo ratings yet
- The Urinary and Reproductive System (J.R) - Policarpio MAT Gen. Sci.Document60 pagesThe Urinary and Reproductive System (J.R) - Policarpio MAT Gen. Sci.john ronald PolicarpioNo ratings yet
- OS 206 Renal PhysiologyDocument9 pagesOS 206 Renal Physiologyalphius_mendoza100% (1)
- Biochem Lab Prelim ReviewerDocument5 pagesBiochem Lab Prelim Revieweramethys manuelNo ratings yet
- The Excretory SystemDocument3 pagesThe Excretory SystemMariel Abatayo0% (1)
- EXCRETORYDocument6 pagesEXCRETORYMohd. ArhanNo ratings yet
- (Week 16) Urinary SystemDocument3 pages(Week 16) Urinary SystemDiana Leen Dela CruzNo ratings yet
- Lecture 19 Urinary Sys BIOL3571 F2023Document55 pagesLecture 19 Urinary Sys BIOL3571 F2023thesoccerprince.10No ratings yet
- Clinical Micrsocopy 1.2Document5 pagesClinical Micrsocopy 1.2monzon.mika1801No ratings yet
- #1 Anatomi Fisiologi Urogenital SystemDocument4 pages#1 Anatomi Fisiologi Urogenital SystemNur azriyati PutriNo ratings yet
- Lec 18Document4 pagesLec 18Lyanna Louise SantosNo ratings yet
- Bladder IrrigationDocument3 pagesBladder IrrigationMyfanway Am-isNo ratings yet
- ANPH111 REVIEWER [URINARY & ENDOCRINE]Document7 pagesANPH111 REVIEWER [URINARY & ENDOCRINE]Maria Clarisse ReyesNo ratings yet
- From The Capillaries Into The Capsule ThroughDocument3 pagesFrom The Capillaries Into The Capsule ThroughRashid DayaoNo ratings yet
- Understanding Medical Surgical Nursing - 0849-0849Document1 pageUnderstanding Medical Surgical Nursing - 0849-0849Anas TasyaNo ratings yet
- 2 - Renal PhysiologyDocument8 pages2 - Renal PhysiologyKunware TropaNo ratings yet
- 6 Bodyfluidregulationandexcretionc-150331101430-Conversion-Gate01Document11 pages6 Bodyfluidregulationandexcretionc-150331101430-Conversion-Gate01Yay SandovalNo ratings yet
- Excretion and Homeostatsis NotesDocument12 pagesExcretion and Homeostatsis NotesrissNo ratings yet
- Urinary SystemDocument9 pagesUrinary SystemPrincess OrsinoNo ratings yet
- Anatomy and Physiology Handout # 17 Urinary SystemDocument8 pagesAnatomy and Physiology Handout # 17 Urinary SystemJounri Arsted Dimabuyu (Kaiz)No ratings yet
- 030722the Physiology of MicturitionDocument3 pages030722the Physiology of MicturitionAnnizah Paramitha100% (1)
- CH ExcretionDocument9 pagesCH ExcretionlatasabarikNo ratings yet
- Kidney Failure and Exceretory System PosterDocument3 pagesKidney Failure and Exceretory System Poster岡本永真No ratings yet
- EXCRETIONDocument9 pagesEXCRETIONMaira CanashinNo ratings yet
- (BIO) Chapter 9 - Excretion in HumansDocument14 pages(BIO) Chapter 9 - Excretion in Humansanya desilvaNo ratings yet
- W8 Year 11 Topic 3 Excretory System WritableDocument4 pagesW8 Year 11 Topic 3 Excretory System WritableAmber YipNo ratings yet
- Three-Part Kidney FormationDocument3 pagesThree-Part Kidney FormationAngel IsalesNo ratings yet
- Urinary SystemDocument10 pagesUrinary SystemAly HannahNo ratings yet
- Excretory System Chapter 9thDocument4 pagesExcretory System Chapter 9thशंकराय नमोNo ratings yet
- Cellular and Molecular Approaches to Fish Ionic RegulationFrom EverandCellular and Molecular Approaches to Fish Ionic RegulationNo ratings yet
- Correlation AnalysisDocument54 pagesCorrelation AnalysisUwen Nalp100% (1)
- ANPH-M2-CU6. Nervous SystemDocument33 pagesANPH-M2-CU6. Nervous SystemMary Grace MapulaNo ratings yet
- 1.14 - Special SensesDocument5 pages1.14 - Special SensesUwen NalpNo ratings yet
- ANPH111 Cardiovascular System OverviewDocument7 pagesANPH111 Cardiovascular System OverviewUwen NalpNo ratings yet
- 1.14 - Graphic Communication and Public Service AnnouncementDocument1 page1.14 - Graphic Communication and Public Service AnnouncementUwen NalpNo ratings yet
- 1.13 - The Endocrine SystemDocument6 pages1.13 - The Endocrine SystemUwen NalpNo ratings yet
- 1.13 - Types of CommunicationDocument2 pages1.13 - Types of CommunicationUwen NalpNo ratings yet
- 1.12 Locsin, AgravanteDocument3 pages1.12 Locsin, AgravanteUwen NalpNo ratings yet
- 1.11 - The Information AgeDocument2 pages1.11 - The Information AgeUwen NalpNo ratings yet
- Biodiversity and a Healthy Society in the PhilippinesDocument3 pagesBiodiversity and a Healthy Society in the PhilippinesUwen NalpNo ratings yet
- 1.11 - 1.12 Communication For Work Purposes and Listening SkillsDocument2 pages1.11 - 1.12 Communication For Work Purposes and Listening SkillsUwen NalpNo ratings yet
- ARTA111 FINALS - Contemporary ArtDocument4 pagesARTA111 FINALS - Contemporary ArtUwen NalpNo ratings yet
- 1.11 - Non-Nursing Theories Relevant To Nursing PracticeDocument6 pages1.11 - Non-Nursing Theories Relevant To Nursing PracticeUwen NalpNo ratings yet
- Topic 3 BRUNEI The Oilfields LabourersDocument3 pagesTopic 3 BRUNEI The Oilfields LabourersRichmond BlancoNo ratings yet
- FAA Instrument Rating Oral Exam PrepDocument8 pagesFAA Instrument Rating Oral Exam Prepvino chandrakumarNo ratings yet
- Pest Management Practices of Farmers in PambujanDocument13 pagesPest Management Practices of Farmers in PambujanLucille MoralesNo ratings yet
- Dr. P S Adhya 7186Document1 pageDr. P S Adhya 7186Partha AdhyaNo ratings yet
- Module 2Document29 pagesModule 2Melody SorianoNo ratings yet
- St. Patrick's DayDocument3 pagesSt. Patrick's DayRobin LamNo ratings yet
- SAMSUNG LCD Service Manual (Internal) - ES15UDocument81 pagesSAMSUNG LCD Service Manual (Internal) - ES15Umeng798651No ratings yet
- Case Study Fire IncidentDocument7 pagesCase Study Fire IncidentD21Sanjana Ubale100% (1)
- Sterilisator Hansin KoreaDocument2 pagesSterilisator Hansin KoreaanggaNo ratings yet
- Lady Wachter's Cult of Darkness InvestigationDocument11 pagesLady Wachter's Cult of Darkness InvestigationWellington Valentin100% (1)
- Pharma AssignDocument8 pagesPharma AssignTHIS PAHADINo ratings yet
- Recent Task 2 Essay Questions 2Document28 pagesRecent Task 2 Essay Questions 2esraaalhajNo ratings yet
- Jounal Club 1 BagavathDocument13 pagesJounal Club 1 Bagavathpraveen kumarNo ratings yet
- AMAZEN Manual ForWebONLY 2 5 19 PDFDocument13 pagesAMAZEN Manual ForWebONLY 2 5 19 PDFkg27r-scribd9325100% (1)
- Ultra-low Profile Dome Key Adds Single-key TypeDocument3 pagesUltra-low Profile Dome Key Adds Single-key TypeMuhamad PriyatnaNo ratings yet
- Cause: Lymphatic System Oriental Rat Flea Human Flea Septicemic PlagueDocument3 pagesCause: Lymphatic System Oriental Rat Flea Human Flea Septicemic PlagueMattNo ratings yet
- Journey by Night EssayDocument2 pagesJourney by Night Essaystillwakingsleep100% (2)
- Human Rights in The PhilippinesDocument2 pagesHuman Rights in The PhilippinesSharmaine FranciscoNo ratings yet
- Grapho CyberneticsDocument3 pagesGrapho CyberneticsmysticblissNo ratings yet
- Ibat-ibang dulog sa paghawak ng klaseDocument2 pagesIbat-ibang dulog sa paghawak ng klaseJovito Limot100% (3)
- Long-Term Memory - ProcessDocument30 pagesLong-Term Memory - ProcessALEXANDRA SAN PEDRONo ratings yet
- CALIMOVEDocument46 pagesCALIMOVERasheedAladdinNGuiomala0% (1)
- Quality Management System: ISO 9001 - 2000 ClausesDocument18 pagesQuality Management System: ISO 9001 - 2000 ClausesRambabuNo ratings yet
- Math ProjectDocument18 pagesMath ProjectChar LotteNo ratings yet
- Notes-RJ Speed Seduction Gold WalkupsDocument7 pagesNotes-RJ Speed Seduction Gold Walkupsdulixuexi100% (1)
- Rundingan Perdagangan Antara Malaysia Dan Indonesia Di Wisma Putra, Kuala Lumpur 1967Document15 pagesRundingan Perdagangan Antara Malaysia Dan Indonesia Di Wisma Putra, Kuala Lumpur 1967nixyingboNo ratings yet
- Fuel System Upgrades For Your QSK-60Document6 pagesFuel System Upgrades For Your QSK-60Josh JonesNo ratings yet
- Banas Bio-Gas PlantDocument30 pagesBanas Bio-Gas Plantjugal rana100% (1)
- Pulseless Arrest Algorithm For Managing AsystoleDocument1 pagePulseless Arrest Algorithm For Managing AsystoleLady MuffinsNo ratings yet
- Mole Calculation Worksheet: Practice & SolutionsDocument3 pagesMole Calculation Worksheet: Practice & SolutionsQurrat Ul AinNo ratings yet










































![ANPH111 REVIEWER [URINARY & ENDOCRINE]](https://imgv2-2-f.scribdassets.com/img/document/719863043/149x198/56e32fc029/1712198043?v=1)